Abstract
Hawai‘i Island faces a growing shortage of obstetric and gynecology providers. Increased exposure of obstetrics and gynecology residents to rural rotations during their core training may increase their interest in rural practice after graduation. In an effort to address the health care needs of women on Hawai‘i Island, the University of Hawai‘i Obstetrics and Gynecology Residency Program established a 4-week required gynecology rotation in the town of Hilo. Between July 2019 and June 2020, third- and fourth-year obstetrics and gynecology residents provided outpatient gynecologic care and participated in gynecologic surgeries at Hilo-based medical facilities. A total of 9 residents participated in this Hilo-based rotation. This retrospective study extracted data from post-rotation evaluations. Eight out of 9 participating residents (89%) felt that the rotation slightly or far exceeded their expectations. After the rotation, 7 residents (78%) reported an interest in practicing in a rural community, while only 3 residents (33%) reported having this interest prior to the rotation. Underserved rural areas seeking to recruit and retain obstetrics and gynecology physicians may benefit from partnering with residency training programs.
Keywords: Medical Education, Obstetrics and Gynecology, Rural Medicine, Medically Underserved Area
Introduction
Across the United States, rural communities are experiencing a shortage of obstetrics and gynecology (ObGyn) providers1 with less than 3% of ObGyn physicians electing to practice in rural small towns.2 The state of Hawai‘i faces a state-wide shortage of medical providers. This deficiency is most significant in rural communities on neighbor islands compared to the island of O‘ahu where 70% of Hawai‘i state residents live.3 O‘ahu is home to the densely populated capitol city of Honolulu and the only medical school in the state. The other 400 000 residents live on the smaller, less populated islands of the Hawai‘i archipelago,4 where they face a growing deficiency of ObGyn clinicians.3 Hawai‘i Island, the largest of these rural islands, is home to 200 000 residents and is short 11 ObGyn physicians to meet the needs of its residents.3 This growing ObGyn physician shortage in rural areas is problematic, likely contributing to health disparities compared to those living in urban areas.1,5 Nationwide, individuals living in rural communities face decreased access to reproductive health services, delayed entry into prenatal care, and higher rates of unintended pregnancy.1
Efforts to address these reproductive health disparities include initiatives to fill the shortage of ObGyn providers.1 Like many rural areas, Hawai‘i Island experiences significant challenges to recruiting and retaining clinicans.6 Strategies to improve physician recruitment to rural areas have included loan repayment programs,3,7 developing a health care pipeline for individuals with ties to rural areas,3,8-10 and introducing rural medicine training opportunities for current medical students and resident physicians through elective and required rotations.8,11 In an effort to fulfill its mission of educating future health care professionals to deliver high-quality health care throughout the state of HawaiȈi and the Pacific,12 the University of Hawai‘i John A Burns School of Medicine (JABSOM) champions the development of neighbor island learning opportunities for resident physicians. Currently, 7 of the 8 JABSOM residency programs offer training opportunities on neighbor islands, including the rural islands of Maui, HawaiȈi, and Kaua.i (see Table 1). Investment in these rotations may be especially vital as previous studies demonstrate that required rural medicine rotations during residency are associated with higher rates of choosing rural settings for permanent practice.13-14 Rural rotations may also enhance the learning experience of ObGyn trainees, providing much-needed opportunities to assist in major gynecology procedures in a community hospital setting. These experiences expose trainees to both the unique health needs of rural populations and the challenges of practicing without immediate access to subspecialists.1,15 Importantly, immersion into a rural community allows junior physicians to meet potential colleagues and mentors for their post-training career, which contributes as a key role in retention of rural medicine physicians.16
Table 1.
Availability of Neighbor Island Rotations among John A. Burns School of Medicine Residency Programs as of 2020
| Program | Neighbor Island Rotation | Duration | Location | Topic |
|---|---|---|---|---|
| Family Medicine | Required | 8 weeks | Maui, Hawai‘i, or Kaua‘i | Rural medicine |
| Elective | 1 to 2 weeks | Maui, Hawai‘i, or Kaua‘i | Varies | |
| General Surgery | Required | 4 weeks | Hawai‘i | Rural medicine |
| Internal Medicine | Required for Primary Care Track | 4 weeks | Hawai‘i | Rural medicine |
| Elective | 4 weeks | Hawai‘i | Rural medicine | |
| Obstetrics & Gynecology | Required | 8 weeks | Hawai‘i | Gynecology |
| Orthopedic Surgery | Not available | - | - | - |
| Pathology | Required | 2 to 4 weeks | Maui | Forensic Pathology |
| Pediatrics | Elective | 2 to 4 weeks | Hawai‘i or Kaua‘i | Rural medicine |
| Psychiatry | Elective | 4 weeks | Kaua‘i | Community Psychiatry |
The JABSOM ObGyn residency program has had 2 neighbor island rotations. In 2009, the department developed a structured 4-week rotation in Maui. Over the course of 7 years, 41 ObGyn residents completed this rotation, and 4 (9.8%) participants chose to return to Maui for permanent practice without any prior connection to the area. In 2016, the Maui rotation concluded, and since that time no residency graduates have elected to practice in the Maui community.
After the Maui rotation ended, the JABSOM ObGyn residency program began the process of establishing a permanent rotation on Hawai‘i Island with the long-term goals of addressing the shortage of ObGyn physicians in this community (see Figure 1). The development of this training opportunity was contingent on adequate faculty presence, which was achieved by securing an agreement for department faculty to be embedded in Bay Clinic, a local Federally Qualified Health Center (FQHC), and establishing a faculty practice location in Hilo, the largest town on the Hawai‘i Island.17 A not-for-profit 501c3 organization, the Hawai’i Health Systems Corporation (HHSC), funded this rotation, covering costs of resident travel, lodging, and full-time equivalent expenses. This non-profit’s mission includes supporting community hospitals in meeting the health care needs of HawaiȈi State residents.18 With HHSC’s funding, the JABSOM ObGyn Residency Program successfully launched a rotation for third- and fourth-year residents in Hilo in July 2019. During residency, each ObGyn resident completes this month-long rotation twice during the latter 2 years of training. Rotating residents participate in gynecologic surgeries and consultations at Hilo Medical Center and provide outpatient care in both faculty practice and FQHC settings. The initial curriculum focused on minimally invasive hysterectomy techniques and preventive well-woman care. As senior-level trainees, these residents have the surgical skills and experience needed to fully participate in the wide breadth of rural gynecology practice. Additionally, these residents lead a monthly Hilo-based journal club for both academic faculty and community physicians. They also participate in regularly scheduled meetings with the local site director and weekly department conferences through video conferencing. Currently, this is the only rotation on a neighbor island available to JABSOM ObGyn residents. With the development of this new Hilo-based training opportunity, this study aimed to evaluate resident satisfaction with the rotation and assess self-perceived interest in practicing in a rural setting using data from previously collected rotational evaluations.
Figure 1.
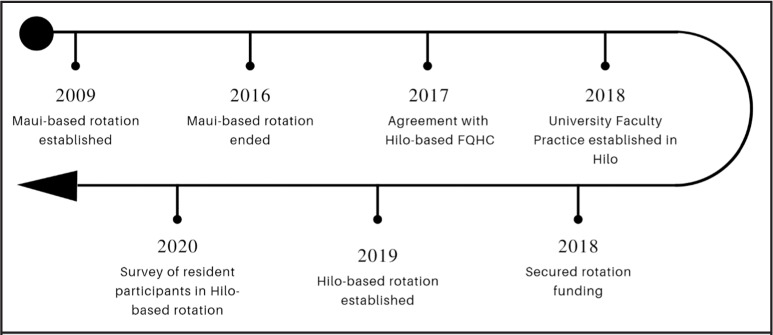
Timeline of Rural Rotation Development at the John A. Burns School of Medicine
FQHC = federally qualified health center
Methods
This retrospective study was submitted to the University of Hawai‘i Human Studies Program and was classified as not human subject research (Protocol #2022-00504). Anonymous data was extracted from an existing data previously collected as part of the ObGyn Residency Program’s annual program evaluation process. In July 2020, the department distributed an 11-item web-based evaluation to all ObGyn residents who had participated in the Hilo-based rotation within the previous 12 months. The residency program regularly surveys residents and faculty concerning the quality of clinical rotations and educational interventions using both internal and external assessments. The evaluation included 10 items with a 5-point Likert scale and 1 question eliciting further free-text comments. Questions focused on assessing quality of clinical experiences, interest in practicing in rural settings, perception of faculty, level of interaction with other trainees, perception of the required reading volume, and satisfaction with housing. No incentives were provided. The aggregated responses related to resident satisfaction with the rotation and interest in rural practice were extracted foranalysis. Survey responses were analyzed using descriptive statistics in Microsoft Excel 2016 Version 16.0.4266 (Microsoft Corporation, Redmond, WA).
Results
From July 2019 to June 2020, 9 JABSOM ObGyn residents completed the new rotation on Hawai‘i Island. Due to 2019 novel coronavirus (COVID-19) pandemic related travel and training restrictions, the rotation was temporarily disrupted for 3 months in spring 2020. Data from 9 evaluations were analyzed in this study. Overall, 8 rotation participants (89%) felt that the rotation slightly exceeded or far exceeded their expectations. Most participants reported feeling satisfied or very satisfied with the gynecology surgery experience (89%) and teaching quality (100%) during the rotation. Seven residents (78%) expressed at least some interest in practicing in a rural community after the rotation, while only 3 participants (33%) reported having at least some interest in practicing in this setting prior to the rotation. See Table 2 for details.
Table 2.
ObGyn Resident Evaluation Results for Hawai‘i Island Rotation (N = 9)
| Far Below Expectations | Slightly Below Expectations | Met Expectations | Slightly Exceeded Expectations | Far Exceeded Expectations | |
| Overall, how would you rate your Hilo experience? | 0 | 0 | 1 (11%) | 7 (78%) | 1 (11%) |
| Very Dissatisfied | Dissatisfied | Neither Satisfied Nor Dissatisfied | Satisfied | Very Satisfied | |
| Were you satisfied or dissatisfied with… | |||||
| …Your experience in [Federally Qualified Health Center] clinic? | 0 | 1 (11%) | 0 | 2 (22%) | 6 (67%) |
| …Your [Hilo University Practice] clinic experience? | 0 | 0 | 0 | 1 (11%) | 8 (89%) |
| …Your gynecologic surgery experience in Hilo? | 0 | 0 | 1 (11%) | 5 (56%) | 3 (33%) |
| …The teaching and supervision by the [Hilo University Practice] faculty? | 0 | 0 | 0 | 0 | 9 (100%) |
| Not at All Interested | Not So Interested | Somewhat Interested | Very Interested | Extremely Interested | |
| Prior to this experience, how interested were you in practicing in a rural community like Hilo after residency? | 2 (22%) | 4 (44%) | 2 (22%) | 1 (11%) | 0 |
| After this experience, how interested were you in practicing in a rural community like Hilo after residency? | 0 | 2 (22%) | 5 (56%) | 0 | 2 (22%) |
Discussion
This study aimed to evaluate satisfaction and interest in rural medicine among residents participating in the first-year of a Hilo-based gynecology rotation. One year after implementing a rural medicine rotation for obstetrics and gynecology residents in Hilo, participating residents expressed high satisfaction with the experience and reported an increased interest in practicing in a rural setting. Frequent assessment of this experience is vital to developing a sustainable rotation that meets the needs of both the resident trainees and the Hilo community. Although this preliminary data includes a small sample size and cannot verify true intent to practice in a rural setting, these findings are consistent with the career choices observed among resident and fellowship graduates since the rotation as established. Two of 16 recent ObGyn department graduates from the classes of 2020 and 2021 (13%; 1 resident and 1 fellow) have already started permanent clinical positions on Hawai‘i Island after the Hilo rotation was established. The remaining 2020 and 2021 graduates chose to practice in urban settings. Future studies assessing long-term career choices of JABSOM obstetrics and gynecology resident graduates are warranted to further evaluate the true influence of this rotation.
The majority of participants in this study reported the Hilo-based rotation exceeded their expectations, suggesting a positive overall experience. While additional qualitative studies may be needed to better understand the factors contributing to the successful reception of this rotation, it is hypothesized that the experience of practicing in a close-knit community and the diversity of surgical case volume may be favorable components. In recent years, the number of hysterectomies have decreased19 and an increasing number of these gynecology cases are now performed using a surgical robot in urban teaching hospitals.20 These changes have led to a decrease in the number of abdominal and laparoscopic hysterectomy training opportunities available to obstetrics and gynecology residents on O‘ahu,21 raising concerns about graduating resident competency for these cases if the current trend continues. In contrast, the majority of hysterectomies in rural hospitals are performed without robot-assistance.22 This difference in approach may create a major barrier to new resident graduates considering rural practice, where they need to possess competency to independently perform non-robotic approaches to major gynecologic surgeries. In Hilo, the JABSOM ObGyn Residency Program’s faculty perform hysterectomies without the use of a robot. It is hypothesized that exposure to abdominal and laparoscopic hysterectomies likely contributes to a much-needed component of gynecology resident education, and potentially improves resident comfort with practicing in rural communities without access to robot-assisted surgery. However, future studies are needed to assess whether this may be true.
While rural rotations may be key to addressing disparities in access to care within rural areas of the state of HawaiȈi,8,11 the JABSOM ObGyn Residency Program faced significant barriers to launching and continuing this rotation. These barriers included: (1) the challenges of establishing and supporting new clinical faculty, (2) the administrative burden of coordinating educational experiences with multiple clinics and a hospital, and (3) the monetary costs of travel arrangements and lodging. The residents required living arrangements with sufficient privacy to accommodate residents with families. Housing also needed to be close to the hospital in order to respond quickly to emergent consultations while on call. Additionally, the COVID-19 pandemic brought unexpected challenges, temporarily disrupting the Hilo rotation. Even after the rotation resumed, COVID-19 continued to exacerbate the administrative challenges of coordinating these programs, such as difficulties navigating quarantine exemptions, changing COVID-19 testing requirements for each clinic and hospital, and the potential need to recall the rotating resident back to Honolulu due to unexpected gaps in resident call coverage. However, this pandemic also revealed the importance of having sufficient health care workers dedicated to rural communities throughout the state, and the limitations of relying on fly-in or locum clinicians. The ongoing health care provider shortage highlights the value of these rotations to ensure access to health care across the state of HawaiȈi.
Limitations of this study include the small sample size and the setting in a single institution. As a result, the findings of this survey may not be generalizable to other training programs or settings. The analysis also depends on self-reported data collected at a single time point, requiring residents to retroactively assess their own interest in rural medicine before and after the rotation. This approach and reliance on self-reported data have the potential to introduce bias and are major limitations of this study. This retrospective cross-sectional study cannot assess the true effect of this rotation on resident intentions. Additionally, this study did not assess for factors unrelated to the Hilo rotation, such as place of birth and proximity of family, which may also influence graduating residents’ career decisions. Further qualitative research is needed to understand why this rotation has been so well received by the participants. Future studies are needed to compare costs and benefits of this initiative and evaluate this rotation’s long-term effects on recruitment of graduating residents, retention of established physicians, and health care outcomes for women in the Hilo community.
Although opportunities for rural medicine exposure are rare among US ObGyn training programs,23 JABSOM ObGyn residents are now routinely experiencing rural medicine through a mandatory, structured clinical rotation as part of a long-term plan to address the growing ObGyn shortage on the state of HawaiȈi neighbor islands. Future plans for this rotation include expanding the rotation to include additional community physicians and incorporating more opportunities for community engagement. Although the initial positive response among rotation participants is promising, ongoing assessments are needed to ensure long-term sustainability and success of this rotation.
Acknowledgements
Ginny Kamikawa; Kathleen Katt MD; Linda Rosen MD
Abbreviations and Acronyms
- COVID-19
Coronavirus Disease of 2019
- FQHC
Federally Qualified Health Center
- HHSC
Hawai‘i Health Systems Corporation
- JABSOM
John A Burns School of Medicine
- ObGyn
Obstetrics and Gynecology
Conflict of Interest
None of the authors identify a conflict of interest.
References
- 1.American College of Obstetricians and Gynecologists Committee Opinion No. 586: Health disparities in rural women. Obstet Gynecol. 2014;123((2)):384–388. doi: 10.1097/01.AOG.0000443278.06393.d6. [DOI] [PubMed] [Google Scholar]
- 2.Chen F, Fordyce M, Andes S, Hart LG. Which medical schools produce rural physicians? A 15-year update. Acad Med. 2010;85((4)) doi: 10.1097/ACM.0b013e3181d280e9. [DOI] [PubMed] [Google Scholar]
- 3.Withy K. University of Hawaii; 2019. Report to the 2020 legislature: Annual report on findings from the Hawai‘i physician workforce assessment project. [Google Scholar]
- 4.Latest Population Estimate Data Department of Business, Economic Development, & Tourism. Updated May 2022. Acessed May 12, 2022. https://census.hawaii.gov/home/population-estimate.
- 5.Cosby AG, McDoom-Echebiri MM, James W, Khandekar H, Brown W, Hanna HL. Growth and Persistence of place-based mortality in the United States: The rural mortality penalty. Am J Public Health. 2019;109((1)):155–162. doi: 10.2105/AJPH.2018.304787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ayers-Kawakami J, Paquiao DF. Addressing health disparities in rural populations: The case of Hawaii county. J Nursing Practice Applications & Reviews of Research. 2017;7((2)):40–48. [Google Scholar]
- 7.Jacobs JL, Kasuya R, Sakai D, Haning W, Izutsu S. Medical education in paradise: Another facet of Hawaii. Med Teach. 2008;30((5)):490–495. doi: 10.1080/01421590802108356. [DOI] [PubMed] [Google Scholar]
- 8.Hixon AL, Buenconsejo-Lum LE. Developing the rural primary care workforce in Hawaii--a 10-point plan. Hawaii Med J. 2010;69((6 Suppl 3)):53–55. [PMC free article] [PubMed] [Google Scholar]
- 9.Muneno J, Mead K, Mapelli P, Davis E, Withy K. Medical school hotline: Pipeline to health careers in Hawai‘i. Hawai‘i J Med Public Health. 2017;76((2)):55–58. [PMC free article] [PubMed] [Google Scholar]
- 10.Schiff T, Felsing-Watkins J, Small C, Takayesu A, Withy K. Addressing the physician shortage in Hawai‘i: Recruiting medical students who meet the needs of Hawai‘i’s rural communities. Hawai‘i J Med Public Health. 2012;71((4)):21–25. [PMC free article] [PubMed] [Google Scholar]
- 11.Lee DM, Nichols T. Physician recruitment and retention in rural and underserved areas. Int J Health Care Qual Assur. 2014;27((7)):642–652. doi: 10.1108/ijhcqa-04-2014-0042. [DOI] [PubMed] [Google Scholar]
- 12.John A Burns School of Medicine: Values, Vision, & Mission. Available from: https://jabsom.hawaii.edu/about-us/values-vision-mission. Accessed January 21, 2022.
- 13.Talley BE, Ann Moore S, Camargo CA, Jr, Rogers J, Ginde AA. Availability and potential effect of rural rotations in emergency medicine residency programs. Acad Emerg Med. 2011;18((3)):297–300. doi: 10.1111/j.1553-2712.2010.00987.x. [DOI] [PubMed] [Google Scholar]
- 14.Farmer J, Kenny A, McKinstry C, Huysmans RD. A scoping review of the association between rural medical education and rural practice location. Hum Resour Health. 2015;13((1)):27. doi: 10.1186/s12960-015-0017-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nelson WA, Pomerantz A, Schwartz J. Putting “rural” into psychiatry residency training programs. Acad Psychiatry. 2007;31((6)):423–429. doi: 10.1176/appi.ap.31.6.423. [DOI] [PubMed] [Google Scholar]
- 16.Hustedde C, Paladine H, Wendling A, et al. Women in rural family medicine: A qualitative exploration of practice attributes that promote physician satisfaction. Rural Remote Health. 2018;18((2)):4355. doi: 10.22605/RRH4355. [DOI] [PubMed] [Google Scholar]
- 17.QuickFacts: Hilo CDP, Hawaii United States Census Bureau. Updated July 2021. Acessed May 12, 2022. https:// https://www.census.gov/quickfacts/hilocdphawaii.
- 18.Mission and Vision Hawaii Health Systems Corporation. Acessed May 12, 2022. https://www.hhsc.org/about-us/mission-and-vision/
- 19.Whiteman MK, Hillis SD, Jamieson DJ, et al. Inpatient hysterectomy surveillance in the United States, 2000-2004. Am J Obstet Gynecol. 2008;198((1)):34.e31–34.e37. doi: 10.1016/j.ajog.2007.05.039. [DOI] [PubMed] [Google Scholar]
- 20.Cohen SL, Vitonis AF, Einarsson JI. Updated hysterectomy surveillance and factors associated with minimally invasive hysterectomy. JSLS. 2014;18((3)):e2014.00096. doi: 10.4293/JSLS.2014.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yamasato K, Casey D, Kaneshiro B, Hiraoka M. Effect of Robotic Surgery on Hysterectomy Trends: Implications for Resident Education. J Minim Invasive Gynecol. 2014;21((3)):399–405. doi: 10.1016/j.jmig.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 22.Smith AJB, AlAshqar A, Chaves KF, Borahay MA. Association of demographic, clinical, and hospital-related factors with use of robotic hysterectomy for benign indications: A national database study. Int J Med Robot. 2020;16((4)):e2107. doi: 10.1002/rcs.2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patterson DG, Andrilla CHA, Garberson LA. Preparing physicians for rural practice: Availability of rural training in rural-centric residency programs. J Grad Med Educ. 2019;11((5)):550–7. doi: 10.4300/JGME-D-18-01079.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


