Abstract
The use of artificial intelligence (AI) in the medical field is increasing and is expected to shape future clinical practice and job security. Therefore, this study aimed to assess the opinions and attitudes of practicing physicians in Bahrain regarding the benefits and drawbacks of AI for their future daily practice. A cross-sectional survey of practicing physicians with a minimum of five years' experience across the main secondary and tertiary care hospitals in Bahrain was conducted. An online questionnaire was used to collect data on demographics, knowledge of AI, attitudes towards the use of AI in 10 tasks of daily clinical practice, and opinions on the benefits and drawbacks of AI. A total of 114 physicians participated in the survey. Among them, 43 (37.7%) were registered psychiatrists, 15 (13.2%) were pathologists, 17 (14.9%) were radiologists, and 39 (34.2%) were surgical specialists. The participants' attitudes were overall positive towards AI. Pathologists were particularly in favor of using AI to “Formulate personalized medication and/or treatment plans for patients” and to “Interview patients in a range of settings to obtain medical history.” Most participants agreed that AI would reduce the time needed to establish a diagnosis and negatively affect employment rates. There were no correlations between the responses and the participants’ age, gender, years of experience, or AI knowledge. This study demonstrates that the attitudes towards the use of AI in medicine among practicing physicians in Bahrain are similar to those of physicians in developed countries in that they are positive and welcoming of AI implementation in practice. However, the potential effects of AI on job security are a major concern.
Keywords: Artificial intelligence, Attitude, Bahrain, Knowledge, Benefits, Physicians, Drawbacks
1. Introduction
Artificial intelligence (AI) is defined as “the science and engineering of making intelligent machines” [1] The application of AI in medicine is anticipated through two main branches – virtual, which involves mathematical algorithms improving learning; physical, which involves the use of robots and medical devices [2,3]. The widespread use of advanced technologies and the imminent challenges of AI could pose a threat to physicians’ jobs [4]. Some AI experts feel that the role of physicians will customarily become a joint team effort between physicians and machines [5]. Hitherto, there has been little contemplation about the attitudes of physicians regarding the future role of AI in medicine and how it will affect their job security and practices.
AI is therefore best defined as a broad field of research that seeks to develop machines that are able to think and act like humans. It involves using sophisticated algorithms, or “intelligence,” to process data and make decisions that can solve a given problem or task [[1], [2], [3], [4], [5]]. AI is used in a variety of fields such as robotics, healthcare, finance, education, and more [[1], [2], [3], [4], [5]]. AI can be used to make more accurate predictions, help develop better decision-making processes, and automate tedious tasks [2,3]. AI has advanced significantly over the past decades and is expected to continue to grow in complexity and applications in the years to come [1,4,5]. In its simplest form, artificial intelligence is a type of technology that enables machines to think, act, and behave as if they were human [3,4]. Through the use of algorithms and data-driven learning, AI systems are able to learn and adapt to different situations, providing actionable insights and solutions [[1], [2], [3], [4], [5]].
A recent global survey of 791 psychiatrists, mostly from developed countries, found that 83% of the study sample believed that it was unlikely that future technology could provide empathetic care, and 3.8% of the respondents felt that it would make their jobs obsolete [6]. In another study involving radiologists, 77% of the participants reported favorable attitudes towards the adoption of AI, and 89% were not afraid of losing their jobs [7]. Another global survey of pathologists revealed a high percentage of acceptance of AI, with only 17.6% of respondents being concerned about their future job security [8]. Likewise, 60% of the neurosurgeons in a study reported using AI for the purpose of predicting outcomes [9], and 90% of the physicians contacted from different specialties in Germany expected the future of medicine to include a mix of human intelligence and AI [10]. Another study from Germany that assessed patients’ opinions regarding the use of AI in clinical practice revealed a strong preference for physicians overseeing the various clinical tasks as compared to AI [11].
On the contrary, a study from the United Kingdom reported that general physicians (GPs) were apprehensive of AI's ability to provide empathetic care [12]. Similarly, an Asian study evaluating physicians' attitudes towards AI found significant disparities in expectations and concerns regarding the legal aspects of AI applications [13]. Several studies have examined the attitudes of physicians towards the use of AI in the Arab world. In Oman, a study involving 300 physicians and 750 medical students from different specialties found that physicians have a positive perspective about the future use of AI and were generally not concerned about AI potentially replacing their jobs [14]. In the United Arab Emirates, a study with 119 radiographers and 34 radiologists reported that 86% of participants disagreed with the idea of AI playing a role in radiology, and 64% of participants were not concerned that AI would negatively affect their professional careers [15]. In a Saudi Arabian study, the majority of the sub-sample of radiologists were in favor of introducing AI in radiology practice (95%), with only 30% concerned about AI replacing their jobs [16]. A study from Syria investigating the knowledge, attitude, and practices of AI among physicians and medical students showed that only a small percentage of participants strongly agreed (8.4%) or agreed (13.1%) that AI could replace physicians in the future [17]. Contrary to the aforementioned studies, another Saudi Arabian study, in which the authors targeted physicians, nurses, and technologists revealed that 77.75% of respondents are concerned about their future jobs [18]. Apart from that, a recent local study was found which utilized A. I to determine clients' satisfaction with inpatient psychiatric services [19].
To further add to the literature in this regard, the authors investigated the opinions of physicians from different specialties in Bahrain about the influence of AI on their daily clinical work, its benefits, and effects on job security. In Bahrain, the use of AI in the healthcare industry is in its earliest stages. The authors speculated that local physicians’ opinions towards AI would be comparable to global opinions in many respects, owing to the extensive use of technology by Bahraini citizens in everyday life.
2. Materials and methods
2.1. Design and participants
A cross-sectional survey was conducted from October to December 2021 involving all registered psychiatrists, pathologists, and physicians practicing Ear, Nose, and Throat (ENT) and ophthalmology specialties in the main secondary care facility in Bahrain. The inclusion criteria included physicians practicing medicine from all sexes and nationalities, with a minimum of five years of experience following medical school graduation. By using a confidence level of 95%, margin of error of 5%, an effective response distribution of assumed 80% of total population size of 228, the estimated sample size is 119, we obtained 114.
Equations for sample size n and margin of error E are given by:
2.2. Procedure
The survey was administered online using Google Forms. Prior to participation, the participants were informed about the objectives of the study and procedure, and informed e-written consent with terms was obtained. Participants had to “check the box” of agree/disagree; participation was voluntary and the participants could withdraw from the study at any stage. The survey was pilot tested for clarity on six physicians. Ethical approval was obtained from the Ethical and Research Committee, College of Medicine and Medical Sciences, Arabian Gulf University, Bahrain (approval number: E34-pi-12-21, dated: December 28, 2021).
2.3. Instrument and data collection
A validated questionnaire from a previous study was used after obtaining formal permission from the original authors (6) via e-mail. The online survey consisted of three parts: 1) Demographic and AI knowledge; 2) Attitudes towards the future use of AI; and 3) AI benefits and drawbacks. The first part included questions regarding age, gender, years of experience, and self-rating of AI knowledge. The second part dealt with the future application of AI in 10 tasks of daily clinical work. The respondents were asked to mark the response to each task question as ‘likely’, ‘unlikely’, or ‘cannot judge’.
The following tasks were included in the questionnaire – “Provide documentation”, “Provide empathetic care to patients”, “Interview patients in a range of settings to obtain medical history”, “Analyze patient information to detect possibility of criminal behavior/assault”, “Analyze patient information to detect self-harmful behavior”, “Synthesize patient information to reach diagnosis”, “Formulate personalized medication and/or treatment plans for patients”, “Evaluate when to refer patients to outpatient versus inpatient treatments”, “Analyze patient information to establish prognoses” and “Perform a physical examination, including mental status examinations”.
The third part of the survey included the following items to evaluate the benefits and drawbacks of AI – “Affect life expectancy through easier access to healthcare”, “Cut down the time needed for diagnosis”, “Impact people with disability and mental health issues”, “Affect employment rates in the healthcare industry”, and “Perform with a less error rate than human physicians”.
2.4. Data analysis
IBM Statistical Package for the Social Sciences (SPSS) version 28 for Windows [IBM Corp., Armonk, NY, USA] was used for data analysis. Categorical data were expressed using frequency and percentages, while continuous data were analyzed using the mean and standard deviation. Analysis of Variance (ANOVA) and Post Hoc analysis with Bonferroni correction were used to assess differences among the means of different physician specialties. A p-value of less than 0.05 was considered statistically significant.
3. Results
A total of 114 physicians responded to the survey, most of whom were women (55.3%). Almost two-thirds (64.3%) of respondents belong to the younger age group of 30–50 years. The respondents were distributed among different clinical specialties as follows: psychiatry (n = 43 out of 53 contacted (81.3%), 10 were excluded due to retirement and change in job), pathology (n = 15/20, 75%), radiology (n = 17/23, 74%), and surgical specialties (n = 39/65, 60%). The population of psychiatrists and pathologists was accessed from a national registry, while radiologists and surgical specialists were physicians practicing medicine in the main general hospital, Salmaniya Medical Complex, Bahrain. The results for the socio-demographic characteristics and AI knowledge of the study participants are shown in Table 1.
Table 1.
Demographic data and AI knowledge (n = 114).
| Item | Category* | Psychiatry |
Pathology |
Radiology |
Surgical Specialties |
Total |
|---|---|---|---|---|---|---|
| (n = 43) |
(n = 15) |
(n = 17) |
(n = 39) |
(n = 114) |
||
| N (%) | ||||||
| Gender | Male | 19 (44.2) | 4 (26.7) | 9 (52.9) | 19 (48.7) | 51 (44.7) |
| Female | 24 (55.8) | 11 (73.3) | 8 (47.1) | 20 (51.3) | 63 (55.3) | |
| Age | 20–40 | 12 (28) | 8 (53.3) | 9 (52.9) | 25 (64.1) | 54 (47.4) |
| 41–60 | 23 (53.5) | 3 (20) | 6 (35.3) | 12 (30.8) | 44 (38.6) | |
| 60+ | 8 (18.6) | 4 (26.7) | 2 (11.8) | 2 (5.1) | 16 (14) | |
| Years of Experience | 6–10 | 8 (18.6) | 8 (53.3) | 7 (41.2) | 22 (56.4) | 45 (39.5) |
| 11–15 | 6 (14) | 3 (17.6) | 5 (12.8) | 14 (12.3) | ||
| 16–20 | 10 (23.3) | 4 (23.5) | 3 (7.7) | 17 (14.9) | ||
| 20+ | 19 (44.2) | 7 (46.7) | 3 (17.6) | 9 (23.1) | 38 (33.3) | |
| Knowledge | Poor | 2 (4.7) | 3 (20) | 4 (10.3) | 9 (7.9) | |
| Below Average | 10 (23.3) | 1 (6.7) | 3 (17.6) | 7 (17.9) | 21 (18.4) | |
| Average | 18 (41.9) | 8 (53.3) | 11 (64.7) | 23 (59) | 60 (52.6) | |
| Above Average | 9 (20.9) | 2 (13.3) | 3 (17.6) | 2 (5.1) | 16 (14) | |
| Excellent | 4 (9.3) | 1 (6.7) | 3 (7.7) | 8 (7) | ||
| Healthcare system equipped? | Yes | 11 (25.6) | 5 (33.3) | 5 (29.4) | 5 (12.8) | 26 (22.8) |
| No | 13 (30.2) | 3 (20) | 6 (35.3) | 13 (33.3) | 35 (30.7) | |
| Unsure | 19 (44.2) | 7 (46.7) | 6 (35.3) | 21 (53.8) | 53 (46.5) | |
Notes: *results are presented as frequency counts and corresponding percentages i.e., N (%).
It was observed that 34.2% of respondents had more than 20 years of work experience and 37.3% had less than 10 years of experience. About 71% of respondents declared average and above average levels of AI knowledge, while only 29% reported poor and below average levels. The level of AI knowledge among participants was not assessed by authors. Only a small proportion of respondents (12.8–29%) stated that the country's healthcare system is not adequately equipped to deal with future AI applications.
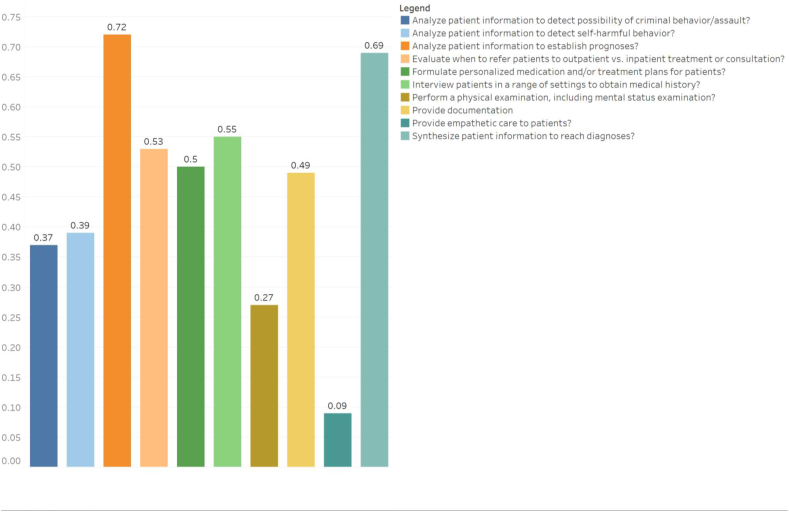
The respondents' opinions varied according to clinical specialty. In general, pathologists were more welcoming and accepting of the future use of technology compared to others; they had a significantly larger proportion of respondents answering ‘likely’ to the “Formulate personalized medication and/or treatment plans for patients” tasks (60%, p = 0.049), “Evaluate when to refer patients to outpatient versus inpatient treatment or consultation” (73.3%, p = 0.039), and “Interview patients in a range of settings to obtain medical history” (80%, p = 0.032). The respondents answered ‘likely’ in the other seven tasks at similar rates, such as “Analyze patient information to detect possibility of criminal behavior/assault” and “Synthesize patient information to reach diagnoses” (p = 0.836, see Table 2 & Fig. 1).
Table 2.
Mean of respondents with an answer of “Likely” to the question “What is the likelihood that AI will replace physicians in performing tasks as well as or better than the average physician?“ (N = 114).
| Task | Psychiatry |
Pathology |
Radiology |
Surgical Specialties |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 43) |
(n = 15) |
(n = 17) |
(n = 39) |
||||||||||
| Mean | SD | 95%CI [UL,LL] | Mean | SD | 95%CI [UL,LL] | Mean | SD | 95%CI [UL,LL] | Mean | SD | 95%CI [UL,LL] | *p-value | |
| Provide documentation (e.g., update medical records) about patients | 0.49 | 0.506 | [0.33,0.64] | 0.73 | 0.458 | [0.48,0.99] | 0.35 | 0.493 | [0.10,0.61] | 0.38 | 0.493 | [0.22,0.54] | 0.098 |
| Provide empathetic care to patients | 0.09 | 0.294 | [0.00,0.18] | 0.13 | 0.352 | [-0.06,0.33] | 0.06 | 0.243 | [-0.07,0.18] | 0.08 | 0.270 | [-0.01,0.16] | 0.892 |
| Formulate personalized medication and/or treatment plans for patients | 0.30 | 0.465 | [0.16,0.45] | 0.60 | 0.507 | [0.32,0.88] | 0.65 | 0.493 | [0.39,0.90] | 0.46 | 0.505 | [0.30,0.63] | 0.049* |
| Evaluate when to refer patients to outpatient vs. inpatient treatment or consultation | 0.33 | 0.474 | [0.18,0.47] | 0.73 | 0.458 | [0.48,0.99] | 0.53 | 0.514 | [0.26,0.79] | 0.51 | 0.506 | [0.35,0.68] | 0.039* |
| Analyze patient information to establish prognoses | 0.67 | 0.474 | [0.53,0.82] | 0.87 | 0.352 | [0.67,1.06] | 0.71 | 0.470 | [0.46,0.95] | 0.64 | 0.486 | [0.48,0.80] | 0.448 |
| Analyze patient information to detect possibility of criminal behavior/assault | 0.35 | 0.482 | [0.20,0.50] | 0.40 | 0.507 | [0.12,0.68] | 0.35 | 0.493 | [0.10,0.61] | 0.36 | 0.486 | [0.20,0.52] | 0.988 |
| Analyze patient information to detect self-harmful behavior | 0.44 | 0.502 | [0.29,0.60] | 0.53 | 0.516 | [0.25,0.82] | 0.35 | 0.493 | [0.10,0.61] | 0.23 | 0.427 | [0.09,0.37] | 0.116 |
| Synthesize patient information to reach diagnoses | 0.72 | 0.454 | [0.58,0.86] | 0.73 | 0.458 | [0.48,0.99] | 0.65 | 0.493 | [0.39,0.90] | 0.64 | 0.486 | [0.48,0.80] | 0.836 |
| Perform a physical examination, including mental status examination | 0.16 | 0.374 | [0.05,0.28] | 0.33 | 0.488 | [0.06,0.60] | 0.29 | 0.470 | [0.05,0.54] | 0.31 | 0.468 | [0.16,0.46] | 0.381 |
| Interview patients in a range of settings to obtain medical history | 0.51 | 0.506 | [0.36,0.67] | 0.8 | 0.414 | [0.57,1.03] | 0.29 | 0.470 | [0.05,0.54] | 0.59 | 0.498 | [0.43,0.75] | 0.032* |
Notes: *p-value is based on one-way analysis of variance (ANOVA).
Fig. 1.
Mean of respondents with an answer of “Likely” to the question “What is the likelihood that Al will replace physicians in performing tasks as well as or better than the average physician?” (Total sample, n = 114).
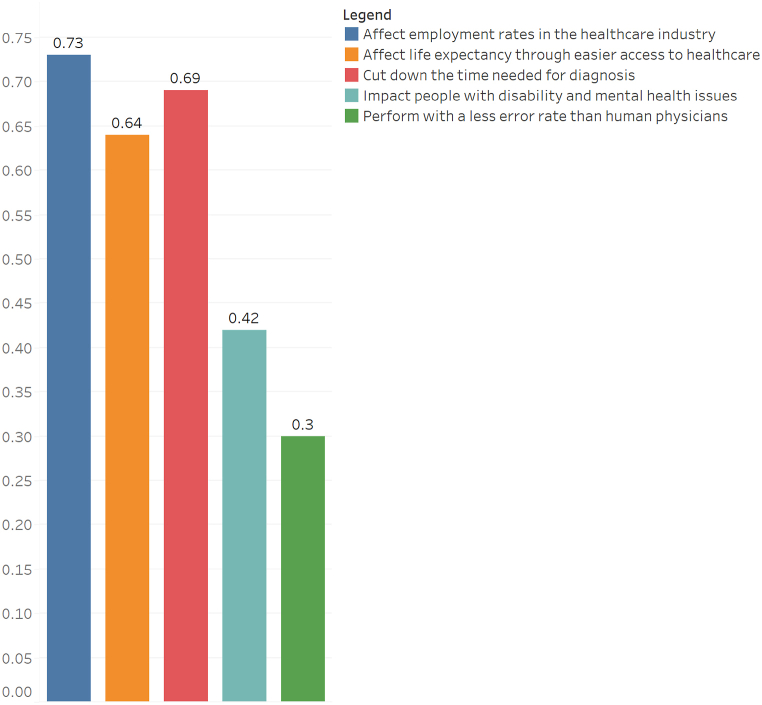
Regarding the benefits and drawbacks of AI, there was no statistically significant differences among the respondents (see Table 3 & Fig. 2). Most physicians agreed that AI would cut down the time needed for diagnosis – the mean response was 0.70(SD:0.465), 0.73(SD:0.458), 0.71(SD:0.470), and 0.62(SD:0.493), for psychiatry, pathology, radiology, and surgical specialties, respectively with no significant differences between them (p = 0.807). Similarly, the majority of respondents answered ‘likely’ to “Affect employment rates in the healthcare industry” – mean values 0.77(SD:0.427), 0.67(SD:0.488), 0.65(SD:0.493), and 0.82(SD:0.393) for psychiatrists, pathologists, radiologists, and surgical specialists, respectively (p = 0241). Around 27.19% of all respondents agreed to the statement that “AI will perform with a less error rate than human physicians,” with a mean value of 0.26(SD:0.441), 0.27(SD:0.458), 0.47(SD:0.514), and 0.21(SD:0.409) for psychiatrists, pathologists, radiologists, and surgical specialties, respectively (p = 0.241).
Table 3.
Mean of respondents with an answer of “Likely” to questions assessing some of the benefits and drawbacks of AI (N = 114).
| Task | Psychiatry |
Pathology |
Radiology |
Surgical Specialties |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 43) |
(n = 15) |
(n = 17) |
(n = 39) |
||||||||||
| Mean | SD | 95%CI [LL,UL] | Mean | SD | 95%CI [LL,UL] | Mean | SD | 95%CI [LL,UL] | Mean | SD | 95%CI [LL,UL] | *p-value | |
| Affect Life Expectancy | 0.66 | 0.480 | [0.51,0.81] | 0.8 | 0.414 | [0.57,1.03] | 0.65 | 0.493 | [0.39,0.90] | 0.46 | 0.505 | [0.30,0.63] | 0.113 |
| Cut down time needed for diagnosis | 0.70 | 0.465 | [0.55,0.84] | 0.73 | 0.458 | [0.48,0.99] | 0.71 | 0.470 | [0.46,0.95] | 0.62 | 0.493 | [0.46,0.78] | 0.807 |
| Positive impact on disabled people | 0.44 | 0.502 | [0.29,0.60] | 0.27 | 0.458 | [0.01,0.52] | 0.59 | 0.507 | [0.33,0.85] | 0.38 | 0.493 | [0.22,0.54] | 0.087 |
| Affect employment rates | 0.77 | 0.427 | [0.64,0.90] | 0.67 | 0.488 | [0.40,0.94] | 0.65 | 0.493 | [0.39,0.90] | 0.82 | 0.393 | [0.69,0.94] | 0.235 |
| Perform with a less error rate than human physicians | 0.26 | 0.441 | [0.12,0.39] | 0.27 | 0.458 | [0.01,0.52] | 0.47 | 0.514 | [0.21,0.74] | 0.21 | 0.409 | [0.07,0.34] | 0.241 |
Notes: *p-value is based on one-way analysis of variance (ANOVA).
Fig. 2.
Mean of respondents with an answer of “Likely” to questions assessing some of the benefits and drawbacks of Al. (Total sample, n = 114).
Lastly, none of these findings were related to respondents’ age, gender, years of experience, or AI knowledge level.
4. Discussion
This study measured the knowledge and attitudes of physicians from different specialties towards future AI applications. The results suggest generally positive attitudes, which is consistent with studies conducted in developed countries [[6], [7], [8]]. These positive attitudes were not related to the respondents’ age, gender, years of experience, or knowledge of AI. These findings were anticipated, given the extensive use of technology by the Bahraini population and the high rate of internet penetration (99%, compared to 92% in the United States in 2022, for instance) [20]. Another possible explanation is that most respondents belonged to a younger age group (30–50 years). The attitudes towards the use of AI in clinical tasks and its benefits and drawbacks were comparable between specialties, except for pathologists, who were more positive about the future use of AI. The application of AI in pathology may be foreseen as essential by pathologists in particular, and can be introduced rapidly provided adequate input from different stakeholders.
Notably, the respondents exhibited a strong consensus on certain issues, such as the threat to future employment rates posed by AI. This particular finding is consistent with previous global studies [6,8]. However, contrary to expectations, this finding did not align with studies conducted in the Arab world [[14], [15], [16], [17]]. Furthermore, with regards to AI performing as well as or better than the average physician in providing empathetic care, the participants in this study concurred with physicians worldwide [6,12,18]. Otherwise, the opinions of physicians in the current study align with those of physicians in a previous study involving 971 psychiatrists from 22 countries [6]. In that study, psychiatrists were more positive about the use of AI in the “Synthesize patient information to reach diagnoses,” “Analyze patient information to establish prognoses,” “Analyze patient information to detect self-harmful behavior,” and “Interview patients in a range of settings to obtain medical history” tasks than international averages. However, they had less positive attitudes towards the “Provide documentation,” “Formulate personalized medication and/or treatment plans for patients,” and “Perform a physical examination, including mental status examination” tasks [6]. Few studies have reported dissimilar findings. In a recent study conducted in Malaysia, almost half of the participants were tech-savvy physicians, and 60% (as opposed to 30% in this study) believed that AI would have lower error rates than physicians [13]. It is worth mentioning that the Malaysian study involved physicians at a single center, while this study included physicians from two out of three major hospitals in Bahrain, thus obtaining a more representative sample of the target population. This study contributes to the literature on the knowledge of and attitudes towards AI among different physicians in the Arab world and provides a wide representation of registered physicians, especially psychiatrists and pathologists. However, certain limitations should be acknowledged. The numbers of radiologists and surgical specialists participating in the study may not be fully representative of these specialties in the country. Also, knowledge of AI was self-reported, and no attempt was made to assess it objectively.
Artificial Intelligence (AI) is becoming an increasingly important tool in medicine, offering promising solutions to many healthcare challenges. AI is the ability of computers to understand and learn from data to accurately simulate and mimic human decisions and tasks. In medicine, AI can be used to make predictions, diagnose health conditions and suggest treatments. It can also be used to streamline the vast amount of information in medical records and to develop more targeted drugs, helping to reduce the cost of treatments and achieve better outcomes for patients.
5. Conclusion
This is one of the few studies in the region that investigates the attitudes and knowledge of practicing physicians towards the future use of AI. The responding physicians were generally welcoming to the use of AI in the field of medicine, which was comparable to global averages. Notably, pathologists were more open to the use of AI in their daily work compared to other specialties. The majority agreed that the health system is not fully equipped to deal with AI and were concerned about the effect of AI on their job security and the inability of AI to replace human skills in providing empathetic care. These findings must be presented to individual participant groups to further analyze the reasons behind the demonstrated attitudes and concerns.
Author contributions statement
1 - Conceived and designed the experiments (MKA, AMA, AHD, HAJ);
2 - Performed the experiments (MKA, AMA, AHD, TAQ);
3 - Analyzed and interpreted the data (MKA, AMA, HAJ);
4 - Contributed reagents, materials, analysis tools or data (MKA, AMA, AHD, TAQ, HAJ);
5 - Wrote the paper (MKA, AMA, AHD, TAQ, HAJ).
Financial support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.McCarthy J. 2007. What Is Artificial Intelligence. [Google Scholar]
- 2.Hamet P., Tremblay J. Artificial intelligence in medicine. Metabolism. 2017;69:S36–S40. doi: 10.1016/j.metabol.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 3.Cornet G. Robot companions and ethics: a pragmatic approach of ethical design. J. Int. Bioethique. 2013;24(4):49–58. doi: 10.3917/jib.243.0049. [DOI] [PubMed] [Google Scholar]
- 4.Krittanawong C. The rise of artificial intelligence and the uncertain future for physicians. Eur. J. Intern. Med. 2018;48:e13–e14. doi: 10.1016/j.ejim.2017.06.017. [DOI] [PubMed] [Google Scholar]
- 5.Verghese A., Shah N.H., Harrington R.A. What this computer needs is a physician: humanism and artificial intelligence. JAMA. 2018;319(1):19–20. doi: 10.1001/jama.2017.19198. [DOI] [PubMed] [Google Scholar]
- 6.Doraiswamy P.M., Blease C., Bodner K. Artificial intelligence and the future of psychiatry: insights from a global physician survey. Artif. Intell. Med. 2020;102 doi: 10.1016/j.artmed.2019.101753. [DOI] [PubMed] [Google Scholar]
- 7.Coppola F., Faggioni L., Regge D., Giovagnoni A., Golfieri R., Bibbolino C., et al. Artificial intelligence: radiologists' expectations and opinions gleaned from a nationwide online survey. La Radiologia Medica. 2021;126(1):63–71. doi: 10.1007/s11547-020-01205-y. [DOI] [PubMed] [Google Scholar]
- 8.Sarwar S., Dent A., Faust K., Richer M., Djuric U., Van Ommeren R., et al. Physician perspectives on integration of artificial intelligence into diagnostic pathology. NPJ Digit. Med. 2019;2(1):1–7. doi: 10.1038/s41746-019-0106-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Staartjes V.E., Volokitin A., Regli L., Konukoglu E., Serra C. Machine vision for real-time intraoperative anatomic guidance: a proof-of-concept study in endoscopic pituitary surgery. Operat. Neurosurg. 2021;21(4):242–247. doi: 10.1093/ons/opab187. [DOI] [PubMed] [Google Scholar]
- 10.Maassen O., Fritsch S., Palm J., Deffge S., Kunze J., Marx G., et al. Future medical artificial intelligence application requirements and expectations of physicians in German university hospitals: web-based survey. J. Med. Internet Res. 2021;23(3) doi: 10.2196/26646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lennartz S., Dratsch T., Zopfs D., Persigehl T., Maintz D., Hokamp N.G., et al. Use and control of artificial intelligence in patients across the medical workflow: single-center questionnaire study of patient perspectives. J. Med. Internet Res. 2021;23(2) doi: 10.2196/24221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blease C., Kaptchuk T.J., Bernstein M.H., Mandl K.D., Halamka J.D., DesRoches C.M. Artificial intelligence and the future of primary care: exploratory qualitative study of UK general practitioners' views. J. Med. Internet Res. 2019;21(3) doi: 10.2196/12802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Selamat E.M., Sobri H.N.M., Hanan M.F.M., Abas M.I., Ishak M.F.M., Azit N.A., et al. Physicians' attitude towards artificial intelligence in medicine, their expectations and concerns: an online mobile survey. Malays. J. Publ. Health Med. 2021;21(1):181–189. [Google Scholar]
- 14.AlZaabi A., AlMaskari S., AalAbdulsalam A. Are physicians and medical students ready for artificial intelligence applications in healthcare? Digit. Health. 2023;9 doi: 10.1177/20552076231152167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abuzaid M.M., Elshami W., Tekin H., Issa B. Assessment of the willingness of radiologists and radiographers to accept the integration of artificial intelligence into radiology practice. Acad. Radiol. 2022;29(1):87–94. doi: 10.1016/j.acra.2020.09.014. [DOI] [PubMed] [Google Scholar]
- 16.Qurashi A.A., Alanazi R.K., Alhazmi Y.M., Almohammadi A.S., Alsharif W.M., Alshamrani K.M. Saudi radiology personnel's perceptions of artificial intelligence implementation: a cross-sectional study. J. Multidiscip. Healthc. 2021:3225–3231. doi: 10.2147/JMDH.S340786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swed S., Alibrahim H., Elkalagi N.K.H., Nasif M.N., Rais M.A., Nashwan A.J., et al. Knowledge, attitude, and practice of artificial intelligence among doctors and medical students in Syria: a cross-sectional online survey. Front. Artif. Intell. 2022;5 doi: 10.3389/frai.2022.1011524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abdullah R., Fakieh B. Health care employees' perceptions of the use of artificial intelligence applications: survey study. J. Med. Internet Res. 2020;22(5) doi: 10.2196/17620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haji E.A., Ebrahim A.H., Fardan H., Jahrami H. Reporting inpatients' experiences and satisfaction in a national psychiatric facility: a study based on the random forest algorithm. J. Patient Exp. 2022;9 doi: 10.1177/23743735211069819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kemp S. DataReportal. DataReportal – Global Digital Insights; 2022. Digital 2022: Bahrain - DataReportal – Global Digital Insights.https://datareportal.com/reports/digital-2022-bahrain [Internet] Available from: [Google Scholar]