Abstract
Background: Youth with HIV (YWH) aged 18–24 are overburdened by tobacco, with half also using cannabis recreationally. Increasing tobacco cessation necessitates exploring providers’ approaches to cessation. Methods: Grounded in social cognitive theory, we explored cognitive, socioenvironmental, and behavioral factors impacting providers’ approaches to tobacco use among recreational cannabis users. Virtual interviews were conducted among healthcare providers caring for YWH in Washington (legalized cannabis), Massachusetts (legalized cannabis), and Alabama (cannabis not legal). Interviews were transcribed and analyzed via deductive and exploratory, thematic approaches using NVivo 12 Plus. Results: Twelve providers participated; 80% were subspecialist physicians. All providers (N = 12) reported discussing tobacco use; none reported discussing tobacco use in conjunction with cannabis use. Identified themes included competing demands including cannabis co-use, prioritization of social determinants of health, and need for youth-tailored tools. Conclusions: YWH disproportionately use tobacco and recreational cannabis. Optimizing clinical visits to identify opportunities to address tobacco is crucial.
Keywords: Youth with HIV, tobacco, tobacco cessation, cannabis, provider perspectives
Background
Smoking is the leading cause of preventable death in the United States (U.S.). 1 Smoking rates are higher among people with HIV/AIDS (PWH), with rates two to three times higher than the general population. 2 Medical advances in HIV treatment have increased life expectancies. 3 Thus, other chronic medical conditions (eg, sequelae from smoking) are now the main causes of death among PWH who adhere to HIV treatment (12.3 years lost to smoking compared to 5.1 years lost due to HIV), emphasizing the importance of smoking cessation in this population. 4
Youth with HIV (YWH) are a critical focus for smoking cessation interventions. More than half of YWH who smoke cigarettes daily also use some form of cannabis.5–7 Co-use of tobacco and cannabis is associated with higher nicotine-dependence compared to cigarette smoking alone. 8 Recreational cannabis use leads to tobacco initiation and difficulties with tobacco cessation and is associated with poor antiretroviral adherence among those with cannabis use disorder.9–13 However, YWH and providers alike may use and recommend cannabis adjunctively or as natural therapy for many conditions (eg, nausea, anxiety) associated with HIV.11,14 Thus, comprehensive HIV care in YWH should address tobacco cessation, including within the context of recreational cannabis co-use.
Few interventions focus on tobacco cessation among YWH, and none focus on tobacco and recreational cannabis co-users. 15 This study uses qualitative methods to investigate how providers from three U.S. institutions approach tobacco use among YWH. We explored attitudes, barriers, and facilitators of discussing tobacco, tobacco cessation, and tobacco cessation in the context of cannabis co-use. We also explored treatment pitfalls and strategies to improve cessation.
Methods
Setting
Participants were recruited from three clinics that provide services to YWH in Massachusetts, Washington, and Alabama. Massachusetts and Washington have legalized recreational and medicinal marijuana. 16 The Massachusetts clinic is a large urban community health center serving approximately 3,700 individuals, predominately non-Hispanic white men (60%) with 2% of their population identifying as transgender; the Washington clinic is an HIV subspecialty clinic serving 2,600 individuals including men who have sex with men (55%), Latino/a (14%), and individuals who use injection drugs (23%). The Alabama clinic is also an HIV subspecialty clinic serving 3,400 individuals with a larger proportion of African Americans (65%) and African-American cis-women (24%) than the other sites.
Participant Recruitment
Purposive sampling was used to identify eligible participants who were physicians, nurse practitioners, or physician assistants with prescribing privileges at one of the sites. An email was sent to prospective participants caring for YWH. Interested participants contacted study staff to schedule a 1-hour Zoom interview, consented verbally, and completed a brief demographic questionnaire administered by the study team. Staff then conducted a semi-structured qualitative interview using a researcher-developed interview guide (IDI).
In-Depth Interviews
The IDI guide was grounded in social cognitive theory (SCT), exploring factors that motivate or demotivate individuals’ engagement in specific behaviors. The three main constructs are personal cognitive factors, socioenvironmental factors, and behavioral factors. 17 The IDI focused on provider's healthcare setting, approach to tobacco and cannabis use, approach to co-use of tobacco and cannabis, and approach to tobacco cessation with YWH compared to other patients (eg, those not living with HIV; PWH older than 24). Example questions are displayed in Table 1. Interviews were conducted by a qualitatively-trained, non-provider study team member (PP), audio recorded, and transcribed until thematic saturation was achieved. Participants were compensated with a $50 pre-paid incentive card for completing the interview.
Table 1.
Example Interview Questions.
| Provider Healthcare Setting |
|
| Approach to tobacco and cannabis use |
|
| Approach to co-use of tobacco and cannabis |
|
| How the approach to tobacco and cannabis cessation varies by population |
|
Analysis
Transcripts were reviewed by two coders (PP and SVH) using exploratory thematic analysis. First, they coded three interviews each to identify codes inductively and to iteratively develop, refine, and finalize a codebook. Discrepancies in coding were discussed and resolved, and subsequent inter-rater coder agreement was 99%. Then after finalizing the codebook, they analyzed all transcripts and identified themes and subthemes. Thematic saturation was achieved.
Ethical Approval and Informed Consents
The Institutional Review Boards of the University of Alabama at Birmingham (IRB approval 300000632), University of Washington (IRB-00006878), and Fenway Health (IRB approval 1368453) approved all study procedures and informed consent documents. All participants provided informed consent.
Results
Demographic Characteristics
Recruitment occurred March to July, 2021. Recruitment emails were sent monthly to each of the recruitment sites. Twelve providers (eight [67%] from the Alabama clinic) completed the screening, were eligible, enrolled in the study, and completed IDIs (Table 2). Participants were predominately physicians (N = 10; 83%), infectious disease specialists (N = 8, 67%), non-Hispanic (N = 11, 92%), white (N = 8, 67%), and female (N = 7, 58%).
Table 2.
Demographics of Participating Providers Caring for Youth With HIV.
| Demographic | Total Participants N (%) | |
|---|---|---|
| Location | Fenway Health | 1 (8.3) |
| The University of Alabama at Birmingham | 8 (66.7) | |
| The University of Washington | 3 (25.0) | |
| Specialty a | Infectious Disease | 8 (66.7) |
| HIV Specialist, Family Medicine | 1 (8.3) | |
| HIV Specialist, Adolescent Medicine | 1 (8.3) | |
| Primary Care Practitioner | 1 (8.3) | |
| Provider Type | ||
| Physician | 10 (83.3) | |
| Nurse Practitioner | 2 (16.7) | |
| Physician Assistant | 0 (0.0) | |
| Years Caring for PLWH b | ||
| 0-10 | 5 (41.7) | |
| 11-20 | 6 (50.0) | |
| 20 or more | 1 (8.3) | |
| Race c | ||
| White | 8 (66.7) | |
| Black or African American | 3 (25.0) | |
| Asian | 2 (16.7) | |
| Other Race | 1 (8.3) | |
| Ethnicity | ||
| Hispanic or Latinx | 1 (8.3) | |
| Non-Hispanic or Latinx | 11 (91.7) | |
| Gender d | Female | 7 (58.3) |
| Male | 5 (41.7) |
There were no participants who identified as HIV Specialists in Internal Medicine or Pediatrics.
PLWH, People living with HIV.
There were no participants who identified as American Indian/Alaska Native or Native Hawaiian/Other Pacific Islander.
There were no participants who identified as Trans male, Trans female, or Gender nonconforming.
Major Themes
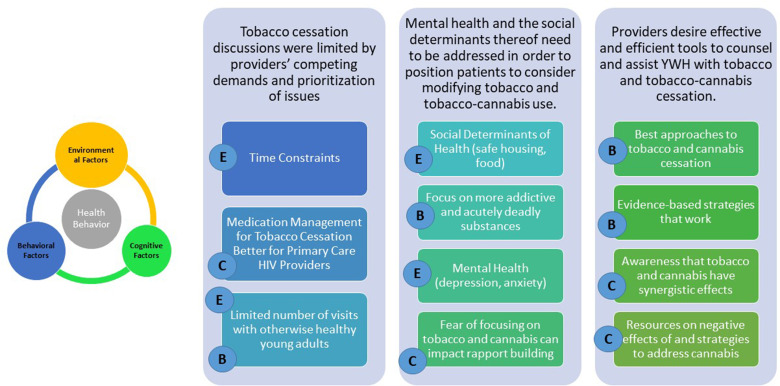
Participating providers expressed confidence with regular inquiry about use of traditional combustible tobacco products; however, provider practice varied in the frequency with which they inquired about recreational cannabis use, making identification and discussion of tobacco and cannabis co-use rare. IDIs revealed the interaction of individual provider and structural factors hindering discussions about use and cessation: (1) tobacco cessation discussions were limited by providers’ competing demands and prioritization of issues; (2) mental health and social determinants thereof need to be addressed in order to position patients to consider modifying tobacco and tobacco-cannabis use; and (3) providers desire effective and efficient tools to assist YWH with tobacco and tobacco-cannabis co-use. Each of these themes and subthemes was mapped back to constructs from the SCT (Figure 1).
Figure 1.
Major themes and subthemes mapped to the social cognitive theory. On the left are the three constructs that affect health behavior-environmental (E), behavioral (B), and cognitive factors (C). Environmental factors include factors such as social norms and structural factors; behavioral factors include adherence skills and self-efficacy; and cognitive factors include knowledge and attitudes about a particular behavior. 17 On the right, each column represents one of the three major themes and its associated subthemes. Each subtheme is mapped back to a construct from Social Cognitive Theory (represented by a circle with a letter).
“It's just not a priority.” Tobacco cessation discussions were limited by providers’ competing demands and prioritization of issues
Providers serve patients who have medical and psychosocial needs in addition to HIV-care needs. However, due to well-established visit time constraints, providers tend to prioritize HIV and mental health over tobacco and cannabis use. One provider explained,
“I’m a firm believer of not biting [off] more than I can chew in a visit, and also not overwhelming patients, so I don’t like to deal with multiple crises at the same time. Usually, I take care of the HIV and other mental health stuff.” (P9: Physician)
“…there are some patients where I can just look at their chart and know that we're not gonna be talking about their smoking for a year.” (P10: Physician)
Additionally, providers noted addressing tobacco and cannabis with YWH specifically, compared to adults with HIV, can be challenging given YWH are overall healthy with fewer chronic medical conditions, and therefore have fewer visits with their HIV providers. Another challenge is the need to address the patients’ desired topics when they come in for an acute-care visit (vs longitudinal well-patient visit), even if patient desires do not align with provider goals.
“… I think in young adults who I find are … usually otherwise healthy … they're just really not coming to the doctor's office that often to talk about sorta healthcare in general. It's usually associated with something urgent, and then oftentimes it's hard to make time and space for [smoking].” (P11: Physician)
-
“How can this person… quit when we’re not providing him any sort of support to quit?” Mental health and the social determinants thereof need to be addressed in order to position patients to consider modifying tobacco and tobacco-cannabis use.
Providers acknowledged that many patients’ substance use is related to mental health and often informed by social determinants of health (SDoH)—the environment where that patient lives, works, and plays. 18 A Nurse Practitioner participant notes,
“…for people who have a lotta chaos and have a lot of anxiety in their life, they prioritize tobacco as a way of dealing with that anxiety, that maladaptive have a cigarette, calm down for a few minutes, as a way to help deal with the anxiety of their life.” (P8)
“…it kinda depends on if their life is otherwise stable too. And during COVID, in this political environment, it has been tough to prioritize these coping mechanisms [tobacco and cannabis use] as things I wanna remove from people. (P9: Physician)
When SDoH are a challenge, cessation of substances like tobacco and cannabis are not patient priorities; thus, providers pivot their focus in response. Providers reported that addressing more addictive and lethal substances such as heroin, crack cocaine, and methamphetamine was a top priority given their ability to negatively impact success in HIV care and greater risk of causing acute damage.
“…if [patients] use marijuana or smoke tobacco along with [heroin], my priority is really to try to keep them from overdosing from heroin… and not necessarily to stop smoking cannabis.” (P4: Physician)
Another provider describes her encounter with a newly diagnosed young person, and how she pivoted her discussion after recognizing his distress.
“He had a lot of social stuff going on as well. So, he was trying to find a safe place to live. And… he was newly diagnosed. Like very, very newly diagnosed with HIV. So, we were also dealing with the pressure, and the stress that comes with that and…Just trying to let him know he was gonna be okay.” (P1: Physician)
Many providers were aware of the cyclical impact poor SDoH have on their ability to address patients’ substance use. Furthermore, poor SDoH can be more challenging to tackle in YWH who have fewer tangible resources and social supports. One provider noted difficulties with managing an individual's cannabis use in light of housing insecurity.
“A lot of these youngsters are smoking cannabis because of the chaotic environment they’re living in. If you’re homeless or living in your car, I can… understand why you would want cannabis. … …how can this person… quit when we’re not providing him any sort of support to quit? … obviously the fundamental aspect of getting him support to quit would be secure housing. But we can’t get housing because he can’t quit.” (P6: Physician)
“’Cause, you almost feel out of touch when your patient is like, ‘I don’t have a safe place to sleep. And I can’t get access to food. And I’m worried that this HIV's gonna kill me. And I have these thoughts of depression. And sometimes I’m thinking about killing myself.’ And you’re like, ‘Oh, by the way, stop smoking.’” (P1: Physician)
Some providers expressed concern that addressing tobacco and/ cannabis among patients could impact rapport or deter a patient from remaining in HIV care.
“…Because I’m trying to establish rapport with these patients—I need them to come back, I need them to stay on their medicine—I personally do not focus on their cannabis use.” (P6: Physician)
“some of it's a matter of addressing what the roadblocks are, or barriers, for them to get care in the first place. And the folks … whose viral loads are elevated, generally, are much more at high risk. Their behaviors are high risk. A lot of times, I’ll see them for substance use and mood disorders that are worsened because of the fact that if I start ‘em on a medicine, then they don’t come back … Their social support systems are non-existent, or their support systems are as chaotic as they are.” (P2: Nurse Practitioner)
“I just wanna … mention it, sorta do some motivational interviewing, leave a teaser and say, like, let's talk about this again because ultimately, I do want people to come back into clinic… ‘Cause I do know that I feel when I go to the dentist, I'm sheepish that I haven't flossed, and I can only imagine how people would feel if they're talking about smoking use.” (P11: Physician)
“Differing strategies based on who the individual is is not something I ever really see training on.” Providers desire effective and efficient tools to assist YWH with tobacco and tobacco-cannabis use.
One common concern was how to approach co-use in this population in general. One provider expressed,
“So if they are serious about quitting, rather than them trying to go cold-turkey, which usually never goes very well, I have suggested nicotine replacements. Marijuana, gosh, I don’t know. I’m not sure what I can offer them to cut off marijuana use. And again, these youngsters, a lot of them could benefit from counselling, but access to counselling services is also somewhat limited…I know that there's lots of printed material that's informational, but I’m not sure how much that resonates with teenagers or young adults. You know? It's more I’m not sure if more information is necessarily what's going to make the difference.” (P6: Physician)
When probed about additional resources they would need, one provider stated, “maybe some more data on what really works.” (P11: Physician)
Most providers stated they had challenges discussing negative effects of cannabis with patients. This challenge was present regardless of the state's legal status of marijuana and was augmented by patients and providers who do not believe marijuana is a harmful substance. A provider noted,
“I will say, ‘Marijuana, poppers, cocaine, crystal meth, GHB, molly, ecstasy, shrooms.’ Like I’ll throw in some of the bar recreational drugs, and I’ll list all of them. They’ll say, ‘Oh, no, I don’t do any of that. I do marijuana.” (P9: Physician)
Most providers reported not being trained to think about combined effects of tobacco and cannabis use.One provider discussed cannabis use explicitly while another discussed a lack of training able to address individual nuances, including co-substance use.
“I generally don’t treat them [tobacco and cannabis co-use compared to singular substance use] differently. And it's partly because I feel like all of my patients use marijuana.” (P6: Physician)
“And the other thing this conversation is bringing to mind is education about the optimal strategies based on the individual, based on their age, based on their HIV status, or co-substance use status, or other conditions, or, differing strategies based on who the individual is, is not something I ever really see training on.” (P12: Physician)
Discussion
YWH disproportionately use tobacco and cannabis recreationally compared to their peers and are at greater risk of experiencing negative consequences from their co-use. This qualitative study is the first to explore providers’ perspectives on tobacco use in the context of recreational cannabis co-use in YWH. While all providers systematically inquired about tobacco use, empathy surrounding disordered patterns of cannabis stifled conversations about recreational cannabis. Thus, identification of patients who may be at risk of compounded negative effects associated with co-use of tobacco and recreational cannabis rarely occurred. Furthermore, all providers emphasized the importance of a holistic patient-centered approach to addressing tobacco use, inclusive of having available and accessible resources for addressing mental health and SDoH. Providers also felt that scientific data about the harms of recreational cannabis and successful approaches to cessation were lacking, and that the absence of this information in conjunction with the unique psychosocial factors affecting YWH made it challenging to focus on addressing this aspect of co-use, often seen as a coping strategy.
Providers’ confidence in managing tobacco use in this study mirrors findings from previous studies among HIV providers.19,20 Furthermore, similar to other studies, providers embraced using a holistic approach to addressing tobacco cessation that factored in mental health and access to resources. 19 However, unlike other studies, these providers did not feel as though addressing smoking was as high priority as mental health, the cessation of other substances, and psychosocial factors affecting medication adherence.19,21 Thus, better and more efficient evidence-based tools that are adaptable to specific patients’ needs are necessary to aid providers in addressing tobacco and cannabis use.
Providers caring for YWH represent both primary care HIV practitioners and HIV or infectious disease subspecialists. Studies show that primary care providers perform better at screening and addressing preventative care and health maintenance topics such as tobacco and cannabis use. 21 One study found HIV providers who self-identified as providing primary HIV care performed better with screening, counseling, and managing their patients’ tobacco use compared to providers self-identifying as HIV or infectious disease specialists. 20 Even though Health and Human Services (HHS) guidelines for adolescents and adults living with HIV strongly recommend that “people with HIV and [substance use disorders] should be offered evidence-based pharmacotherapy (eg, opioid agonist therapy, tobacco cessation treatment, alcohol use disorder treatment) as part of comprehensive HIV care in clinical settings,” there is still a debate about which setting is best suited for managing substance use. 22
The U.S. Preventative Services Task Force has recommended several interventions in addition to pharmacological tobacco cessation tools. 23 While some of these recommendations are brief (eg, referral to a quit line), other interventions are more time-intensive (eg, 5 A's and motivational interviewing). Furthermore, PWH have a higher prevalence of substance use and psychiatric disorders, which is compounded by individuals’ use of substances to cope with psychiatric diagnoses and/or HIV. 24 The addition of cannabis as a coping or symptom-management tool further complicates tobacco cessation, as heavy cannabis use can impede tobacco cessation and result in re-initiation of tobacco use among those who have successfully quit. 24 HIV clinics have interdisciplinary models of care that are uniquely positioned to provide medical, psychological, and social resources capable of addressing tobacco use within this context. However, a large national survey revealed that only 20% of providers had received formal training on tobacco counseling and treatment. 21 While co-location of HIV, mental health, and substance use services has been shown to result in better health outcomes, expertise and specialized training on tobacco still remains limited. 25 One recent practical guideline for providers caring for PWH who smoke tobacco states that there are no explicit recommendations for youth. 26 Indeed there are no studies specifically focused on addressing tobacco use among YWH. Table 3 provides some resources available to providers. Focused studies on YWH are needed because youth are cognitively still immature and have less experience and fewer resources to navigate the structural barriers present in managing tobacco and cannabis co-use, with polysubstance use, mental health comorbidities, and poorer SDoH further complicating care. Furthermore, smoking morbidity is one of the leading causes of death among PWH; focusing on tobacco cessation when PWH are young will have the greatest impact on quality adjusted life years. 27 Thus, it is not surprising that providers are unsure of the best approaches in YWH.
Table 3.
Practical Resources for Approaching Tobacco Use in Youth with HIV.
| National Quitline - For English: 1-800-QUIT NOW (1-800-784-8669) - For Spanish: 1-855-335-3569 - Additional languages available |
| Smoke Free - smokefree.gov - https://teen.smokefree.gov/ |
| BecomeAnEX.com |
| Freedom from Smoking (American Lung Association) - https://www.lung.org/quit-smoking/join-freedom-from-smoking |
This study should be viewed within the context of some limitations. Study sample size was small, with the majority of providers representing one site, and may have been impacted by the COVID-19 pandemic and competing responsibilities among potential participants. Participating providers may have been more interested in this topic, and there may have been social desirability bias to emphasize that screening is occurring at all visits. In spite of these limitations, this study was able to explore the perspectives of providers practicing in three different states within three different regions of the country. The study specifically focused on exploring this topic within YWH in order to understand how their unique needs affect management and distinguish provision of care among this population compared with adults with HIV and the general population. Finally, this study's intentional inclusion of cannabis co-use provides a comprehensive realistic lens of how polysubstance use may complicate tobacco cessation discussions.
Conclusions
This study illustrates the complexity in addressing tobacco cessation among YWH, including those who co-use recreational cannabis. While providers are well-trained in screening for substance use, providers desire additional training in evidence-based tools for both tobacco and cannabis cessation. Research exploring which tools can be adapted to, and developmentally appropriate for YWH is needed to update provider guidelines for youth. Furthermore, providers remain empathetic to holistically caring for YWH and thus will need to leverage interdisciplinary services to address co-morbid psychiatric and socioeconomic challenges.
Nevertheless, there are at least some resources available to these providers (Table 3). While recent practice guidelines do not provide recommendations for smoking cessation in YWH, nor address strategies to reduce cannabis use, providers can incorporate current tobacco cessation clinical recommendations and behavioral interventions. In the future, research on and dissemination of synergistic effects of tobacco and cannabis use, combined with the development of evidence-based guidelines specific to YWH on approaching tobacco and tobacco-cannabis cessation should be developed.
Acknowledgements
The authors would like to acknowledge the UAB Centers for AIDS Research's Developmental Core for their support of this study.
Abbreviations
- U.S.
United States
- PWH
People with HIV/AIDS
- YWH
Youth with HIV
- IDI
In-depth interview
- SCT
Social Cognitive Theory
- SDoH
Social Determinates of Health
Footnotes
Authors’ Contributions: SVH, HMC, OC, LTM, and KC conceptualized this study with LTM and KC providing mentorship during the entirety of this study. SVH, PP, and LTM have conducted the study, interviewed participants, and interpreted the data. SVH, LTC, KC, HMC, and OC all worked on drawing conclusions and crafting the manuscript. LTM and KC are co-senior authors. All have approved of the submitted version of this manuscript and have agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Availability of Data and Materials: The datasets generated and analyzed during the current study are not publicly available due the potential to risk to individual privacy but are available from the corresponding author on reasonable request.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Approval and Consent to Participate: The Institutional Review Boards at the University of Alabama at Birmingham, University of Washington, and Fenway Health all approved this study. Each participant was provided an informed consent document via email and allowed to review the consent form, sign it and send it back to study personnel prior to the study.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: the National Institute on Drug Abuse (grant number 3R01DA044112).
ORCID iDs: Samantha V. Hill https://orcid.org/0000-0002-4103-9329
Lynn T. Matthews https://orcid.org/0000-0001-6167-6328
References
- 1.Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco product use among adults—United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(46):1736–1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mann-Jackson L, Choi D, Sutfin EL. A qualitative systematic review of cigarette smoking cessation interventions for persons living with HIV. J Cancer Educ. 2019;34(6):1045–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samji H, Cescon A, Hogg RS Closing the gap: Increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLOS ONE. 2013;8(12):e81355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cropsey KL, Willig JH, Mugavero MJ. Cigarette smokers are less likely to have undetectable viral loads: Results from four HIV clinics. J Addict Med. 2016;10(1):13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gamarel KE, Westfall AO, Lally MA, Hosek S, Wilson CM, Adolescent Medicine Trials Network for HIVAI. Tobacco use and sustained viral suppression in youth living with HIV. AIDS Behav. 2018;22(6):2018–2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schauer GL, King BA, McAfee TA. Prevalence, correlates, and trends in tobacco use and cessation among current, former, and never adult marijuana users with a history of tobacco use, 2005–2014. Addict Behav. 2017;73:165–171. [DOI] [PubMed] [Google Scholar]
- 7.McKelvey K, Baiocchi M, Halpern-Felsher B. Adolescents’ and young adults’ use and perceptions of pod-based electronic cigarettes. JAMA Netw Open. 2018;1(6):e183535–e183535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang JB, Ramo DE, Lisha NE, Cataldo JK. Medical marijuana legalization and cigarette and marijuana co-use in adolescents and adults. Drug Alcohol Depend. 2016;166:32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gross IM, Hosek S, Richards MH, Fernandez MI Predictors and profiles of antiretroviral therapy adherence among African American adolescents and young adult males living with HIV. AIDS Patient Care STDS. 2016;30(7):324–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Desai N, Burns L, Gong Y. An update on drug-drug interactions between antiretroviral therapies and drugs of abuse in HIV systems. Expert Opin Drug Metab Toxicol. 2020;16(11):1005–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonn-Miller MO, Oser ML, Bucossi MM, Trafton JA. Cannabis use and HIV antiretroviral therapy adherence and HIV-related symptoms. J Behav Med. 2014;37(1):1–10. [DOI] [PubMed] [Google Scholar]
- 12.Weinberger AH, Platt J, Copeland J, Goodwin RD. Is Cannabis use associated with increased risk of cigarette smoking initiation, persistence, and relapse? Longitudinal data from a representative sample of US adults. J Clin Psychiatry. 2018;79(2):17m11522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Voci S, Zawertailo L, Baliunas D, Masood Z, Selby P. Is cannabis use associated with tobacco cessation outcome? An observational cohort study in primary care. Drug Alcohol Depend. 2020;206:107756. [DOI] [PubMed] [Google Scholar]
- 14.Wilson NL, Peterson SN, Ellis RJ. Cannabis and the gut–brain axis communication in HIV infection. Cannabis Cannabinoid Res. 2021;6(2):92–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Escota G, Onen N. HIV-infected adolescent, young adult and pregnant smokers: important targets for effective tobacco control programs. Int J Environ Res Public Health. 2013;10(6):2471–2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hutzler A. Legal weed: where the pro-cannabis movement stands halfway through 2019. Newsweek. 2019. [Google Scholar]
- 17.Glanz KRB, Viswanath K. Health Behavior: Theory, Research, and Practice. Jossey Bass; 2015. [Google Scholar]
- 18.Office of Disease Prevention and Health Promotion. Healthy People 2030: Social Determinants of Health. [cited 2022 February 21]; Available from: https://health.gov/healthypeople/objectives-and-data/social-determinants-health.
- 19.Horvath KJ, Eastman M, Prosser R, Goodroad B, Worthington L. Addressing smoking during medical visits: patients with human immunodeficiency virus. Am J Prev Med. 2012;43(5 Suppl 3):S214–S221. [DOI] [PubMed] [Google Scholar]
- 20.Vijayaraghavan M, Yuan P, Gregorich S. Disparities in receipt of 5As for smoking cessation in diverse primary care and HIV clinics. Prev Med Rep. 2017;6:80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shuter J, Salmo LN, Shuter AD, Nivasch EC, Fazzari M, Moadel AB. Provider beliefs and practices relating to tobacco use in patients living with HIV/AIDS: a national survey. AIDS Behav. 2012;16(2):288–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clinical Info HIV.gov. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents Living with HIV. Guidelines 2021 June 3, 2021 [cited 2022 February 21]; Available from: https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-arv/substance-use-disorders-and-hiv?view=full.
- 23.US Preventive Services Task Force. Tobacco Smoking Cessation in Adults, Including Pregnant Persons: Interventions. 2021 [cited 2022 February 21]; Available from: https://www.uspreventiveservicestaskforce.org/uspstf/document/RecommendationStatementFinal/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions. [DOI] [PubMed]
- 24.Nahvi S, Cooperman NA. Review: the need for smoking cessation among HIV-positive smokers. AIDS Educ Prev. 2009;21(3 Suppl):14–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mizuno Y, Higa DH, Leighton CA, Mullins M, Crepaz N. Is co-location of services with HIV care associated with improved HIV care outcomes? A systematic review. AIDS Care. 2019;31(11):1323–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reddy KP, Kruse GR, Lee S, Shuter J, Rigotti NA. Tobacco use and treatment of tobacco dependence among people with HIV: a practical guide for clinicians. Clin Infect Dis. 2022;15(1):37–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maciosek MV, LaFrance AB, Dehmer SP. Health benefits and cost-effectiveness of brief clinician tobacco counseling for youth and adults. Ann Fam Med. 2017;15(1):37–47. [DOI] [PMC free article] [PubMed] [Google Scholar]