Abstract
Background
There are well‐recognized benefits of behavioral interventions that include exercise for children and adolescents with obesity. However, such behavioral weight management programs may precipitate unintended consequences. It is unclear if different exercise modalities impact eating behaviors differently in youth with obesity.
Objectives
The purpose of this study was to examine the effects of aerobic, resistance, and combined aerobic and resistance exercise training on eating attitudes and behaviors (uncontrolled eating, restrained eating, emotional eating, external eating and food craving) among adolescents with overweight and obesity.
Methods
N = 304 (70% female) adolescents with overweight and obesity participated in the 6‐month Healthy Eating Aerobic and Resistance Training in Youth (HEARTY) randomized controlled trial. All participants were inactive post‐pubertal adolescents (15.6 ± 1.4 years) with a mean BMI = 34.6 ± 4.5 kg/m2. The Food Craving Inventory (food cravings), Dutch Eating Behavior Questionnaire (restrained eating, emotional eating, external eating), and the Three‐Factor Eating Questionnaire (uncontrolled eating) were used to assess eating attitudes and behaviors.
Results
All exercise groups showed within‐group decreases in external eating and food cravings. Participants randomized to the Combined training group and were more adherent showed the greatest improvements in eating behaviors and cravings.
Conclusions
A 6‐month exercise intervention produced improvements in disordered eating behaviors and food cravings, but effects may be gender and modality‐specific. Findings highlight the need to tailor exercise intervention to participant characteristics for the promotion of healthier eating and weight management outcomes in youth with obesity.
Clinical Trial Registration # and Date: ClinicalTrials.Gov NCT00195858, September 12, 2005
Keywords: children, eating habits, eating pathology, overweight, physical activity, youth
1. INTRODUCTION
The first line of treatment for children and adolescents with obesity is often a behavioral intervention that utilizes dietary and exercise components to induce negative energy balance, reducing the risk of weight‐related issues. 1 Beyond weight loss, there are well‐recognized physical and mental health benefits of exercise in adolescents with obesity. 2 , 3 However, concerns have been raised that restricting caloric intake in behavioral weight management programs may precipitate unintended consequences, 4 such as disordered eating behaviors, and food cravings post‐intervention. Food craving is defined as an intense desire to consume a particular food 5 and has been shown to predict changes in body weight during weight management interventions in adults. 6 Disordered eating behaviors have also been associated with food overconsumption and weight gain among adolescents. 7
Adolescence is a high‐risk period for the development of disordered eating attitudes and behaviors (i.e., feelings indicating risk of an eating disorder) that are associated with body dissatisfaction, depressive symptoms, poor mental health and quality of life. 8 , 9 Disordered eating also increases the risk for the development of an eating disorder. 10 Examples of disordered eating behaviors include uncontrolled eating (i.e., eating more than usual due to loss of control over food intake), restrained eating (i.e., restricting food intake in order to control body weight), emotional eating (i.e., eating in response to negative or positive arousal states) and external eating (i.e., eating in response to food‐related stimuli, regardless of internal state of hunger or satiety). 11 , 12 Disordered eating is more prevalent in girls than boys 13 and in youth with obesity compared to youth without obesity. 14 Sex differences have also been reported in children's eating behaviors including food acceptance, food intake, appetitive traits, eating regulation and eating speed. 15 A systematic review of cross‐sectional and longitudinal observational studies of children and adolescents aged 11–18 years old revealed that boys consumed fast food more frequently whereas body image concerns, dieting and eating disorders were more common among girls. 16
A recent systematic review and meta‐analysis of the impact of obesity interventions with a dietary component reported reduced symptoms, risk, and prevalence of eating disorders in children and adolescents with obesity. 17 However, this review synthesized interventions with multiple treatment components (i.e., cognitive behavioral therapy, motivational interviewing, diet and physical activity educational counseling, structured physical activity, family‐based approaches). The included studies also primarily reported on per‐protocol rather than intention‐to‐treat analyses (decreasing representation of participants who withdrew from treatment) without examining differences in effects from different exercise modalities on eating behaviors.
Exercise influences energy balance through its effect on energy expenditure and energy intake. 18 A systematic review reported mean energy intake reductions of 323 ± 286 kcal in children and adolescents with obesity following chronic exercise interventions without dietary restriction (i.e., weeks to months of consistent exercise training). 19 Although the effects of exercise interventions on energy intake have been documented among children and adolescents with obesity, published studies have not consistently found that changes in eating behaviors and food cravings lead to such changes in daily energy intake or determined that differences in types of exercise modalities matter. 19 , 20 Considering that different exercise modalities (i.e., resistance vs. aerobic vs. combined training) have differential impacts on body composition, 21 physiological 3 and psychological outcomes, 22 exercise modality could differentially impact eating attitudes and behaviors in youth with obesity that warrant further study.
The purpose of this study was to determine the effects of aerobic training, resistance training, and combined aerobic and resistance exercise training on eating behaviors (uncontrolled, emotional, external and restrained eating) and food cravings in adolescents with obesity who participated in the HEARTY (Healthy Eating, Aerobic and Resistance Training in Youth) exercise trial. 21 , 23 The findings of the HEARTY exercise trial indicated that all exercise modalities (aerobic training, resistance training, and combined) reduced percent body fat. 21 Since previous studies have shown sex differences in the prevalence of eating disorders 13 and obesity 14 and sex differences children's eating behaviors, 15 the present study fills knowledge gaps from the aforementioned systematic review 17 by reporting results from intention‐to‐treat, per‐protocol and sex‐specific analyses from the HEARTY trial. The HEARTY trial showed decreases in daily energy intake in all three exercise groups (aerobic, resistance and their combination) with no significant between‐group differences. 21
This paper examined secondary outcomes of the HEARTY study to determine: 1) the effects of exercise training (aerobic, resistance and their combination) on eating behaviors and food cravings and 2) if these effects differed by sex. Participants' eating behaviors (emotional, external, and uncontrolled eating) and food cravings will decrease from baseline to post‐intervention. Despite the paucity of sex‐specific results from exercise interventions in adolescents with obesity, girls tend to have higher prevalence of disordered eating, thus, girls will have greater improvements in eating behaviors post‐intervention.
2. METHODS
2.1. Materials and methods
The rationale, design, methods, and main outcome results (percent body fat and cardiovascular risk markers) of the HEARTY trial have been published elsewhere. 21 , 23 The HEARTY trial was reviewed and approved by the Children's Hospital of Eastern Ontario and the Ottawa Hospital research ethics boards. All participants (and parents for participants younger than 16 years) provided written informed consent. The HEARTY study was powered to detect the primary outcome (percent body fat) as stated in the published methods paper 21 , 23 and paper reporting the original outcomes. 21 , 23 In this paper reporting secondary analyses, post hoc power for all secondary outcomes are not calculated based on the observed effect sizes.
2.2. Participants
Participant characteristics are presented in Table 1. After a 4‐week run‐in to assess exercise adherence (see next paragraph for details), 304 post‐pubertal (Tanner stage IV‐V) adolescents aged 14–18 years, body mass index (BMI) >95th percentile for age and sex, or >85th percentile plus a diabetes or cardiovascular risk factor, were randomized into 4 groups for 22 weeks (5 months): 1) Aerobic training (Aerobic, n = 75), 2) Resistance training (Resistance, n = 78), 3) Combined aerobic and resistance training (Combined, n = 75) or 4) Non‐exercising control (Control, n = 76). The CONSORT diagram is shown in Figure 1.
TABLE 1.
Baseline participant characteristics
| Aerobic | Resistance | Combined | Control | |
|---|---|---|---|---|
| N | 75 | 78 | 75 | 76 |
| Age (years) | 15.5 (1.4) | 15.9 (1.5) | 15.5 (1.3) | 15.6 (1.3) |
| Weight (kg) | 96.7 (15.1) | 99.9 (17.4) | 97.5 (16.3) | 97.9 (18.8) |
| Height (cm) | 166.9 (7.0) | 168.3 (7.5) | 167.5 (7.6) | 168.3 (7.7) |
| BMI (kg/m2) | 34.7 (4.2) | 35.1 (4.6) | 34.6 (4.2) | 34.1 (4.9) |
| Waist circumference (cm) | 96.4 (10.1) | 98.8 (11.4) | 96.8 (10.5) | 95.2 (11.8) |
| Body fat (%) | 49.1 (5.8) | 49.9 (5.8) | 50.3 (5.3) | 48.6 (5.3) |
| VO2peak (mLO2/kg/min) | 30.6 (5.1) | 29.9 (5.0) | 30.5 (5.1) | 30.6 (4.8) |
Note: Values are means (SD). Adherence was calculated for weeks 1–26 as the number of exercise sessions attended divided by 4, as participants were instructed to perform exercise 4 times per week.
Abbreviation: VO2peak,, Peak oxygen consumption.
FIGURE 1.
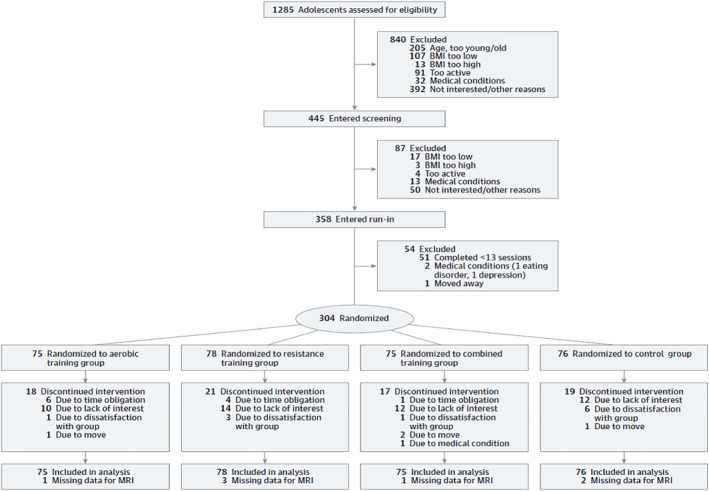
HEARTY screening, enrolment, and follow‐up
2.3. Intervention
Details of the exercise training program and diet counseling were published previously. 23 Briefly, participants in all four groups received dietary counseling by a registered dietitian, designed to promote healthy eating with a maximum daily energy deficit of 250 kcal. All participants and the individuals in their households involved in food preparation attended an initial visit with the dietitian to discuss weight and diet history, fast food consumption and current eating habits. Additional visits with the dietitian occurred at baseline, 3 and 6 months, with additional support provided by phone at 6 weeks and 4 months. Participants began with a 4‐week run‐in program whereby they were asked to perform both aerobic and resistance training four times per week. Aerobic exercise was performed at an intensity equivalent to 65% of the participants' maximum heart rate (HRmax), as determined by the baseline maximal treadmill exercise test, for 15–30 min per session. For the resistance training component of the sessions, participants were required to complete one to three sets of 15 reps at 15 Repetitions Maximum (RM; i.e., the maximum that could be moved 15 times through the full range of motion while maintaining proper form for the resistance training component). Participants who attended at least 13 of the 16 exercise run‐in sessions were then randomized to one of four groups for 22 weeks (weeks 5–26). Participants randomized to the three exercise groups exercised four sessions per week at local fitness centers in the Ottawa/Gatineau (Canada) region. They were supervised by personal trainers weekly for 8 weeks after randomization, then every 2 weeks thereafter. Participants in the aerobic training group exercised on treadmills, cycle ergometers, and/or elliptical machines; sessions progressed from 20 to 45 min in length. The Resistance training group performed three sets of seven whole‐body exercises per session on resistance machines and using free weights. The combined training group performed both the aerobic and the resistance components during each exercise session. The participants in the control group were asked to revert to their baseline activity levels and were offered the exercise program of their choice after the intervention period. The Exercise Specialist (responsible for overseeing all personal trainers) monitored attendance (for sessions that were directly supervised and those that were not) by reviewing sign‐in sheets and exercise logs and worked with the personal trainers in an effort to maximize attendance and progression over time to higher volumes and intensities of exercise. Adherence was calculated as the total number of exercise sessions the participant attended divided by the total number of sessions prescribed from baseline to the end of the intervention.
3. MEASUREMENTS
3.1. Energy intake, eating behaviors and food cravings
Energy intake and all questionnaires assessing eating behaviors and food cravings were assessed at baseline, 3, and 6 months. A 3‐day food log was used to determine total energy intake and separate macronutrient intake (carbohydrates, protein, and fat). The food logs were analyzed using food composition analysis software (The Food Processor SQL 2006; ESHA Research, Salem).
Participant food cravings were assessed with the Food Craving Inventory (FCI). The FCI is a 28‐item questionnaire with acceptable psychometric properties that measures specific food cravings and yields a total food cravings score. 24 This measure defines a food craving as “an intense desire to consume a particular food (or food type) that is difficult to resist”. 24 FCI measures cravings for four food categories: high‐fat foods (8 items), sweets (8 items), carbohydrates/starches (8 items), and fast‐foods (4 items). Using a 5‐point Likert scale ranging from 1 “not at all” to 5 “nearly every day”, participants rate how frequently they experience cravings for the specific foods. Scores for each food category are averages of the individual items within that subscale. As total scores are calculated as an average of all food item scores, the range of possible scores is from 1 “not at all” to 5 “nearly every day”. Higher scores indicate more frequent cravings for a specific food subscale. A validation study of the FCI in a sample consisting solely of adolescents with obesity has not been conducted. In this sample, the Cronbach's alpha for the FCI total scale as well as the high‐fat foods, sweets, carbohydrates/starches, and fast‐foods subscales were 0.91, 0.74, 0.88, 0.80 and 0.79, respectively.
The Dutch Eating Behavior Questionnaire (DEBQ) is a 33‐item questionnaire with acceptable psychometric properties that measures three eating behaviors: restrained (10 items), emotional (13 items), and external eating (10 items). 25 , 26 External eating is defined as eating in response to food‐related stimuli, regardless of the internal state of hunger or satiety. 25 , 27 Emotional eating is defined as eating in response to negative arousal states (emotions) such as anger, fear or anxiety. 28 Restrained eating is defined as a tendency to restrict food intake in order to control body weight. 11 , 29 Using a 5‐point Likert‐scale ranging from 1 “never” to 5 “very often”, participants rate how frequently they experienced each eating behavior. A score for each subscale (restrained, emotional and external eating) was calculated by summing the score for each item in that subscale, the range of possible scores is 10 to 50, 13 to 65 and 10 to 50, respectively. Higher scores are indicative of greater frequencies of emotional and external eating and greater restraint. This questionnaire has been validated in adolescents with normal weight, overweight, and obesity. 26 In this sample, the Cronbach's alpha for the restrained, emotional, and external eating subscales of the DEBQ were 0.89, 0.97, and 0.85, respectively.
The Three‐factor Eating Questionnaire (TFEQ) is a questionnaire used to measure emotionally‐ and externally‐triggered eating behaviors with three factors: cognitive restraint, uncontrolled eating, and emotional eating. 30 , 31 For the HEARTY study, only the uncontrolled eating subscale was used. This subscale measures the tendency to eat more than usual due to loss of control over food intake that is often accompanied by hunger. 12 To measure frequency of a behavior or how true a statement was, participants responded on a 4‐point Likert scale. 30 As uncontrolled eating subscale scores were calculated by summing the score for each item in that subscale, the range of possible scores is 0–16. Higher scores on the uncontrolled eating subscale indicated greater uncontrolled eating. 30 , 31 This scale showed acceptable psychometric properties among individuals with obesity. 30 Although more recent revised shortened and child versions of the TFEQ have been validated, it appears as though the original TFEQ has not been validated in adolescents with obesity. In this sample, the Cronbach's alpha for the uncontrolled eating subscale of the TFEQ was 0.76.
4. STATISTICAL ANALYSIS
The a priori analysis was intention‐to‐treat. Linear mixed‐effects regression modeling for repeated measures over time (0, 3, and 6 months) was used to assess the effects of exercise training modality on changes in eating behaviors and food cravings over time, with indicators of food craving (FCI), restrained eating, emotional eating, external eating behavior (DEBQ), and uncontrolled eating (TFEQ) as the dependent variables, and Time, Group (Aerobic, Resistance, Combined, Control), and Time × Group interaction as the independent variables, with adjustment for age and sex. Per‐protocol analyses of participants who completed ≥70% of prescribed exercise sessions (∼≥2.8 sessions/week) were also conducted. Sex‐specific analyses were also run to determine if eating behaviors and food cravings differed in response to exercise training modality by sex. Statistical analyses were performed using SAS, version 9.4 (SAS Institute, Cary, North Carolina).
5. RESULTS
5.1. Overall sample
The overall sample consisted of 304 adolescents with a mean BMI 34.6 ± 4.5 kg/m2 aged 15.6 ± 1.4 years old, and mainly females (70%) (Table 1). Most participants (282 of 304 [92.8%]) had obesity (BMI ≥95th percentile for age and sex). Median exercise training adherence did not differ between groups [62% (interquartile range, 36%–81%) in Aerobic, 56% (interquartile range, 37%–75%) in Resistance and 64% (interquartile range, 39%–75%) in Combined]. Energy intake and background physical activity intention‐to‐treat results have previously been published, 21 reproduced with permission in Table S1. Per‐protocol analysis results are presented in Table S2.
Intention‐to‐treat analysis in the overall sample showed that Combined training decreased cravings for sweets by 0.4 (−0.7, −0.1) units compared to Resistance alone (Table 2). Significant within‐group decreases from baseline to 6‐month were also observed for external eating (aerobic: −0.3, resistance: −0.2, combined: −0.3), overall food cravings (aerobic: −2 (−3.8, −0.3), resistance: −2.8 (−4.6, −1.1), combined: −2.4 (−4.1, −0.8)], sweets [aerobic: −2 (−3.8, −0.3), resistance: −2.8 (−4.6, −1.1), combined: −2.4 (−4.1, −0.8)], and fast‐food cravings [aerobic: −2 (−3.8, −0.3), resistance: −2.8 (−4.6, −1.1), combined: −2.4 (−4.1, −0.8)] in all exercise groups. However, there were no other significant between‐group differences in eating behaviors or food cravings over time.
TABLE 2.
Intention‐to‐treat analysis of eating behaviors and food cravings at baseline and changes after 3 and 6 months
| Mean (SE) | Mean (95% confidence interval) | |||||
|---|---|---|---|---|---|---|
| Variable | N | Baseline | 3 months | 6 months | Within‐group change from baseline to 6 months | Between‐group change from baseline to 6 months |
| TFEQ | ||||||
| Uncontrolled eating | ||||||
| Aerobic | 67 | 7.2 (0.4) | 6.8 (0.5) | 6.4 (0.4) | −0.8 (−1.5, 0) | |
| Resistance | 75 | 7.2 (0.4) | 6.7 (0.5) | 6 (0.4) | −1.2 (−2, −0.4)** | |
| Combined | 68 | 7.8 (0.4) | 7.3 (0.4) | 6.5 (0.4) | −1.3 (−2.1, −0.6)*** | |
| Control | 71 | 7.7 (0.4) | 7.3 (0.5) | 6.8 (0.4) | −0.9 (−1.7, −0.2)* | |
| Aerobic versus control | 0.2 (−0.9, 1.3) | |||||
| Resistance versus control | −0.3 (−1.3, 0.8) | |||||
| Combined versus aerobic | −0.6 (−1.6, 0.5) | |||||
| Combined versus resistance | −0.1 (−1.2, 0.9) | |||||
| DEBQ | ||||||
| Eating restraint | ||||||
| Aerobic | 67 | 25.5 (0.9) | 27.7 (1.1) | 26.8 (1) | 1.4 (−0.7, 3.4) | |
| Resistance | 75 | 23.3 (0.8) | 25.5 (1) | 24.3 (1) | 1 (−1, 3) | |
| Combined | 69 | 24.3 (0.8) | 25.6 (1) | 27.1 (0.9) | 2.8 (0.8, 4.8)** | |
| Control | 71 | 24.6 (0.8) | 24.6 (1.1) | 24.2 (1) | −0.4 (−2.4, 1.6) | |
| Aerobic versus control | 1.8 (−1.1, 4.7) | |||||
| Resistance versus control | 1.4 (−1.4, 4.3) | |||||
| Combined versus aerobic | 1.4 (−1.4, 4.3) | |||||
| Combined versus resistance | 1.8 (−1, 4.6) | |||||
| Emotional eating | ||||||
| Aerobic | 67 | 28.5 (1.5) | 28.9 (1.8) | 27.7 (1.7) | −0.8 (−3.9, 2.3) | |
| Resistance | 75 | 29.6 (1.4) | 26.6 (1.7) | 25.8 (1.7) | −3.7 (−6.8, −0.7)* | |
| Combined | 69 | 32.4 (1.5) | 30.3 (1.7) | 31 (1.7) | −1.3 (−4.3, 1.6) | |
| Control | 71 | 32.2 (1.5) | 32.2 (1.7) | 31.6 (1.7) | −0.6 (−3.6, 2.4) | |
| Aerobic versus control | −0.2 (−4.6, 4.1) | |||||
| Resistance versus control | −3.2 (−7.5, 1.1) | |||||
| Combined versus aerobic | −0.5 (−4.8, 3.7) | |||||
| Combined versus resistance | 2.4 (−1.8, 6.6) | |||||
| External eating | ||||||
| Aerobic | 66 | 29.9 (0.8) | 28.2 (0.9) | 27.8 (1) | −2 (−3.8, −0.3)* | |
| Resistance | 73 | 30.3 (0.8) | 28.8 (0.9) | 27.5 (1) | −2.8 (−4.6, −1.1)** | |
| Combined | 66 | 30.3 (0.8) | 28.5 (0.9) | 27.9 (0.9) | −2.4 (−4.1, −0.8)** | |
| Control | 69 | 29.6 (0.8) | 29.3 (0.9) | 28.5 (1) | −1.1 (−2.8, 0.6) | |
| Aerobic versus control | −1 (−3.4, 1.4) | |||||
| Resistance versus control | −1.8 (−4.2, 0.7) | |||||
| Combined versus aerobic | −0.4 (−2.8, 2) | |||||
| Combined versus resistance | 0.4 (−2, 2.8) | |||||
| FCI | ||||||
| Total | ||||||
| Aerobic | 66 | 2.2 (0.1) | 2.1 (0.1) | 1.9 (0.1) | −0.3 (−0.4, −0.1)*** | |
| Resistance | 75 | 2.3 (0.1) | 2 (0.1) | 2.1 (0.1) | −0.2 (−0.4, −0.1)** | |
| Combined | 69 | 2.4 (0.1) | 2.2 (0.1) | 2 (0.1) | −0.3 (−0.5, −0.2)*** | |
| Control | 71 | 2.1 (0.1) | 2 (0.1) | 2 (0.1) | −0.1 (−0.3, 0) | |
| Aerobic versus control | −0.2 (−0.4, 0) | |||||
| Resistance versus control | −0.1 (−0.3, 0.1) | |||||
| Combined versus aerobic | 0 (−0.2, 0.2) | |||||
| Combined versus resistance | −0.1 (−0.3, 0.1) | |||||
| Fats | ||||||
| Aerobic | 66 | 1.8 (0.1) | 1.6 (0.1) | 1.6 (0.1) | −0.2 (−0.4, −0.1)** | |
| Resistance | 75 | 1.8 (0.1) | 1.6 (0.1) | 1.7 (0.1) | −0.1 (−0.3, 0) | |
| Combined | 69 | 1.9 (0.1) | 1.8 (0.1) | 1.7 (0.1) | −0.1 (−0.3, 0) | |
| Control | 71 | 1.7 (0.1) | 1.7 (0.1) | 1.6 (0.1) | −0.1 (−0.2, 0.1) | |
| Aerobic versus control | −0.1 (−0.3, 0.1) | |||||
| Resistance versus control | 0 (−0.3, 0.2) | |||||
| Combined versus aerobic | 0.1 (−0.1, 0.3) | |||||
| Combined versus resistance | 0 (−0.2, 0.2) | |||||
| Sweets | ||||||
| Aerobic | 66 | 2.5 (0.1) | 2.3 (0.1) | 2.1 (0.1) | −0.4 (−0.6, −0.1)** | |
| Resistance | 75 | 2.5 (0.1) | 2.1 (0.1) | 2.3 (0.1) | −0.2 (−0.4, 0)* | |
| Combined | 69 | 2.7 (0.1) | 2.4 (0.1) | 2.2 (0.1) | −0.6 (−0.8, −0.4)*** | |
| Control | 71 | 2.3 (0.1) | 2.3 (0.1) | 2.1 (0.1) | −0.2 (−0.4, 0.1) | |
| Aerobic versus control | −0.2 (−0.5, 0.1) | |||||
| Resistance versus control | −0.1 (−0.4, 0.2) | |||||
| Combined versus aerobic | −0.2 (−0.5, 0.1) | |||||
| Combined versus resistance | −0.4 (−0.7, −0.1)* | |||||
| Carbohydrates | ||||||
| Aerobic | 66 | 2.1 (0.1) | 2.1 (0.1) | 1.9 (0.1) | −0.2 (−0.3, 0) | |
| Resistance | 75 | 2.2 (0.1) | 2.1 (0.1) | 2 (0.1) | −0.2 (−0.4, −0.1)* | |
| Combined | 69 | 2.2 (0.1) | 2.1 (0.1) | 1.9 (0.1) | −0.2 (−0.4, 0)* | |
| Control | 71 | 2 (0.1) | 1.9 (0.1) | 1.9 (0.1) | −0.1 (−0.3, 0.1) | |
| Aerobic versus control | −0.1 (−0.3, 0.2) | |||||
| Resistance versus control | −0.2 (−0.4, 0.1) | |||||
| Combined versus aerobic | −0.1 (−0.3, 0.2) | |||||
| Combined versus resistance | 0 (−0.2, 0.3) | |||||
| Fast foods | ||||||
| Aerobic | 66 | 2.7 (0.1) | 2.4 (0.1) | 2.2 (0.1) | −0.5 (−0.7, −0.2)*** | |
| Resistance | 75 | 2.9 (0.1) | 2.5 (0.1) | 2.5 (0.1) | −0.4 (−0.6, −0.1)** | |
| Combined | 69 | 3 (0.1) | 2.7 (0.1) | 2.6 (0.1) | −0.4 (−0.6, −0.2)** | |
| Control | 71 | 2.8 (0.1) | 2.5 (0.1) | 2.6 (0.1) | −0.2 (−0.5, 0) | |
| Aerobic versus control | −0.3 (−0.6, 0.1) | |||||
| Resistance versus control | −0.2 (−0.5, 0.2) | |||||
| Combined versus aerobic | 0.1 (−0.3, 0.4) | |||||
| Combined versus resistance | 0 (−0.3, 0.3) | |||||
Note: Scoring: TFEQ: 4‐point Likert‐scale ranging from 1 “almost never” to 4 “almost always”; DEBQ and FCI: 5‐point Likert‐scale ranging from 1 “never” to 5 “very often”.
Abbreviations: DEBQ, Dutch Eating Behavior Questionnaire; FCI, Food Craving Inventory; TFEQ, Three Factor Eating Questionnaire.
*p < 0.05, **p < 0.01, ***p < 0.001.
Per‐protocol analyses revealed that the participants with ≥70% adherence in the Combined training showed greater decreases in cravings for sweets by 0.7 (−1.2, −0.2) units compared to Resistance and by the same amount compared to Aerobic alone (−1.2, −0.3). Similarly, Combined training resulted in a decrease of 1.8 (−3.2, −0.5) units in uncontrolled eating compared to Aerobic alone (Table 3). Per‐protocol analysis revealed no between‐group differences in eating restraint, emotional eating, or food cravings.
TABLE 3.
Per‐protocol analysis of eating behaviors and food cravings at baseline and changes after 3 and 6 months
| Mean SE | Mean (95% confidence interval) | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | N | Baseline | N | 3 months | N | 6 months | Within‐group change from baseline to 6 months | Between‐group change from baseline to 6 months |
| TFEQ | ||||||||
| Uncontrolled eating | ||||||||
| Aerobic | 31 | 7.2 (0.6) | 24 | 7.3 (0.7) | 31 | 6.4 (0.6) | −0.8 (−1.7, 0.1) | |
| Resistance | 20 | 7 (0.7) | 18 | 6.9 (0.8) | 20 | 5.8 (0.7) | −1.2 (−2.3, −0.1)* | |
| Combined | 25 | 7.7 (0.6) | 23 | 6.4 (0.7) | 25 | 5.1 (0.6) | −2.6 (−3.6, −1.6)*** | |
| Control | 52 | 7.3 (0.4) | 42 | 7.1 (0.5) | 52 | 6.5 (0.4) | −0.8 (−1.5, −0.1)* | |
| Aerobic versus control | 0 (−1.1, 1.2) | |||||||
| Resistance versus control | −0.4 (−1.7, 0.9) | |||||||
| Combined versus aerobic | −1.8 (−3.2, −0.5)** | |||||||
| Combined versus resistance | −1.4 (−2.9, 0.1) | |||||||
| DEBQ | ||||||||
| Eating restraint | ||||||||
| Aerobic | 31 | 26.1 (1.2) | 25 | 28.9 (1.5) | 31 | 27.5 (1.3) | 1.4 (−1.4, 4.2) | |
| Resistance | 20 | 22.8 (1.5) | 19 | 23.3 (1.8) | 20 | 23.6 (1.6) | 0.8 (−2.8, 4.3) | |
| Combined | 25 | 23.5 (1.3) | 22 | 25.4 (1.6) | 25 | 26.9 (1.5) | 3.4 (0.2, 6.5)* | |
| Control | 52 | 24 (0.9) | 43 | 24.5 (1.1) | 52 | 23.9(1) | −0.1 (−2.3, 2.1) | |
| Aerobic versus control | 1.5 (−2.1, 5.1) | |||||||
| Resistance versus control | 0.8 (−3.3, 5) | |||||||
| Combined versus aerobic | 2 (−2.3, 6.2) | |||||||
| Combined versus resistance | 2.6 (−2.1, 7.3) | |||||||
| Emotional eating | ||||||||
| Aerobic | 31 | 27.7 (2.1) | 25 | 30.1 (2.3) | 31 | 28.9 (2.2) | 1.1 (−2.7, 5) | |
| Resistance | 20 | 29.8 (2.7) | 19 | 28 (2.8) | 20 | 26.2 (2.8) | −3.6 (−8.4, 1.2) | |
| Combined | 25 | 31.1 (2.4) | 22 | 28.4 (2.6) | 25 | 26.7 (2.5) | −4.3 (−8.7, 0)* | |
| Control | 52 | 29.7 (1.6) | 43 | 30.7 (1.8) | 52 | 30.1 (1.7) | 0.4 (−2.6, 3.4) | |
| Aerobic versus control | 0.7 (−4.2, 5.6) | |||||||
| Resistance versus control | −4 (−9.7, 1.6) | |||||||
| Combined versus aerobic | −5.5 (−11.3, 0.3) | |||||||
| Combined versus resistance | −0.7 (−7.2, 5.7) | |||||||
| External eating | ||||||||
| Aerobic | 30 | 30.7 (1.2) | 24 | 29.8 (1.2) | 30 | 29.2 (1.2) | −1.5 (−3.5, 0.4) | |
| Resistance | 20 | 31.3 (1.4) | 16 | 28.5 (1.5) | 20 | 27.6 (1.5) | −3.8 (−6.1, −1.4)** | |
| Combined | 23 | 29.2 (1.3) | 19 | 26.8 (1.4) | 23 | 24.9 (1.4) | −4.3 (−6.5, −2.1)*** | |
| Control | 48 | 29.2 (0.9) | 39 | 29.3(1) | 48 | 28.5(1) | −0.8 (−2.3, 0.8) | |
| Aerobic versus control | −0.8 (−3.2, 1.7) | |||||||
| Resistance versus control | −3 (−5.8, −0.2)* | |||||||
| Combined versus aerobic | −2.8 (−5.7, 0.2) | |||||||
| Combined versus resistance | −0.5 (−3.8, 2.7) | |||||||
| FCI | ||||||||
| Total | ||||||||
| Aerobic | 29 | 2.1 (0.1) | 23 | 2 (0.1) | 29 | 1.9 (0.1) | −0.2 (−0.3, 0) | |
| Resistance | 20 | 2.2 (0.1) | 19 | 2 (0.1) | 20 | 2.1 (0.1) | −0.2 (−0.4, 0) | |
| Combined | 24 | 2.5 (0.1) | 22 | 2 (0.1) | 24 | 2 (0.1) | −0.5 (−0.7, −0.3)*** | |
| Control | 51 | 2 (0.1) | 42 | 2 (0.1) | 51 | 1.9 (0.1) | −0.1 (−0.2, 0.1) | |
| Aerobic versus control | −0.1 (−0.3, 0.1) | |||||||
| Resistance versus control | −0.1 (−0.4, 0.1) | |||||||
| Combined versus aerobic | −0.4 (−0.6, −0.1)* | |||||||
| Combined versus resistance | −0.3 (−0.6, 0)* | |||||||
| Fats | ||||||||
| Aerobic | 29 | 1.7 (0.1) | 23 | 1.5 (0.1) | 29 | 1.5 (0.1) | −0.2 (−0.4, 0) | |
| Resistance | 20 | 1.8 (0.1) | 19 | 1.6 (0.1) | 20 | 1.7 (0.1) | −0.1 (−0.3, 0.1) | |
| Combined | 24 | 1.9 (0.1) | 22 | 1.5 (0.1) | 24 | 1.6 (0.1) | −0.3 (−0.5, −0.1)* | |
| Control | 51 | 1.6 (0.1) | 42 | 1.6 (0.1) | 51 | 1.6 (0.1) | 0 (−0.2, 0.1) | |
| Aerobic versus control | −0.1 (−0.4, 0.1) | |||||||
| Resistance versus control | −0.1 (−0.4, 0.2) | |||||||
| Combined versus aerobic | −0.1 (−0.4, 0.2) | |||||||
| Combined versus resistance | −0.2 (−0.5, 0.2) | |||||||
| Sweets | ||||||||
| Aerobi | 29 | 2.4 (0.2) | 23 | 2.5 (0.1) | 29 | 2.2 (0.1) | −0.3 (−0.6, 0) | |
| Resistance | 20 | 2.6 (0.2) | 19 | 2 (0.2) | 20 | 2.3 (0.2) | −0.3 (−0.6, 0.1) | |
| Combined | 24 | 3.1 (0.2) | 22 | 2.2 (0.2) | 24 | 2.1 (0.2) | −1 (−1.3, −0.7)*** | |
| Control | 51 | 2.2 (0.1) | 42 | 2.3 (0.1) | 51 | 2.1 (0.1) | −0.1 (−0.3, 0.1) | |
| Aerobic versus control | −0.2 (−0.5, 0.2) | |||||||
| Resistance versus control | −0.2 (−0.6, 0.3) | |||||||
| Combined versus aerobic | −0.7 (−1.2, −0.3)** | |||||||
| Combined versus resistance | −0.7 (−1.2, −0.2)** | |||||||
| Carbohydrates | ||||||||
| Aerobic | 29 | 1.9 (0.1) | 23 | 2 (0.1) | 29 | 1.9 (0.1) | 0 (−0.2, 0.3) | |
| Resistance | 20 | 2.1 (0.2) | 19 | 2 (0.2) | 20 | 2 (0.2) | −0.1 (−0.4, 0.2) | |
| Combined | 24 | 2.3 (0.1) | 22 | 2 (0.2) | 24 | 2 (0.2) | −0.3 (−0.5, 0) | |
| Control | 51 | 1.9 (0.1) | 42 | 1.8 (0.1) | 51 | 1.8 (0.1) | 0 (−0.2, 0.2) | |
| Aerobic versus control | 0 (−0.3, 0.3) | |||||||
| Resistance versus control | −0.1 (−0.4, 0.3) | |||||||
| Combined versus aerobic | −0.3 (−0.6, 0.1) | |||||||
| Combined versus resistance | −0.2 (−0.6, 0.2) | |||||||
| Fast foods | ||||||||
| Aerobic | 29 | 2.5 (0.2) | 23 | 2.4 (0.2) | 29 | 2.2 (0.2) | −0.3 (−0.6, 0) | |
| Resistance | 20 | 2.9 (0.2) | 19 | 2.5 (0.2) | 20 | 2.5 (0.2) | −0.4 (−0.8, 0)* | |
| Combined | 24 | 3 (0.2) | 22 | 2.5 (0.2) | 24 | 2.4 (0.2) | −0.6 (−1, −0.3)*** | |
| Control | 51 | 2.6 (0.1) | 42 | 2.5 (0.1) | 51 | 2.5 (0.1) | −0.1 (−0.4, 0.1) | |
| Aerobic versus control | −0.2 (−0.6, 0.2) | |||||||
| Resistance versus control | −0.3 (−0.8, 0.1) | |||||||
| Combined versus aerobic | −0.3 (−0.8, 0.1) | |||||||
| Combined versus resistance | −0.2 (−0.7, 0.3) | |||||||
Note: Participants who completed ≥70% of prescribed exercise sessions (∼≥2.8 sessions/week) were included in the per‐protocol analysis. Scoring: TFEQ: 4‐point Likert‐scale ranging from 1 “almost never” to 4 “almost always”; DEBQ and FCI: 5‐point Likert‐scale ranging from 1 “never” to 5 “very often”.
Abbreviations: DEBQ, Dutch Eating Behavior Questionnaire; FCI, Food Craving Inventory; TFEQ, Three Factor Eating Questionnaire.
*p < 0.05, **p < 0.01, ***p < 0.001.
5.2. Females
Intention‐to‐treat analysis only showed greater decreases in cravings for sweets with Combined training compared to Resistance alone (Table S3). Combined training also showed greater decreases in external eating compared to Aerobic alone.
Per‐protocol analysis showed that Combined training had greater decreases in uncontrolled eating compared to Aerobic alone and Resistance alone (Table S4). Decreases in emotional eating were also greater in Combined training compared to Aerobic alone. External eating decreased more in Combined training versus Aerobic training alone and in Resistance compared to Control. Overall food cravings and cravings for sweets decreased more in Combined training compared to Aerobic and Resistance groups alone. Per‐protocol analysis in females revealed no between‐group differences in eating restraint, cravings for fats, carbohydrates and fast foods.
5.3. Males
In contrast to the results observed in females only, intention‐to‐treat analysis in males only showed that the decreases in external eating in Aerobic and Resistance were greater than in Combined (Table S5).
Per‐protocol analyses revealed no significant differences in eating attitudes and behaviors when males were analyzed separately (Table S6).
6. DISCUSSION
This study is amongst the first that examined the effects of different exercise modalities on eating behaviors and food cravings in adolescents with obesity and the first to examine sex differences in these relationships. The results of this study showed that participants who were randomized to the Combined aerobic and resistance training group and were more adherent showed the greatest improvements in eating behaviors and cravings. The same pattern of results was observed among the females who completed ≥70% of prescribed exercise sessions (i.e., more adherent) but not the males, suggesting that these effects were mainly driven by female participants. Improvements in food cravings have been associated with long‐term weight loss in a clinical sample of adults with obesity. 32 Considering that disordered eating is more prevalent in girls than boys 13 and in youth with obesity compared to youth without obesity, 14 consistent monitoring of adolescent female eating behaviors during and after behavioral weight management interventions is warranted based on the changes observed in the current study. These findings indicate some improvements in eating behaviors from participating in the HEARTY trial from baseline to 6 months, although a longer‐term follow‐up is needed. It is safe for this population to engage in the HEARTY exercise and healthy eating program that has shown many physical and mental health benefits in previously published HEARTY papers. However, future weight management trials should monitor potential unintended consequences such as risks and harms of exercise as an intervention especially for youth at increased risk of disordered eating behaviors and eating disorders over time. Along with previous HEARTY findings showing improvements in psychological functioning 22 and health‐related quality of life 33 from exercise participation, these findings suggest that Combined exercise training and resistance training improved adolescents' disordered eating patterns and mental health during a 6‐month intervention period.
Due to the paucity of adolescent literature on this specific topic, the adult literature has been examined to guide speculations regarding this adolescent sample. One study examining the cross‐sectional and longitudinal associations of different exercise modalities and food cravings in healthy young adults reported that different exercise modalities have differential impacts on frequency and strength of food cravings and results differ by sex. 34 The researchers found that aerobic exercise was associated with cravings for fruits and difficulty resisting food cravings while walking was associated with increased chocolate cravings and the associations were more favorable for men compared to women. Specifically, they found positive effects of resistance exercise on food cravings in men but not in women. The greater improvements in eating behaviors and cravings observed with Combined training in this sample might be due to the larger dose of exercise (more time spent performing exercise per session over a 6‐month period) and the greater proportion of females (70%) in this sample, who tend to have greater food cravings and eating disorder psychopathology than males. 35 Females have also reported relating food cravings to their menstrual cycle 36 and changes in ovarian and serotonin hormone levels throughout the menstrual cycle. 37 These factors may have driven the improvements observed in eating behaviors while enrolled in a behavioral weight management intervention. However, more research is needed to understand the association between duration and intensity of exercise in relation to eating habits and food cravings (Figure 1).
Improvements in food cravings following acute and chronic aerobic training have been attributed to reduced activity in brain regions (i.e., the insula and putamen) 38 involved in food reward and visual food cues. 38 , 39 The insula is also involved in the regulation of other eating behaviors such as overeating disinhibition (i.e., uncontrolled eating). 39 , 40 To speculate, perhaps reduced neuronal activation related to visual food cues may also explain observed decreases in external eating (i.e., eating in response to food‐related stimuli) that were observed in all exercising groups post‐intervention. Future research on potential mechanisms is needed to investigate the influence of different exercise modalities on appetite hormones and neuronal responses involved in food reward and visual food cues, and how these relate to eating behaviors and food cravings and may have sex‐specific outcomes.
Exercise training positively impacts emotional state, mood and reduces stress 41 which can also influence eating attitudes and behaviors related to emotional regulation. In fact, previous analysis showed that all three HEARTY exercise groups improved their mood from baseline to 6 months by reduced anger and increased vigor 22 which aligns with the current findings showing decreases in external eating and food cravings in all exercise groups following the intervention. Exercise could impact eating behaviors through several psychological pathways, however, specific psychological mechanisms including motivation for food, palatability, wanting and food reinforcement were not assessed in this study but warrant further exploration especially in children and adolescents living with obesity.
Strengths of the study include the novelty of the research question, the randomized controlled trial design, which strengthens the internal validity of the data, and the inclusion of both intention‐to‐treat analyses and per‐protocol analyses to better evaluate exercise intervention effects on adherent participants. The statistical power to determine sex differences in eating behaviors and food cravings is limited by the unequal distribution of adolescent females versus males. Despite limited power, these findings demonstrate some sex‐related differences which suggest future studies with larger samples should examine exercise training effects on eating patterns in male versus female adolescents with obesity. In addition, the outcome variables (eating behaviors and food cravings) were assessed with the use of self‐reported questionnaires, which are subjective measures with inherent measurement error. The eating behaviors and food craving measures assessed in the HEARTY trial do not capture the full spectrum of eating disorder risks that could follow participation in behavioral interventions. In fact, the need for psychometrically‐strong measures of disordered eating symptoms specific to treatment‐seeking populations in weight management contexts has been identified as an important target for future research. 17
These results provide an important contribution to the literature in revealing that the current exercise trial had no unintentional consequences on the eating behaviors that were measured in most of the adolescents following participation in the HEARTY exercise program despite the trial's prescription of mild caloric restriction (∼250 kcal/day). It does, however, remain possible that eating disorder symptoms or eating disorder diagnoses may develop many years post‐intervention. 42 Future research is needed to examine other measures of eating behaviors and disordered eating specific to the weight loss context. To monitor the potential risk for disordered eating and mental health issues that may develop post intervention, follow‐up (>6 months) measures must be employed. 17 There is longitudinal evidence showing that greater disordered eating attitudes and behaviors were associated with lower body satisfaction, lower self‐esteem, greater depressive symptoms and greater BMI. 43 Thus, it is important to continuously monitor patients to ensure that healthy interventions do not transition to unhealthy and dangerous behaviors over time. 44 These findings align with findings from a systematic review and meta‐analysis of the impact of obesity interventions with a dietary component that revealed reductions in eating disorder prevalence, risk and related symptoms in children and adolescents with overweight or obesity. 17 However, the findings from the review paired with the results of the current study highlight the need for a future systematic review to discern the effects of structured exercise interventions alone (without confounding effects of other behavioral intervention components) on disordered eating patterns and eating disorder risk in children and adolescents with obesity.
7. CONCLUSION
The findings demonstrate that adolescents with overweight or obesity who showed good exercise adherence to 6‐month of combined aerobic and resistance exercise training reported improved eating behaviors, overall food cravings and sweet cravings compared to aerobic training alone. Analyses showed these effects were driven primarily by females. In the future, it is important that energy intake, eating behaviors, food cravings, and other disordered eating symptoms be regularly monitored as part of exercise intervention study designs and at follow‐up. Understanding how eating behaviors change throughout an exercise program could help explain mechanisms of how energy intake changes during and following exercise interventions, identify potentially negative unintended consequences and reduce risk of harm of participating in behavioral weight management programs.
AUTHOR CONTRIBUTIONS
Angela S. Alberga led the development and conceptualization of the manuscript. Angela Alberga S. Alberga and Iyoma Edache drafted the manuscript. All authors contributed important intellectual content and critically reviewed the manuscript. Steve Doucette conducted all statistical analyses. Angela S. Alberga collected data for the HEARTY study. Ronald J. Sigal, Glen P. Kenny, Gary S. Goldfield, Stasia Hadjiyannakis and Denis Prud'homme obtained federal funding for the HEARTY trial and contributed to the HEARTY study concept and design. Ronald J. Sigal was the Principal Investigator of the overall HEARTY study.
CONFLICT OF INTEREST
The author declares that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
We gratefully thank all the HEARTY participants and all the HEARTY research staff who assisted with training, data collection and analysis. von Ranson is a member of the University of Calgary's Mathison Center for Research and Education, O’Brien Institute for Public Health, Alberta Children's Hospital Research Institute, and Hotchkiss Brain Institute. The HEARTY trial was supported by a Canadian Institutes of Health Research (CIHR) grant (MCT‐71979). Alberga was supported by a Doctoral Student Research Award from the Canadian Diabetes Association during the trial and currently by a Chercheur Boursier Junior 1 Award from les Fonds de Recherche du Québec‐Santé. Ms. Iyoma Edache was supported by the France Andre Desmarais and William Sellers graduate student fellowships at Concordia University, Montreal. Goldfield was supported by a New Investigator Award from CIHR for part of the trial and was also supported by an Endowed Research Scholarship from the Children's Hospital of Eastern Ontario Volunteer Association Board. Sigal was supported by a Health Senior Scholar award from Alberta Innovates‐Health Solutions and by a Research Chair from the Ottawa Hospital Research Institute during part of this trial. Dr. Kenny was supported by a University of Ottawa Research Chair.
Alberga AS, Edache IY, Sigal RJ, et al. Effects of the HEARTY exercise randomized controlled trial on eating behaviors in adolescents with obesity. Obes Sci Pract. 2023;9(2):158‐171. 10.1002/osp4.620
REFERENCES
- 1. Carr KA, Epstein LH. Choice is relative: reinforcing value of food and activity in obesity treatment. Am Psychol. 2020;75(2):139‐151. 10.1037/amp0000521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Goldfield GS, Adamo KB, Rutherford J, Murray M. The effects of aerobic exercise on psychosocial functioning of adolescents who are overweight or obese. J Pediatr Psychol. 2012;37(10):1136‐1147. 10.1093/jpepsy/jss084 [DOI] [PubMed] [Google Scholar]
- 3. Alberga AS, Prud'homme D, Sigal RJ, et al. Effects of aerobic training, resistance training, or both on cardiorespiratory and musculoskeletal fitness in adolescents with obesity: the HEARTY trial. Appl Physiol Nutr Metabol = Physiologie appliquee, Nutr Metabol. 2016;41(3):255‐265. 10.1139/apnm-2015-0413 [DOI] [PubMed] [Google Scholar]
- 4. Devine CM, Barnhill A. The ethical and public health importance of unintended consequences: the case of behavioral weight loss interventions. Publ Health Ethics. 2018;11(3):356‐361. [Google Scholar]
- 5. Nielsen SJ, Siega‐Riz AM, Popkin BM. Trends in energy intake in U.S. between 1977 and 1996: similar shifts seen across age groups. Obes Res. 2002;10(5):370‐378. 10.1038/oby.2002.51 [DOI] [PubMed] [Google Scholar]
- 6. Smithson EF, Hill AJ. It is not how much you crave but what you do with it that counts: behavioural responses to food craving during weight management. Eur J Clin Nutr. 2017;71(5):625‐630. 10.1038/ejcn.2016.235 [DOI] [PubMed] [Google Scholar]
- 7. He J, Cai Z, Fan X. Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: an exploratory meta‐analysis. Int J Eat Disord. 2017;50(2):91‐103. 10.1002/eat.22661 [DOI] [PubMed] [Google Scholar]
- 8. Herpertz‐Dahlmann B, Dempfle A, Konrad K, Klasen F, Ravens‐Sieberer U, Group BS. Eating disorder symptoms do not just disappear: the implications of adolescent eating‐disordered behaviour for body weight and mental health in young adulthood. Eur Child Adolesc Psychiatr. 2015;24(6):675‐684. [DOI] [PubMed] [Google Scholar]
- 9. Allen KL, Byrne SM, Oddy WH, Crosby RD. DSM–IV–TR and DSM‐5 eating disorders in adolescents: prevalence, stability, and psychosocial correlates in a population‐based sample of male and female adolescents. J Abnorm Psychol. 2013;122(3):720‐732. [DOI] [PubMed] [Google Scholar]
- 10. Jebeile H, Lister NB, Baur LA, Garnett SP, Paxton SJ. Eating disorder risk in adolescents with obesity. Obes Rev. 2021;22. 10.1111/obr.13173 [DOI] [PubMed] [Google Scholar]
- 11. Herman CP, Mack D. Restrained and unrestrained eating 1. J Pers. 1975;43(4):647‐660. [DOI] [PubMed] [Google Scholar]
- 12. De Lauzon B, Romon M, Deschamps V, et al. The Three‐Factor Eating Questionnaire‐R18 is able to distinguish among different eating patterns in a general population. J Nutr. 2004;134(9):2372‐2380. [DOI] [PubMed] [Google Scholar]
- 13. Neumark‐Sztainer D, Story M, Hannan PJ, Perry CL, Irving LM. Weight‐related concerns and behaviors among overweight and nonoverweight adolescents: implications for preventing weight‐related disorders. Arch Pediatr Adolesc Med. 2002;156(2):171‐178. 10.1001/archpedi.156.2.171 [DOI] [PubMed] [Google Scholar]
- 14. Lampard AM, Maclehose RF, Eisenberg ME, Larson NI, Davison KK, Neumark‐Sztainer D. Adolescents who engage exclusively in healthy weight control behaviors: who are they? Int J Behav Nutr Phys Act. 2016;13:5. 10.1186/s12966-016-0328-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Keller KL, Kling SMR, Fuchs B, et al. A biopsychosocial model of sex differences in children's eating behaviors. Nutrients. 2019;11(3):682. Epub 2019/03/27. 10.3390/nu11030682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fletcher A, Bonell C, Sorhaindo A. You are what your friends eat: systematic review of social network analyses of young people's eating behaviours and bodyweight. J Epidemiol Commun Health. 2011;65(6):548‐555. 10.1136/jech.2010.113936 [DOI] [PubMed] [Google Scholar]
- 17. Jebeile H, Gow ML, Baur LA, Garnett SP, Paxton SJ, Lister NB. Treatment of obesity, with a dietary component, and eating disorder risk in children and adolescents: a systematic review with meta‐analysis. Obes Rev. 2019;20(9):1287‐1298. 10.1111/obr.12866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Blundell JE, Caudwell P, Gibbons C, et al. Role of resting metabolic rate and energy expenditure in hunger and appetite control: a new formulation. Dis Models Mech. 2012;5(5):608‐613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schwartz C, King NA, Perreira B, Blundell J, Thivel D. A systematic review and meta‐analysis of energy and macronutrient intake responses to physical activity interventions in children and adolescents with obesity. Pediatr Obesity. 2017;12(3):179‐194. [DOI] [PubMed] [Google Scholar]
- 20. Thivel D, Rumbold P, King NA, Pereira B, Blundell J, Mathieu M‐E. Acute post‐exercise energy and macronutrient intake in lean and obese youth: a systematic review and meta‐analysis. Int J Obes. 2016;40(10):1469. [DOI] [PubMed] [Google Scholar]
- 21. Sigal RJ, Alberga AS, Goldfield GS, et al. Effects of aerobic training, resistance training, or both on percent body fat and cardiometabolic risk markers in obese adolescents: the HEARTY trial. JAMA Pediatr. 2014;168(11):1006‐1014. 10.1001/jamapediatrics.2014.1392 [DOI] [PubMed] [Google Scholar]
- 22. Goldfield GS, Kenny GP, Alberga AS, et al. Effects of aerobic training, resistance training, or both on psychological health in adolescents with obesity: the HEARTY randomized controlled trial. J Consult Clin Psychol. 2015;83(6):1123‐1135. 10.1037/ccp0000038 [DOI] [PubMed] [Google Scholar]
- 23. Alberga AS, Goldfield GS, Kenny GP, et al. Healthy eating, aerobic and resistance training in youth (HEARTY): study rationale, design and methods. Contemp Clin Trials. 2012;33(4):839‐847. 10.1016/j.cct.2012.04.004 [DOI] [PubMed] [Google Scholar]
- 24. Dohm FA, Striegel‐Moore RH, Wilfley DE, Pike KM, Hook J, Fairburn CG. Self‐harm and substance use in a community sample of Black and White women with binge eating disorder or bulimia nervosa. Int J Eat Disord. 2002;32(4):389‐400. 10.1002/eat.10104 [DOI] [PubMed] [Google Scholar]
- 25. Van Strien T, Frijters JE, Bergers GP, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord. 1986;5(2):295‐315. [Google Scholar]
- 26. Wu S, Cai T, Luo X. Validation of the Dutch Eating Behavior Questionnaire (DEBQ) in a sample of Chinese adolescents. Psychol Health Med. 2017;22(3):282‐288. [DOI] [PubMed] [Google Scholar]
- 27. Schachter S, Goldman R, Gordon A. Effects of fear, food deprivation, and obesity on eating. J Pers Soc Psychol. 1968;10(2):91. [DOI] [PubMed] [Google Scholar]
- 28. Kaplan HI, Kaplan HS. The psychosomatic concept of obesity. J Nerv Ment Dis. 1957. [DOI] [PubMed] [Google Scholar]
- 29. Herman C, Polivy J. Restrained eating. In: Stunkard AJ, ed. Obesity. WB Saunders; 1980:208‐225. [Google Scholar]
- 30. Karlsson J, Persson L‐O, Sjöström L, Sullivan M. Psychometric properties and factor structure of the Three‐Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. Int J Obes. 2000;24(12):1715. [DOI] [PubMed] [Google Scholar]
- 31. Stunkard AJ, Messick S. The three‐factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71‐83. [DOI] [PubMed] [Google Scholar]
- 32. Dalton M, Finlayson G, Walsh B, Halseth AE, Duarte C, Blundell JE. Early improvement in food cravings are associated with long‐term weight loss success in a large clinical sample. Int J Obes (Lond). 2018;42(1):119. 10.1038/ijo.2017.238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Goldfield GS, Kenny GP, Alberga AS, et al. Effects of aerobic or resistance training or both on health‐related quality of life in youth with obesity: the HEARTY trial. Appl Physiol Nutr Metabol = Physiol Appl. 2017;42(4):361‐370. 10.1139/apnm-2016-0386 [DOI] [PubMed] [Google Scholar]
- 34. Drenowatz C, Evensen LH, Ernstsen L, et al. Cross‐sectional and longitudinal associations between different exercise types and food cravings in free‐living healthy young adults. Appetite. 2017;118:82‐89. [DOI] [PubMed] [Google Scholar]
- 35. Chao AM, Grilo CM, Sinha R. Food cravings, binge eating, and eating disorder psychopathology: exploring the moderating roles of gender and race. Eat Behav. 2016;21:41‐47. 10.1016/j.eatbeh.2015.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hormes JM, Orloff NC, Timko CA. Chocolate craving and disordered eating. Beyond the gender divide? Appetite. 2014;83:185‐193. 10.1016/j.appet.2014.08.018 [DOI] [PubMed] [Google Scholar]
- 37. Krishnan S, Tryon RR, Horn WF, Welch L, Keim NL. Estradiol, SHBG and leptin interplay with food craving and intake across the menstrual cycle. Physiol Behav. 2016;165:304‐312. 10.1016/j.physbeh.2016.08.010 [DOI] [PubMed] [Google Scholar]
- 38. Evero N, Hackett LC, Clark RD, Phelan S, Hagobian TA. Aerobic exercise reduces neuronal responses in food reward brain regions. J Appl Physiol. 2012;112(9):1612‐1619. [DOI] [PubMed] [Google Scholar]
- 39. Cornier M‐A, Melanson EL, Salzberg AK, Bechtell JL, Tregellas JR. The effects of exercise on the neuronal response to food cues. Physiol Behav. 2012;105(4):1028‐1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cornier M‐A, Salzberg AK, Endly DC, Bessesen DH, Rojas DC, Tregellas JR. The effects of overfeeding on the neuronal response to visual food cues in thin and reduced‐obese individuals. PLoS One. 2009;4(7):e6310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pedersen BK, Saltin B. Exercise as medicine – evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25(Suppl 3):1‐72. 10.1111/sms.12581 [DOI] [PubMed] [Google Scholar]
- 42. Jebeile H, Gow ML, Baur LA, Garnett SP, Paxton SJ, Lister NB. A response to the comments by Ms Adams on our paper “Treatment of obesity, with a dietary component, and eating disorder risk in children and adolescents: a systematic review with meta‐analysis”. Obes Rev. 2020;21(3):e12971. 10.1111/obr.12971 [DOI] [PubMed] [Google Scholar]
- 43. Yoon C, Simone M, Mason S, Neumark‐Sztainer D. A single summative global scale of disordered eating attitudes and behaviors: findings from Project EAT, a 15‐year longitudinal population‐based study. Eat Behav. 2020;39:101418. 10.1016/j.eatbeh.2020.101418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. National Eating Disorders Collaboration . Eating disorders and obesity treatments: a systematic review of the physical, psychological and eating disorders outcomes from obesity treatments; 2017. https://www.nedc.com.au/assets/NEDC-Publications/Obesity-Review-electronic-copy-cover2.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


