Abstract
Background
The effect of noninvasive respiratory support (NRS), including high-flow nasal oxygen, bi-level positive airway pressure and continuous positive airway pressure (noninvasive ventilation (NIV)), for preventing and treating post-extubation respiratory failure is still unclear. Our objective was to assess the effects of NRS on post-extubation respiratory failure, defined as re-intubation secondary to post-extubation respiratory failure (primary outcome). Secondary outcomes included the incidence of ventilator-associated pneumonia (VAP), discomfort, intensive care unit (ICU) and hospital mortality, ICU and hospital length of stay (LOS), and time to re-intubation. Subgroup analyses considered “prophylactic” versus “therapeutic” NRS application and subpopulations (high-risk, low-risk, post-surgical and hypoxaemic patients).
Methods
We undertook a systematic review and network meta-analysis (Research Registry: reviewregistry1435). PubMed, Embase, CENTRAL, Scopus and Web of Science were searched (from inception until 22 June 2022). Randomised controlled trials (RCTs) investigating the use of NRS after extubation in ICU adult patients were included.
Results
32 RCTs entered the quantitative analysis (5063 patients). Compared with conventional oxygen therapy, NRS overall reduced re-intubations and VAP (moderate certainty). NIV decreased hospital mortality (moderate certainty), and hospital and ICU LOS (low and very low certainty, respectively), and increased discomfort (moderate certainty). Prophylactic NRS did not prevent extubation failure in low-risk or hypoxaemic patients.
Conclusion
Prophylactic NRS may reduce the rate of post-extubation respiratory failure in ICU patients.
Short abstract
Noninvasive respiratory support may be useful for preventing, but not treating, post-extubation respiratory failure in ICU patients. Prophylactic NIV and HFNO decreased the rate of extubation failure in high-risk and post-surgical patients, respectively. https://bit.ly/3uSJXZG
Introduction
Extubation failure, as defined by re-intubation secondary to post-extubation respiratory failure in a time interval varying from 48 h to 7 days among studies [1], has been described to occur in up to 23.5% of patients [2–6]. The incidence is even higher in high-risk patients, such as those aged >65 years or those affected by chronic cardiac disease, lung disease or other severe pulmonary disorders [6–8]. For surgical patients, the reported incidence of extubation failure varies between 5% and 10%, and depends on the patient's underlying comorbidities, type of surgery and anaesthesia, and intra-operative settings of mechanical ventilation, which overall define the predictive post-operative risk profile of each patient [9–11].
Several studies showed that post-extubation respiratory failure affects patient prognosis [3, 4, 6, 12]. In fact, re-intubated patients are characterised by increased mortality (up to 50%), even after adjusting for clinical severity, suggesting a direct adverse effect of re-intubation on patient outcome [5, 6]. Furthermore, post-extubation respiratory failure usually leads to prolonged invasive mechanical ventilation and to a higher risk of ventilator-associated pneumonia (VAP), critical weakness and delirium [13–15]. Lastly, extubation failure increases resource utilisation and costs, and patient discomfort [13, 16].
Forms of noninvasive respiratory support (NRS), including high-flow nasal oxygen (HFNO), continuous positive airway pressure (CPAP) and bi-level positive airway pressure, commonly referred to as noninvasive ventilation (NIV) [5, 17, 18, 19], have been proposed for avoiding re-intubation secondary to post-extubation failure, by maintaining adequate gas exchange, breathing pattern, inspiratory effort and tracheobronchial secretion clearance [10–26].
NRS has been used for prevention (“prophylactic” NRS) or treatment (“therapeutic” NRS) of post-extubation respiratory failure [5, 18, 19, 20, 27]. The most recent 2017 European Respiratory Society (ERS)/American Thoracic Society (ATS) clinical practice guidelines recommend the use of NIV for preventing post-extubation respiratory failure in high-risk patients (moderate certainty of evidence), but not in low-risk patients (conditional recommendation, very low certainty of evidence) [5]. The 2022 ERS guidelines recommend the use of HFNO, over conventional oxygen therapy (COT), in surgical and nonsurgical patients at low risk (conditional recommendation, low certainty of evidence) [18].
The purpose of this systematic review and network meta-analysis of randomised controlled trials (RCTs) is to provide an updated assessment of the effects of post-extubation NRS application on the rate of extubation failure (primary outcome), and on the incidence of VAP, patient discomfort, ICU and hospital mortality, ICU and hospital length of stay (LOS), and time to re-intubation (secondary outcomes). Additional subgroup analyses were planned for investigating, separately, the effect of “prophylactic” and “therapeutic” NRS application on the rate of extubation failure and the impact of NRS on predefined ICU subpopulations (high-risk, low-risk, post-surgical and hypoxaemic patients).
Methods
This article was written following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement extension for network meta-analysis [28–30]. The PRISMA checklist is available as supplementary table S1. A review protocol was written before conducting this study and prospectively registered at Research Registry (reviewregistry1435) on 22 June 2022.
Search strategy
We performed a systematic research of the medical literature for the identification, screening and inclusion of articles in the following databases from inception until 20 June 2022: PubMed, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), Scopus and Web of Science. To take into account possible publication biases, ongoing trials at ClinicalTrials.gov were also retrieved. In addition, backward snowballing (i.e. checking the reference lists of included studies, and of pertinent reviews and guidelines) was employed. Abstracts and conference proceedings were excluded. Further detailed information about the search strategy is available in supplementary table S2. No restrictions on language and year of publication were applied.
Study selection
Two researchers (A. Boscolo and T. Pettenuzzo) independently screened titles and abstracts of the identified papers to select relevant and nonrelevant papers. Each potentially relevant citation was reviewed with full-text retrieval. All studies meeting the following PICOS (Population, Intervention, Control, Outcomes, Study) criteria were included in the analysis: P) adult ICU patients (≥18 years old); I) randomisation for COT or one type of NRS (i.e. CPAP, NIV or HFNO); C) randomisation for COT or NRS, different from the one tested as intervention; O) incidence of post-extubation respiratory failure, defined as re-intubation (primary outcome) [1] and/or VAP, patient discomfort, ICU and hospital mortality, ICU and hospital LOS, and time to re-intubation (secondary outcomes); S) only RCTs. Note that CPAP was classified as NIV in the analysis.
Trials were excluded when focused on patients developing self-extubation, requiring palliative care, or when NRS had been used before the first cycle of invasive mechanical ventilation or as a “weaning” approach to allow early extubation after a failed spontaneous breathing trial (SBT) [31, 32].
With regard to the primary outcome, in the absence of a clearly accepted definition of extubation failure timing, we included all studies investigating the need for re-intubation, using an endotracheal tube, at any point during the hospital stay [27].
Moreover, we excluded from the quantitative analysis all studies investigating combinations of NRS devices administered in sequence, as reported by Thille et al. [33].
Data extraction
After identifying those studies meeting the inclusion criteria, three researchers (M. Zatta, A. De Cassai and A. Bruni) independently reviewed and assessed each of the included studies. Any disagreement on both study selection and data extraction was resolved by discussion with a further author (F. Zarantonello) or by contacting the corresponding author. The following information was independently collected by two investigators (A. De Cassai and A. Bruni): first author, year of study, eligibility criteria, exclusion criteria, total number of ICU patients per group and subgroups (classified as high-risk, low-risk, post-surgical and hypoxaemic), patients' age and gender, “prophylactic” or “therapeutic” NRS modality, and primary and secondary outcomes.
Quality assessment and certainty of evidence assessment
Two researchers (M. Zatta and C. Pretto) independently evaluated the quality of included RCTs by using the Cochrane Collaboration's Risk of Bias 2 tool [34]. The study-level risk of bias was expressed on a three-grade scale (“low risk of bias”, “high risk of bias” or “some concerns”). Disagreements were resolved by discussion with a third researcher (F. Geraldini). The GRADE (Grading of Recommendations Assessment, Development and Evaluations) approach was used to assess the certainty of evidence related to the outcomes [35]. GRADE addresses the domains of risk of bias, inconsistency, indirectness, publication bias, intransitivity, incoherence and imprecision. Imprecision for each comparison was only incorporated at the network level, not at the level of the direct or indirect estimate. A minimally contextualised approach, considering COT as reference, was applied to evaluate the magnitude of the intervention effect [36, 37].
Statistical methods
Meta-analysis of data was performed using R version 4.1 “Camp Pontanezen” (R Foundation for Statistical Computing, Vienna, Austria) and the package “netmeta”. A random effects model was used for all outcomes.
The primary outcome, i.e. extubation failure, as defined by need for re-intubation consequent to post-extubation respiratory failure, was investigated in the overall population and through subgroup analyses (i.e. “prophylactic” versus “therapeutic” NRS and in pre-registered subpopulations (see Subgroup analyses section)). The secondary outcomes (VAP, patient discomfort, ICU and hospital mortality, ICU and hospital LOS (days), and time to re-intubation (days)) were investigated only in the overall population. The treatment effect for continuous outcomes was expressed as mean difference with 95% confidence interval. The treatment effect for dichotomous outcomes was expressed as odds ratio with 95% confidence interval. A ranking among treatments was performed based on the frequentist analogue of the surface under the cumulative ranking curve (SUCRA). SUCRA represents the overall ranking of each treatment for the specified outcome and ranges from 0 (minimum) to 1 (maximum) [38, 39]. Wherever necessary, we converted reported median and interquartile range to estimated mean and standard deviation using the method of Hozo et al. [40] or Luo et al. [41] as appropriate. No continuity correction was applied in case of zero events.
Subgroup analyses
Additional pre-registered analyses were performed according to the following subgroups: 1) “prophylactic” (applied immediately after extubation) versus “therapeutic” support (defined as NRS application only after evidence of respiratory deterioration) [27], and 2) ICU high-risk and low-risk patients, post-surgical patients (undergoing NRS exclusively in the ICU), and hypoxaemic patients.
Patients were classified at high risk when aged >65 years or affected by heart disease, respiratory disease or other severe pulmonary disorders [6–8], otherwise they were classified at low risk of post-extubation respiratory failure.
Patients were defined as hypoxaemic when the arterial oxygen tension/inspiratory oxygen fraction (PaO2/FiO2) ratio at the end of the SBT was <300 mmHg [42].
Regarding ICU post-surgical patients, we excluded studies enrolling patients undergoing NRS in the operating room, in the post-anaesthesia care unit or in medical/surgical wards.
Inconsistency and heterogeneity analysis
For assessment of study heterogeneity, the Chi-squared test and I2-statistic were used. Heterogeneity was defined as low for I2<25%, moderate for I2=25–50% and high for I2>50%) [43]. Within-design heterogeneity and between-design inconsistency were evaluated using τ2.
Results
Study selection, characteristics and risk of bias assessment
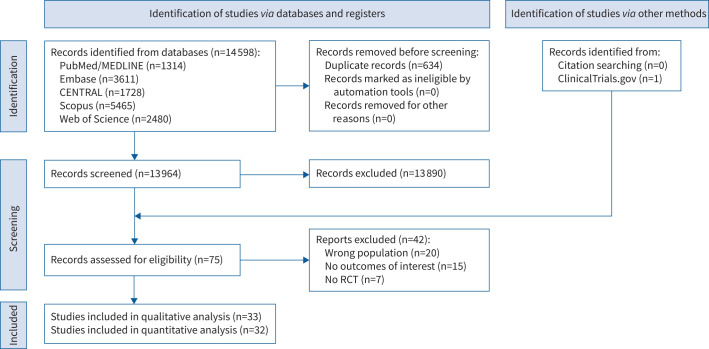
Bibliographic search results are shown in the study flowchart (figure 1). The initial screening found 14 598 studies. Of those, 33 (5711 patients) entered the qualitative analysis and 32 (5063 patients) entered the quantitative analysis. Characteristics of the included trials are available for consultation as supplementary table S3 and supplementary figure S1 [8, 33, 24, 26, 42, 44–71].
FIGURE 1.
PRISMA flowchart. RCT: randomised controlled trial.
Overall, 12 (36%) studies (1955 patients (34%)) compared HFNO to COT [24, 26, 42, 44–49, 69–71], while five (15%) studies (1104 patients (19%)) compared HFNO to NIV [50–54]. 15 (46%) studies (2004 patients (35%)) investigated NIV versus COT [8, 55–68] (figure 1). Finally, one (3%) study (648 patients (11%)) comparing HFNO to NIV plus HFNO (administered in sequence) was excluded from the quantitative analysis for limited comparability [33].
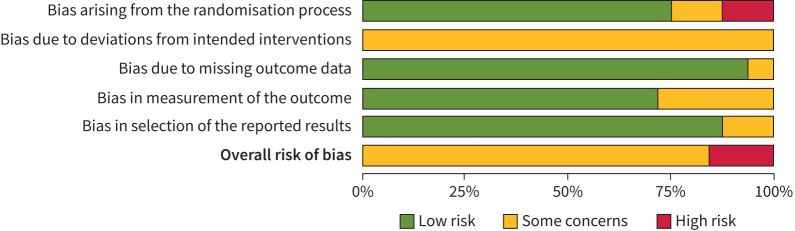
Risk of bias assessments are shown in figure 2 and supplementary table S4. The majority of trials were considered at low or moderate risk of bias. Only four studies were considered at high risk of bias due to questionable randomisation processes [56, 63, 66, 69].
FIGURE 2.
Risk of bias assessments.
Primary outcome in the overall population
As shown in figure 3, in the overall population, both HFNO (OR 0.60, 95% CI 0.43–0.84; p=0.003) and NIV (OR 0.61, 95% CI 0.46–0.81; p<0.001) reduced the incidence of extubation failure compared with COT (moderate certainty) (table 1, and supplementary tables S5 and S6). Moreover, no differences were found between HFNO versus NIV (p=0.844). Heterogeneity was moderate (I2=36%).
FIGURE 3.
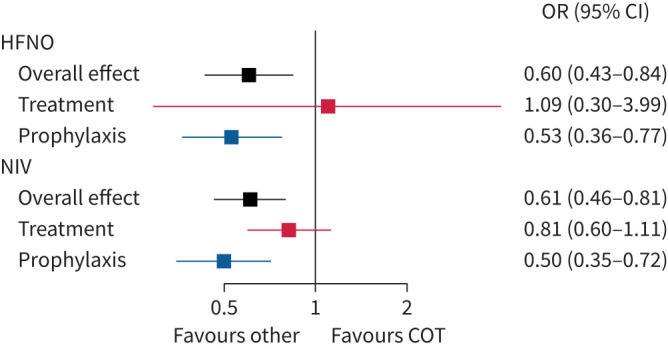
Impact of overall, “therapeutic” and “prophylactic” noninvasive respiratory support on primary outcome (re-intubation). COT: conventional oxygen therapy; HFNO: high-flow nasal oxygen; NIV: noninvasive ventilation.
TABLE 1.
Network estimates evaluating the impact of the interventions on primary and secondary outcomes in the overall population
| Comparison | MD or OR (95% CI) | p-value | I2 (%) | τ2 | K | GRADE# | Classification of intervention¶ |
| Re-intubation | 36 | 0.120 | |||||
| HFNO versus COT | 0.60 (0.43–0.84) | 0.003 | 11 | Moderatea | Large beneficial effect | ||
| NIV versus COT | 0.61 (0.46–0.81) | <0.001 | 15 | Moderatea | Large beneficial effect | ||
| NIV versus HFNO | 0.98 (0.69–1.40) | 0.844 | 5 | Moderateb | |||
| VAP | 0 | 0 | |||||
| HFNO versus COT | 0.36 (0.18–0.71) | 0.003 | 3 | Moderatea | Large beneficial effect | ||
| NIV versus COT | 0.49 (0.34–0.73) | <0.001 | 7 | Moderatea | Large beneficial effect | ||
| NIV versus HFNO | 0.74 (0.39–1.38) | 0.855 | 1 | Moderateb | |||
| Discomfort | 49 | 0.493 | |||||
| HFNO versus COT | 2.60 (0.79–8.60) | 0.117 | 7 | Lowa,b | Large harmful effect | ||
| NIV versus COT | 13.14 (5.94–29.04) | <0.001 | 1 | Moderatea | Large harmful effect | ||
| NIV versus HFNO | 0.20 (0.06–0.62) | 0.050 | 1 | High | |||
| ICU mortality | 6 | 0.017 | |||||
| HFNO versus COT | 0.81 (0.44–1.48) | 0.489 | 5 | Lowa,b | Small beneficial effect | ||
| NIV versus COT | 0.64 (0.39–1.05) | 0.075 | 8 | Moderatea | Large beneficial effect | ||
| NIV versus HFNO | 1.26 (0.63–2.52) | 0.834 | 1 | Lowa,b | |||
| Hospital mortality | 6 | 0.017 | |||||
| HFNO versus COT | 0.86 (0.62–1.18) | 0.431 | 5 | Moderatea | Small beneficial effect | ||
| NIV versus COT | 0.64 (0.47–0.87) | 0.981 | 11 | Moderatea | Large beneficial effect | ||
| NIV versus HFNO | 1.35 (0.97–1.86) | 0.194 | 4 | Moderateb | |||
| ICU length of stay | 87 | 1.048 | |||||
| HFNO versus COT | −0.12 (−0.85–0.61) | 0.741 | 9 | Very lowa,b,c,d | Trivial beneficial effect | ||
| NIV versus COT | −0.72 (−1.44–0.00) | 0.049 | 14 | Very lowa,c,d | Small beneficial effect | ||
| NIV versus HFNO | 0.60 (−0.33–1.53) | 0.032 | 4 | Very lowb,c,d | |||
| Hospital length of stay | 86 | 2.230 | |||||
| HFNO versus COT | −0.04 (−1.27–1.18) | 0.264 | 8 | Very lowa,b,c | Trivial beneficial effect | ||
| NIV versus COT | −2.38 (−3.69– −1.07) | 0.999 | 10 | Lowa,c | Large beneficial effect | ||
| NIV versus HFNO | 2.34 (0.80–3.88) | 0.189 | 3 | Very lowa,b,c | |||
| Time to re-intubation | 89 | 87.485 | |||||
| HFNO versus COT | 2.99 (−8.13–14.10) | 0.564 | 3 | Very lowa,b,c | Trivial harmful effect | ||
| NIV versus COT | 9.17 (−1.06–19.40) | 0.105 | 4 | Very lowa,b,c | Small harmful effect | ||
| NIV versus HFNO | −6.18 (−18.86–6.5) | 0.371 | 1 | Very lowa,b,c |
MD: mean difference; OR: odds ratio; τ2 and I2: loop heterogeneity; K: number of studies providing direct evidence; GRADE: Grading of Recommendations Assessment, Development and Evaluations; HFNO: high-flow nasal oxygen; COT: conventional oxygen therapy; NIV: noninvasive ventilation; VAP: ventilator-associated pneumonia; ICU: intensive care unit. #: GRADE certainty of evidence: a: lowered one level for risk of bias; b: lowered one level for imprecision as confidence intervals do not allow excluding harm; c: lowered one level for inconsistency; d: lowered one level for incoherence. ¶: for dichotomous outcome variables, large intervention effects were considered for OR >1.3 or <0.7, moderate intervention effects for 1.2<OR≤1.3 or 0.7≤OR<0.8, small intervention effects for 1.1<OR≤1.2 or 0.8≤OR<0.9 and trivial intervention effects for 1.0<OR≤1.1 or 0.9≤OR<1.0; for length of stay, large intervention effects were considered for MD>2, moderate intervention effects for 1<MD≤2, small intervention effects for 0.5<MD≤1 and trivial intervention effects for 0<MD≤0.5; for time to re-intubation, large intervention effects were considered for MD>24, moderate intervention effects for 12<MD≤24, small intervention effects for 6<MD≤12 and trivial intervention effects for 0<MD≤6. COT was considered as the reference intervention. Bold indicates p<0.05.
Secondary outcomes in the overall population
Incidence of VAP
Both HFNO (OR 0.36, 95% CI 0.18–0.71; p=0.003) and NIV (OR 0.49, 95% CI 0.34–0.73; p<0.001) were associated to a lower rate of VAP (moderate certainty) compared with COT (table 1, and supplementary tables S5 and S6). Heterogeneity was very low (I2=0%).
Discomfort
NIV (OR 13.14, 95% CI 5.94,29.04; p<0.001, moderate certainty), but not HFNO, was associated with a higher patient discomfort compared with COT (table 1, and supplementary tables S5 and S6). Heterogeneity was moderate (I2=49%).
ICU and hospital mortality
Neither HFNO nor NIV affected ICU mortality compared with COT. NIV, but not HFNO, reduced hospital mortality (OR 0.64, 95% CI 0.47–0.87; p=0.981, moderate certainty) compared with COT (table 1, and supplementary tables S5 and S6). Heterogeneity was low (I2=6%).
ICU and hospital LOS
NIV shortened ICU LOS (days) (MD −0.72, 95% CI −1.44–0.00; p=0.049, very low certainty), despite a high heterogeneity (I2=87%), compared with COT. HFNO did not show any benefit (table 1, and supplementary tables S5 and S6).
Time to re-intubation
Neither HFNO nor NIV affected the time to re-intubation (days) compared with COT. Heterogeneity was very high (I2=89%) (table 1, and supplementary tables S5 and S6).
Subgroup analysis
Prophylactic NRS
As shown in figure 3, in the overall population, both prophylactic HFNO (OR 0.53, 95% CI 0.36–0.77; p=0.001) and NIV (OR 0.50, 95% CI 0.35–0.72; p<0.001) were significantly correlated to a lower risk of extubation failure compared with COT [8, 25, 38, 40–51, 53, 54, 57–63, 65–67]. Heterogeneity was moderate (I2=39%) (supplementary tables S5–S7).
In high-risk patients (12 studies (1702 patients)), only prophylactic NIV significantly reduced the risk of extubation failure (OR 0.50, 95% CI 0.33–0.75; p<0.001) compared with COT (figure 4). Heterogeneity was very low (I2=0%) (supplementary tables S5–S7).
FIGURE 4.
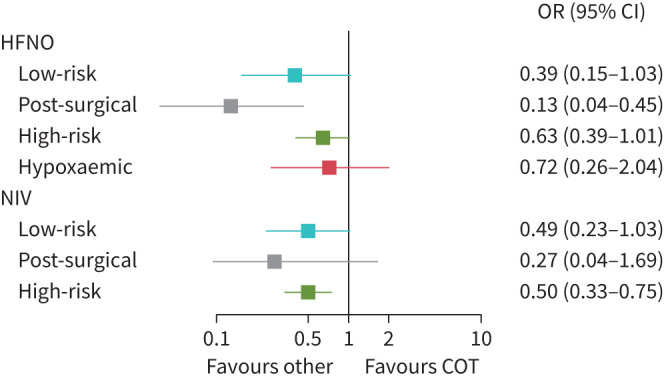
Impact of “prophylactic” noninvasive respiratory support on predefined subgroups (re-intubation). COT: conventional oxygen therapy; HFNO: high-flow nasal oxygen; NIV: noninvasive ventilation.
In low-risk patients (seven studies (1433 patients)), neither prophylactic HFNO nor NIV affected the primary outcome compared with COT (figure 4). Heterogeneity was high (I2=61%) (supplementary tables S5–S7).
In ICU post-surgical patients (five studies (544 patients)), prophylactic HFNO (OR 0.13, 95% CI 0.04–0.45; p=0.001), but not prophylactic NIV (OR 0.27, 95% CI 0.04–1.69; p=0.162), decreased the incidence of extubation failure compared with COT. Heterogeneity was very low (I2=0%) (supplementary tables S5–S7).
In hypoxaemic patients (three studies (663 patients)), prophylactic HFNO did not affect the rate of post-extubation respiratory failure (figure 4). Heterogeneity was high (I2=69%) (supplementary tables S5–S7).
Therapeutic NRS
The application of HFNO or NIV, as treatment for established post-extubation respiratory failure, showed no benefits in the overall population compared with COT [23, 52, 55, 56, 64]. Heterogeneity was very low (I2=0%) (supplementary tables S5–S7).
Additional subgroup analyses were not feasible due to the limited number of RCTs investigating the use of NRS for treating established post-extubation respiratory failure in medical and post-surgical populations.
Discussion
In this network meta-analysis, we found that: 1) HFNO and NIV reduced the rate of extubation failure and VAP compared with COT; 2) NIV, but not HFNO, reduced hospital mortality and ICU and hospital LOS; 3) neither HFNO nor NIV showed any benefit on ICU mortality or time to re-intubation; 4) patient discomfort was worsened by NIV compared with COT and HFNO; 5) prophylactic NIV, but not HFNO, reduced the rate of extubation failure in high-risk patients compared with COT; 6) prophylactic HFNO, but not NIV, reduced the rate of post-extubation respiratory failure in post-surgical patients compared with COT; 7) neither prophylactic NIV nor HFNO reduced the rate of extubation failure in low-risk or hypoxaemic patients; and 8) the therapeutic use of NIV or HFNO showed no benefits compared with COT.
Our results are consistent with those of another recent network meta-analysis on 36 RCTs (6806 patients) showing that, compared with COT, NRS overall reduced the rate of re-intubation when applied to prevent post-extubation respiratory failure, but it did not improve hospital mortality [27]. Nonetheless, the two network meta-analyses present several differences. First, the previous meta-analysis was more focused on low-risk patients (14 (39%) studies) rather than on patients at high risk of extubation failure (seven (19%) studies), as opposed to the present meta-analysis (eight (25%) low-risk studies and 13 (41%) high-risk studies). Second, despite a higher number of patients included (6806 versus 5063 patients), the previous network meta-analysis enrolled 2259 (33%) surgical patients undergoing NRS not exclusively in the ICU, but also in the operating room, post-anaesthesia care unit or medical/surgical wards [62–75]. On the contrary, we considered only post-operative patients admitted to the ICU. Third, three studies included in the previous network meta-analysis investigated NRS application as a “weaning” strategy to allow early extubation after failed SBT [20, 31, 32, 76], which is, in our opinion, a quite different population of patients than that of patients extubated after a successful SBT. Finally, some of our secondary outcomes, such as time to re-intubation and ICU or hospital LOS, were not considered in the previous meta-analysis [27].
With respect to HFNO in surgical patients, our results are in accordance with the statements of the 2022 ERS guidelines, which recommend prophylactic HFNO, over COT, after extubation in surgical patients both at low and high risk of extubation failure (conditional recommendation, low certainty of evidence) [18]. While different from those guidelines, recommending the prophylactic use of HFNO also in nonsurgical patients at low risk of failure (conditional recommendation, low certainty of evidence) [18], our analysis did not observe a significant difference between HFNO and COT in nonsurgical low-risk patients (p=0.057, I2=61%).
With respect to the impact of prophylactic HFNO on hypoxaemic patients, our network meta-analysis did not show any difference on the rate of post-extubation respiratory failure between HFNO and COT, as recently reported by Maggiore et al. [42].
In keeping with the statements of the 2017 ERS/ATS guidelines, our network meta-analysis showed that prophylactic, but not therapeutic, NIV decreased the rate of post-extubation respiratory failure in high-risk patients, but not in low-risk patients, compared with COT [5].
With regard to surgical patients, the 2017 ERS/ATS guidelines discussed the possible therapeutic application of NIV in post-surgical patients with established respiratory failure (conditional recommendation, moderate certainty of evidence) [5]. Based on our network meta-analysis, we showed that the therapeutic use of NIV did not reduce the rate of extubation failure in the overall population compared with COT. However, a subgroup analysis, exclusively focused on ICU patients, after surgery was not feasible due to the limited number of RCTs available (n=2 [59, 68]).
Finally, in accordance with the 2022 ERS guidelines, our analysis confirmed that NIV, but not HFNO, reduced the rate of post-extubation respiratory failure in high-risk nonsurgical patients [18]. With respect to surgical patients, conversely, our network meta-analysis showed that only prophylactic HFNO reduced the risk of extubation failure, while the 2022 ERS guidelines stated that either HFNO or NIV may reduce the rate of extubation failure in surgical patients at high risk of post-operative respiratory complications (conditional recommendation, low certainty of evidence) [18]. It is worth emphasising, as already mentioned, that we considered only surgical patients exclusively treated with NRS after extubation in the ICU, without any stratification between patients at low or high risk of post-operative respiratory failure. Therefore, we cannot exclude that the use of NIV may have a different impact on surgical patients enrolled in the operating room or post-anaesthesia care unit.
Finally, we did not find any difference between NRS modalities with respect to time to re-intubation. However, the very low certainty of evidence limits the robustness of this finding. It is worth remarking that longer time to re-intubation may result in delayed intubation in the patients who need it more, such as those experiencing post-extubation respiratory failure and receiving therapeutic NRS.
Study strengths and limitations
This review has some points of strength since it included: 1) a broad and systematic search of five different databases; 2) a pre-planned network meta-analysis with rigorous subset analyses to investigate the impact of post-extubation NRS in different subpopulations; and 3) a large number of studies, including more than 5000 enrolled patients. Moreover, our network analysis showed a relatively low incoherence between direct and indirect findings. Despite these assumptions, some limitations require discussion. First, we included several studies published more than 10 years ago and, in the meantime, clinical practice may have changed, thus introducing potential intransitivity. Second, we could not account for the heterogeneity attributable to the different outcome definitions among studies. Third, only 24% (eight out of 33) of trials included more than 100 patients per group, which may introduce bias due to small-study effects.
Points for clinical practice
NRS may be useful for preventing, but not for treating, post-extubation respiratory failure in ICU patients.
Prophylactic NIV decreased the rate of extubation failure in ICU high-risk patients; prophylactic HFNO decreased the rate of extubation failure in ICU post-surgical patients.
Conclusions
In the overall population, NRS reduced the rate of post-extubation respiratory failure and VAP compared with COT. NIV, but not HFNO, improved hospital mortality, and ICU and hospital LOS, despite worsened patient discomfort. Prophylactic, but not therapeutic, NRS decreased the rate of extubation failure in high-risk patients (NIV) and in post-surgical patients (HFNO), but not in the low-risk and hypoxaemic subgroups of patients.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material ERR-0196-2022.supplement (477.1KB, pdf)
Footnotes
Provenance: Commissioned article, peer reviewed.
Previous articles in this series: No. 1: Bureau C, Van Hollebeke M, Dres M. Managing respiratory muscle weakness during weaning from invasive ventilation. Eur Respir Rev 2023; 32: 220205. No. 2: van den Biggelaar R, Hazenberg A, Duiverman ML. The role of telemonitoring in patients on home mechanical ventilation. Eur Respir Rev 2023; 32: 220207.
Author contributions: A. Boscolo, T. Pettenuzzo, P. Navalesi, A. Peralta, L. Muraro, F. Geraldini and N. Sella made substantial contributions to the conception and design of the work, and drafted and reviewed the manuscript critically for important intellectual content. M. Zatta, M. Salvagno, M. Tassone, C. Pretto, F. Zarantonello, A. De Cassai and A. Bruni made substantial contributions to the acquisition, analysis and interpretation of data for the work, and drafted the manuscript. All authors approved the final version of the manuscript and confirm that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved.
This article has an editorial commentary: https://doi.org/10.1183/16000617.0027-2023
Number 3 in the Series “Respiratory Failure and Mechanical Ventilation Conference reviews” Edited by Leo Heunks and Marieke L. Duiverman
Conflict of interest: None related to the present work. P. Navalesi's research lab has received grants/research equipment from Draeger, Intersurgical SPA and Gilead. P. Navalesi receives royalties from Intersurgical SPA for the Helmet Next invention. He has also received speaking fees from Getinge, Intersurgical SPA, Mindray, Gilead, MSD, Draeger and Medicair. The other authors have no other competing interests to declare.
References
- 1.Thille AW, Richard JCM, Brochard L. The decision to extubate in the intensive care unit. Am J Respir Crit Care Med 2013; 187: 1294–1302. doi: 10.1164/rccm.201208-1523CI [DOI] [PubMed] [Google Scholar]
- 2.Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991; 324: 1445–1450. doi: 10.1056/NEJM199105233242101 [DOI] [PubMed] [Google Scholar]
- 3.Esteban A, Alía I, Tobin MJ, et al. Effect of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med 1999; 159: 512–518. doi: 10.1164/ajrccm.159.2.9803106 [DOI] [PubMed] [Google Scholar]
- 4.Epstein SK. Predicting extubation failure: is it in (on) the cards? Chest 2001; 120: 1061–1063. doi: 10.1378/chest.120.4.1061 [DOI] [PubMed] [Google Scholar]
- 5.Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J 2017; 50: 1602426. doi: 10.1183/13993003.02426-2016 [DOI] [PubMed] [Google Scholar]
- 6.Thille AW, Harrois A, Schortgen F, et al. Outcomes of extubation failure in medical intensive care unit patients. Crit Care Med 2011; 39: 2612–2618. doi: 10.1097/CCM.0b013e3182282a5a [DOI] [PubMed] [Google Scholar]
- 7.Nava S, Navalesi P, Conti G. Time of non-invasive ventilation. Intensive Care Med 2006; 32: 361–370. doi: 10.1007/s00134-005-0050-0 [DOI] [PubMed] [Google Scholar]
- 8.Nava S, Gregoretti C, Fanfulla F, et al. Noninvasive ventilation to prevent respiratory failure after extubation in high-risk patients. Crit Care Med 2005; 33: 2465–2470. doi: 10.1097/01.CCM.0000186416.44752.72 [DOI] [PubMed] [Google Scholar]
- 9.Jammer I, Wickboldt N, Sander M, et al. Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol 2015; 32: 88–105. doi: 10.1097/EJA.0000000000000118 [DOI] [PubMed] [Google Scholar]
- 10.Miu T, Joffe AM, Yanez ND, et al. Predictors of reintubation in critically ill patients. Respir Care 2014; 59: 178–185. doi: 10.4187/respcare.02527 [DOI] [PubMed] [Google Scholar]
- 11.Demling RH, Read T, Lind LJ, et al. Incidence and morbidity of extubation failure in surgical intensive care patients. Crit Care Med 1988; 16: 573–577. doi: 10.1097/00003246-198806000-00001 [DOI] [PubMed] [Google Scholar]
- 12.Thille AW, Cortés-Puch I, Esteban A. Weaning from the ventilator and extubation in ICU. Curr Opin Crit Care 2013; 19: 57–64. doi: 10.1097/MCC.0b013e32835c5095 [DOI] [PubMed] [Google Scholar]
- 13.Adhikari NKJ, Fowler RA, Bhagwanjee S, et al. Critical care and the global burden of critical illness in adults. Lancet 2010; 376: 1339–1346. doi: 10.1016/S0140-6736(10)60446-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rajakaruna C, Rogers CA, Angelini GD, et al. Risk factors for and economic implications of prolonged ventilation after cardiac surgery. J Thorac Cardiovasc Surg 2005; 130: 1270–1277. doi: 10.1016/j.jtcvs.2005.06.050 [DOI] [PubMed] [Google Scholar]
- 15.Boscolo A, Pasin L, Sella N, et al. Outcomes of COVID-19 patients intubated after failure of non-invasive ventilation: a multicenter observational study. Sci Rep 2021; 11: 17730. doi: 10.1038/s41598-021-96762-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dasta JF, McLaughlin TP, Mody SH, et al. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med 2005; 33: 1266–1271. doi: 10.1097/01.CCM.0000164543.14619.00 [DOI] [PubMed] [Google Scholar]
- 17.Nava S, Navalesi P, Carlucci A. Non-invasive ventilation. Minerva Anestesiol 2009; 75: 31–36. [PubMed] [Google Scholar]
- 18.Oczkowski S, Ergan B, Bos L, et al. ERS clinical practice guidelines: high-flow nasal cannula in acute respiratory failure. Eur Respir J 2022; 59: 2101574. doi: 10.1183/13993003.01574-2021 [DOI] [PubMed] [Google Scholar]
- 19.Crimi C, Noto A, Princi P, et al. A European survey of noninvasive ventilation practices. Eur Respir J 2010; 36: 362–369. doi: 10.1183/09031936.00123509 [DOI] [PubMed] [Google Scholar]
- 20.Burns KEA, Stevenson J, Laird M, et al. Non-invasive ventilation versus invasive weaning in critically ill adults: a systematic review and meta-analysis. Thorax 2022; 77: 752–761. doi: 10.1136/thoraxjnl-2021-216993 [DOI] [PubMed] [Google Scholar]
- 21.De Jong A, Casey JD, Myatra SN. Focus on noninvasive respiratory support before and after mechanical ventilation in patients with acute respiratory failure. Intensive Care Med 2020; 46: 1460–1463. doi: 10.1007/s00134-020-06100-8 [DOI] [PubMed] [Google Scholar]
- 22.Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med 2017; 195: 438–442. doi: 10.1164/rccm.201605-1081CP [DOI] [PubMed] [Google Scholar]
- 23.Turner E, Jenks M. Cost-effectiveness analysis of the use of high-flow oxygen through nasal cannula in intensive care units in NHS England. Expert Rev Pharmacoecon Outcomes Res 2018; 18: 331–337. doi: 10.1080/14737167.2018.1411804 [DOI] [PubMed] [Google Scholar]
- 24.Matsuda W, Hagiwara A, Uemura T, et al. High-flow nasal cannula may not reduce the re-intubation rate compared with a large-volume nebulization-based humidifier. Respir Care 2020; 65: 610–617. doi: 10.4187/respcare.07095 [DOI] [PubMed] [Google Scholar]
- 25.Lee JH, Rehder KJ, Williford L, et al. Use of high flow nasal cannula in critically ill infants, children, and adults: a critical review of the literature. Intensive Care Med 2013; 39: 247–257. doi: 10.1007/s00134-012-2743-5 [DOI] [PubMed] [Google Scholar]
- 26.Maggiore SM, Idone FA, Vaschetto R, et al. Nasal high-flow versus Venturi mask oxygen therapy after extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med 2014; 190: 282–288. doi: 10.1164/rccm.201402-0364OC [DOI] [PubMed] [Google Scholar]
- 27.Fernando SM, Tran A, Sadeghirad B, et al. Noninvasive respiratory support following extubation in critically ill adults: a systematic review and network meta-analysis. Intensive Care Med 2022; 48: 137–147. doi: 10.1007/s00134-021-06581-1 [DOI] [PubMed] [Google Scholar]
- 28.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Rev Esp Cardiol 2021; 74: 790–799. doi: 10.1016/j.recesp.2021.06.016 [DOI] [PubMed] [Google Scholar]
- 29.Moher D, Liberati A, Altman DG, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 2015; 162: 777–784. doi: 10.7326/M14-2385 [DOI] [PubMed] [Google Scholar]
- 31.Vaschetto R, Longhini F, Persona P, et al. Early extubation followed by immediate noninvasive ventilation vs. standard extubation in hypoxemic patients: a randomized clinical trial. Intensive Care Med 2019; 45: 62–71. doi: 10.1007/s00134-018-5478-0 [DOI] [PubMed] [Google Scholar]
- 32.Stéphan F, Barrucand B, Petit P, et al. High-flow nasal oxygen vs noninvasive positive airway pressure in hypoxemic patients after cardiothoracic surgery: a randomized clinical trial. JAMA 2015; 313: 2331–2339. doi: 10.1001/jama.2015.5213 [DOI] [PubMed] [Google Scholar]
- 33.Thille AW, Muller G, Gacouin A, et al. Effect of postextubation high-flow nasal oxygen with noninvasive ventilation vs high-flow nasal oxygen alone on reintubation among patients at high risk of extubation failure: a randomized clinical trial. JAMA 2019; 322: 1465–1475. doi: 10.1001/jama.2019.14901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Puhan MA, Schünemann HJ, Murad MH, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 2014; 349: g5630. doi: 10.1136/bmj.g5630 [DOI] [PubMed] [Google Scholar]
- 36.Brignardello-Petersen R, Florez ID, Izcovich A, et al. GRADE approach to drawing conclusions from a network meta-analysis using a minimally contextualised framework. BMJ 2020; 371: m3900. doi: 10.1136/bmj.m3900 [DOI] [PubMed] [Google Scholar]
- 37.Zeng L, Brignardello-Petersen R, Hultcrantz M, et al. GRADE Guidelance 34: updated on rating imprecision using a minimally contextualized approach. J Clin Epidemiol 2022; 150: 216–224. doi: 10.1016/j.jclinepi.2022.07.014 [DOI] [PubMed] [Google Scholar]
- 38.Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol 2015; 15: 58. doi: 10.1186/s12874-015-0060-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seide SE, Jensen K, Kieser M. A comparison of Bayesian and frequentist methods in random-effects network meta-analysis of binary data. Res Synth Methods 2020; 11: 363–378. doi: 10.1002/jrsm.1397 [DOI] [PubMed] [Google Scholar]
- 40.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005; 5: 13. doi: 10.1186/1471-2288-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Luo D, Wan X, Liu J, et al. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 2018; 27: 1785–1805. doi: 10.1177/0962280216669183 [DOI] [PubMed] [Google Scholar]
- 42.Maggiore SM, Jaber S, Grieco DL, et al. High-flow versus VenturiMask oxygen therapy to prevent re-intubation in hypoxemic patients after extubation: a multicenter, randomized clinical trial. Am J Respir Crit Care Med 2022; 206: 1452–1462. doi: 10.1164/rccm.202201-0065OC [DOI] [PubMed] [Google Scholar]
- 43.Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cho JY, Kim HS, Kang H, et al. Comparison of postextubation outcomes associated with high-flow nasal cannula vs. conventional oxygen therapy in patients at high risk of reintubation: a randomized clinical trial. J Korean Med Sci 2020; 35: e194. doi: 10.3346/jkms.2020.35.e194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Corley A, Bull T, Spooner AJ, et al. Direct extubation onto high-flow nasal cannulae post-cardiac surgery versus standard treatment in patients with a BMI ≥30: a randomised controlled trial. Intensive Care Med 2015; 41: 887–888. doi: 10.1007/s00134-015-3765-6 [DOI] [PubMed] [Google Scholar]
- 46.Fernandez R, Subira C, Frutos-Vivar F, et al. High-flow nasal cannula to prevent postextubation respiratory failure in high-risk non-hypercapnic patients: a randomized multicenter trial. Ann Intensive Care 2017; 7: 47. doi: 10.1186/s13613-017-0270-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hernández G, Vaquero C, González P, et al. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA 2016; 315: 1354–1361. doi: 10.1001/jama.2016.2711 [DOI] [PubMed] [Google Scholar]
- 48.Song HZ, Gu JX, Xiu HQ, et al. The value of high-flow nasal cannula oxygen therapy after extubation in patients with acute respiratory failure. Clinics 2017; 72: 562–567. doi: 10.6061/clinics/2017(09)07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Theologou S, Ischaki E, Zakynthinos SG, et al. High flow oxygen therapy at two initial flow settings versus conventional oxygen therapy in cardiac surgery patients with postextubation hypoxemia: a single-center, unblinded, randomized, controlled trial. J Clin Med 2021; 10: 2079. doi: 10.3390/jcm10102079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hernández G, Vaquero C, Colinas L, et al. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: a randomized clinical trial. JAMA 2016; 316: 1565–1574. doi: 10.1001/jama.2016.14194 [DOI] [PubMed] [Google Scholar]
- 51.Tan D, Walline JH, Ling B, et al. High-flow nasal cannula oxygen therapy versus non-invasive ventilation for chronic obstructive pulmonary disease patients after extubation: a multicenter, randomized controlled trial. Crit Care 2020; 24: 489. doi: 10.1186/s13054-020-03214-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Theerawit P, Natpobsuk N, Petnak T, et al. The efficacy of the WhisperFlow CPAP system versus high flow nasal cannula in patients at risk for postextubation failure: a randomized controlled trial. J Crit Care 2021; 63: 117–123. doi: 10.1016/j.jcrc.2020.09.031 [DOI] [PubMed] [Google Scholar]
- 53.Tongyoo S, Tantibundit P, Daorattanachai K, et al. High-flow nasal oxygen cannula vs. noninvasive mechanical ventilation to prevent reintubation in sepsis: a randomized controlled trial. Ann Intensive Care 2021; 11: 135. doi: 10.1186/s13613-021-00922-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jing G, Li J, Hao D, et al. Comparison of high flow nasal cannula with noninvasive ventilation in chronic obstructive pulmonary disease patients with hypercapnia in preventing postextubation respiratory failure: a pilot randomized controlled trial. Res Nurs Health 2019; 42: 217–225. doi: 10.1002/nur.21942 [DOI] [PubMed] [Google Scholar]
- 55.Al Jaaly E, Fiorentino F, Reeves BC, et al. Effect of adding postoperative noninvasive ventilation to usual care to prevent pulmonary complications in patients undergoing coronary artery bypass grafting: a randomized controlled trial. J Thorac Cardiovasc Surg 2013; 146: 912–918. doi: 10.1016/j.jtcvs.2013.03.014 [DOI] [PubMed] [Google Scholar]
- 56.Esteban A, Frutos-Vivar F, Ferguson ND, et al. Noninvasive positive-pressure ventilation for respiratory failure after extubation. N Engl J Med 2004; 350: 2452–2460. doi: 10.1056/NEJMoa032736 [DOI] [PubMed] [Google Scholar]
- 57.Ferrer M, Valencia M, Nicolas JM, et al. Early noninvasive ventilation averts extubation failure in patients at risk: a randomized trial. Am J Respir Crit Care Med 2006; 173: 164–170. doi: 10.1164/rccm.200505-718OC [DOI] [PubMed] [Google Scholar]
- 58.Ferrer M, Sellarés J, Valencia M, et al. Non-invasive ventilation after extubation in hypercapnic patients with chronic respiratory disorders: randomised controlled trial. Lancet 2009; 374: 1082–1088. doi: 10.1016/S0140-6736(09)61038-2 [DOI] [PubMed] [Google Scholar]
- 59.Jaber S, Lescot T, Futier E, et al. Effect of noninvasive ventilation on tracheal reintubation among patients with hypoxemic respiratory failure following abdominal surgery: a randomized clinical trial. JAMA 2016; 315: 1345–1353. doi: 10.1001/jama.2016.2706 [DOI] [PubMed] [Google Scholar]
- 60.Keenan SP, Powers C, McCormack DG, et al. Noninvasive positive-pressure ventilation for postextubation respiratory distress: a randomized controlled trial. JAMA 2002; 287: 3238–3244. doi: 10.1001/jama.287.24.3238 [DOI] [PubMed] [Google Scholar]
- 61.Khilnani GC, Galle AD, Hadda V, et al. Non-invasive ventilation after extubation in patients with chronic obstructive airways disease: a randomised controlled trial. Anaesth Intensive Care 2011; 39: 217–223. doi: 10.1177/0310057X1103900210 [DOI] [PubMed] [Google Scholar]
- 62.Kindgen-Milles D, Müller E, Buhl R, et al. Nasal-continuous positive airway pressure reduces pulmonary morbidity and length of hospital stay following thoracoabdominal aortic surgery. Chest 2005; 128: 821–828. doi: 10.1378/chest.128.2.821 [DOI] [PubMed] [Google Scholar]
- 63.Mohamed KAE, Abdalla MH. Role of non invasive ventilation in limiting re-intubation after planned extubation. Egypt J Chest Dis Tuberc 2013; 62: 669–674. doi: 10.1016/j.ejcdt.2013.08.010 [DOI] [Google Scholar]
- 64.Ornico SR, Lobo SM, Sanches HS, et al. Noninvasive ventilation immediately after extubation improves weaning outcome after acute respiratory failure: a randomized controlled trial. Crit Care 2013; 17: R39. doi: 10.1186/cc12549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Su CL, Chiang LL, Yang SH, et al. Preventive use of noninvasive ventilation after extubation: a prospective, multicenter randomized controlled trial. Respir Care 2012; 57: 204–210.doi: 10.4187/respcare.01141 [DOI] [PubMed] [Google Scholar]
- 66.Thanthitaweewat V, Muntham D, Chirakalwasan N. Targeted-volume noninvasive ventilation reduces extubation failure in postextubated medical intensive care unit patients: a randomized controlled trial. Indian J Crit Care Med 2018; 22: 639–645. doi: 10.4103/ijccm.IJCCM_236_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vargas F, Clavel M, Sanchez-Verlan P, et al. Intermittent noninvasive ventilation after extubation in patients with chronic respiratory disorders: a multicenter randomized controlled trial (VHYPER). Intensive Care Med 2017; 43: 1626–1636. doi: 10.1007/s00134-017-4785-1 [DOI] [PubMed] [Google Scholar]
- 68.Yang Y, Liu N, Sun L, et al. Noninvasive positive-pressure ventilation in treatment of hypoxemia after extubation following type-A aortic dissection. J Cardiothorac Vasc Anesth 2016; 30: 1539–1544. doi: 10.1053/j.jvca.2016.03.129 [DOI] [PubMed] [Google Scholar]
- 69.Yu Y, Qian X, Liu C, et al. Effect of high-flow nasal cannula versus conventional oxygen therapy for patients with thoracoscopic lobectomy after extubation. Can Respir J 2017; 2017: 7894631. doi: 10.1155/2017/7894631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sahin M, El H, Akkoç I. Comparison of mask oxygen therapy and high-flow oxygen therapy after cardiopulmonary bypass in obese patients. Can Respir J 2018; 2018: 1039635. doi: 10.1155/2018/1039635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Huang HW, Sun XM, Shi ZH, et al. Effect of high-flow nasal oxygen vs. conventional oxygen therapy on extubation outcomes and physiologic changes for patients with high risk of extubation failure in the medical ICU: a tertiary center, randomized, controlled trial. J Intensive Care Med 2018; 33: 609–623. doi: 10.1177/0885066617705118 [DOI] [PubMed] [Google Scholar]
- 72.Brainard J, Scott BK, Sullivan BL, et al. Heated humidified high-flow nasal cannula oxygen after thoracic surgery – a randomized prospective clinical pilot trial. J Crit Care 2017; 40: 225–228. doi: 10.1016/j.jcrc.2017.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Futier E, Paugam-Burtz C, Godet T, et al. Effect of early postextubation high-flow nasal cannula vs conventional oxygen therapy on hypoxaemia in patients after major abdominal surgery: a French multicentre randomised controlled trial (OPERA). Intensive Care Med 2016; 42: 1888–1898. doi: 10.1007/s00134-016-4594-y [DOI] [PubMed] [Google Scholar]
- 74.Parke R, McGuinness S, Dixon R, et al. Open-label, phase II study of routine high-flow nasal oxygen therapy in cardiac surgical patients. Br J Anaesth 2013; 111: 925–931. doi: 10.1093/bja/aet262 [DOI] [PubMed] [Google Scholar]
- 75.Tatsuishi W, Sato T, Kataoka G, et al. High-flow nasal cannula therapy with early extubation for subjects undergoing off-pump coronary artery bypass graft surgery. Respir Care 2020; 65: 183–190. doi: 10.4187/respcare.06382 [DOI] [PubMed] [Google Scholar]
- 76.Girault C, Bubenheim M, Abroug F, et al. Noninvasive ventilation and weaning in patients with chronic hypercapnic respiratory failure: a randomized multicenter trial. Am J Respir Crit Care Med 2011; 184: 672–679. doi: 10.1164/rccm.201101-0035OC [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material ERR-0196-2022.supplement (477.1KB, pdf)