Abstract
Background
COVID-19 surge events exacerbated many healthcare facilities’ pre-existing nursing shortages. To address staff shortfalls, nurse leaders adopted a variety of strategies to supplement their workforce.
Purpose
To identify and assess the interplay between board of nursing (BON) emergency guidance and the strategies healthcare facilities adopted to bolster their nursing workforce during peak pandemic periods.
Methods
A national survey of nurse executives, as identified by the American Organization for Nursing Leadership, was conducted. Univariable and multivariable ordinal logistic regression models were used to evaluate the significance of observed trends.
Results
Half of the 391 nurse executives who completed the survey indicated that their facility needed to supplement their RN staffing during peak periods of the COVID-19 pandemic (n = 202, 51.7%). Most relied on hiring local experienced nurses (n = 111) or some combination of travel nurses (n = 61) or support workers (n = 60) to drive a median 10% increase in nurse staffing (n = 153, range 0%–100%). A large proportion of respondents also indicated their facility simply increased the work volume and hours of their current RN staff. Respondents rated retired nurses as significantly more competent relative to licensed new nurse graduates and pre-NCLEX new nurse graduates.
Conclusion
Although the small sample limits the generalizability of these findings, preliminary evidence suggests recently retired nurses and prelicensure nursing students may provide valuable support services in the event of another public health emergency.
Keywords: Workforce management, nursing shortages, regulatory impact, pandemic, COVID-19
The COVID-19 pandemic has profoundly impacted nearly every facet of life, including nursing education and employment. As of March 2023, the World Health Organization (n.d.) reported well over 700 million confirmed cases of the coronavirus and more than six and a half million deaths. Now, as life returns to some semblance of normalcy 3 years after the first confirmed case of COVID-19 in the United States (Centers for Disease Control and Prevention, 2020), it is imperative to examine the efficacy of the numerous strategies employed to combat the global health crisis. Chief among these strategies were the initiatives that nursing leaders, including regulators, around the country undertook to bolster the nursing workforce during COVID-19 surges and to address the influx of patients that, at times, overwhelmed the U.S. healthcare system. To build more resilient health systems for the future, additional research is needed on the effectiveness of BON emergency guidance and, in turn, on employers’ staffing strategies to inform best practices in the event of another public health emergency.
Background
Before the COVID-19 pandemic, many scholars raised concerns over an impending nursing shortage and the likely negative impact of such a shortage on care processes (Buerhaus et al., 2007; Snavely, 2016; Marć et al., 2019). The pandemic, however, accelerated many of these trends for a variety of reasons (e.g., furlough of nursing staff, early retirement, etc.) and thus greatly exacerbated pre-existing workforce issues (Hass et al., 2020). Spetz (2020) noted that the pandemic presented a dual challenge for the U.S. healthcare workforce: (a) a shortage of intensive care unit beds and (b) a deficit of nurses to provide care for the surge of patients. In 2022, the Office of the Assistant Secretary for Planning and Evaluation conducted a detailed examination of the impact of the COVID-19 pandemic on the healthcare workforce and found that many facilities “reported critical staffing shortages over the course of the pandemic, particularly when case numbers were high” (p. 1). Additionally, studies on how the pandemic has amplified healthcare workers’ pre–COVID-19 experiences of burnout and stress (Aiken et al., 2002; McHugh et al., 2011; Aiken et al., 2018; Lasater et al., 2021), largely driven by increased patient volume and acuity (Galanis et al., 2021; Murat et al., 2021; Smiley et al., 2023), are abundant.
Compounding these issues, many prelicensure nursing programs faced enormous difficulty in securing traditional in-person clinical placements, which directly affected the supply and preparedness of new nurse graduates (Emory et al., 2021; Lanahan et al., 2022). Especially during the early stages of the pandemic, many healthcare facilities restricted prelincensure nursing students’ access to reduce the spread of COVID-19 and preserve personal protective equipment for their healthcare staff (Dewart et al., 2020). In response, many prelicensure nursing programs had no choice but to swiftly shift their traditional clinical instruction to simulation- and virtual simulation-based experiences (Benner, 2020; Innovations in Nursing Education, 2020; Kaminski-Ozturk, 2023; Martin, Kaminski-Ozturk, Smiley, et al., 2023). Seymour-Walsh et al. (2020) noted that this shift to simulation-based experiences was particularly challenging for education in the health professions because most programs were typically administered entirely in person; thus, this pivot forced faculty and administrators to rapidly develop online and simulated curricula, often in a manner entirely inconsistent with their academic training (Booth et al., 2016).
To address the dual challenges of disruptions to prelicensure nursing education and insufficient facility staffing, many U.S. boards of nursing (BONs) issued broad emergency guidance. On one hand, they sought to ease restrictions on the replacement of clinical hours with simulation-based experiences for prelicensure nursing students; on the other hand, they sought to broaden the pool of nurses who were permitted to enter or re-enter practice. For prelicensure nursing students, many states adjusted the proportion of clinical hours that could be completed in simulation; in some cases, they waived thresholds entirely (National Council of State Boards of Nursing [NCSBN], 2021a). The patchwork of regulations across the United States was in turn mirrored by nursing programs, which employed an array of strategies to maintain the continuity of students’ clinical education (Emory et al., 2021; Martin, Kaminski-Ozturk, Smiley, et al., 2023). However, emerging evidence suggests that new nurse graduates need more hands-on experience and underscores graduates’ frustration over the apparent mismatch between their clinical experiences during the pandemic and their role as nurses entering the profession during a global health crisis (Crismon et al., 2021; Bultas & L’Ecuyer, 2022; Lanahan et al., 2022).
To further address staffing challenges wrought by the COVID-19 pandemic, many BONs also permitted historically restricted populations of nurses to practice within their jurisdictions (NCSBN, 2021b). Nearly all BONs (n = 46) issued emergency licensing waivers, including every jurisdiction that was not part of the Nurse Licensure Compact (NLC) in 2020, allowing nurses licensed in other jurisdictions to practice within their borders (NCSBN, 2021b). In addition, many states (n = 24) specifically permitted retired nurses, or nurses who held an inactive license, to return to practice (NCSBN, 2021b). Most of these jurisdictions specified these licenses were temporary (e.g., the duration of the public health emergency) and placed specific stipulations on eligibility. For instance, nearly a third of these BONs (n = 7) noted eligible applicants’ licenses could only have been inactive for a period of 5 years or less. Furthermore, to incent applications, many BONs waived associated fees (n = 11) or continuing education requirements (n = 5) and stressed that all reviews would be expedited (n = 9) (NCSBN, 2021b).
In addition, a small number of BONs (n = 6) also explicitly waived or extended license expiration dates or permitted prelicensure nursing students or new graduates of nursing programs approved by their jurisdiction’s BON (n = 8) to temporarily practice as nurses (NCSBN, 2021b; Mississippi State Board of Nursing, 2020). In such instances, BONs again explicitly stated certain eligibility criteria. For current prelicensure students, applicants often needed to be in good academic standing at an approved nursing education program. Some BONs also stipulated that students had to have advanced standing in their program (e.g., senior) and must have completed certain minimum coursework, such as fundamentals and pharmacology. Regarding new graduates who had not yet taken the NCLEX-RN, in order to practice, jurisdictions often noted they had to have graduated from an approved program, and some further indicated they needed to have already secured their authorization to test (NCSBN, 2021b).
Work completed before the COVID-19 pandemic already illustrated employers’ unease with the quality of new nurse graduates’ clinical preparation and, thus, their preference for hiring more experienced frontline workers (Budden, 2011). To address the dual challenges presented by potential deficiencies in prelicensure students’ clinical education and regional workforce shortages, in 2020, NCSBN recommended a national practice–academic partnership model (NCSBN, 2020). The objective of this model was to provide nursing students with in-person clinical experiences during the pandemic and to provide employers an opportunity to alleviate staffing shortages (Spector et al., 2021). Then, now, and moving forward, such partnerships are critical not just to support and improve the clinical training of prelicensure students but also to mitigate the need for extra mentoring and continuing education for recent graduates (Smith et al., 2021; Michel et al., 2021; Crismon et al., 2021; Bultas & L’Ecuyer, 2022; Lanahan et al., 2022). Recognizing the need for additional insight into how healthcare facilities adapted their hiring practices during the COVID-19 pandemic in light of BON emergency guidance, NCSBN developed a study to address the following three primary research questions:
-
a.
What strategies did healthcare facilities that experienced workforce shortages during the COVID-19 pandemic implement to address these shortfalls?
-
b.
How effective do nurse executives perceive their facilities’ strategies to have been in addressing their staffing needs?
-
c.
What lessons emerged, if any, that can be used to inform future regulatory guidance in the event of another public health crisis?
Methodology
Study Sample
In this cross-sectional study, we surveyed nurse executives from across the United States regarding their experiences in hiring nurses to address staffing shortages during the COVID-19 pandemic. As key informants, nurse executives’ responses were used to represent facility policy in this study. A total of 8,272 active (e.g., did not result in a hard bounce) nurse executive contacts (titles included chief nursing officer, vice president of nursing, director of nursing, manager of nursing, assistant manager of nursing, supervisor of nursing, etc.) from 6,238 healthcare facilities were purchased from the American Organization for Nursing Leadership (AONL). Of the eligible participants, an estimated 1,331 executives reviewed the introductory email for an open rate of 16.1%. In total, 391 of the nurse executives who opened the invitation submitted a response for a final completion rate of 29.4%. In total, responses from executives representing 375 different institutions across all 50 states and the District of Columbia were included in the analysis (Figure 1 ). Prior to commencing any outreach, the study was reviewed and approved by the Western Institutional Review Board.
FIGURE 1.
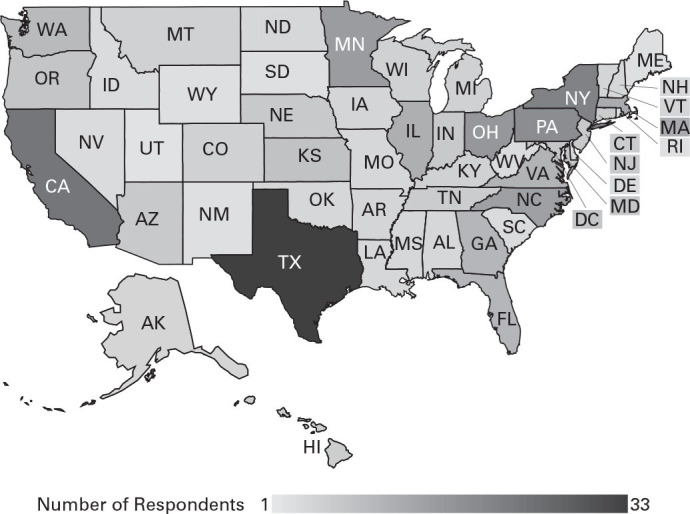
Distribution of Respondents to the Nurse Executive Survey
Study Design
Prior to final dissemination, an initial draft of the survey was distributed to a randomly selected group of 100 AONL contacts (approximately 1% of the mailing list sample) to complete the survey and provide detailed feedback to establish internal consistency and face validity. Participants who completed this step were compensated with a $10 Visa electronic gift card in recognition of their efforts. Based on their feedback, final revisions were made to the instrument to improve clarity.
The final survey consisted of 39 items that were primarily divided into three domains: (a) demographic and facility information, (b) workforce trends, and (c) hiring strategies. The primary focus of the first domain was on the experience (e.g., number of years as hiring manager) and educational background of the nurse executive, but information on the healthcare setting was also solicited to supplement data purchased from AONL. The workforce trends section included queries on the timing and magnitude of decisions to increase RN staffing during the COVID-19 pandemic, as well as questions regarding the type and efficacy of strategies to bolster the ranks of frontline nurses to treat COVID-19 patients specifically. Finally, the domain on hiring strategies focused on facilities’ decisions regarding when and to what extent to employ prelicensure nursing students, new nurse graduates (including those who had not yet taken the NCLEX-RN), and retired nurses (or those with previously inactive licenses). In this study, “pre-NCLEX new nurse graduates” are defined as graduates of an approved nursing program who have not yet sat for the NCLEX-RN.
This confidential online survey was administered using Qualtrics (Provo, UT). An introductory email with a link to the survey was sent to eligible participants in November 2021. Weekly scheduled reminders were sent until the survey closed in early January 2022. To incentivize participation, all eligible participants who submitted a survey response were entered into a raffle. Three participants were then selected at random to receive prizes; each prize had a monetary value of $185. Survey findings were then augmented with embedded metadata from the acquired contact list, including the size and geographic location of the nurse executive’s healthcare facility. Multiple respondents from a single institution were allowed, and responses of nurse executives from the same institution were compared for consistency regarding institutional information.
Nonresponse Bias Analysis
Despite the large number of institutions and geographic diversity of our sample, the low open rate drove a final response rate of just 4.7%. Therefore, to ensure that the respondents were representative of the original sample, a formal nonresponse analysis was run including all available institutional characteristics (Table 1 ). There were two levels to the analysis. First, we compared all respondents to nonresponders. Second, we compared all respondents who indicated they increased RN staffing levels during COVID-19 surge events to the remaining sample. The latter comparison was included because that cohort constituted the sample for the model-based analyses. Categorical variables were compared using Pearson chi-squared tests. For group comparisons on continuous outcomes, the nonparametric analog to the independent samples t test, the Wilcoxon rank sum test, was employed to account for the heavily skewed nature of institutional employee and annual revenue reporting. As the descriptive results suggest, there were no statistically significant differences found between the nonresponder group, and the two study groups (all p > .05), which alleviated concerns regarding the representativeness of the retained sample.
TABLE 1.
Nonresponse Bias Analysis: Employer Characteristics by Survey Response Status
| Employer Characteristics | Nonrespondents (N = 7,881) |
All Respondents (N = 391) |
Hiring Surge Respondents (N = 202) |
|---|---|---|---|
| NLC Status of Jurisdiction | |||
| Awaiting NLC Membership | 899 (11.4%) | 49 (12.5%) | 24 (11.9%) |
| NLC Member | 4,250 (53.9%) | 208 (53.2%) | 108 (53.5%) |
| Not NLC Member | 2,732 (34.7%) | 134 (34.3%) | 70 (34.6%) |
| U.S. Census Region | |||
| Northeast | 1,469 (18.6%) | 78 (19.9%) | 39 (19.3%) |
| Midwest | 1,972 (25.0%) | 102 (26.1%) | 52 (25.7%) |
| Pacific | 38 (0.5%) | 4 (1.0%) | 3 (1.4%) |
| South | 2,772 (35.2%) | 132 (33.8%) | 74 (36.6%) |
| West | 1,630 (20.7%) | 75 (19.2%) | 34 (16.8%) |
| No. of Employees, Mdn (range) | 10 (8–950) | 11 (8–850) | 15 (8–825) |
| Annual Revenue, in Millions, Mdn (range) | $0.9 ($0.4–$4.1) | $1.2 ($0.5–$4.6) | $1.6 ($0.5–$6.9) |
| Job Function | |||
| DON/CNO | 2,202 (27.9%) | 100 (25.6%) | 58 (28.7%) |
| Assistant/associate DON/CNO | 4,188 (53.1%) | 226 (57.8%) | 109 (54.0%) |
| Manager/supervisor | 895 (11.4%) | 48 (12.3%) | 26 (12.9%) |
| Other | 596 (7.6%) | 17 (4.4%) | 9 (1.4%) |
Notes. CNO = chief nursing officer; DON = director of nursing; NLC = Nurse Licensure Compact. Categorical results presented as n (%). Continuous variables presented as median (range).
Dependent Variable
The goal of this study was to better understand and evaluate the interplay between BON emergency guidance and various strategies implemented by healthcare facilities to address RN staffing shortfalls. Thus, the primary dependent variable used in the analysis was the frequency with which facilities used key personnel to care for COVID-19 patients specifically. The variable was measured on a five-point Likert scale, ranging from 1, which indicated a provider “never cared for COVID-19 patients,” to 5, which indicated that the provider “always cared for COVID-19 patients.” This variable provided insight into not only how but also to what extent each cohort (e.g., prelicensure nursing students, pre-NCLEX new graduates, recently licensed new graduates, and re-activated retirees) was utilized during peak COVID-19 periods. By utilizing the original scaling, nuances beyond simpler dichotomous outcomes (e.g., used/not used to treat COVID-19–positive patients) were achievable, facilitating a more detailed examination of the variables of interest.
Statistical Analysis
A descriptive summary of the sample is provided, with categorical variables presented using counts and proportions; continuous variables are expressed as means and standard deviations or medians and ranges, as appropriate. As repeated measures did not factor into the statistical analyses, fixed-effects univariable and multivariable ordinal logistic regression models were used to determine the significance of observed trends. A multinomial distribution was specified for each model with cumulative logit links to determine the odds ratio for each predictor. The proportional odds assumption was assessed and retained for all reported effects (Agresti, 2013). All independent predictors with p ≤ .20 were considered for inclusion in the multivariable model, and a stepwise approach was used to identify issues of multicollinearity. The final composition of the multivariable model was determined to achieve the most parsimonious and informative combination of available characteristics across all domains. As this study was an analysis of nurse executives, only respondents with a job function of manager/supervisor or above were included in the modeling. The threshold for statistical significance was set at p ≤ .05, and all analyses were conducted using SAS version 9.4 (Cary, NC).
Results
A total of 391 participants representing 375 unique institutions completed the survey (Table 2 ). In line with the outreach strategy, more than 80% of respondents self-identified as a director or chief of nursing (n = 326, 83.4%), including associates and assistants, followed by manager or supervisor (n = 48, 12.3%). There was a near-even distribution by U.S. Census region, and all 50 states and the District of Columbia were represented. Most institutions were located in NLC member jurisdictions (n = 208, 53.2%). Respondents reported annual operating budgets of approximately $1.2 million and a median of 11 employees per facility (range, 8–850). Among all respondents, just over half (n = 202, 51.7%) indicated they had increased their RN staffing levels to some degree in response to COVID-19 surge events.
TABLE 2.
Descriptive Summary of Employer Sample (N = 391)
| Employer Characteristics | Total N | Total |
|---|---|---|
| U.S. Census Region | 391 | |
| Northeast | 78 (19.9%) | |
| Midwest | 102 (26.1%) | |
| Pacific | 4 (1.0%) | |
| South | 132 (33.8%) | |
| West | 75 (19.2%) | |
| Job Function | 391 | |
| DON/CNO | 100 (25.6%) | |
| Asst/Assoc DON/CNO | 226 (57.8%) | |
| Manager/Supervisor | 48 (12.3%) | |
| Other | 17 (4.4%) | |
| NLC Status of Jurisdiction | 391 | |
| Awaiting NLC Membership | 49 (12.5%) | |
| NLC Member | 208 (53.2%) | |
| Not NLC Member | 134 (34.3%) | |
| Annual Revenue, in Millions, Mdn (range) | 223 | $1.2 ($0.5–$4.6) |
| No. Employees at Facility, Mdn (range) | 320 | 11 (8–850) |
| Pandemic RN Hiring | 391 | |
| Yes | 202 (51.7%) | |
| No | 189 (48.3%) |
Note. Assoc = associate; Asst = assistant; CNO = chief nursing officer; DON = director of nursing; NLC = Nurse Licensure Compact; RN = registered nurse. Valid N for each item varies based on observed nonresponse rates. Categorical results presented as n (%). Continuous variables presented as median (range).
Nurse executives from these facilities reported a median increase of 10% in nurse staffing (range, 0%–100%, Table 3 ). On average, respondents who represented these institutions reported being involved in the process of evaluating and hiring new nurses for approximately 12 years (M = 11.7, SD = 9.1). Most respondents had either a baccalaureate (n = 62, 44.6%) or some level of graduate training (master’s degree: n = 50, 36.0%; doctoral degree: n = 10, 7.2%). Three-quarters of respondents (n = 101, 72.7%) identified registered nurse (RN) as their highest nursing credential. A plurality of respondents worked in a hospital setting (n = 47, 33.8%), but notable proportions also reported long-term care (n = 19, 13.7%) or outpatient settings (n = 18, 12.9%).
TABLE 3.
Descriptive Summary of Employers That Increased RN Staffing to Address COVID-19 Surge Events (N = 202)
| Employer Characteristics | Total N | Total |
|---|---|---|
| % Increase RN Staff, Mdn (range) | 153 | 10% (0%–100%) |
| Tenure of Hiring Manager, y, M (SD) | 126 | 11.7 (9.1) |
| Highest Academic Credential of Hiring Manager | 139 | |
| Associate degree | 17 (12.2%) | |
| Baccalaureate degree | 62 (44.6%) | |
| Master’s degree | 50 (36.0%) | |
| Doctoral degree | 10 (7.2%) | |
| Highest Nursing Credential of Hiring Manager | 139 | |
| LPN/LVN | 4 (2.9%) | |
| RN | 101 (72.7%) | |
| APRN | 23 (16.6%) | |
| DNP | 5 (3.6%) | |
| Not a nurse | 6 (4.3%) | |
| Facility Type | 139 | |
| Hospital | 47 (33.8%) | |
| Long-term care home | 19 (13.7%) | |
| Outpatient clinic | 18 (12.9%) | |
| Rural health clinic | 12 (8.6%) | |
| Home health agency | 8 (5.8%) | |
| Private practice | 8 (5.8%) | |
| Assisted living facility | 5 (3.6%) | |
| Hospice | 5 (3.6%) | |
| Public health | 4 (2.9%) | |
| Urgent care facility | 2 (1.4%) | |
| Retail health clinic | 1 (0.7%) | |
| Other | 10 (7.2%) |
Note. APRN = advanced practice registered nurse; DNP = doctor of nursing practice; LPN/LVN = licensed practical nurse/licensed vocational nurse; RN = registered nurse. Valid N for each item varies based on observed nonresponse rates. Categorical results presented as n (%). Continuous variables presented as median (range) or mean (SD).
Most nurse executives indicated they hired local experienced nurses (n = 111, 70.3%) to address staffing shortfalls. However, many respondents also indicated their facility simply increased the work volume and hours of their current RN staff (n = 67, 42.4%) to address COVID-19 surge events (Table 4 ). Others hired some combination of travel nurses (n = 61, 38.6%), support workers (n = 60, 38.0%), additional licensed practical nurses/licensed vocational nurses (n = 47, 29.7%), and/or shifted nonclinical nurses in administrative positions to patient care roles (n = 46, 29.1%). When asked to rate the effectiveness of these various strategies, there was broad (albeit lackluster) synchrony across executives’ responses, with all but one category (“Other”) receiving a median rating of 2 (“somewhat effective”). Nearly half of nursing leaders reported being moderately to extremely concerned about patient safety (n = 74, 49.3%) due to the range of strategies employed. For those who sought external nurses to supplement their staffing, 39.3% (n = 29) agreed that their state’s participation in the NLC facilitated their efforts.
TABLE 4.
Employers’ Reported Strategies to Increase RN Staffing Levels During COVID-19 Surge Events
| Total N | Total | |
|---|---|---|
| Strategies for Supporting RN Staffa | 158 | |
| Hired local experienced nurses who applied for positions | 111 (70.3%) | |
| Increased work hours for current staff | 67 (42.4%) | |
| Hired travel nurses | 61 (38.6%) | |
| Hired support workers (e.g., nursing assistants) | 60 (38.0%) | |
| Hired additional LPNs/LVNs | 47 (29.7%) | |
| Shifted nonclinical nurses to patient care roles | 46 (29.1%) | |
| Shifted staff from one facility to another | 30 (19.0%) | |
| Hired pre-NCLEX new graduates | 16 (16.5%) | |
| Hired prelicensure students | 13 (8.2%) | |
| Hired retired nurses | 13 (8.2%) | |
| Other | 11 (7.0%) | |
| Patient Safety Concerns | 150 | |
| Not at all concerned | 24 (16.0%) | |
| Slighted concerned | 52 (34.7%) | |
| Moderately concerned | 39 (26.0%) | |
| Very concerned | 21 (14.0%) | |
| Extremely concerned | 14 (9.3%) | |
| NLC Facilitated Nurse Hiring | 74 | |
| Strongly disagree | 9 (12.2%) | |
| Disagree | 4 (5.4%) | |
| Unsure | 32 (43.2%) | |
| Agree | 20 (27.0%) | |
| Strongly agree | 9 (12.2%) |
Notes. LPNs/LVNS = licensed practical nurses/licensed vocational nurses; NLC = Nurse Licensure Compact; RN = registered nurse. Valid N for each item varies based on observed nonresponse rates. Categorical results presented as n (%).
Respondents asked to select all that apply.
In line with existing literature, the majority of respondents to this national survey (n = 115 of 143, 80.4%) likewise indicated that prelicensure nursing students were not allowed onsite during peak COVID-19 surges. Of the few facilities that did (n = 28, 19.6%), half (n = 15, 53.6%) did so only to allow students to complete their core clinical requirements. Eleven executives (39.3%) also indicated prelicensure nursing students served as paid support staff at their facilities as part of a practice–academic partnership. Even in these cases, most (n = 15, 53.6%) indicated prelicensure students were never or rarely allowed to provide direct care to COVID-19 patients.
The independent associations between facility characteristics, hiring strategies, and how direct patient care to those with COVID-19 was coordinated were initially the focus of the analysis (Table 5 ). Overall, there was a trend toward pre-NCLEX new nurse graduates (OR: 2.83, 95% CI: 1.23–6.52, p = .01) and licensed new nurse graduates (OR: 2.28, 95% CI: 1.12–4.65, p = .02) being more likely to care for COVID-19 patients compared to prelicensure nursing students. Across all other staff types, including retired nurses or those who previously held an inactive license, there was less variation. Similarly, for every 25% increase in a facility’s RN staffing, a nurse executive was 2.18 times more likely to report that recently hired staff coordinated COVID-19 care (95% CI: 1.31–3.65, p < .001). Respondents who reported heightened patient concerns (“moderate” or above) were also 2.77 times more likely to indicate new staff were coordinating care for COVID-19 patients (95% CI: 1.28–5.99, p = .01). All observed effects were sustained on multivariable analysis after further adjustments for other important covariates.
TABLE 5.
Univariable and Multivariable Models Examining COVID-19 Care
| Independent Variables | Coordination of COVID-19 Care |
|||
|---|---|---|---|---|
| OR (95% CI) | p | AOR (95% CI) | p | |
| Strategies to Address Staff Shortages | .11 | .06 | ||
| Prelicensure nursing students (Ref) | - | - | ||
| Pre-NCLEX new nurse graduates | 2.83 (1.23–6.52) | .01 | 2.91 (1.30–6.50) | .01 |
| Licensed new nurse graduates | 2.28 (1.12–4.65) | .02 | 2.47 (1.16–5.23) | .02 |
| Retired nurse, or nurse with an inactive license | 1.81 (0.60–5.49) | .30 | 2.49 (0.69–8.90) | .16 |
| NLC Status | .19 | .21 | ||
| Awaiting | 0.62 (0.24–1.63) | .33 | 0.55 (0.17–1.80) | .32 |
| Yes | 1.38 (0.60–3.19) | .45 | 1.31 (0.66–3.72) | .31 |
| No (Ref) | - | - | ||
| % Increase RN Staff (Unit = 25%) | 2.18 (1.31–3.65) | <.001 | 1.80 (1.07–3.04) | .01 |
| # Employees at Facility (Unit = 10) | 1.02 (0.98–1.06) | .31 | ||
| # of Strategies Employed (Unit = 1) | 1.12 (0.91–1.38) | .28 | ||
| Avg. Effectiveness of Strategies (Unit = 1) | 1.34 (0.94–1.91) | .15 | 1.35 (0.94–1.92) | .13 |
| Patient Safety Concerns (Ref = “None or Slight”) | 2.77 (1.28–5.99) | .01 | 2.43 (1.07–5.49) | .04 |
| Clinical Competency (Unit = 1) | 1.12 (0.95–1.33) | .19 | ||
Note. AOR = adjusted odds ratio; NLC = Nurse Licensure Compact; RN = registered nurse. The final composition of the multivariable model was determined to achieve the parsimonious and informative combination of available characteristics across all domains. Because prelicensure nursing students’ clinical competency was not directly evaluated, this variable was not included in the multivariable model.
When asked to compare pre-NCLEX new nurse graduates, licensed new nurse graduates, and retired/inactive nurses on clinical competence (ranging from 1, which indicated a provider was “among the weakest,” to 10, they were “among the best”), nurse executives were significantly more likely to rate the knowledge and skills of the recently retired workforce higher. Nurse executives rated retired nurses with a median competence score of 8.5 (interquartile range [IQR]: 5–10), or “among the best”), whereas they reported significantly lower scores for licensed new nurses (Mdn: 5.5, IQR: 4–7) and pre-NCLEX new nurse graduates (Mdn: 4.5, IQR: 3–7) (p = .03).
Discussion
Concerns over regional nursing shortages across the United States long predated the pandemic (Buerhaus et al., 2007; Snavely, 2016; Marć et al., 2019), but COVID-19 greatly exacerbated pre-existing workforce issues (Hass, 2020; Galanis et al., 2021; Murat et al., 2021). The critical deficit of nurses to provide care for the surge of acutely ill patients during the pandemic (Spetz, 2020; Office of the Assistant Secretary for Planning and Evaluation, 2022) has now morphed into a chronic and defining characteristic of the U.S. healthcare system (Smiley et al., 2023). In light of widespread disruptions to nurse staffing and education during peak pandemic periods, many BONs issued broad emergency guidance to provide nursing education programs and employers alike sufficient flexibility to tailor solutions appropriate to their local contexts. The findings from this study shed light on the interplay between BON emergency guidance and employer staffing and, in doing so, inform strategies in the event of a future public health crisis.
To assist healthcare facilities in combatting the pandemic, BONs sought to broaden the pool of nurses who were permitted to enter or re-enter practice (NCSBN, 2021b). Strategies included issuing emergency licensing waivers (n = 46) to facilitate cross-border care, permitting retired nurses or nurses who held an inactive license to return to practice (n = 24), and explicitly waiving or extending license expiration dates (n = 6). In turn, this allowed respondents to our survey to try a multitude of different strategies (M: 2.40, range: 0–4) to augment capacity. In line with prior research (Budden, 2011), most facilities in our study preferred to hire experienced licensed nurses (111 of 158, 70.3%) when possible, while notably smaller proportions, aided by emergency orders, reported recruiting from previously restricted populations, such as pre-NCLEX new nurse graduates (26 of 158, 16.5%), retired nurses (13 of 158, 8.2%), or prelicensure nursing students (13 of 158, 8.2%).
In this national study, approximately half of the nurse executives (n = 202), who represented 198 institutions across 48 states, reported their facility had to increase their staffing to address acute RN shortages (Mdn: 10%, range: 0–100%) during peak COVID-19 periods. Nurse executives indicated that equal proportions of licensed new graduates (21.2%), pre-NCLEX new graduates (23.1%), and retired nurses (25.0%) coordinated direct care for COVID-19 patients. Across these three groups, nurse executives were significantly more likely to rate the knowledge and skills of the recently retired workforce higher. This result possibly reflects two realities. One, retired nurses were perhaps an underutilized resource during peak COVID-19 periods, and efforts to recruit former RNs fitting this profile, particularly in their first few years of retirement, during future crises may pay dividends. Two, it may illustrate potential deficiencies nurse executives identified in early career nurses’ preparation.
Although both conclusions may have merit, emerging literature on the impact of COVID-19 on prelicensure nursing education certainly highlights potential deficiencies in new nurse graduates’ clinical preparation (Crismon et al., 2021; Bultas & L’Ecuyer, 2022; Lanahan et al., 2022). Especially during the early stages of the pandemic, many healthcare facilities restricted prelincensure nursing students’ access (Dewart et al., 2020), forcing nursing programs to shift their traditional clinical placements to simulation- and virtual simulation-based experiences (Benner, 2020; Innovations in Nursing Education, 2020; Kaminski-Ozturk, 2023; Martin, Kaminski-Ozturk, Smiley, et al., 2023). The challenges this posed to nursing education programs (Booth et al., 2016; Seymour-Walsh et al., 2020) and students (Crismon et al., 2021; Konrad et al., 2021; Michel et al., 2021; Smith et al., 2021; Bultas & L’Ecuyer, 2022; Lanahan et al., 2022) alike have been widely discussed. Approximately 4 in 5 respondents to this national survey indicated that prelicensure nursing students were not allowed onsite during peak COVID-19 surges. Of the few facilities that did, most did so only to allow students to complete their core clinical requirements.
Despite early efforts by many, including NCSBN, to push for a national practice–academic partnership model in 2020, survey response trends indicate limited progress on the issue (NCSBN, 2020; Spector et al., 2021). Executives representing only 11 facilities indicated prelicensure nursing students served as paid support staff during the pandemic. Furthermore, even among the small cadre of respondents who indicated their facility allowed prelicensure students onsite, most indicated they were never or rarely allowed to provide direct care to COVID-19 patients. Rather, nurse executives reported that prelicensure nursing students often staffed vaccine clinics, rotated on general or medical-surgical units, or assisted with patient screening or transfers. This fact, if truly more widespread, may in part account for new nurse graduates’ frustration over the apparent mismatch between their clinical experiences and their role as nurses entering the profession during a global health crisis (Crismon et al., 2021).
Limitations
There are several limitations to the current analysis that bear further consideration. First and foremost, despite the large (institution N = 375) and geographically diverse (all 50 states and the District of Columbia) respondent pool, the low open (16.1%), completion (29.4%), and response (4.7%) rates limit our ability to broadly generalize these findings. While the results of a formal nonresponse analysis suggested strong representation among our retained sample, further research on this topic is warranted to confirm these preliminary results. In addition, COVID-19 restrictions, particularly those issued during the early stages of the pandemic, varied considerably by region both in terms of their reach and timing. Similarly, as documented in the literature, the location and severity of nursing workforce shortages ranged widely as well, suggesting the compounding effect of the pandemic was likely also not uniform. This variability and the resulting durability of the observed trends reported in this analysis were difficult to capture in the modeling. Finally, the trends documented in this study are correlational and do not support causal inference.
Conclusion
The COVID-19 pandemic has profoundly impacted nearly every facet of life, including nursing education and employment. Nursing shortages that long predated the pandemic and nurses’ experience of burnout and stress during COVID-19 surges have the potential to contribute to chronic workforce issues (Martin, Kaminski-Ozturk, O'Hara, et al., 2023; Smiley et al., 2023). The results of this study suggest that recently retired nurses and prelicensure nursing students were potentially underutilized during the pandemic, but they may provide valuable support services in the event of another public health emergency. Furthermore, greater adoption of a national practice–academic partnership model may serve as a viable solution to address the dual challenges of disruptions to prelicensure nursing education and insufficient facility staffing in the event that in-person clinical placements once again need to be severely restricted. By critically examining the intersection, or lack thereof, of BON emergency guidance and employers’ resulting staffing strategies, regulators and nurse executives can play critical roles in building more resilient health systems fit for the future.
Footnotes
Conflicts of Interest: None.
References
- Agresti A. (3rd ed.). John Wiley & Sons, Inc; 2013. Categorical data analysis. [Google Scholar]
- Aiken L.H., Clarke S.P., Sloane D.M., Sochalski J., Silber J.H. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aiken L.H., Sloane D.M., Barnes H., Cimiotti J.P., Jarrín O.F., McHugh M.D. Nurses’ and patients’ appraisals show patient safety in hospitals remains a concern. Health Affairs. 2018;37(11):1744–1751. doi: 10.1377/hlthaff.2018.0711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benner P. Finding online clinical replacement solutions during the COVID-19 pandemic. Educating Nurses. 2020, March 19 https://www.educatingnurses.com/author/pbenner/page/4/ [Google Scholar]
- Booth T.L., Emerson C.J., Hackney M.G., Souter S. Preparation of academic nurse educators. Nurse Education in Practice. 2016;19:54–57. doi: 10.1016/j.nepr.2016.04.006. [DOI] [PubMed] [Google Scholar]
- Budden J.S. A survey of nurse employers on professional and practice issues affecting nursing. Journal of Nursing Regulation. 2011;1(4):17–25. doi: 10.1016/S2155-8256(15)30312-4. [DOI] [Google Scholar]
- Buerhaus P.I., Donelan K., Ulrich B.T., Norman L., DesRoches C., Dittus R. Impact of the nurse shortage on hospital patient care: Comparative perspectives. Health Affairs. 2007;26(3):853–862. doi: 10.1377/hlthaff.26.3.853. [DOI] [PubMed] [Google Scholar]
- Bultas M.W., L’Ecuyer K.M. A longitudinal view of perceptions of entering nursing practice during the COVID-19 pandemic. The Journal of Continuing Education in Nursing. 2022;53(6):256–262. doi: 10.3928/00220124-20220505-07. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention First travel-related case of 2019 novel coronavirus detected in the United States [Press release] 2020, January 21. https://www.cdc.gov/media/releases/2020/p0121-novel-coronavirus-travel-case.html
- Crismon D., Mansfield K.J., Hiatt S.O., Christensen S.S., Cloyes K.G. COVID-19 pandemic impact on experiences and perceptions of nurse graduates. Journal of Professional Nursing. 2021;27(5):857–865. doi: 10.1016/j.profnurs.2021.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewart G., Corcoran L., Thirsk L., Petrovic K. Nursing education in a pandemic: Academic challenges in response to COVID-19. Nurse Education Today. 2020;92 doi: 10.1016/j.nedt.2020.104471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emory J., Kippenbrock T., Buron B. A national survey of the impact of COVID-19 on personal, academic, and work environments of nursing students. Nursing Outlook. 2021;69(6):1116–1125. doi: 10.1016/j.outlook.2021.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanis P., Vraka I., Fragkou D., Bilali A., Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Advanced Nursing. 2021;77(8):3286–3302. doi: 10.1111/jan.14839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas S., Swan B.A., Jessie A.T. The impact of the coronavirus pandemic on the global nursing workforce. Nursing Economic$ 2020;38(5):231–237. [Google Scholar]
- Innovations in nursing education: Recommendations in response to the COVID-19 pandemic. 2020, March 30. https://nepincollaborative.org/wp-content/uploads/2020/08/Nursing-Education-and-COVID-Pandemic-March-30-2020-FINAL.pdf
- Kaminski-Ozturk N., Martin B. Prelicensure nursing clinical simulation and regulation during the COVID-19 pandemic (in press). Journal of Nursing. Regulation. 2023 doi: 10.1016/S2155-8256(23)00065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad S., Fitzgerald A., Deckers C. Nursing fundamentals—Supporting clinical competency online during the COVID-19 pandemic. Teaching and Learning in Nursing. 2021;16(1):53–56. doi: 10.1016/j.teln.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanahan M., Montalvo B., Cohn T. The perception of preparedness in undergraduate nursing students during COVID-19. Journal of Professional Nursing. 2022;42:111–121. doi: 10.1016/j.profnurs.2022.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasater K.B., Aiken L.H., Sloane D.M., French R., Martin B., Reneau K., Alexander M., McHugh M.D. Chronic hospital nurse understaffing meets COVID-19: An observational study. BMJ Quality & Safety. 2021;30(8):639–647. doi: 10.1136/bmjqs-2020-011512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marć M., Bartosiewicz A., Burzyńska J., Chmiel Z., Januszewicz P. A nursing shortage—A prospect of global and local policies. International Nursing Review. 2019;66(1):9–16. doi: 10.1111/inr.12473. [DOI] [PubMed] [Google Scholar]
- Martin B., Kaminski-Ozturk N., O’Hara C., Smiley R. Examining the impact of the COVID-19 pandemic on burnout and stress among U.S. nurses. Journal of Nursing Regulation. 2023;14(1):4–12. doi: 10.1016/S2155-8256(23)00063-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin B., Kaminski-Ozturk N., Smiley R., Spector N., Silvestre J., Bowles W., Alexander M. Assessing the impact of the COVID-19 pandemic on nursing education: A national study of prelicensure RN programs. Journal of Nursing Regulation. 2023;14(S1):S1–S68. doi: 10.1016/S2155-8256(23)00041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh M.D., Kutney-Lee A., Cimiotti J.P., Sloane D.M., Aiken L.H. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems in patient care. Health Affairs. 2011;30(2):202–210. doi: 10.1377/hlthaff.2010.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michel A., Ryan N., Mattheus D., Knopf A., Abuelezam N.N., Stamp K., Branson S., Hekel B., Fontenot H. Undergraduate nursing students’ perceptions on nursing education during the 2020 COVID-19 pandemic: A national sample. Nursing Outlook. 2021;69(5):903–912. doi: 10.1016/j.outlook.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mississippi State Board of Nursing Mississippi State Board of Nursing proclamation. 2020, March 16. https://www.msbn.ms.gov/sites/default/files/Board%20of%20Nursing%20Proclamation_1.pdf
- Murat M., Köse S., Savaşer S. Determination of stress, depression, and burnout levels of front-line nurses during the COVID-19 pandemic. International Journal of Mental Health Nursing. 2021;30(2):533–543. doi: 10.1111/inm.12818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Council of State Boards of Nursing Policy brief: US nursing leadership supports practice/academic partnerships to assist the nursing workforce during the COVID-19 crisis. 2020. https://www.ncsbn.org/public-files/PolicyBrief_US_Nursing_Leadership_COVID19_updated.pdf
- National Council of State Boards of Nursing NCSBN’s environmental scan: COVID-19 and its impact on nursing and regulation. Journal of Nursing Regulation. 2021;11(4S):S1–S36. doi: 10.1016/S2155-8256(21)00002-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Council of State Boards of Nursing State response to COVID-19 as of October 13, 2021. 2021. https://www.ncsbn.org/State_COVID-19_Response.pdf Retrieved May 1, 2021, from.
- Office of the Assistant Secretary for Planning and Evaluation Impact of the COVID-19 pandemic on the hospital and outpatient clinician workforce. 2022, May 3. https://aspe.hhs.gov/sites/default/files/documents/9cc72124abd9ea25d58a22c7692dccb6/aspe-covid-workforce-report.pdf U.S. Department of Health and Human Services.
- Seymour-Walsh A.E., Bell A., Weber A., Smith T. Adapting to a new reality: COVID-19 coronavirus and online education in the health professions. Rural and Remote Health. 2020;20(2) doi: 10.22605/RRH6000. [DOI] [PubMed] [Google Scholar]
- Smiley R.A., Allgeyer R.L., Shobo Y., Lyons K.C., Letourneau R., Zhong E., Kaminski-Ozturk N., Alexander M. The 2022 national nursing workforce survey (in press) Journal of Nursing Regulation. 2023;14(2S):S1–S92. [Google Scholar]
- Smith S.M., Buckner M., Jessee M.A., Robbins V., Horst T., Ivory C.H. Impact of COVID-19 on new graduate nurses’ transition to practice: Loss or gain? Nurse Educator. 2021;46(4):209–214. doi: 10.1097/NNE.0000000000001042. [DOI] [PubMed] [Google Scholar]
- Snavely T.M. A brief economic analysis of the looming nursing shortage in the United States. Nursing Economic$ 2016;34(2):98–101. [PubMed] [Google Scholar]
- Spector N.M., Buck M., Phipps S. A new framework for practice–academic partnerships during the pandemic—and into the future. American Journal of Nursing. 2021;121(12):39–44. doi: 10.1097/01.naj.0000803192.68710.8f. [DOI] [PubMed] [Google Scholar]
- Spetz J. There are not nearly enough nurses to handle the surge of coronavirus patients: Here’s how to close the gap quickly. Health Affairs Forefront. 2020, March 31 doi: 10.1377/forefront.20200327.714037. [DOI] [Google Scholar]
- World Health Organization. (n.d.). WHO coronavirus (COVID-19) dashboard. Retrieved March 12, 2023, from https://covid19.who.int/


