Abstract
Aim
Despite well-established protocols for cardiopulmonary resuscitation training, performance during real-life cardiac arrests can be suboptimal. Understanding personal characteristics which could influence performance of high-quality chest compressions could provide insight into the practice-performance gap. This study examined chest compression performance, while employing feedback and introducing code team sounds as an anxiety-inducing factor in registered nurses using a cardiopulmonary resuscitation training manikin.
Methods
Participants included 120 registered nurses with basic life support certification randomized to one of the following groups: no feedback and no code team sounds, feedback without code team sounds, or feedback with code team sounds. Chest compression sessions occurred at baseline, 30-days and 60-days. Demographic variables and anxiety level were also collected. The primary outcome was chest compression performance, defined as average percent of time with correct rate and percent with correct depth as captured by the defibrillator. Statistical analysis included linear mixed effects analysis.
Results
The effect of feedback on chest compression performance depended on the value of other parameters. The benefit of feedback on the primary outcome depended on: age, with feedback less beneficial among older participants (p = 0.0413); and time, with feedback more beneficial with repetition (p = 0.011). These interactions also affected the outcome percent of time with correct compression depth. Increased anxiety was associated with decreased percent correct compression depth (p < 0.001).
Conclusion
Feedback emerged as important in determining chest compression performance. Chest compression quality was limited by the performer’s age and anxiety level. Future research should focus on identifying factors related to individual characteristics which may influence chest compression performance.
Keywords: CPR, Cardiopulmonary resuscitation training, CPR education, chest compression quality, manikin training, high quality cpr, cpr performance
Introduction
Cardiopulmonary resuscitation (CPR) is a high-stakes intervention which requires a prompt and competent response. Approximately 292,000 United States adult patients per year experience an in-hospital cardiac arrest.1 Rates of survival to hospital discharge range from 16% to 52%, depending on factors such as age and whether the presenting heart rhythm is shockable.2, 3 However, despite ongoing research and changes to resuscitation training guidelines, it is unknown which educational interventions most impact real-world performance and clinical outcomes.4 Therefore, isolating and examining specific aspects of performing CPR may be beneficial. Performance of proper chest compressions is an important component of performing high-quality CPR. Since chest compressions are often performed by individuals, understanding the potential impact of personal characteristics could provide insights leading to improved cardiac arrest outcomes.
Health care systems and other healthcare service providers across the United States mandate basic life support training for many of their direct care staff. In order to maintain CPR certification, training frequencies, which include the performance of chest compressions, range from 90-day repetition cycles to once every two years. The underlying assumption of such training is it will generalize into the patient care environment. However, when applying learning principles, it is imperative to clearly delineate the performance gap and how chest compression training can lead to improved clinical performance.
When seeking to understand CPR training gaps, an individual’s response to stress and anxiety from in-hospital cardiac arrests must be considered.5, 6 Current CPR training methods do not routinely assess anxiety-producing components which could affect physical performance. However, incorporating anxiety-producing components may enhance the value of simulation training.5 Alternatively, nursing students' CPR performance in a randomized trial, examining the effect of simulated family-witnessed resuscitation scenarios, found that timing of compressions and compression depth was improved when no family member was present.6 The result of these studies raise the question about the value of incorporating anxiety producing factors during chest compression training. Additionally, healthcare provider physical characteristics, such as age, may influence the degree to which they can perform high quality CPR.7, 8, 9
Real-time chest compression feedback devices have been used to help gauge and enhance compression performance. Evidence does support the use of real-time feedback devices during simulated cardiac arrest situations.10, 11, 12, 13, 14 While use of feedback devices is recommended by the American Heart Association,15 further evaluation of the use of such devices in some populations may be warranted.
These findings prompt questions about the relative importance of established chest compression training recommendations for repetition and feedback when considering individual characteristics. There is a paucity of literature examining these factors together in a single study. A lack of understanding about whether or how these factors interact with one another may undermine the effectiveness of strategies designed to improve chest compression performance and patient outcomes. Unlike other studies conducted to date, this study examined the use of an audio recording of code team sounds, as an anxiety producing factor, on the performance of chest compressions using a CPR manikin. The purpose of this study was to examine if personal characteristics impact chest compression performance while employing feedback, repetition, and an anxiety-inducing factor in registered nurses over time.
Methods
This randomized, controlled trial took place at two urban hospitals within a non-profit community health system in New York State, USA, and received approval from Walden University and the health system’s Institutional Review Boards.
Participants. Participants included licensed medical and surgical acute care registered nurses with current basic life support certification. Exclusion criteria were having performed CPR in the clinical setting or on a manikin within the 90 days preceding baseline, and currently working in critical care areas such as the intensive care unit or emergency department. Participants were recruited from a pool of approximately 650 employed nurses through flyers and verbal announcements at staff meetings. All participants signed an informed consent document prior to commencing research activities and were not compensated for their participation.
Interventions. The interventions studied included real-time audio and visual feedback on chest compression performance (“feedback”) from a Zoll R Series defibrillator (Chelmsford, MA USA) based on the 2015 American Heart Association CPR guidelines (those in place during data collection in April to July 2019) related to compression rate and compression depth. The Zoll R Series defibrillator uses an accelerometer to measure rate and depth, while documenting performance metrics. Participants not assigned to chest compression feedback received neither audio nor visual cues. A second intervention involved playing a recording of typical sounds heard, from the code team, during a hospital cardiac arrest situation (code team sounds). The recording was an audio-rendered portion of a simulated cardiac arrest situation developed by the Kaiser Permanente School of Anesthesia (2016) played at maximum volume on a computer. Participants were assigned to one of three conditions: no chest compression feedback and no code team sounds, code team sounds without chest compression feedback, and code team sounds with chest compression feedback. Participants performed chest compression under their assigned condition at 30 and 60 days after their baseline session.
Outcomes and Key Measurements. The primary outcome was chest compression performance during a two-minute session on a CPR manikin, defined as the average of the proportion of time with correct compression rate and proportion of time with correct compression depth recorded by the Zoll R Series defibrillator. The accelerometer was placed at the correct position for proper CPR compressions by the first author. The same CPR manikin was used for all sessions. The guidelines for acceptable chest compressions include a rate of 100–120 per minute and a depth of 2–2.4 inches (5–6 cm).15 Immediately after their chest compression session, participants completed the Cognitive and Somatic Anxiety Questionnaire, a 20-question, validated self-report instrument which assesses the physical and mental effects of anxiety within the immediate time frame (permission received from Elsevier).16, 17 At baseline, participants provided information on gender, age group, years in nursing, category of nursing unit, and whether they had a current CPR certification. At each CPR session the participant indicated whether they had performed CPR on a patient or on a manikin within the last 30 days.
Randomization. The first author employed a simple random sampling strategy to assign participants in a 1:1:1 fashion to one of the three study conditions. Pieces of paper were marked with a code-linked study group (i.e., “1,” “2,” “3”), which were then folded so that the number was not visible and placed in a container. When the participant arrived for the 30-day session, the first author selected one piece of paper from the container without looking at it. Due to the nature of the study, neither the participants nor the first author were blinded to study conditions.
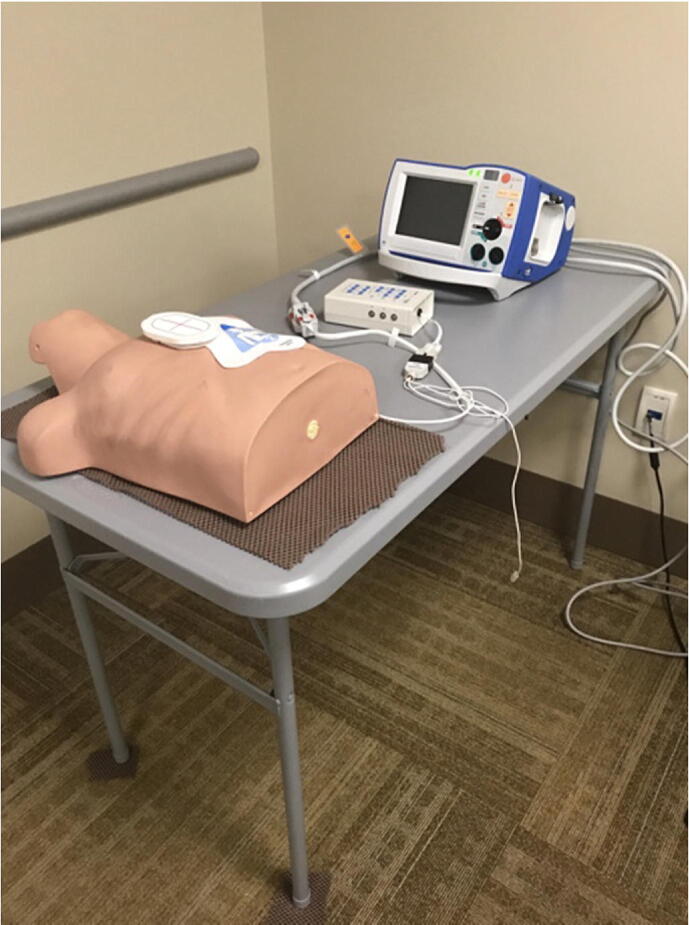
Data collection. Fig. 1 describes the flow of participants through the trial. Individuals agreeing to participate completed the baseline two-minute chest compression session which for all participants included chest compression feedback without code team sounds. For all chest compression sessions, the first author placed a portable table against a wall for stability and two non-slip pads under the table legs to minimize table movement. A non-slip pad was placed under the manikin (Fig. 2). Thirty- and 60-day sessions began with a two-minute chest compression session, immediately followed by completion of the Cognitive and Somatic Anxiety Questionnaire and the question on whether the participant had performed CPR within the last 30 days. Study participation ended after the 60-day session.
Fig. 1.
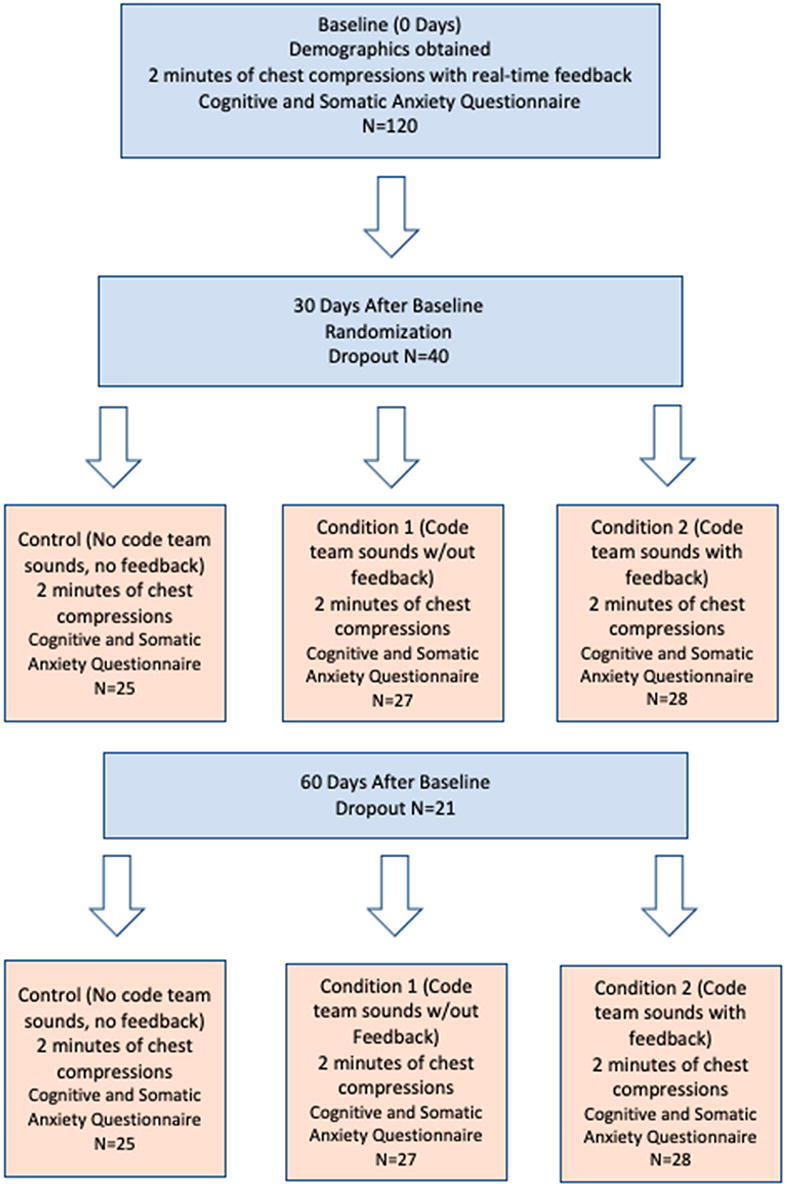
Participant flow through the study.
Fig. 2.
Setup showing the CPR manikin, portable table, nonslip material under the manikin and front table legs, and Zoll Series R Defibrillator on the table.
Sample size and statistical analysis. The sample size for the study was calculated using G*Power 3.1 (Heinrich Heine Universität, Düsseldorf, Germany), assuming a Cohen’s d effect size of 0.25, a type 1 error of 5%, type 2 error of 20% and correlation of 0.5 within repeated measures. The estimated sample size of 108 was increased to 120 to account for attrition during the trial. The Wilcoxon rank sum test compared study groups with respect to chest compression performance at each time point. Linear mixed effects modeling with random intercepts accounted for repeated measures within subjects and allowed for use of the data from participants who dropped out prior to 60 days after an exploratory analysis indicated data were missing at random. Data were analyzed using R version 3.4.3 (The R Foundation for Statistical Computing, Vienna, Austria) and SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
One hundred-twenty nurses agreed to participate in the study. Of those returning for the 30-day session, 25 were assigned to the control condition, 27 to code team sounds without feedback (condition 1), and 28 to code team sounds with feedback (condition 2). Overall, attrition from baseline to 30-days was 40 (33%), increasing to 61 (51%) at 60-days. Attrition from 30-days to 60-days did not differ by study condition (Table 1, p = 0.6622). The common reasons provided to the first author by participants for not returning for further data collection included work scheduling changes and illness. There was no crossover to an unassigned study condition. Table 1 provides participant characteristics by study condition. Females represented 92.5% of participants (n = 111), which closely represents the U.S. registered nurse population.18 All participants reported they were current with their CPR certification and none had reported they performed CPR on a patient or manikin within the 90 days prior to baseline or during the study period.
Table 1.
Descriptive characteristics of study participants.
| Control Group (No code team sounds, no feedback) | Code team sounds without feedback | Code team sounds with feedback | |
|---|---|---|---|
| Age Group | |||
| ≤25 | 4 (16%) | 6 (22.2%) | 5 (17.9%) |
| 26–35 | 5 (20%) | 9 (33.3%) | 10 (35.7%) |
| 36–45 | 7 (28%) | 5 (18.5%) | 4 (14.3%) |
| 46–55 | 1 (4%) | 3 (11.1%) | 6 (21.4%) |
| ≥56–65 | 8 (32%) | 4 (14.8%) | 3 (10.7%) |
| Years as Registered Nurse | |||
| <5 | 8 (32%) | 11 (40.7%) | 9 (32.1%) |
| 05-Sep | 4 (16%) | 4 (14.8%) | 8 (28.6%) |
| Oct-19 | 3 (12%) | 5 (18.5%) | 3 (10.7%) |
| 20–29 | 4 (16%) | 3 (11.1%) | 4 (14.3%) |
| ≥30 | 6 (24%) | 4 (14.8%) | 4 (14.3%) |
| Mean Anxiety Level at Baseline1 | |||
| 1.00–1.50 | 3 (12%) | 1 (3.7%) | 0 (0%) |
| 1.51–2.00 | 7 (28%) | 11 (40.7%) | 19 (67.9%) |
| 2.01–2.50 | 5 (20%) | 5 (18.5%) | 8 (28.6%) |
| 2.51–3.00 | 6 (24%) | 5 (18.5%) | 1 (3.6%) |
| 3.01–3.50 | 2 (8%) | 5 (18.5%) | 0 (0%) |
| 3.51–4.00 | 2 (8%) | 0 (0%) | 0 (0%) |
| Attrition at 60-days | 8 (32%) | 7 (26%) | 6 (21%) |
Lower scores indicate a lower level of anxiety.
Table 2 provides details on chest compression performance by study condition and time, for the primary outcome and for the individual components of percent of time with correct depth and percent of time with correct rate. Results at baseline demonstrate no statistically significant difference among the groups, including participants who dropped out after the baseline session. Only the 60-day time point showed statistically significant differences among the groups, with improved chest compression overall performance and depth percent correct among participants hearing code team sounds and receiving feedback.
Table 2.
Cardiopulmonary Resuscitation Performance by Time and Study Group.
| Chest Compression Performance | Attrition After Baseline | Control Group (No code team sounds, no feedback) | Code team sounds without feedback | Code team sounds with feedback | |
|---|---|---|---|---|---|
| Time Point | Mean (SD) | Mean (SD) | Mean (SD) | Mean | p-value |
| Baseline | 54.7 (22.4) | 50.2 (30.9) | 58.8 (24.0) | 60.7 (24.4) | 0.504 |
| 30 Days | – | 45.5 (26.7 | 39.8 (26.4) | 56.7 (31.0) | 0.078 |
| 60 Days | – | 31.2 (23.7) | 39.7 (33.7) | 67.2 (20.9) | <0.001 |
| Chest Compression Depth | Mean (SD) | Mean (SD) | Mean (SD) | Mean | p-value |
| Baseline | 40.4 (31.3) | 39.6 (32.3) | 46.0 (30.1) | 49.4 (29.3) | 0.553 |
| 30 Days | – | 38.6 (30.8) | 33.5 (24.5) | 54.0 (32.3) | 0.067 |
| 60 Days | – | 22.6 (24.3) | 35.0 (29.5) | 63.6 (27.0) | <0.001 |
| Chest Compression Rate | Mean (SD) | Mean (SD) | Mean (SD) | Mean | p-value |
| Baseline | 69.1 (26.7) | 60.8 (34.9) | 71.7 (30.0) | 72.1 (29.8) | 0.595 |
| 30 Days | – | 49.1 (36.8) | 46.1 (40.3) | 59.3 (39.8) | 0.455 |
| 60 Days | – | 39.7 (38.9) | 44.3 (44.8) | 70.8 (32.0) | 0.104 |
1CC = chest compressions. CC performance = mean of the percent of time during the session the CC rate was within guidelines and the percent of time during the session the CC depth was within guidelines.
CC Depth = the percent of time during the session the CC depth was within guidelines.
CC Rate = the percent of time during the session the CC rate was within guidelines.
2The number of participants who dropped out after baseline was n = 40. For the control group, the number of participants was: baseline and 30-days, n = 25; 60-days, n = 17. For code team sounds without feedback, the number of participants was: baseline and 30-days, n = 27; 60-days, n = 20. For code team sounds with feedback, the number of participants was: baseline and 30-days, n = 28; 60-days, n = 22.
Code team sounds were not associated with the Cognitive and Somatic Anxiety Questionnaire score. At 30-days, participants hearing code team sounds had a mean (SD) anxiety of 2.18 (0.55) and those not hearing code team sounds had a mean (SD) anxiety of 2.33 (0.76) (p = 0.3207). At 60-days, these figures were 2.11 (0.55) for code team sounds and 2.03 (0.66) for no code team sounds (p = 0.6349).
Linear mixed-effects analyses identified factors which affected the primary outcome, chest compression performance, and its individual components related to depth and rate of compressions. The study condition factors of interest were time (baseline, 30-days, 60-days), feedback and playing of code team sounds. Table 3 presents the final model for the primary outcome. Two interactions affected chest compression performance (denoted by asterisk in Table 3). Interactions indicate that the effect of one factor on an outcome depends upon the level of a second independent variable. For chest compression performance, the effect of feedback depended on: 1) age, with feedback having a less beneficial effect among older participants (p = 0.041); and 2) time, with feedback having a more beneficial effect at 30 and 60 days (p = 0.011). When added to the model in Table 3, neither anxiety (p = 0.085), or years’ experience as a registered nurse (p = 0.782), had a statistically significant association with chest compression performance.
Table 3.
Linear Mixed Effects Model for the Primary Outcome of CPR Performance.
| Factor | Est β1 | se(β)2 | DF3 | t-value | p-value |
|---|---|---|---|---|---|
| Intercept | 62.77 | 12.73 | 118 | 4.93 | <0.001 |
| Age Group (each level up) | −0.0001 | 2.08 | 134 | −0.00 | 0.999 |
| Cardiac Arrest Related CPR Hospital Noises | −5.17 | 4.73 | 134 | −1.09 | 0.277 |
| Feedback (Yes vs. No) | 0.08 | 13.98 | 134 | 0.01 | 0.995 |
| Time (baseline, 30 days, 60 days) | −8.45 | 4.29 | 134 | −1.97 | 0.051 |
| Age Group × Feedback* | −4.43 | 2.15 | 134 | −2.06 | 0.041 |
| Time × Feedback* | 14.50 | 5.60 | 134 | 2.59 | 0.011 |
*interaction term: 1) does the effect of feedback depend on age group; 2) does the effect of feedback depend on the time point.
Est β = the estimated change in the outcome per unit increase in the predicting variable.
se(β) = the standard error of the estimated β, or an indication of its accuracy.
DF = degrees of freedom, the number of independent values used in calculating the β.
The interactions identified between age group and feedback, and time and feedback were also found when the outcome was the percent of time compressions were at the correct depth (Table 4). The benefits of feedback diminished with increasing age (p < 0.05) and increased at 30 and 60 days (p = 0.018). Furthermore, increased anxiety was associated with decreased percent correct depth compressions (p = 0.003). Code team sounds had no statistically significant association (p = 0.902).
Table 4.
Linear Mixed Effects Model for CPR Performance: Percent of Time with Correct Depth.
| Factor | Est β1 | se(β)2 | DF3 | t-value | p-value |
|---|---|---|---|---|---|
| Intercept | 76.82 | 17.68 | 118 | 4.34 | <0.001 |
| Age Group (each level increase) | −0.50 | 2.29 | 133 | −0.22 | 0.827 |
| Feedback (Yes vs. No) | −3.36 | 17.42 | 133 | −0.19 | 0.848 |
| Cognitive and Somatic Anxiety Questionnaire (each 1pt increase) | −9.72 | 3.17 | 133 | −3.07 | 0.003 |
| Code Team Sound | 0.6837 | 5.56 | 133 | 0.12 | 0.902 |
| Time (baseline, 30 days, 60 days) | −8.80 | 5.47 | 133 | −1.61 | 0.110 |
| Age Group × Feedback* | −5.13 | 2.59 | 133 | −1.98 | <0.05 |
| Time × Feedback* | 16.74 | 6.97 | 133 | 2.40 | 0.018 |
*interaction term: 1) does the effect of feedback depend on age group; 2) does the effect of feedback depend on the time point.
Est β = the estimated change in the outcome per unit increase in the predicting variable.
se(β) = the standard error of the estimated β, or an indication of its accuracy.
DF = degrees of freedom, the number of independent values used in calculating the β.
With respect to the percent of time compressions were performed at the correct rate, only feedback had a clear effect in improving the percent correct rate (data not shown), with no statistically significant interactions identified.
Discussion
The results of this study suggest that the effectiveness of standard CPR training methods varies according to an individual’s characteristics. By assessing chest compression performance at baseline, 30 days, and 60 days under varying conditions, we found that only the group with feedback performed better than the group without feedback, although this benefit declined among older participants. Anxiety had a negative effect on maintaining correct compression depth. Unlike some investigators, we did not observe an increase in the quality of CPR performance specifically due to 30-day repetition of practice sessions in the control group.19, 20, 21 The findings suggest chest compression training repetition is not as important as in-the-moment performance feedback.
The inability of feedback to improve chest compression performance among older participants requires further examination, as this study cannot address specific age-related factors. Our results align with the findings from Park et al, which reported the main variable associated with poor quality CPR was older age.7 However, other studies have shown individual characteristics related to physical fitness, which may or may not be related to age, may enhance CPR performance.9, 22 Therefore, a study focused on individual characteristics and examining age-related factors on chest compression quality could be valuable.
The limitations of this study primarily relate to generalizability of the results outside the participant population studied. The sample involved a relatively small group of hospital-based registered nurses from general medical and surgical units and where males comprised only 9 of the 120 participants. The low number of male participants did not allow for assessing gender-related differences with respect to chest compression performance, although it was representative of the nursing population in the United States. Although attrition was larger than expected, use of linear effects analysis and lack of any identified differences between participants who dropped out and those who remained suggest we obtained unbiased results. Future research should aim at assessing environment, anxiety, and age-related factors which may adversely impact the performance of high-quality chest compressions. Identifying optimal thresholds would be helpful for determining who is most likely to execute chest compressions successfully. This could provide a consistent, high-quality approach to chest compression that may improve results and would allow the healthcare member (who is not comfortable or frequently trained in CPR) to focus on providing initial interventions until the code team arrives.
There are still many unanswered questions related to CPR training. This study explores the impact of anxiety on chest compressions and supports the value of receiving real-time chest compression feedback for the lower aged bracket participants. However, the findings also indicated that percent of time with correct rate was higher than percent of time with correct depth for all groups over all time points (Table 2). Attaining the correct chest compression rate may not be as affected by anxiety or age as these variables have on correct compression depth. Training which includes receiving chest compression feedback and how to manage anxiety could help to optimize performance.
Conclusions
Current chest compression training mentality is standardized, which does not allow for considering individual differences. However, the results of this study suggest it may be beneficial to customize training according to an individual’s characteristics. If a person is not able to perform high-quality chest compression, repetition and feedback will not be enough to correct that gap. Optimizing chest compression performance outcomes may best be enhanced by expanding the focus beyond current learning-related outcomes. Instead, future research should include identifying factors related to individual characteristics which may influence chest compression performance.
Funding
This research was not supported by any source of funding.
Conflicts of interest
The authors have no conflicts of interest to declare.
References
- 1.Holmberg M.J., Ross C.E., Fitzmaurice G.M., et al. Annual incidence of adult and pediatric in-hospital cardiac arrest in the United States. Circ Cardiovasc Qual Outcomes. 2019;9:e005580. [PMC free article] [PubMed] [Google Scholar]
- 2.Benjamin E.J., Virani S.S., Callaway C.W., et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association [published correction appears in Circulation. 2018 Mar 20;137:e493] Circulation. 2018;137:e67–e492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 3.Andersen L.W., Holmberg M.J., Berg K.M., Donnino M.W., Granfeldt A. In-Hospital Cardiac Arrest: A Review. JAMA. 2019;321:1200–1210. doi: 10.1001/jama.2019.1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheng A., Magid D.J., Auerbach M., et al. Part 6: Resuscitation education science: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S551–S579. doi: 10.1161/CIR.0000000000000903. [DOI] [PubMed] [Google Scholar]
- 5.Hordacre B., Immink M.A., Ridding M.C., Hillier S. Perceptual-motor learning benefits from increased stress and anxiety. Hum Mov Sci. 2016;49:36–46. doi: 10.1016/j.humov.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Kenny G., Bray I., Pontin D., Jefferies R., Albarran J. A randomised controlled trial of student nurse performance of cardiopulmonary resuscitation in a simulated family-witnessed resuscitation scenario. Nurse Educ Pract. 2017;24:21–26. doi: 10.1016/j.nepr.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Park H.J., Jeong W.J., Moon H.J., et al. Factors associated with high-quality cardiopulmonary resuscitation performed by bystander. Emerg Med Int. 2020;2020:8356201. doi: 10.1155/2020/8356201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin C.-C., Kuo C.-W., Ng C.-J., Li W.-C., Weng Y.-M., Chen J.-C. Rescuer factors predict high-quality CPR—a manikin-based study of health care providers. Am J Emerg Med. 2016;34:20–24. doi: 10.1016/j.ajem.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 9.Ock S.M., Kim Y.M., Chung J.h., Kim S.H. Influence of physical fitness on the performance of 5-minute continuous chest compression. Eur J Emerg Med. 2011;18:251–256. doi: 10.1097/MEJ.0b013e328345340f. [DOI] [PubMed] [Google Scholar]
- 10.Buléon C., Delaunay J., Parienti J.J., et al. Impact of a feedback device on chest compression quality during extended manikin CPR: a randomized crossover study. Am J Emerg Med. 2016;34:1754–1760. doi: 10.1016/j.ajem.2016.05.077. [DOI] [PubMed] [Google Scholar]
- 11.Wee J.C., Nandakumar M., Chan Y.H., et al. Effect of using an audiovisual CPR feedback device on chest compression rate and depth. Ann Acad Med Singap. 2014;43:33–38. [PubMed] [Google Scholar]
- 12.Kirkbright S., Finn J., Tohira H., Bremner A., Jacobs I., Celenza A. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation. 2014;85:460–471. doi: 10.1016/j.resuscitation.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 13.Gugelmin-Almeida D., Tobase L., Polastri T.F., Peres H.H.C., Timerman S. Do automated real-time feedback devices improve CPR quality? A systematic review of literature. Resusc Plus. 2021;6 doi: 10.1016/j.resplu.2021.100108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goharani R., Vahedian-Azimi A., Farzanegan B., et al. Real-time compression feedback for patients with in-hospital cardiac arrest: a multi-center randomized controlled clinical trial. J Intensive Care. 2019;7:5. doi: 10.1186/s40560-019-0357-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kleinman M.E., Brennan E.E., Goldberger Z.D., et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S414–S435. doi: 10.1161/CIR.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz G.E., Davidson R.J., Goleman D.J. Patterning of cognitive and somatic processes in the self-regulation of anxiety: effects of meditation versus exercise. Psychosom Med. 1978;40:321–328. doi: 10.1097/00006842-197806000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Steptoe A., Kearsley N. Cognitive and somatic anxiety. Behav Res Ther. 1990;28:75–81. doi: 10.1016/0005-7967(90)90057-p. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. 2019. Brief summary results from the 2018 National Sample Survey of Registered Nurses, Rockville, Maryland, USA
- 19.Oermann M.H., Krusmark M.A., Kardong-Edgren S., Jastrzembski T.S., Gluck K.A. Training interval in cardiopulmonary resuscitation. PLoS One. 2020;15(1):e0226786. doi: 10.1371/journal.pone.0226786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson R., Sebaldt A., Lin Y., Cheng A. Optimal training frequency for acquisition and retention of high-quality CPR skills: A randomized trial. Resuscitation. 2019;135:153–161. doi: 10.1016/j.resuscitation.2018.10.033. [DOI] [PubMed] [Google Scholar]
- 21.Niles D.E., Nishisaki A., Sutton R.M., et al. Improved retention of chest compression psychomotor skills with brief “rolling refresher” training. Simul Healthc. 2017;12:213–219. doi: 10.1097/SIH.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 22.Chang C.H., Hsu Y.J., Li F., et al. The feasibility of emergency medical technicians performing intermittent high-quality cardiopulmonary resuscitation. Int J Med Sci. 2021;18:2615–2623. doi: 10.7150/ijms.59757. [DOI] [PMC free article] [PubMed] [Google Scholar]