Abstract
Objective
To assess pain relief and overall birth experience in induced vs. spontaneous-onset labours and to clarify variables among induced parturients determining satisfaction and dissatisfaction.
Study design
A prospective study of 2042 women. 575 women with induced and 1467 with spontaneous-onset labour answered multiple questions in a questionnaire regarding the experience of birth giving. Satisfaction was numerically assessed via a visual analogue scale (VAS 0–10).
Results
Induction of labour (IOL) did not worsen the average experience of pain relief, but the proportion of women dissatisfied with pain relief was slightly higher after IOL compared with spontaneous-onset labour (SOL). IOL was associated with lower satisfaction with overall birth experience compared with SOL (VAS 8.0 vs. 8.4; p < 0.001). Among IOL parturients incorrect timing of pain relief was strongly associated with dissatisfaction with pain relief, as were deficient information and induction with misoprostol. Epidural blockade was the most important factor preventing dissatisfaction with pain relief. Unsatisfactory overall experience of birth was associated with deficient pain relief, its incorrect timing or deficient information, as well as vacuum extraction as the mode of delivery.
Conclusions
Induction of labour is a risk factor of dissatisfaction regarding pain relief and overall birth experience. The strongest impact on dissatisfaction among induced parturients concerning pain relief was delayed timing of effective labour analgesia. Poor pain relief, its incorrect timing and deficient information on pain relief were strong predictive factors of dissatisfaction with the overall birth experience.
Keywords: Childbirth experience, Childbirth satisfaction, Pain relief in labour, Induction of labour
1. Introduction
Induction of labour (IOL) is an increasing obstetric intervention worldwide [1]. About every third delivery is induced, and in Finland the induction rate has more than doubled over the past two decades, being almost 32 % in 2019 [2]. There are controversial data on the connection between induction and women’s overall experience of birth and labour pain. In some studies women who have undergone induction are generally less satisfied with their birth experience compared with those having spontaneous-onset labours (SOLs); the need for pain relief is stronger and satisfaction with provided care is lower [3], [4], [5]. On the other hand, there are contrasting findings of post-term induced women having shorter labours with more intense and frequent contractions but positive experiences nevertheless [6]. Nuutila et al. found that women who had undergone IOL had similar positive experiences as women with spontaneous-onset labours; only pre-labour expectations differed [7].
Labour pain is usually the most intensive acute pain a woman will ever experience. But unlike other acute-pain conditions, which usually reflect a pathological process, labour pain is part of normal physiology [8], [9]. The experience of labour pain is a highly individual and complex process with multiple physiological and psychosocial aspects [9]. It has been shown that women underestimate in advance the pain they might experience in labour [10]. Ranta et al. found that 4 % of primiparous and 14 % of multiparous women expected antenatally to have no need of pain relief during labour, but 52 % of them required pain relief nevertheless [11]. Influences of personal expectations, support of caregivers and involvement in decision-making were important aspects when women evaluated their childbirth [12]. In a study by Dickinson et al., maternal satisfaction with intrapartum analgesia was significantly higher with epidural vs. non-epidural analgesic techniques. However, overall satisfaction scores for labour were high regardless of the analgesic approach, reflecting the multiple issues other than pain relief involved in the childbirth experience [13].
The aim of this study was to evaluate satisfaction with pain relief and overall birth experience in cases of induced labour vs. SOL. The secondary objective was to determine factors related to negative experiences with pain relief and birth experience among induced parturients.
2. Material and methods
2.1. Study population
This questionnaire study is part of a study of a 14-month cohort of mothers with successful vaginal birth between November 2015 and December 2016, focusing on satisfaction with labour-pain relief and overall birth satisfaction. Ethics approval for the study was given by the Ethics Committee of Pirkanmaa Hospital District (R15146), on the 16th of November 2015. All women with vaginal delivery and ability to answer the Finnish-language questionnaire were recruited. After written consent, midwives at the postnatal ward delivered the questionnaires to the parturients and they were asked to complete it on the second postpartum day. During the study period a total of 2042 women returned the forms. Of these women, 575 had undergone IOL and 1467 SOL. Most indications for IOL were medical, such as rupture of membranes, prolonged pregnancy, gestational diabetes, cholestasis of pregnancy and pre-eclampsia.
2.2. Study design
In the questionnaire, background factors and expectations of labour were assessed by way of open and multichoice questions. Overall birth experience and pain relief were measured by means of a visual analogue scale (VAS). This was presented as a straight 10-centimetre horizontal line, the ends being defined as 0 (completely dissatisfied) to 10 (completely satisfied). The women marked on the line the point that they felt represented their perception. Further, some multiple-choice questions were also used. If a woman had received more than one type of pain relief, she was asked to name the main type. An English translation of the questionnaire is shown in Appendix A. A VAS value of five was defined as a threshold for dissatisfaction, as in studies by Adler and Larsson [14], [15], five or less meaning lower satisfaction. VAS values of eight to ten were taken to mean satisfaction, in a similar manner as in the SWEPIS study [16].
2.3. Statistical analysis
Statistical analysis was performed by using IBM SPSS Statistics for Windows software, Version 26.0 (Armonk, NY, USA, 2019). Variables were tested for normality by using Shapiro–Wilk and Kolmogorov– Smirnov tests. Differences in continuous variables were studied by using Student’s t test in cases of normality and by the Mann–Whitney U test in cases of skewed distribution. Categorial variables were compared by using the chi-square test and Fisher’s exact test, as appropriate. R-squared values and lines of best fit from simple linear regression were used for presenting the relationship between birth experience and pain relief (Fig. 1). Binary logistic regression analyses were performed to assess the relative risk of a low VAS score (≤ 5) regarding the experiences of pain relief and giving birth. Each categorial variable was first analysed separately. Only the statistically significant variables in univariate models were included in multivariable models in order to control for possible confounding factors. When there were too few cases or missing answers the data were excluded in multivariable models (Tables 3 and 4). Odds ratios (ORs) with 95 % confidence intervals (CIs) are presented. A p-value of < 0.05 was considered statistically significant.
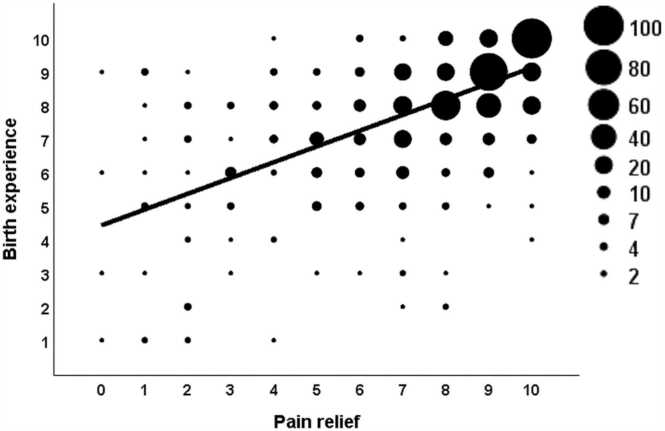
Fig. 1.
Scatter plot with marker size indicating the number of observations. There was a positive correlation between satisfaction with pain relief and the overall birth experience (r2 = 0.36, p < 0.001).
Table 3.
Determinants of dissatisfaction with pain relief among induced parturients. The statistically significant variables in univariate models were included in multivariable models.
| VAS ≤ 5 | VAS > 5 | Univariable analysis |
Multivariable analysis |
|||||
|---|---|---|---|---|---|---|---|---|
| n = 98 n (%) | n = 475 n (%) | OR | 95 % CI | p-value | OR | 95 % CI | p-value | |
| Primipara | 52 (53) | 245 (52) | 1.06 | 0.69–1.64 | 0.789 | |||
| Age > 35 | 17 (17) | 66 (14) | 1.30 | 0.73–2.33 | 0.378 | |||
| BMI > 35 | 8 (8) | 32 (7) | 1.23 | 0.55–2.76 | 0.614 | |||
| Misoprostol for induction | 51 (52) | 185 (39) | 1.70 | 1.10–2.63 | 0.017 | 1.69 | 1.05–2.73 | 0.031 |
| Balloon for induction | 13 (13) | 85 (18) | 0.70 | 0.37–1.32 | 0.70 | |||
| Oxytocin for induction | 43 (44) | 220 (46) | 0.91 | 0.59–1.40 | 0.91 | |||
| Amniotomy for induction | 31 (32) | 204 (43) | 0.62 | 0.39–0.98 | 0.039 | 1.21 | 0.73–2.00 | 0.456 |
| No pain relief | 4 (4) | 18 (4) | 1.08 | 0.36–3.27 | 0.891 | |||
| Oxycodone intramuscular only | 11 (11) | 11 (2) | 5.33 | 2.24–12.7 | < 0.001 | 2.08 | 0.91–4.79 | 0.084 |
| Nitrous oxide only | 19 (19) | 49 (10) | 2.09 | 1.17–3.74 | 0.013 | 1.12 | 0.70–1.78 | 0.650 |
| Paracervical block | 7 (7) | 25 (5) | 1.39 | 0.58–3.30 | 0.462 | |||
| Epidural analgesia | 30 (31) | 296 (62) | 0.27 | 0.17–0.43 | < 0.001 | 0.42 | 0.29–0.62 | < 0.001 |
| Spinal analgesia | 14 (14) | 55 (12) | 1.27 | 0.68–2.39 | 0.454 | |||
| Incorrect timing of pain relief | 69 (70) | 28 (6) | 40.5 | 22.6–72.8 | < 0.001 | 25.12 | 17.78–35.47 | < 0.001 |
| Deficient information | 32 (33) | 32 (7) | 6.79 | 3.90–11.8 | < 0.001 | 2.00 | 1.29–3.10 | 0.002 |
| Side effects of analgesic methods | 41 (42) | 250 (53) | 0.65 | 0.42–1.00 | 0.053 | |||
| Pre-labour wish for pain relief | 48 (49) | 266 (56) | 0.82 | 0.39–1.72 | 0.594 | |||
| Pre-labour wish for no pain relief | 6 (6) | 44 (9) | 0.65 | 0.27–1.57 | 0.340 | |||
| Dissatisfaction (VAS ≤ 5) with midwife | 9 (9) | 5 (1) | 9.51 | 3.1–29.0 | < 0.001a | |||
| Dissatisfaction (VAS ≤ 5) with obstetricianb | 3 (3) | 4 (1) | 3.78 | 0.82–17.4 | 0.088 | |||
| Dissatisfaction (VAS ≤ 5) with anesthesiologistc | 12 (12) | 12 (3) | 7.09 | 3.0–16.6 | < 0.001a | |||
| Mode of delivery | ||||||||
| Spontaneous delivery | 85 (87) | 413 (87) | 1.00 | |||||
| Vacuum delivery | 11 (11) | 55 (12) | 0.97 | 0.49–1.92 | 0.920 | |||
| Breech delivery | 2 (2) | 7 (1) | 1.39 | 0.29–6.81 | 0.682 | |||
Two parturients did not evaluate their pain relief.
These factors were not included in the multivariable analysis because of too few dissatisfied cases and missing answers.
333 answers (VAS ≤ 5, n = 57, VAS > 5, n = 276).
461 answers (VAS ≤ 5, n = 66, VAS > 5, n = 395).
Table 4.
Determinants of dissatisfaction with the overall birth experience among induced parturients. The statistically significant variables in univariate models were included in multivariable models.
| VAS ≤ 5 | VAS > 5 | Univariable analysis |
Multivariable analysis |
|||||
|---|---|---|---|---|---|---|---|---|
| n = 52 n (%) | n = 520 n (%) | OR | 95 % CI | p-value | OR | 95 % CI | p-value | |
| Primipara | 31 (60) | 264 (51) | 1.43 | 0.80–2.56 | 0.255 | |||
| Age > 35 | 9 (17) | 75 (14) | 1.24 | 0.58–2.65 | 0.576 | |||
| BMI > 35 | 5 (10) | 35 (7) | 1.47 | 0.55–3.94 | 0.437 | |||
| Misoprostol for induction | 27 (52) | 206 (40) | 1.65 | 0.93–2.92 | 0.087 | |||
| Balloon for induction | 7 (14) | 91 (18) | 0.73 | 0.32–1.68 | 0.463 | |||
| Oxytocin for induction | 29 (56) | 234 (45) | 1.54 | 0.87–2.74 | 0.140 | |||
| Amniotomy for induction | 21 (40) | 215 (41) | 0.96 | 0.54–1.72 | 0.893 | |||
| No medication | 1 (2) | 21 (4) | 0.47 | 0.06–3.54 | 0.460 | |||
| Oxycodone intramuscular only | 1 (2) | 20 (4) | 0.49 | 0.06–3.73 | 0.491 | |||
| Nitrous oxide only | 4 (8) | 64 (12) | 0.59 | 0.21–1.70 | 0.332 | |||
| Paracervical block | 4 (8) | 28 (5) | 1.46 | 0.49–4.35 | 0.492 | |||
| Epidural analgesia | 33 (63) | 291 (56) | 1.37 | 0.76–2.47 | 0.300 | |||
| Spinal analgesia | 6 (12) | 63 (12) | 0.95 | 0.39–2.31 | 0.903 | |||
| Incorrect timing of pain relief | 29 (56) | 65 (13) | 8.69 | 4.74–15.9 | < 0.001 | 2.54 | 1.06–6.06 | 0.036 |
| Insufficient information | 17 (33) | 46 (9) | 5.12 | 2.66–9.87 | < 0.001 | 2.66 | 1.20–5.88 | 0.016 |
| Side effects of analgesic methods | 27 (52) | 261 (50) | 1.07 | 0.61–1.90 | 0.812 | |||
| Pre-labour wish for pain relief | 7 (14) | 55 (11) | 1.31 | 0.56–3.04 | 0.534 | |||
| Pre-labour wish for no pain relief | 5 (10) | 45 (9) | 1.12 | 0.42–2.95 | 0.825 | |||
| Dissatisfaction (VAS ≤ 5) with pain relief | 31 (60) | 65 (13) | 10.3 | 5.58–19.0 | < 0.001 | 4.91 | 2.11–11.40 | < 0.001 |
| Dissatisfaction (VAS ≤ 5) with midwife | 9 (17) | 5 (1) | 21.6 | 6.92–67.2 | < 0.001a | |||
| Dissatisfaction (VAS ≤ 5) with obstetrician | 0 (0) | 7 (2)b | - | - | - | |||
| Dissatisfaction (VAS ≤ 5) with anesthesiologist | 3 (6) | 21 (5)c | 1.38 | 0.39 - 4.81 | 0.617 | |||
| Mode of delivery | ||||||||
| Spontaneous delivery | 40 (77) | 458 (88) | 1.00 | |||||
| Vacuum delivery | 12(23) | 53 (10) | 2.59 | 1.28 - 5.25 | 0.008 | 4.30 | 1.90–9.76 | < 0.001 |
| Breech delivery | 0 (0) | 9 (2) | - | - | - | |||
Three parturients did not evaluate their birth experience.
This factor was not included in the multivariable analysis because there were too few dissatisfied cases.
332 answers (VAS ≤ 5, n = 32, VAS > 5, n = 300).
416 answers (VAS ≤ 5, n = 44, VAS > 5, n = 416).
3. Results
During the study period 4740 women gave birth vaginally. Of these women, 2042 (41 %) completed and returned the questionnaire. Among induced mothers the response rate was 49 % and in the SOL group, 41 % responded (p < 0.001). The median time point at which the questionnaire was completed was two days postpartum. Demographic data concerning the parturients in the IOL and SOL groups are shown in Table 1.
Table 1.
Demographic data concerning IOL and spontaneous onset of labour.
| Characteristic | Induced |
Spontaneous |
p-value | |
|---|---|---|---|---|
| n = 575 | n = 1467 | |||
| Age (years) | ||||
| mean (SD) | 30 (5.2) | 30 (4.9) | ||
| median (range) | 30 (18–43) | 30 (16–47) | 0.874 | |
| Age > 35 n (%) | 84 (15) | 164 (11) | 0.033 | |
| BMI | ||||
| mean (SD) | 26 (5.5) | 24 (4.2) | ||
| median (range) | 24 (17–62) | 23 (16–45) | < 0.001 | |
| Gestational age at birth (days) | ||||
| mean (SD) | 279 (12.0) | 279 (9.6) | ||
| median (range) | 280 (177–297) | 281 (195–295) | 0.834 | |
| Primipara n (%) | 297 (52) | 278 (45) | 0.005 | |
| Mode of delivery n (%) | 0.009 | |||
|
500 (87) | 1335 (91) | ||
|
66 (11) | 107 (7) | ||
|
9 (2) | 25 (2) | ||
| Mode of induction n (%)a | ||||
|
236 (41) | |||
|
98 (17) | |||
|
264 (46) | |||
|
236 (41) | |||
| Pain-relief method n (%)b | < 0.001 | |||
|
22 (4) | 103 (7) | ||
|
22 (4) | 28 (2) | ||
|
68 (12) | 204 (14) | ||
|
32 (6) | 119 (8) | ||
|
326 (57) | 710(48) | ||
|
69 (12) | 220 (15) | ||
More than one mode of induction was needed among a few parturients. All methods used are shown.
The parturient chose the main pain-relief method by themselves. Six percent of cases in both groups were missing.
Satisfaction with pain relief was high among the total study population, mean VAS scores being 7.7 in the IOL group and 7.9 in the SOL group, with no significant difference between groups. The proportions of satisfied women (VAS ≥ 8) did not differ between the groups as regards pain relief. However, the proportion of those rating pain relief as unsatisfactory (VAS ≤ 5) was higher in the IOL group compared with the SOL group. Comparison of satisfaction rates in the two groups (IOL vs. SOL) as regards several components of labour care is shown in Table 2. Satisfaction with the overall birth experience was higher among SOL vs. IOL parturients. Likewise, women after SOL more often regarded their birth experience as good (VAS ≥ 8) and they were less often dissatisfied (VAS ≤ 5) compared with those after IOL. Satisfaction with caregivers was generally excellent, and there were no differences between the groups. Side-effects of the analgesic methods were assessed by the patients’ descriptions. The most common side-effects were itching and nausea.
Table 2.
Differences in birth-satisfaction scores in the IOL and SOL groups. Values adjusted by parity, BMI, age > 35, mode of delivery and main pain relief.
| Induced n = 575 | Spontaneous n = 1467 | p-value | Adjusted OR (95% CI); p-value | |
|---|---|---|---|---|
| Pain reliefa mean (SD) | 7.7 (2.40) | 7.9 (2.20) | 0.100 | |
| Dissatisfaction with pain | ||||
| relief (VAS ≤ 5) n (%) | 98 (17) | 174 (12) | 0.003 | 1.51 (1.12–2.04); 0.007 |
| Satisfaction (VAS ≥ 8) n (%) | 371 (65) | 992 (69) | 0.082 | 0.88 (0.71–1.10); 0.264 |
| Overall birth experiencea mean (SD) | 8.0 (1.84) | 8.4 (1.54) | < 0.001 | |
| Dissatisfaction with birth | ||||
| experience (VAS ≤ 5) n (%) | 52 (9) | 74 (5) | 0.001 | 1.60 (1.05–2.31); 0.028 |
| Satisfaction (VAS ≥ 8) n (%) | 411 (72) | 1150 (79) | 0.001 | 0.79 (0.62–1.00); 0.054 |
| Timing of pain reliefa mean (SD) | 7.8 (2.79) | 8.0 (2.49) | 0.405 | |
| Dissatisfaction with timing | ||||
| (VAS ≤ 5) n (%) | 96 (17) | 197 (13) | 0.125 | 0.86 (0.64–1.16); 0.322 |
| Satisfaction (VAS ≥ 8) n (%) | 393 (69) | 1017 (73) | 0.086 | 0.86 (0.68–1.08); 0.201 |
| Information about pain reliefa | ||||
| mean (SD) | 8.4 (2.12) | 8.3 (1.98) | 0.503 | |
| Dissatisfaction with | ||||
| information (VAS ≤ 5) n (%) | 64 (11) | 157 (11) | 0.875 | 1.00 (0.72–1.40); 0.984 |
| Satisfaction (VAS ≥ 8) n (%) | 434 (76) | 1085 (76) | 0.863 | 1.08 (0.85–1.38); 0.539 |
| Satisfaction with midwifea mean (SD) | 9.5 (1.20) | 9.5 (1.04) | 0.561 | |
| Dissatisfaction with midwife | ||||
| (VAS ≤ 5) n (%) | 14 (2) | 21 (1) | 0.131 | 0.62 (0.30–1.29); 0.197 |
| Satisfaction (VAS ≥ 8) n (%) | 549 (95) | 1389 (95) | 0.818 | 1.24 (0.75–2.06); 0.399 |
| Satisfaction with obstetriciana | ||||
| mean (SD) | 9.3 (1.22) | 9.2 (1.49) | 0.895 | |
| Dissatisfaction with | ||||
| obstetrician (VAS ≤ 5) n (%) | 7(2) | 23 (4) | 0.127 | 2.06 (0.82–5.20); 0.126 |
| Satisfaction (VAS ≥ 8) n (%) | 311 (93) | 509 (89) | 0.074 | 1.57 (0.93–2.66); 0.093 |
| Satisfaction with anaesthesiologista mean (SD) | 9.3 (1.66) | 9.1 (1.73) | 0.957 | |
| Dissatisfaction with | ||||
| anaesthesiologist (VAS ≤ 5) n (%) | 24 (5) | 58 (5) | 0.902 | 1.08 (0.64–1.82); 0.765 |
| Satisfaction (VAS ≥ 8) n (%) | 418 (91) | 943 (89) | 0.243 | 1.34 (0.91–1.97); 0.140 |
Scale 0–10, in which 0 = extremely poor and 10 = extremely good.
3.1. Dissatisfaction with pain relief among women in the IOL group
Factors affecting dissatisfaction with pain relief among IOL parturients were examined further and are shown in Table 3. In univariate regression analyses, induction with misoprostol showed an association with a negative experience, while amniotomy as the mode of induction affected the experience positively. Epidural analgesia resulted in the best satisfaction scores, while oxycodone and nitrous oxide were rated the most unsatisfactory as the principal pain-relief methods. After multivariable regression analysis, late timing of pain relief raised the risk of an unsatisfactory experience of pain treatment 25-fold. Epidural analgesia was the most important factor decreasing dissatisfaction, while deficient information and IOL with misoprostol doubled the risk of a negative experience.
3.2. Dissatisfaction with the overall birth experience among women in the IOL group
Table 4 shows the level of dissatisfaction (VAS ≤ 5) regarding the overall birthing experience among IOL parturients. According to the results of multivariable analysis, an experience of poor pain relief raised the risk of dissatisfaction fivefold, and vacuum delivery raised it over fourfold. Also, lack of information about pain-relief methods during labour, and incorrect timing of pain relief were negatively associated with the overall experience. Contentment with midwives’ work was high, as only 14 (2 %) women experienced their actions as being unsatisfactory. Dissatisfaction with the midwife was significantly connected to an unsatisfactory overall birth experience.
Among the IOL group, a strong positive correlation between satisfaction with pain relief and the overall birth experience was found (r2 = 36; p < 0.001) (Fig. 1). However, only 60 % of those women evaluating their overall birth experience as unsatisfactory were found to be dissatisfied with the pain relief, and on the other hand, only 32 % of the IOL parturients who evaluated their pain relief as being unsatisfactory had a negative birth experience. Further, there were 27 parturients who rated their experience of pain relief as unsatisfactory (VAS ≤ 5), but their overall birth-giving experience score was as much as eight or more.
4. Discussion
4.1. Main findings
Although the women in the study population were generally satisfied with their pain relief and overall birth experience, women in the IOL group showed a 1.5-fold greater risk of dissatisfaction. When focusing on satisfaction with pain relief, the strongest impact on dissatisfaction among IOL parturients was delayed timing of pain relief during labour, while epidural analgesia protected them from a negative experience of pain relief. When women in the IOL group considered their overall birth experience, unsatisfactory pain relief and its incorrect timing were found to be the most significant determinants of dissatisfaction, but also insufficient information about pain treatment during labour, as well as vacuum extraction as the mode of delivery were significant factors associated with dissatisfaction.
4.2. Strengths and limitations
A strength of this study is the large single-centre population of more than two thousand women who underwent vaginal birth. All evaluations concerning pain relief and the overall experience of birth were accomplished within a fairly narrow time range of approximately two days after birth. Although VAS scoring as an evaluation implement is subjective and may be influenced by several factors, it has been validated to reliably reflect birth experience and patient satisfaction [15], [17]. The cut-off point of five for dissatisfaction has been used in earlier studies [14], and by selecting this score negative experiences were definitely not underestimated. Also, the cut-off point of eight for satisfaction has been used earlier in a randomised controlled trial [16] for identifying women who were genuinely contented.
Answering the questionnaire relatively shortly after delivery may be considered a weakness, as evaluation of the birth experience so early could possibly be influenced by positive feelings towards the newborn [18]. We did not have a follow-up questionnaire later which could have brought a new view of the study. A higher proportion of women in the IOL group than in the SOL group participated in this study. The reason for this may be relatively larger numbers of primiparas and operative vaginal deliveries in the IOL group, which may have led to longer times in hospital postpartum. The difference in the proportions of women answering the questionnaire might have affected the results slightly and the lack of data from non-responders may also conceal selection bias.
4.3. Interpretation
In line with the results of our study, IOL has also been shown to be a risk factor of a poorer birth experience in studies carried out by Henderson and Hildingsson [4], [19]. In a study by Adler et al. the risk of a poor birth experience was twofold greater after IOL than after SOL, but the results of our study were not so striking [14].
Obesity, primiparity [20], [21] and advanced age have been found to be associated with both IOL and an unsatisfactory experience of birth [22], [23], but such associations were not seen in our study. Induction of labour has been associated with a risk of operative delivery [24], and in this study also the proportion of vacuum deliveries was greater in the IOL group than in the SOL group. As in former studies [14], [25], operative vaginal delivery led more often to a negative birthing experience. In our study there was a more than fourfold risk of a negative birth experience after vacuum extraction. Among induction methods, the use of misoprostol was to a slight degree connected to lower satisfaction with pain relief. It is possible that in these cases pain relief was inadequate or delayed because of the relatively long latent phase of labour. Capogna et al. also found that in labours induced with prostaglandins there were significantly greater analgesic requirements than among parturients undergoing SOL [26].
Epidural blockade is the gold standard in labour analgesia [27] and was used frequently in our study, more often among IOL than SOL parturients. Its use had a strong impact on satisfaction with pain relief, but it did not significantly influence the overall birth experience, not even according to the results of univariate analysis. This finding differed from that in a study by Karlsdottir et al., which showed that use of epidural blockade was a predictor of a positive childbirth experience [28]. The use of epidural blockade in our study was twice as common as in their study, which may partly explain the different results. It is possible that with frequent use of epidural blockade, factors other than pain relief may be the most important determinants of the birth experience.
Delayed timing of pain relief during labour had the strongest impact on dissatisfaction with both pain relief and overall birth experience among IOL parturients. Perfect timing of pain relief may be difficult to assess because of differences in women’s coping mechanisms during labour. Analgesia may also be delayed because of attitudes, such as fear of negative effects of epidural blockade on the progress of labour. This may be a particular problem among women undergoing IOL, because of the relatively long latent phase [29]. Similarly, Attanasio et al. found that among women with neuraxial analgesia during labour, both delayed and premature timing of pain relief had negative effects on their experience [30].
Only 32 % of the IOL parturients who evaluated their pain relief as unsatisfactory had a negative birth experience, but 60 % of the women whose birth experience was unsatisfactory were dissatisfied with their pain relief, which showed that the impact of pain relief alone on the birth experience may not be very strong. Although birth experience and pain relief during labour were strongly related to each other, 5 % of the parturients reported a good birth experience in spite of dissatisfaction with pain relief. Similar findings were also seen in a systematic review by Hodnett, suggesting that pain and pain relief do not have as powerful or direct influences on birth experience as attitudes and behaviour of caregivers [12]. In comparison of the IOL and SOL groups there was a difference in dissatisfaction with pain relief but not with satisfaction, while birth experience evaluations showed differences concerning both dissatisfaction and satisfaction, which indicates that pain relief is often more unequivocal, while birth experience is affected by several factors.
In our study only 14 (2 %) women who underwent IOL were dissatisfied with the care provided by their midwives, and they all had a negative birth experience, which shows the indispensable role of the midwife. A study by Sigurdardottir and colleagues showed that the support of midwives during pregnancy and birth had a significant impact on women’s birth experience [31]. Satisfaction with the work of obstetricians and anesthesiologists was also high, but it was not associated with the overall birth experience.
5. Conclusions
Induction of labour is a risk factor of dissatisfaction with both pain relief and overall birth experience. Induction with misoprostol may particularly increase this risk. Among factors protecting women undergoing IOL from dissatisfaction, good pain relief, its adequate timing and good information about it are most important. Although good pain relief is an important determinant of birth experience, good cooperation with caregivers, especially midwives, will also greatly influence the experience. Focusing on those women who rate their pain relief as satisfactory but report a negative overall birth experience might reveal important psychological aspects of labour care.
CRediT authorship contribution statement
KKM: study design, data collection, data analyses, manuscript preparation. OLP: study design, manuscript preparation. HJK: study design, data collection, manuscript preparation. MTH: data analyses. JTU: study design, manuscript preparation.
Funding
This study was financially supported by Tampere University Hospital Support Foundation, Tampere University Hospital. Funding sources have not been involved in the collection, analysis or interpretation of data or writing of the manuscript.
Conflicts of interest
The authors report no conflicts of interest.
Acknowledgements
We thank all the women who participated in this study in their very sensitive situation. Special thanks are owed to all midwives in the postnatal wards for making the study protocol possible.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.eurox.2023.100185.
Appendix A. Supplementary material
Supplementary material
References
- 1.Humphrey T., Tucker J.S. Rising rates of obstetric interventions: exploring the determinants of induction of labour. J Public Health [Internet] 2009;31(1):88–94. doi: 10.1093/pubmed/fdn112. [Available from: 〈 https://www.ncbi.nlm.nih.gov/pubmed/19141563〉] [DOI] [PubMed] [Google Scholar]
- 2.Sirkka K, Mika G, Anna H. Perinatal statistics—parturients, deliveries and newborns 2019. Statistical report 48/2020. National Institute for Health and Welfare (THL); 2020.
- 3.Shetty A., Burt R., Rice P., Templeton A. Women’s perceptions, expectations and satisfaction with induced labour—a questionnaire-based study. Eur J Obstet Gynecol [Internet] 2005;123(1):56–61. doi: 10.1016/j.ejogrb.2005.03.004. [Available from: 〈 https://www.sciencedirect.com/science/article/pii/S0301211505001363〉] [DOI] [PubMed] [Google Scholar]
- 4.Henderson J., Redshaw M. Women’s experience of induction of labor: a mixed methods study. Acta Obstet Gynecol Scand. 2013;92(10):1159–1167. doi: 10.1111/aogs.12211. [DOI] [PubMed] [Google Scholar]
- 5.Schaal N.K., Fehm T., Albert J., Heil M., Pedersen A., Fleisch M., et al. Comparing birth experience and birth outcome of vaginal births between induced and spontaneous onset of labour: a prospective study. Arch Gynecol Obstet [Internet] 2019;300(1):41–47. doi: 10.1007/s00404-019-05150-8. [Available from: 〈 https://www.ncbi.nlm.nih.gov/pubmed/30976970〉] [DOI] [PubMed] [Google Scholar]
- 6.Heimstad R., Romundstad P.R., Hyett J., Mattsson L.-Å., Salvesen K.Å. Women’s experiences and attitudes towards expectant management and induction of labor for post-term pregnancy. Acta Obstet Gynecol Scand [Internet] 2007;86(8):950–956. doi: 10.1080/00016340701416929. [Available from: 〈 https://www.ncbi.nlm.nih.gov/pubmed/17653880〉] [DOI] [PubMed] [Google Scholar]
- 7.Nuutila M., Halmesmaki E., Hiilesmaa V., Ylikorkala O. Womens anticipations of and experiences with induction of labor. Acta Obstet Gynecol Scand [Internet] 1999;78(8):704–709. [Available from: 〈 http://www.ingentaconnect.com/content/apl/aog/1999/00000078/00000008/art00008〉] [PubMed] [Google Scholar]
- 8.Whitburn L.Y., Jones L.E., Davey M.-A., McDonald S. The nature of labour pain: an updated review of the literature. Women Birth [Internet] 2019;32(1):28–38. doi: 10.1016/j.wombi.2018.03.004. [Available from: 〈 https://www.sciencedirect.com/science/article/pii/S1871519217306297〉] [DOI] [PubMed] [Google Scholar]
- 9.Lowe N.K. Parity and pain during parturition. J Obstet Gynecol Neonatal Nurs Jognn. 1987;16(5):340–346. doi: 10.1111/j.1552-6909.1987.tb01593.x. [DOI] [PubMed] [Google Scholar]
- 10.Lally J.E., Murtagh M.J., Macphail S., Thomson R. More in hope than expectation: a systematic review of women’s expectations and experience of pain relief in labour. BMC Med [Internet] 2008;6(1):7. doi: 10.1186/1741-7015-6-7. [Available from: 〈 https://www.ncbi.nlm.nih.gov/pubmed/18366632〉] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ranta P., Spalding M., Kangas‐Saarela T., Jokela R., Hollmén A., Jouppila R., et al. Maternal expectations and experiences of labour pain — options of 1091 Finnish parturients. Acta Anaesthesiol Scand [Internet] 1995;39(1):60–66. doi: 10.1111/j.1399-6576.1995.tb05593.x. [Available from: 〈 https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1399-6576.1995.tb05593.x〉] [DOI] [PubMed] [Google Scholar]
- 12.Hodnett E.D. Pain and women’s satisfaction with the experience of childbirth: a systematic review. Am J Obstet Gynecol. 2002 doi: 10.1067/mob.2002.121141. [DOI] [PubMed] [Google Scholar]
- 13.Dickinson J.E., Paech M.J., McDonald S.J., Evans S.F. Maternal satisfaction with childbirth and intrapartum analgesia in nulliparous labour. Aust New Zeal J Obstet Gynaecol. 2003;43(6):463–468. doi: 10.1046/j.0004-8666.2003.00152.x. [DOI] [PubMed] [Google Scholar]
- 14.Adler K., Rahkonen L., Kruit H. Maternal childbirth experience in induced and spontaneous labour measured in a visual analog scale and the factors influencing it; a two-year cohort study. BMC Pregnancy Childbirth [Internet] 2020;20(1):1–415. doi: 10.1186/s12884-020-03106-4. [Available from: 〈 https://search.proquest.com/docview/2435262952〉] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Larsson C., Saltvedt S., Edman G., Wiklund I., Andolf E. Factors independently related to a negative birth experience in first-time mothers. Sex Reprod Health [Internet] 2011;2(2):83–89. doi: 10.1016/j.srhc.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Nilvér H., Wessberg A., Dencker A., Hagberg H., Wennerholm U.B., Fadl H., et al. Women’s childbirth experiences in the Swedish Post-term Induction Study (SWEPIS): a multicentre, randomised, controlled trial. BMJ Open. 2021;11(4):1–10. doi: 10.1136/bmjopen-2020-042340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Voutilainen A., Pitkäaho T., Kvist T., Vehviläinen‐Julkunen K. How to ask about patient satisfaction? The visual analogue scale is less vulnerable to confounding factors and ceiling effect than a symmetric Likert scale. J Adv Nurs [Internet] 2016;72(4):946–957. doi: 10.1111/jan.12875. [Available from: 〈 https://onlinelibrary.wiley.com/doi/abs/10.1111/jan.12875〉] [DOI] [PubMed] [Google Scholar]
- 18.Soet J.E., Brack G.A., DiIorio C. Prevalence and predictors of women’s experience of psychological trauma during childbirth. Birth [Internet] 2003;30(1):36–46. doi: 10.1046/j.1523-536x.2003.00215.x. ]Available from: 〈 https://search.datacite.org/works/10.1046/j.1523-536x.2003.00215.x〉] [DOI] [PubMed] [Google Scholar]
- 19.Hildingsson I., Karlström A., Nystedt A. Women’s experiences of induction of labour – findings from a Swedish regional study. Aust New Zeal J Obstet Gynaecol [Internet] 2011;51(2):151–157. doi: 10.1111/j.1479-828X.2010.01262.x. [Available from: 〈 https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1479-828X.2010.01262.x〉] [DOI] [PubMed] [Google Scholar]
- 20.Dupont C., Blanc-Petitjean P., Cortet M., Gaucher L., Salomé M., Carbonne B., et al. Dissatisfaction of women with induction of labour according to parity: results of a population-based cohort study. Midwifery [Internet] 2020;84 doi: 10.1016/j.midw.2020.102663. [Available from: 〈 http://www.sciencedirect.com/science/article/pii/S026661382030036X〉] [DOI] [PubMed] [Google Scholar]
- 21.Waldenström U. Experince of labour and birth in 1111 women. J Psychosom Res. 1999;47(5):471–482. doi: 10.1016/s0022-3999(99)00043-4. [DOI] [PubMed] [Google Scholar]
- 22.O’Dwyer V., Kelly S., Monaghan B., Rowan A., Farah N., Turner M.J. Maternal obesity and induction of labor. Acta Obstet Gynecol Scand [Internet] 2013;92(12):1414–1418. doi: 10.1111/aogs.12263. [Available from: 〈 https://api.istex.fr/ark:/67375/WNG-H827B702-W/fulltext.pdf〉] [DOI] [PubMed] [Google Scholar]
- 23.Pinheiro R.L., Areia A.L., Mota Pinto A., Donato H. Advanced maternal age: adverse outcomes of pregnancy, a meta-analysis. Acta Med Port [Internet] 2019;32(3):219–226. doi: 10.20344/amp.11057. [Available from: 〈 https://www.ncbi.nlm.nih.gov/pubmed/30946794〉] [DOI] [PubMed] [Google Scholar]
- 24.Fruscalzo A., Londero A.P., Calcagno A., Cipriani I., Bertozzi S., Marchesoni D., et al. Building a prediction model for vacuum-assisted operative vaginal delivery risk. Gynecol Obstet Invest. 2015;80(4):246–252. doi: 10.1159/000381544. [DOI] [PubMed] [Google Scholar]
- 25.Bossano C.M., Townsend K.M., Walton A.C., Blomquist J.L., Handa V.L. The maternal childbirth experience more than a decade after delivery. Am J Obstet Gynecol [Internet] 2017;217(3):342.e1–342.e8. doi: 10.1016/j.ajog.2017.04.027. [Available from: 〈 https://search.datacite.org/works/10.1016/j.ajog.2017.04.027〉] [DOI] [PubMed] [Google Scholar]
- 26.Capogna G., Parpaglioni R., Lyons G., Columb M., Celleno D. Minimum analgesic dose of epidural sufentanil for first-stage labor analgesia: a comparison between spontaneous and prostaglandin-induced labors in nulliparous women. Anesthesiology [Internet] 2001;94(5):740–744. doi: 10.1097/00000542-200105000-00009. [Available from: 〈 https://www.ncbi.nlm.nih.gov/pubmed/11388522〉] [DOI] [PubMed] [Google Scholar]
- 27.Sng B.L., Leong W.L., Zeng Y., Siddiqui F.J., Assam P.N., Lim Y., et al. Early versus late initiation of epidural analgesia for labour. Cochrane Database Syst Rev. 2014;(10):CD007238. doi: 10.1002/14651858.CD007238.pub2. [CD007(10)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karlsdottir S.I., Sveinsdottir H., Kristjansdottir H., Aspelund T., Olafsdottir O.A. Predictors of women’s positive childbirth pain experience: findings from an Icelandic national study. Women Birth [Internet] 2018;31(3):e178–e184. doi: 10.1016/j.wombi.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 29.Østborg T.B., Romundstad P.R., Eggebø T.M. Duration of the active phase of labor in spontaneous and induced labors. Acta Obstet Gynecol Scand [Internet] 2017;96(1):120–127. doi: 10.1111/aogs.13039. [Available from: 〈 https://onlinelibrary.wiley.com/doi/abs/10.1111/aogs.13039〉] [DOI] [PubMed] [Google Scholar]
- 30.Attanasio L., Kozhimannil K., Jou J., McPherson M., Camann W. Women’s experiences with neuraxial labor analgesia in the listening to mothers II survey: a content analysis of open-ended responses. Anesth Analg [Internet] 2015;121(4):974–980. doi: 10.1213/ANE.0000000000000546. [Available from: 〈 https://www.ncbi.nlm.nih.gov/pubmed/25412403〉] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sigurdardottir V.L., Gamble J., Gudmundsdottir B., Kristjansdottir H., Sveinsdottir H., Gottfredsdottir H. The predictive role of support in the birth experience: a longitudinal cohort study. Women Birth [Internet] 2017;30(6):450–459. doi: 10.1016/j.wombi.2017.04.003. [Available from: 〈 https://search.datacite.org/works/10.1016/j.wombi.2017.04.003〉] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material