Abstract
We examine the relationship between contemporaneous fine particulate matter exposure and COVID-19 morbidity and mortality using an instrumental variable approach. Harnessing daily changes in county-level wind direction, we show that arguably exogenous fluctuations in local air quality impact the incidence of confirmed COVID-19 cases and deaths. We find that a one g/m increase in PM 2.5, or 15% of the average PM 2.5 concentration in a county, increases the number of same-day confirmed cases by 1.8% from the mean case incidence in a county. A one g/m increase in PM 2.5 increases the same-day death rate by just over 4% from the mean. These effects tend to increase in magnitude over longer time horizons and are robust to a host of sensitivity tests. When analyzing potential mechanisms, we also demonstrate that an additional unit of PM 2.5 increases COVID-19-related hospitalizations by 0.8% and use of intensive care units by 0.5% on the same day. Using individual case records, we also show that higher PM 2.5 exposure at the time of case confirmation increases risk of later mechanical ventilation and mortality. These results suggest that air pollution plays an important role in mediating the severity of respiratory syndromes such as COVID-19.
Keywords: Pollution, Air quality, PM 2.5, COVID-19, Health, Mortality
1. Introduction
The 2019 novel Coronavirus has claimed millions of lives globally. The total number of confirmed Coronavirus cases is in the order of hundreds of millions. The global economy suffered substantially as well. Policymakers around the world faced difficult trade-offs between public health and economic performance, especially in the early phase of the pandemic, as many policies to curb the spread of the disease entailed important consequences for the economy. We consider one element of this trade-off: contemporaneous air pollution exposure, with a specific focus on fine particulate matter. Fine particulate matter, or PM 2.5, refers to airborne particles with diameter of 2.5 m or less. When inhaled, these particles can travel deep into the respiratory system and have been linked to a wide range of adverse health outcomes (Currie et al., 2014). While PM 2.5 was associated with COVID-19 outcomes very early in the pandemic’s development (see Wu et al., 2020), to the best of our knowledge very little action has been taken to address contemporaneous air pollution exposure in possibly helping to alleviate severe COVID-19 illnesses, with the exception perhaps of stringent traffic restrictions in China during the early phases of the pandemic, as described further in Chen et al. (2020a). One potential explanation is the wealth of correlational findings and relative dearth of causal evidence, especially at the outset of the pandemic (see Cox and Popken, 2020 for a discussion).
Hence, this paper aims to contribute to our understanding of the contemporaneous effects of air pollution on respiratory illnesses, with the goal of informing policy in response to respiratory-related pandemics. To this end, we use plausibly random daily changes in wind direction over the period from January 22 to August 15, 2020, to predict local fine particulate matter concentrations, providing quasi-experimental evidence of the effect of PM 2.5 exposure on COVID-19 outcomes. We leverage an established identification strategy that pre-dates the COVID-19 pandemic (Luechinger, 2014, Deryugina et al., 2019, Anderson, 2020). In our preferred high dimensional fixed effects specification with weather, local policy, and social distancing controls from Unacast cell phone data, we show that a one increase in PM 2.5 increases the same-day number of confirmed cases by 1.8% from the mean case incidence in a county, where confirmed cases are likely to be a measure for severe cases given that many individuals infected with COVID-19 do not show symptoms (Day, 2020, Gandhi et al., 2020, Persico and Johnson, 2021). In the three-day period following a perturbation in air quality, the relationship between fine particulate matter exposure and cases is over twice as large, at 0.35 additional cases per 100,000 individuals. Meanwhile, a one increase in PM 2.5 increases the same-day mortality rate by 4% from the mean, or between 0.009 and 0.012 additional deaths per 100,000 individuals in a county. Our study also finds that contemporaneous exposure to PM 2.5 increases COVID-19-related hospitalizations and the use of intensive care units, suggesting that air pollution increases the severity of illnesses. These results are in line with a growing literature in economics linking air pollution exposure with respiratory issues, and which stresses the immediacy of such a relationship (Ransom and Pope III, 1995, Beatty and Shimshack, 2011, Ward, 2015, Schlenker and Walker, 2016, Jans et al., 2018, Deryugina et al., 2019, Anderson, 2020; see also Currie et al., 2014 for a general review of the literature). Our findings are also consistent with the recent COVID-19-specific medical literature suggesting a role for air pollution in modulating COVID-19 illness severity. In particular, local air pollution, and especially PM 2.5, may contribute to the severity of an infectious disease such as COVID-19 by debilitating the cardiovascular and immune systems (Ackermann et al., 2020, Miyashita et al., 2020, Prunicki et al., 2021).
Our paper contributes to several strands of literature. To start, it complements research by two concurrent papers that also apply causal inference techniques to add to our understanding of the relationship between local air pollution and COVID-19 outcomes. Our paper, Persico and Johnson (2021), and Isphording and Pestel (2021) all conclude that contemporaneous exposure to local air pollution worsens COVID-19 outcomes. Our studies, however, have some distinct features. Our study’s application of the same identification strategy as Deryugina et al. (2019) to a wider range of COVID-19 outcomes is unique, including not just cases and deaths but also hospitalizations, intensive care unit use, ventilator use, viral tests, and positivity rates. For these analyses, we leverage both daily state-level records as well as restricted individual-level case surveillance information from the Centers for Disease Control and Prevention (CDC). We assess these COVID-19 outcomes in the context of the United States, the largest economy in the world and the nation with the most recorded COVID-19 cases and deaths over our sample period and overall. Persico and Johnson (2021) also study the context of the United States, but focus on increased pollution from industrial facilities reporting to the Toxic Release Inventory (TRI). TRI facilities emit a variety of harmful pollutants into air and other environmental media, including no less than 770 toxic substances that cause cancer or acute human health effects (see EPA, 2021 for a full list of TRI chemicals). Further, populations near TRI facilities may be more vulnerable to the effects of pollution than other communities, in part due to past exposure to TRI emissions. Hence, despite the rather widespread presence of TRI facilities in the United States, estimates in Persico and Johnson (2021) apply to different pollutants and underlying populations than our nationwide study. As such, Persico and Johnson (2021) tend to find a stronger relationship between pollution and COVID-19 outcomes than we do. In contrast, Isphording and Pestel (2021) apply an empirical approach that resembles ours, using plausibly exogenous changes in wind as an instrument for PM 10 as the main pollutant of interest. However, their focus is on Germany, a highly developed country like the United States, but one with possibly different institutional factors, public health policy during the COVID-19 pandemic, cultural preferences for compliance with regulation, and demand for environmental protection. In particular, case incidence per 100,000 individuals in Germany was less than one quarter the figure for the United States over our respective sample periods (1.7 compared to 7.9), and death incidence was similarly close to one half the US figure (0.09 to 0.2). Yet, we note with interest that our estimates are very well aligned with those in Isphording and Pestel (2021), potentially speaking to the external validity of our two studies.
These three studies, together, set the basis for what we hope may be an emerging literature applying causal inference techniques to examine the relationship between air pollution and COVID-19 outcomes and, along with Clay et al. (2018) and Graff Zivin and Neidell (2009), outcomes from viral infections at large. This strand of literature complements the epidemiological literature, generally correlational in nature, which is led by Wu et al. (2020). With respect to Wu et al. (2020) and the other epidemiological studies (such as Bhaskar et al., 2020, Wang et al., 2020a, Bourdrel et al., 2021), our approach is different in at least three dimensions. First, we use plausible exogenous variation to address potential endogeneity issues. Second, we focus on current exposure to particulate matter. The contemporaneous dimension is crucial during a pandemic because policymakers have the ability to influence contemporaneous pollution levels and individual avoidance behavior, but have no control over past exposure to air pollution. Third, we explore the underlying mechanisms linking pollution exposure to COVID-19 outcomes, such as analyses of hospitalizations, intensive care unit use, and mechanical ventilation.
Further, our study contributes to a growing literature showing detrimental effects of air pollution on a wide range of outcomes. For empirical reasons, such literature initially considered mostly early-life outcomes such as infant mortality (e.g., Chay and Greenstone, 2003, Chay et al., 2003, Currie and Neidell, 2005, Knittel et al., 2016) and birth weight (e.g., Currie and Walker, 2011), but it has expanded substantially over the last decade to adult outcomes such as emergency room visits, hospitalizations, and adult mortality (e.g. Schlenker and Walker, 2016, Jans et al., 2018, Deryugina et al., 2019, Simeonova et al., 2019), dementia (e.g., Bishop et al., 2018), contemporaneous and long-run education outcomes (e.g., Sanders, 2012, Ebenstein et al., 2016), and other measures of productivity (e.g., He et al., 2019). Our study is especially relevant to this body of work regarding adult mortality, adding additional evidence that COVID-19 cases, hospitalizations, use of intensive care units, and mortality respond to local air pollution. Further, it adds to the growing body of work illustrating the short-term effect of pollution on health outcomes, including the relationship between days of exposure to pollution and mortality (e.g., Arceo et al., 2016, Simeonova et al., 2019, Deryugina et al., 2019, Anderson, 2020). Overall, we contribute to the literature on pollution and health by showing that air pollution, and in particular PM 2.5, plays an important role in the management of deadly infectious diseases such as COVID-19, and that these effects emerge very rapidly.
Finally, our study contributes to an emerging literature on the economics of the COVID-19 pandemic, aimed at identifying the best policy responses to this emergency (see Brodeur et al., 2020 for a review). As such, our findings have important policy implications, which the paper discusses in detail. Such policy implications apply both to pandemic and non-pandemic times. From the contemporaneous relationship between PM 2.5 and COVID-19 morbidity and mortality, it follows that keeping pollution at low levels may have an immediate payoff in reducing severe cases and deaths during a pandemic. Policymakers have a wide range of short- and long-term policy levers available to reach this goal, as discussed in Section 6.
The remainder of the paper is organized as follows. Section 2 provides some information about the context of our study and the related literature. Section 3 describes our data. Section 4 introduces our empirical methods, highlighting how our identification strategy is designed to overcome endogeneity of pollution exposure and measurement error. Section 5 presents our primary results for confirmed cases and deaths. We also include an extensive battery of sensitivity tests, analysis of potential mechanisms, and discussion of heterogeneous treatment effects in Sections 5.3, 5.4, and 5.5. Section 6 illustrates our main policy implications. Section 7 concludes and suggests avenues for future research.
2. Background
In this section, we cover the context of the COVID-19 pandemic and then refer to the literature preceding the emergence of COVID-19 that relates air pollution and health, with a particular focus on respiratory illnesses and fatalities. The literature review provides the basis for the main relationship that we study in this paper and guides the analyses that we perform to shed more light on the mechanisms behind such relationship.
2.1. Epidemiological and medical context
The 2019 novel coronavirus emerged as a cluster of pneumonia-like infections in Wuhan, China. The earliest studies of the illness documented symptom presentation in a relatively limited set of hospitalized individuals (see, for example, Chen et al., 2020b). While the earliest studies necessarily focused on the most severe illnesses resulting in hospitalization, they nevertheless demonstrated a set of common symptoms as well as risk factors for mortality. The most common symptoms were fever, cough, and shortness of breath. More serious respiratory symptoms were observed in some patients, with Chen et al. (2020b) observing bilateral lung damage associated with pneumonia in 75% of patients, “ground-glass” opacities in computerized tomography (CT) scans of lung tissue in 14% of patients, and a collapsed lung in one patient. In another early study of 191 hospitalized patients, fever and cough were again identified as the most common symptoms, with respiratory failure and acute respiratory distress syndrome (ARDS) occurring in 98% and 93% of 54 non-surviving patients (Zhou et al., 2020). Non-surviving patients often exhibited rapid progression of lung lesions in CT scans, again emphasizing the prominence of lung damage in the progression of severe cases (Wang et al., 2021).
By May of 2020, a broader set of characteristics of severe illness were identified and validated through meta-analysis (Huang et al., 2020) or by aggregating case information across hundreds of hospitals in China. For example, Guan et al. (2020) confirmed prior findings that the most common symptoms among hospitalized patients were fever (88%), cough (67%), fatigue (38%), sputum production (34%), and shortness of breath (19%). The same study also summarized frequency of abnormal chest CT scans, with 86% of chest CTs showing some abnormality, including ground-glass opacity (56%) and patchy shadowing in both lungs (52%). In the US context, Vahey et al. (2021) found that a higher proportion of hospitalized individuals reported cough (83%), fatigue (90%), and shortness of breath (72%). In a meta-analysis of five studies with combined 5328 patients, Huang et al. (2020) showed that the clinical presentations most commonly associated with severe illness included shortness of breath, acute cardiac injury, acute respiratory distress syndrome, and acute kidney injury, demonstrating that multiple organ systems could be affected. A related meta-analysis also found that shortness of breath as well as hemoptysis (i.e., coughing up blood) was associated with more severe illness (He et al., 2021). Other research highlighted the co-morbidities or pre-existing characteristics most associated with severe disease progression such as hypertension, heart disease, diabetes, and chronic obstructive pulmonary disease (Lv and Lv, 2021, Khodeir et al., 2021). Despite the broader systemic impacts and vulnerabilities, lung injury remained a hallmark of severe cases and focal point of research, with studies such as Rendeiro et al. (2021) detailing acute COVID-19 lung injury at the cellular level in humans. Collectively, this literature provides strong evidence that COVID-19 affects the respiratory system and that respiratory distress is associated with severe illness and mortality.
Building on this early work, epidemiological studies documented a wider array of symptoms associated with COVID-19. In particular, these include loss of taste and smell in nearly 40% of patients (Hannum et al., 2022), a potentially lethal inflammatory response that aggravates acute respiratory distress syndrome known as a cytokine storm (Ragab et al., 2020), neurological symptoms such as brain fog, amnesia, and stroke (Tsai et al., 2021), as well as lingering symptoms of COVID-19 occurring in as many as 87% of patients, with such symptoms referred to as Post COVID-19 Syndrome or “long COVID” (Mahase, 2020). The most common symptoms of Post COVID-19 Syndrome are fatigue and cognitive impairment, which in a third of cases lasts over 12 weeks (Ceban et al., 2022). Research also shed more light on the clinical progression of the illness. For example, Wang et al. (2020b) show that the median incubation period from exposure to symptom onset was 7 days, with a typical range of 4–12 days, notably finding that onset of symptoms could take place up to two weeks after the initial infection. More recent meta-analysis has shown a shorter incubation period of 5 days for the original COVID-19 strain and increasingly shorter incubation periods for Delta and Omicron strains of 4.4 and 3.2 days, respectively (Wu et al., 2022). In addition, lung injury may occur before symptom onset and before hospitalization (Wang et al., 2021), although lung scarring or fibrosis was typically observed three weeks after the onset of symptoms (Polak et al., 2020). Meta-analyses also demonstrate that time in hospital can vary significantly across patients, with median hospital stay duration across 42 studies ranging from 5 to 29 days (Rees et al., 2020). Finally, in one study of New York City hospitalizations at the start of the pandemic, time from hospitalization to mortality was a median 9 days (interquartile range of 5–15 days), although mortality was observed up to 30 days after admission (Cummings et al., 2020). As for time from symptom onset to mortality, Lu and Reis (2021) leverage Google search data to show that COVID-19 symptom search spikes preceded mortality increases by 22 days on average. In general, studies show a wide range in timelines from symptom onset to hospitalization and from severe illness to mortality.
Overall, the epidemiological literature provides a strong basis for our investigation of the contemporaneous impacts of air pollution on COVID-19 morbidity and mortality. It also provides a justification for investigating health impacts up to two weeks after a pollution shock, in our case driven by changes in wind direction according to our identification strategy.
2.2. Relationship with local air pollution
A large literature has aimed at establishing the effect of local air pollution on human health, including potential impacts to human capital accumulation, productivity, violent and criminal behavior, as well as earnings (see Currie et al., 2014 for a review of the first decades of this literature and Aguilar-Gomez et al., 2022 for a more recent review focused on productivity and cognitive abilities).
Part of this literature focuses on contemporaneous impacts of local air pollution on respiratory conditions, which are especially relevant for our study on COVID-19 outcomes. Several studies establish a causal relationship between contemporaneous local air pollution and respiratory conditions, most likely starting with Ransom and Pope III (1995), who leverage the temporary closure of a steel mill in Utah to show that steel production increases hospital admissions related to respiratory conditions. Beatty and Shimshack (2011) focus on the particulate matter and toxic substances released by diesel-powered school buses, finding that a retrofit program to reduce bus emissions led to a large decline in bronchitis, asthma, and pneumonia incidence for both children and adults with chronic respiratory conditions. Ward (2015) analyzes the role of particulate matter in the Canadian province of Ontario in driving respiratory hospitalizations among children, making the case that particulate matter is mostly imported from the United States and thus exogenous to local conditions. Schlenker and Walker (2016) exploit the delays that East Coast airports may create to flights in California, which lead to increased taxiing and thus higher local air pollution in California, to identify a relationship between the pollution from taxiing and hospital visits due to asthma and other respiratory issues. Jans et al. (2018) exploit plausibly exogenous changes in local air pollution driven by thermal inversions to study the relationship between pollution and health care visits for Swedish children. The authors find a considerable impact of pollution on healthcare visits, as well as on parents’ work absences for care of sick children, disproportionately affecting low-income households that tend to have worse baseline health conditions. Deryugina et al. (2019), using the identification strategy that we borrow for our empirical approach, assess the impact of fine particulate matter on healthcare use, inpatient spending, and mortality from any medical reason in the United States using Medicare data. Deryugina et al. (2019) find important effects of fine particulate matter on all these outcomes, concluding that fine particulate matter causes substantial costs to society. Simeonova et al. (2019) assess the change in local air pollution, including particulate matter, following the implementation of the Stockholm congestion charge and find a decline in acute asthma attacks in young children. Anderson (2020) examines long-run exposure to particulate matter, exploiting plausibly exogenous variation in pollution levels along major highways around Los Angeles as driven by wind patterns. Anderson (2020) find that more time spent downwind of a major highway leads to considerably higher mortality. Collectively, these studies provide consistent evidence of a causal relationship between exposure to air pollution, and in particular particulate matter, and respiratory conditions.
A potential role for local air pollution in severe acute respiratory syndromes was first suggested years before the COVID-19 pandemic, following previous outbreaks such as SARS in 2002–2004 and MERS in 2012. For instance, Cui et al. (2003) compare SARS mortality across geographical areas of China and point to a correlation between polluted areas and higher mortality. A similar correlation is found over time in Beijing by Kan et al. (2005). However, to our knowledge, minimal causal evidence supported such a potential relationship before the emergence of literature on COVID-19, thus the importance of research on the causal relationship between local air pollution and COVID-19 outcomes. We note two potential exceptions, though. A recent study by Clay et al. (2018) uses coal-fired capacity for electricity generation as a proxy for local air pollution to investigate the link between the latter and mortality during the 1918 Spanish influenza pandemic. A related study by Graff Zivin et al. (2020) leverages changes in wind direction to assess the effect of PM 2.5 on influenza-related hospitalizations. They find an effect in the order of 35% extra hospitalizations attributable to the flu per standard deviation increase in the Air Quality Index (AQI). However, flu shots, whose effectiveness varies from season to season for largely random reasons, can considerably mitigate such relationship. Together, these studies and ours contribute to an emerging strand of literature causally assessing the impact of local air pollution on infectious diseases.
Regarding the potential mechanisms at play, local air pollution, and in particular PM 2.5, may make individuals more vulnerable to airborne diseases such as COVID-19 by affecting their cardiovascular and immune systems, thus potentially leading to a more problematic clinical course. The medical literature provides supporting evidence. Prunicki et al. (2021) show that local air pollution and PM 2.5 exposure lead to cardiovascular dysregulation, immune system alterations such as methylation of immunoregulatory genes, altered immune cell profiles, and increased blood pressure, which are all relevant to COVID-19 prognosis. Related evidence shows that smoking may increase the risk of respiratory infections, such as COVID-19, where (second-hand) smoke and pollution share similar properties in how they affect the human body (Guan et al., 2020, Smith et al., 2020). One meta-analysis of COVID-19 patients found that nearly one third of individuals with smoking history experienced progression to more severe conditions including death, while only 17% of non-smokers experienced the same (Patanavanich and Glantz, 2020). Based on findings from smoking, where increased angiotensin-converting enzyme 2 (ACE2) expression is found in lower airway cells in active smokers, Miyashita et al. (2020) hypothesize that the same mechanism may be at play for particulate matter. The interaction between ACE2 and the spike protein of the novel coronavirus is key to cell infection in the COVID-19 pandemic, as ACE2 represents the receptor for the novel coronavirus in human respiratory epithelial cells. As a result, ACE2 expression has been studied in vitro, with particulate matter collected along a heavily trafficked road in Central London. Miyashita et al. (2020) confirm that particulate matter leads to significantly higher ACE2 expression. A second channel may connect PM 2.5 and COVID-19 outcomes. Several studies suggest a potential relationship between increased presence of fine particulate matter in the air and the airborne transmission of COVID-19 via attachment to these particles (Setti et al., 2020, Zhang et al., 2020). However, little evidence exists in support of this second channel, despite the widespread attention that it has received by both the media and academic circles (Ishmatov, 2022), thus our limited coverage.
As mentioned in the introduction, our study is not the only one to identify a causal relationship between local air pollution and COVID-19 cases and deaths. Two concurrent studies, by Isphording and Pestel (2021) and Persico and Johnson (2021), also provide evidence similar to ours. Persico and Johnson (2021) exploit the temporary lifting of monitoring and compliance requirements at TRI facilities, which led to increased emissions of a variety of pollutants. Isphording and Pestel (2021) use an empirical approach based on regional wind direction that resembles our methods. However, the three studies differ in their focus and, as a result, may differ as well in the magnitude of the effects that they find. Persico and Johnson (2021), for example, find that counties with more TRI sites experienced 14% more deaths and 53% more cases after EPA rollback of enforcement rules. Given that this environmental deregulation only led to a 0.7 unit increase in PM 2.5 on average, these effects are much larger than our estimates. Since TRI sites release many hazardous air pollutants other than fine particulate matter, it seems reasonable that the magnitude of the estimates in Persico and Johnson (2021) would be larger than those that we observe, as anticipated in Section 1 and as described in detail in the following sections. Further, populations exposed to pollution from TRI sites may be more vulnerable for diverse reasons, including past exposure to the many harmful pollutants released at those sites. As for Isphording and Pestel (2021), they focus on a different country, Germany. While Germany and the United States share comparable levels of development, they differ in important dimensions related to the governmental approach to the COVID-19 pandemic, social norms and compliance with regulations, including related to COVID-19, as well as environmental preferences. Results in Isphording and Pestel (2021) are also not directly comparable to ours because their outcomes are disaggregated by age group, and the independent variable is PM 10 instead of PM 2.5. Despite the underlying differences, it is interesting to note that the estimated relationships are very similar in magnitude. For example, Isphording and Pestel (2021) find that a one-unit increase in PM 10 increases death incidence of females aged 60 and 79 by 0.01 per 100,000, which is almost identical to our population-level estimate, as described in detail in the following sections. For males aged 60 and 79, the figure in Isphording and Pestel (2021) is a larger 0.04 per 100,000, although again this figure is not directly comparable to our population-level effects. For cases, Isphording and Pestel (2021) find that an additional unit of PM 10 leads to between 0.2 and 0.45 more cases per 100,000 population depending on the age group considered, which is larger but roughly similar to our primary estimates despite the different case incidences observed in Germany and the United States. Effect sizes with respect to cases may be larger in Isphording and Pestel (2021) due to more accurate and standardized case reporting in Germany, in accordance with the country’s Infection Protection Act, as described in their paper. Alternatively, the use of PM 10 instead of PM 2.5 could account for slightly different effect sizes. Overall, the similarity of our results, which we find very reasonable given the common empirical approach, may also speak in favor of the external validity of our results and those of Isphording and Pestel (2021). Further, when incorporating individual case records from the Centers for Disease Control and Prevention (CDC), which have more accurate case detection dates as described in Section 3, our results are indeed even more similar to those of Isphording and Pestel (2021).
We can also compare our findings to the epidemiological literature, correlational in nature, which mostly relies on past exposure to PM 2.5 rather than contemporaneous exposure. While the epidemiological literature has expanded very quickly (see the reviews in Bhaskar et al., 2020, Wang et al., 2020a, Bourdrel et al., 2021), the main reference remains as mentioned the early study by Wu et al. (2020). The study provides correlational evidence of a relationship between past pollution exposure and COVID-19 outcomes, while cautioning against any causal interpretation of such findings. Wu et al. (2020) find that an additional unit of past fine particulate exposure is associated with an 8% increase in COVID-19 mortality, which is twice as large as our estimated contemporaneous relationship.
3. Data
This paper uses daily information on outcomes related to the COVID-19 pandemic, air quality, wind, weather, and social distancing behavior at the county level from January 22 to August 15, 2020. We also incorporate data on state and county policies adopted to curb the spread of the virus and individual mask-wearing behavior as measured by survey responses. Our sample is limited to the contiguous United States and counties with an EPA air quality monitoring station. In the following sections, we describe data sources and construction of the analytic panel. Supplemental sources of information are listed in Appendix B.
3.1. Measuring severity of the COVID-19 pandemic
In what follows, we present our COVID-19 outcomes. We first describe all relevant data sources. Second, we discuss standard cleaning procedures. We conclude with discussion of the main summary statistics.
We source daily COVID-19 mortality and caseload information from the 2019 Novel Coronavirus Data Repository by the Johns Hopkins University Center for Systems Science and Engineering (CSSE).2 The CSSE COVID-19 Data Repository was developed for researchers, public health authorities, and the general public to track the latest information on the COVID-19 outbreak from all available local sources. This online repository has arguably become the standard source of data for cases and deaths in the growing COVID-19 literature. The repository tracks cumulative county case and mortality figures posted on state and county health department websites since January 22, 2020. The underlying state and county health department websites are generally surveillance and tracking dashboards, updated daily, designed to apprise the public on the spread of COVID-19. Cases and death totals therefore reflect the most-timely information available from testing centers, care providers, and other institutions required to report to a local public health regulatory body. For each date in the sample, the cumulative COVID-19 information is pulled from the state website at 12:50 a.m. the morning after the recorded date. As such, the timestamp of these variables is the cumulative figure a state or county had posted on its website shortly after the end of any given day.3 Due to imperfect information on the lag between symptom onset and case or death reporting as well as the possibility of lagged clinical impacts from recent pollution exposure, we also assess the relationship between contemporaneous exposure to PM 2.5 and outcomes over 3-day, 7-day, 10-day, and 14-day periods.
Acknowledging that fluctuations in reported COVID-19 cases and deaths may arise through several distinct mechanisms, we also use daily information collected by the COVID-19 Tracking Project on hospitalizations, intensive care unit admissions, ventilator use, and viral tests administered.4 The Tracking Project data was developed by a crowd-sourced team of volunteers who manually entered, checked, and double-checked over 870 data elements from state public health websites each day between 5:30 p.m. and 7:00 p.m. Eastern Standard Time. There are two shortcomings of the COVID-19 Tracking Project data. First, unlike the data from the CSSE COVID-19 Data Repository, all variables in the Tracking Project are at the state level. Second, certain information, such as ventilator use or intensive care unit admission, is not reported in all states. We investigate the relationship between air pollution exposure and these outcomes over 3-day and 7-day time horizons.
In addition to the COVID-19 Tracking Project, we obtained the COVID-19 Case Surveillance Restricted Access Detailed Data published by the CDC.5 The surveillance data is patient-level case information collected by hospitals, healthcare providers, and laboratories and reported to state public health authorities. These public health authorities then submit standardized case reporting forms to the CDC via the National Notifiable Diseases Surveillance System (NNDSS).6 For each case, the surveillance data includes information about the patient such as demographic characteristics, county of residence, and presence of co-morbidities. It also indicates illness characteristics such as time of case detection and disease severity, which is documented in terms of both symptom presentation and clinical course through, for example, hospitalization and mortality. The CDC data present two limitations for our purposes. First, while the date of case onset is known, the data do not provide information on the timing of hospitalization, admission to intensive care unit, ventilator use, and mortality. Second, detailed patient-level information is available only when the healthcare practitioner or laboratory collected it as part of their testing and questionnaire protocol. As such, case reports frequently do not include complete information on demographics, symptoms, or clinical course. Variables relating to clinical course, in particular, are reported as unknown or are missing in a high proportion of cases. For example, 55% of mortality, 41% of hospitalization, 92% of mechanical ventilation, and 91% of ICU entry indicators are missing. Because these missing outcomes could represent cases that resulted in mortality or other severe outcomes, we do not assign zeros to these missing outcomes. The uncertainty in timing of these clinical outcomes, paired with the high frequency of missing information, led us not to use these data for our primary regressions, which instead rely on the Johns Hopkins and COVID-19 Tracking Project data.
We perform straightforward data cleaning procedures on these COVID-19 outcomes. First, we convert Johns Hopkins cumulative case and death figures into daily totals of new cases or deaths by subtracting the reported total on a given day by the reported total the prior day in the same county. Next, to ensure comparability across counties, we transform these count variables to incidence rates per 100,000 individuals.7 We also generate variables for the incidence of new cases and deaths per 100,000 population over 3-day, 7-day, 10-day, and 14-day periods following day . For data elements in the COVID-19 Tracking Project, we use raw variables for the number of individuals currently hospitalized, in an intensive care unit, or on a ventilator for a state. We also generate 3-day and 7-day totals of these variables, similar to our construction of case and death incidence variables over longer time horizons.8 We also use the COVID-19 Tracking Project’s preferred total tests variable, which reflects the daily state increase in viral tests. This measure does not count new antigen or antibody tests. We calculate the positivity rate as the increase in new positive viral tests divided by the increase in total tests at the state level.9 We also calculate the positivity rate over 3-day and 7-day periods by summing the positive tests and total tests over all days in the time horizon and computing the percent of tests that are positive from the totals.
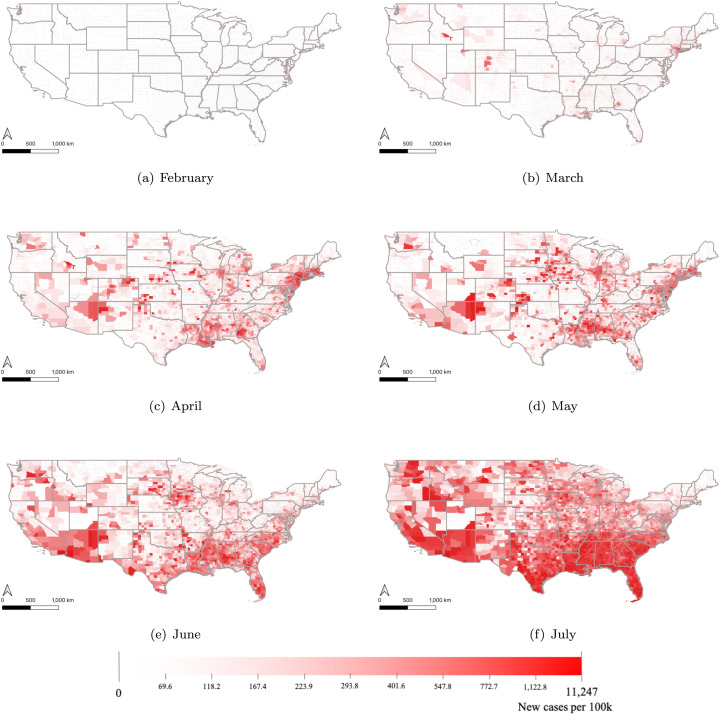
Summary statistics of the Johns Hopkins CSSE and COVID-19 Tracking Project are presented in the first and third panel of Table 1, while CDC case surveillance descriptive statistics are in Table 2. Descriptive statistics of additional patient-level characteristics are presented in Table C2. Fig. 1, Fig. 2 present the development of new cases or deaths across the United States over the sample period. The first of these figures represents the pattern of new confirmed cases over the course of the outbreak in our sample’s time frame, illustrating the late March and June waves of contagion in the United States. Fig. 2 represents the geographic spread of the disease in each month of the outbreak. In this figure, we depict the total monthly rate of new cases per 100,000 people at the county level from February (Fig. 2(a)) to July (Fig. 2(f)).10 Our data reflects the well-known pattern of contagion across the United States, with increasing cases in the Northeast by March and then a spread to new hot spots in the southern and western regions by June.
Table 1.
Summary statistics .
| Mean | S.E. | Min | Max | |
|---|---|---|---|---|
| County-level COVID-19 cases and deaths | ||||
| Daily case incidence per 100k people | 7.875 | 16.202 | 0.000 | 674.427 |
| Daily count of new cases | 39.771 | 153.047 | 0.000 | 7198.000 |
| Daily death incidence per 100k people | 0.216 | 0.871 | 0.000 | 62.826 |
| Daily count of new deaths | 1.314 | 9.780 | 0.000 | 1553.000 |
| County-level air pollution | ||||
| PM 2.5 | 6.640 | 4.231 | 0.000 | 116.967 |
| Weighted PM 2.5 | 6.169 | 4.172 | 0.000 | 87.700 |
| Air Quality Index | 27.007 | 14.710 | 0.000 | 182.667 |
| State-level COVID-19 outcomes | ||||
| Individuals hospitalized on day t | 1646.326 | 2486.516 | 1.000 | 18 825.000 |
| Individuals in ICU on day t | 639.858 | 835.736 | 1.000 | 5225.000 |
| Individuals on ventilators on day t | 207.997 | 283.617 | 0.000 | 2425.000 |
| New COVID-19 viral test results on day t | 14 745.724 | 23 740.560 | 0.000 | 187 926.000 |
| Test positivity rate on day t | 0.114 | 0.175 | 0.000 | 1.000 |
| Observations | 97,885 | |||
| Counties | 737 | |||
Reported statistics are at the county-day level. Note that only observations in the main specification are included.
Table 2.
CDC case surveillance data summary statistics .
| Mean | S.E. | Min | Max | Obs | |
|---|---|---|---|---|---|
| Cases reported with death of patient | 0.077 | 0.266 | 0.000 | 1.000 | 2,421,282 |
| Cases reported with hospitalization | 0.169 | 0.375 | 0.000 | 1.000 | 2,952,214 |
| Cases reported with mechanical ventilator | 0.044 | 0.206 | 0.000 | 1.000 | 442,456 |
| Cases reported with entry to ICU | 0.111 | 0.314 | 0.000 | 1.000 | 471,670 |
Reported statistics are at the individual level. Observations included are only those with non-missing clinical outcomes.
The total number of reported cases is 5,109,250.
Fig. 1.
New confirmed COVID-19 cases and deaths in the United States. Notes: Cases and deaths sourced from the Johns Hopkins COVID-19 Data Repository. Smoothed average calculated with seven lead and seven lag days.
Fig. 2.
New confirmed cases per 100,000 people by US county. Notes: Cases and deaths sourced from the Johns Hopkins COVID-19 Data Repository.
3.2. Air quality
We source air quality measurements from the EPA’s daily outdoor air quality information, AirNow.11 These air quality measurements include PM 2.5, PM 10, ozone, NO2, SO2, and the AQI. We focus our analysis on PM 2.5 because of the well-known and wide-ranging cardiovascular, lung-functioning, and mortality effects associated with exposure to this pollutant (EPA, 2019). While we also analyze health impacts of other pollutants in AirNow, such as ozone, unfortunately their sampling coverage is generally too limited to satisfy the identifying assumptions of our empirical specification, which was conceived for the analysis of PM 2.5. Hence, we can only control for ozone while addressing the issue represented by missing observations.
Fine particulate matter, or PM 2.5, is a complex mixture of particles with diameter of 2.5 m or less, such as nitrates, sulfates, ammonium, and carbon. PM 2.5 found in a given area can be either produced locally or transported from other areas. According to the EPA’s 2017 National Emissions Inventory, a comprehensive estimate of criteria air pollutant emissions, the primary sources of PM 2.5 in the United States include fires, agricultural dust, road-borne dust, construction dust, waste disposal, commercial cooking, fossil fuel combustion, and industrial processes.12 Fine particulate matter often serves as a proxy for air pollution more broadly, but unlike heavier pollutants, the small size of PM 2.5 makes it particularly suitable for an identification strategy relying on plausibly exogenous changes in wind direction as an instrument. Transported PM 2.5 is a large share of total PM 2.5 in a given region because, unlike some other hazardous air pollutants, PM 2.5 is often transported over long distances (Meng et al., 2020). Wind speed and direction can therefore greatly influence the source, concentration, and type of PM 2.5 exposure facing a given community, even over relatively short windows of time (Muller and Mendelsohn, 2007, Deryugina et al., 2019).
Air quality monitoring stations with PM 2.5 measurements from January to August 2020, and their density by county, are represented in Fig. 3. We aggregate air quality information to the county-day level. In counties with more than one monitoring station, air quality data is population weighted by the number of individuals in census blocks in a 10 km buffer around the air quality monitor. Following Deryugina et al. (2019), the EPA’s air quality monitors are classified into 100 clusters based on their location; these clusters are represented in Fig. 4.13 Summary statistics are presented in the second panel of Table 1. Fig. 5 maps the mean daily concentration in each month across United States counties. We also show the trend in nationwide fine particulate matter levels and air quality index over the course of the period of study in Fig. 6. While media portrayals suggested widespread decreases in air pollution during early phases of the COVID-19 pandemic, Fig. 6 shows relatively stable average PM 2.5 and AQI levels across all monitors. Because the largest sources of PM 2.5 are fires and dust, much of which is likely unrelated to lockdown practices, we find stable nationwide PM 2.5 levels to be plausible. Actually, Persico and Johnson (2021) find that counties with more TRI sites saw increased PM 2.5 levels during the early stages of the pandemic, partly resulting from COVID-related regulatory changes. Similar evidence is provided in Bekbulat et al. (2020), although we note that the experience of cities might have been different, as described in Berman and Ebisu (2020) and Zhang et al. (2021). We devote several analyses to the examination of heterogeneity within our sample for descriptive purposes in Section 5.5.
Fig. 3.
EPA air quality monitors. Notes: Each dot represents an EPA air quality monitor reporting PM 2.5 in 2020.
Fig. 4.
EPA air quality monitor clusters. Notes: Each color represents one of 100 air quality monitor clusters. These clusters are grouped according to the location of the air quality monitors by the k-means cluster algorithm following the strategy in Deryugina et al. (2019).
Fig. 5.
Fine particulate mean daily concentration by month and county. Notes: For each county, the value for each month is calculated by averaging the daily concentration of PM 2.5, weighted by the number of people in census blocks in a 10 km buffer around the air quality monitor.
Fig. 6.
Air quality during the pandemic. Notes: Figures plot average county-level fine particulate matter or air quality index on each date. County-level figures derived by averaging values over all monitors reporting on any given day.
3.3. Wind, temperature, and precipitation
We incorporate wind speed and direction information from the National Oceanic and Atmospheric Administration’s daily weather station data.14 Figure C1 presents the spatial distribution and density of the 2543 weather stations that record wind speed and direction in the contiguous United States from January to August, 2020.15 Given the importance of wind fluctuations for our identification strategy, it is worth describing how we construct wind direction and speed variables at the county-day level in further detail. First, we aggregate wind speed and direction to the station-day level. To this end, we compute the simple average of wind speed (measured in miles per hour) for each station for each day. Then, since wind direction is measured in degrees, we aggregate direction for each weather station to the daily level following the techniques laid out in Grange (2014).16 We next link wind information from the nearest four weather stations to each air quality monitor, again following the methods of Grange (2014), to compute an average wind direction measurement, where these directional components are further weighted by their distance from the air quality monitors in a county.17 Finally, wind direction is re-coded in the same way as Deryugina et al. (2019) such that the daily mean wind direction is grouped into four categories (1°–90°, 91°–180°, 181°–270°, and 271°–360°). Wind speed, reported in miles-per-hour, is re-coded into four dummy variables representing quartiles of the speed distribution.
We source precipitation and temperature information at the county-day level from the Parameter-elevation Regressions on Independent Slopes Model (PRISM) created by the PRISM Climate Group at Oregon State University.18 The PRISM Climate Group collects climatic data from many monitoring networks, cleans the data, and then estimates geospatially precise weather variables for each gridded cell across the United States.19 We average precipitation and temperature variables over all gridded cells within a county for each day. We then convert these variables into five indicators for each quantile of the daily minimum temperature, daily maximum temperature, and average precipitation distribution. By construction, these five quantile indicators reflect equal portions of the distributed temperature and precipitation variables from January to August of 2020. Summary statistics of the wind and weather variables are reported in Table C1.
3.4. Social distancing metrics
The data company Unacast creates social distancing records by county using cell phone information (Unacast, 2020).20 We use three relevant variables created by Unacast: change to average daily distance traveled from pre-COVID baseline, change to average daily visits to non-essential locations from pre-COVID baseline, and change to average daily encounters per square kilometer from baseline. Change to average distance traveled is a z-score difference in mean distance traveled for all cell phones in a county from the average traveled distance on the same weekday in a pre-COVID period (March 8, 2021 or earlier). The second indicator, change to average daily visits, controls for essential movements by distinguishing between essential and non-essential facilities.21 As with change to average distance traveled, changes to visits are reported as z-scores. Finally, the rate of encounters captures person-to-person contact. Since Unacast’s underlying cell phone data do not identify if two people have met, they define person-to-person contact as each time two users are within 50 m of each other for 60 min or less. This value is then normalized by the counties’ area (in square kilometers) and compared to a national baseline defined as the average encounters for a pre-outbreak period (February 10 to March 8, 2021).22 In all regression specifications, we use the average of all daily values from the previous 2-week period as control variables. Summary statistics are presented in Table C1.
3.5. Local COVID-19 policies and mask-wearing behavior
State and local policies responding to the pandemic likely played an important role in shaping viral transmission rates as well as health outcomes (see, for example, Courtemanche et al., 2020). We control for variation in local policies with information from two datasets. First, we use the COVID-19 Government Response Event Dataset (CoronaNet v1.0) via Safegraph to account for policy adoption of state governments (Cheng et al., 2020).23 Next, we use the COVID-19 State and County Policy Orders Dataset provided by the United States Department of Health and Human Services.24 This second source of local policy information includes all policies reported in three constituent databases. The first constituent data source is the COVID-19 US State Policy Database (Raifman et al., 2021). The second set of data elements consists of all stay at home orders available in WikiData. A final set of local policies in the COVID-19 State and County Policy Orders Dataset was curated specifically for this database by a dedicated team of Virtual Student Federal Service Interns. For each state, we create indicator variables equal to one if a state policy has started and has not yet ended. We perform the same with county-level policies, thereby generating a set of state and county policies at the daily level. We report summary statistics for the full list of policies in Table C1.25
Finally, to test sensitivity of our results to geographical and temporal differences in mask-wearing behavior, we use survey responses to the Understanding America Survey’s Understanding Coronavirus in America.26 Over our sample time horizon, this survey asked 7754 internet panel members detailed questions on their behavior with respect to the pandemic every other week, including on whether the survey respondent wore a mask. The survey responses are therefore at the individual survey-response level, where state of residence is the most detailed geographic information available per respondent. For each date in our sample, we collapse these survey responses to a simple average of the yes or no responses for a given state over the prior seven days. This information allows us to test whether, irrespective of local mask-wearing mandates and other policies, differential aversive behaviors may influence our results. Mask wearing reduces the spread of COVID-19 (Andrejko et al., 2022), but it could also protect from air pollutants, including particulate matter (Zhang and Mu, 2018)
4. Methods
Our objective is to estimate the causal relationship between short-term fine particulate matter exposure and COVID-19 morbidity and mortality, as well as potential channels leading to such morbidity and mortality. However, pollution exposure is not randomly geographically assigned, and so many confounding factors may correlate with pollution exposure and COVID-19 outbreak severity. Moreover, EPA-monitored air quality is an imperfect proxy for population exposure to pollution due to the non-random and sparse placement of monitors within and across counties (see Grainger and Schreiber, 2019). We therefore instrument for air pollution with local wind direction, following the methodology introduced in Deryugina et al. (2019). While pollution exposure may not be randomly assigned across communities, daily variation in wind direction within a county is plausibly random. The methods in Deryugina et al. (2019) further reduce measurement error by identifying PM 2.5 changes only from the regional impact of wind on PM 2.5. The regional effect of wind on PM 2.5 is constructed by clustering air quality monitors into 100 regional groups and employing air monitor cluster-specific wind direction instruments.27 By restricting the wind-induced impact on PM 2.5 to be the regional effect across clusters in many counties, the influence of any potentially-endogenous locally-generated fine particulate matter is minimized.28
We instrument for air pollution with local wind direction, with the aim of identifying the effect of acute exposure to air pollution on our outcomes of interest, by employing the following empirical specification. Let represent the average PM 2.5 concentration in county , state , week of the outbreak , and day . is the health outcome of interest; these outcomes include the daily incidence of confirmed COVID-19 cases per 100,000 population and the incidence of confirmed COVID-19 deaths per 100,000 population.29 We also explore the same case and death outcomes over 3-day, 7-day, 10-day, and 14-day periods to account for possible reporting lags and delayed disease progression. Consider the following two stage least squares regression equation:
| (1) |
In Eq. (1), represents three wind direction dummies indicating whether average wind direction falls into one of three 90° quadrants for county on day . The superscript on , as well as the same subscript on , refers to wind directions in the set {0°–90°, 91°–180°, 181°–270°}, where wind direction from angles 271°–360° is the omitted category. As in Deryugina et al. (2019), variable is an indicator function asserting that county belongs to air quality monitor group in the set of all air quality monitor clusters . Our excluded instruments are the full interaction of air quality monitoring clusters with wind direction dummies. Intuitively, the coefficients capture how wind direction influences PM 2.5 levels across a regional cluster of air quality monitors .30 Aside from the excluded instruments, Eq. (1) includes the term for a suite of time-varying controls for state and county COVID-19 mitigation policies, day of the week, five county-level dummies for wind speed quantiles, five county indicators for each minimum and maximum temperature quantile, five county indicators for each precipitation quantile, two lagged wind direction-by-monitor cluster interactions, and prior 2-week averages of Unacast social distancing metrics based on cell phone data. Unacast social distancing variables are the change in average distance traveled from county-level baseline, change in visits from baseline, and change in the rate of human encounters per square kilometer. We incorporate lagged 2-week averages for these variables to control for behavior over the relevant incubatory period of COVID-19.31 is a random error term clustered at the county level. The coefficient of interest in Eq. (1) is , an estimate of the relationship between an additional of PM 2.5 and case or death incidence from COVID-19. We note that is an estimate of the local average treatment effect of an additional unit of PM 2.5. Providing causal evidence based on local average treatment effects has implications for external validity. In particular, we infer from compliers, individuals whose COVID-19 status is affected by PM 2.5 and who would not have added to COVID-19 caseloads or deaths in a counterfactual scenario with lower PM 2.5. While never takers are unlikely, always takers represented by unhealthy individuals are plausible in the context of COVID-19. Section 5.4 expands our analysis to hospitalizations, use of intensive care units, and use of ventilators, which are more likely for vulnerable individuals. If the fraction of always takers was large for these outcome variables, one would expect the effect of PM 2.5 to be muted.
Eq. (1) incorporates high-dimensional county and state-by-week fixed effects, and .32 These fixed effects control for time-constant county heterogeneity and time-varying state characteristics.33 Due to the nature of the spread of a contagion, the state-by-week fixed effects are best suited for controlling for the evolving baseline infection rate in a local population, endogenous responses to the infection rate, and the ways in which underlying heterogeneity may interact with these dynamics. Intuitively, these fixed effects allow us to ask how better or worse air quality impacts the severity of the COVID-19 outbreak while taking a ceteris paribus approach with respect to local characteristics, infection rate, and behaviors. For the purpose of comparison, we also show results with metropolitan statistical area (MSA)-by-week or core-based statistical area (CBSA)-by-week fixed effects. CBSAs are groupings of counties anchored to one or more population centers of population greater than 10,000 individuals, whereas MSAs are groupings of counties around population centers with population greater than 50,000 individuals.34
In line with Deryugina et al. (2019), the identifying assumption is that, after flexibly controlling for the above-mentioned variables, county-level variation in daily wind direction is unrelated to variation in morbidity and mortality in the same county, if not through variation in primarily regionally-transported wind-dependent air pollution. Since we control for two lagged wind instruments within air monitor cluster, the instrument is moreover identified only from same-day changes from recent wind direction, which reduces the likelihood that wind direction in general may be jointly correlated with COVID-19 outcomes and PM 2.5 concentrations. Moreover, identification requires that our wind direction by monitor cluster instruments strongly predict local air pollution.35 Hence, this empirical approach provides quasi-experimental evidence of the effect of air pollution, instrumented by changes in wind direction, on health outcomes, while addressing common issues identified in the literature such as measurement error from various sources.
5. Results
In this section, we present estimates of the impact of PM 2.5 on a variety of COVID-19 outcomes, leveraging plausibly causal variation in air pollution as described in Section 4. This section is organized as follows. First, we show how this harmful form of air pollution affects COVID-19 case incidence and then death incidence at the county level. Next, we provide a battery of robustness tests and sensitivity analyses. Then, we explore the mechanisms underlying our case and death incidence results, showing that our findings primarily result from worsening of existing cases. Finally, we conduct heterogeneity analyses to provide suggestive evidence of the types of counties most impacted by pollution with respect to COVID-19.
5.1. COVID-19 cases
Contemporaneous exposure to air pollution may influence the severity of illness, thereby increasing the number of confirmed cases. Table 3 shows our primary results on confirmed cases across a range of fixed effects specifications. In columns (1) through (3), we show the relationship between PM 2.5 and case incidence per 100,000 individuals in a county across specifications with state-by-week, MSA-by-week, and CBSA-by-week fixed effects. In column (1), we find that an increase of one of fine particulate matter in a county increases the number of confirmed cases per 100,000 population by 0.15. This is a 2% increase from the mean case incidence per county on a given day. In columns (2) and (3), we show that this increase is similar when adopting MSA-by-week or CBSA-by-week fixed effects. We find similar yet larger effects on case incidence when using restricted CDC case surveillance data, as shown in the first three columns of Table 10. These results, which are likely more accurate with respect to timing of case confirmation, are between 0.24 and 0.27 per 100,000 population, or a 2.4 to 2.7% increase relative to mean case incidence per additional unit of PM 2.5. Our results on case incidence are comparable to those of Isphording and Pestel (2021), who find that one additional unit of fine particulate matter averaged over three-day periods increased COVID-19 case incidence in Germany by between 0.2 and 0.45 per 100,000 population depending on the age group considered.
Table 3.
Wind and PM 2.5 IV — Confirmed COVID-19 cases .
| (1) | (2) | (3) | |
|---|---|---|---|
| Weighted PM 2.5 | 0.146** | 0.128** | 0.133** |
| (0.0684) | (0.0647) | (0.0659) | |
| F Stat | 14.28 | 14.89 | 15.13 |
| Dep Var Mean | 7.875 | 7.882 | 7.882 |
| Pct change mean | 1.849 | 1.627 | 1.689 |
| Controls | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ||
| County and MSA-by-week FEs | ✓ | ||
| County and CBSA-by-week FEs | ✓ | ||
| Observations | 97,885 | 97,783 | 97,740 |
, , . Standard errors clustered at the county level in parentheses. Outcomes are daily case incidence per 100,000 population. Controls include state-level and county-level policy adoption, wind speed, minimum and maximum daily temperature, precipitation, prior two-week social distancing behavior, day-of-week, and two lagged wind direction-by-monitor cluster interactions. Displayed output of a two-stage least squares regression model with county and state-by-week, MSA-by-week, or CBSA-by-week fixed effects in which wind direction and air quality monitor cluster interactions are used to predict PM 2.5 levels in a county on a given day. F-statistics of the relevance test are computed assuming first-stage standard errors are not serially correlated.
Table 10.
County case and mortality incidence using CDC case surveillance records .
| Cases |
Deaths |
|||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Weighted PM 2.5 | 0.240*** | 0.272*** | 0.261*** | 0.00602 | 0.00721* | 0.00494 |
| (0.0906) | (0.0879) | (0.0905) | (0.00432) | (0.00425) | (0.00420) | |
| F Stat | 11.23 | 11.50 | 11.63 | 11.23 | 11.50 | 11.63 |
| Dep Var Mean | 9.880 | 9.893 | 9.895 | 0.305 | 0.305 | 0.305 |
| Pct change mean | 2.425 | 2.746 | 2.641 | 1.977 | 2.364 | 1.621 |
| Controls | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ✓ | ||||
| County and MSA-by-week FEs | ✓ | ✓ | ||||
| County and CBSA-by-week FEs | ✓ | ✓ | ||||
| Observations | 76,111 | 75,973 | 75,919 | 76,111 | 75,973 | 75,919 |
, , . Standard errors clustered at the county level in parentheses. Outcomes are daily case or mortality incidence per 100,000 population at the county-day level. Controls include state-level and county-level policy adoption, wind speed, minimum and maximum daily temperature, precipitation, prior two-week social distancing behavior, day-of-week, and two lagged wind direction-by-monitor cluster interactions. Displayed output of a two-stage least squares regression model with county and state-by-week, MSA-by-week, or CBSA-by-week fixed effects in which wind direction and air quality monitor cluster interactions are used to predict PM 2.5 levels in a county on a given day. F-statistics of the relevance test are computed assuming first-stage standard errors are not serially correlated.
We quantify the magnitude of these findings in three ways. First, these results imply that a 10% increase in PM 2.5 within a county would lead to 0.09 or 1.2% greater case incidence on the same day. Second, we compare our results to the relevant standard deviation of PM 2.5. The within-county standard deviation of average daily PM 2.5 over our sample period is 3.6 . Therefore, a wind-induced shift in PM 2.5 of one standard deviation would be expected to increase cases in any given county by at least 6.5% from the mean. Third, we estimate the approximate change over the support of wind-induced PM 2.5 shifts. We incorporate four wind-direction dummies. Within any county, the wind direction associated with lowest PM 2.5 levels has an average PM 2.5 level of 4.9 ; the second is 5.9, third is 6.9, and the highest wind direction is associated with mean PM 2.5 level of 7.9 . These categories illustrate that any given county has wide variation in PM 2.5 levels associated with wind direction, ranging an average of 3 from lowest to highest wind direction-pollution combination. Therefore, any given county would be expected to see at least 5.4% more confirmed cases on the worst wind-pollution combination days in comparison to the best ones, or at least a 1.8% increase in confirmed cases from even a slight step up in PM 2.5 associated with a marginal change in wind direction.
Estimates including the complete set of covariates are presented in columns (1) to (3) of Table C3. The point estimates for these covariates should only be interpreted as correlational, and so it is not surprising to see that many policies, such as county quarantine and mask-wearing mandates, are actually positively associated with case incidence. This pattern seems plausible if the timing of some state and local policy reflects a response to higher community infection rates. On the other hand, some measures such as statewide K-12 policies, creating an administrative task force, and regulating religious establishments are generally negatively associated with new case incidence. As for social distancing behavior, we find that traveling less distance away from home over the prior two-week period is strongly negatively associated with case incidence, while the rate of encounters over the past two weeks is positively associated with case incidence.
Further, we show how air pollution impacts the number of cases over the following 3, 7, 10, and 14 day periods in the first panel of Table 5. For concision, we show only specifications with county and state-by-week fixed effects.36 In column (1), we see our previous result that a one increase in PM 2.5 increases the case incidence by 0.15. Column (2) of the table suggests that a one unit increase in fine particulate matter in a given county is expected to increase the number of cases per 100,000 population by 0.35 over the following three-day period. While this effect in magnitude is over twice as large, it is a smaller percent increase relative to the mean 3-day combined case rate at 1.5%. Meanwhile, the same one unit increase would be expected to increase the case rate by 0.4 over a seven-day period, 0.65 over a ten-day period, and by 0.3 over a two-week period. It seems reasonable that the magnitude of the effects would increase over longer time horizons before plateauing, as a given exposure to pollution may lead the severity of cases to increase over several days, and testing or reporting lags may further delay the time of confirmation. Yet, our estimates also become noisier over longer time horizons.
Table 5.
Wind and PM 2.5 IV — Confirmed COVID-19 cases and deaths across 1, 3, 7, 10, and 14 day periods .
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Same-day | 3-day total | 7-day total | 10-day total | 14-day total | |
| Case incidence per 100,000 | |||||
| Weighted PM 2.5 | 0.146** | 0.351** | 0.393 | 0.656 | 0.316 |
| (0.0684) | (0.158) | (0.332) | (0.457) | (0.579) | |
| F Stat | 14.28 | 14.28 | 14.28 | 14.28 | 14.28 |
| Dep Var Mean | 7.875 | 23.787 | 56.541 | 81.911 | 116.792 |
| Pct change mean | 1.849 | 1.475 | 0.694 | 0.801 | 0.270 |
| Controls | ✓ | ✓ | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ✓ | ✓ | ✓ | ✓ |
| Observations | 97,885 | 97,885 | 97,885 | 97,885 | 97,885 |
| Death incidence per 100,000 | |||||
| Weighted PM 2.5 | 0.00918 | 0.00785 | 0.0307** | 0.0153 | 0.0141 |
| (0.00571) | (0.00874) | (0.0139) | (0.0168) | (0.0212) | |
| F Stat | 14.28 | 14.28 | 14.28 | 14.28 | 14.28 |
| Dep Var Mean | 0.216 | 0.649 | 1.537 | 2.218 | 3.150 |
| Pct change mean | 4.256 | 1.209 | 1.998 | 0.688 | 0.448 |
| Controls | ✓ | ✓ | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ✓ | ✓ | ✓ | ✓ |
| Observations | 97,885 | 97,885 | 97,885 | 97,885 | 97,885 |
, , . Standard errors clustered at the county level in parentheses. Controls include state-level and county-level policy adoption, wind speed, minimum and maximum daily temperature, precipitation, prior two-week social distancing behavior, day-of-week, and two lagged wind direction-by-monitor cluster interactions. Displayed output of a two-stage least squares regression model with county and state-by-week fixed effects in which wind direction and air quality monitor cluster interactions are used to predict PM 2.5 levels in a county on a given day. The outcomes in column (1) are same-day incidence of cases or deaths. Outcomes in column (2) are incidence of cases or deaths over the same day and the following two days. Outcomes in column (3) are deaths over the same day and the following nine days. Outcomes in column (4) are incidence of cases or deaths over the same day and the following thirteen days. All regressions use same-day predicted fine particulate matter as dependent variable. F-statistics of the relevance test are computed assuming first-stage standard errors are not serially correlated.
5.2. COVID-19 deaths
Table 4 displays point estimates for the relationship between levels of fine particulate matter and confirmed COVID-19 deaths. As in Table 3, columns (1) through (3) display results on death incidence per 100,000 individuals across our three primary fixed effects specifications. The point estimate in column (1) suggests that an additional unit of wind-induced PM 2.5 would raise the same-day death rate from COVID-19 by 0.009. This coefficient is slightly larger and more statistically precise when adopting MSA-by-week or CBSA-by-week fixed effects in place of the state-by-week fixed effects, as displayed in columns (2) and (3). These results suggest a 4%–6% increase from the mean daily death rate of 0.2 per 100,000 population in a county.37 These results are similar to those in Isphording and Pestel (2021), who find that an average increase of one additional unit of PM 10 over a three-day period would increase COVID-19 death incidence in Germany by 0.04 per 100,000 male individuals between 60 and 79, or by 0.01 for females of the same age group. This impact among patients aged 60–79 is not directly comparable to our population-level estimates, although we note that it is nevertheless very similar to the impacts we observe, especially for female patients of this demographic group. To provide additional context for the magnitude of our estimates with respect to wind, our estimates suggest that a 10% increase in mean PM 2.5 on a given day would increase mortality incidence from COVID-19 by 0.006–0.007 per 100,000 population in a county depending on the fixed effects specification, or at minimum a 2.7% increase from the mean daily incidence. Similarly, a one standard deviation increase in PM 2.5, or a within-county shift of 4.2 , would lead to an increase in 0.04 deaths per 100,000 population, a nearly 15% increase from the mean death incidence. Lastly, another way to interpret our results would suggest that wind shifting within a county from the dirtiest to the cleanest direction would lead to 13% more deaths, or 0.03 individuals per 100,000 population.
Table 4.
Wind and PM 2.5 IV — Confirmed COVID-19 deaths .
| (1) | (2) | (3) | |
|---|---|---|---|
| Weighted PM 2.5 | 0.00918 | 0.0122** | 0.0103* |
| (0.00571) | (0.00600) | (0.00600) | |
| F Stat | 14.28 | 14.89 | 15.13 |
| Dep Var Mean | 0.216 | 0.216 | 0.216 |
| Pct change mean | 4.256 | 5.646 | 4.785 |
| Controls | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ||
| County and MSA-by-week FEs | ✓ | ||
| County and CBSA-by-week FEs | ✓ | ||
| Observations | 97,885 | 97,783 | 97,740 |
, , . Standard errors clustered at the county level in parentheses. Outcomes are daily death incidence per 100,000 population. Controls include state-level and county-level policy adoption, wind speed, minimum and maximum daily temperature, precipitation, prior two-week social distancing behavior, day-of-week, and two lagged wind direction-by-monitor cluster interactions. Displayed output of a two-stage least squares regression model with county and state-by-week, MSA-by-week, or CBSA-by-week fixed effects in which wind direction and air quality monitor cluster interactions are used to predict PM 2.5 levels in a county on a given day. F-statistics of the relevance test are computed assuming first-stage standard errors are not serially correlated.
We perform the same regression on mortality incidence derived from the restricted CDC case surveillance data in Table 10. While these data have accurate dates of case confirmation, they do not include information on the timing of mortality. Hence, we simply assign each mortality event to the date of case confirmation. As we might expect, these results are attenuated in comparison to estimates using Johns Hopkins data. In particular, columns (4) through (6) demonstrate that a one unit increase in PM 2.5 on the day of case confirmation increases the later mortality incidence associated with these cases by 0.004 to 0.007, a 1.6–2.3% increase from the mean. These are half as large as our primary estimates for which timing of mortality is known. We take this as evidence that air pollution exposure impacts case severity and case progression to mortality after initial infection and case confirmation. We return to this discussion in Section 5.4.
Finally, consistent with Deryugina et al. (2019), we examine the relationship between exposure to an additional unit of PM 2.5 and COVID-19 deaths over longer time horizons. The corresponding estimates are provided in Table 5. For death incidence, we show that the relationship remains roughly constant at 0.008 over a 3-day period. Over a 7-day period, we observe that an additional unit of PM 2.5 increases death incidence by 0.03 per 100,000 population, which is three times the magnitude of the same-day effect but only a 2% percent increase relative to the 7-day mean death incidence. We observe noisier relationships between exposure to PM 2.5 and death incidence over 10- and 14-day periods, with a magnitude slightly larger but roughly consistent with the same-day impact. To provide some context for these magnitudes, our results suggest that a county would have 6% fewer deaths if wind came from the least-polluted direction for one week, in comparison to itself if wind came from the most-polluted direction for the same period of time.
5.3. Robustness tests
We assess the sensitivity of our results to a battery of robustness tests. We proceed as follows. First, we incorporate different combinations of time-varying daily controls. In particular, we confirm our results when controlling for local infection severity. We also test the sensitivity of our results to differential self-reported mask-wearing behavior. Next, we re-estimate our main model with controls for ozone concentrations as in Isphording and Pestel (2021). Further, we explore alternative specifications relying on inverse hyperbolic sine-transformed case and death outcomes or using ordinary least squares. We also exclude various localities with possibly unique characteristics. We then re-examine our methods for assigning wind direction to the local level and incorporating weather controls. Finally, we test how reporting inconsistencies may impact our results by dropping each day of the week from our regression sample one at a time.
Inclusion of different time-varying controls:
Our primary regressions control for local policies to control the spread of COVID-19, wind speed, daily precipitation, daily minimum and maximum temperature, past two-week average social distancing information, day of the week, and two days of lagged wind-direction combinations. In Table 6, we determine whether our primary results differ when subsets of controls are employed.
Table 6.
Wind and PM 2.5 IV — Model sensitivity to included controls .
| Cases |
Deaths |
|||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| Weighted PM 2.5 | 0.0870* | 0.125** | 0.135** | 0.133* | 0.0112*** | 0.0121*** | 0.0119*** | 0.00919 |
| (0.0473) | (0.0624) | (0.0627) | (0.0680) | (0.00362) | (0.00439) | (0.00448) | (0.00562) | |
| F Stat | 22.00 | 15.43 | 15.32 | 14.38 | 22.00 | 15.43 | 15.32 | 14.38 |
| Dep Var Mean | 6.321 | 6.320 | 6.320 | 7.875 | 0.169 | 0.169 | 0.169 | 0.216 |
| Pct change mean | 1.377 | 1.972 | 2.140 | 1.684 | 6.592 | 7.152 | 7.040 | 4.262 |
| County & State-by-week FEs | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Lagged instruments | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Day-of-week FEs | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Weather controls | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Policies controls | ✓ | ✓ | ||||||
| Social distancing controls | ✓ | ✓ | ||||||
| Observations | 128,314 | 128,247 | 128,247 | 97,885 | 128,314 | 128,247 | 128,247 | 97,885 |
, , . Standard errors clustered at the county level in parentheses. Displayed output of a two-stage least squares regression model with county and state-by-week fixed effects in which wind direction and air quality monitor cluster interactions are used to predict PM 2.5 levels in a county on a given day. All regressions include controls for day-of-week and two lagged wind direction-by-monitor cluster interactions. Baseline results with only these controls are depicted in columns (1) and (5). Columns (2) and (6) add weather controls for precipitation, minimum temperature, and maximum temperature. Columns (3) and (7) include weather controls and add controls for state and local policies. Columns (4) and (8) include weather controls as well as three controls for prior two-week social distancing behavior, although state and local policy controls are dropped. F-statistics of the relevance test are computed assuming first-stage standard errors are not serially correlated.
To start, we show results with only our primary fixed effects for county, state-by-week, day of the week, and lagged wind instruments in columns (1) and (5), hence dropping controls for weather, state and local policies, and social distancing behaviors. In this specification, we see a relationship between fine particulate matter and cases that is of smaller magnitude to our primary estimates for cases, at roughly 1.3% increase from the mean compared to 1.8%, although statistical precision is similar. For deaths, we see a relationship of larger magnitude and statistical precision at a 6.5% increase from the mean relative to 4.2% in our main specification. The difference in how these controls affect point estimates for cases and mortality could reflect the fact that some of these controls are more or less influential on cases than mortality. It is also possible that weather events are correlated with PM 2.5 and mortality, hence driving up the estimated relationship between PM 2.5 and mortality. These possibilities highlight the importance of controlling for these variables. In columns (2) and (6), we adjust the model to include daily precipitation and temperature controls. For cases and deaths, we observe, likely because of omitted variable bias being gradually addressed, larger point estimates of comparable statistical precision to the simple case presented in columns (1) and (5), suggesting that one unit of fine particulate matter in a county led to a 2% increase in daily case incidence and a 7% increase in daily death incidence. Adjusting the model to include local policies, in columns (3) and (7), leaves the magnitude of the point estimates and statistical precision largely unchanged for both cases and deaths. In these cases, again, we observe somewhat smaller point estimates for cases than our primary specification in Table 3, Table 4. Finally, in columns (4) and (8), we drop policy controls and add our past 2-week social distancing behavior controls. While this specification change does not particularly affect our point estimate on cases, it tends to decrease the magnitude and precision of our relationship between fine particulate exposure and death incidence. Still, in general, the results in Table 6 are roughly comparable to our primary estimates, with the magnitude for cases situated between an increase of 1.3%–2% and for deaths between 4%–7%. This evidence compounds that provided in Deryugina et al. (2019) on the validity of wind direction as an instrument for air pollution.
The results in Table 6 suggest attenuation with inclusion of prior two-week social distancing controls. We note that two-week average social distancing behavior may be correlated with pollution through two channels, avoidance behavior (Graff Zivin and Neidell, 2009, Neidell, 2009, Deschênes et al., 2017) and the fact that past social distancing behavior may imply less pollution. These factors may lead to the attenuation dynamics that we observe. We therefore further explore the sensitivity of our results to different formulations of social distancing controls in Table C6. In general, we observe point estimates of very similar magnitude when adopting different variations of these controls. Importantly, in column (1), we see point estimates of similar magnitude and even greater statistical precision for death incidence when dropping social distancing controls altogether. This analysis suggests that including social distancing controls in our empirical model leads to more conservative estimates.
Lastly, since case and death incidence from COVID-19 may be largely dependent on the accumulated local caseload over a recent period, we consider additional controls related to the local severity of the pandemic within a county in Table 7, as Persico and Johnson (2021) and Isphording and Pestel (2021) also do. In columns (1) and (4), we condition on the number of days since the first death in a county. In columns (2) and (5), we condition on the cumulative number of cases seven days prior. Similarly, columns (3) and (6) condition on cumulative number of cases fourteen days prior. Each regression uses county and state-by-week fixed effects and the standard controls of Table 3, Table 4. For each additional control, our point estimates on case incidence are slightly larger but vary by less than 0.003 in magnitude compared with our baseline estimations and remain the same in terms of statistical significance. The magnitude of the point estimates on death incidence also vary little with inclusion of these controls, by no more than 0.0004. However, inclusion of controls for accumulated cases in the weeks prior increases precision of point estimates on death incidence, which now reach statistical significance. Overall, the inclusion of these controls increases the magnitude and precision of our results, suggesting they may be an important factor to account for in the estimations. Hence, the results in Table 7 point to our baseline estimations as rather conservative.
Table 7.
Wind and PM 2.5 IV — Controlling for severity of the pandemic .
| Cases |
Deaths |
|||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Weighted PM 2.5 | 0.146** | 0.147** | 0.149** | 0.00917 | 0.00951* | 0.00957* |
| (0.0683) | (0.0683) | (0.0682) | (0.00571) | (0.00572) | (0.00573) | |
| F Stat | 14.28 | 14.27 | 14.27 | 14.28 | 14.28 | 14.28 |
| Dep Var Mean | 7.875 | 7.875 | 7.875 | 0.216 | 0.216 | 0.216 |
| Pct change mean | 1.854 | 1.867 | 1.886 | 4.251 | 4.407 | 4.437 |
| Controls | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Days since first death | ✓ | ✓ | ||||
| Cumulative cases 7 days prior | ✓ | ✓ | ||||
| Cumulative cases 14 days prior | ✓ | ✓ | ||||
| Observations | 97,885 | 97,885 | 97,885 | 97,885 | 97,885 | 97,885 |
, , . Standard errors clustered at the county level in parentheses. Controls include state-level and county-level policy adoption, wind speed, minimum and maximum daily temperature, precipitation, prior two-week social distancing behavior, day-of-week, and two lagged wind direction-by-monitor cluster interactions. All regressions include county and state-by-week fixed effects. Displayed output of sensitivity tests including three additional controls related to the county-level severity of the pandemic. Columns (1) and (4) include a control for the number of days since the first reported death in a given county. Columns (2) and (5) include a control for the cumulative number of cases or deaths, respectively, seven days prior to day of the case or death incidence outcome in the same county. Columns (3) and (6) include a control for the cumulative number of cases and deaths 14 days prior to the case or death outcome. F-statistics of the relevance test are computed assuming first-stage standard errors are not serially correlated.
Mask-wearing behavior:
We next test how the inclusion of survey measures of mask-wearing behavior affects our results. For this sensitivity analysis, we use survey responses to the Understanding Coronavirus in America questions in the Understanding America Study. Table C7 reports our primary results when including this variable as a control. The point estimates of interest are very similar in magnitude although somewhat less precise, which we take as evidence that differential masking behavior is not driving the relationship between pollution and COVID-19 severity. Rather, mask-wearing behavior may slightly attenuate the relationship between pollution and COVID-19 case severity by limiting transmission and in some cases also protecting from air pollution. We nevertheless note that these results should be interpreted with caution as mask-wearing behavior is not only self-reported, but also endogenous to pandemic severity, potentially leading to endogenous self-reporting as well. Indeed, the second row of results in Table C7 shows that recent mask-wearing behavior is strongly negatively correlated with case transmission, as we might expect, but it is positively associated with mortality. This positive association likely reflects that individuals are more likely to wear masks, or to report that they do, when mortality is high in the same state.
Controlling for ozone:
We use PM 2.5 as our primary independent variable to represent air pollution. The main rationale is that our empirical strategy, based on Deryugina et al. (2019), is very much geared towards capturing the causal effect of PM 2.5 on the outcomes of interest. Yet, a variety of pollutants contribute to air quality. Several pollutants tend to be correlated with PM 2.5, but their measurement is much sparser, leaving us with a much smaller sample size (that is the case for instance for NO2 and SO2). Further, measures such as the EPA’s Air Quality Index (AQI) tend to be highly dependent on variation in PM 2.5, so that estimates for PM 2.5 and AQI would tell a very similar story (as we report in Austin et al., 2020). However, as discussed in Isphording and Pestel (2021), one pollutant, ozone, stands out for its negative correlation with PM 2.5 (see Jia et al., 2017). Further, ozone may also be responsible for immediate, adverse health effects, in particular with respect to respiratory issues. As a result, in this section we test the robustness of our results to controlling for ozone.
As with PM 2.5, we construct ozone variables by population-density weighting pollution measures when more than one ozone monitor is present in a county. As mentioned, missing observations are an important issue for all pollutants other than PM 2.5, albeit slightly less so for ozone than it would be for instance for NO2 and SO2. Hence, we code our variable so as to isolate the effect of a missing observation through a random number. The results are presented in Table C8. All columns indicate that our main results for both cases and deaths are robust to the inclusion of ozone as a control variable. If anything, point estimates become slightly larger, suggesting that our main estimates are rather conservative. The coefficients for ozone, instead, do not point to any particular pattern in our sample.
Alternative empirical specifications:
Here, we present results for two alternative empirical specifications in Table 8. First, we demonstrate the robustness of our findings to applying an inverse hyperbolic sine transformation to case and death incidence variables in columns (1) and (3). A log transformation may help to eliminate skew in case or death incidence. We use the inverse hyperbolic sine transformation as opposed to a simple natural logarithm due to the presence of many zeros for cases and deaths in our data. The relationship between air pollution and hyperbolic-sine-transformed cases and deaths is statistically significant for both case and death incidence, although the point estimates are somewhat smaller. We find that a one unit increase in fine particulate matter increases case incidence by 1% and death incidence by 0.5% from the mean.38
Table 8.
Alternative specifications .
| Cases |
Deaths |
|||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Weighted PM 2.5 | 0.00968* | 0.0589** | 0.00468** | −0.000800 |
| (0.00495) | (0.0260) | (0.00211) | (0.000770) | |
| F Stat | 14.28 | 14.28 | ||
| Dep Var Mean | 1.675 | 7.875 | 0.152 | 0.216 |
| Pct change mean | 0.968 | 0.748 | 0.468 | −0.371 |
| Controls | ✓ | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ✓ | ✓ | ✓ |
| Inverse hyperbolic sine | ✓ | ✓ | ||
| Ordinary least squares | ✓ | ✓ | ||
| Observations | 97 885 | 97 885 | 97 885 | 97 885 |
, , . Standard errors clustered at the county level in parentheses. Controls include state-level and county-level policy adoption, wind speed, minimum and maximum daily temperature, precipitation, prior two-week social distancing behavior, day-of-week, and two lagged wind direction-by-monitor cluster interactions. All regressions include county and state-by-week fixed effects. Displayed output of alternative modeling specifications. Columns (1) and (3) apply the inverse hyperbolic sine transformation to the incidence of cases or deaths. Columns (2) and (4) present the results of an Ordinary Least Squares estimation procedure instead of the two-stage least squares model.
Next, we show reduced-form ordinary least squares (OLS) estimates of our relationship of interest. The previous literature has identified measurement error of pollution exposure as an important issue when analyzing the effect of air pollution on health outcomes, thus leading to the use of an instrumental variable approach (Luechinger, 2014, Deryugina et al., 2019, Anderson, 2020). The instrumental variable approach can also tackle other non-random sources of variation in pollution exposure, which may limit the extent to which naïve OLS estimations approximate causality. To shed light on the potential biases of a naïve regression, we display estimates obtained via OLS in columns (2) and (4) of Table 8. We estimate these relationships with county and state-by-week fixed effects as well as the same controls as in our baseline specifications. We find that an additional unit of PM 2.5 is statistically significantly associated with 0.06 increased cases per 100,000 population. This is a 0.7% increase relative to the mean daily case incidence in a county, which is slightly over one third the magnitude of our primary estimates for case incidence. In column (4), we show that a one unit increase in PM 2.5 is negatively associated with daily death incidence in a county, although the association is insignificant and the magnitude of the point estimate is a small 0.3% of the mean death incidence. We take the differences in magnitude or sign of these OLS point estimates as evidence confirming the conclusions in Luechinger (2014), Deryugina et al. (2019), and Anderson (2020) on the influence of measurement error and non-random pollution exposure in naïve regressions.
Excluding specific geographies:
We test how localities with unique characteristics or reporting practices may impact our primary estimates in Table C9. In columns (1) and (4), we show results without New York City, the location of the first major outbreak of COVID-19 in the United States. New York City may be considered an outlier in many respects, including population density, initial outbreak intensity, COVID-19 policy response, and pollution levels. We also drop counties in the multi-state Kansas City region in columns (2) and (5), as cases and deaths are reported for the entire city as opposed to by county in the CSSE COVID-19 Data Repository. Lastly, Utah reports COVID-19 outcomes by collections of counties (i.e., health districts), and so in columns (3) and (6) we show our primary results when dropping this state. These robustness checks mirror similar checks performed in Persico and Johnson (2021). In all models, we see effect sizes of similar if not greater magnitude and statistical precision. Removing New York City notably increases the magnitude and statistical precision of our point estimates for death incidence from 0.009 to 0.014 per 100,000 population. This represents an increase from 4% to 7%. Dropping Kansas City and Utah, conversely, barely changes the point estimates in magnitude and precision in comparison to our baseline model. From these results, we conclude that our findings are robust to the exclusion of geographies with unique characteristics or reporting practices. If anything, their inclusion may add some statistical noise to our estimates, pointing once more to the conservativeness of our baseline estimates.
Next, because the inclusion of New York City seems to affect the precision of our point estimates, we test our results when limiting the sample to counties in MSA regions in Table C10. Here we include the same controls as before and display estimates with county-by-week and MSA-by-week fixed effects. One might expect counties constituting MSA regions to have different COVID-19 transmission, policy adherence, aversion behavior, or other characteristics that might impact our relationships of interest. In all regressions limited to MSA regions, we see statistically insignificant point estimates related to fine particulate matter. The magnitude of the point estimate for cases is roughly two thirds as large as our primary estimates, at 0.9–0.1 cases per 100,000 instead of 0.15. For death incidence, we see noisy point estimates with positive and negative signs. These results may largely reflect the smaller sample size that is left when limiting to MSA regions. However, they may also be in part suggestive of a pattern by which more urban regions may have experienced differential impacts from pollution exposure with respect to COVID-19 in comparison to the rest of the country. We devote more attention to this heterogeneity of impacts in Section 5.5.
Alternative approaches to weather and wind:
Wind and weather information is of crucial importance to our identification strategy. We therefore test the sensitivity of our results to alternative methods of assigning wind directions as well as different configurations of weather controls. To start with wind direction, we assign wind direction variables to air quality monitors by inverse-distance weighting wind direction values of the four nearest weather stations, where the inverse distance weights are applied to directional wind vectors as described in Section 4. These monitor-specific wind direction measurements are similarly population-weighted to derive county-level measurements. We also present results under two alternative assignment mechanisms. First, we assign wind direction based on only the closest weather station with non-missing wind information on a given day. Next, we assign wind direction based on inverse-distance weighting wind direction values of the twelve nearest weather stations. We present our main empirical specifications with these alternate wind direction assignments in Table C11. When assigning wind direction based on only the closest weather station, in columns (1) and (4), point estimates for cases are slightly larger while our results for deaths are marginally smaller in magnitude in comparison to our baseline findings, which are presented in columns (2) and (5). Statistical precision is similar in either case. In columns (3) and (6), when taking the distance-weighted average of wind direction across the nearest 12 weather stations, we note similar results for cases but a somewhat attenuated point estimate with respect to deaths at 0.008 instead of 0.009. These results suggest that our estimates are similar across different methods of aggregating wind direction measurements to the county level.
Further, given the importance of weather conditions in potentially moderating the activity and infectivity of the COVID-19 virus (see Sarkodie and Owusu, 2020), we explore alternative combinations of weather controls in Table C12. Columns (1) and (3) reflect our base model with wind speed, temperature, and precipitation controls for day only. In columns (2) and (4), we include additional lagged weather variables representing day , , and . Evidently, conditioning on these lagged weather variables improves the magnitude and statistical precision of our point estimate for deaths, raising it from 0.009 to a statistically significant 0.01, or a jump from 4.2% relative to the mean to 4.8%. The point estimate for cases, meanwhile, is slightly smaller in magnitude but very similar to our baseline regressions. We take these results as suggesting that including more weather controls in our model would not attenuate our estimated relationship between fine particulate matter and COVID-19 outcomes and, if anything, would lead to larger estimates for death incidence.
Time horizons of reporting:
In Section 3, we note uncertainties related to the time stamp of case and death reporting. In general, the timestamp of cases and deaths reflects the date a state reported them on COVID-19 web-based dashboards. As such, our results may be influenced by inconsistent, lagged, and lumpy reporting by states and corresponding healthcare institutions. In particular, institutions may be less likely to report new data on holidays or weekends. To determine how inconsistent reporting across specific days of the week may influence our results, we drop each day of the week one at a time in Table C13. In columns (3) through (6), we observe that excluding week days that are less likely to have abnormal reporting typically leads to point estimates of lower magnitude and statistical precision for deaths. Results for cases are mostly lower as well with the exception of Thursday. These lower point estimates likely result from reducing the sample size and data signal without simultaneously improving accuracy of case and death timing assignment. Conversely, excluding days that are more likely to have abnormal reporting, such as the weekend and Monday, when recent weekend outcomes may be reported, results in point estimates that are generally larger and more statistically precise, as one might have expected. For example, dropping any day from Saturday to Monday results in statistically significant point estimates on death incidence in the range of 0.011 to 0.014, or a 5%–6% increase relative to the mean as opposed to our base estimates of 4.2%. Our point estimates for case incidence over the weekend are split, with much larger estimates than our baseline when dropping Saturday but a smaller estimate when dropping Sunday. While these patterns are not perfectly uniform, they generally suggest that lumpy or inaccurate timing issues may be an attenuation factor in our main findings. That is, while these issues may not substantively alter the overall interpretation of our results, they also point to our baseline estimates as rather conservative.
5.4. Mechanisms
In this section, we discuss the potential mechanisms driving the relationship between PM 2.5 and COVID-19 cases and mortality, building upon the literature covered in Section 2. We proceed in two ways. First, we adjust our empirical approach to accommodate COVID-19 Tracking Project data at the state-day level and test the relationship between PM 2.5 and hospitalizations, use of intensive care units, and use of ventilators, with the goal of determining the causal chain potentially leading from air pollution exposure to death from COVID-19. In related analyses, we consider viral testing counts and positivity rates as outcome variables. Second, we use the restricted CDC case surveillance data, as described in Section 3, to analyze mechanisms at the individual level, aggregating at the county level for case incidence in line with our main estimations and with an individual-level analysis for other outcomes. The goal of this second set of analyses is to complement the first approach and shed further light on the mechanisms behind our main relationship of interest. As mentioned in Section 3, while we possess information on the location of the individual records at the county level, one downside of this approach relates to how we observe timing. In particular, we do not observe the timing of hospitalization, admission to intensive care units, ventilator use, or mortality. We investigate how these eventual outcomes vary with air pollution on the day of case confirmation, and in separate analyses we also incorporate longer time horizons of pollution corresponding to the period after initial case confirmation. Yet, because the temporal match of our wind instrument is important to our identification strategy, these results should be interpreted with this timing issue in mind. Hence, the two approaches, state-level variables with the same timing as in our main estimations and county-level variables as in our main estimations but with unknown timing of clinical outcomes, provide different but complementary views of the mechanisms underlying our findings.
COVID-19 Tracking Project state-level outcomes:
We start with the empirical analysis of the relationship between PM 2.5 and hospitalizations, use of intensive care units, and use of ventilators, all observed in the COVID-19 Tracking Project at the state-day level. We also consider testing and positivity rates. Table 9 provides the main estimates in three panels, one for each outcome variable: hospitalizations, use of intensive care units, and use of ventilators. The first three columns provide same-day estimates with fixed effect specification changes that parallel our approach in Section 5, while columns (4) and (5) examine effects over three and seven days, respectively, where the outcome variable is represented by total patient-day use of these services over the corresponding period at the state level. The first panel of Table 9 shows that changes in PM 2.5 lead to more hospitalizations or longer hospital stays, in the order of about 10 to 16 additional hospitalization-days per state per county increase. This contemporaneous relationship suggests that changes in pollution can affect the clinical course of severe COVID-19 patients, leading to increased risk of hospitalization or longer hospitalizations. Point estimates tend to be larger, although not statistically significantly so, over three and seven days, with the latter specification being more imprecisely estimated.
Table 9.
Wind and PM 2.5 IV — Regressions over alternative outcomes: Hospitalizations, use of ICUs, and use of ventilators .
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Same-day | Same-day | Same-day | 3-day | 7-day | |
| Hospitalizations | |||||
| Weighted PM 2.5 | 13.18*** | 10.15*** | 16.41*** | 22.31** | 22.27 |
| (3.495) | (3.672) | (4.902) | (10.08) | (25.15) | |
| F Stat | 9.65 | 9.88 | 9.98 | 9.60 | 9.59 |
| Dep Var Mean | 1646.36 | 1647.19 | 1647.18 | 4962.06 | 1.2e+04 |
| Pct change mean | 0.800 | 0.616 | 0.996 | 0.450 | 0.191 |
| Controls | ✓ | ✓ | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ✓ | ✓ | ||
| County and MSA-by-week FEs | ✓ | ||||
| County and CBSA-by-week FEs | ✓ | ||||
| Observations | 70,875 | 70,823 | 70,801 | 70,757 | 70,587 |
| Intensive care units | |||||
| Weighted PM 2.5 | 3.260** | 3.192** | 4.433*** | 3.892 | 9.823 |
| (1.430) | (1.446) | (1.641) | (3.914) | (7.771) | |
| F Stat | 13.09 | 13.14 | 13.06 | 13.05 | 13.03 |
| Dep Var Mean | 639.95 | 640.08 | 640.22 | 1925.66 | 4507.23 |
| Pct change mean | 0.509 | 0.499 | 0.692 | 0.202 | 0.218 |
| Controls | ✓ | ✓ | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ✓ | ✓ | ||
| County and MSA-by-week FEs | ✓ | ||||
| County and CBSA-by-week FEs | ✓ | ||||
| Observations | 42,307 | 42,276 | 42,266 | 42,207 | 42,064 |
| Ventilators | |||||
| Weighted PM 2.5 | −0.0993 | 0.333 | 0.0985 | 0.0935 | 2.396 |
| (0.477) | (0.581) | (0.556) | (1.190) | (2.617) | |
| F Stat | 18.07 | 17.40 | 17.54 | 18.43 | 17.84 |
| Dep Var Mean | 207.99 | 207.99 | 208.00 | 615.11 | 1392.01 |
| Pct change mean | −0.048 | 0.160 | 0.047 | 0.015 | 0.172 |
| Controls | ✓ | ✓ | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ✓ | ✓ | ||
| County and MSA-by-week FEs | ✓ | ||||
| County and CBSA-by-week FEs | ✓ | ||||
| Observations | 30,614 | 30,591 | 30,580 | 30,561 | 30,484 |
, , . Standard errors clustered at the county level in parentheses. Controls include state-level and county-level policy adoption, wind speed, minimum and maximum daily temperature, precipitation, prior two-week social distancing behavior, day-of-week, and two lagged wind direction-by-monitor cluster interactions. The table displays regressions over three different outcomes: hospitalizations, use of Intensive Care Units (ICU), and use of ventilators, at the state-day level. All outcomes represent the number of patients using these healthcare resources on a given day. Columns (1) through (3) analyze these outcomes on the same day over three types of geography-by-week fixed effects. Column (4) and column (5) display the relationship between fine particulate matter and summed daily outcomes over three days and seven days, respectively. Regressions employ county population weights. F-statistics of the relevance test are computed assuming first-stage standard errors are not serially correlated.
If the clinical course of a COVID-19 patient does not improve with hospitalization, or if the symptoms are very concerning at the time of hospitalization, a move to an intensive care unit may be necessary. The second panel of Table 9 indicates that a same-day increase in PM 2.5 leads to higher use of intensive care units, in the order of about 3 to 4 additional intensive care units used per day per state for each increase, depending on the specification. Hence, a contemporaneous relationship between PM 2.5 and patient outcomes is identified for both hospitalizations and intensive care unit use. As mentioned, patients may be exposed to such higher levels of pollution while already hospitalized, or be immediately given a spot in an intensive care unit when transported to the hospital. We are unable to disentangle these two channels. Still, we discuss in Section 6 potential interventions to improve air quality in hospital rooms and indoor pollution in general. Estimates over three and seven days tend to be less precisely estimated. The coefficient for the seven-day period tends to be substantially larger than the ones in previous columns, pointing to a potential ramping up of the relationship, but the relatively large standard errors limit our ability to confirm such interpretation. Comparing estimates for hospitalizations and use of intensive care units, we observe that the identified relationship is about three to four times stronger for hospitalizations than it is for use of intensive care units. Recall that, as shown in the summary statistics provided in Table 1, state-level hospitalizations average 1646 while state-level use of intensive care units averages 640. Hence, on average, only 1 in 3 patients entered intensive care.
The third panel in Table 9 considers ventilator use by patients whose clinical course is more severe. While most coefficients suggest a positive and large, if not statistically significant, relationship between PM 2.5 and use of ventilators, the estimates tend to be noisy. As shown in the summary statistics provided in Table 1, the state average in ventilator use per day is around 208, so the number of observations from which to derive inference is relatively limited, given also the more spatially aggregate variable compared to our main specifications in Section 5. Further, it is possible that with ventilators the fraction of always-takers, in causal jargon, is larger, and thus the fraction of compliers from whom to infer smaller, contributing to the above-mentioned noise. Hence, the observed statistical imprecision prevents us from making any conclusive statements regarding ventilator use using these data alone.
We also consider how PM 2.5 affected viral testing and positivity rates. PM 2.5 may increase testing if people experience new symptoms associated with COVID-19 or more severe COVID-19 symptoms. While our fixed effects specifications are designed to hold statewide infection rates roughly constant within a given week, PM 2.5 may nevertheless increase positivity rates if more individuals with COVID-19 experience symptoms and get tested compared to a counterfactual where a larger fraction of tests is taken by asymptomatic individuals, either because of testing requirements or because they might have been in contact with an individual who then tested positive. PM 2.5 could also potentially increase the positivity rate if PM 2.5 accelerates transmission of COVID-19 as hypothesized by Setti et al. (2020) and Zhang et al. (2020). However, as mentioned, there is little evidence in favor of this latter channel. Lastly, we note the possibility that elevated exposure to PM 2.5 could even decrease the positivity rate if many individuals seek testing after mistaking symptoms of air pollution exposure with COVID-19 infection.
Table C14 shows our results for viral testing and positivity rates. First, we observe that air pollution shocks increase the number of new viral tests, in columns (4) and (5), on the order of 450 new tests per state over the following three-day period. This is a 1% increase relative to the mean viral tests conducted daily. For context, in Table 5 we show that a one unit of additional PM 2.5 increases case incidence by 1.5% over a three-day period, suggesting that individuals seeking out testing due to new or worsening symptoms could be an important mechanism driving the increase in COVID-19 cases. For the positivity rate, we see uniformly positive point estimates, but these coefficients are imprecisely estimated and statistically indistinguishable from zero.
CDC case surveillance records:
As described in Section 3, the CDC case surveillance records provide information on COVID-19 patients collected by hospitals, healthcare providers, and laboratories, with details of illness progression and socio-demographic characteristics. In Section 5, we implement our main model specification on these records collapsed to the county-day level, as shown in Table 10, and we report that these results are very similar to those seen with the John Hopkins data in Table 3 and Table 4. In this section, we take advantage of the patient-level structure of these records to explore the mechanisms behind our main results regarding COVID-19 cases and mortality. Specifically, we adjust the two-stage approach in Eq. (1) to model individual-level adverse clinical outcomes including a patient’s likelihood of mortality, hospitalization, ICU admittance, and mechanical ventilation. Since the unit of observation is the individual, we also add controls for individual characteristics that might relate to COVID-19 illness severity including sex, race and ethnicity, age group, and pre-existing medical conditions, which are summarized in Table C2. There are two limitations of this specification, as mentioned previously in this section as well as in Section 3. First, clinical outcomes are frequently missing in the case surveillance records. Second, we expect additional noise because the date of clinical transitions is not observed. As such, these results should be interpreted as the effect of an additional random shock of air pollution exposure on the day that a patient has their case confirmed via testing.
Table 11 displays regressions of the individual-level outcomes of mortality, hospitalization, admission to intensive care units, and mechanical ventilation on daily wind-fitted PM 2.5 levels in the same county. These results again confirm that additional air pollution exposure, even if only at the start of a COVID-19 illness, worsens the severity of illness and increases the likelihood of mortality. Columns (1) through (3) in the first panel of Table 11 indicate that an additional unit of air pollution on the day of case confirmation increases the likelihood of eventual mortality by 0.13 to 0.15 percentage points, or a 1.1 to 1.3 percent increase from the mean mortality rate of 11.4%. Recall that this mortality outcome is only for cases where eventual mortality is known, and missing values may be more likely to reflect no mortality. This percent change in likelihood of mortality is roughly one fourth the percent increase reported in Table 3, which may be because air pollution exposure at the start of an illness has less of an impact on mortality likelihood than air pollution exposure when a case is more advanced. Similarly, columns (1) through (3) of the second panel of Table 11 show that an additional unit of air pollution exposure on the day of case confirmation increases the likelihood of eventual mechanical ventilation by 0.12 to 0.17 percentage points, or a 2%–3% increase from the mean likelihood of ventilation of 6% for cases where this outcome is known with certainty. This effect is much more precise than the estimates based on state outcomes observed in Table 9, which were generally positive but not statistically significant. We see no statistically significant relationship between air pollution shocks at the start of an illness and hospitalization, while the relationship between air pollution at the start of illness and later admission to intensive care units is positive and close to statistical significance. Results for admission to intensive care units and hospitalization are noisier than those observed for state outcomes in Table 9, where hospitalization and admission to intensive care units were generally significant.
Table 11.
Mortality, Hospitalization, Mechanical ventilation, and ICU entry propensity using CDC case surveillance records .
| Deaths |
Hospitalization |
|||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Weighted PM 2.5 | 0.00154** | 0.00137** | 0.00133** | −0.000754 | −0.000214 | −0.0000299 |
| (0.000597) | (0.000535) | (0.000537) | (0.000909) | (0.000793) | (0.000792) | |
| F Stat | 115.00 | 121.70 | 122.74 | 137.67 | 142.05 | 142.68 |
| Dep Var Mean | 0.114 | 0.114 | 0.114 | 0.235 | 0.235 | 0.235 |
| Pct change mean | 1.343 | 1.203 | 1.167 | −0.321 | −0.091 | −0.013 |
| Controls | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ✓ | ||||
| County and MSA-by-week FEs | ✓ | ✓ | ||||
| County and CBSA-by-week FEs | ✓ | ✓ | ||||
| Observations | 311,591 | 311,456 | 311,380 | 382,686 | 382,597 | 382,557 |
| Mechanical ventilation |
Intensive care unit |
|||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Weighted PM 2.5 | 0.00171** | 0.00125* | 0.00131* | 0.00149 | 0.000955 | 0.00115 |
| (0.000808) | (0.000719) | (0.000713) | (0.00101) | (0.000940) | (0.000935) | |
| F Stat | 79.28 | 83.81 | 92.88 | 74.86 | 75.99 | 84.15 |
| Dep Var Mean | 0.061 | 0.061 | 0.061 | 0.107 | 0.107 | 0.106 |
| Pct change mean | 2.786 | 2.038 | 2.148 | 1.395 | 0.896 | 1.079 |
| Controls | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| County & State-by-week FEs | ✓ | ✓ | ||||
| County and MSA-by-week FEs | ✓ | ✓ | ||||
| County and CBSA-by-week FEs | ✓ | ✓ | ||||
| Observations | 177,336 | 177,224 | 177,179 | 177,356 | 177,211 | 177,091 |
, , . Standard errors clustered at the county level in parentheses. Outcomes are a binary indicator for whether an individual confirmed case resulted in mortality, hospitalization, mechanical ventilation, or ICU entry. Controls include state-level and county-level policy adoption, wind speed, minimum and maximum daily temperature, precipitation, prior two-week social distancing behavior, day-of-week, and two lagged wind direction-by-monitor cluster interactions. Individual-level controls include sex, age, race and ethnicity, and pre-existing medical conditions. Displayed output of a two-stage least squares regression model with county and state-by-week, MSA-by-week, or CBSA-by-week fixed effects in which wind direction and air quality monitor cluster interactions are used to predict PM 2.5 levels in a county on a given day. F-statistics of the relevance test are computed assuming first-stage standard errors are not serially correlated.
We run two sensitivity analyses for these outcomes. First, in Table C18, we test whether any of these results are sensitive to the inclusion or exclusion of specific individual-level covariates such as sex, age, ethnicity, or pre-existing medical conditions. These covariates do not substantially affect the results. Next, given the high proportion of missing clinical outcomes, we run these regressions with weights for the likelihood of missing clinical observations.39 These weights are intended to emphasize the informational value of records in states and counties where this information is more likely to be known with a higher degree of confidence. In Table C19, we present individual-level regressions of likelihood of adverse clinical outcomes on air pollution with weights for the inverse likelihood of an observed case having non-missing clinical outcomes. In these regressions, the weights employed vary depending on the clinical outcome because different outcomes have a different share of missing observations. For each clinical outcome, point estimates are larger and more statistically precise than without weights. In particular, the relationship between an air pollution shock at the start of an illness and the likelihood of mortality is twice as large as the estimate observed in Table 11. We take this sensitivity test as evidence that our primary results are conservative.
To determine the extent to which the differences between individual-level and state-level clinical progressions reflect differing observed timing of each event in each dataset, we test the relationship between longer-term pollution and the likelihood of more severe clinical outcomes in Table C20. For these results, we modify our primary regressor of interest, PM 2.5, by replacing it with the average concentration over a 3, 7, 10, or 14-day period after the day of case confirmation. This change ensures that cases resulting in mortality or hospitalization are being regressed on air pollution concentrations that may be more relevant to the dates surrounding clinical progression compared to the time of case confirmation, as used in Table 11. This procedure temporally separates wind direction variables from the relevant air pollution measurements to an extent. As such, we observe declining F-statistics from 115 to 66, 72, 45, and 35 as we progress from panel (a) to (e) of Table C20 and to longer PM 2.5 time horizons. The impact of air pollution over longer time horizons does appear larger for mortality. Average PM 2.5 concentrations in the same county over a 10- or 14-day period result in twice as large an impact on mortality as the air pollution shock on the day of case confirmation, increasing risk of mortality by roughly 0.3–0.4 percentage points or 3%. We see similar results for mechanical ventilation but only over a shorter time horizon of three days, with average PM 2.5 concentration over the 3-day period following case confirmation increasing risk of mechanical ventilation by 0.4 percentage points, which is over twice as high as the same-day impact. For hospitalizations, we observe that pollution is positively associated with hospitalization for periods from 3 to 14 days, unlike the same day effect observed in Table 11. The point estimate is generally stable around a 0.1 percentage point increase in likelihood of hospitalization, but it is not statistically significant in any specification. For admission to intensive care units, we see no clear pattern in Table C20, with values that are positive and suggestive over 3-day and 14-day periods but that are essentially zero over 7-day and 10-day periods.
Overall, the COVID-19 Tracking Project information and the restricted CDC case surveillance data provide complementary views of the mechanisms by which air pollution impacts severity of COVID-19 illnesses. The COVID-19 Tracking Project data, which has accurate timing of clinical progression information at the state level, shows that air pollution increases the number of cases resulting in hospitalization and admission to intensive care units. The CDC case surveillance data, meanwhile, which is county-level but does not have time stamps for clinical progression outcomes, suggest that individuals exposed to worse air pollution at the time of case confirmation are more likely to require mechanical ventilation and ultimately succumb to COVID-19 illness.
5.5. Heterogeneity
In this section, we focus on potential heterogeneity in the relationship between PM 2.5 and COVID-19 cases, mortality, and measures of clinical progression such as use of mechanical ventilation. We use two sources of data for the analysis of heterogeneity. First, we rely on the restricted CDC case surveillance data and leverage individual characteristics to conduct regressions over subsets of the population by age, gender, and race and ethnicity categories. Second, we rely on our primary dataset of COVID-19 cases and deaths and consider dimensions of heterogeneity at the county level such as the fraction of essential workers, urbanization rates, population density, vaccination rates as of May 2021 as proxy for risk attitudes with respect to COVID-19, vaccine hesitance, and self-reported mask-wearing behavior. Our empirical approach still relies on the identification strategies presented in Section 4, and a detailed description of this analysis is provided in Appendix A.
Before summarizing the main findings, we note that the purpose of this analysis is descriptive and subject to important caveats. To start, the CDC case surveillance regressions infer from noisier estimates because of smaller sample sizes. This is particularly true for results regarding Native American communities. These regressions also have a high proportion of missing clinical outcomes and uncertainty in timing as discussed previously. Next, with regards to the analysis of heterogeneity across county-level characteristics, the interaction terms should be understood as correlational and not causal links. Several of the variables that we include as interactions are correlated, and there may be additional characteristics that we do not observe.
The heterogeneity analysis using CDC case surveillance data, described in detail in Appendix A, provides evidence that population groups with increased potential social vulnerability are also more likely to see larger increases in reported case numbers related to air pollution exposure. As shown in Table C21, individuals aged 60 and over see twice the percent increase in confirmed case incidence from a unit of PM 2.5 in comparison to individuals under the age of 20. Individuals aged 80 and over see the largest increase in case incidence per unit of PM 2.5; the point estimate of 1 case per 100,000 is over four times as large as the population-level effect observed in Table 10. In the same table, we also observe that Black and Hispanic communities see a greater increase in case incidence per unit of PM 2.5 than White populations, suggesting disparate cumulative risks from pollution exposure and COVID-19 for people of color and the elderly. We also observe that males see larger increases in mortality and mechanical ventilation in comparison to females, as shown in Table C22. The heterogeneity analysis with respect to age and sex are very much in line with Isphording and Pestel (2021), who find the largest impacts of air pollution on COVID-19 mortality accrue to male patients over the age of 80.
We report findings from the heterogeneity analysis of county characteristics in Table C16. The interaction terms suggest a stronger relationship between PM 2.5 and COVID-19 cases in counties with a higher fraction of essential workers. We also observe a weaker relationship between air pollution and cases and deaths in counties with higher population density, urbanization rates, and eventual vaccination in 2021. Population density and urbanization rates correlate positively with propensity to seek vaccination once it becomes available after the time frame of our study, as shown in Table C15. Thus, these results could suggest that differential cautionary behavior may have moderated the relationship between PM 2.5 and COVID-19 morbidity and mortality in more urbanized areas. We explore the potential role of differential cautionary behavior with a separate analysis of heterogeneity across vaccine hesitance in Table C17, discussed further in Appendix A. Additional sensitivity analysis with respect to self-reported mask-wearing behavior, which protects against COVID-19 and may also directly mitigate exposure to air pollution, is reported in Table C7 and described in Section 5.3. Finally, we note that the inclusion of interaction terms with PM 2.5 and each dimension of heterogeneity increases the precision and generally increases the magnitude of our estimated relationship between PM 2.5 and cases or mortality at the mean level of the interacted variable, as reported at the bottom of Table C15.
6. Policy relevance
Our findings indicate that higher contemporaneous exposure to PM 2.5 leads to higher COVID-19 morbidity and mortality. These findings are relevant for the current pandemic as well as future ones. As mentioned in Section 2, local air pollution has been linked to more severe outcomes in previous outbreaks. Further, pollution levels have been shown to increase the severity of the regular flu (Graff Zivin et al., 2020). Our results add to this established literature assessing the causal relationship between local air pollution and health outcomes, which often calls for additional measures to mitigate such adverse effects (see Currie et al., 2014 for a review).
In what follows, we provide a set of policy implications starting with actions that policymakers could undertake in the context of the ongoing pandemic and then expanding to levers affecting pollution over a longer time frame. These lessons tend to be valid for ensuing variants of COVID-19 as well as potential future pandemics. They may also be used in the context of especially problematic variants of the regular flu, including localized outbreaks. The severity of a given winter’s flu may for instance depend on the ability of vaccines to prevent it, which varies from year to year, a plausibly random feature that Graff Zivin et al. (2020) exploit for identification purposes.
While concentrations of PM 2.5 may have been lower in 2020 than in previous years for some U.S. cities in the early days of the COVID-19 outbreak (see Berman and Ebisu, 2020, Zhang et al., 2021), we document in Section 3 little change in PM 2.5 or AQI levels nationwide over the course of the pandemic, a finding consistent with Bekbulat et al. (2020). Further, Persico and Johnson (2021) report an increase in particulate matter in counties with TRI sites at the start of the pandemic, suggesting that environmental deregulation may have offset decreases in air pollution from less motorized traffic in many regions. Fig. 6 shows a pattern consistent with these elements. Meanwhile, the cumulative number of COVID-19 cases and deaths increased in the United States as well as globally during the duration of the pandemic. It follows from our findings that there is a rationale for limiting pollution levels while managing a pandemic. There exist several policy levers to accomplish this goal. Private companies may also contribute to keep contemporaneous pollution down as part of their corporate social responsibility strategies by letting employees telework whenever appropriate. As suggested in Persico and Johnson (2021), hospitals may consider using air purifiers in rooms with COVID-19 patients, or influenza patients, to limit exposure to indoor air pollution and prevent the need for ventilators. Individuals are indeed exposed to pollution not only outdoors but also indoors, an issue that is especially severe in emerging countries but also in developed countries, especially for the most vulnerable individuals (Jeuland et al., 2015).
Regulations can limit the extent with which people move for non-essential activities and encourage continued teleworking, in case voluntary efforts by companies are deemed insufficient. Local governments can also regulate traffic and pollution directly. For instance, adjusting speed limits on highways to traffic conditions can reduce pollution (Bel and Rosell, 2013). Temporary policies using alternate license plates can be enforced for non-essential movements, for instance allowing individuals with an even final digit on the license plate number to circulate only on even days of the month (Davis, 2008, Gallego et al., 2013, Li, 2018). Retrofitted public transit vehicles can be used whenever possible (Beatty and Shimshack, 2011, Austin et al., 2019), especially where the number of routes and the frequency of service may be adjusted downward during an outbreak.
These policy implications apply globally. For instance, cities with congestion charges already in place, such as Gothenburg, London, Milan, Singapore, or Stockholm, may consider adjusting the price level to reflect pollution levels and the spread of COVID-19 or any other disease increasing the marginal damage of pollution through more severe health outcomes (Coria et al., 2015). Congestion charges have indeed been shown to reduce overall traffic and pollution (Leape, 2006, Gibson and Carnovale, 2015, Tang, 2021). Several cities around the world also limit access to city centers or entire regions to some vehicles, depending on vintage, fuel type, and efficiency (e.g., Barahona et al., 2019). The use of low emission zones can contribute to reduce air pollution in urban areas and improve health outcomes (Wolff, 2014, Gehrsitz, 2017, Pestel and Wozny, 2021). Such regulations may also be adjusted during a pandemic.
Finally, reducing actual pollution may not be the only lever available to policymakers. Governments could also try to reduce exposure to local air pollution. Many jurisdictions around the world provide their citizens with air quality information (or “smog alerts”), which have been shown to increase avoidance behavior (Neidell, 2009). Combining information on COVID-19 cases and deaths with air quality information, while informing the public of the relationship between the two, could be an inexpensive approach to reducing cases and deaths.
Over the longer run, pandemic-related deaths could be used as an additional impetus to internalize known externalities from local air pollution (e.g. Parry and Small, 2005, Muller and Mendelsohn, 2009), also in consideration of the relationship between local air pollution and flu outcomes. Besides pollution pricing, complementary policies that have been shown to reduce local air pollution may include expanding current public transit infrastructure to limit local air pollution (Lalive et al., 2018, Li et al., 2019) and expanding subsidies for electric or hybrid vehicles and charging stations (Beresteanu and Li, 2011, Li et al., 2017, Muehlegger and Rapson, 2018), although in the latter case local contextual factors may need to be taken into account (Holland et al., 2016). Finally, it is important to acknowledge the potentially important recessionary forces related to pandemics. While economic downturns may justify some relaxation of environmental policies based on costs and benefits, such relaxation should in principle never be arbitrary, as discussed in Annicchiarico et al. (2021). That is, environmental policies should ideally include from their implementation rules that relate to business cycles, so that regulators tie their hands and potentially arbitrary rollbacks, as observed following the onset of the COVID-19 outbreak, can be avoided. Such rules may also need to account for the fact that pandemic-related recessions may be different from other recessions since, as this paper shows for COVID-19, local air pollution increases the pandemic’s severity.
7. Conclusion
The novel Coronavirus has caused millions of deaths and severe economic damage across the world. The common experience of many countries showed that a trade-off exists between the speed at which economic activity is relaunched and the risk of further cases and deaths. This trade-off is usually described as between two important but conflicting goals: jobs and economic recovery on one side, and limiting cases and deaths on the other. Our paper adds one dimension to this trade-off, pointing to an untapped potential to limit severe cases and deaths while sustaining economic recovery. Our study shows that the observed trade-off between the two aforementioned desirable goals can be relaxed by keeping contemporaneous air pollution at low levels, contributing to a recent stream of causal studies pointing to similar relationships between local air pollution and COVID-19 outcomes, such as Persico and Johnson (2021) and Isphording and Pestel (2021).
In particular, our study finds strong evidence that contemporaneous air quality almost immediately affects the severity of COVID-19 illness. According to our results, a one increase in PM 2.5 (about 15% of the average concentration of PM 2.5) increases the number of confirmed cases by roughly 2% and deaths by 4% from the mean daily incidence in a county. Our results rely on arguably exogenous variation in wind direction and are robust to a wide variety of specifications. Furthermore, we estimate a positive and significant relationship between PM 2.5 and COVID-19-related hospitalizations, intensive care unit use, and ventilator use. Overall, our study implies a role for policies aimed at lowering pollution in addressing pandemics. Further, our findings speak to the general relationship between exposure to PM 2.5 and human health, in particular concerning respiratory issues. They provide additional justification for optimally regulating local air pollution.
Finally, our study also paves the way for additional causal research in this space. First, while our analysis provides evidence of a relationship between PM 2.5 exposure and COVID-19 cases, hospitalizations, use of intensive care units, use of ventilators, and mortality, estimates obtained with our model are sometimes statistically imprecise. This is especially true for demographic breakouts such as age, sex, and race or ethnicity groups. It is also often difficult to ascertain the timeline of air pollution’s impact on COVID-19 case progression. Future research may combine data from many countries and longer periods to shed more light on this question. Such research may also make use of more-complete individual health records to explore issues of inconsistent reporting, disease progression, or environmental justice concerns in the extent to which pollution drives inequity in COVID-19 mortality. Such research may also explore the role of long-term exposure to pollution, which our study does not analyze and the epidemiological literature assesses in correlational terms. Doing so would add to a recent stream of research on the role of place on health (Banzhaf et al., 2019, Deryugina and Molitor, 2021). Further, there seems to be room for randomized interventions to improve air quality in hospital rooms in the context of pandemics. Second, while our study provides descriptive evidence on potential interesting dimensions of heterogeneity, the role that additional factors such as mask wearing, vaccine uptake, and compliance with social distancing may have in potentially mitigating the relationship between PM 2.5 and COVID-19 outcomes largely remains to be explored. Third, the above-mentioned strand of literature applying causal models to examine the relationship between air pollution and COVID-19 outcomes has so far focused on developed countries only. However, such relationship may be even stronger in contexts where pollution levels tend to be higher and very volatile as well as where healthcare systems may be unable to offer the same quality and quantity of services. Consistently, the scope for randomization may be even larger in such contexts.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
We thank Garth Heutel, Julie Hotchkiss, Daniel Kreisman, Rafael Lalive, James Marton, Givi Melkadze, Bryan Parthum, Andrew Schreiber, and Jonathan Smith for very helpful comments on a previous version of this paper, which first appeared in 2020 as (Austin et al., 2020), as well as three anonymous reviewers. We also thank Unacast, which provided the restricted access data on social distancing, as well as the U.S. Centers for Disease Control and Prevention, which provided individual case surveillance data. We acknowledge the use of Advanced Research Computing Technology and Innovation Core (ARCTIC) resources at Georgia State University’s Research Solutions made available by the National Science Foundation Major Research Instrumentation (MRI), United States grant number CNS-1920024. Carattini acknowledges support from the Grantham Foundation for the Protection of the Environment through the Grantham Research Institute on Climate Change and the Environment and from the ESRC Centre for Climate Change Economics and Policy as well as from the Swiss National Science Foundation, Switzerland , grant number PZ00P1_180006/1. Gomez-Mahecha acknowledges support from the program Pasaporte a la Ciencia - Bioeconomía (Passport to Science - Bioeconomy track) of the Colombian government. No funder had any involvement in the study design; the collection, analysis and interpretation of data; the writing of the report; or in the decision to submit the article for publication. The U.S. Centers for Disease Control and Prevention do not take responsibility for the scientific validity or accuracy of methodology, results, statistical analyses, or conclusions presented.
See Dong et al. (2020) for more information on the 2019 Novel Coronavirus COVID-19 (2019-nCoV) Data Repository by Johns Hopkins CSSE. See https://github.com/CSSEGISandData/COVID-19. Last accessed: February 10, 2021.
We note that there may be unobservable variation across and within states in the exact timing of case and death reporting. While these data are generally the most timely available, there are likely lags between when a health outcome occurred and when it became known to the state department of health or posted to the online tracking system. Some of these reporting delays are corrected ex post by state health departments to reflect more accurate time-stamps; we nevertheless explore sensitivity of our results to temporal alignment in Section 5.3 of the paper.
See https://covidtracking.com/data/download. Last accessed: July 7, 2021.
See https://data.cdc.gov/Case-Surveillance/COVID-19-Case-Surveillance-Restricted-Access-Detai/mbd7-r32t. Last accessed: May 16, 2022.
A template case reporting form can be viewed here: https://www.cdc.gov/coronavirus/2019-ncov/downloads/pui-form.pdf. Last accessed: May 16, 2022.
We calculate incidence for county on day as .
We note that these variables reflect patient-day totals rather than unique patient admissions, as patients can be hospitalized or be in an intensive care unit for multiple days.
See https://covidtracking.com/about-data/data-definitions for more information on these data elements. Last accessed: July 7, 2021.
In terms of weeks since the first non-travel-related COVID-19 case, Fig. 2 panel (a) represents the new cases during the first week of the outbreak, panel (b) new cases during weeks 2 to 5, (c) weeks 6 to 10, and (f) weeks 18 to 22.
See https://www.epa.gov/outdoor-air-quality-data/download-daily-data. Last accessed: July 7, 2021.
Authors’ calculation using the 2017 NEI data. For more information, see: https://www.epa.gov/air-emissions-inventories/2017-national-emissions-inventory-nei-data. Last accessed: July 7, 2021.
The clustering of air quality monitors over large geographic regions is an important element of our instrumental variables specification. This step ensures that identification of PM 2.5 relies on regionally transported PM 2.5 rather than local generation. We discuss this step in more detail in Section 4.
See https://www.ncei.noaa.gov/data/local-climatological-data/archive/2020.tar.gz. Last accessed: February 27, 2021.
The data also include information on weather conditions such as precipitation and temperature, but we source this information from elsewhere due to many missing values, as described below. We also limit the stations to the contiguous United States, reducing the total number of stations from 2820 to 2543.
Averaging wind direction requires decomposing wind direction into and directional vectors that are weighted by the magnitude of the direction (i.e., wind speed for each measurement in a day). The directional vector is . The directional vector is . We can then average and directional vectors for each station-day combination and compute daily average wind direction as .
To account for the fact that some weather stations are closer to an air quality monitor, the assigned wind direction for EPA air quality monitor at time () is given by , where is a matrix representing the scalar and wind direction components of the th nearest weather station at time , and is the weight of the th monitor based on the distance between and (. The convention of inverse-distance weighting the four nearest weather stations is based on Deryugina et al. (2019), but we explore the sensitivity of our results to this wind direction-to-air quality assignment mechanism in Section 5.3 and more specifically Table C11.
See PRISM (2004) and also https://prism.oregonstate.edu/ for more information. Last accessed: July 7, 2021.
We use the R package ‘prism’ to download daily minimum and maximum temperature, as well as precipitation, for each 800 × 800 meter gridded cell in the United States (Edmund et al., 2020). We make use of tmin, tmax, tmean, and precip_sum options in the “prism” R package.
See https://www.unacast.com/. Last accessed: September 2, 2020.
Unacast categorized “essential” based on states’ guidelines. Essential locations include facilities like food stores, pet stores, and pharmacies, while non-essential facilities include restaurants, department and clothing stores, spas and hair salons, among others. See https://www.unacast.com/post/unacast-updates-social-distancing-scoreboard for more details on Unacast’s methodology. Last accessed: September 2, 2020.
For more detail on the indicator’s origin and the methodology followed by Unacast, see https://www.unacast.com/post/rounding-out-the-social-distancing-scoreboard. Last accessed: September 2, 2020.
See https://www.coronanet-project.org/download.html. Last accessed: September 2, 2020.
See https://healthdata.gov/dataset/COVID-19-State-and-County-Policy-Orders/gyqz-9u7n. Last accessed: February 10, 2021.
The full list of state policies includes limiting mass gatherings, social distancing actions, stay at home or quarantine orders, school closures, testing initiatives, state border closures, public surface cleaning, curfews, information campaigns, state of emergency declarations, administrative task forces, policies to provide greater access to personal protective equipment, and other policies to increase access to healthcare resources (such as respirators). The full list of county policies includes mask mandates, quarantines, and policies with respect to K-12 education, essential and non-essential businesses, religious establishments, manufacturing establishments, and recreation activities.
See https://covid19pulse.usc.edu/. Last accessed: April 12, 2022.
See Fig. 4 for a map of all air monitor clusters.
Deryugina et al. (2019) perform many robustness tests to confirm that this regional-based specification is not identifying local generation of fine particulate matter. The authors perform randomization tests across monitors within regional cluster, showing that the results are the same for all randomized sub-groups within cluster. See their Online Appendix A, “Source of Identifying Variation”, for a detailed discussion.
Each week of the outbreak is defined as one plus the number of weeks since January 19, 2020, which is the first week of reporting in the Johns Hopkins Data. Therefore, each weekly period is measured from Sunday to Saturday.
For example, a given wind direction is allowed to influence air pollution in the Chesapeake Bay region differently than the same wind direction in the San Francisco bay region. Moreover, each is common to all monitors within a larger region, and so a few monitors near local sources in a given county should not systematically identify each .
We note that social distancing behavior over the previous two-week period may potentially be correlated with air quality. We take this theoretical possibility seriously and test the sensitivity of our results to alternative specifications in which we alter the control variables in our model, as shown in Table C6. We further discuss this potential issue in Section 5.3.
Please refer to Correia (2016) for more details.
The use of state-by-week fixed effects, or within-state-and-week comparisons, imply that we are not investigating how air quality affects the speed of transmission of the virus but rather how air quality affects the severity of illness among already-infected individuals. Confirmed cases are expected to represent more severe cases, for which infected individuals experience symptoms and seek testing (Day, 2020, Gandhi et al., 2020). We do not expect air pollution to change the threshold of symptoms leading individuals to seek testing, but rather to increase the number of people whose symptoms exceed such threshold. The often-lengthy incubation period, testing lags, and reporting lags mean that our estimation procedure does not identify the speed of transmission. Section 5.4 further examines potential transmission channels as discussed in the literature and how they may relate to our empirical framework.
In each of these alternative fixed effect specifications, counties that are not in an MSA or CBSA are assigned state-by-week fixed effects. For example, a county and MSA-by-week fixed effects specification would make within-MSA, within-week comparisons for MSAs, while rural regions would be compared to other non-MSA regions in the same state and week. To avoid over-fitting, any MSA or CBSA with only one county is assigned the state-by-week fixed effect. Analyses are also provided where we focus only on MSAs.
As in Deryugina et al. (2019), we report F-statistics computed by assuming that first-stage errors are not serially correlated. We have also computed the F-statistics assuming serially correlated first-stage errors. As in Deryugina et al. (2019), F-statistics computed assuming serially correlated errors are substantially larger than those we report. In either case, both computation methods yield F-statistics above 10 for our primary empirical specifications on PM 2.5.
MSA-by-week and CBSA-by-week fixed effects specifications point to very similar patterns. The corresponding estimates are presented in Table C4 and Table C5 in the Appendix.
Regression results with the complete set of covariates can be found in Table C3, columns (4) to (6).
We conducted an analysis of residuals to compare log-transformed and regular outcomes. The log-transformed model eliminated a small share of the upward skew in our residuals. However, they also introduced some degree of bias. We noted a slight downward line of fit between the residuals and fitted values in log-transformed models, while our main model displayed a flat relationship between fitted values and the residuals. We believe this analysis supports our use of non-transformed case and death incidence variables as primary outcomes, a decision that is also in line with Isphording and Pestel (2021).
We assume that missing clinical information can be described as missing at random, in which case weighting is a method for improving statistical precision (see Raghunathan, 2004 and Kennedy et al., 2019 for further details). Observations from states or counties that are more likely to have missing clinical information are weighted less than observations in areas that are more frequently non-missing. To estimate likelihood weights, we capture the predicted values from a logit regression of the case count, county population, and state dummies on a binary indicator for whether a case observation is dropped from our primary CDC case surveillance regressions.
Supplementary material related to this article can be found online at https://doi.org/10.1016/j.jeem.2023.102815.
Appendix A. Supplementary data
The following is the Supplementary material related to this article.
The appendix includes heterogeneity analysis, supplemental sources of information, and additional tables and figures.
References
- Ackermann M., Verleden S.E., Kuehnel M., Haverich A., Welte T., Laenger F., Vanstapel A., Werlein C., Stark H., Tzankov A., Li W.W., Li V.W., Mentzer S.J., Jonigk D. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N. Engl. J. Med. 2020;383(2):120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguilar-Gomez S., Dwyer H., Graff Zivin J., Neidell M. This is air: The ‘non-health’ effects of air pollution. Annu. Rev. Resour. Econ. 2022;14(1):403–425. [Google Scholar]
- Anderson M.L. As the wind blows: The effects of long-term exposure to air pollution on mortality. J. Eur. Econom. Assoc. 2020;18(4):1886–1927. doi: 10.1093/jeea/jvz051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrejko K.L., Pry J.M., Myers J.F., Fukui N., DeGuzman J.L., Openshaw J., Watt J.P., Lewnard J.A., Jain S., Abdulrahim Y., Barbaduomo C.M., Bermejo M.I., Cheunkarndee J., Cornejo A.F., Corredor S., Dabbagh N., Dong Z.N., Dyke A., Fang A.T., Felipe D., Frost P.M., Ho T., Javadi M.H., Kaur A., Lam A., Li S.S., Miller M., Ni J., Park H., Poindexter D.J., Samani H., Saretha S., Spencer M., Spinosa M.M., Tran V.H., Walas N., Wan C., Xavier E. Effectiveness of face mask or respirator use in indoor public settings for prevention of SARS-CoV-2 infection — California, February–2021. MMWR Morb. Mortal. Wkly Rep. 2022;71(6):212–216. doi: 10.15585/mmwr.mm7106e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annicchiarico B., Carattini S., Fischer C., Heutel G. National Bureau of Economic Research; 2021. Business Cycles and Environmental Policy: Literature Review and Policy Implications: Working Paper 29032. [Google Scholar]
- Arceo E., Hanna R., Oliva P. Does the effect of pollution on infant mortality differ between developing and developed countries? Evidence from Mexico City. Econ. J. 2016;126(591):257–280. [Google Scholar]
- Austin W., Carattini S., Gomez Mahecha J., Pesko M. Grantham Research Institute on Climate Change and the Environment; 2020. COVID-19 Mortality and Contemporaneous Air Pollution: Working Paper 352. [Google Scholar]
- Austin W., Heutel G., Kreisman D. School bus emissions, student health and academic performance. Econ. Educ. Rev. 2019;70:109–126. [Google Scholar]
- Banzhaf S., Ma L., Timmins C. Environmental justice: The economics of race, place, and pollution. J. Econ. Perspect. 2019;33(1):185–208. [PubMed] [Google Scholar]
- Barahona N., Gallego F.A., Montero J.-P. Vintage-specific driving restrictions. Rev. Econom. Stud. 2019;87(4):1646–1682. [Google Scholar]
- Beatty T.K.M., Shimshack J.P. School buses, diesel emissions, and respiratory health. J. Health Econ. 2011;30(5):987–999. doi: 10.1016/j.jhealeco.2011.05.017. [DOI] [PubMed] [Google Scholar]
- Bekbulat B., Apte J.S., Millet D.B., Robinson A., Wells K.C., Marshall J.D. 2020. PM2.5 and ozone air pollution levels have not dropped consistently across the US following societal COVID response. [Google Scholar]
- Bel G., Rosell J. Effects of the 80 km/h and variable speed limits on air pollution in the metropolitan area of Barcelona. Transp. Res. D. 2013;23:90–97. [Google Scholar]
- Beresteanu A., Li S. Gasoline prices, government support, and the demand for hybrid vehicles in the United States. Internat. Econom. Rev. 2011;52(1):161–182. [Google Scholar]
- Berman J.D., Ebisu K. Changes in U.S. air pollution during the COVID-19 pandemic. Sci. Total Environ. 2020;739 doi: 10.1016/j.scitotenv.2020.139864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhaskar, A., Chandra, J., Braun, D., Cellini, J., Dominici, F., 2020. Air Pollution, SARS-CoV-2 Transmission, and COVID-19 Outcomes: A State-of-the-Science Review of a Rapidly Evolving Research Area. Technical report.
- Bishop K.C., Ketcham J.D., Kuminoff N.V. National Bureau of Economic Research; 2018. Hazed and Confused: The Effect of Air Pollution on Dementia: Report 0898-2937. [Google Scholar]
- Bourdrel T., Annesi-Maesano I., Alahmad B., Maesano C.N., Bind M.-A. The impact of outdoor air pollution on COVID-19: A review of evidence from in vitro, animal, and human studies. Eur. Respir. Rev. 2021;30(159) doi: 10.1183/16000617.0242-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodeur A., Gray D.M., Islam A., Bhuiyan S. Social Science Research Network; Rochester, NY: 2020. A Literature Review of the Economics of COVID-19: SSRN Scholarly Paper ID 3636640. [Google Scholar]
- Ceban F., Ling S., Lui L.M., Lee Y., Gill H., Teopiz K.M., Rodrigues N.B., Subramaniapillai M., Di Vincenzo J.D., Cao B., Lin K., Mansur R.B., Ho R.C., Rosenblat J.D., Miskowiak K.W., Vinberg M., Maletic V., McIntyre R.S. Fatigue and cognitive impairment in post-COVID-19 syndrome: A systematic review and meta-analysis. Brain Behav. Immun. 2022;101:93–135. doi: 10.1016/j.bbi.2021.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chay K., Dobkin C., Greenstone M. The Clean Air Act of 1970 and adult mortality. J. Risk Uncertain. 2003;27(3):279–300. [Google Scholar]
- Chay K., Greenstone M. The impact of air pollution on infant mortality: Evidence from geographic variation in pollution shocks induced by a recession. Q. J. Econ. 2003;118(3):1121–1167. [Google Scholar]
- Chen K., Wang M., Huang C., Kinney P.L., Anastas P.T. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet. Health. 2020;4(6):e210–e212. doi: 10.1016/S2542-5196(20)30107-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Xia J., Yu T., Zhang X., Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng C., Barceló J., Hartnett A., Kubinec R., Messerschmidt L. 2020. COVID-19 Government Response Event Dataset (CoronaNet v1.0) [DOI] [PubMed] [Google Scholar]
- Clay K., Lewis J., Severnini E. Pollution, infectious disease, and mortality: Evidence from the 1918 Spanish influenza pandemic. J. Econ. Hist. 2018;78(4):1179–1209. [Google Scholar]
- Coria J., Bonilla J., Grundström M., Pleijel H. Air pollution dynamics and the need for temporally differentiated road pricing. Transp. Res. A. 2015;75:178–195. [Google Scholar]
- Correia, S., 2016. Linear Models with High-Dimensional Fixed Effects: An Efficient and Feasible Estimator. Working Paper.
- Courtemanche C., Garuccio J., Le A., Pinkston J., Yelowitz A. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff. 2020;39(7):1237–1246. doi: 10.1377/hlthaff.2020.00608. PMID: 32407171. [DOI] [PubMed] [Google Scholar]
- Cox L.A., Popken D.A. Should air pollution health effects assumptions be tested? Fine particulate matter and COVID-19 mortality as an example. Glob. Epidemiol. 2020;2 doi: 10.1016/j.gloepi.2020.100033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y., Zhang Z.-F., Froines J., Zhao J., Wang H., Yu S.-Z., Detels R. Air pollution and case fatality of SARS in the People’s Republic of China: An ecologic study. Environ. Health. 2003;2(1):15. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings M.J., Baldwin M.R., Abrams D., Jacobson S.D., Meyer B.J., Balough E.M., Aaron J.G., Claassen J., Rabbani L.E., Hastie J., Hochman B.R., Salazar-Schicchi J., Yip N.H., Brodie D., O’Donnell M.R. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet. 2020;395(10239):1763–1770. doi: 10.1016/S0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J., Neidell M. Air pollution and infant health: What can we learn from California’s recent experience? Q. J. Econ. 2005;120(3):1003–1030. [Google Scholar]
- Currie J., Walker R. Traffic congestion and infant health: Evidence from E-ZPass. Am. Econ. J.: Appl. Econ. 2011;3(1):65–90. [Google Scholar]
- Currie J., Zivin J.G., Mullins J., Neidell M. What do we know about short- and long-term effects of early-life exposure to pollution? Annu. Rev. Resour. Econ. 2014;6(1):217–247. [Google Scholar]
- Davis L.W. The effect of driving restrictions on air quality in Mexico City. J. Polit. Econ. 2008;116(1):38–81. [Google Scholar]
- Day M. COVID-19: Four fifths of cases are asymptomatic, China figures indicate. BMJ. 2020;369 doi: 10.1136/bmj.m1375. [DOI] [PubMed] [Google Scholar]
- Deryugina T., Heutel G., Miller N.H., Molitor D., Reif J. The mortality and medical costs of air pollution: Evidence from changes in wind direction. Amer. Econ. Rev. 2019;109(12):4178–4219. doi: 10.1257/aer.20180279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deryugina T., Molitor D. The causal effects of place on health and longevity. J. Econ. Perspect. 2021;35(4) doi: 10.1257/jep.35.4.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deschênes O., Greenstone M., Shapiro J.S. Defensive investments and the demand for air quality: Evidence from the NOx Budget Program. Amer. Econ. Rev. 2017;107(10):2958–2989. [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebenstein A., Lavy V., Roth S. The long-run economic consequences of high-stakes examinations: Evidence from transitory variation in pollution. Am. Econ. J.: Appl. Econ. 2016;8(4) [Google Scholar]
- Edmund H., Bell K., Butler A. 2020. Access data from the Oregon State Prism Climate Project. R package version 0.2.0. [Google Scholar]
- EPA . U.S. Environmental Protection Agency; Washington, DC: 2019. Integrated Science Assessment (ISA) for Particulate Matter: Technical Report EPA/600/R-19/188. [PubMed] [Google Scholar]
- EPA . U.S. Environmental Protection Agency; Washington, DC: 2021. Changes to the Tri List of Toxic Chemicals: Technical report. [Google Scholar]
- Gallego F., Montero J.-P., Salas C. The effect of transport policies on car use: Evidence from Latin American cities. J. Public Econ. 2013;107:47–62. [Google Scholar]
- Gandhi M., Yokoe D.S., Havlir D.V. Asymptomatic transmission, the Achilles’ heel of current strategies to control COVID-19. N. Engl. J. Med. 2020;382(22):2158–2160. doi: 10.1056/NEJMe2009758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gehrsitz M. The effect of Low Emission Zones on air pollution and infant health. J. Environ. Econ. Manag. 2017;83:121–144. [Google Scholar]
- Gibson M., Carnovale M. The effects of road pricing on driver behavior and air pollution. J. Urban Econ. 2015;89:62–73. [Google Scholar]
- Graff Zivin J., Neidell M. Days of haze: Environmental information disclosure and intertemporal avoidance behavior. J. Environ. Econ. Manag. 2009;58(2):119–128. [Google Scholar]
- Graff Zivin J.S., Neidell M.J., Sanders N.J., Singer G. National Bureau of Economic Research; 2020. When externalities collide: Influenza and pollution: Technical Report w27982. [Google Scholar]
- Grainger C., Schreiber A. Discrimination in ambient air pollution monitoring? AEA Pap. Proc. 2019;109:277–282. [Google Scholar]
- Grange, S., 2014. Technical Note: Averaging Wind Speeds and Directions. Technical report.
- Guan W.-j., Ni Z.-y., Hu Y., Liang W.-h., Ou C.-q., He J.-x., Liu L., Shan H., Lei C.-l., Hui D.S., Du B., Li L.-j., Zeng G., Yuen K.-Y., Chen R.-c., Tang C.-l., Wang T., Chen P.-y., Xiang J., Li S.-y., Wang J.-l., Liang Z.-j., Peng Y.-x., Wei L., Liu Y., Hu Y.-h., Peng P., Wang J.-m., Liu J.-y., Chen Z., Li G., Zheng Z.-j., Qiu S.-q., Luo J., Ye C.-j., Zhu S.-y., Zhong N.-s. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannum M.E., Koch R.J., Ramirez V.A., Marks S.S., Toskala A.K., Herriman R.D., Lin C., Joseph P.V., Reed D.R. Taste loss as a distinct symptom of COVID-19: A systematic review and meta-analysis. Chem. Senses. 2022;47 doi: 10.1093/chemse/bjac001. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- He X., Cheng X., Feng X., Wan H., Chen S., Xiong M. Clinical symptom differences between mild and severe COVID-19 patients in China: A meta-analysis. Front. Public Health. 2021;8 doi: 10.3389/fpubh.2020.561264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J., Liu H., Salvo A. Severe air pollution and labor productivity: Evidence from industrial towns in China. Am. Econ. J.: Appl. Econ. 2019;11(1):173–201. [Google Scholar]
- Holland S.P., Mansur E.T., Muller N.Z., Yates A.J. Are there environmental benefits from driving electric vehicles? The importance of local factors. Amer. Econ. Rev. 2016;106(12):3700–3729. [Google Scholar]
- Huang D., Lian X., Song F., Ma H., Lian Z., Liang Y., Qin T., Chen W., Wang S. Clinical features of severe patients infected with 2019 novel coronavirus: A systematic review and meta-analysis. Ann. Transl. Med. 2020;8(9) doi: 10.21037/atm-20-2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishmatov A. SARS-CoV-2 is transmitted by particulate air pollution: Misinterpretations of statistical data, skewed citation practices, and misuse of specific terminology spreading the misconception. Environ. Res. 2022;204 doi: 10.1016/j.envres.2021.112116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isphording I.E., Pestel N. Pandemic meets pollution: Poor air quality increases deaths by COVID-19. J. Environ. Econ. Manag. 2021;108 doi: 10.1016/j.jeem.2021.102448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jans J., Johansson P., Nilsson J.P. Economic status, air quality, and child health: Evidence from inversion episodes. J. Health Econ. 2018;61:220–232. doi: 10.1016/j.jhealeco.2018.08.002. [DOI] [PubMed] [Google Scholar]
- Jeuland M., Pattanayak S.K., Bluffstone R. The economics of household air pollution. Annu. Rev. Resour. Econ. 2015;7(1):81–108. [Google Scholar]
- Jia M., Zhao T., Cheng X., Gong S., Zhang X., Tang L., Liu D., Wu X., Wang L., Chen Y. Inverse relations of PM2.5 and O3 in air compound pollution between cold and hot seasons over an urban area of East China. Atmosphere. 2017;8(3) [Google Scholar]
- Kan H.-D., Chen B.-H., Fu C.-W., Yu S.-Z., Mu L.-N. Relationship between ambient air pollution and daily mortality of SARS in Beijing. Biomed. Environ. Sci. 2005;(1):1–4. [PubMed] [Google Scholar]
- Kennedy E.H., Mauro J.A., Daniels M.J., Burns N., Small D.S. Handling missing data in instrumental variable methods for causal inference. Annu. Rev. Stat. Appl. 2019;6(1):125–148. doi: 10.1146/annurev-statistics-031017-100353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khodeir M.M., Shabana H.A., Alkhamiss A.S., Rasheed Z., Alsoghair M., Alsagaby S.A., Khan M.I., Fernández N., Al Abdulmonem W. Early prediction keys for COVID-19 cases progression: A meta-analysis. J. Infect. Public Health. 2021;14(5):561–569. doi: 10.1016/j.jiph.2021.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knittel C.R., Miller D.L., Sanders N.J. Caution, drivers! Children present: Traffic, pollution, and infant health. Rev. Econ. Stat. 2016;98(2):350–366. [Google Scholar]
- Lalive R., Luechinger S., Schmutzler A. Does expanding regional train service reduce air pollution? J. Environ. Econ. Manag. 2018;92:744–764. [Google Scholar]
- Leape J. The London congestion charge. J. Econ. Perspect. 2006;20(4):157–176. [Google Scholar]
- Li S. Better lucky than rich? Welfare analysis of automobile licence allocations in Beijing and Shanghai. Rev. Econom. Stud. 2018;85(4):2389–2428. [Google Scholar]
- Li S., Liu Y., Purevjav A.-O., Yang L. Does subway expansion improve air quality? J. Environ. Econ. Manag. 2019;96:213–235. [Google Scholar]
- Li S., Tong L., Xing J., Zhou Y. The market for electric vehicles: Indirect network effects and policy design. J. Assoc. Environ. Resour. Econ. 2017;4(1):89–133. [Google Scholar]
- Lu T., Reis B.Y. Internet search patterns reveal clinical course of COVID-19 disease progression and pandemic spread across 32 countries. Npj Digit. Med. 2021;4(1) doi: 10.1038/s41746-021-00396-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luechinger S. Air pollution and infant mortality: A natural experiment from power plant desulfurization. J. Health Econ. 2014;37:219–231. doi: 10.1016/j.jhealeco.2014.06.009. [DOI] [PubMed] [Google Scholar]
- Lv Z., Lv S. Clinical characteristics and analysis of risk factors for disease progression of COVID-19: A retrospective cohort study. Int. J. Biol. Sci. 2021;17(1):1–7. doi: 10.7150/ijbs.50654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahase E. COVID-19: What do we know about long COVID? Br. Med. J. 2020;370 doi: 10.1136/bmj.m2815. [DOI] [PubMed] [Google Scholar]
- Meng F., Wang J., Li T., Fang C. Pollution characteristics, transport pathways, and potential source regions of PM2.5 and PM10 in Changchun City in 2018. Int. J. Environ. Res. Public Health. 2020;20 doi: 10.3390/ijerph17186585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyashita, L., Foley, G., Semple, S., Grigg, J., 2020. Traffic-derived particulate matter and angiotensin-converting enzyme 2 expression in human airway epithelial cells. Technical report.
- Muehlegger E., Rapson D.S. National Bureau of Economic Research; 2018. Subsidizing Mass Adoption of Electric Vehicles: Quasi-Experimental Evidence from California: Working Paper 25359. [Google Scholar]
- Muller N.Z., Mendelsohn R. Measuring the damages of air pollution in the United States. J. Environ. Econ. Manag. 2007;54(1):1–14. [Google Scholar]
- Muller N.Z., Mendelsohn R. Efficient pollution regulation: Getting the prices right. Amer. Econ. Rev. 2009;99(5):1714–1739. [Google Scholar]
- Neidell M. Information, avoidance behavior, and health: The effect of ozone on asthma hospitalizations. J. Hum. Resour. 2009;44(2):450–478. [Google Scholar]
- Parry I.W.H., Small K.A. Does Britain or the United States have the right gasoline tax? Amer. Econ. Rev. 2005;95(4):1276–1289. [Google Scholar]
- Patanavanich R., Glantz S.A. Smoking is associated with COVID-19 progression: A meta-analysis. Nicotine Tob. Res. 2020;22(9):1653–1656. doi: 10.1093/ntr/ntaa082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persico C.L., Johnson K.R. The effects of increased pollution on COVID-19 cases and deaths. J. Environ. Econ. Manag. 2021;107 doi: 10.1016/j.jeem.2021.102431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pestel N., Wozny F. Health effects of Low Emission Zones: Evidence from German hospitals. J. Environ. Econ. Manag. 2021;109 [Google Scholar]
- Polak S.B., Gool I.C.V., Cohen D., von der Thüsen J.H., van Paassen J. A systematic review of pathological findings in COVID-19: A pathophysiological timeline and possible mechanisms of disease progression. Mod. Pathol. 2020;33(11):2128–2138. doi: 10.1038/s41379-020-0603-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PRISM Parameter-elevation regressions on independent slopes model. Dataset. 2004 [Google Scholar]
- Prunicki M., Cauwenberghs N., Lee J., Zhou X., Movassagh H., Noth E., Lurmann F., Hammond S.K., Balmes J.R., Desai M., Wu J.C., Nadeau K.C. Air pollution exposure is linked with methylation of immunoregulatory genes, altered immune cell profiles, and increased blood pressure in children. Sci. Rep. 2021;11(1):4067. doi: 10.1038/s41598-021-83577-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ragab D., Salah Eldin H., Taeimah M., Khattab R., Salem R. The COVID-19 cytokine storm; What we know so far. Front. Immunol. 2020;11(1446) doi: 10.3389/fimmu.2020.01446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raghunathan T.E. What do we do with missing data? Some options for analysis of incomplete data. Annu. Rev. Public Health. 2004;25:99–117. doi: 10.1146/annurev.publhealth.25.102802.124410. [DOI] [PubMed] [Google Scholar]
- Raifman J., Nocka K., Jones D., Bor J., Lipson S., Jay J., Cole M., Krawczyk N., Benfer E.A., Chan P., Galea S. 2021. COVID-19 US state policy database. www.tinyurl.com/statepolicies. [Google Scholar]
- Ransom M.R., Pope III C.A. External health costs of a steel mill. Contemp. Econ. Policy. 1995;13(2):86–97. [Google Scholar]
- Rees E.M., Nightingale E.S., Jafari Y., Waterlow N.R., Clifford S., Pearson C.A.B., Group C.W., Jombart T., Procter S.R., Knight G.M. COVID-19 length of hospital stay: A systematic review and data synthesis. BMC Med. 2020;18(1) doi: 10.1186/s12916-020-01726-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendeiro A.F., Ravichandran H., Bram Y., Chandar V., Kim J., Meydan C., Park J., Foox J., Hether T., Warren S., Kim Y., Reeves J., Salvatore S., Mason C.E., Swanson E.C., Borczuk A.C., Elemento O., Schwartz R.E. The spatial landscape of lung pathology during COVID-19 progression. Nature. 2021;593(7860):564–569. doi: 10.1038/s41586-021-03475-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders N.J. What doesn’t kill you makes you weaker: Prenatal pollution exposure and educational outcomes. J. Hum. Resour. 2012;47(3):826–850. [Google Scholar]
- Sarkodie S.A., Owusu P.A. Impact of meteorological factors on COVID-19 pandemic: Evidence from top 20 countries with confirmed cases. Environ. Res. 2020;191 doi: 10.1016/j.envres.2020.110101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlenker W., Walker W.R. Airports, air pollution, and contemporaneous health. Rev. Econom. Stud. 2016;83(2):768–809. [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M.G., Borelli M., Palmisani J., Di Gilio A., Torboli V., Fontana F., Clemente L., Pallavicini A., Ruscio M., Piscitelli P., Miani A. SARS-Cov-2RNA found on particulate matter of Bergamo in Northern Italy: First evidence. Environ. Res. 2020;188 doi: 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simeonova E., Currie J., Nilsson P., Walker R. Congestion pricing, air pollution, and children’s health. J. Hum. Resour. 2019;0218 [Google Scholar]
- Smith J.C., Sausville E.L., Girish V., Yuan M.L., Vasudevan A., John K.M., Sheltzer J.M. Cigarette smoke exposure and inflammatory signaling increase the expression of the SARS-CoV-2 receptor ACE2 in the respiratory tract. Dev. Cell. 2020;53(5):514–529.e3. doi: 10.1016/j.devcel.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang C.K. The cost of traffic: Evidence from the London Congestion Charge. J. Urban Econ. 2021;121 [Google Scholar]
- Tsai P.-H., Lai W.-Y., Lin Y.-Y., Luo Y.-H., Lin Y.-T., Chen H.-K., Chen Y.-M., Lai Y.-C., Kuo L.-C., Chen S.-D., Chang K.-J., Liu C.-H., Chang S.-C., Wang F.-D., Yang Y.-P. Clinical manifestation and disease progression in COVID-19 infection. J. Chin. Med. Assoc. 2021;84(1):3–8. doi: 10.1097/JCMA.0000000000000463. [DOI] [PubMed] [Google Scholar]
- Unacast . 2020. Unacast social distancing dataset. https://www.unacast.com/data-for-good. Version from 17 2020. [Google Scholar]
- Vahey G.M., Marshall K.E., McDonald E., Martin S.W., Tate J.E., Midgley C.M., Killerby M.E., Kawasaki B., Herlihy R.K., Alden N.B., and J.E.S. Symptom profiles and progression in hospitalized and nonhospitalized patients with coronavirus disease, colorado, USA, 2020. Emerg. Infect. Diseases. 2021;27(2):385–395. doi: 10.3201/eid2702.203729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B., Chen H., Chan Y.L., Oliver B.G. Is there an association between the level of ambient air pollution and COVID-19? Am. J. Physiol. Lung Cell. Mol. Physiol. 2020;319(3) doi: 10.1152/ajplung.00244.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F., Qu M., Zhou X., Zhao K., Lai C., Tang Q., Xian W., Chen R., Li X., Li Z., He Q., Liu L. The timeline and risk factors of clinical progression of COVID-19 in Shenzhen, China. J. Transl. Med. 2020;18(1) doi: 10.1186/s12967-020-02423-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Zheng X., Chen J. Clinical progression and outcomes of 260 patients with severe COVID-19: An observational study. Sci. Rep. 2021;11(1) doi: 10.1038/s41598-021-82943-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward C.J. It’s an ill wind: The effect of fine particulate air pollution on respiratory hospitalizations. Can. J. Econ. 2015;48(5):1694–1732. [Google Scholar]
- Wolff H. Keep your clunker in the suburb: Low-Emission Zones and adoption of green vehicles. Econ. J. 2014;124(578):F481–F512. [Google Scholar]
- Wu Y., Kang L., Guo Z., Liu J., Liu M., Liang W. Incubation period of COVID-19 caused by unique SARS-CoV-2 strains. JAMA Netw. Open. 2022;5(8) doi: 10.1001/jamanetworkopen.2022.28008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Nethery R.C., Sabath M.B., Braun D., Dominici F. Air pollution and COVID-19 mortality in the United States: Strengths and limitations of an ecological regression analysis. Sci. Adv. 2020;6(45) doi: 10.1126/sciadv.abd4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Li H., Khanna N. Environmental justice and the COVID-19 pandemic: Evidence from New York State. J. Environ. Econ. Manag. 2021;110 doi: 10.1016/j.jeem.2021.102554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Li Y., Zhang A.L., Wang Y., Molina M.J. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc. Natl. Acad. Sci. 2020;117(26):14857–14863. doi: 10.1073/pnas.2009637117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Mu Q. Air pollution and defensive expenditures: Evidence from particulate-filtering facemasks. J. Environ. Econ. Manag. 2018;92:517–536. [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The appendix includes heterogeneity analysis, supplemental sources of information, and additional tables and figures.