Abstract
Tuberculosis (TB) is a significant public health concern. Globally, TB is among the top 10 and the leading cause of death due to a single infectious agent. Providing standard anti-TB therapy for at least 6 months is recommended as one of the crucial strategies to control the TB epidemic. However, the long duration of TB treatment raised the issue of non-adherence. Non-adherence to TB therapy could negatively affect clinical and public health outcomes. Thus, directly observed therapy (DOT) has been introduced as a standard strategy to improve anti-TB medication adherence. Nonetheless, the DOT approach has been criticized due to inconvenience, stigma, reduced economic productivity, and reduced quality of life, which ultimately could complicate adherence issues. Apart from that, its effectiveness in improving anti-TB adherence is debatable. Therefore, digital technology could be an essential tool to enhance the implementation of DOT. Incorporating the health belief model (HBM) into digital technology can further increase its effectiveness in changing behavior and improving medication adherence. This article aimed to review the latest evidence regarding TB medication non-adherence, its associated factors, DOT’s efficacy and its alternatives, and the use of digital technology and HBM in improving medication adherence. This paper used the narrative review methodology to analyze related articles to address the study objectives. Conventional DOT has several disadvantages in TB management. Integrating HBM in digital technology development is potentially effective in improving medication adherence. Digital technology provides an opportunity to improve medication adherence to overcome various issues related to DOT implementation.
Keywords: Tuberculosis, Adherence, Directly Observed Therapy, Digital Technology, Health Belief Model
Key Figure
Introduction
Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis. TB is considered as a significant public health threat worldwide, and is among the top 10 causes of death and the leading cause of death due to a single infectious agent [1]. Globally, it was estimated that 10.6 million (range, 9.9 to 11.0 million) people fell ill due to TB, causing the deaths of 1.6 million in 2021 [2]. Recent systematic reviews and meta-analyses found that almost one-quarter of the world’s population could be infected by TB [3]. The findings showed a large pool of infected individuals, constituting an enormous source of active TB transmission. TB is treatable using a standard medication regimen for at least 6 months [4]. Standard 6-month treatment with anti-TB medication is highly effective for drug-susceptible TB, whose main aim is to cure the disease and reduce the risk of transmission [5].
The long duration of anti-TB treatment posed significant challenges to TB patients, especially non-adherence to medication. A study in South Africa estimated that treatment loss mainly occurred at treatment completion, with only 53% of overall TB cases completing their treatment [6]. Failure to complete anti-TB medications can lead to an increased risk of relapse, acquired drug-resistant TB, treatment failure, progression of disease leading to complication and death, and ongoing transmission of infection [7,8].
Adherence to TB therapy is critical for the success of TB treatment. According to the World Health Organization (WHO), anti-TB medication adherence is multifaceted and complex, necessitating specific attention through the delivery of person-centered care. One of the key objectives of the sustainable development goals is to end the TB epidemic, which calls for a comprehensive strategy that includes biological, public health, social, and economic intervention [9]. Effective intervention through overcoming the issues of non-adherence to anti-TB medications is critical to ending the TB epidemic. Therefore, tackling non-adherence to TB medications requires a concerted effort from many social determinants of TB disease. The End TB Strategy encompassed a comprehensive intervention package consisting of three pillars. The first pillar placed a focus on integrated, patient-centered care and prevention, which necessitates enhancing and extending the key activities of TB programs, including the use of modern technology to improve patient care [10].
Implementation of directly observed therapy (DOT) posed significant challenges to treatment adherence and outcomes. Although WHO introduced this strategy to ensure treatment adherence, the approach has been associated with substantial inconvenience to patients and healthcare workers [11,12]. Furthermore, a review of various literatures has found no rigorous, supportive evidence of the effectiveness of DOT in improving adherence and treatment outcomes [13]. Hence, applying a patient-centered approach might be a wise reallocation of resources to improve adherence and treatment outcomes. Improved global access to the internet and communication technology provide an excellent opportunity to overcome various challenges in TB management. This article aimed to update evidence available on the definition of non-adherence to anti-TB medications, factors contributing to medication non-adherence, effectiveness of DOT and its alternatives, and the application of the health belief model (HBM) to improve medication adherence.
Methods of Literature Review
The present literature review was conducted using narrative review approach. Our search was done according to preferred reporting items for systematic reviews and meta-analyses guidelines. Two web-based search engines were used in the literature search: PubMed and Google Scholar. Any unpublished manuscripts, letters to the editor, articles with no measurement of the outcome of interest, animal studies, non-English language articles, and conference abstracts were excluded.
The search string used to find articles related to the definition of non-adherence is as follows: “tuberculosis” AND “medication” AND (“non-adherence” OR “default” OR “loss to follow-up”). To identify the articles related to the factors associated with non-adherence to medication, the search string was used as follows: (“default” OR “loss to follow-up” OR “non-adherence”) AND “tuberculosis” AND (“factors” OR “predictors”). The search string as follows was used to capture the articles for DOT’s effectiveness and its alternatives: (“DOT” OR “directly observed therapy” OR “VOT” OR “video observed therapy”) AND (“effectiveness” OR “feasibility” OR “acceptability”). For articles describing the behavioral theory to predict medication adherence, the search strategy used is as follows: (“health belief model” OR “behavioral theory”) AND (“adherence” OR “medication adherence”). Subsequently, all articles identified will be screened by reading the title and abstract only to determine the relevance of the pieces to our review.
Definition of Anti-TB Medication Adherence
The importance of getting specific values in measuring medication adherence influences the conclusion made in evaluating the performance of interventions in clinical trials. Different values in determining medication adherence could lead to misleading decision about intervention performance.
There is no standard definition of TB medication adherence [14,15]. The definition varied and tailored to assess different types of interventions, which can lead to difficulties in generalizing and comparing. Generally, adherence can be defined as completeness to medication in which the patients follow the instructions of medical professionals [16]. According to WHO, adherence is “the extent to which the patient follows medical instructions” [14]. Globally, it was estimated that the average non-adherence to medication for chronic illness in developed countries was 50%. In contrast, the average rate of non-adherence among developing countries is even higher [14]. Therefore, WHO has identified that non-adherence to medication is a significant barrier to controlling chronic diseases, including TB.
Another term that has been commonly used in studies related to treatment adherence is concordance. Concordance refers to harmonious cooperation or agreement between patients, doctors, and healthcare workers regarding treatment plans and action, mainly focused on consultation and negotiation [17]. It is an approach taken by parties related to patient management to ensure the patients are well informed about the diagnosis and treatment, understand their benefits and risks, and assist in their decision to optimize the potential use of medical care. However, it differs from compliance or adherence to medication because it is often referred to as one-way communication. The patient follows instructions from healthcare professionals, as opposed to concordance, which involves two-way communication and agreement between two parties [18]. Various definitions of TB medication adherence according to the different types of studies are summarized in Table 1 [19-28].
Table 1.
Definition of adherence according to different studies
| Method | Type of study | Definition | |
|---|---|---|---|
| Default | Follow-up or medication refill visit | Prospective cohort | Interruption of treatment for more than 2 consecutive months [19] |
| Retrospective cohort | Treatment was interrupted for 2 consecutive months or more [20] | ||
| Loss to follow-up | DOT | Retrospective cohort study | Not start treatment or whose treatment was interrupted for 2 consecutive months or more [21] |
| Non-adherent to medication | Follow-up or medication refill visit | Prospective cohort | Missing at least one dose of drugs or one follow-up appointment during the treatment course [19] |
| Follow-up or medication refill visit | Mixed method cross-sectional | Missed ≥10% of the total planned dose in patients belonged to either the intensive or maintenance phase [22] | |
| Self-reporting number of pills taken | Cross-sectional | Missed ≥10% of the total planned dose [23,24] | |
| Adherence | DOT/VOT | Randomized trial | Completed 80% or more treatment observations scheduled in 2 months following randomization [25] |
| DOT | Retrospective cohort | ≥90% of expected TB medication doses were taken [26] | |
| VOT | Prospective cohort | Completed all doses of medication [27] | |
| DOT | Cross-sectional | Not miss any dose of medication [28] |
DOT: directly observed therapy; VOT: video observed therapy; TB: tuberculosis.
Factors Contributing to Anti-TB Medication Adherence
Adherence to TB medication is essential to TB treatment’s success. Suboptimal medication adherence is widespread in diseases that require long-term therapy, such as diabetes, hypertension, bronchial asthma, and TB [14]. Medication adherence is a complex human behavior that could be influenced by various factors, including patient-related, health system, condition-related, therapy-related, and socioeconomic factors.
1. Patient-related factors
Medication adherence is closely related to intra-individual variability, affecting motivation and willingness to adopt recommended health-related behaviors. The non-modifiable factor has been closely related to non-adherence to medication, including male gender [20], younger age [20,29,30], and marriage status (being divorced and widowed) [28]. On the other hand, modifiable factors include psychological and cognitive factors (forgetfulness, lack of knowledge, perceived barrier, psychological distress, and stigma) [17,28,29,31,32], and behavioral factors (alcohol and cigarette smoking use [23] are associated with non-adherent to TB medications. In addition, social acceptance of traditional medicine and a lack of family support have been recognized as key factors in non-adherence to anti-TB treatment regimens [33]. This condition might be attributed to a lack of awareness and misperception regarding TB, leading to adverse health behavior [34].
2. Health system factor
Positive patient experience in healthcare significantly influences patient satisfaction, affecting adherence to anti-TB medications [14]. A previous study found that a poor patient-provider relationship is significantly associated with non-adherence to anti-TB medicines [24]. This finding is supported by another study, where the concordance behavior of healthcare workers was associated with the attitudes of the patients and medication-taking behavior [17]. A strained patient-provider relationship can lead to a breakdown in communication, leaving the patient unaware of their risky behavior and with the mistaken belief that their actions have no consequences [23]. However, empathic relationships are challenging when healthcare workers are not well trained, have an overburdened health system, and lack supervision, especially in low-resourced and high TB burden settings [14,33].
3. Condition-related factors
The condition of a patient might affect the adherence of an individual to anti-TB medications. On top of numerous medical issues and clinic visits, the requirement to take multiple medications can subsequently affect their motivation to follow their doctor’s instructions [24]. Several studies found that the prevalence of depression among diabetics ranged from 21.6% to 37.6% [35-37]. The possibility of mental disorders can raise the likelihood of being hospitalized, along with underlying comorbidities and TB. History of hospitalization has been identified as one of the factors that could lead to poor adherence to anti-TB medications [32]. Thus, the combination of the risk factors should be considered to plan strategies to address the issues.
Co-infected with human immunodeficiency virus (HIV) are less likely to be non-adherent to anti-TB medications [20]. This finding is significant in light of the worldwide strategy to eradicate TB, which calls for HIV patients to undergo TB screenings and receive proper anti-TB and anti-retroviral treatment (ART) [9]. Another condition that is associated with non-adherence to treatment is TB relapse [20,23].
4. Therapy-related factors
The complexity and potential side effects of TB treatment can also affect medication adherence. Consumption of anti-TB medication can lead to multiple side effects such as gastrointestinal upset (18.4%), psychiatric illness (5.5%), arthralgia (4.7%), acute liver injury (3.9%), peripheral neuropathy (3.1%), thyroid disorder (2.3%), epilepsy (2.0%), skin disorder (2.0%), hearing problem (1.6%), and kidney injury (1.2%) [38]. Anti-TB drug toxicity and its other side effects were found to serve as a barrier for TB patients to continue their medications [29,33]. In addition, TB patients are often affected by regimen complexity. They are more likely to be co-infected with HIV, which further adds to the high tablet burden (to take both anti-TB and ART medication) [31]. Non-adherence to anti-TB medications is strongly associated with being in the maintenance phase of TB treatment [24]. Clinical and well-being improvements during the maintenance phase may have caused non-adherence since patients felt better and were less attentive with their daily medications [39].
5. Socioeconomic factors
TB commonly affects low socioeconomic groups, especially the homeless, unemployed, and poor [31]. Low socioeconomic status can increase the likelihood of the individual and their household being exposed to the TB risk factors, such as malnutrition, crowded home, and hazardous working environment. In addition, those who live in low socioeconomic status are more prone to adopt risky behavior such as alcohol consumption and cigarette smoking. Poor socioeconomic background can also lead to a lack of enabling environment (lack of health care access, poor transportation, and financial support), making people non-adherence to medication [40].
Efecfectiveness and Alternatives of DOT
DOT has been a standard of care in TB control programs since its recommendation by WHO around the 1990s. Although DOT can be provided in an institutional setting (e.g., health clinic, workplace, amongst others) or community (by family members or community volunteers), it can still cause substantial disadvantages to patients and healthcare workers. DOT approach can cause inconvenience in terms of healthcare access, inflexible timing of healthcare facilities for patients coming for DOT, poor attitude by a healthcare worker, stigma, fear, and financial hardship [11]. According to a previous study, TB infection and DOT negatively affect social functioning and mental and emotional quality of life of patients [12].
According to a recent systematic review, it was shown that the effectiveness of DOT is varied compared to self-administered therapy. DOT by family members was not superior in improving treatment outcomes compared to self-administered therapy. Meanwhile, institutional DOT provided for latent TB infection effectively improved treatment success [41]. The finding is consistent with another systematic review (n=11 clinical trials with a total of 5,662 participants), which found that treatment success (sum of TB cure and TB treatment completion) was low and intervention using DOT was not substantially improving treatment success [11].
Innovative strategies have been developed and tested in various clinical trials to find a better method for improving adherence to anti-TB medications. For example, digital technology by video-based directly observed therapy (VDOT/video observed therapy [VOT]) has been clinically tested for its effectiveness and feasibility. Several studies showed that using VOT significantly improved medication adherence compared to the usual DOT. An randomized controlled trial (RCT) study reported that those who belonged to the intervention arm had substantially better compliance than family-based DOT (100% vs. 87.3%, p<0.01) [42]. Another RCT study (n=226) conducted in the United Kingdom found that, after restricted analysis, 77% of patients on VOT achieved 80% adherence to anti-TB medication compared to only 63% on usual DOT [25]. The superiority of VOT compared to conventional DOT in improving anti-TB medication adherence also has been consistently observed by other RCTs in the United States of America (n=174 in VOT and n=159 in-person DOT) [43]. Another innovation, such as a mobile application with a bi-directional communication platform, was also found to have a lower non-adherence rate than the control groups [44]. However, another RCT study (n=405) conducted among TB patients admitted to Shandong Provincial Chest Hospital, China, among bacteriologically confirmed pulmonary tuberculosis, found no significant differences in treatment completion between the VOT and DOT arm [45]. Even though the findings differed, several studies consistently showed that VOT has a better user experience than DOT, especially in reducing observation time, reducing the cost incurred because of observation [45], and improving user preference [46]. Furthermore, the use of VOT has been found to have a better psychosocial impact, including knowledge, depression, stigma, quality of life, and social support among its users compared to DOT [42].
Potential of Digital Technology in Medication Adherence
The global expansion of mobile phones and internet access provides an excellent opportunity to incorporate digital technology into public health practice. According to the Global System for Mobile Communication Association (GSMA) report, half of the world’s population is connected to the internet. Other than that, it was reported that more than half of people in the low-middle-income country have been using mobile phones as the primary means of internet access [47]. Even though there is an assumption of a low level of digital literacy and a perceived lack of relevance, the gap in the usage of mobile phones has decreased from 24% to only 10% worldwide, which is mainly due to increased affordability and internet access [47]. The widespread usage of mobile devices and internet access may offer an alternative method to enhancing the prevention and treatment of TB patients.
The use of digital technology to enhance adherence to TB therapy is crucial and relevant to rethinking TB care delivery. From a public health perspective, improving adherence to anti-TB treatment can help prevent relapse, drug resistance, and TB transmission in the community [48]. Inadequate adherence to anti-TB therapy is one of the key predictors of TB recurrence, according to a significant, nested case-control study conducted in Vietnam [49]. The current strategy of DOT to ensure patient compliance with TB treatment might cause problems, as the patients are required to come to health facilities daily to take the medication. Additionally, frequent visits to health clinics could cause disruption to their work, reduce production time, and increase the risk of job insecurity [50].
Furthermore, the disease mainly affects the age group with high economic productivity [51]. Daily visits to healthcare facilities could also cause inconvenience to patients due to increased travel time, waiting hours, and reduced participation in social activities [50]. In addition, the disease and treatment can significantly impact a patient’s life, such as quality of life as well as their physical, psychological, and emotional well-being [50,52,53].
Therefore, WHO has recommended implementing a patient-centered approach in TB care. The patient-centered care is an approach that emphasizes respectfully providing care and responsiveness to the individual patient’s preferences, values, and needs [9]. The approach is documented as the first pillar in the End TB Strategy by WHO, which puts the patient at the heart of TB service delivery. According to a previous study, delivering TB care in a patient-centered approach has improved the efficiency and timeliness of TB management [54]. WHO has recommended using innovative information and communication technology to enhance a patient-centered approach to TB care [9]. Using a patient-centric approach, especially digital adherence technology, could help reduce TB treatment’s financial and social impact.
The use of digital technology in TB care can provide an essential tool to improve TB management. When DOT was introduced and implemented as one of the critical strategies to improve adherence to TB therapy in the early 1990s, little consideration was given to the needs of patients, especially who are economically productive. According to a recent systematic review, it was shown that DOT’s effectiveness is varied compared to self-administered therapy. For example, DOT by family members was not superior in improving treatment adherence compared to self-administered therapy. However, institutional DOT provided for latent TB infection effectively improved treatment completion [41]. The finding is consistent with another systematic review, which found that treatment adherence was low and intervention using DOT was not substantially improving treatment adherence [11].
Using digital technology to increase TB therapy adherence could help reduce patient inconvenience due to travel to health facilities, the risk of hospital-acquired infection among visitors, and the burden of supervision on healthcare workers. Technology solutions have been identified as one of the strategies to increase the relevance of DOT, particularly in this age of the 4.0 Industrial Revolution. With the increased use of mobile technology and widespread internet coverage, technology is becoming a viable solution for increasing the importance of DOT.
Digital adherence technology has several advantages over conventional DOT strategy in TB care. Previous studies found that VOT is superior in feasibility, preferability, confidentiality, and time to travel [27,55,56]. A superior, analyst-blinded randomized clinical trial also found that using VOT has significantly higher TB medication adherence than conventional DOT [25]. In addition, VOT is also a better option as it was proven to reduce observation time [45], reduce the cost incurred because of observation [45], user preference [46], and better psychosocial impact [42]. However, most of the study has limited robust methodology, such as no control group to make a comparison [56], non-probability sampling [27], and small sample size [55]. A previous systematic review also concluded that currently, there is a limited number of evidence on the use of digital technology to improve treatment outcomes [57]. Given the promising potential of technology to improve medication adherence, VOT should be considered, especially in a setting with high TB patients among the productive age group, increased mobility, high smartphone usage, and comprehensive internet coverage [10].
Health Belief Model to Improve Adherence
Medication adherence can pose a significant challenge when providing treatment that requires longterm therapy, especially for TB. Human behavior is related to compliance, which reflects a person’s capacity to adhere to prescription medicine guidelines from medical professionals [16]. Thus, it is critical to consider the patient’s psychology as an essential determinant of medication adherence [58]. One of the most used behavioral theories to improve medication adherence was HBM [59].
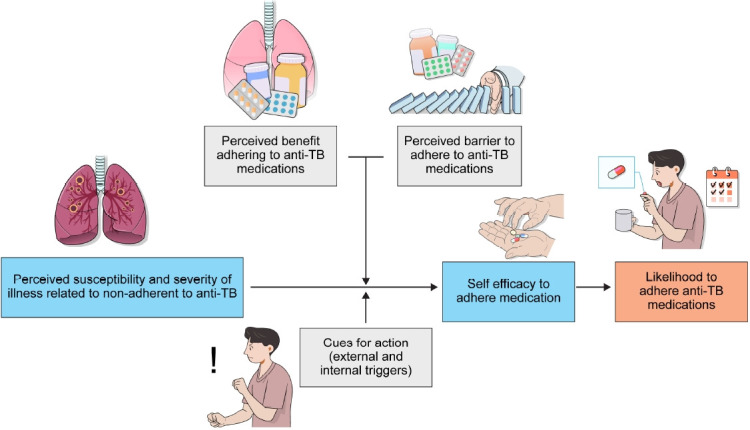
HBM highlights the importance of human behavior and explains the failure of individuals to adopt the recommended preventive measures or screening tests for early disease diagnosis. The HBM states that an individual’s perception of susceptibility to a particular illness and their perception regarding the seriousness of the disease, and the person’s belief in the effectiveness of recommended health-related behavior can predict the likelihood of the individual adopting the behavior. The HBM consists of six constructs, as shown in Figure 1.
Fig. 1.
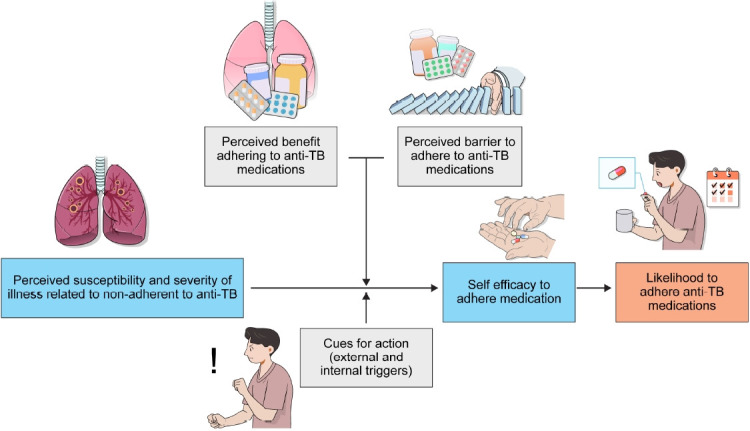
Health belief model (HBM) for medication adherence. Boxes within dotted lines show constructs of HBM. TB: tuberculosis.
HBM has been applied in various studies to improve adherence to long-term therapy for various chronic diseases, such as HIV [60], hypertension [61,62], post-kidney transplantation [63], cystic fibrosis [64], and type 2 diabetes mellitus65. Even though there is evidence that HBM is an essential predictor of medication adherence, there is a lack of available randomized clinical trials that evaluate the effectiveness of HBM in predicting anti-TB medication adherence [25,34].
Long-term ART for HIV patients has been recommended to all HIV patients regardless of their immune status. Adherence to ART is central to achieving viral suppression and prolonging life expectancy. HBM has been used as one of the models to develop strategies to improve compliance with ART. Patients’ beliefs on their susceptibility and severity to consequences of non-adherent to ART and their perception of certain obstacles are correlated with the likelihood of HIV patients adhering to the medication [60].
In hypertensive patients, their belief in perceived susceptibility, cues for action, and low perceived barriers were significantly associated with good anti-hypertensive medication adherence [62]. A previous RCT found that a comprehensive reminder system intervention incorporating HBM is effective in improving medication adherence and blood pressure control and prevents disability among stroke patients [61].
Cystic fibrosis and post-renal transplantation also require long-term medication therapy. Medication adherence is critical for cystic fibrosis patients because it is linked to poor health outcomes such as pulmonary disease exacerbation, decreased baseline lung function, and prolonged hospitalization [66]. Meanwhile, post-renal transplantation requires strict adherence to immunosuppressive therapy to prevent acute rejection and loss of graft [67]. A previous study found that HBM constructs (perceived barriers and cues for action) are essential to predicting children’s adherence to medication [64]. In assessing adherence to immunosuppressive medications among post-renal transplant patients, their beliefs about susceptibility to acute graft rejection and perceived benefits of adhering to medication were essential predictors of medication adherence [63].
Type 2 diabetes mellitus has become an emerging problem globally because of the transition in behavior and lifestyle. As a result, the annual prevalence of type 2 diabetes mellitus has increased [68]. Adherence to medication and lifestyle modifications are the central importance in managing patients with diabetes. A previous study has shown the importance of HBM in developing strategies to improve medication adherence. A cross-sectional study found that perceived susceptibility to diabetes complications, perceived benefits of adhering to diabetes medications, and self-efficacy significantly predict medication adherence [65].
Several studies have been conducted to identify the usefulness of HBM constructs in improving adherence to anti-TB medications. Appropriate perception of self-vulnerability, perceived seriousness of non-adherent to medication, perceived barriers, self-confidence to adhere to the medication, and self-belief in the benefit of medication adherence were crucial in influencing medication adherence anti-TB [69,70]. Programmatic intervention, such as hypnotherapy, was found to be effective in adopting HBM and improving medication adherence [69].
Even though HBM helped develop strategies for changing behavior, especially in improving medication adherence, the model has several limitations. For example, HBM does not consider a person’s habitual behavior, which could inform the decision-making process to adopt the recommended behavior. Furthermore, HBM does not consider social acceptability that could complicate the behavioral changes, especially when particular ‘bad’ behavior is collectively accepted as a norm in society. HBM also assumes that everyone has equal access to information regarding illness and disease and could make those who are socially disadvantaged (e.g., poor, socially marginalized population, amongst others) unequally benefit from HBM intervention.
Limitations of Video Observed Therapy
Advancement of digital intervention may not only create the pace of changes and new opportunities but could potentially raise several issues, primarily technical and ethical dilemmas.
The use of VOT might not be equally accessible for those who are in a low socioeconomic background. The limitation might range from low smartphone access, low mobile internet subscription, limited internet connection, and low smartphone proficiency. Therefore, socioeconomically disadvantaged people are not equitably accessible to the needed intervention. However, according to the Department of Statistics Malaysia findings, 98% of Malaysian are using mobile phones. Among those using mobile phones, smartphone users have substantially increased from 89% in 2018 to 91% in 2019. This shows that affordability and accessibility to mobile phones are increasing and presumably will be followed by increasing smartphone literacy [71].
In terms of technicality, it is assumed that using VOT can subsequently reduce face-to-face contact. Thus, it raised the patient safety issue, whereby the patient might be missed if the patient developed anti-TB drug toxicity. Therefore, developing a strategy to maintain patient safety while adapting the new technology is essential.
Operability and usability are essential considerations in adopting new digital interventions. Operability is a measure of how well a new system works when operating. Meanwhile, acceptability refers to the user’s experience when interacting with a product or system, including websites, software, devices, or applications. Therefore, prior training to the related staff and a pilot study should be conducted before the digital intervention is implemented on a large scale.
Conclusion
Changing behavior is one of the critical factors that should be considered to improve medication adherence. Currently implemented DOT has several disadvantages that make medication adherence difficult. Digital technology provides an opportunity to improve medication adherence to overcome various issues related to DOT implementation. Nevertheless, most digital technology tools in TB do not apply the principle in behavioral change theory, thus making its effectiveness debatable. Thus, integrating the HBM and digital technology can likely achieve behavioral change and increase medication adherence. Applying HBM could provide a greater understanding of human behavior, while digital technology can enhance the implementation of DOT through the information obtained from HBM. Hence, it would be worthwhile to conduct a randomized clinical trial to formally investigate the effectiveness of applying HBM in modern digital technology tools to improve medication adherence.
Acknowledgments
The authors would like to thank the University of Malaysia of Sabah for permission to publish this paper.
Footnotes
Authors’ Contributions
Conceptualization: Sazali MF. Methodology: Sazali MF. Project supervision: Syed Abdul Rahim SS, Jeffree MS, Atil A. Writing - original draft preparation: Sazali MF. Writing - review and editing: Syed Abdul Rahim SS, Mohammad AH, Kadir F, Payus AO, Avoi R, Omar A, Ibrahim MY, Dapari R, Lansing MG, Abdul Rahim AA, Azhar ZI. Approval of final manuscript: all authors.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Funding
This research was partly funded by Universiti Malaysia Sabah’s SKIM GERAN INOVASI (SGI) UMS Research Grant (Grant ID: SGI0173).
REFERENCES
- 1.World Health Organization . Geneva: WHO; 2020. Global tuberculosis report 2020 [Internet] [cited 2022 Dec 26]. Available from: https://www.who.int/publications/i/item/9789240013131. [Google Scholar]
- 2.World Health Organization . Geneva: WHO; 2022. Global tuberculosis report [Internet] [cited 2022 Dec 26]. Available from: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022. [Google Scholar]
- 3.Cohen A, Mathiasen VD, Schon T, Wejse C. The global prevalence of latent tuberculosis: a systematic review and meta-analysis. Eur Respir J. 2019;54:1900655. doi: 10.1183/13993003.00655-2019. [DOI] [PubMed] [Google Scholar]
- 4.Ministry of Health Malaysia. Academy of Medicine Malaysia. Malaysian Thoracic Society. World Health Organization. Clinical . Putrajaya: Ministry of Health Malaysia; 2012. Clinical practice guidelines management of tuberculosis 3rd ed [Internet] [cited 2022 Dec 26]. Available from: https://www.moh.gov.my/moh/attachments/8612.pdf. [Google Scholar]
- 5.Choi R, Jeong BH, Koh WJ, Lee SY. Recommendations for optimizing tuberculosis treatment: therapeutic drug monitoring, pharmacogenetics, and nutritional status considerations. Ann Lab Med. 2017;37:97–107. doi: 10.3343/alm.2017.37.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naidoo P, Theron G, Rangaka MX, Chihota VN, Vaughan L, Brey ZO, et al. The South African tuberculosis care cascade: estimated losses and methodological challenges. J Infect Dis. 2017;216(Suppl 7):S702–13. doi: 10.1093/infdis/jix335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iribarren S, Beck S, Pearce PF, Chirico C, Etchevarria M, Cardinale D, et al. TextTB: a mixed method pilot study evaluating acceptance, feasibility, and exploring initial efficacy of a text messaging intervention to support TB treatment adherence. Tuberc Res Treat. 2013;2013:349394. doi: 10.1155/2013/349394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van LH, Phu PT, Vinh DN, Son VT, Hanh NT, Nhat LT, et al. Risk factors for poor treatment outcomes of 2266 multidrug-resistant tuberculosis cases in Ho Chi Minh city: a retrospective study. BMC Infect Dis. 2020;20:164. doi: 10.1186/s12879-020-4887-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization . Geneva: World Health Organization; 2015. The End TB Strategy [Internet] [cited 2022 Dec 26]. Available from: https://www.who.int/publications/i/item/WHO-HTM-TB-2015.19. [Google Scholar]
- 10.Subbaraman R, de Mondesert L, Musiimenta A, Pai M, Mayer KH, Thomas BE, et al. Digital adherence technologies for the management of tuberculosis therapy: mapping the landscape and research priorities. BMJ Glob Health. 2018;3:e001018. doi: 10.1136/bmjgh-2018-001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karumbi J, Garner P. Directly observed therapy for treating tuberculosis. Cochrane Database Syst Rev. 2015;5:CD003343. doi: 10.1002/14651858.CD003343.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salehitali S, Noorian K, Hafizi M, Dehkordi AH. Quality of life and its effective factors in tuberculosis patients receiving directly observed treatment short-course (DOTS) J Clin Tuberc Other Mycobact Dis. 2019;15:100093. doi: 10.1016/j.jctube.2019.100093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McLaren ZM, Milliken AA, Meyer AJ, Sharp AR. Does directly observed therapy improve tuberculosis treatment? More evidence is needed to guide tuberculosis policy. BMC Infect Dis. 2016;16:537. doi: 10.1186/s12879-016-1862-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization . Geneva: WHO; 2003. Adherence to long-term therapies: evidence for action [Internet] [cited 2022 Dec 26]. Available from: https://apps.who.int/iris/handle/10665/42682. [Google Scholar]
- 15.Valencia S, Leon M, Losada I, Sequera VG, Fernandez Quevedo M, Garcia-Basteiro AL. How do we measure adherence to anti-tuberculosis treatment? Expert Rev Anti Infect Ther. 2017;15:157–65. doi: 10.1080/14787210.2017.1264270. [DOI] [PubMed] [Google Scholar]
- 16.Vernon A, Fielding K, Savic R, Dodd L, Nahid P. The importance of adherence in tuberculosis treatment clinical trials and its relevance in explanatory and pragmatic trials. PLoS Med. 2019;16:e1002884. doi: 10.1371/journal.pmed.1002884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wahyuni AS, Soeroso NN, Wahyuni DD. Analysis of concordance of medication-taking behaviour in tuberculosis patients in Medan, Indonesia. Open Access Maced J Med Sci. 2018;6:1699–701. doi: 10.3889/oamjms.2018.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dickinson D, Wilkie P, Harris M. Taking medicines: concordance is not compliance. BMJ. 1999;319:787. doi: 10.1136/bmj.319.7212.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lei X, Huang K, Liu Q, Jie YF, Tang SL. Are tuberculosis patients adherent to prescribed treatments in China? Results of a prospective cohort study. Infect Dis Poverty. 2016;5:38. doi: 10.1186/s40249-016-0134-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kigozi G, Heunis C, Chikobvu P, Botha S, van Rensburg D. Factors influencing treatment default among tuberculosis patients in a high burden province of South Africa. Int J Infect Dis. 2017;54:95–102. doi: 10.1016/j.ijid.2016.11.407. [DOI] [PubMed] [Google Scholar]
- 21.Tok PS, Liew SM, Wong LP, Razali A, Loganathan T, Chinna K, et al. Determinants of unsuccessful treatment outcomes and mortality among tuberculosis patients in Malaysia: a registry-based cohort study. PLoS One. 2020;15:e0231986. doi: 10.1371/journal.pone.0231986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Woimo TT, Yimer WK, Bati T, Gesesew HA. The prevalence and factors associated for anti-tuberculosis treatment non-adherence among pulmonary tuberculosis patients in public health care facilities in South Ethiopia: a cross-sectional study. BMC Public Health. 2017;17:269. doi: 10.1186/s12889-017-4188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ajema D, Shibru T, Endalew T, Gebeyehu S. Level of and associated factors for non-adherence to anti-tuberculosis treatment among tuberculosis patients in Gamo Gofa zone, southern Ethiopia: cross-sectional study. BMC Public Health. 2020;20:1705. doi: 10.1186/s12889-020-09827-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mekonnen HS, Azagew AW. Non-adherence to anti-tuberculosis treatment, reasons and associated factors among TB patients attending at Gondar town health centers, Northwest Ethiopia. BMC Res Notes. 2018;11:691. doi: 10.1186/s13104-018-3789-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Story A, Aldridge RW, Smith CM, Garber E, Hall J, Ferenando G, et al. Smartphone-enabled video-observed versus directly observed treatment for tuberculosis: a multicentre, analyst-blinded, randomised, controlled superiority trial. Lancet. 2019;393:1216–24. doi: 10.1016/S0140-6736(18)32993-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kayigamba FR, Bakker MI, Mugisha V, De Naeyer L, Gasana M, Cobelens F, et al. Adherence to tuberculosis treatment, sputum smear conversion and mortality: a retrospective cohort study in 48 Rwandan clinics. PLoS One. 2013;8:e73501. doi: 10.1371/journal.pone.0073501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nguyen TA, Pham MT, Nguyen TL, Nguyen VN, Pham DC, Nguyen BH, et al. Video directly observed therapy to support adherence with treatment for tuberculosis in Vietnam: a prospective cohort study. Int J Infect Dis. 2017;65:85–9. doi: 10.1016/j.ijid.2017.09.029. [DOI] [PubMed] [Google Scholar]
- 28.Fang XH, Shen HH, Hu WQ, Xu QQ, Jun L, Zhang ZP, et al. Prevalence of and factors influencing anti-tuberculosis treatment non-adherence among patients with pulmonary tuberculosis: a cross-sectional study in Anhui Province, Eastern China. Med Sci Monit. 2019;25:1928–35. doi: 10.12659/MSM.913510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Du L, Chen X, Zhu X, Zhang Y, Wu R, Xu J, et al. Determinants of Medication adherence for pulmonary tuberculosis patients during continuation phase in Dalian, Northeast China. Patient Prefer Adherence. 2020;14:1119–28. doi: 10.2147/PPA.S243734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gavrilova A, Bandere D, Rutkovska I, Smits D, Maurina B, Poplavska E, et al. Knowledge about disease, medication therapy, and related medication adherence levels among patients with hypertension. Medicina (Kaunas) 2019;55:715. doi: 10.3390/medicina55110715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tola HH, Garmaroudi G, Shojaeizadeh D, Tol A, Yekaninejad MS, Ejeta LT, et al. The effect of psychosocial factors and patients’ perception of tuberculosis treatment non-adherence in Addis Ababa, Ethiopia. Ethiop J Health Sci. 2017;27:447–58. doi: 10.4314/ejhs.v27i5.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tesfahuneygn G, Medhin G, Legesse M. Adherence to anti-tuberculosis treatment and treatment outcomes among tuberculosis patients in Alamata District, northeast Ethiopia. BMC Res Notes. 2015;8:503. doi: 10.1186/s13104-015-1452-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang J, Yang Y, Qiao X, Wang L, Bai J, Yangchen T, et al. Factors influencing medication nonadherence to pulmonary tuberculosis treatment in Tibet, China: a qualitative study from the patient perspective. Patient Prefer Adherence. 2020;14:1149–58. doi: 10.2147/PPA.S252448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tola HH, Shojaeizadeh D, Tol A, Garmaroudi G, Yekaninejad MS, Kebede A, et al. Psychological and educational intervention to improve tuberculosis treatment adherence in Ethiopia based on health belief model: a cluster randomized control trial. PLoS One. 2016;11:e0155147. doi: 10.1371/journal.pone.0155147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Albasheer OB, Mahfouz MS, Solan Y, Khan DA, Muqri MA, Almutairi HA, et al. Depression and related risk factors among patients with type 2 diabetes mellitus, Jazan area, KSA: a cross-sectional study. Diabetes Metab Syndr. 2018;12:117–21. doi: 10.1016/j.dsx.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 36.Engidaw NA, Wubetu AD, Basha EA. Prevalence of depression and its associated factors among patients with diabetes mellitus at Tirunesh-Beijing general hospital, Addis Ababa, Ethiopia. BMC Public Health. 2020;20:266. doi: 10.1186/s12889-020-8360-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Azniza MR, Draman N, Siti Suhaila MY, Muhamad R. Depression and potential risk factors among the elderly with type 2 diabetes mellitus in Kedah, Malaysia. Med J Malaysia. 2019;74:103–8. [PubMed] [Google Scholar]
- 38.Yang TW, Park HO, Jang HN, Yang JH, Kim SH, Moon SH, et al. Side effects associated with the treatment of multidrug-resistant tuberculosis at a tuberculosis referral hospital in South Korea: a retrospective study. Medicine (Baltimore) 2017;96:e7482. doi: 10.1097/MD.0000000000007482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dar SA, Shah NN, Wani ZA, Nazir D. A prospective study on quality of life in patients with pulmonary tuberculosis at a tertiary care hospital in Kashmir, Northern India. Indian J Tuberc. 2019;66:118–22. doi: 10.1016/j.ijtb.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 40.Peh KQ, Kwan YH, Goh H, Ramchandani H, Phang JK, Lim ZY, et al. An adaptable framework for factors contributing to medication adherence: results from a systematic review of 102 conceptual frameworks. J Gen Intern Med. 2021;36:2784–95. doi: 10.1007/s11606-021-06648-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pradipta IS, Houtsma D, van Boven JF, Alffenaar JC, Hak E. Interventions to improve medication adherence in tuberculosis patients: a systematic review of randomized controlled studies. NPJ Prim Care Respir Med. 2020;30:21. doi: 10.1038/s41533-020-0179-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khachadourian V, Truzyan N, Harutyunyan A, Petrosyan V, Davtyan H, Davtyan K, et al. People-centred care versus clinic-based DOT for continuation phase TB treatment in Armenia: a cluster randomized trial. BMC Pulm Med. 2020;20:105. doi: 10.1186/s12890-020-1141-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Garfein RS, Liu L, Cuevas-Mota J, Collins K, Munoz F, Catanzaro DG, et al. Tuberculosis treatment monitoring by video directly observed therapy in 5 health districts, California, USA. Emerg Infect Dis. 2018;24:1806–15. doi: 10.3201/eid2410.180459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ratchakit-Nedsuwan R, Nedsuwan S, Sawadna V, Chaiyasirinroje B, Bupachat S, Ngamwithayapong-Yanai J, et al. Ensuring tuberculosis treatment adherence with a mobile-based CARE-call system in Thailand: a pilot study. Infect Dis (Lond) 2020;52:121–9. doi: 10.1080/23744235.2019.1688862. [DOI] [PubMed] [Google Scholar]
- 45.Guo P, Qiao W, Sun Y, Liu F, Wang C. Telemedicine technologies and tuberculosis management: a randomized controlled trial. Telemed J E Health. 2020;26:1150–6. doi: 10.1089/tmj.2019.0190. [DOI] [PubMed] [Google Scholar]
- 46.Browne SH, Umlauf A, Tucker AJ, Low J, Moser K, Gonzalez Garcia J, et al. Wirelessly observed therapy compared to directly observed therapy to confirm and support tuberculosis treatment adherence: a randomized controlled trial. PLoS Med. 2019;16:e1002891. doi: 10.1371/journal.pmed.1002891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bahia K, Suardi S. London: Global System for Mobile Communication Association; 2019. Connected society: the state of mobile internet connectivity 2019 [Internet] [cited 2022 Dec 26]. Available from: https://www.gsma.com/mobilefordevelopment/wp-content/uploads/2019/07/GSMA-State-of-Mobile-Internet-Connectivity-Report-2019.pdf. [Google Scholar]
- 48.Subbaraman R, Nathavitharana RR, Mayer KH, Satyanarayana S, Chadha VK, Arinaminpathy N, et al. Constructing care cascades for active tuberculosis: a strategy for program monitoring and identifying gaps in quality of care. PLoS Med. 2019;16:e1002754. doi: 10.1371/journal.pmed.1002754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bestrashniy JR, Nguyen VN, Nguyen TL, Pham TL, Nguyen TA, Pham DC, et al. Recurrence of tuberculosis among patients following treatment completion in eight provinces of Vietnam: a nested case-control study. Int J Infect Dis. 2018;74:31–7. doi: 10.1016/j.ijid.2018.06.013. [DOI] [PubMed] [Google Scholar]
- 50.Lee HK, Teo SSH, Barbier S, Tang SC, Yeo GH, Tan NC. The impact of direct observed therapy on daily living activities, quality of life and socioeconomic burden on patients with tuberculosis in primary care in Singapore. Proc Singap Healthc. 2016;25:235–42. [Google Scholar]
- 51.Goroh MM, Rajahram GS, Avoi R, Van Den Boogaard CH, William T, Ralph AP, et al. Epidemiology of tuberculosis in Sabah, Malaysia, 2012-2018. Infect Dis Poverty. 2020;9:119. doi: 10.1186/s40249-020-00739-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bojorquez I, Salazar I, Garfein RS, Cerecer P, Rodwell TC. Surveillance or support: the experience of direct observation during tuberculosis treatment. Glob Public Health. 2018;13:804–18. doi: 10.1080/17441692.2016.1240823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Furin J, Loveday M, Hlangu S, Dickson-Hall L, le Roux S, Nicol M, et al. “A very humiliating illness”: a qualitative study of patient-centered care for rifampicin-resistant tuberculosis in South Africa. BMC Public Health. 2020;20:76. doi: 10.1186/s12889-019-8035-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fatima R, Haq MU, Yaqoob A, Mahmood N, Ahmad KL, Osberg M, et al. Delivering patient-centered care in a fragile state: using patient-pathway analysis to understand tuberculosis-related care seeking in Pakistan. J Infect Dis. 2017;216(Suppl 7):S733–9. doi: 10.1093/infdis/jix380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Donahue ML, Eberly MD, Rajnik M. Tele-TB: using telemedicine to increase access to directly observed therapy for latent tuberculosis infection. Mil Med. 2021;186(Suppl 1):25–31. doi: 10.1093/milmed/usaa300. [DOI] [PubMed] [Google Scholar]
- 56.Garfein RS, Collins K, Munoz F, Moser K, Cerecer-Callu P, Raab F, et al. Feasibility of tuberculosis treatment monitoring by video directly observed therapy: a binational pilot study. Int J Tuberc Lung Dis. 2015;19:1057–64. doi: 10.5588/ijtld.14.0923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ngwatu BK, Nsengiyumva NP, Oxlade O, Mappin-Kasirer B, Nguyen NL, Jaramillo E, et al. The impact of digital health technologies on tuberculosis treatment: a systematic review. Eur Respir J. 2018;51:1701596. doi: 10.1183/13993003.01596-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Klonoff DC. Behavioral theory: the missing ingredient for digital health tools to change behavior and increase adherence. J Diabetes Sci Technol. 2019;13:276–81. doi: 10.1177/1932296818820303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Maiman LA, Becker MH. The health belief model: origins and correlates in psychological theory. Health Educ Monogr. 1974;2:336–53. [Google Scholar]
- 60.Ashraf M, Virk RN. Determinants of medication adherence in patients with HIV: application of the health belief model. J Pak Med Assoc. 2021;71:1409–12. doi: 10.47391/JPMA.1463. [DOI] [PubMed] [Google Scholar]
- 61.Wang MY, Shen MJ, Wan LH, Mo MM, Wu Z, Li LL, et al. Effects of a comprehensive reminder system based on the health belief model for patients who have had a stroke on health behaviors, blood pressure, disability, and recurrence from baseline to 6 months: a randomized controlled trial. J Cardiovasc Nurs. 2020;35:156–64. doi: 10.1097/JCN.0000000000000631. [DOI] [PubMed] [Google Scholar]
- 62.Yue Z, Li C, Weilin Q, Bin W. Application of the health belief model to improve the understanding of antihypertensive medication adherence among Chinese patients. Patient Educ Couns. 2015;98:669–73. doi: 10.1016/j.pec.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 63.Kung PC, Yeh MC, Lai MK, Liu HE. Renal transplant recipients: the factors related to immunosuppressive medication adherence based on the health belief model. J Nurs Res. 2017;25:392–7. doi: 10.1097/JNR.0000000000000181. [DOI] [PubMed] [Google Scholar]
- 64.Dempster NR, Wildman BG, Masterson TL, Omlor GJ. Understanding treatment adherence with the health belief model in children with cystic fibrosis. Health Educ Behav. 2018;45:435–43. doi: 10.1177/1090198117736346. [DOI] [PubMed] [Google Scholar]
- 65.Alatawi YM, Kavookjian J, Ekong G, Alrayees MM. The association between health beliefs and medication adherence among patients with type 2 diabetes. Res Social Adm Pharm. 2016;12:914–25. doi: 10.1016/j.sapharm.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 66.Eakin MN, Riekert KA. The impact of medication adherence on lung health outcomes in cystic fibrosis. Curr Opin Pulm Med. 2013;19:687–91. doi: 10.1097/MCP.0b013e3283659f45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sellares J, de Freitas DG, Mengel M, Reeve J, Einecke G, Sis B, et al. Understanding the causes of kidney transplant failure: the dominant role of antibody-mediated rejection and nonadherence. Am J Transplant. 2012;12:388–99. doi: 10.1111/j.1600-6143.2011.03840.x. [DOI] [PubMed] [Google Scholar]
- 68.Jai AN, Kassim ABM, Samad AA, Baharuddin A, Rosman A, Naidu BM, et al. Kuala Lumpur: Kementeri Kesihat Malaysia; 2016. National Health and Morbidity Survey 2016: maternal and child health [Internet] [cited 2022 Dec 26]. Available from: http://www.iku.gov.my/images/IKU/Document/REPORT/2016/NHMS2016ReportVolumeII-MaternalChildHealthFindingsv2.pdf. [Google Scholar]
- 69.Azizi N, Karimy M, Salahshour VN. Determinants of adherence to tuberculosis treatment in Iranian patients: application of health belief model. J Infect Dev Ctries. 2018;12:706–11. doi: 10.3855/jidc.9653. [DOI] [PubMed] [Google Scholar]
- 70.Prasetya H, Murti B, Anantanyu S, Syamsulhadi M. The effect of hypnosis on adherence to antituberculosis drugs using the health belief model. Int J Clin Exp Hypn. 2018;66:211–27. doi: 10.1080/00207144.2018.1421361. [DOI] [PubMed] [Google Scholar]
- 71.World Health Organization . Geneva: WHO; 2017. Digital technologies to support tuberculosis medication adherence [Internet] [cited 2022 Dec 26]. Available from: http://apps.who.int/iris/bitstream/10665/205222/1/WHO_HTM_TB_2015.21_eng.pdf?ua=1. [Google Scholar]


