Abstract
Social capital could protect mental health. We examined whether the COVID-19 context and province-level COVID-19 situation altered the longitudinal association between cognitive social capital (generalized trust, trust in neighbors, trust in local government officials, and reciprocity) and depression. Results from multilevel mixed-effects linear regression models showed that trust in neighbors, trust in local government officials, and reciprocity were more crucial in longitudinally reducing depression in 2020 than in 2018. Also, as compared with provinces where the COVID-19 situation was less poor, trust in local government officials in 2018 was more crucial in reducing depression in 2020 in provinces with a worse COVID-19 situation. Therefore, cognitive social capital should be taken into account for pandemic preparedness and mental health resilience.
Keywords: Cognitive social capital, COVID-19, Depression, Longitudinal association, Pandemic preparedness, China
1. Introduction
The COVID-19 pandemic has affected every aspect of human society, from the economy and politics on the macro level to livelihoods and socializing on the individual level. Regarding its impact on population health, in addition to the millions of COVID-19 cases and deaths worldwide (Dong et al., 2020), the pandemic also triggered a mental health crisis. As estimated, the pandemic caused a 27.6% increase in cases of major depressive disorder globally in 2020 (COVID-19 Mental Disorders Collaborators, 2021).
Social capital, broadly referring to resources available to members of social groups and social networks (Villalonga-Olives and Kawachi, 2015), was considered a social determinant of mental health (Lund et al., 2018) and, therefore, may protect mental health against the pandemic. As a concept imported from social science, social capital was conceptualized in two approaches in public health studies: the network approach and the cohesion approach (Moore and Kawachi, 2017). The network approach mainly follows Lin (1999) and conceptualizes social capital as social resources embedded in individuals’ social networks, whereas the cohesion approach mainly follows Putnam (2000) and Coleman (1988) and emphasizes structural and cognitive dimensions of social capital. Structural social capital refers to the degree to which individuals participate in social networks, associations, and civic events and emphasizes what people do; in contrast, cognitive social capital refers to perceptions of trust and reciprocity and emphasizes what people feel (Kawachi et al., 2008). A systematic review showed that cognitive social capital was protective against developing common mental disorders (CMD), while results about structural social capital and CMD were less consistent (Ehsan and De Silva, 2015). A previous study even found that greater structural social capital was associated with worse mental health in some specific circumstances (Thuy and Berry, 2013).
Social capital could also protect mental health following natural disasters, such as the 2005 Hurricane Katrina in the US (Beaudoin, 2007), the 2008 Wenchuan earthquake in China (Zhao, 2013), and the 2011 Great East Japan Earthquake and Tsunami (Kawachi et al., 2020). Moreover, pre-disaster social capital was conducive to disaster resilience. As shown previously, pre-disaster social capital could facilitate survivors' housing reconstruction after the 2008 Wenchuan earthquake (Wei and Han, 2018) and lower older survivors' risk of developing posttraumatic stress disorder (PTSD) after the 2011 Great East Japan Earthquake and Tsunami (Hikichi et al., 2016). Furthermore, social capital was more important in protecting mental health for survivors with more severe housing damage than for those with less severe housing damage (Hikichi et al., 2017, 2018), suggesting that disaster experiences moderated the association between social capital and survivors’ mental health.
Although the COVID-19 pandemic differs from natural disasters as it requires physical distancing and lasts for months, even years, it still shares some similarities with natural disasters regarding the impact on human life. Previous research showed that during the COVID-19 pandemic, social capital was also associated with better mental health (Chan et al., 2021). Moreover, pre-COVID-19 cognitive social capital could reduce older people's risk of developing depressive symptoms during COVID-19 (Sato et al., 2022). Additionally, neighborhood social support could buffer the negative effect of COVID-19-related stressors on psychological distress (Chen et al., 2021), indicating that COVID-19 experiences might also moderate the association between social capital and mental health.
However, few studies have compared the longitudinal association between social capital and mental health in a disaster/pandemic scenario with that in a pre-disaster/pre-pandemic scenario. Therefore, it is unclear whether social capital is more or less important in prospectively protecting mental health when facing a disaster or a pandemic as compared with facing no such event. Moreover, within a disaster/pandemic scenario, ecological-level severity of the situation may serve as a contextual effect threatening mental health. Nevertheless, previous studies mainly focused on whether social capital was more important in protecting mental health as individual-level disaster-related damage (e.g., housing damage) increased, but few studies examined how the strength of the association between social capital and mental health varied as ecological-level disaster/pandemic situations escalated.
We aim to fill the above-mentioned research gap with a focus on the early stage of the COVID-19 pandemic in China. China experienced its first large-scale COVID-19 outbreak in early 2020. To contain the first COVID-19 outbreak, China implemented a strict lockdown of Wuhan, the epicenter of China's first COVID-19 outbreak, on January 23rd, 2020. Following the lockdown of Wuhan, provinces around the country issued Tier 1 public health emergency responses between January 23rd and January 29th, 2020 (State Council, 2020). The first outbreak was generally under control since mid-March 2020, and at the end of April, China entered a “normalization” stage of COVID-19 prevention and control defined by the Chinese government (State Council, 2020). In this study, we measured peri-COVID-19 depression in 2020 during the “normalization” stage of COVID-19 prevention and control (State Council, 2020). During the time of data collection in 2020, the Chinese government had not proposed the “Dynamic Zero-COVID-19” policy.
Specifically, using a prospective cohort survey in China, which included two waves of data before COVID-19 and one after the end of the first COVID-19 outbreak in China, we examined whether the longitudinal association between social capital and depression in the peri-COVID-19 context was stronger compared with the pre-COVID-19 context. Furthermore, we examined within the COVID-19 context (i.e., 2020) whether the association between pre-COVID-19 social capital (in 2016 and 2018) and peri-COVID-19 depression became stronger in provinces with worse COVID-19 situations. We focused on cognitive social capital in this study. By examining the association between pre-COVID-19 cognitive social capital and peri-COVID-19 depression, this study can contribute to understanding the role of cognitive social capital in pandemic preparedness.
2. Methods
2.1. Data source and participants
We employed data from 2016, 2018, and 2020 waves of the China Family Panel Studies (CFPS) in the main analysis, with 2016 as the baseline. We further used the data collected in 2014 in the sensitivity analysis. CFPS surveys were conducted by face-to-face interviews before the COVID-19 pandemic. However, in 2020, due to the COVID-19 pandemic, CFPS surveys were mainly conducted through telephone surveys. The 2020 data was collected from July to December 2020, after the first outbreak of COVID-19 in China.
CFPS is a nationally representative longitudinal household survey in China conducted by Peking University since 2010. CFPS used a multi-stage probability strategy for sampling. Generally, at the first stage, CFPS sampled county-level administrative regions within each province using systematic probability proportional to size (PPS) sampling. Second, within each selected county-level administrative region, CFPS selected communities using systematic PPS sampling. At the third stage, CFPS randomly sampled households in selected communities using systematic sampling based on maps of dwelling units in each selected community. Finally, all the household members in the selected households were surveyed. More details of the sampling design can be found in previous literature (Xie and Lu, 2015).
It should be noted that according to the CFPS project team (Xie and Lu, 2015), CFPS contains oversamples in five province-level administrative regions (“provinces” hereafter) so that the samples from the five provinces can be representative of the populations in each of the five provinces. To deal with the oversampling issue, CFPS conducted resampling within the sample of the five provinces. The resampled data within the five provinces and data from other provinces comprised a nationally representative sample (Xie and Lu, 2015). The CFPS dataset provided a variable to help users to identify the resampled nationally representative sample. In our study, we employed the resampled nationally representative sample.
The participants of our study were Chinese aged 16 years old or above. As mentioned above, CFPS planned to collect information from all the household members in the selected households. When household members could not be contacted to complete the survey, CFPS invited selected participants to answer objective questions for their uncontactable household members. However, participants could not help their household members to answer subjective questions, including depression. Hence, these uncontactable household members with no data about depression were excluded, resulting in a sample size of 21,762 in 2016. Among the 21,762 participants, 10,431 were successfully followed up in both 2018 and 2020, and 9819 had complete data on all variables. Therefore, the 9819 participants comprised our analytical sample. We conducted a sensitivity analysis detailed below to account for the loss of follow-up.
Additionally, we obtained the number of province-level COVID-19 cases and deaths from the 2019 Novel Coronavirus Visual Dashboard (Dong et al., 2020), and obtained population density data from National Bureau of Statistic of China (National Bureau of Statistic of China, 2022).
2.2. Measurements
The outcome was a depression score assessed by the 8-item Center for Epidemiological Studies-Depression Scale (CES-D-8) (Turvey et al., 1999) (Cronbach's α = 0.7779, 0.7644, and 0.7731 in 2016, 2018, and 2020, respectively), which is a short version of CES-D-20 (Radloff, 1977). The depression score ranged from 0 to 24, with a higher score indicating a greater level of depression. Depression was measured in 2016, 2018, and 2020 consistently.
We measured cognitive social capital in 2016 and 2018 separately using generalized trust (low/high), trust in neighbors (0–10), trust in local government (county/district government) officials (0–10), and reciprocity (low/high) consistently (Supplementary Table S1). In the questionnaire of CFPS, generalized trust and reciprocity were measured using binary variables. In contrast, trust in neighbors and trust in local government officials were measured using a scale from 0 to 10. In this study, we employed the original measurement of the above four variables as in the CFPS questionnaire.
We regarded the survey year 2020 as representing the COVID-19 context. Additionally, within the COVID-19 context, we assessed the province-level COVID-19 situation using the cumulative number of COVID-19 cases and deaths (on logarithmic scales) in each province up to May 2nd, 2020, when Hubei lifted the Tier 1 public health emergency response. Hubei was the last province to lift the Tier 1 public health emergency response after the end of the first COVID-19 outbreak in China. As the cumulative number of cases and the cumulative number of deaths (on logarithmic scales) were highly correlated with each other (Pearson's correlation coefficient = 0.7518), we employed factor analysis to combine the cumulative number of cases and deaths as a factor score (Supplementary Table S2). Moreover, we also used the cumulative number of cases and deaths separately in the regression analysis.
Additionally, we included sociodemographic factors, socioeconomic factors, lifestyle factors, place of residence, and physical discomfort as covariates. We measured all covariates consistently using data in 2016 and 2018 separately. Specially, we included gender (female vs. male), age groups, ethnicity (Han vs. non-Han) and marital status (single/divorced/widowed vs. cohabit/married) as sociodemographic factors, and education (no formal education, primary school, junior secondary school, senior secondary school, and college or above), quintiles of equivalized household income, and employment status (non-employed (unemployed/students/not in the labor market) vs. employed) as socioeconomic factors. We calculated equivalized household income by dividing household income in the past 12 months by the square root of the number of household members (OECD, 2012).
We also included smoking (no vs. yes), drinking (no vs. yes), and frequency of exercise in the past week (0, once or twice, 3–5 times, 6 times or above) as lifestyle factors (Supplementary Table S1). Furthermore, we included the regions of participants' residence (eastern, middle, western, or northeastern) (National Bureau of Statistics of China, 2011) and whether the participant was living in a rural or urban area as place of residence. Additionally, we adjusted for participants’ physical discomfort (no vs. yes) (Supplementary Table S1).
2.3. Statistical analysis
We conducted descriptive statistics and reported mean with standard deviations (SD) for continuous variables and frequency with percentages for categorical variables. We performed two-sample t-tests and ANOVA to test the difference in depression scores by sample characteristics at baseline.
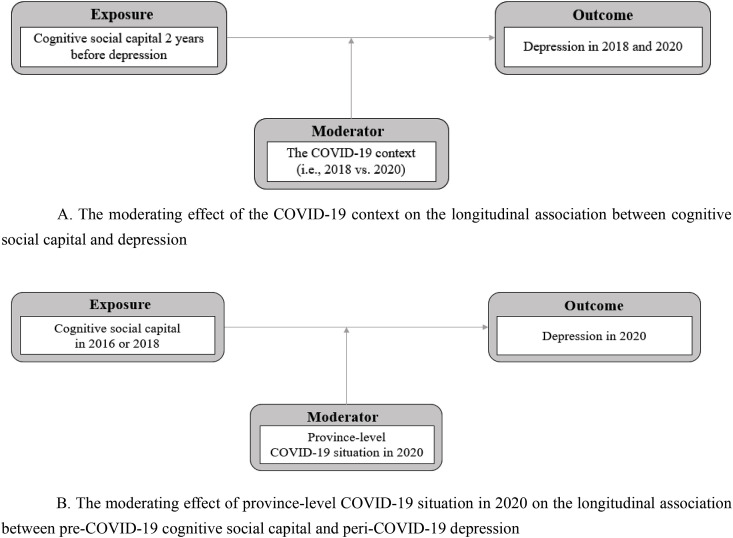
The data had a three-level hierarchical structure each year: individuals (level-1) were nested within households (level-2), and households were nested within provinces (level-3). When the analysis involved repeated measures on the same individual, the data structure would have four levels: observations (level-1) were nested within individuals (level-2), individuals were nested within households (level-3), and households were nested within provinces (level-4). Therefore, we performed multilevel mixed-effects linear regression models with random intercepts to examine the moderating effect of the COVID-19 context and province-level COVID-19 situation on the longitudinal association between cognitive social capital and depression. We examined the moderating effect of the COVID-19 context using interaction terms between cognitive social capital indicators and year (Fig. 1 A), and examined the moderating effect of province-level COVID-19 situation using interaction terms between cognitive social capital indicators and province-level COVID-19 situation (Fig. 1B). We examined each interaction term, one at a time, in multilevel mixed-effects linear regression models (Hosmer and Lemeshow, 2000). We adjusted for lagged covariates and lagged depression in all models. Specifically, if the outcome was depression score in 2018, then the exposures (i.e., cognitive social capital) and all covariates would be measured in 2016, and the depression score in 2016 would also be adjusted for. Similarly, if the outcome was depression score in 2020, then the exposure (i.e., cognitive social capital) and all covariates would be measured in 2018, and the depression score in 2018 would also be adjusted for. In other words, we included lagged exposures, lagged covariates, and lagged dependent variables in the above-mentioned regression models and the lagged period was 2 years. When we examined the longitudinal association between cognitive social capital in 2016 and depression in 2020, we adjusted for covariates as well as depression in 2016. In this case, the lagged period was 4 years.
Fig. 1.
Analytical framework
A. The moderating effect of the COVID-19 context on the longitudinal association between cognitive social capital and depression
B. The moderating effect of province-level COVID-19 situation in 2020 on the longitudinal association between pre-COVID-19 cognitive social capital and peri-COVID-19 depression.
We also conducted several sensitivity analyses detailed in the results section. We analyzed the data using Stata/MP 14.2, with a p-value <0.05 considered to be statistically significant.
3. Results
3.1. Descriptive statistics
Table 1 shows that the depression score increased by 0.46 from 4.90 (SD = 3.90) in 2016 to 5.36 (SD = 3.83) in 2018. Between 2018 and 2020, it increased by 0.17 from 5.36 (SD = 3.83) to 5.53 (SD = 4.08). In other words, no acceleration of the upward trend of depression was observed in China. Table 1 also shows that greater baseline cognitive social capital was associated with a lower depression score at baseline and follow-ups.
Table 1.
Depression from 2016 to 2020 by sample characteristics at baseline, China.
| n (%)/Mean (SD) | Depression in 2016 |
Depression in 2018 |
Depression in 2020 |
||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | p valuea | Mean (SD) | p valuea | Mean (SD) | p valuea | ||
| Total | 9819 (100.00%) | 4.90 (3.90) | 5.36 (3.83) | 5.53 (4.08) | |||
| Sociodemographic factors | |||||||
| Gender | <0.001 | <0.001 | <0.001 | ||||
| Female | 5037 (51.30%) | 5.24 (3.96) | 5.77 (3.90) | 5.89 (4.11) | |||
| Male | 4782 (48.70%) | 4.53 (3.80) | 4.94 (3.71) | 5.14 (4.02) | |||
| Age groups (years) | <0.001 | <0.001 | 0.003 | ||||
| 16-29 | 2042 (20.80%) | 4.39 (3.23) | 4.99 (3.36) | 5.21 (3.64) | |||
| 30-39 | 1704 (17.35%) | 4.82 (3.48) | 5.50 (3.47) | 5.52 (3,67) | |||
| 40-49 | 2211 (22.52%) | 5.14 (4.10) | 5.62 (4.01) | 5.70 (4.16) | |||
| 50-59 | 1988 (20.25%) | 5.00 (4.09) | 5.34 (4.01) | 5.58 (4.32) | |||
| 60-69 | 1444 (14.71%) | 5.15 (4.41) | 5.40 (4.13) | 5.59 (4.47) | |||
| ≥70 | 430 (4.38%) | 5.03 (4.39) | 5.25 (4.27) | 5.74 (4.56) | |||
| Ethnicity | <0.001 | <0.001 | <0.001 | ||||
| Non-Han | 857 (8.73%) | 5.51 (4.15) | 5.90 (3.79) | 6.14 (4.22) | |||
| Han | 8962 (91.27%) | 4.84 (3.87) | 5.31 (3.83) | 5.47 (4.06) | |||
| Marital status | <0.001 | 0.1052 | 0.2829 | ||||
| Single/divorced/widowed | 1689 (17.20%) | 5.21 (4.04) | 5.50 (3.91) | 5.62 (4.08) | |||
| Cohabit/married | 8130 (82.80%) | 4.83 (3.87) | 5.33 (3.81) | 5.51 (4.08) | |||
| Socioeconomic factors | |||||||
| Education | <0.001 | <0.001 | <0.001 | ||||
| No formal education | 1904 (19.39%) | 5.89 (4.54) | 6.38 (4.49) | 6.45 (4.63) | |||
| Primary school | 2084 (21.22%) | 5.16 (4.01) | 5.41 (3.85) | 5.82 (4.18) | |||
| Junior secondary school | 3124 (31.82%) | 4.60 (3.65) | 5.20 (3.63) | 5.26 (3.89) | |||
| Senior secondary school | 1575 (16.04%) | 4.38 (3.58) | 4.76 (3.39) | 4.98 (3.69) | |||
| College or above | 1132 (11.53%) | 4.28 (3.22) | 4.84 (3.34) | 4.92 (3.62) | |||
| Equivalized household income | <0.001 | <0.001 | <0.001 | ||||
| Q1 (lowest income group) | 1965 (20.01%) | 5.81 (4.31) | 6.36 (4.22) | 6.38 (4.45) | |||
| Q2 | 1996 (20.33%) | 5.16 (4.01) | 5.65 (3.93) | 5.87 (4.24) | |||
| Q3 | 1937 (19.73%) | 4.80 (3.77) | 5.15 (3.60) | 5.36 (3.97) | |||
| Q4 | 1959 (19.95%) | 4.35 (3.59) | 4.88 (3.55) | 5.02 (3.82) | |||
| Q5 (highest income group) | 1962 (19.98%) | 4.35 (3.57) | 4.76 (3.57) | 4.99 (3.70) | |||
| Employment status | 0.238 | 0.060 | 0.151 | ||||
| Non-employed (unemployed/students/not in labor market) | 2522 (25.68%) | 4.98 (4.16) | 5.24 (3.87) | 5.42 (4.11) | |||
| Employed | 7297 (74.32%) | 4.87 (3.81) | 5.41 (3.82) | 5.56 (4.07) | |||
| Place of residence | |||||||
| Area | <0.001 | <0.001 | <0.001 | ||||
| Urban | 5048 (51.41%) | 4.75 (3.79) | 5.05 (3.65) | 5.22 (3.93) | |||
| Rural | 4771 (48.59%) | 5.06 (4.01) | 5.70 (3.99) | 5.85 (4.21) | |||
| Region | <0.001 | <0.001 | <0.001 | ||||
| Eastern | 3500 (35.65%) | 4.62 (3.70) | 5.03 (3.76) | 5.12 (3.95) | |||
| Middle | 2858 (29.11%) | 4.92 (3.91) | 5.39 (3.77) | 5.60 (4.04) | |||
| Western | 2398 (24.42%) | 5.29 (4.05) | 5.86 (3.80) | 6.02 (4.18) | |||
| Northeastern | 1063 (10.83%) | 4.85 (4.09) | 5.26 (4.15) | 5.57 (4.27) | |||
| Lifestyle factors | |||||||
| Smoking | 0.041 | 0.002 | 0.057 | ||||
| No | 7184 (73.16%) | 4.95 (3.89) | 5.44 (3.82) | 5.57 (4.05) | |||
| Yes | 2635 (26.84%) | 4.76 (3.93) | 5.16 (3.85) | 5.40 (4.15) | |||
| Drinking | <0.001 | <0.001 | <0.001 | ||||
| No | 8287 (84.40%) | 4.96 (3.90) | 5.43 (3.85) | 5.61 (4.11) | |||
| Yes | 1532 (15.60%) | 4.54 (3.86) | 4.97 (3.73) | 5.05 (3.89) | |||
| Exercise per week (times) | <0.001 | <0.001 | <0.001 | ||||
| 0 | 5599 (57.0%) | 5.01 (3.93) | 5.60 (3.90) | 5.73 (4.13) | |||
| 1-2 | 907 (9.2%) | 5.10 (3.71) | 5.70 (3.69) | 5.59 (3.89) | |||
| 3-5 | 1031 (10.50%) | 4.64 (3.56) | 4.93 (3.56) | 5.13 (3.85) | |||
| ≥6 | 2282 (23.24%) | 4.66 (4.04) | 4.85 (3.77) | 5.17 (4.09) | |||
| Physical discomfort | <0.001 | <0.001 | <0.001 | ||||
| No | 7123 (72.54%) | 4.20 (3.43) | 4.91 (3.59) | 5.10 (3.83) | |||
| Yes | 2696 (27.46%) | 6.75 (4.44) | 6.57 (4.18) | 6.66 (4.48) | |||
| Cognitive social capital | |||||||
| Generalized trust | <0.001 | <0.001 | <0.001 | ||||
| Low | 4236 (43.14%) | 5.59 (4.15) | 5.88 (4.05) | 6.08 (4.24) | |||
| High | 5583 (56.86%) | 4.37 (3.62) | 4.97 (3.61) | 5.11 (3.90) | |||
| Trust in neighbors (0–10) b | 6.66 (2.15) | – | – | <0.001 | <0.001 | ||
| Low (0–5) | 3498 (35.62%) | 5.64 (4.21) | <0.001 | 5.90 (4.05) | 6.13 (4.29) | ||
| High (6–10) | 6321 (64.38%) | 4.48 (3.65) | 5.07 (3.67) | 5.19 (3.92) | |||
| Trust in local government officials (0–10) b | 4.98 (2.64) | – | <0.001 | – | <0.001 | <0.001 | |
| Low (0–5) | 6266 (63.82%) | 5.24 (3.98) | 5.59 (3.87) | 5.77 (4.09) | |||
| High (6–10) | 3553 (36.18%) | 4.29 (3.67) | 4.97 (3.72) | 5.09 (4.02) | |||
| Reciprocity | <0.001 | <0.001 | <0.001 | ||||
| Low | 2695 (27.45%) | 5.85 (4.23) | 6.01 (4.04) | 6.23 (4.29) | |||
| High | 7124 (72.55%) | 4.54 (3.70) | 5.12 (3.72) | 5.26 (3.97) | |||
Two-sample t-tests or ANOVA.
We divided trust scores into two groups to compare CES-D-8 score between groups in descriptive statistics. We still used the original trust score in regression analysis.
3.2. Moderating effect of the COVID-19 context and province-level COVID-19 situation
Using data from 2016 to 2020, we examined the moderating effect of the COVID-19 context on the longitudinal association between cognitive social capital and depression (Table 2 , full results in Supplementary Table S3). Model 1a in Table 2 shows that in the pre-COVID-19 context, after adjusting for depression and covariates in 2016, high generalized trust in 2016, compared with low generalized trust in 2016, was associated with a 0.17-unit (95% CI: −0.32, −0.02) decrease in depression score in 2018; every one-unit increase in trust in neighbors in 2016 was associated with a 0.04-unit decrease (95% CI: −0.08, −0.01) in depression score in 2018; and high reciprocity in 2016, compared with low reciprocity in 2016, was associated with a 0.17-unit (95% CI: −0.34, −0.01) decrease in depression score in 2018. However, trust in local government officials in 2016 was not significantly associated with depression in 2018.
Table 2.
Longitudinal association between cognitive social capital and depression in 2018 and 2020, China.
| Depression in 2018 Model 1a: β coefficient (n = 9819) |
Depression in 2020 Model 1b: β coefficient (n = 9819) |
Moderating effect |
||||
|---|---|---|---|---|---|---|
| Model 2a: β coefficient (n = 19,638) |
Model 2b: β coefficient (n = 19,638) |
Model 2c: β coefficient (n = 19,638) |
Model 2d: β coefficient (n = 19,638) |
|||
|
Cognitive social capital (lagged by 2 years) | ||||||
| Generalized trust | ||||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | −0.17* (−0.32,-0.02) |
−0.16* (−0.32,-0.01) |
−0.10 (−0.25,0.04) |
−0.18** (−0.28,-0.07) |
−0.18** (−0.29,-0.07) |
−0.18** (−0.29,-0.07) |
| Trust in neighbors (0–10) |
−0.04* (−0.08,-0.01) |
−0.08*** (−0.12,-0.05) |
−0.06*** (−0.09,-0.04) |
−0.03* (−0.07,-0.00) |
−0.06*** (−0.09,-0.04) |
−0.06*** (−0.09,-0.04) |
| Trust in local government officials (0–10) |
−0.02 (−0.04,0.01) |
−0.04** (−0.07,-0.01) |
−0.03** (−0.05,-0.01) |
−0.03** (−0.05,-0.01) |
−0.01 (−0.03,0.02) |
−0.03** (−0.05,-0.01) |
| Reciprocity | ||||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | −0.17* (−0.34,-0.01) |
−0.29*** (−0.46,-0.12) |
−0.23*** (−0.34,-0.11) |
−0.23*** (−0.34,-0.11) |
−0.23*** (−0.34,-0.11) |
−0.09 (−0.25,0.07) |
| Year | ||||||
| 2018 | – | – | Ref. | Ref. | Ref. | Ref. |
| 2020 | – | – | 0.06 (−0.09,0.20) |
0.35* (0.03,0.67) |
0.19 (−0.01,0.39) |
0.16 (−0.01,0.34) |
|
Cognitive social capital (lagged by 2 years) × year (ref.: 2018) | ||||||
| Generalized trust (High) × 2020 |
– | – | −0.15 (−0.34,0.04) |
– | – | – |
| Trust in neighbors × 2020 | – | – | – | −0.06* (−0.10,-0.01) |
– | – |
| Trust in local government officials × 2020 | – | – | – | – | −0.04* (−0.08,-0.01) |
– |
| Reciprocity (High) × 2020 |
– | – | – | – | – | −0.27* (−0.48,-0.06) |
*p < 0.05, **p < 0.01, ***p < 0.001; “Ref.” indicates the reference group.
In all models, we adjusted for the following variables in 2016 for depression in 2018 and the same variables in 2018 for depression in 2020: sociodemographic factors, socioeconomic factors, lifestyle factors, place of residence, physical comfort, and CES-D-8 Score. Full results are shown in Supplementary Table S3.
Model 1b in Table 2 shows the association between cognitive social capital in 2018 and depression in 2020. Specifically, after adjusting for depression and covariates in 2018, high generalized trust in 2018, compared with low generalized trust in 2018, was associated with a 0.16-unit (95% CI: −0.32, −0.01) decrease in depression score in 2020; every one-unit increase in trust in neighbors in 2018 was associated with a 0.08-unit decrease (95% CI: −0.12, −0.05) in depression score in 2020; every one-unit increase in trust in local government officials in 2018 was associated with a 0.04-unit decrease (95% CI: −0.07, −0.01) in depression score in 2020; and high reciprocity in 2018, compared with low reciprocity in 2018, was associated with a 0.29-unit (95% CI: −0.46, −0.12) decrease in depression score in 2020.
Moreover, the longitudinal associations of trust in neighbors, trust in local government officials, and reciprocity in 2018 with decreased depression in 2020 (i.e., the peri-COVID-19 context) were stronger than the longitudinal associations of the same three variables in 2016 with decreased depression in 2018 (i.e., the pre-COVID-19 context). Specifically, the interaction term in Model 2b shows that after adjusting for 2-year lagged depression and 2-year lagged covariates, in 2020, compared with 2018, every one-unit increase in trust in neighbors (lagged by 2 years) was associated with an additional 0.06-unit (95% CI: −0.10, −0.01) decrease in depression score. Also, the interaction term in Model 2c shows that after adjusting for 2-year lagged depression and 2-year lagged covariates, in 2020, compared with 2018, every one-unit increase in trust in local government officials (lagged by 2 years) was associated with an additional 0.04-unit (95% CI: −0.08, −0.01) decrease in depression score. Additionally, the interaction term in Model 2d shows that after adjusting for 2-year lagged depression and 2-year lagged covariates, in 2020, compared with 2018, high (ref.: low) reciprocity (lagged by 2 years) was associated with an additional 0.27-unit (95% CI: −0.48, −0.06) decrease in depression score. However, the interaction effect between generalized trust and year was not significant (Model 2a).
Furthermore, using data from 2018 to 2020, we examined the moderating effect of province-level COVID-19 situation on the longitudinal association between cognitive social capital and depression within the COVID-19 context. We reported the results in Table 3 (full results in Supplementary Table S4.1 – S4.3). In Section A in Table 3, we reported the results based on the factor score of province-level COVID-19 cases and deaths. In Section B and Section C in Table 3, we reported the results based on the number of province-level COVID-19 cases and deaths, respectively. In Section A, the interaction between trust in local government officials in 2018 and province-level COVID-19 situation in 2020 (Model 3d) indicated that trust in local government officials in 2018 was more strongly associated with decreased depression in 2020 in provinces with worse COVID-19 situation, compared with provinces where the COVID-19 situation was less poor. Specifically, after adjusting for depression and covariates in 2018, with a one-unit increase in the factor score of province-level COVID-19 situation, every one-unit increase in trust in local government officials in 2018 was associated with an additional 0.05-unit (95% CI: −0.09, −0.02) decrease in depression score in 2020. We also found the same pattern when using the number of province-level COVID-19 cases (Model 4d in Section B) and deaths (Model 5d in Section C), respectively.
Table 3.
Longitudinal association between cognitive social capital in 2018 and depression in 2020, China (n = 9819).
| Main effect |
Moderating effect |
||||
|---|---|---|---|---|---|
|
β coefficient (95% CI) |
β coefficient (95% CI) |
β coefficient (95% CI) |
β coefficient (95% CI) |
β coefficient (95% CI) |
|
| Section A: Moderating effect of province-level COVID-19 Situation (factor score) |
Model 3a | Model 3b | Model 3c | Model 3d | Model 3e |
|
Cognitive social capital (in 2018) | |||||
| Generalized trust | |||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | −0.16* (−0.32,-0.01) |
−0.17* (−0.33,-0.01) |
−0.16* (−0.32,-0.01) |
−0.16* (−0.32,-0.00) |
−0.16* (−0.32,-0.01) |
| Trust in neighbors (0–10) |
−0.08*** (−0.12,-0.05) |
−0.08*** (−0.12,-0.05) |
−0.08*** (−0.12,-0.04) |
−0.08*** (−0.12,-0.05) |
−0.08*** (−0.12,-0.05) |
| Trust in local government officials (0–10) |
−0.04** (−0.07,-0.01) |
−0.04** (−0.07,-0.01) |
−0.04** (−0.07,-0.01) |
−0.03 (−0.06,0.00) |
−0.04** (−0.07,-0.01) |
| Reciprocity | |||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | −0.29*** (−0.46,-0.12) |
−0.29*** (−0.46,-0.12) |
−0.29*** (−0.46,-0.12) |
−0.29*** (−0.46,-0.12) |
−0.29** (−0.46,-0.11) |
|
Province-level COVID-19 Situation in 2020 (factor score) |
0.06 (−0.11,0.22) |
0.04 (−0.15,0.23) |
0.20 (−0.14,0.53) |
0.32* (0.07,0.58) |
0.07 (−0.15,0.28) |
| Cognitive social capital in 2018 × Province-level COVID-19 Situation in 2020 | |||||
| Generalized trust (High) × Province-level COVID-19 Situation in 2020 |
– | 0.03 (−0.15,0.21) |
– | – | – |
| Trust in neighbors × Province-level COVID-19 Situation in 2020 | – | – | −0.02 (−0.07,0.02) |
– | – |
| Trust in local government officials × Province-level COVID-19 Situation in 2020 | – | – | – | −0.05** (−0.09,-0.02) |
– |
| Reciprocity (High) × Province-level COVID-19 Situation in 2020 |
– | – | – | – | −0.01 (−0.21,0.18) |
|
Section B: Moderating effect of the number of province-level COVID-19 cases |
Model 4a |
Model 4b |
Model 4c |
Model 4d |
Model 4e |
|---|---|---|---|---|---|
|
Cognitive social capital (in 2018) | |||||
| Generalized trust | |||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | −0.16* (−0.32,-0.01) |
−0.20 (−1.01,0.62) |
−0.16* (−0.32,-0.01) |
−0.16* (−0.32,-0.00) |
−0.16* (−0.32,-0.01) |
| Trust in neighbors (0–10) |
−0.08*** (−0.12,-0.05) |
−0.08*** (−0.12,-0.05) |
−0.01 (−0.21,0.19) |
−0.08*** (−0.12,-0.05) |
−0.08*** (−0.12,-0.05) |
| Trust in local government officials (0–10) |
−0.04** (−0.07,-0.01) |
−0.04** (−0.07,-0.01) |
−0.04** (−0.07,-0.01) |
0.18* (0.02,0.34) |
−0.04** (−0.07,-0.01) |
| Reciprocity | |||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | −0.29*** (−0.46,-0.12) |
−0.29*** (−0.46,-0.12) |
−0.29*** (−0.46,-0.12) |
−0.29*** (−0.46,-0.12) |
−0.30 (−1.19,0.59) |
|
The number of province-level COVID-19 cases in 2020 (on a logarithmic scale) |
0.03 (−0.09,0.16) |
0.03 (−0.11,0.18) |
0.11 (−0.13,0.36) |
0.22* (0.04,0.40) |
0.03 (−0.12,0.19) |
|
Cognitive social capital in 2018 × The number of province-level COVID-19 cases in 2020 (on a logarithmic scale) | |||||
| Generalized trust (High) × The number of province-level COVID-19 cases in 2020 |
– | 0.01 (−0.12,0.13) |
– | – | – |
| Trust in neighbors × The number of province-level COVID-19 cases in 2020 | – | – | −0.01 (−0.04,0.02) |
– | – |
| Trust in local government officials × The number of province-level COVID-19 cases in 2020 | – | – | – | −0.04** (−0.06,-0.01) |
– |
| Reciprocity (High) × The number of province-level COVID-19 cases in 2020 |
– | – | – | – | 0.00 (−0.14,0.14) |
|
Section C: Moderating effect of the number of province-level COVID-19 deaths |
Model 5a |
Model 5b |
Model 5c |
Model 5d |
Model 5e |
|---|---|---|---|---|---|
|
Cognitive social capital (in 2018) | |||||
| Generalized trust | |||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | −0.16* (−0.32,-0.01) |
−0.21 (−0.45,0.03) |
−0.16* (−0.32,-0.01) |
−0.16* (−0.32,-0.00) |
−0.16* (−0.32,-0.01) |
| Trust in neighbors (0–10) |
−0.08*** (−0.12,-0.05) |
−0.08*** (−0.12,-0.05) |
−0.06* (−0.12,-0.00) |
−0.08*** (−0.12,-0.05) |
−0.08*** (−0.12,-0.05) |
| Trust in local government officials (0–10) |
−0.04** (−0.07,-0.01) |
−0.04** (−0.07,-0.01) |
−0.04** (−0.07,-0.01) |
0.01 (−0.04,0.05) |
−0.04** (−0.07,-0.01) |
| Reciprocity | |||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | −0.29*** (−0.46,-0.12) |
−0.29*** (−0.46,-0.12) |
−0.29*** (−0.46,-0.12) |
−0.29*** (−0.46,-0.12) |
−0.27* (−0.52,-0.01) |
|
The number of province-level COVID-19 deaths in 2020 (on a logarithmic scale) |
0.03 (−0.06,0.13) |
0.02 (−0.09,0.13) |
0.12 (−0.07,0.32) |
0.18* (0.03,0.32) |
0.04 (−0.08,0.16) |
|
Cognitive social capital in 2018 × The number of province-level COVID-19 deaths in 2020 (on a logarithmic scale) | |||||
| Generalized trust (High) × The number of province-level COVID-19 deaths in 2020 |
– | 0.03 (−0.08,0.13) |
– | – | – |
| Trust in neighbors × The number of province-level COVID-19 deaths in 2020 | – | – | −0.01 (−0.04,0.01) |
– | – |
| Trust in local government officials × The number of province-level COVID-19 deaths in 2020 | – | – | – | −0.03* (−0.05,-0.01) |
– |
| Reciprocity (High) × The number of province-level COVID-19 deaths in 2020 |
– | – | – | – | −0.01 (−0.12,0.10) |
*p < 0.05, **p < 0.01, ***p < 0.001; “Ref.” indicates the reference group.
In all models, we adjusted for sociodemographic factors, socioeconomic factors, lifestyle factors, place of residence, physical comfort, CES-D-8 Score in 2018, and province-level population density in 2019. Full results are shown in Supplementary Table S4.1-S4.3.
However, the longitudinal associations between cognitive social capital indicators in 2016 and decreased depression in 2020 was not significantly moderated by province-level COVID-19 situation (Supplementary Table S5).
3.3. Sensitivity analysis
In the above analysis, we found that the associations between the various cognitive social capital variables in 2018 and depression in 2020 were stronger than the associations between these variables in 2016 and depression in 2018 (i.e., interaction terms in Table 2). However, this above change could be due to either the COVID-19 pandemic in 2020 or other factors other than COVID-19. In other words, if the longitudinal associations between the cognitive social capital variables and depression had already become stronger over time before 2020, we might consider the change above in Table 2 to be a time trend rather than the results of the outbreak of COVID-19. Hence, we conducted further sensitivity analysis with the data from 2014 to examine whether the longitudinal associations between the cognitive social capital variables and depression also became stronger over time before 2020. Our results (Supplementary Table S6) showed that in the pre-COVID-19 context from 2014 to 2018, the strength of the longitudinal associations between the social capital variables and decreased depression did not change significantly, indicating that the interaction results in Table 2 were more related to COVID-19 than a continuation of previous trends from before COVID-19.
Additionally, we conducted three sensitivity analyses for Table 2, Table 3. First, we excluded participants in Hubei Province since Wuhan, the capital city of Hubei Province, was the epicenter of COVID-19 in China, i.e., Hubei data might be outliers (Supplementary Table S7.1 and S7.2). Second, we removed participants who moved out of their counties/districts during the follow-up, since trust in neighbors and local (county/district) government officials might not be a good indicator of cognitive social capital to predict future depression for those who left (Supplementary Table S8.1 and S8.2). Third, to account for the loss of follow-up and make the analytical sample representative of the study population, we employed inverse probability weighting and poststratification weighting (Supplementary Table S9.1 and S9.2). We calculated inverse probability weights using logistic regression with baseline covariates and depression to account for the loss to follow-up from 2016 to 2020. We further applied poststratification weighting so that each wave of the sample would be representative of the study population. We calculated the poststratification weights using gender, age groups, and areas (rural/urban) according to the 2015 One-percent Population Sample Survey of China (National Bureau of Statistic of China, 2016).
In Supplementary Table S8.1, the p-value of the interaction term between trust in neighbors and year increased to 0.057 (i.e., still <0.1) after removing participants who moved out of their counties/districts during the follow-up. Other results from the sensitivity analyses (Supplementary Table S7.1, Table S7.2, Table S8.2, Table S9.1, and Table S9.2) are consistent with the results in Table 2, Table 3, with p < 0.05 being considered statistically significant.
4. Discussion
To our knowledge, this is the first prospective cohort study in China examining the moderating effect of the COVID-19 context and province-level COVID-19 situation on the longitudinal association between social capital and depression. To summarize, no acceleration of the upward trend of depression was observed in China. However, we found that the longitudinal associations of pre-COVID-19 trust in neighbors, trust in local government officials, and reciprocity with decreased peri-COVID-19 depression in the peri-COVID-19 period were stronger than their associations in the pre-COVID-19 period. Additionally, pre-COVID-19 trust in local government officials was more strongly associated with decreased peri-COVID-19 depression in provinces with a worse COVID-19 situation.
We expanded on previous studies in two aspects. First, pre-disaster social capital was considered a “shock absorber” (Kawachi et al., 2020) that could immunize people against developing severe PTSD symptoms after an earthquake (Hikichi et al., 2016). However, to claim that social capital is a “shock absorber,” a comparison of the health effect of social capital between a scenario with a “shock” and a scenario without a “shock” is needed. In other words, only when the health effect of social capital becomes stronger in a scenario with a “shock” than in a scenario without a “shock” can it be argued that social capital “absorbs” the effect of a “shock.” In this sense, we expanded on previous studies by comparing the longitudinal association between social capital and depression in the pre-COVID-19 context with that in the peri-COVID-19 context. Additionally, previous studies found that individual-level disaster damage (e.g., housing damage) could moderate the association between social capital and mental health (Hikichi et al., 2017, 2018). We expanded on these previous studies by examining the moderating effect of group-level severity (i.e., province-level COVID-19 situation) on the longitudinal association.
4.1. COVID-19 and depression
COVID-19 increased the prevalence of depression symptoms in the US by three times (Ettman et al., 2020) and accelerated the upward trend in mental distress in the UK (Pierce et al., 2020); however, we did not find a similar trend in China in the early stage of the pandemic in 2020. This might be due to the survey time. The 2020 data we used was collected from July to December 2020, after the end of the first COVID-19 outbreak in China, and a study in Hubei, China found that people reported the highest level of psychological distress at the peak of the first outbreak and became less psychologically distressed as the outbreak waned (Jin et al., 2022). The general relief felt after the end of the first outbreak might lead to a lower level of depression than during the peak of the outbreak. Nevertheless, as COVID-19 was far away from being over, studies monitoring mental health during the pandemic are still needed.
4.2. The moderating effect of the COVID-19 context and province-level pandemic situation
The stronger longitudinal association between trust in neighbors and depression in the peri-COVID-19 context than in the pre-COVID-19 context could be because greater trust in neighbors was associated with higher level of perceived social cohesion in a neighborhood (Han and Chung, 2022; Hikichi et al., 2017), which could help reduce anxiety and chronic stress (Abbott and Freeth, 2008). Compared with the pre-COVID-19 period, people might feel more stressed and anxious during the pandemic. Hence, a trustworthy and cohesive neighborhood, where people spend a considerable portion of their time (Duncan and Kawachi, 2018), could be more important for mental health.
Also, there might be several possible explanations for the stronger longitudinal association between trust in local government officials and depression in the peri-COVID-19 context than in the pre-COVID-19 context and in places with worse province-level COVID-19 situation. First, trust in government officials might indicate to what extent people trust the official information. When facing a new infectious disease like COVID-19, there were much more unknowns than knowns, making people anxious and stressed. Hence, obtaining COVID-19-related knowledge and information was important for mental health (Galić et al., 2020). Since the government was the main information source of COVID-19, people had to rely more and mainly on the government to obtain health-related information. Therefore, trust in government officials could become more important in protecting against depression during COVID-19, especially in provinces with worse COVID-19 situation.
Additionally, trust in local government officials might indicate how confident people were in the government's ability to cope with emergencies. During the COVID-19 pandemic, the local government was responsible for implementing pandemic control policies. Hence, compared with the pre-COVID-19 period, people might rely more on the local government officials for disease prevention and health protection. Also, the more severe the pandemic was, the more people might have to rely on the local government officials for their health. In this situation, the confidence in the local government's ability and reliability might be more important to help lower stress and anxiety. Therefore, it makes sense that trust in local government officials was found to be more strongly associated with decreased depression in the peri-COVID-19 context, especially in provinces with worse COVID-19 situation.
Furthermore, reciprocity was shown to be more important in prospectively reducing depression in the peri-COVID-19 than in the pre-COVID-19 context. The perception of reciprocity might reflect a reciprocal social environment which could lessen people's worry about the unavailability of help (Aldrich, 2012) and improve sense of control over life (Han et al., 2023), thereby reducing depression. Moreover, as compared with the pre-COVID-19 period, people might have a higher demand for help during the pandemic, making the worry about lack of help in the pandemic more harmful to mental health. Hence, a reciprocal social environment could be more important to protect against depression during the pandemic.
Moreover, the longitudinal associations of trust in neighbors, trust in local government officials, and reciprocity with depression were moderated by the COVID-19 context; however, within the COVID-19 context in 2020, only the longitudinal association of trust in local government officials with peri-COVID-19 depression was moderated by province-level COVID-19 situation. The above-mentioned results might suggest that it was the general social atmosphere and context induced by the pandemic rather than the specific pandemic severity people experienced during the outbreak that mattered more for the strength of the longitudinal association between pre-COVID-19 cognitive social capital and peri-COVID-19 depression (measured after the first outbreak of COVID-19). In other words, a wave of the COVID-19 outbreak finished; however, the pandemic was far from being over. In this case, the COVID-19 pandemic atmosphere haunting people made cognitive social capital important in protecting against depression.
Additionally, the moderating effect of the COVID-19 context and province-level COVID-19 situation was also related to the stress-buffering model (Cohen and Wills, 1985) and the stress process model (Pearlin et al., 1981). According to the stress-buffering model (Cohen and Wills, 1985), social support was considered a moderator, whereas stress was exposure, and social support could buffer the negative effect of stress on health. However, we did not find that the COVID-19 context or province-level COVID-19 situation was associated with depression. In contrast, we found that the COVID-19 context and province-level COVID-19 situation moderated the association between cognitive social capital and depression. Hence, in our study, cognitive social capital served as exposure, whereas the COVID-19 context and province-level COVID-19 situation were moderators, which were different from the classic stress-buffering model (Cohen and Wills, 1985).
The above-mentioned difference from the classic stress-buffering model (Cohen and Wills, 1985) may indicate that even if an event (e.g., COVID-19) does not threaten health directly, the health effect of social capital could also become stronger when facing this event (e.g., COVID-19), which might be understood from the perspective of the stress process model (Pearlin et al., 1981). As indicated in the stress process model (Pearlin et al., 1981), stressful events may not affect depression directly but could affect depression indirectly through multiple serial mediators. Additionally, social support could buffer the effect of the above mediators on depression, thereby becoming more crucial for depression when facing stressful events. In our case, COVID-19 could be a “distant” factor for depression and could trigger some unmeasured “proximate” factors which were significantly associated with depression. In this sense, the interaction effect between cognitive social capital and the COVID-19 context/province-level COVID-19 situation might result from the buffering effect of cognitive social capital on the association between some unmeasured “proximate” factors and depression, which deserves further empirical testing.
4.3. Public health implication
In China, treatment rates for depression were very low, and few people received adequate treatment (Lu et al., 2021), making prevention play a critical role in coping with depression. Cognitive social capital could be a crucial tool for preventing depression, especially during the COVID-19 pandemic. As the pandemic is ongoing, cognitive social capital that was present before each outbreak is thus important to protect against depression. In other words, destruction of cognitive social capital could threaten mental health, especially in places with worse province-level COVID-19 situations. Therefore, policymakers should avoid damaging cognitive social capital when implementing pandemic control measures, especially when province-level COVID-19 situation escalates. For example, suppose stringent pandemic control measures implemented by the local government could not effectively control the pandemic. In that case, people may lose their trust in the local government officials, which might further threaten people's mental health, even if the initial purpose of the stringent control measures was good.
4.4. Limitations
We did not examine whether individual-level COVID-19 experiences moderated the longitudinal association between cognitive social capital and depression as we had no information on infection, isolation, and quarantine. Also, we only examined the moderating effect of province-level COVID-19 situation, which might have less variation than city-level COVID-19 situation. This might impede our observation of the contextual effect of COVID-19 situation on depression. However, we had no information about the participants’ city names. Hence, we could only leave this research gap for future studies. Moreover, cognitive social capital was subjective and perceptual; hence, it might be endogenous to participants’ depression. Additionally, unmeasured variables may affect cognitive social capital and depression, resulting in omitted variable bias. In other words, even if the exposures were measured before the outcome, the results could not be interpreted as causal due to the omitted variable bias.
5. Conclusion
Cognitive social capital is critical to mental health resilience in a pandemic; therefore, it should be taken into account for pandemic preparedness and response. Since the COVID-19 pandemic is still ongoing, cognitive social capital could be critical to protecting mental health. Policymakers should avoid damaging cognitive social capital, especially trust in local government officials, when implementing control measures. Moreover, even if we can go back to “normal,” building and maintaining cognitive social capital will still be essential for mental health protection, especially considering that another pandemic will come in the future, and it is only a matter of when.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgment
We would like to acknowledge the China Family Panel Studies project team at Peking University for collecting and releasing the data. We would also like to thank Dr. Xi Chen at the Department of Sociology and Social Policy, Lingnan University for questions, suggestions, and comments on an early version of this study. YH would also like to thank Dr. Shi Zhao at JC School of Public Health and Primary Care, The Chinese University of Hong Kong for suggestions and comments on statistical analysis, and thank Jingwen Liu at the Department of Sociology, University of Maryland for suggestions and comments on the initial research idea of this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.healthplace.2023.103022.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Abbott S., Freeth D. Social capital and health: starting to make sense of the role of generalized trust and reciprocity. J. Health Psychol. 2008;13:874–883. doi: 10.1177/1359105308095060. [DOI] [PubMed] [Google Scholar]
- Aldrich D.P. University of Chicago Press; 2012. Building Resilience: Social Capital in Post-Disaster Recovery. [Google Scholar]
- Beaudoin C.E. News, social capital and health in the context of Katrina. J. Health Care Poor Underserved. 2007;18:418–430. doi: 10.1353/hpu.2007.0024. [DOI] [PubMed] [Google Scholar]
- Chan S.-M., Chung G.K.-K., Chan Y.-H., Woo J., Yeoh E.K., Chung R.Y.-N., Wong S.Y.-S., Marmot M., Lee R.W.-T., Wong H. The mediating role of individual-level social capital among worries, mental health and subjective well-being among adults in Hong Kong during the COVID-19 pandemic. Curr. Psychol. 2021 doi: 10.1007/s12144-021-02316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Zou Y., Gao H. Role of neighborhood social support in stress coping and psychological wellbeing during the COVID-19 pandemic: evidence from Hubei, China. Health Place. 2021;69 doi: 10.1016/j.healthplace.2021.102532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985;98:310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- Coleman J.S. Social capital in the creation of human capital. Am. J. Sociol. 1988;94:S95–S120. doi: 10.1086/228943. [DOI] [Google Scholar]
- COVID-19 Mental Disorders Collaborators Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021:1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan D.T., Kawachi I. Oxford University Press; 2018. Neighborhoods and Health. [Google Scholar]
- Ehsan A.M., De Silva M.J. Social capital and common mental disorder: a systematic review. J. Epidemiol. Community. 2015;69:1021–1028. doi: 10.1136/jech-2015-205868. [DOI] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galić M., Mustapić L., Šimunić A., Sić L., Cipolletta S. COVID-19 related knowledge and mental health: case of Croatia. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.567368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han Y., Chen X., Chung R.Y.-N. Sense of control as a mediator of the association between social capital and health inequality in China. Prev. Med. 2023;166 doi: 10.1016/j.ypmed.2022.107382. [DOI] [PubMed] [Google Scholar]
- Han Y., Chung R.Y.-N. The role of neighborhood social capital on health and health inequality in rural and urban China. Prev. Med. 2022 doi: 10.1016/j.ypmed.2022.106989. [DOI] [PubMed] [Google Scholar]
- Hikichi H., Aida J., Matsuyama Y., Tsuboya T., Kondo K., Kawachi I. Community-level social capital and cognitive decline after a natural disaster: a natural experiment from the 2011 Great East Japan Earthquake and Tsunami. Soc. Sci. Med. 2018 doi: 10.1016/j.socscimed.2018.09.057. [DOI] [PubMed] [Google Scholar]
- Hikichi H., Aida J., Tsuboya T., Kondo K., Kawachi I. Can community social cohesion prevent posttraumatic stress disorder in the aftermath of a disaster? A natural experiment from the 2011 tohoku earthquake and tsunami. Am. J. Epidemiol. 2016;183:902–910. doi: 10.1093/aje/kwv335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hikichi H., Tsuboya T., Aida J., Matsuyama Y., Kondo K., Subramanian S.V., Kawachi I. Social capital and cognitive decline in the aftermath of a natural disaster: a natural experiment from the 2011 Great East Japan Earthquake and Tsunami. Lancet Planet. Health. 2017;1:e105. doi: 10.1016/S2542-5196(17)30041-4. e113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer D.W., Lemeshow S. first ed. John Wiley & Sons, Ltd; 2000. Applied Logistic Regression. [DOI] [Google Scholar]
- Jin L., Chen X., Lin F., Zou Y., Gao H. Does education matter for psychological recovery amidst the COVID-19 pandemic? Evidence from a panel survey in Hubei, China. Anxiety, Stress. COPING. 2022;35:101–110. doi: 10.1080/10615806.2021.1978431. [DOI] [PubMed] [Google Scholar]
- Kawachi I., Aida J., Hikichi H., Kondo K. Disaster resilience in aging populations: lessons from the 2011 Great East Japan earthquake and tsunami. J. Roy. Soc. N. Z. 2020;0:1–16. doi: 10.1080/03036758.2020.1722186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Subramanian S.V., Kim D., editors. Social Capital and Health. Springer; New York ; London: 2008. [Google Scholar]
- Lin N. Building a network theory of social capital. Connections. 1999:28–51. [Google Scholar]
- Lu J., Xu Xiufeng, Huang Y., Li T., Ma C., Xu G., Yin H., Xu Xiangdong, Ma Y., Wang L., Huang Z., Yan Y., Wang B., Xiao S., Zhou L., Li L., Zhang Y., Chen H., Zhang T., Yan J., Ding H., Yu Y., Kou C., Shen Zonglin, Jiang Linling, Wang Z., Sun X., Xu Y., He Y., Guo W., Jiang Lijun, Li S., Pan W., Wu Y., Li G., Jia F., Shi J., Shen Zhongxia, Zhang N. Prevalence of depressive disorders and treatment in China: a cross-sectional epidemiological study. Lancet Psychiatr. 2021;8:981–990. doi: 10.1016/S2215-0366(21)00251-0. [DOI] [PubMed] [Google Scholar]
- Lund C., Brooke-Sumner C., Baingana F., Baron E.C., Breuer E., Chandra P., Haushofer J., Herrman H., Jordans M., Kieling C., Medina-Mora M.E., Morgan E., Omigbodun O., Tol W., Patel V., Saxena S. Social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews. Lancet Psychiatr. 2018;5:357–369. doi: 10.1016/S2215-0366(18)30060-9. [DOI] [PubMed] [Google Scholar]
- Moore S., Kawachi I. Twenty years of social capital and health research: a glossary. J. Epidemiol. Community. 2017;71:513–517. doi: 10.1136/jech-2016-208313. [DOI] [PubMed] [Google Scholar]
- National Bureau of Statistic of China National data-Population density in each province [WWW Document] 2022. https://data.stats.gov.cn/search.htm?s=%E5%90%84%E7%9C%81%E4%BA%BA%E5%8F%A3%E5%AF%86%E5%BA%A6
- National Bureau of Statistic of China . The 2015 One-Percent Population Sample Survey of China. China Statistics Press; Beijing: 2016. [Google Scholar]
- National Bureau of Statistics of China . 2011. Divisions of Eastern, Middle, Western, and Northeastern Regions.http://www.stats.gov.cn/ztjc/zthd/sjtjr/dejtjkfr/tjkp/201106/t20110613_71947.htm (东西中部和东北地区划分方法) [WWW Document]. URL. 12.28.20. [Google Scholar]
- OECD . 2012. Quality Review of the OECD Database on Household Incomes and Poverty and the OECD Earnings Database Part I. [Google Scholar]
- Pearlin L.I., Menaghan E.G., Lieberman M.A., Mullan J.T. The stress process. J. Health Soc. Behav. 1981;22:337–356. doi: 10.2307/2136676. [DOI] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K.M. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatr. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam R.D. Simon and Schuster; New York, NY: 2000. Bowling Alone: the Collapse and Revival of American Community. [Google Scholar]
- Radloff L.S. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Sato K., Kondo N., Kondo K. Pre-pandemic individual- and community-level social capital and depressive symptoms during COVID-19: a longitudinal study of Japanese older adults in 2019-21. Health Place. 2022;74 doi: 10.1016/j.healthplace.2022.102772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- State Council Fighting covid-19 China in action [WWW document] 2020. http://www.gov.cn/zhengce/2020-06/07/content_5517737.htm
- Thuy N.T.M., Berry H.L. Social capital and mental health among mothers in Vietnam who have children with disabilities. Glob. Health Action. 2013;6 doi: 10.3402/gha.v6i0.18886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turvey C.L., Wallace R.B., Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int. Psychogeriatr. 1999;11:139–148. doi: 10.1017/S1041610299005694. [DOI] [PubMed] [Google Scholar]
- Villalonga-Olives E., Kawachi I. The measurement of social capital. Gac. Sanit. 2015;29:62–64. doi: 10.1016/j.gaceta.2014.09.006. [DOI] [PubMed] [Google Scholar]
- Wei J., Han Y. Pre-disaster social capital and disaster recovery in wenchuan earthquake-stricken rural communities. Sustainability. 2018;10:2046. doi: 10.3390/su10062046. [DOI] [Google Scholar]
- Xie Y., Lu P. The sampling design of the China family panel studies (CFPS) Chinese Journal of Sociology. 2015;1:471–484. doi: 10.1177/2057150X15614535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y. In: Economic Stress, Human Capital, and Families in Asia: Research and Policy Challenges, Quality of Life in Asia. Yeung W.-J.J., Yap M.T., editors. Springer Netherlands; Dordrecht: 2013. Social networks and reduction of risk in disasters: an example of the wenchuan earthquake; pp. 171–182. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.