Abstract
Background:
The United States is currently experiencing an unprecedented rise in fatal drug overdoses, which is in part due to the arrival of fentanyl, fentanyl analogs, and other synthetic drugs into the illicit drug supply. Traditional urine drug testing is often unable to detect fentanyl analogs and other novel synthetic drugs, which places physicians and first responders in the difficult position of treating patients who are intoxicated with or overdosing on unknown substances.
Design and methods:
We report, as a feasibility study, the development of a novel program to use a handheld Raman spectrometry device in our hospital’s Emergency Department to surveil our local illicit drug supply in terms of what substances are being sold and used.
Results:
Using our novel program, we were able to detect 27 substances in our illicit drug supply over a 10 month period, including fentanyl analogues. We shared, through our local opioid safety coalition, real-time information to first responders, substance use treatment programs, and physicians about the novel substances we detected using the handheld Raman spectrometer.
Conclusions:
A community partnership of using handheld Raman spectrometry in our hospital’s Emergency Department was successful in providing information to health care providers about novel substances in our illicit drug market. Additionally, the implementation of this program improved collaboration between local health care providers and local law enforcement.
Keywords: Overdose, illicit drug supply, community partnership, Raman spectrometry
Introduction
The United States is currently struggling with substance use and deaths from drug overdoses at extremely high levels not seen previously in history, initially fueled by the overprescribing of opiates by medical providers.1–5 2020, a year turned upside down by the COVID-19 pandemic, proved to be the most lethal of any year in US history from drug overdose deaths, with 92,000 Americans dying from a drug overdose. 6 While total overdose deaths are increasing, deaths from cocaine and prescription opioids remain constant. This points toward illicit opioids being the cause for the increased rate of deaths from drug overdose. 7 Unfortunately, illicit drugs are cut with multiple substances depending on the local illicit drug market and the availability of cutting agents. Known common adulterants of street drugs include acetaminophen, caffeine, diphenhydramine, methorphan, alprazolam, quetiapine, chloroquine, diltiazem, cocaine, procaine, lidocaine, quinine, quinidine, phenacetin, thiamine, and other substances.8–10
Digging further into the overdose deaths, 2018 data noted that 75% of opioid deaths involved a non-methadone synthetic opioid, the most common of which was fentanyl. 7 Fentanyl, due to its high potency, has proven to be easy to produce and smuggle into the United States, saturating the illicit drug supply, and resulting in increased overdose deaths.7,11,12 Beyond fentanyl, other chemical agents are rapidly arriving in the US illicit drug supply, such as etizolam—a benzodiazepine not legal for use in the United States, most of which are not able to be picked up by traditional urine drug screens. 13 In summary, illicit drugs across the planet are constantly changing in terms of what is being used and what is cut or mixed into them, and our usual methods of drug testing are unable to detect them.7,9,10 As medical providers, it is important to know what is in our local illicit drug supply so as to be able to know what might be causing drug dependence or overdoses in our local patient population as well as the appropriate treatment.
Design and methods
Working closely with community organizations and local law enforcement agencies, our hospital identified a community need to be able to rapidly and safely identify which substances are in our local illicit drug supply. Handheld Raman spectrometry has been shown to be an accurate, rapid, and useful tool in the detection of illicit drugs. 14 We identified a handheld Raman spectrometry device that could inform police, first responders, and healthcare providers about the illicit drugs and drug combinations being sold and used in our community and thereby help our medical providers determine what patients have been exposed to so as to provide appropriate treatment and prevent overdose deaths.
We hypothesized that we could develop a program to use a handheld Raman spectrometer based in our hospital’s Emergency Department that would allow a partnership between our hospital, our local opioid safety coalition, and the law enforcement agencies in our County to be able to surveil what substances are in our local illicit drug supply. We then performed a feasibility study of this hypothesis, describing how we designed the program and its efficacy over the first 10 months of the program, and report the results of our feasibility study in this manuscript. To the best of our knowledge, this is the first report of using handheld Raman spectrometry in a community partnership between healthcare providers and law enforcement as a part of an opioid safety coalition to be able to identify new substances and adulterants in our local illicit drug supply.
Our hospital purchased a handheld Raman spectrometer (TruNarc, Thermo Scientific, Waltham, MA, https://www.thermofisher.com/order/catalog/product/TRUNARC) to allow for analysis and surveillance of the illicit street drugs and drug combinations being sold in our community. The device can identify close to 500 chemicals in the illicit drug supply, from opiates (including fentanyl and even more potent fentanyl derivatives), to stimulants (including methamphetamine), to depressants (including the new highly potent illicit benzodiazepines), to hallucinogens, as well as precursors and fillers/cutting agents. These chemicals are all quickly able to be identified without coming into direct contact with the substance, as the user can scan directly through plastic bags or non-opaque glass containers to minimize exposure. The manufacturer maintains a library of substances that can be detected by the device, and this is updated on a regular basis by the manufacturer as new substances are identified as potential chemicals in the illicit drug supply. The device can analyze powders, liquids, pills, and crystals—but not organic material such as plant matter. The manufacturer maintains the database of chemicals that can be detected, and when an analysis is performed, if a drug of abuse is detected, the result is shown on a screen with red background (see Figure 1). If a common filler or cutting agent is detected, the result is shown on a screen with an orange background to suggest that a drug of abuse might be detected and that a repeat scan should be done in a different area of the specimen. If the chemical or substance is not recognized, an “inconclusive” result is given. To ensure the device is functioning correctly and accurately, the device has a quality check function and this quality check is done as a part of our protocol before any substance is analyzed. A photo of the device showing the result of an analysis is shown in Figure 1. In one preliminary study, this device was able to detect the target drug in nearly 80% of samples with reproducible results in approximately 85% of cases, outperforming another similar type of device. 15 If more than one substance is in a specimen, the device can detect multiple substances at the same time and will display all substances detected on the screen. However, with some specimens, such as counterfeit pills, substances are not evenly distributed through the specimen, so performing multiple scans on a specimen in different areas ensures that all substances in the specimen are detected.
Figure 1.
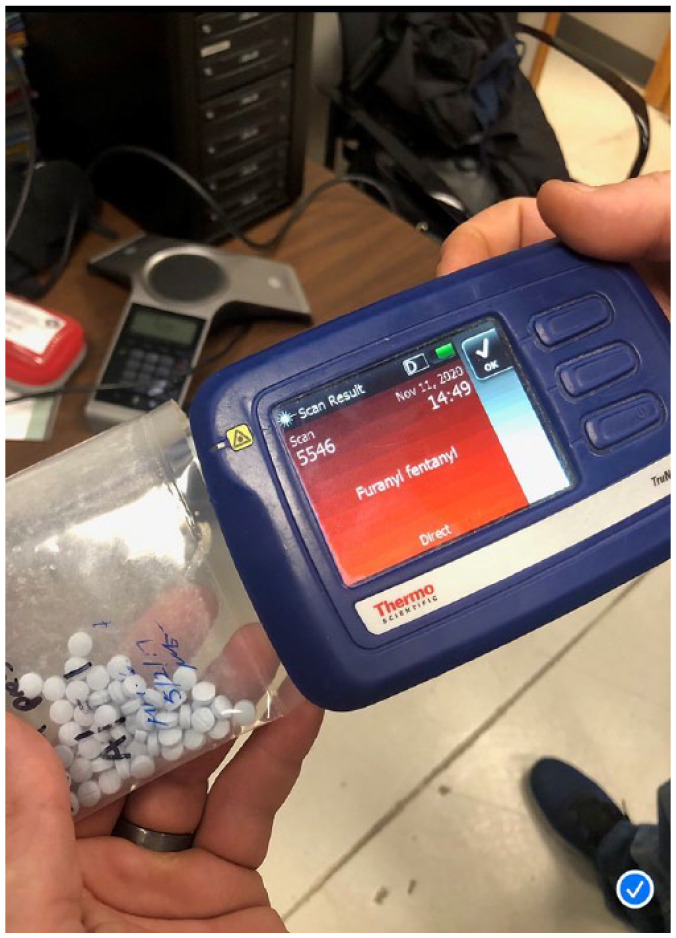
Handheld mass spectrometer showing the result of an analysis.
The effort to design, develop, and implement this initiative was led by a local Emergency Physician who is the lead clinical physician in our local opioid safety coalition. Our county has had a local opioid safety coalition since 2014 involving local hospitals, law enforcement, substance use treatment programs, first responders, and other community organizations. Once the device was purchased by the hospital, multiple stakeholder meetings were held to determine how the device would be used, monitored, and safely secured on our hospital campus. The coalition lead physician is on the medical staff of our hospital and conducted educational trainings on how to use the device. This physician was also responsible for reviewing all analyses done by the device on a scheduled basis to collect and review all available information about illicit drugs detected in our community.
We identified that there would be two ways for us to use the device to be able to identify the substances in our local illicit drug market. First, we developed a protocol for local law enforcement to come to the hospital campus and analyze any drug product they had seized, with hospital security assisting officers to and from the device. Hospital security did not use the device; they were only responsible for supervising who used the device and had access to the device. Furthermore, the hospital did not participate in any investigations or prosecutions. Officers simply brought any product that they wanted to analyze to the hospital and performed an analysis using the device. The device records information from all scans performed in a de-identified fashion, which allowed the physician supervising the program to review the scans on the device on a scheduled basis to review what substances had been detected. Second, we developed a hospital protocol for how to analyze any illicit substances (or substances suspected to be illicit) that were found to be in a patient’s possession. The hospital, prior to this initiative, had a policy in place that when an illicit substance (or substance suspected to be illicit) was found on a patient’s person, the substance was confiscated and sent to the pharmacy for destruction. Consistent with privacy laws, information that an illicit (or suspected illicit) substance was found to be in a patient’s possession was not shared with law enforcement or any disciplinary body. We modified this protocol so that any illicit substance (or substance suspected to be illicit) detected on a patient was analyzed using the handheld Raman spectrometer before being sent to the hospital pharmacy for destruction. As with the scans performed by law enforcement, the physician supervising the program reviewed the scans on the device on a scheduled basis to review what substances had been detected. Clinicians taking care of the patient could document in the medical record that the patient had a substance found on their person, as well as a physical description of the substance and what the patient reported that the substance contained. Clinicians could document that the substance was to be destroyed per hospital protocol, and that a handheld Raman spectrometry analysis was done or was to be done on the substance. The device is designed for forensic analysis only and was not used to replace any laboratory drug testing.
As both trained law enforcement and trained hospital clinicians and pharmacists used the same device, this broadened our surveillance of the illicit drug supply in our community as we were able to get information from both the law enforcement and healthcare settings in our community. Working with our existing opioid safety coalition, we developed plans to share information on what substances were detected in our street drug supply on a scheduled basis with local hospitals, law enforcement, substance use treatment programs, and other community organizations. Information could also be shared through the opioid safety coalition on an urgent basis if a new substance was detected that was particularly concerning or novel to the community. We ultimately chose to house the device in our Emergency Department as it is open 24 hours per day, the Emergency Department is a common site at which patients with substance use seek care, and we have security in our hospital’s Emergency Department to supervise use of the device and interact with law enforcement.
Results
As a part of our preparation of this program, we identified that there were 17 different law enforcement agencies in our County. We were able to train 14 of those agencies on how to use the device, the farthest of which was 65 miles away from our hospital.
During the 10-month period after implementation from December 2021 to September 2022, the device was used 236 times to scan substances that were thought to be illicit drugs. We were not able to determine which scans were done by healthcare providers and which scans were done by law enforcement. We identified 27 different substances in our local illicit drug supply, including etizolam, fentanyl, acetyl fentanyl, and acrylfentanyl. Table 1 provides a complete list of all substances that were identified in our local illicit drug supply, as well as how many times each substance was detected. More than one substance was detected in nine scans: Mannitol + Inositol (four scans), Mannitol + Lactose (two scans), Epsom Salt + Cellulose (two scans), and Lactose + Cellulose (one scan). Of the 236 scans that were performed, 77 (27%) had results that were inconclusive. Two cases involving use of the device stood out as particularly useful that we felt were worth discussing individually.
Table 1.
Complete list of all substances identified in our local illicit drug supply during the 10 month period after implementation of the program (with the number of times each substance was detected).
| Drugs of abuse |
| Methamphetamine (21) |
| Cocaine (6) |
| Fentanyl (5) |
| Acryl fentanyl (3) |
| Heroin (3) |
| Ethanol (3) |
| Amphetamine (1) |
| Diazepam (1) |
| Etizolam (1) |
| Acetyl fentanyl (1) |
| Other substances |
| Acetaminophen (43) |
| Mannitol (34) |
| Polystyrene (8) |
| Aspirin (7) |
| Lactose (6) |
| Caffeine (5) |
| Inositol (4) |
| Polypropylene (3) |
| Cellulose (3) |
| Low density polyethylene (2) |
| Ibuprofen (2) |
| Epsom salt (2) |
| Diphenhydramine (1) |
| Sorbitol (1) |
| Naproxen (1) |
| Barium sulfate (1) |
| Baking soda (1) |
Case 1. After confiscation from a justice-involved person, a local law enforcement officer brought a small bag of pills to our hospital to be tested using our handheld Raman spectrometer. The pills were blue in color, with the marking “M 30” on them. These pills have been known in our community to be sold on the street and to contain fentanyl based on our previous experience treating patients using them. For this particular set of pills, the officer used the device to analyze them and surprisingly did not find fentanyl in the pills. The officer scanned multiple different pills from the set and scanned pills in different locations on their surfaces. The only substance detected was etizolam, a benzodiazepine that is not legal in the US, as discussed above. This was novel information for our community that blue M 30 pills contained etizolam, and we shared this information on an urgent basis with physicians and first responders through our local opioid safety coalition to warn of this finding in order to guide care of patients using these pills.
Case 2. A 25-year-old female was referred to our Emergency Department by a local drug treatment program as she appeared to be in severe withdrawal from opiates when she arrived to enter the program. While sitting in the waiting room, the triage nurse noted that the patient’s appearance changed, so she went to assess the patient. The patient was found to have clinical signs of an opiate overdose. Naloxone was immediately administered and the patient was brought back to a resuscitation room for immediate attention. During her resuscitation, a white powder was found in a container on the patient’s person. This powder was confiscated as a suspected illicit substance, and our Emergency Department pharmacist shortly after analyzed the powder with the handheld Raman spectrometer which identified the substance as fentanyl. We shared this information, namely that we had detected fentanyl as a white powder, with physicians and first responders through our local opioid safety coalition to warn of this finding, as most of the fentanyl in the community to date had been in the form of counterfeit pills.
Discussion
Since implementation of this novel program, we have been able to identify multiple substances in our street drug supply, some not previously known to have been in our community. Our hospital’s urine drug screen does not test for many of these substances, which has made understanding what substances are causing intoxication and overdose extremely challenging. By using this handheld Raman spectrometer, we have been able to inform our first responders, law enforcement, and health care providers with more information about our community’s illicit drug supply than we could have ever done just using our hospital’s routine urine drug screens. While we ultimately cannot definitively identify every substance in our community using this device, we are able to detect the substances that our patients are using more comprehensively and more rapidly than before implementation. Information about substances detected using the device—including substance form, color, street name, and what the substance is sold as—is shared monthly with our physicians, first responders, and local police departments. This information is also shared at all scheduled meetings of our local substance use safety coalition. Additionally, while fillers or cutting agents may be perceived as innocuous compared to the drugs of abuse, several of the substances we detected are pharmaceutically active and could affect a patient who took multiple doses of the illicit product, such as acetaminophen and aspirin. As an example of how information detected by the device is used by healthcare providers, we have discussed as a coalition that if we see an increasing percentage of specimens that test positive for aspirin and acetaminophen in the future, we could change our practice at the hospital to routinely obtaining serum levels of these medications after an overdose out of concern for unexpected toxicity due to the filler or cutting agent.
One finding that stands out in Table 1 is the high frequency with which acetaminophen and mannitol were detected. We suspect that this is due to the need to scan specimens multiple times to detect all substances in the specimen, as substances may not be evenly distributed through the specimen (such as with counterfeit pills). If a specimen was scanned, and an illicit substance was suspected but only a common cutting agent was detected, the specimen was re-scanned again multiple times on other areas so as to detect any illicit substances in the specimen.
From a law enforcement, healthcare provider, and first responder standpoint, access to this device is extremely useful as it allows safe and rapid testing. Currently, when law enforcement agencies find illicit drugs in our community, they send them to the Department of Justice (DOJ) for testing so as to determine what chemical or chemicals were in the illicit drug product. Due to a high volume of specimens being sent for analysis, testing by the DOJ can take up to several months to result, and not all specimens end up getting tested. While awaiting test results, we as a community of healthcare providers and first responders have no information about what chemical or chemicals were in that illicit drug product sent for analysis. In comparison, use of the handheld Raman spectrometer allows for the detection of substances in the drug supply in real time. Additionally, by being able to scan through plastic bags and non-opaque containers, this device allows healthcare providers and law enforcement officers to safely test products quickly and easily without being exposed to the substance being tested.
Another benefit of this program has been to strengthen the relationship between law enforcement, first responders, and health care providers. Law enforcement is frequently on our campus to use the device, which has involved collegial discussions about our illicit drug supply and how to protect our community. From discussions during the planning and implementation of this program, we have developed an overdose response team to serve the surrounding area of the hospital that will consist of hospital staff, law enforcement, and substance use providers. Our program using the handheld Raman spectrometer has been viewed as so beneficial to the community that another hospital in the county will be purchasing the device for use on their own campus in a similar fashion to the program at our hospital. Currently, all law enforcement agencies in our county can use the device in our hospital, and the addition of a second device at another hospital in the county will reduce travel time for officers and increase the surveillance of street drugs in our county. Both hospitals are in our local opioid safety coalition and will work to share data about what substances are detected to keep our community informed.
This program can be easily implemented at any hospital in the country in the opinion of the authors. The device may be purchased from the manufacturer (Thermo Scientific). From a law enforcement perspective, it is helpful for the officers to have access to the device as it provides rapid and safe drug analysis. Given the benefit to law enforcement and as law enforcement inherently works closely with Emergency Departments (assault, violence, behavioral health holds, etc.), there is minimal effort required to make contact with and get engagement from local law enforcement agencies to build a program.
While overall, the implementation of this program has been highly successful in our community, there are some limitations that must be considered. First, using the handheld Raman spectrometer takes training, and an inexperienced user may not know how to adequately test a specimen, resulting in a false negative for one or more substances when the specimen is tested. To combat this, our users of the device were trained to scan each specimen multiple times in multiple locations to maximize our ability to detect each substance in a given specimen. A second limitation of our program is that we were only able to review the scan data from the TruNarc device and were not able to record how many times a single specimen was scanned. As such, we do not precisely know how frequently various cutting agents are used, as many specimens, once a cutting agent such as acetaminophen was detected, were scanned multiple times. Third, the handheld Raman spectrometer only has a finite number of chemicals that can be detected, so there could have been other chemicals that were present but not detected. While the manufacturer regularly updates the database of chemicals detected, “street” chemists are constantly detecting new substances that can be used as recreational drugs. Fourth, as noted previously, even when used correctly in one study, the TruNarc device may not detect all specimens in the library (such as when a substance is present in a very small amount), so this may have resulted in us not detecting some substances in the products we tested. Finally, our surveillance of the illicit substances in our community is limited to substances obtained by local law enforcement and substances found on the person of patients seeking medical attention in our hospital and Emergency Department.
Conclusion
A novel hospital-based program of using a handheld Raman spectrometer in partnership with law enforcement to detect substances in the local illicit drug supply in real time has been feasible and effective in our community, and likely could be beneficial in other communities if replicated. Benefits in our community included improving collaboration between health care providers and law enforcement, increasing local efforts to prevent overdoses, and providing real-time information to the community on what substances are in our illicit drug supply and causing overdoses.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Significance for public health: The United States is currently experiencing an unprecedented rise in fatal drug overdoses as the US drug supply is increasingly contaminated with novel substances, including fentanyl analogues. Our community opioid safety coalition, which includes law enforcement, identified the need to be able to rapidly detect novel substance in our illicit drug supply so as to be able to inform front line medical providers as to what substances might be causing overdoses. We found the use of a shared Raman spectrometry device available to health care providers and law enforcement to be an effective way to identify novel substances in our drug supply in our community. The information about what substances we have detected has helped us to educate our front-line medical providers on how to respond to overdoses in real time and helped us improve our substance use and overdose prevention efforts.
ORCID iD: Casey Grover  https://orcid.org/0000-0002-2930-9867
https://orcid.org/0000-0002-2930-9867
References
- 1.Vivolo-Kantor AM, Seth P, Gladden M, et al. Vital signs: trends in emergency department visits for suspected opioid overdoses – United States, July 2016 – September 2017. MMWR Morb Mortal Wkly Rep 2018; 67(9): 279–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones CM, McAnich JK. Emergency department visits and overdose deaths from combined use of opioids and benzodiazepines. Am J Prev Med 2015; 49(4): 493–501. [DOI] [PubMed] [Google Scholar]
- 3.Gwira Baumblatt JA, Wiedman C, Dunn JR, et al. High-risk use by patients prescribed opioids for pain and its role in overdose deaths. JAMA Intern Med. 2014; 174(5): 796–801. [DOI] [PubMed] [Google Scholar]
- 4.Paulozzi LJ, Strickler GK, Kreiner PW, et al. Controlled substance prescribing patterns – prescription behavior surveillance system, eight states, 2013. MMWR Surveill Summ 2015; 64(9): 1–14. [DOI] [PubMed] [Google Scholar]
- 5.Guy GP, Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep 2017; 66(26): 697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. Hyattsville, MD: National Center for Health Statistics, 2021. [Google Scholar]
- 7.Singh VM, Browne T, Montgomery J. The emerging role of toxic adulterants in street drugs in the US illicit opioid crisis. Public Health Rep 2020; 135(1): 6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fiorentin TR, Fogarty M, Limberger RP, et al. Determination of cutting agents in seized cocaine samples using GC-MS, GC-TMS, and LC-MS/MS. Forensic Sci Int 2019; 295: 199–206. [DOI] [PubMed] [Google Scholar]
- 9.Phillips KA, Hirsch GA, Epstein DH, et al. Cardiac complications of unwitting co-injection of quinine/quinidine with heroin in an intravenous drug user. J Gen Intern Med 2012; 27(12): 1722–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fiorentin TR, Logan BK. Analytical findings in used syringes from a syringe exchange program. Int J Drug Policy 2020; 81: 102770. [DOI] [PubMed] [Google Scholar]
- 11.Pergolizzi J, Magnusson P, LeQuang JA, et al. Illicitly manufactured fentanyl entering the United States. Cureus 2021; 13(8): e17496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dai Z, Abate MA, Smith GS, et al. Fentanyl and fentanyl-analog involvement in drug related deaths. Drug Alcohol Depend 2019; 196: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nielsen S, McAuley A. Etizolam: a rapid review on pharmacology, non-medical use and harms. Drug Alcohol Rev 2020; 39(4): 330–336. [DOI] [PubMed] [Google Scholar]
- 14.Kranenburg RF, Verduin J, de Ridder R, et al. Performance evaluation of handheld Raman spectroscopy for cocaine detection on forensic case samples. Drug Test Anal 2021; 13(5): 1054–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spicher C, Yeatman T, Alford I, et al. The evaluation of portable handheld Raman systems for the presumptive identification of narcotics: thermo scientific TruNarc and Chemring detection systems PGR-1064. Marshall University. https://www.marshall.edu/forensics/files/SpicherCristina_FINAL-Research-Paper_8_3_-2016.pdf (accessed 10 April 2022). [Google Scholar]


