Abstract
Behavioural non-pharmaceutical interventions (NPIs) (e.g., mask wearing, quarantine, restriction on gatherings, physical distancing) have been used to interrupt transmission of COVID-19 and to reduce the impacts of the pandemic. The aim of this scoping review was to document the efficacy of behavioural NPIs to positively influence COVID-19 outcomes. Following PRISMA guidelines, a systematic search was conducted of PubMed, ScienceDirect, Psych INFO, Medline, CINAHL and Scopus for studies published between January 2020 and February 2023. Seventy -seven studies were eligible to be included in the review. Majority of the studies were conducted in high-income countries, with fewer studies in low- or middle-income countries. School closure, mask wearing, and non-essential business closure and shelter-in-place orders were the most prevalent NPIs investigated. School closure and mask wearing reported high effectiveness while shelter-in-place orders reported less effectiveness. Shelter-in-place orders when used in conjunction with other measures, did not enhance effectiveness. Public event bans, physical distancing, handwashing, and travel restrictions were largely effective, while the effectiveness of gathering restrictions depended on the limitation on numbers. Early implementation was associated with a higher effectiveness in reducing COVID-19 cases and deaths, the use of behavioural NPIs in combinations was reported to yield more effective results. Moreover, behavioural NPIs were reported to be dependent on their consistent use and were difficult behaviours to maintain, highlighting the need for behavioural change. This review highlighted the effectiveness of behavioural NPIs to positively influence COVID-19 reduction outcomes. Further research to promote country- and context-specific documents that will enhance the effectiveness of behavioural NPIs.
Keywords: COVID-19, Behavioural change, Non-pharmaceutical interventions, Effectiveness, Policy documents
1. Introduction
Since its identification in early 2020, COVID-19 has spread globally and has currently infected >526.55 million individuals worldwide and has resulted in approximately 6.28 million deaths (World Health Organisation, 2022). At the onset of the pandemic, and in the absence of an effective vaccine against the disease, governments and the World Health Organization promoted the use of nonpharmaceutical interventions (NPIs) that required behaviour change, such as social distancing measures and mask wearing to prevent the spread of COVID-19 (World Health Organization, 2020a; World Health Organization, 2020b). The effectiveness of these behavioural NPIs has been largely dependent on the willingness of individuals to change behaviours (Coroiu et al., 2020). Fortunately, several vaccines have since been developed and approved for use for clinical and commercial use (World Health Organisation, 2020). Vaccines have proven to be efficacious in reducing the spread and severity of disease (Yan et al., 2021). However, vaccination rates against COVID-19 remain lower low and middle-income regions. This is, in part can be attributed to vaccine hesitancy and challenges in the equity of the distribution of the vaccines (Asundi et al., 2021; Loembé and Nkengasong, 2021; Kabakama et al., 2022). Confirming this, as of 14 February 2023 only 26.4% of people living in low and middle income countries (LMICs) had received one dose of a COVID-19 vaccine (Mathieu et al., 2021; Mathieu et al., n.d.). As such, the use of NPIs in LMICs remains essential to curb the spread of the virus.
Research on the effective implementation of NPIs anchored in behavioural change principles, is integral not only for application in forecasted future pandemics, but also for use in addressing other global challenges such as climate change (Webster, 1997). However, behaviour change approaches and principles have not been systematically applied in the implementation of NPIs for COVID-19 prevention. Additionally, at a national policy level there exists limited guidance on behaviour change. A search for publicly available country level policy documents was conducted, and the findings are summarised in Table 1 . Specifically, this search was aimed at identifying documents that provide a structured approach to achieving behaviour change in support of policy objectives. The United Kingdom is the only country with such a comprehensive document. We did not find any other government specific documents for other countries. However, we did find behavioural change documents for countries by non-governmental organisations such as USAID, United Nations, and European Union. Additionally, the Australian government has commissioned the development of a behaviour change document.
Table 1.
Country level behaviour change documents for health promotion.
| Country | Title | Year | Website and purpose |
|---|---|---|---|
| United Kingdom | Achieving behaviour change: a guide for national government. | 2020 |
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/933328/UFG_National_Guide_v04.00__1___1_.pdf This document aims to provide a structured approach to achieving behaviour change in support of policy objectives. It is based on an interdisciplinary approach known as the Behaviour Change Wheel (BCW) that was developed by integrating 19 behavioural science frameworks from many disciplines and sectors. |
| United Nations | Behaviour changes strategies and health: the role of health systems | 2017 |
https://sustainabledevelopment.un.org/content/documents/2404Behavioral%20Insights.pdf Through the development of country specific and disease specific guidelines, the United Nations aims to develop people centred policies to achieve effective program out puts. |
| India | COVID-19 Communication Handbook | 2020 |
https://csbc.org.in/wp-content/uploads/2020/07/FINAL_CSBC-COVID-19-Communication-Handbook-09072020.pdf This non- governmental organization handbook aims to provide practical guidance on how to use behaviourally informed insights to design effective communication to address the rapid behaviour change needed during this pandemic. |
| Australia | Changing behaviour: a public policy perspective | 2018 |
https://legacy.apsc.gov.au/changing-behaviour-public-policy-perspective Australia has commissioned a behaviour change document but does not have one currently. This document aims to provide evidence that behavioural theory and empirical research can add to the fundamental building block of behavioural change for policy makers. |
| Pan American Health rganisation | Building better health: a handbook of behavioural change | 2003 |
https://iris.paho.org/bitstream/handle/10665.2/706/9275115907.pdf?sequence=2&isAllowed=y This book was written independently for Pan American countries. It promotes the use of behavioural sciences in conjunction with disease prevention practices to improve health. |
| New Zealand - | New Zealand Guideline Group | 1998 |
https://www.health.govt.nz/system/files/documents/publications/effective-health-behaviour-change-long-term-conditions.pdf The document aims to provide guidelines for effective health behaviour change interventions for people with long-term conditions. |
| European Union | Behavioural Insights Applied to Policy | 2016 |
https://ec.europa.eu/jrc/sites/jrcsh/files/jrc-biap2016-italy_en.pdf The document was compiled by the European Union for Italy. It aims to highlight the importance of the use of behavioural insights to policy making. It showcases examples of behavioural interventions in a range of policy areas, such as employment, consumer policy, health, taxation, environment, or transport, pointing to their respective outcome whenever this was available. |
| USAID | Tools for behaviour change communication | 2021 |
https://www.usaid.gov/what-we-do/global-health/cross-cutting-areas/social-and-behavior-change This handbook highlights the importance of the use of behaviour change techniques in improving health. |
It is hence important to document the effectiveness of behavioural NPIs intended to positively influence COVID-19 outcomes to support their future implementation. The primary aim of this review was therefore to document the evidence of effectiveness of behavioural NPIs to positively influence COVID-19 outcomes. The secondary aim was to make recommendations on these interventions for research, policy, and practice. For the purposes of this review, behavioural NPIs included face masks, handwashing, and social distancing. Social distancing measures included physical distancing, school closures, border closures, public event bans, gathering bans, non-essential business closure, restricted movement, quarantine and stay-at-home orders. COVID-19 outcomes included the spread of infections, hospitalisation, and death (Hale et al., 2020).
2. Methods
In this review, we followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA). Databases searched included PubMed, ScienceDirect, PsychINFO, Medline, CINAHL and Scopus; the search was restricted to articles available in English from 1 January 2020 and 31 October 2021. All searches were done using different combinations of the following keywords COVID-19, corona virus, SARS CoV2, impact, effect*, evaluation, quarantine, isolation, masks, handwashing, hand sanitising, social distancing, physical distancing, and lockdown. Studies were included in the review if they:
-
•
Assessed or compared behavioural NPIs effectiveness only in the context of COVID-19.
-
•
Included at least one of the following NPIs, as described and categorised in the Oxford COVID-19 Government Response Tracker (OxCGRT) (Hale et al., 2020): Social distancing measures namely physical distancing, school closures, border closures, public event bans, gathering bans, non-essential business closure, restricted movement, quarantine and stay-at-home orders, and mask wearing policies.
-
•
Were either observational or interventional (i.e., quasi-experimental or experimental) studies of empirical data.
-
•
Analysed NPI behavioural effectiveness in the general population of any geographical area.
-
•
Directly measured the effect of the application of behavioural NPIs on any COVID-19 outcome (infection, hospitalisation, and death).
Studies were excluded from the review if they:
-
•
Were based on forecasts.
-
•
Did not assess the direct link between NPIs and the COVID-19 outcomes stipulated (for example, no direct link between COVID-19 outcome and NPI).
-
•
Analysed the impact of adherence or compliance to NPIs.
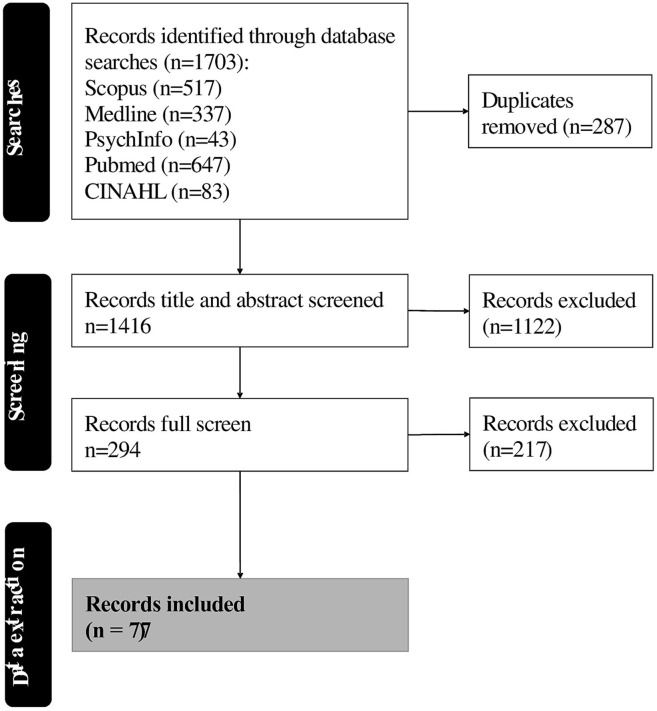
Fig. 1 outlines the search, screening, and data extraction phases. One reviewer (TMS) screened all titles and abstracts, and second reviewer (CED) screened 10% of titles and abstracts, and discrepancies in decisions were discussed to reach consensus. One consensus was reach, TS conducted full text screening and data extraction.
Fig. 1.
Search strategy for studies on the effectiveness of behaviour change interventions influence on COVID-19 outcomes.
Ethical approval for the study was obtained from the Human Research Ethics Committee (Non-Medical) at the University of the Witwatersrand (Ref: H21/10/06).
3. Results
The details of the studies included are presented in Table 2 . A significant proportion of the studies were conducted in high-income countries (HICs, 58%), with only 15% of studies in low-income countries. The methodologies used in the articles were observational and quasi experimental studies (63%), modeling studies (33%), case control studies (3%), and randomized controlled trial (1%). The number of participants in the studies varied substantially, from hundreds to millions of participants. Observation time varied among the studies, even among studies done in the same country. Most of the studies were on the effectiveness of social distancing measures (n = 71), followed by the effectiveness of mask wearing (n = 26); very few were on hand sanitising (n = 5). Some studies evaluated the effect of both social distancing measures and mask wearing concurrently. Only one study made use of behavioural principles in the application of behavioural NPIs (Abaluck et al., 2021).
Table 2.
NPI study details (Alfano, 2022; Andrejko et al., 2022; Dave et al., 2021; Dzator et al., 2022; Figueiredo et al., 2020; García-García et al., 2022; Ghosal et al., 2020; Guzzetta et al., 2020; Hendrix, 2020; Herstein et al., 2021; Hyafil and Moriña, 2020; Islam et al., 2020; Karaivanov et al., 2020; Kwon et al., 2021; Lyu and Wehby, 2020; Mitze et al., 2020; Olney et al., 2021; Pozo-Martin et al., 2021; Rader et al., 2021; Saez et al., 2020; Saki et al., 2021; Scott et al., 2021; Sharif et al., 2021; Silva et al., 2020; Singh et al., 2021; Sypsa et al., 2021; Tran et al., 2021; Triukose et al., 2021; Van Dyke et al., 2020; Wagner et al., 2020; Wang et al., 2020; Woskie et al., 2021; Yang et al., 2021; Zhang and Warner, 2020; Zhou, 2021).
*behavioural principles applied
1. Abaluck J, Kwong L, Styczynski A. The Impact of Community Masking on COVID-19: A Cluster-Randomized Trial in Bangladesh. The Innovations for Poverty Action (IPA) Working Paper. 2021.
2. Alfano V. The Effects of School Closures on COVID-19: A Cross-Country Panel Analysis. Applied health economics and health policy. 2022;20(2):223-33.
3. Alfano V, Ercolano S. The Efficacy of Lockdown Against COVID-19: A Cross-Country Panel Analysis. Applied health economics and health policy. 2020;18(4):509-17.
4. Alimohamadi Y, Holakouie-Naieni K, Sepandi M, Taghdir M. Effect of social distancing on COVID-19 incidence and mortality in Iran since February 20 to May 13, 2020: an interrupted time series analysis. Risk management and healthcare policy. 2020;13:1695.
5. Andrejko KL, Pry JM, Myers JF, Fukui N, DeGuzman JL, Openshaw J, et al. Effectiveness of Face Mask or Respirator Use in Indoor Public Settings for Prevention of SARS-CoV-2 Infection — California, February–December 2021. MMWR Recommendations and Reports. 2022;71(6):212-6.
6. Banholzer N, van Weenen E, Lison A, Cenedese A, Seeliger A, Kratzwald B, et al. Estimating the effects of non-pharmaceutical interventions on the number of new infections with COVID-19 during the first epidemic wave. PLoS One. 2021;16(6):e0252827.
7. Bo Y, Guo C, Lin C, Zeng Y, Li HB, Zhang Y, et al. Effectiveness of non-pharmaceutical interventions on COVID-19 transmission in 190 countries from 23 January to 13 April 2020. International Journal of Infectious Diseases. 2021;102:247-53.
8. Brauner JM, Mindermann S, Sharma M, Johnston D, Salvatier J, Gavenčiak T, et al. Inferring the effectiveness of government interventions against COVID-19. Science (New York, NY). 2021;371(6531).
9. Bundgaard H, Bundgaard JS, Raaschou-Pedersen DET, von Buchwald C, Todsen T, Norsk JB, et al. Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers: A Randomized Controlled Trial. Annals of internal medicine. 2021;174(3):335-43.
10. Castaneda MA, Saygili M. The Effect of Shelter-in-Place Orders on Social Distancing and the Spread of the COVID-19 Pandemic: A Study of Texas. Front Public Health. 2020;8:596607.
11. Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Chance elections, social distancing restrictions, and Kentucky's early COVID-19 experience. PLoS ONE. 2021;16(7 July).
12. Cowling BJ, Ali ST, Ng TWY, Tsang TK, Li JCM, Fong MW, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. The Lancet Public health. 2020;5(5):e279-e88.
13. Cruz CHB. Social distancing in São Paulo State: demonstrating the reduction in cases using time series analysis of deaths due to COVID-19. Rev Bras Epidemiol. 2020;23:e200056.
14. Dave D, Friedson AI, Matsuzawa K, Sabia JJ. WHEN DO SHELTER‐IN‐PLACE ORDERS FIGHT COVID‐19 BEST? POLICY HETEROGENEITY ACROSS STATES AND ADOPTION TIME. Economic inquiry. 2021;59(1):29-52.
15. De Brouwer E, Raimondi D, Moreau Y. Modeling the COVID-19 outbreaks and the effectiveness of the containment measures adopted across countries. MedRxiv. 2020.
16. Deb P, Furceri D, Ostry JD, Tawk N. The effect of containment measures on the COVID-19 pandemic. 2020.
17. Delen D, Eryarsoy E, Davazdahemami B. No place like home: Cross-national data analysis of the efficacy of social distancing during the COVID-19 pandemic. JMIR Public Health and Surveillance. 2020;6(2).
18. DePhillipo NN, Chahla J, Busler M, LaPrade RF. Mobile phone GPS data and prevalence of COVID-19 infections: Quantifying parameters of social distancing in the U.S. Archives of Bone and Joint Surgery. 2021;9(2):217-23.
19. Doung-ngern P, Suphanchaimat R, Panjangampatthana A, Janekrongtham C, Ruampoom D, Daochaeng N, et al. Associations between wearing masks, washing hands, and social distancing practices, and risk of COVID-19 infection in public: a cohort-based case-control study in Thailand. 2020.
20. Dreher N, Spiera Z, McAuley FM, Kuohn L, Durbin JR, Marayati NF, et al. Policy Interventions, Social Distancing, and SARS-CoV-2 Transmission in the United States: A Retrospective State-level Analysis. The American journal of the medical sciences. 2021;361(5):575-84.
21. Durmuş H, Gökler ME, Metintaş S. The Effectiveness of Community-based Social Distancing for Mitigating the Spread of the COVID-19 Pandemic in Turkey. Journal of preventive medicine and public health = Yebang Uihakhoe chi. 2020;53(6):397-404.
22. Dzator J, Acheampong AO, Dzator M, Paolucci F, Yawe BL, Asmah EE, et al. Policy Stringency, Handwashing and COVID-19 cases: Evidence from Global dataset. Health Policy and Technology. 2022;11(2).
23. Ebrahim S, Ashworth H, Noah C, Kadambi A, Toumi A, Chhatwal J. Reduction of COVID-19 Incidence and Nonpharmacologic Interventions: Analysis Using a US County-Level Policy Data Set. Journal of medical Internet research. 2020;22(12):e24614.
24. Esra RT, Jamesion L, Fox MP, Letswalo D, Ngcobo N, Mngadi S, et al. Evaluating the impact of non-pharmaceutical interventions for SARS-CoV-2 on a global scale. MedRxiv. 2020.
25. Fazio RH, Ruisch BC, Moore CA, Granados Samayoa JA, Boggs ST, Ladanyi JT. Social distancing decreases an individual’s likelihood of contracting COVID-19. Proceedings of the National Academy of Sciences of the United States of America. 2021;118(8).
26. Flaxman S, Mishra S, Gandy A, Unwin HJT, Mellan TA, Coupland H, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257-61.
27. Gallaway MS, Rigler J, Robinson S, Herrick K, Livar E, Komatsu KK, et al. Trends in COVID-19 Incidence After Implementation of Mitigation Measures - Arizona, January 22-August 7, 2020. MMWR Morbidity and mortality weekly report. 2020;69(40):1460-3.
28. García-García D, Herranz-Hernández R, Rojas-Benedicto A, León-Gómez I, Larrauri A, Peñuelas M, et al. Assessing the effect of non-pharmaceutical interventions on COVID-19 transmission in Spain, 30 August 2020 to 31 January 2021. Eurosurveillance. 2022;27(19).
29. Saki M, Ghanbari MK, Behzadifar M, Imani-Nasab MH, Behzadifar M, Azari S, et al. The Impact of the Social Distancing Policy on COVID-19 Incidence Cases and Deaths in Iran from February 2020 to January 2021: Insights from an Interrupted Time Series Analysis. Yale J Biol Med. 2021;94(1):13-21.
30. Ghosal S, Bhattacharyya R, Majumder M. Impact of complete lockdown on total infection and death rates: A hierarchical cluster analysis. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;14(4):707-11.
31. Guzzetta G, Riccardo F, Marziano V, Poletti P, Trentini F, Bella A, et al. The impact of a nation-wide lockdown on COVID-19 transmissibility in Italy. arXiv preprint arXiv:200412338. 2020.
32. Hendrix MJ. Absence of apparent transmission of SARS-CoV-2 from two stylists after exposure at a hair salon with a universal face covering policy—Springfield, Missouri, May 2020. MMWR Morbidity and mortality weekly report. 2020;69.
33. Herstein JJ, Degarege A, Stover D, Austin C, Schwedhelm MM, Lawler JV, et al. Characteristics of SARS-CoV-2 transmission among meat processing workers in Nebraska, USA, and effectiveness of risk mitigation measures. Emerging Infectious Diseases. 2021;27(4):1032-9.
34. Hunter PR, Colon-Gonzalez F, Brainard JS, Rushton S. Impact of non-pharmaceutical interventions against COVID-19 in Europe: A quasi-experimental study. MedRxiv. 2020.
35. Hyafil A, Moriña D. Analysis of the impact of lockdown on the evolution Covid-19 epidemics in Spain. medRxiv. 2020.
36. Islam N, Sharp SJ, Chowell G, Shabnam S, Kawachi I, Lacey B, et al. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. Bmj. 2020;370:m2743.
37. Karaivanov A, Lu S, Shigeoka H. Face mask mandates slowed the spread of COVID-19 in Canada. VoxEU org. 2020;5.
38. Kaufman BG, Whitaker R, Mahendraratnam N, Hurewitz S, Yi J, Smith VA, et al. State variation in effects of state social distancing policies on COVID-19 cases. BMC public health. 2021;21(1):1239.
39. Koh WC, Naing L, Wong J. Estimating the impact of physical distancing measures in containing COVID-19: an empirical analysis. International journal of infectious diseases: IJID: official publication of the International Society for Infectious Diseases. 2020;100:42-9.
40. Kwon S, Joshi AD, Lo C-H, Drew DA, Nguyen LH, Guo C-G, et al. Association of social distancing and face mask use with risk of COVID-19. Nature Communications. 2021;12(1):3737.
41. Lemaitre JC, Perez-Saez J, Azman AS, Rinaldo A, Fellay J. Assessing the impact of non-pharmaceutical interventions on SARS-CoV-2 transmission in Switzerland. Swiss Medical Weekly. 2020;150(21-22).
42. Liu Y, Morgenstern C, Kelly J, Lowe R, Jit M. The impact of non-pharmaceutical interventions on SARS-CoV-2 transmission across 130 countries and territories. BMC medicine. 2021;19(1):40.
43. Lio CF, Cheong HH, Lei CI, Lo IL, Yao L, Lam C, et al. Effectiveness of personal protective health behaviour against COVID-19. BMC public health. 2021;21(1):1-10.
44. Loewenthal G, Abadi S, Avram O, Halabi K, Ecker N, Nagar N, et al. COVID‐19 pandemic‐related lockdown: response time is more important than its strictness. EMBO molecular medicine. 2020;12(11):e13171-n/a.
45. Lyu W, Wehby GL. Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US: Study examines impact on COVID-19 growth rates associated with state government mandates requiring face mask use in public. Health affairs. 2020;39(8):1419-25.
46. Figueiredo AM, Codina AD, Figueiredo D, Saez M, León AC. Impact of lockdown on COVID-19 incidence and mortality in China: an interrupted time series study. Bull World Health Organ. 2020;6.
47. Mégarbane B, Bourasset F, Scherrmann JM. Is Lockdown Effective in Limiting SARS-CoV-2 Epidemic Progression?—a Cross-Country Comparative Evaluation Using Epidemiokinetic Tools. Journal of General Internal Medicine. 2021;36(3):746-52.
48. Milazzo A, Giles L, Parent N, McCarthy S, Laurence C. The impact of non-pharmaceutical interventions on COVID-19 cases in South Australia and Victoria. Australian and New Zealand Journal of Public Health. 2022;46(4):482-7.
49. Mitze T, Kosfeld R, Rode J, Wälde K. Face masks considerably reduce COVID-19 cases in Germany. Proc Natl Acad Sci U S A. 2020;117(51):32293-301.
50. Nader IW, Zeilinger EL, Jomar D, Zauchner C. Onset of effects of non-pharmaceutical interventions on COVID-19 infection rates in 176 countries. BMC public health. 2021;21(1):1472.
51. Olney AM, Smith J, Sen S, Thomas F, Unwin HJT. Estimating the Effect of Social Distancing Interventions on COVID-19 in the United States. American Journal of Epidemiology. 2021;190(8):1504-9.
52. Piovani D, Christodoulou MN, Hadjidemetriou A, Pantavou K, Zaza P, Bagos PG, et al. Effect of early application of social distancing interventions on COVID-19 mortality over the first pandemic wave: An analysis of longitudinal data from 37 countries. Journal of Infection. 2021;82(1):133-42.
53. Pozo-Martin F, Weishaar H, Cristea F, Hanefeld J, Bahr T, Schaade L, et al. The impact of non-pharmaceutical interventions on COVID-19 epidemic growth in the 37 OECD member states. European journal of epidemiology. 2021:1-12.
54. Qureshi AI, Suri MFK, Chu H, Suri HK, Suri AK. Early mandated social distancing is a strong predictor of reduction in peak daily new COVID-19 cases. Public Health. 2021;190:160-7.
55. Rader B, White LF, Burns MR, Chen J, Brilliant J, Cohen J, et al. Mask-wearing and control of SARS-CoV-2 transmission in the USA: a cross-sectional study. Lancet Digit Health. 2021;3(3):e148-e57.
56. Reis RF, de Melo Quintela B, de Oliveira Campos J, Gomes JM, Rocha BM, Lobosco M, et al. Characterization of the COVID-19 pandemic and the impact of uncertainties, mitigation strategies, and underreporting of cases in South Korea, Italy, and Brazil. Chaos, Solitons & Fractals. 2020;136:109888.
57. Ryu S, Ali ST, Noh E, Kim D, Lau EHY, Cowling BJ. Transmission dynamics and control of two epidemic waves of SARS-CoV-2 in South Korea. BMC Infectious Diseases. 2021;21(1).
58. Saez M, Tobias A, Varga D, Barceló MA. Effectiveness of the measures to flatten the epidemic curve of COVID-19. The case of Spain. Science of the Total Environment. 2020;727:138761.
59. Sanchez JN, Reyes GA, Martínez‐López B, Johnson Christine K. Impact of social distancing on early SARS‐CoV‐2 transmission in the United States. Zoonoses and public health. 2022;69(6):746-56.
60. Scott N, Saul A, Spelman T, Stoove M, Pedrana A, Saeri A, et al. The introduction of a mandatory mask policy was associated with significantly reduced COVID-19 cases in a major metropolitan city. PLoS One. 2021;16(7):e0253510.
61. Sharif N, Alzahrani KJ, Ahmed SN, Opu RR, Ahmed N, Talukder A, et al. Protective measures are associated with the reduction of transmission of COVID-19 in Bangladesh: A nationwide cross-sectional study. PLoS ONE. 2021;16(11 November).
62. Siedner MJ, Harling G, Reynolds Z, Gilbert RF, Haneuse S, Venkataramani AS, et al. Social distancing to slow the US COVID-19 epidemic: Longitudinal pretest-posttest comparison group study. PLoS Med. 2020;17(8):e1003244.
63. Silva L, Figueiredo Filho D, Fernandes A. The effect of lockdown on the COVID-19 epidemic in Brazil: evidence from an interrupted time series design. Cad Saude Publica. 2020;36(10):e00213920.
64. Singh S, Shaikh M, Hauck K, Miraldo M. Impacts of introducing and lifting nonpharmaceutical interventions on COVID-19 daily growth rate and compliance in the United States. Proc Natl Acad Sci U S A. 2021;118(12).
65. Stokes J, Turner AJ, Anselmi L, Morciano M, Hone T. The relative effects of non-pharmaceutical interventions on wave one Covid-19 mortality: natural experiment in 130 countries. BMC Public Health. 2022;22(1):1113.
66. Sypsa V, Roussos S, Paraskevis D, Lytras T, Tsiodras S, Hatzakis A. Effects of Social Distancing Measures during the First Epidemic Wave of Severe Acute Respiratory Syndrome Infection, Greece. Emerging infectious diseases. 2021;27(2):452-62.
67. Tran P, Tran L, Tran L. The influence of social distancing on COVID-19 mortality in US counties: Cross-sectional study. JMIR Public Health and Surveillance. 2021;7(3).
68. Triukose S, Nitinawarat S, Satian P, Somboonsavatdee A, Chotikarn P, Thammasanya T, et al. Effects of public health interventions on the epidemiological spread during the first wave of the COVID-19 outbreak in Thailand. PLoS ONE. 2021;16(2 February 2021).
69. Van Dyke ME, Rogers TM, Pevzner E, Satterwhite CL, Shah HB, Beckman WJ, et al. Trends in County-Level COVID-19 Incidence in Counties With and Without a Mask Mandate - Kansas, June 1-August 23, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(47):1777-81.
70. Verma BK, Verma M, Verma VK, Abdullah RB, Nath DC, Khan HTA, et al. Global lockdown: An effective safeguard in responding to the threat of COVID‐19. Journal of evaluation in clinical practice. 2020;26(6):1592-8.
71. Wagner AB, Hill EL, Ryan SE, Sun Z, Deng G, Bhadane S, et al. Social distancing merely stabilized COVID‐19 in the United States. Stat (International Statistical Institute). 2020;9(1):e302-n/a.
72. Wang Y, Tian H, Zhang L, Zhang M, Guo D, Wu W, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob Health. 2020;5(5).
73. Woskie LR, Hennessy J, Espinosa V, Tsai TC, Vispute S, Jacobson BH, et al. Early social distancing policies in Europe, changes in mobility & COVID-19 case trajectories: Insights from Spring 2020. PLoS One. 2021;16(6):e0253071.
74. Yang W, Shaff J, Shaman J. Effectiveness of non-pharmaceutical interventions to contain COVID-19: a case study of the 2020 spring pandemic wave in New York City. J R Soc Interface. 2021;18(175):20200822.
75. Zhang X, Warner ME. COVID-19 Policy Differences across US States: Shutdowns, Reopening, and Mask Mandates. Int J Environ Res Public Health. 2020;17(24).
76. Zhang R, Li Y, Zhang AL, Wang Y, Molina MJ. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proceedings of the National Academy of Sciences. 2020;117(26):14857-63.
77. Zhou C, editor Evaluating System for Effectiveness of Mask Mandates and the Most Influential Factor in Each State in the USA. Journal of Physics: Conference Series; 2021: IOP Publishing.
In relation to the measures used to evaluate the effect of social distancing measures on COVID-19 outcomes, most studies used regression models and estimated compartmental models to estimate infection, death, or hospitalisation rates, while others evaluated changes in the reproduction number (Rt). The studies on hand sanitising and mask wearing mainly evaluated infection rates, or the assessment of relative risk. Some studies used more than one of the evaluation measures (Rt, infection, or death rates). The definition of social distancing varied; some studies considered social distancing as a combination of certain restrictions (Lemaitre et al., 2020; Kaufman et al., 2021; Alimohamadi et al., 2020; Cruz, 2020; Delen et al., 2020; DePhillipo et al., 2021; Durmuş et al., 2020; Fazio et al., 2021; Qureshi et al., 2021; Reis et al., 2020; Ryu et al., 2021; Zhang et al., 2020; Siedner et al., 2020; Bo et al., 2021; Ghanbari et al., 2020), while some studies considered social distancing as the encouragement given by governments to keep a prescribed physical distance between individuals. Doung-Ngern et al. (2020) reported that keeping a physical distance was effective in reducing COVID-19 impacts. Similarly, all studies that assessed the effectiveness as a social distancing as a mix of measures reported effectiveness. Supporting this, Gallaway et al. (2020) highlighted that the implementation of behavioural NPIs in combinations yielded greater effectiveness. In a study done in Europe by Flaxman and his colleagues a combination of interventions reduced Rt below 1 (probability Rt < 1.0 is >99%) (Flaxman et al., 2020).
The most prevalent behavioural NPI to be assessed were lockdowns (n = 18), non-essential business closures (n = 26) and school closure (n = 21). Twenty out of the twenty-one studies on school closure reported significant effectiveness with Li et al. (2021), Liu et al. (2021), Brauner et al. (2021), Esra et al. (2020), Courtemanche et al. (2021), Hunter et al. (2020), Nader et al. (2021) reporting that this behavioural NPI was highly effective in reducing COVID-19 negative outcomes. Non-essential business closure was largely effective, with seventeen of the twenty-one studies reporting effectiveness. Brauner et al. (2021) and Banholzer et al. (2021) in their studies reported that it was the most effective behavioural NPI in reducing the impact of COVID-19. In contrast, lockdowns or stay at home measures reported mixed effectiveness. Koh et al. (2020) reported that strict lockdowns were not as effective as non-essential business closures in curbing the spread of COVID-19. While Brauner et al. (2021) highlighted that in their study the effect of lockdowns was not seen when other behavioural NPIs were in place. However, other studies (Esra et al., 2020; Ebrahim et al., 2020; Courtemanche et al., 2021; Dreher et al., 2021) reported that lockdowns were highly effective, with Flaxman et al. reporting that lockdowns were the only behavioural NPI to reduce the reproduction number below one (Flaxman et al., 2020). Ebrahim et al. (2020) also reported that partial lockdowns, were as effective as complete lockdowns in reducing the impact of COVID-19. Furthermore, though lockdowns were effective in reducing mobility to grocery stores, schools, business, workplaces etc., Delen et al. (2020) reported that during lockdowns there was increased residential mobility.
Public event bans were found to be effective in 66% of the studies. Li et al found in their study that this behavioural NPI was the most effective, reducing the reproduction number by 25%, 28 days after its implementation (Li et al., 2021). Most studies reported that gathering restrictions were largely effective in reducing the impacts of COVID-19. Nonetheless, Brauner et al highlighted that the effect of gathering restrictions was dependent on the numbers limited. Their study reported a large effect size for limiting gatherings to 10 people or less, a moderate-to-large effect for 100 people or less, and a small-to-moderate effect for 1000 people or less (Brauner et al., 2021). Moreover, both internal and international travel restrictions were associated with a reduction in the reproduction number, growth rate or incidence-related outcomes in 73% of the studies.
Some studies (Koh et al., 2020; Loewenthal et al., 2020; Deb et al., 2020; Mégarbane et al., 2021; Piovani et al., 2021; Stokes et al., 2022; Sanchez et al., 2022; Verma et al., 2020) highlighted that the effectiveness of the behavioural NPIs was dependent on the timing of their implementation, emphasising the need for early implementation. Loewenthal et al. (2020) highlighted in their study that a 7.49 day delay in lockdown implementation resulted in doubled deaths. Other studies (Nader et al., 2021; De Brouwer et al., 2020; Milazzo et al., 2022) reported that the effect of behavioural NPIs was not immediate and had a more gradual effect on COVID-19 health outcomes, with Alfano and Ercolano (2020) reporting efficacy detectable 100 days after implementation. Few studies assessed the effectiveness of hand sanitising; Lio et al. (2021) reported that hand sanitising reduced the odds of infection after an outdoor activity (adjusted odds ratio (OR), 0.021 [95% confidence interval (CI), 0.003–0.134], P < 0.005).. In the same study handwashing before touching the mouth and nose area also reduced the odds of infection (OR, 0.303 [95% CI, 0.114–0.808], P < 0.05) (Lio et al., 2021). Moreover, the effectiveness of handwashing was directly linked to the duration of handwashing (Lio et al., 2021).
Twenty-six studies analysed the effect of wearing masks on the variation of infection rates and transmission rates (Table 2 and supplementary tables). Most studies reported that wearing masks was effective in reducing the transmission rates of COVID-19. In Thailand, mask wearing was associated with a 77% reduced infection risk (adjusted odds ratio, 0.23 [95% CI, 0.09–0.60]) (Doung-ngern et al., 2020). However, a study in Denmark reported that the mask wearing while other measures were in place, did not further reduce the COVID-19 infection rate among wearers by >50% (Bundgaard et al., 2021). Though overall, mask wearing and other behavioural NPIs were found to be largely effective against COVID-19, mask effectiveness is reported to be affected by how individuals use them. Cowling et al. in their study reported that at the onset of the pandemic only half of the respondents in their study indicated that they could confidently implement the government mandated measures (Cowling et al., 2020). Furthermore, Doung-ngern et al. (2020) highlighted that wearing a mask all the time when in contact with others was effective, but not wearing a mask all the time did not lower risk of infection (Doung-ngern et al., 2020). Additionally, Gallaway et al. (2020) in their study noted that both physical distancing and mask wearing were behaviours that were difficult to maintain.
4. Discussion
The findings of this scoping review contribute to the literature highlighting the effectiveness of behavioural NPIs as effective interventions to reduce transmission and mitigating the impact of the COVID-19 pandemic. It is likely that COVID-19 will become endemic (Torjesen, 2021) but because of vaccine inequality and low vaccine coverage and acceptance rates in low-or middle-income countries especially, the use of behavioural NPIs may remain integral to prevention. Consequently, long-term behavioural adjustments will need to be made by the public. It has been argued that for effective application of behavioural NPIs in the public, there needs to be a complete change in the way the economy, business, and life (including home life) is organised, to protect vulnerable groups, such as the elderly, pregnant women and immune-compromised individuals (Regmi and Lwin, 2021).
Our findings highlight that behavioural NPIs are effective and furthermore, the use of a combination of multiple measures, e.g., school closure, business closure, gathering restrictions and travel restrictions appeared to be more effective in reducing the transmission, hospitalisation, and mortality due to COVID-19. Similar mitigation measures which aimed not to interrupt transmission completely, but to reduce the health impact of an epidemic were adopted by the United States in 1918, and by the world more generally in the 1957, 1968 and 2009 influenza pandemics, and were found to be effective (Ferguson et al., 2020; World Health Organization, 2006; Vukotich et al., 2010; Mitchell et al., 2011). However, of concern are the limited number of studies in LMICs on the effectiveness of behavioural NPIs. As behavioural NPIs remain vital in these low resource settings, more research needs to be done to understand the effectiveness of behavioural NPIs in these settings.
Some studies included in this review highlighted that strict stay-at-home orders or complete lockdown may not be necessary to mitigate COVID-19 spread. Complete lockdowns may have detrimental economic effects to those living in LMICs and hence employing other social distancing measures rather than strict lockdowns maybe of more benefit in low resource settings. For example, a study done in India on the impact of COVID-19 lockdowns on livelihoods of families found that during a hard lockdown, weekly household income dropped by 88% which resulted in significantly reduced meal portions and fewer food items consumed (Gupta et al., 2021).
The effectiveness of behavioural NPIs in both HICs and LMICs is made challenging by the fact that social distancing measures and mask wearing are not typically part of culture (Miguel and Mobarak, 2021). In addition, it is well documented that purposeful health behaviour change is both difficult to achieve and even more difficult to maintain (Bundy, 2004). Confirming this, Yeung et al. (2020) reported that though mask wearing was effective, only 13% of participants wore the masks as recommended, exposing individuals to possible infections. Moreover, Delen et al. (2020) showed that though lockdowns were effective in reducing mobility to business, recreation centres and other communal places, they also resulted in increased residential mobility.
While we have provided evidence of the effectiveness of behavioural NPIs to curb the spread of COVID-19, the public must be willing and able to use these behavioural NPIs. During the 1918 influenza pandemic Whitelaw (1919) made the following statement: “To sum up, it is evident, that no public health law, which has not the endorsation and support of the public generally, can ever be reasonably well enforced.” Hence, the use of a behavioural framework to plan interventions based on key country specific barriers, will ensure countries implement appropriate and targeted responses. As mentioned, the United Kingdom has a national health behaviour change document that makes use of the Behaviour Change Wheel (Michie et al., 2011). The guide supports policy makers in times of crisis (such as with the current pandemic), to develop or adapt interventions to suit the context. By using the acronym APEASE, the United Kingdom document ensures that the behavioural changes needed to be employed by the citizens are acceptable, practical, effective, affordable, considers possible side effects of the behaviour change, as well as promotes equity. Furthermore, this document considers factors such as capability, opportunity, and motivation of the adopters, when planning interventions. Considering the aforementioned acronym and factors when drafting policy allows for behavioural NPIs to be well thought through and may prevent the mandating of behavioural NPIs that cannot easily be applied in a specific setting. For instance, in African countries because of socioeconomic issues, the proposed behavioural NPIs measures are challenging to comply with and hence, this has led to some ignoring lockdown and quarantine policies and engaging in communal activities to earn incomes for their families (Bundgaard et al., 2021; Castaneda and Saygili, 2020). Additionally, compared to higher income countries, most African countries have little governmental financial support being provided for local businesses (Mehtar et al., 2020; Musa et al., 2020; Abdool Karim, 2020). It is therefore evident that a one size fits all approach to pandemics may not be effective (Salihu Sabiu Musa et al., 2022). A country specific behaviour change document will also allow governments to construct precise messaging, which in turn will also promote social trust among their citizens which is needed to address any unprecedented challenge to the healthcare systems of nations. Lastly, as the effectiveness of behavioural NPIs is affected by their timing of implementation, having the government policies in place will facilitate the swift and effective implementation of behavioural NPIs.
To our knowledge, this is the first scoping review to examine the effectiveness of the implementation of behavioural NPIs to reduce transmission of COVID-19 in conjunction with a search of government behavioural change policy documents for pandemics. Several factors limited the present study. Our search strategy was limited to the adult population (>18 years), and we were unable to review grey literature. Secondly, identified studies are variable in sample size, quality, and study population. Most of them had some methodological weaknesses and were open to bias, and the heterogeneity of data precludes a meaningful meta-analysis to measure the impact of specific enablers or barriers. However, given the nature of the pandemic, and that many of these studies would have been in rapid response to the research need, we believe these findings can still provide insights into the effectiveness of behavioural NPIs to reduce transmission of COVID-19.
5. Conclusions
Our review has highlighted the importance of behavioural NPIs for reducing COVID-19 infection in the context of global uncertainty. Behavioural NPIs are a complex form of intervention, that require the participation and behaviour change of the public. This review has identified that implementing behavioural NPIs, e.g., social distancing and mask wearing, are generally effective and one of the best ways for preventing or reducing transmission. This study, however, suggests that the effectiveness of any behavioural NPIs in isolation is likely to be limited, therefore, a combination of multiple measures appeared to be more effective in reducing COVID-19. In addition to this the study highlights the importance of the application of behaviour change principles when implementing NPIs.
Funding
The study was funded by the DSI-NRF Centre of Excellence in Human Development at the University of the Witwatersrand, Johannesburg, South Africa.
Contributions: All authors:
1. Conceived and/or designed the work that led to the submission, acquired data, and/or.
played an important role in interpreting the results.
2. Drafted or revised the manuscript.
3. Approved the final version.
4. Agreed to be accountable for all aspects of the work in ensuring that questions related to.
the accuracy or integrity of any part of the work are appropriately investigated and.
resolved.
Declaration of Competing Interest
The authors declare no conflict of interest.
Data availability
Data will be made available on request.
References
- Abaluck J., Kwong L., Styczynski A. The Innovations for Poverty Action (IPA) Working Paper. 2021. The impact of community masking on COVID-19: a cluster-randomized trial in Bangladesh. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdool Karim S. The South African response to the pandemic. New Engl. J. Med. 2020;382(24) doi: 10.1056/NEJMc2014960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfano V. The effects of school closures on COVID-19: a cross-country panel analysis. Appl. Health Econ. Health Policy. 2022;20(2):223–233. doi: 10.1007/s40258-021-00702-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfano V., Ercolano S. The efficacy of lockdown against COVID-19: a cross-country panel analysis. Appl. Health Econ. Health Policy. 2020;18(4):509–517. doi: 10.1007/s40258-020-00596-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alimohamadi Y., Holakouie-Naieni K., Sepandi M., Taghdir M. Effect of social distancing on COVID-19 incidence and mortality in Iran since February 20 to May 13, 2020: an interrupted time series analysis. Risk Manage. Healthcare Policy. 2020;13:1695. doi: 10.2147/RMHP.S265079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrejko K.L., Pry J.M., Myers J.F., Fukui N., DeGuzman J.L., Openshaw J., et al. Effectiveness of face mask or respirator use in indoor public settings for prevention of SARS-CoV-2 infection — California, February–December 2021. MMWR Recommend. Rep. 2022;71(6):212–216. doi: 10.15585/mmwr.mm7106e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asundi A., O’Leary C., Bhadelia N. Global COVID-19 vaccine inequity: the scope, the impact, and the challenges. Cell Host Microbe. 2021;29(7):1036–1039. doi: 10.1016/j.chom.2021.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banholzer N., Van Weenen E., Lison A., Cenedese A., Seeliger A., Kratzwald B., et al. Estimating the effects of non-pharmaceutical interventions on the number of new infections with COVID-19 during the first epidemic wave. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0252827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bo Y., Guo C., Lin C., Zeng Y., Li H.B., Zhang Y., et al. Effectiveness of non-pharmaceutical interventions on COVID-19 transmission in 190 countries from 23 January to 13 April 2020. Int. J. Infect. Dis. 2021;102:247–253. doi: 10.1016/j.ijid.2020.10.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brauner J.M., Mindermann S., Sharma M., Johnston D., Salvatier J., Gavenčiak T., et al. Inferring the effectiveness of government interventions against COVID-19. Science (New York, NY). 2021;371(6531) doi: 10.1126/science.abd9338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundgaard H., Bundgaard J.S., Raaschou-Pedersen D.E.T., von Buchwald C., Todsen T., Norsk J.B., et al. Effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection in Danish mask wearers: a randomized controlled trial. Ann. Intern. Med. 2021;174(3):335–343. doi: 10.7326/M20-6817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundy C. Changing behaviour: using motivational interviewing techniques. J. R. Soc. Med. 2004;97(Suppl. 44):43. [PMC free article] [PubMed] [Google Scholar]
- Castaneda M.A., Saygili M. The effect of shelter-in-place orders on social distancing and the spread of the COVID-19 pandemic: a study of Texas. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.596607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coroiu A., Moran C., Campbell T., Geller A.C. Barriers and facilitators of adherence to social distancing recommendations during COVID-19 among a large international sample of adults. PLoS One. 2020;15(10) doi: 10.1371/journal.pone.0239795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtemanche C., Garuccio J., Le A., Pinkston J., Yelowitz A. Chance elections, social distancing restrictions, and KENTUCKY’s early COVID-19 experience. PLoS One. 2021;16(7) doi: 10.1371/journal.pone.0250152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling B.J., Ali S.T., Ng T.W.Y., Tsang T.K., Li J.C.M., Fong M.W., et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5(5):e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz CHdB. Social distancing in São Paulo State: demonstrating the reduction in cases using time series analysis of deaths due to COVID-19. Rev. Brasil. Epidemiol. 2020;23 doi: 10.1590/1980-549720200056. [DOI] [PubMed] [Google Scholar]
- Dave D., Friedson A.I., Matsuzawa K., Sabia J.J. When do shelter‐in‐place orders fight Covid‐19 best? Policy heterogeneity across states and adoption time. Econ. Inquiry. 2021;59(1):29–52. doi: 10.1111/ecin.12944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Brouwer E., Raimondi D., Moreau Y. Modeling the COVID-19 outbreaks and the effectiveness of the containment measures adopted across countries. MedRxiv. 2020:2020–2024. [Google Scholar]
- Deb P., Furceri D., Ostry J.D., Tawk N. 2020. The effect of containment measures on the COVID-19 pandemic. [Google Scholar]
- Delen D., Eryarsoy E., Davazdahemami B. No place like home: cross-national data analysis of the efficacy of social distancing during the COVID-19 pandemic. JMIR Public Health Surveil. 2020;6(2) doi: 10.2196/19862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePhillipo N.N., Chahla J., Busler M., LaPrade R.F. Mobile phone GPS data and prevalence of COVID-19 infections: quantifying parameters of social distancing in the U.S. Arch. Bone Joint Surg. 2021;9(2):217–223. doi: 10.22038/abjs.2020.48515.2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doung-ngern P., Suphanchaimat R., Panjangampatthana A., Janekrongtham C., Ruampoom D., Daochaeng N., et al. Associations between wearing masks, washing hands, and social distancing practices, and risk of COVID-19 infection in public: a cohort-based case-control study in Thailand. The Lancet. 2020:2020–2026. [Google Scholar]
- Dreher N., Spiera Z., McAuley F.M., Kuohn L., Durbin J.R., Marayati N.F., et al. Policy interventions, social distancing, and SARS-CoV-2 transmission in the United States: a retrospective state-level analysis. Am. J. Med. Sci. 2021;361(5):575–584. doi: 10.1016/j.amjms.2021.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durmuş H., Gökler M.E., Metintaş S. The effectiveness of community-based social distancing for mitigating the spread of the COVID-19 pandemic in Turkey. J. Prev. Med. Public Health = Yebang Uihakhoe chi. 2020;53(6):397–404. doi: 10.3961/jpmph.20.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzator J., Acheampong A.O., Dzator M., Paolucci F., Yawe B.L., Asmah E.E., et al. Policy Stringency, handwashing and COVID-19 cases: evidence from global dataset. Health Policy Technol. 2022;11(2) doi: 10.1016/j.hlpt.2021.100574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahim S., Ashworth H., Noah C., Kadambi A., Toumi A., Chhatwal J. Reduction of COVID-19 incidence and nonpharmacologic interventions: analysis using a US county-level policy data set. J. Med. Internet Res. 2020;22(12) doi: 10.2196/24614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esra R., Jamieson L., Fox M.P., Letswalo D., Ngcobo N., Mngadi S., et al. Evaluating the impact of non-pharmaceutical interventions for SARS-CoV-2 on a global scale. MedRxiv. 2020:2020–2027. [Google Scholar]
- Fazio R.H., Ruisch B.C., Moore C.A., Granados Samayoa J.A., Boggs S.T., Ladanyi J.T. Social distancing decreases an individual’s likelihood of contracting COVID-19. Proc. Natl. Acad. Sci. USA. 2021;118(8) doi: 10.1073/pnas.2023131118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson N., Laydon D., Nedjati-Gilani G., Imai N., Ainslie K., Baguelin M., et al. Report 9: impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. Imperial College London. 2020;10(77482):491–497. [Google Scholar]
- Figueiredo A.M., Codina A.D., Figueiredo D., Saez M., León A.C. Impact of lockdown on COVID-19 incidence and mortality in China: an interrupted time series study. Bull. World Health Organ. 2020;6 [Google Scholar]
- Flaxman S., Mishra S., Gandy A., Unwin H.J.T., Mellan T.A., Coupland H., et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- Gallaway M.S., Rigler J., Robinson S., Herrick K., Livar E., Komatsu K.K., et al. Trends in COVID-19 incidence after implementation of mitigation measures—Arizona, January 22–August 7, 2020. Morbid. Mortal. Wkly. Rep. 2020;69(40):1460. doi: 10.15585/mmwr.mm6940e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-García D., Herranz-Hernández R., Rojas-Benedicto A., León-Gómez I., Larrauri A., Peñuelas M., et al. Assessing the effect of non-pharmaceutical interventions on COVID-19 transmission in Spain, 30 August 2020 to 31 January 2021. Eurosurveillance. 2022;27(19) doi: 10.2807/1560-7917.ES.2022.27.19.2100869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghanbari M.K., Behzadifar M., Imani-Nasab M.H., Behzadifar M., Bakhtiari A., Mir I., et al. 2020. The impact of the social distancing policy on COVID-19 new cases in Iran: Insights from an interrupted time series analysis. [PMC free article] [PubMed] [Google Scholar]
- Ghosal S., Bhattacharyya R., Majumder M. Impact of complete lockdown on total infection and death rates: a hierarchical cluster analysis. Diab. Metab. Syndr. Clin. Res. Rev. 2020;14(4):707–711. doi: 10.1016/j.dsx.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta A., Zhu H., Doan M.K., Michuda A., Majumder B. Economic impacts of the COVID− 19 lockdown in a remittance‐dependent region. Am. J. Agric. Econ. 2021;103(2):466–485. [Google Scholar]
- Guzzetta, G., Riccardo, F., Marziano, V., Poletti, P., Trentini, F., Bella, A., et al., 2020. The impact of a nation-wide lockdown on COVID-19 transmissibility in Italy.
- Hale T., Webster S., Petherick A., Phillips T., Kira B. Vol. 8. 2020. Oxford COVID-19 government response tracker (OxCGRT). Last updated; p. 30. [DOI] [PubMed] [Google Scholar]
- Hendrix M.J. Absence of apparent transmission of SARS-CoV-2 from two stylists after exposure at a hair salon with a universal face covering policy—Springfield, Missouri, May 2020. MMWR Morbid. Mortal. Wkly. Rep. 2020;69 doi: 10.15585/mmwr.mm6928e2. [DOI] [PubMed] [Google Scholar]
- Herstein J.J., Degarege A., Stover D., Austin C., Schwedhelm M.M., Lawler J.V., et al. Characteristics of SARS-CoV-2 transmission among meat processing workers in Nebraska, USA, and effectiveness of risk mitigation measures. Emerg. Infect. Dis. 2021;27(4):1032–1039. doi: 10.3201/eid2704.204800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter P.R., Colón-González F.J., Brainard J., Rushton S. Impact of non-pharmaceutical interventions against COVID-19 in Europe: a quasi-experimental study. MedRxiv. 2020;26(28):2001401. doi: 10.2807/1560-7917.ES.2021.26.28.2001401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyafil A., Moriña D. Analysis of the impact of lockdown on the evolution Covid-19 epidemics in Spain. medRxiv. 2020 [Google Scholar]
- Islam N., Sharp S.J., Chowell G., Shabnam S., Kawachi I., Lacey B., et al. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. Bmj. 2020;370 doi: 10.1136/bmj.m2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabakama S., Konje E.T., Dinga J.N., Kishamawe C., Morhason-Bello I., Hayombe P., et al. Commentary on COVID-19 vaccine hesitancy in sub-Saharan Africa. Trop. Med. Infect. Dis. 2022;7(7):130. doi: 10.3390/tropicalmed7070130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaivanov A., Lu S., Shigeoka H. Face mask mandates slowed the spread of COVID-19 in Canada. VoxEU org. 2020:5. [Google Scholar]
- Kaufman B.G., Whitaker R., Mahendraratnam N., Hurewitz S., Yi J., Smith V.A., et al. State variation in effects of state social distancing policies on COVID-19 cases. BMC Public Health. 2021;21(1):1239. doi: 10.1186/s12889-021-11236-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh W.C., Naing L., Wong J. Estimating the impact of physical distancing measures in containing COVID-19: an empirical analysis. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2020;100:42–49. doi: 10.1016/j.ijid.2020.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon S., Joshi A.D., Lo C.-H., Drew D.A., Nguyen L.H., Guo C.-G., et al. Association of social distancing and face mask use with risk of COVID-19. Nat. Commun. 2021;12(1):3737. doi: 10.1038/s41467-021-24115-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemaitre J.C., Perez-Saez J., Azman A.S., Rinaldo A., Fellay J. Assessing the impact of non-pharmaceutical interventions on SARS-CoV-2 transmission in Switzerland. Swiss Med. Wkly. 2020;150:21–22. doi: 10.4414/smw.2020.20295. [DOI] [PubMed] [Google Scholar]
- Li Y., Li M., Rice M., Zhang H., Sha D., Li M., et al. The impact of policy measures on human mobility, COVID-19 cases, and mortality in the US: a spatiotemporal perspective. Int. J. Environ. Res. Public Health. 2021;18(3):996. doi: 10.3390/ijerph18030996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lio C.F., Cheong H.H., Lei C.I., Lo I.L., Yao L., Lam C., et al. Effectiveness of personal protective health behaviour against COVID-19. BMC Public Health. 2021;21(1) doi: 10.1186/s12889-021-10680-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Morgenstern C., Kelly J., Lowe R., Jit M. The impact of non-pharmaceutical interventions on SARS-CoV-2 transmission across 130 countries and territories. BMC Med. 2021;19(1):40. doi: 10.1186/s12916-020-01872-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loembé M.M., Nkengasong J.N. COVID-19 vaccine access in Africa: global distribution, vaccine platforms, and challenges ahead. Immunity. 2021;54(7):1353–1362. doi: 10.1016/j.immuni.2021.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewenthal G., Abadi S., Avram O., Halabi K., Ecker N., Nagar N., et al. COVID‐19 pandemic‐related lockdown: response time is more important than its strictness. EMBO Mol. Med. 2020;12(11):e13171. doi: 10.15252/emmm.202013171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyu W., Wehby G.L. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US: study examines impact on COVID-19 growth rates associated with state government mandates requiring face mask use in public. Health Affairs. 2020;39(8):1419–1425. doi: 10.1377/hlthaff.2020.00818. [DOI] [PubMed] [Google Scholar]
- Mathieu E., Ritchie H., Ortiz-Ospina E., Roser M., Hasell J., Appel C., et al. A global database of COVID-19 vaccinations. Nat. Human Behav. 2021:1–7. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- Mathieu E.R.H., Ortiz-Ospina E., Roser M., Hasell J., Appel C., et al. Coronavirus (COVID-19) Vaccinations. https://ourworldindata.org/covid-vaccinations2023
- Mégarbane B., Bourasset F., Scherrmann J.M. Is lockdown effective in limiting SARS-CoV-2 epidemic progression?—a cross-country comparative evaluation using epidemiokinetic tools. J. Gen. Intern. Med. 2021;36(3):746–752. doi: 10.1007/s11606-020-06345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehtar S., Preiser W., Lakhe N.A., Bousso A., TamFum J.-J.M., Kallay O., et al. Limiting the spread of COVID-19 in Africa: one size mitigation strategies do not fit all countries. Lancet Global Health. 2020;8(7):e881–e883. doi: 10.1016/S2214-109X(20)30212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Van Stralen M.M., West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci. 2011;6(1):1–12. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miguel E., Mobarak A.M. National Bureau of Economic Research; 2021. The economics of the covid-19 pandemic in poor countries. [Google Scholar]
- Milazzo A., Giles L., Parent N., McCarthy S., Laurence C. The impact of non-pharmaceutical interventions on COVID-19 cases in South Australia and Victoria. Austral. New Zeal. J. Public Health. 2022;46(4):482–487. doi: 10.1111/1753-6405.13249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell T., Dee D.L., Phares C.R., Lipman H.B., Gould L.H., Kutty P., et al. Non-pharmaceutical interventions during an outbreak of 2009 pandemic influenza A (H1N1) virus infection at a large public university, April–May 2009. Clin. Infect. Dis. 2011;52(suppl_1):S138–S145. doi: 10.1093/cid/ciq056. [DOI] [PubMed] [Google Scholar]
- Mitze T., Kosfeld R., Rode J., Wälde K. Face masks considerably reduce COVID-19 cases in Germany. Proc. Natl. Acad. Sci. USA. 2020;117(51):32293–32301. doi: 10.1073/pnas.2015954117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musa S.S., Zhao S., Wang M.H., Habib A.G., Mustapha U.T., He D. Estimation of exponential growth rate and basic reproduction number of the coronavirus disease 2019 (COVID-19) in Africa. Infect. Dis. Poverty. 2020;9(1):1–6. doi: 10.1186/s40249-020-00718-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nader I.W., Zeilinger E.L., Jomar D., Zauchner C. Onset of effects of non-pharmaceutical interventions on COVID-19 infection rates in 176 countries. BMC Public Health. 2021;21(1):1472. doi: 10.1186/s12889-021-11530-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olney A.M., Smith J., Sen S., Thomas F., Unwin H.J.T. Estimating the effect of social distancing interventions on COVID-19 in the United States. Am. J. Epidemiol. 2021;190(8):1504–1509. doi: 10.1093/aje/kwaa293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piovani D., Christodoulou M.N., Hadjidemetriou A., Pantavou K., Zaza P., Bagos P.G., et al. Effect of early application of social distancing interventions on COVID-19 mortality over the first pandemic wave: an analysis of longitudinal data from 37 countries. J. Infect. 2021;82(1):133–142. doi: 10.1016/j.jinf.2020.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pozo-Martin F., Weishaar H., Cristea F., Hanefeld J., Bahr T., Schaade L., et al. The impact of non-pharmaceutical interventions on COVID-19 epidemic growth in the 37 OECD member states. Eur. J. Epidemiol. 2021;1-12 doi: 10.1007/s10654-021-00766-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qureshi A.I., Suri M., Chu H., Suri H., Suri A. Early mandated social distancing is a strong predictor of reduction in peak daily new COVID-19 cases. Public Health. 2021;190:160–167. doi: 10.1016/j.puhe.2020.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rader B., White L.F., Burns M.R., Chen J., Brilliant J., Cohen J., et al. Mask-wearing and control of SARS-CoV-2 transmission in the USA: a cross-sectional study. Lancet Digit Health. 2021;3(3):e148–e157. doi: 10.1016/S2589-7500(20)30293-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regmi K., Lwin C.M. Factors associated with the implementation of non-pharmaceutical interventions for reducing coronavirus disease 2019 (COVID-19): a systematic review. Int. J. Environ. Mental Res. Public Health. 2021;18(8):4274. doi: 10.3390/ijerph18084274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis R.F., de Melo Quintela B., de Oliveira Campos J., Gomes J.M., Rocha B.M., Lobosco M., et al. Characterization of the COVID-19 pandemic and the impact of uncertainties, mitigation strategies, and underreporting of cases in South Korea, Italy, and Brazil. Chaos Solitons Fractals. 2020;136 doi: 10.1016/j.chaos.2020.109888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu S., Ali S.T., Noh E., Kim D., Lau E.H., Cowling B.J. Transmission dynamics and control of two epidemic waves of SARS-CoV-2 in South Korea. BMC Infect. Dis. 2021;21(1):1–9. doi: 10.1186/s12879-021-06204-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saez M., Tobias A., Varga D., Barceló M.A. Effectiveness of the measures to flatten the epidemic curve of COVID-19. The case of Spain. Sci. Total Environ. 2020;727 doi: 10.1016/j.scitotenv.2020.138761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saki M., Ghanbari M.K., Behzadifar M., Imani-Nasab M.H., Behzadifar M., Azari S., et al. The impact of the social distancing policy on COVID-19 incidence cases and deaths in Iran from February 2020 to January 2021: insights from an interrupted time series analysis. Yale J. Biol. Med. 2021;94(1):13–21. [PMC free article] [PubMed] [Google Scholar]
- Salihu Sabiu Musa X.W., Zhao S., Li S., Hussaini N., Wang W., He D. The heterogeneous severity of COVID-19 in African countries: a modeling approach. Bull. Math. 2022;84(3):32. doi: 10.1007/s11538-022-00992-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez J.N., Reyes G.A., Martínez‐López B., Johnson Christine K. Impact of social distancing on early SARS‐CoV‐2 transmission in the United States. Zoon. Public Health. 2022;69(6):746–756. doi: 10.1111/zph.12909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott N., Saul A., Spelman T., Stoove M., Pedrana A., Saeri A., et al. The introduction of a mandatory mask policy was associated with significantly reduced COVID-19 cases in a major metropolitan city. PLoS One. 2021;16(7) doi: 10.1371/journal.pone.0253510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharif N., Alzahrani K.J., Ahmed S.N., Opu R.R., Ahmed N., Talukder A., et al. Protective measures are associated with the reduction of transmission of COVID-19 in Bangladesh: a nationwide cross-sectional study. PLoS One. 2021;16(11 November) doi: 10.1371/journal.pone.0260287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siedner M.J., Harling G., Reynolds Z., Gilbert R.F., Haneuse S., Venkataramani A.S., et al. Social distancing to slow the US COVID-19 epidemic: longitudinal pretest–posttest comparison group study. PLoS Med. 2020;17(8) doi: 10.1371/journal.pmed.1003244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva L., Figueiredo Filho D., Fernandes A. The effect of lockdown on the COVID-19 epidemic in Brazil: evidence from an interrupted time series design. Cad Saude Publica. 2020;36(10) doi: 10.1590/0102-311X00213920. [DOI] [PubMed] [Google Scholar]
- Singh S., Shaikh M., Hauck K., Miraldo M. Impacts of introducing and lifting nonpharmaceutical interventions on COVID-19 daily growth rate and compliance in the United States. Proc. Natl. Acad. Sci. USA. 2021;118(12) doi: 10.1073/pnas.2021359118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes J., Turner A.J., Anselmi L., Morciano M., Hone T. The relative effects of non-pharmaceutical interventions on wave one Covid-19 mortality: natural experiment in 130 countries. BMC Public Health. 2022;22(1):1113. doi: 10.1186/s12889-022-13546-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sypsa V., Roussos S., Paraskevis D., Lytras T., Tsiodras S., Hatzakis A. Effects of social distancing measures during the first epidemic wave of severe acute respiratory syndrome infection, Greece. Emerg. Infect. Dis. 2021;27(2):452–462. doi: 10.3201/eid2702.203412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torjesen I. Covid-19 will become endemic but with decreased potency over time, scientists believe. BMJ: Brit. Med. J. (Online). 2021:372. doi: 10.1136/bmj.n494. [DOI] [PubMed] [Google Scholar]
- Tran P., Tran L., Tran L. The influence of social distancing on COVID-19 mortality in US counties: cross-sectional study. JMIR Public Health Surveil. 2021;7(3) doi: 10.2196/21606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triukose S., Nitinawarat S., Satian P., Somboonsavatdee A., Chotikarn P., Thammasanya T., et al. Effects of public health interventions on the epidemiological spread during the first wave of the COVID-19 outbreak in Thailand. PLoS One. 2021;16(2 February 2021) doi: 10.1371/journal.pone.0246274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Dyke M.E., Rogers T.M., Pevzner E., Satterwhite C.L., Shah H.B., Beckman W.J., et al. Trends in county-level COVID-19 incidence in counties with and without a mask mandate - Kansas, June 1-August 23, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69(47):1777–1781. doi: 10.15585/mmwr.mm6947e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma B.K., Verma M., Verma V.K., Abdullah R.B., Nath D.C., Khan H.T.A., et al. Global lockdown: an effective safeguard in responding to the threat of COVID‐19. J. Eval. Clin. Pract. 2020;26(6):1592–1598. doi: 10.1111/jep.13483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vukotich C.J., Coulborn R.M., Aragon T.J., Baker M.G., Burrus B.B., Aiello A.E., et al. 2010. Findings, gaps, and future direction for research in nonpharmaceutical interventions for pandemic influenza. [DOI] [PubMed] [Google Scholar]
- Wagner A.B., Hill E.L., Ryan S.E., Sun Z., Deng G., Bhadane S., et al. Social distancing merely stabilized COVID‐19 in the United States. Stat (International Statistical Institute) 2020;9(1):e302. doi: 10.1002/sta4.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Tian H., Zhang L., Zhang M., Guo D., Wu W., et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob Health. 2020;5(5) doi: 10.1136/bmjgh-2020-002794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster R.G. Predictions for future human influenza pandemics. J. Infect. Dis. 1997;176(Supplement_1):S14–S19. doi: 10.1086/514168. [DOI] [PubMed] [Google Scholar]
- Whitelaw T. The practical aspects of quarantine for influenza. Can. Med. Assoc. J. 1919;9(12):1070. [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation . 2020. Draft landscape of COVID-19 candidate vaccines–4 March 2020. [Google Scholar]
- World Health Organisation WHO Coronavirus (COVID-19) Dashboard. 2022. https://covid19.who.int/2022
- World Health Organization Nonpharmaceutical interventions for pandemic influenza, national and community measures. Emerg. Infect. Dis. 2006;12(1):88. doi: 10.3201/eid1201.051371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; 2020. Advice on the use of masks in the context of COVID-19: interim guidance, 5 June 2020. [Google Scholar]
- World Health Organization . World Health Organisation; 2020. Coronavirus disease 2019 (COVID-19) situation report-51. [Google Scholar]
- Woskie L.R., Hennessy J., Espinosa V., Tsai T.C., Vispute S., Jacobson B.H., et al. Early social distancing policies in Europe, changes in mobility & COVID-19 case trajectories: insights from Spring 2020. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0253071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan Y., Pang Y., Lyu Z., Wang R., Wu X., You C., et al. The COVID-19 vaccines: recent development, challenges and prospects. Vaccines. 2021;9(4):349. doi: 10.3390/vaccines9040349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W., Shaff J., Shaman J. Effectiveness of non-pharmaceutical interventions to contain COVID-19: a case study of the 2020 spring pandemic wave in New York City. J. R. Soc. Interface. 2021;18(175):20200822. doi: 10.1098/rsif.2020.0822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung W., Ng K., Fong J.N., Sng J., Tai B.C., Chia S.E. Assessment of proficiency of N95 mask donning among the general public in Singapore. JAMA Network Open. 2020;3(5):e209670. doi: 10.1001/jamanetworkopen.2020.9670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Warner M.E. COVID-19 policy differences across US States: shutdowns, reopening, and mask mandates. Int. J. Environ. Res. Public Health. 2020;17(24) doi: 10.3390/ijerph17249520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Li Y., Zhang A.L., Wang Y., Molina M.J. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc. Natl. Acad. Sci. 2020;117(26):14857–14863. doi: 10.1073/pnas.2009637117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou C. Evaluating system for effectiveness of mask mandates and the most influential factor in each state in the USA. J. Phys. Conf. Ser. 2021;1994(1) IOP Publishing. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.