Abstract
Since early May 2022, an outbreak due to Mpox virus (formerly called monkeypox) has occurred in many countries around the world. On July 23, the World Health Organization declared the outbreak ‘Public Health Emergency of International Concern’. In order to combat the outbreak, it is important to have effective infection prevention and control plans. The first step is to qualitatively and quantitatively determine the risks of infections, followed by the design and implementation of infection prevention and control measures. Mpox is transmitted through direct, indirect, and prolonged contact, through sexual transmission, and via the respiratory route. Men who have sex with men are identified as the most vulnerable population. Home pet-raisers, and health care workers are at risk of catching the disease. The outcome of infection is catastrophic among the elderly, immunocompromised individuals, pregnant female and children. The spillover to animals is of great concern. It is important to communicate the risks and have community engagement in the control of this outbreak. The availability of vaccines will add to the capability of containing the outbreak. It is critical to prevent the virus from spreading further. Hence, we review the recent findings on the risk management of Mpox along with the preventive strategies.
Keywords: Monkeypox, Mpox, Outbreak, Infection prevention and control, Risk assessment
Introduction
Mpox virus formerly Monkeypox virus; is a double-stranded DNA virus with two distinct genetic clades: clade I (circulating in Central Africa; former Congo Basin clade) and clade II, divided into subclades IIa and IIb (former West African clade). Together with the variola virus, the causative agent of smallpox, they are members of the Poxviridae family. In 1980, after the eradication of smallpox, the smallpox vaccination campaigns, which conferred protection against other poxviruses as well, including Mpox, were discontinued. Hence, individuals borne thereafter have become susceptible to acquiring infection from members of the Poxviridae family. While most circulation of Mpox occurs in Africa, over the past couple of decades sporadic cases have been reported outside that region [1]. More recently, in May 2022, a multi-country outbreak of Mpox infection was reported in multiple countries around the globe.
Mpox virus is a zoonosis with the potential for human-to-human transmission, predominantly through direct contact with body fluids, lesion material, or fomites (e.g., contaminated linens) and after prolonged face-to-face contact. Being an orthopoxvirus, it spreads primarily by respiratory droplets. For individuals whose infection extends to the lower respiratory tract or develops severe systemic disease requiring hospitalization, the possibility of an airborne route of infection has not been excluded [2]. Sexual transmission has also been proven based on many findings, including the occurrence of cases predominately among men who have sex with men (MSM), the association with unexpected anal and genital lesions, and the detection of the Mpox virus in seminal fluid, genital and rectal lesions, feces, and saliva of confirmed cases [3], [4]. The invasive route of infection, such as intercourse vs. exposure to fomites, causes a severer form of the disease and a shorter incubation period [5]. Vertical virus transmission can occur via the placenta from mother to fetus or through close contact during and after birth. Limited data suggest that infection during pregnancy may lead to adverse outcomes for the fetus [2].
The Mpox infection begins with a rash that may be situated on or near the genitals or anus. Rash could appear on other body areas, depending on the route of transmission. The rash will go through several stages before healing and may be painful or itchy. The rash may appear first, or sometimes flu-like symptoms may be evident before the rash [1]. The spectrum of the disease ranges from mild to severe and can be fatal depending on the initial health status of the patient, their immune response, previous vaccination, the presence of comorbidities, and the route of exposure [6]. In addition to the clinical picture and history of contact with a suspected or confirmed case, the laboratory diagnosis of Mpox is confirmed by two-stage testing, first with a panorthopox polymerase chain reaction (PCR) followed by a specific Mpox PCR test. The PCR tests utilize samples collected from skin lesions: the roof, fluid from vesicles and pustules, and dry crusts, or from the throat, depending on the phase of the disease [7]. Treatment is generally supportive and potentially involves the use of antiviral drugs. Two antiviral medications, tecovirimat and brincidofovir, were approved for use in smallpox by the United States Food and Drug Administration (US FDA), but neither was tested on humans in phase 3 efficacy trials [8], [9].
Since its global emergence in early May 2022, cases of Mpox have been growing steadily. As of March 2023, a total of 86,496 laboratory confirmed cases and 111 death, have been reported to the WHO from 110 countries/areas/territories. The World Health Organization (WHO) risk assessment, categorizes African region, Eastern Mediterranean region, European region and region of the Americas as Moderate, while south east Asia region, Western Pacific region as low. All samples from the current global outbreak have been identified as subclade IIb. Mpox deaths have been mostly connected to viral encephalitis, brain edema, and underlying immunocompromising disorders and comorbidities [10]. The spread of the Mpox beyond non-endemic countries ("Central and West African countries") resulted in the declaration of the current Mpox virus outbreak's ongoing spread as a Public Health Emergency of International Concern ("PHEIC") by the WHO on July 23rd, 2022 [11]. This announcement signals the seriousness and urgency with which countries around the world should respond. Ending the Mpox outbreak is a critical priority, calling for the exploration of every option on the table to combat it and protect communities at risk. Designing and implementing sound infection prevention and control (IPC) programs provide an efficient means for terminating the outbreak. An infection control risk assessment should precede, which involves recognizing activities that contribute to infection dissemination and identifying individuals who are most vulnerable to catching the disease. This review will adopt the risk management approach to discuss Mpox disease, based on which, the multi-faceted approaches to the IPC strategies are recommended.
Risk assessment of Mpox
The quantitative determination of overall risk is the sum of the infection probability and the disease impact on the affected population [7].
The recent international spread of human cases of Mpox has been reported predominantly among MSM and persons with multiple sexual partners [5]. It was also diagnosed among persons raising pet mammals at home [12], mainly rodents, and among health care workers (HCWs).
MSM associated risk
A considerable proportion of the MSM population is vulnerable to Mpox infection. Specific sexual patterns (e.g., having multiple casual sexual contacts and/or multiple sexual partners in interconnected sexual networks, attending sexual events occurring in Europe over the spring and summer months, and attending chemsex parties) could further facilitate the disease transmission [13]. Enclosed spaces, such as back rooms, saunas, and private or public sex clubs where intimate, often anonymous sexual contact occurs, provide a favorable place for Mpox spreading [14].
In the current outbreak, and so far, most cases reported among MSM have been described as mild. The low impact of Mpox coupled with the high likelihood of infection results in an overall moderate threat. However, it is to be emphasized that this moderate risk may be higher for the elderly, those with untreated HIV infection, or immunocompromised individuals [2], as shown in Table 1.
Table 1.
Summary of risk assessment for the different population categories.
| Community level |
Healthcare facility level |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| MSM and persons with multiple sexual partners | General population |
High risk groups |
Pet contact |
HCWs |
Laboratory workers |
||||
| Protected | Unprotected | Protected | Unprotected | ||||||
| Probability | High | Very low | Low | HIGH | Very low | High | Medium | Very low | High |
| Impact | Low | very low to low | High | Low-high | Low | Low | Low | Low | Moderate |
| Overall risk | Moderate | Low | Moderate | Moderate/high | Low | Moderate | Moderate/low | Low | High |
Risk for the broader population, including home pet-raisers
Overall, the likelihood of further spread of Mpox among the broader population is estimated to be very low, leading to an overall low risk. However, the individual risk for elderly or immunocompromised individuals, home pet-raisers, young children, and pregnant women could be higher (Table 1).
Gatherings and crowds are associated with an enhanced possibility of acquiring the infection. During such activities, attendees' expected high density and movement display a conducive environment for close, lengthy, and frequent interactions between people. Of critical importance are events associated with the wide adoption of risky behaviors and unsafe practices, including unsafe sexual practices [14], which extensively contribute to the spread of the disease. All those factors should be studied on an ongoing basis for each locality to assess its epidemiological profile and get insight into the dynamic changes expected among the local risk categories.
Risk for HCWs
Occupational exposure to the mypox virus has recently been identified as an issue of major concern. Mpox virus can remain on surfaces for a long time, although its potential for infection is unknown [15]. In contrast to transmission to HCW in endemic settings, which is well described, available literature outside endemic regions is limited by non-standardized exposure definitions and limited detail describing acquaintances [16]. The hazard of healthcare-connected infection was documented in 2018 in the UK before the current Mpox outbreak [17]. The likelihood of Mpox transmission to HCWs donning proper personal protective equipment (PPE) is extremely low. With the disease having an estimated low impact, an overall low risk is anticipated in this category. Unprotected HCWs are at medium or high risk of infection based on the appropriateness of used PPE [7], [17]. They have a medium risk of contracting the infection in the following scenarios: 1) fulfilling activities leading to contact between any components of clothing and the patient’s skin lesions or bodily fluids, or soiled linen or dressings, or helping with transfer while wearing gloves but not a gown, 2) close proximity with no direct contact in the same room or indoor physical space as a symptomatic Mpox patient, without a surgical mask at a minimum. However, the overall risk of infection ranges from low/to medium in certain situations. Unprotected HCWs are at high risk of infection when: 1) their skin or mucous membranes are exposed to the skin, lesions, or bodily fluids from a patient or contaminated material (e.g., linen or clothing), 2) during a procedure inside the patient’s room that may generate aerosols from oral or respiratory secretions, skin lesions, or the resuspension of dry exudates; 3) they inhale droplets or dust from patients or their immediate environment, 4) exposed to penetrating sharps’ injury from a device or via broken gloves; 4) exposed to penetrating sharps' injury from a device or broken gloves; The overall risk is assessed as moderate (Table 1). So, at each HCW’s exposure, the risk should be thoroughly assessed to determine the expected level of catching the infection. Accordingly, HCWs should receive counseling on self-monitoring, timely reporting, and isolation. Mpox risk mitigation among HCWs shouldn’t take over the current outbreak.
Risk for laboratory personnel
The Advisory Committee on Dangerous Pathogens (ACDP), ranks Mpox virus as an ACDP Category 3 pathogen [18]. The chance of occupational vulnerability is low for personnel pursuing proper biosafety approaches. Unprotected exposure carries a high likelihood of infection and a moderate risk of the disease (due to the direct exposure of mucosae to a potentially substantial quantity of virus). The danger for unprotected laboratory staff is estimated to be high (Table 1). Laboratory managers, personnel, and occupational health officers for each facility must perform site- and activity-specific risk assessments for Mpox testing to determine whether enhanced safety precautions are needed.
Risk for household contacts
The current outbreak of mpox is caused by clade II, which is classified as a non-high consequence infectious disease (non-HCID). This is reflected on the risk assessment and follow-up of contacts of symptomatic mpox cases. There are three risk categories with three different management plans: 1: high-risk (category 3), which comprises unprotected direct contact or high-risk environmental contact; 2: medium-risk (category 2), which includes unprotected exposure to infectious materials, including droplets or airborne potential routes; and 3: low-risk (category 1), which involves protected physical or droplet exposure, no physical contact, unlikely droplet exposure). The secondary attack rate ranges from 0 % to 11 % among unvaccinated household contacts [19].
Risk for travelers and mass gatherings
Based on available information at this time, travelers, passengers, and others who may have had prolonged and near contact with an infectious individual may catch the infection [20]. In countries with recently imported cases of monkeypox, or those that are otherwise experiencing human-to-human transmission, national authorities should establish risk-based policies and guidance related to border measures and international travel.
Risk of spillover events to animal species
The probability of spillover is determined by the interactions among the barriers and the associated bottlenecks that might prevent cross-species transmission. Many of these interactions are nonlinear and dynamic in space and time. Mpox transmission from humans to animals, with pets being of concern, cannot be excluded. A spillover event could likely lead to the virus establishment in wildlife and the disease turning into an endemic zoonosis. So far, USA Animal Health Authorities have found that the probability of the spill-over event in the US is very low [21]. However, in June 2022, the evidence of the first human-to-dog transmission of Mpox in France was published in the Lancet on August 10 [22]. Additional cases have been notified in Brazil [23].
Pets are an essential part of the western world household. In the USA, according to the 2021–2022 National Pet Owners Survey, it is established that 70 % of U.S. households, or about 90.5 million families, own a pet, and small animals rank fifth by type of animal, surpassing 56 % of households in 1988 and 67 % in 2019 [24]. In the U.K. in 2020, an estimated 100,000 rats were kept as pets [25]. The absence of appropriate pet home-raising legalization can contribute significantly to the augmented probability of Mpox virus transmission from human to animal. Since rodents, and particular species of the family Sciuridae (squirrels), are likely to be proper hosts, more so than humans, transmission from humans to (pet) animals is a serious event that could potentially lead to the virus establishment in wildlife and the disease evolving into an endemic zoonosis, leading to more spread of Mpox virus among the broader population.
Point of care risk assessment
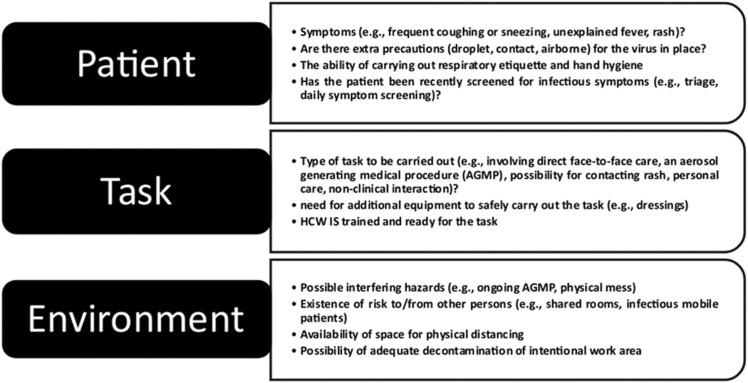
At health care facilities the risk assessment hierarchy ends with the point of care risk assessment (PCRA), which every HCW should apply for all Mpox patients, whether suspected or confirmed. PCRA objectives are to identify the risk of exposure, determine appropriate routine practices, and propose additional precautions that can contribute to high quality of care. By applying PCRA, HCWs apply necessary component coupled with the routine practices for prevention and control of Mpox [26], [27] ( Fig. 1).
Fig. 1.
Point of care risk assessment (PCRA): before each patient interaction, the HCW should inquire about issues related to the patient, the tasks to be done, and the surrounding environment [26], [27].
Risk management, communication, and community engagement
Mpox-related risks and consequent hazards are to be communicated to all vulnerable groups and the population. Community leaders, non-governmental and civil society organizations, and HCWs, including those at sexual health clinics, should be involved in such communications. Regional, national, sub-national, and local organizations, including activist groups and community testing organizations (i.e., checkpoints) working on health for MSM and lesbian, gay, bisexual, and transgender (LGBT) communities, should join after being notified and requested to participate with their members, users, and networks in raising awareness as regards various aspects of Mpox [14]. Patients recovering from Mpox can help in that respect. Once they leave the health care facility, much of the IPC rests in their hands. They should have additional comprehensive information to strengthen their capability to influence and impress others [2].
IPC interventions
IPC activities implemented to contain the pandemic can be broadly categorized into empirical and specific measures.
IPC empirical measures
Implementation of appropriate IPC measures both in community and health care settings is essential to mitigate and control transmission. To achieve this goal, collaborative work must meet two strategic objectives: the first is to eliminate the role of animals as primary transmitters, and the second is to abolish the possibility of human-to-human transmission.
Preventive measures for primary (animal-to-human) transmission of Mpox
In order to control the current epidemic, good interventions, regulations, and legalization targeting pets are to be formulated and implemented. Pets that were in contact with a symptomatic Mpox patient need to be kept away from other animals/people for the incubation period of 21 days. Mpox infected patients should not take care of exposed pets, and pets with Mpox infection may need to be cared for in designated places [12]. At an individual level, if one’s pet shows signs of Mpox or has been exposed to the virus, it is not recommended to get rid of it unless directed by a veterinarian, whose guidelines should also be sought for case management. Hand hygiene and appropriate PPE are mandatory for any contact. An infected pet should be isolated after becoming ill until full recovery. Pregnant women, young children (< 8 years of age), immunocompromised individuals, or those with a history of atopic dermatitis or eczema should not deliver care for an ill animal. Waste should be disposed of promptly and not left or disposed of outdoors as Mpox virus infections in wildlife may ensue [21]. If appropriate for the species and the plumbing system, flush the animal waste down the toilet. Household disinfection is to follow the general guidance on cleaning and disinfecting non-healthcare settings [28]. In order to avoid the spillover phenomenon, people with Mpox should avoid contact with animals, and someone else in a separate home is to take care of it [12]. If a history of close contact is evident, the pet should be kept at home and away from other animals and people for 21 days after the most recent contact. After the person with Mpox is recovered, a home should be disinfected before bringing healthy animals back [28].
Preventive measures for secondary (human-to-human) transmission of Mpox
Symptomatic contacts should be isolated during their investigation until Mpox is excluded. Confirmed, suspected, or probable cases are advised to refrain from sex until all skin lesions have crusted, the scabs have dropped off, and a fresh layer of skin has developed underneath, or until the infection is excluded. Abstain from sex with anyone having a history of exposure for 21 days. Using a condom alone is not enough to safeguard against transmission of Mpox virus because transmission through droplets in prolonged face-to-face contact is also possible. If sex practice is inevitable, practice safely [26], including the use of condoms and dental dams for 12 weeks after recovery while limiting the number of sex partners. Involvement of sexual health services in partner notification for sexually transmitted diseases is advised [1].
Specific IPC measures
IPC at healthcare facilities
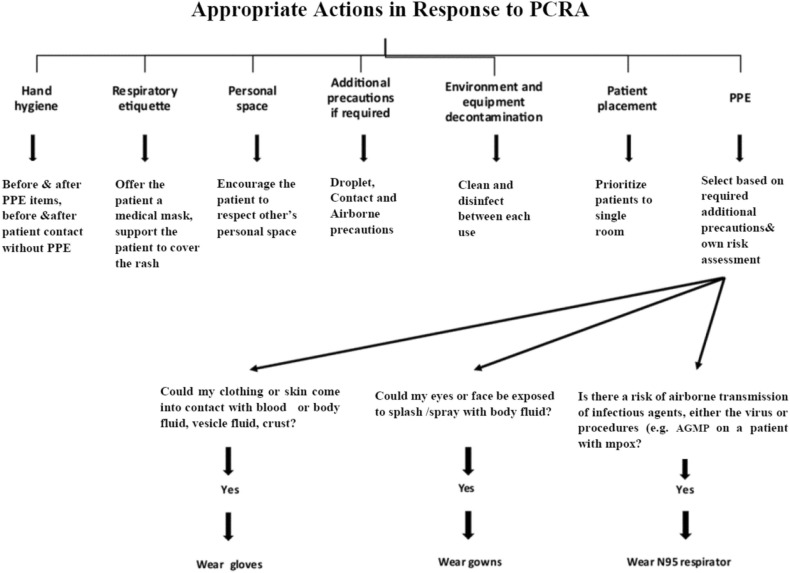
IPC at health care facilities falls into three implementation integrating pathways: engineering, administrative, and PPE controls. Competency-based training for Mpox case definition and diagnosis and IPC isolation precautions should be provided [2]. Appropriate actions in response to PCRA are to be taken ( Fig. 2).
Fig. 2.
Health care workers’ appropriate actions, in response to PCRA adapted from[26], [27]. AGMP; Aerosol Generating Medical Procedures.
After diagnosis, the patient is to be given a well-fitting, fluid-resistant mask and isolated in a well-ventilated single room or cohorted with other patients having a similar clinical diagnosis (or in an airborne-isolation room, if required by health authorities). HCWs entering the room should preferably be immunized against smallpox [29]. All recommendations for transferring an infected patient should be applied when transfer is mandatory inside or outside the hospital [26]. Cases, including immunosuppressed patients, may show prolonged viral shedding from the upper respiratory tract and may be re-evaluated to decide when isolation precautions can be terminated [2]. The infectivity of patients with positive upper respiratory tract swabs and crusted skin lesions remains doubtful, an area calling for further study [6].
Cleaning of the patient room is carried out by procedures applied to high-risk areas, followed by disinfection with Sodium hypochlorite [11]. Thorough management of soiled laundry [2] and waste materials is mandatory. It is worth mentioning that medical waste from patients in the current outbreak (clade IIb) should be managed as a "category A" infectious substance; an infectious substance capable of causing permanent disability or life-threatening disease, while medical waste from patients infected with clade I is considered "category B"; not capable of causing such damage [30].
IPC measures for the laboratory personnel
Manipulating, processing, and testing specimens suspected to contain Mpox virus are recommended in biosafety level 2 (BSL-2) facilities with vaccinated staff [31]. If staff is not vaccinated, it is recommended to use BSL-3 facilities [32]. For non-lesion specimens (e.g., urine, blood), culture/sensitivity testing, and when viral DNA is extracted, using a BSL-2 containment facility and procedures is enough. Laboratory waste should be decontaminated on-site before disposal [30].
IPC at home
All types of sex are prohibited, and neither pets nor domestic animals are allowed in the patient’s environment. All elements of Standard Precautions, Contact Precautions, Droplet Precautions, and Airborne Precautions, if healthcare authorities require them) should be strictly followed by both patient and household until the infectious period ends [32].
IPC at a broader population level
Self-protection includes avoiding close contact with suspected Mpox cases, avoiding sharing of places and/or personal items, strict adherence to hand hygiene, and maintaining respiratory etiquette. Precautions should last 21 days from the last exposure or until the infection is excluded. All close contact(s) is/are advised to: self-monitor for the development of symptoms; defer from blood, organ, or bone marrow donations; and avoid close physical contact with young children, pregnant women, and immunocompromised persons [5].
Emphasis should be placed on athletic community. It is essential to educate all stakeholders (especially high-risk sports), including athletes, parents, coaches, administrators, medical personnel (i.e., athletic trainers, physical therapists, team physicians), and other affiliated personnel (e.g., massage therapists, strength and conditioning coaches) on Mpox, how it compares to other infectious diseases, and the importance of preventing outbreaks. This may help individuals identify Mpox before sports-related exposures take place and cause an outbreak, [33]. The risk of Mpox spread during large sports events with inevitable mass gatherings, and recommended IPC measures were discussed in detail in our previous publication [34].
Prisons and jails are ‘potentially high-risk’ for mpox. Routine IPC measures are mandatory for prisoners and those working in prisons as well as visitors. Mpox should be considered as part of regular screening for newly admitted or transferred individuals. Effective communication is the key for discussion keeping in mind the necessity of avoiding stigmatization [35].
Advisory for international passengers
Centres for Disease Control and Prevention (CDC) raised the Mpox travel advisory to Level 2, i.e., practicing enhanced precautions applicable when traveling to both endemic and non-endemic countries experiencing Mpox outbreaks [19]. The list of countries to which the travel health notice is applied undergoes regular updates according to the epidemiologic situation.
Public health administrators must work with travel operators and their public health counterparts to contact passengers and others who may have had close contact with an infectious individual while traveling. Health promotion and risk management materials are to be obtainable at points of entry, including information on how to identify signs and symptoms consistent with Mpox, the preventive actions suggested for curtailing its dissemination, and how to pursue medical supervision at the site of arrival when required [20].
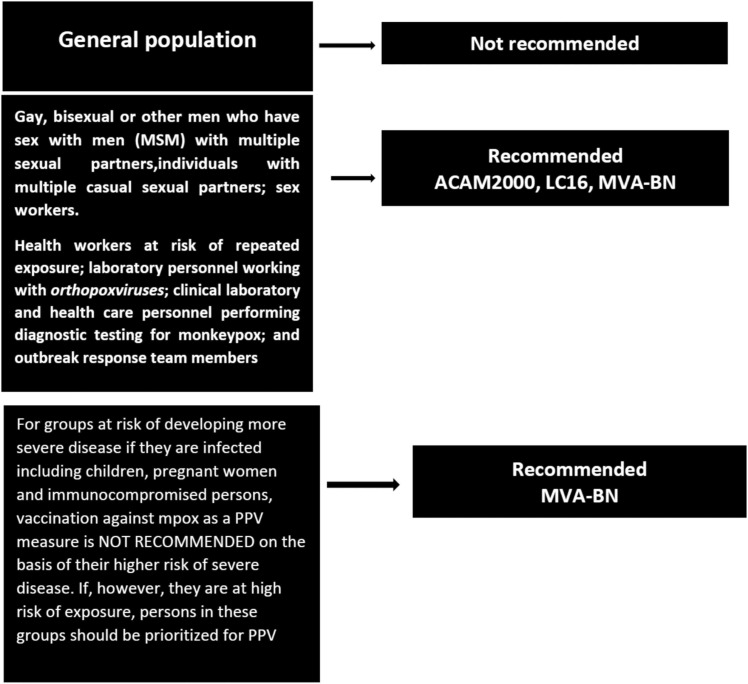
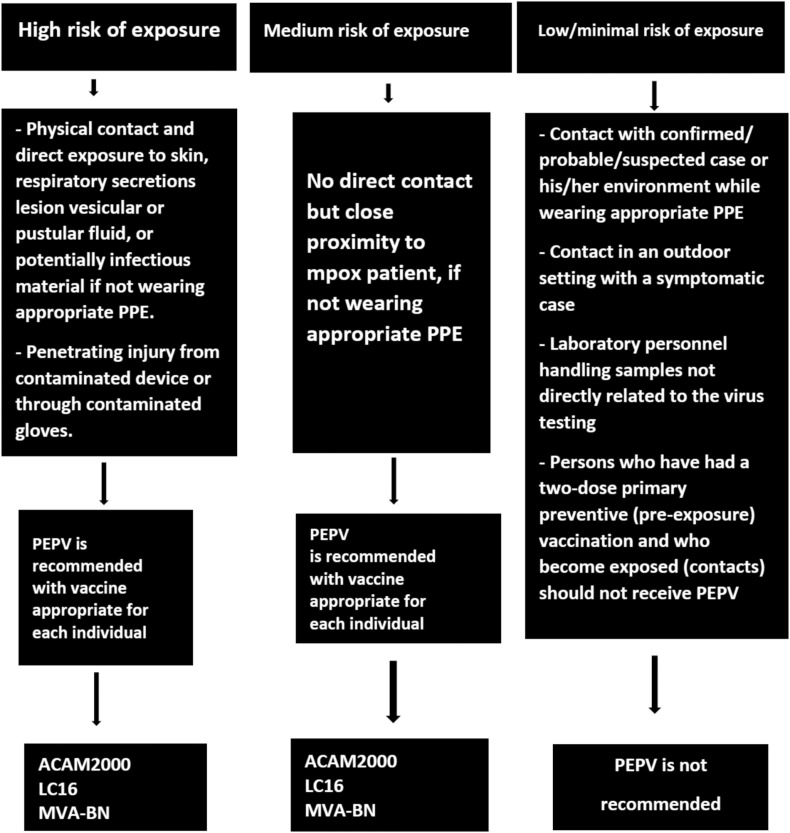
Immunoprophylaxis
National authorities should assess the approved Mpox/smallpox vaccines in response to the Mpox outbreaks. For post-exposure preventive vaccination (PEPV), the vaccine is provided within four days from the date of exposure for the best chance of preventing the onset of the disease. If given between 4 and 14 days after the date of exposure, symptoms may be reduced, but the disease may not be averted [29]. Persons exposed to Mpox virus who have not obtained the smallpox vaccine within the last three years should consider getting vaccinated. Vaccine options that can be considered for approved or off-label use for primary preventive (pre-exposure) vaccination (PPV) ( Fig. 3 ) or PEPV ( Fig. 4 ) of Mpox include MVA-BN, LC16, or ACAM2000 [36]. Because many facets of these vaccines are still under investigation, the indication for use and the risk of adverse reactions should be determined after a careful need-risk-benefit analysis [29]. For groups at risk of developing more severe disease if they are infected with Mpox virus, including children, pregnant women, and immunocompromised persons, vaccination against Mpox as a PPV measure is not recommended on the basis of their higher risk of severe disease. If, however, they are at high risk of exposure, persons in these groups should be prioritized for PPV. Other prioritization factors for getting the Mpox vaccine have been set in different countries according to the epidemiology of the groups at the highest risk of infection. It is worth mentioning that there are supply constraints in some countries at this time, owing to several issues including regulatory, policy, price, product preference, and supply availability.
Fig. 3.
Primary Preventive Vaccination (PPV) for Mpox [29].
Fig. 4.
Post-Exposure Preventive Vaccination (PEPV) of Mpox [29].
Discussion
Disease Global Burden
In the light of the reviewed articles, official reports, research papers and interim recommendations from different organizations worldwide responding to what has been declared as ‘PHEIC’ it is clear that Mpox is neither trivial, nor merely an insignificant skin and respiratory disease. So far, during the global outbreak, 111 death, have been reported to the WHO from 110 countries/areas/territories [10]. It is to be emphasized, the actual incidence of death is almost undoubtedly higher. In low- and middle-income parts of the globe, including Africa, all deaths might not be captured due to limited resources for testing and surveillance. Death rates could still escalate, especially if the virus spreads more extensively among high-risk individuals.
An important issue that compromising the quality of life is that, Mpox disease for the mostly affected; MSM, it is extremely painful [37]. The pain arises from the distinctive fluid-filled lesions that the disease causes. It has been very common to see Mpox cases hospitalized for pain management, even more than those hospitalized for deadly complications [38]. In the existing outbreak, a higher proportion of lesions are appearing on mucosal tissues and are therefore more difficult to identify than skin lesions [21]. Although they aren’t fundamentally more severe, mucosal lesions worsen sensitive tissue, leading to massive pain interfere with swallowing, eating, or drinking when in the throat, or urinating and defecating when in the genital and rectal areas. Complications of the disease have been reported that add to its seriousness, e.g., abscesses (perianal, groin, tonsillar), eye involvement, rectal perforation, secondary bacterial infection of penis, superimposed bacterial lower respiratory tract infection, and disseminated lesions in the context of immunocompromised patients and rectal perforation [36]. Finally, post- illness effects of a severe case of mpox after an infection clears, which can be quite serious, have not yet been identified. Post-viral syndrome is a wide range of complex conditions involving physical, cognitive, emotional and neurological difficulties that vary in severity over time and may continue for weeks, months or longer [38].
Collaborative interventions to fight Mpox
The primary step in fighting the Mpox outbreak is to meticulously assess the risks associated with the spread of infection. Risks should be evaluated for every sector directly, indirectly, or potentially related to Mpox since it is one of the cornerstones of IPC. Mpox risk assessment must also consider prevailing community cultures that impact disease transmission, e.g., degree of sexual liberation, chemsex culture [39], and rodent home-raising.
MSM and LGBT
Hitherto, Mpox has predominantly affected the LGBT community, especially young adult MSM, with the co-occurrence of associated sexually transmitted infections, including HIV, hepatitis, gonorrhea, chlamydia, syphilis, pubic lice or crabs, and others [40]. It is assessed that the likelihood of further disseminating Mpox virus among such communities is high. With the continuation of the sexual activities and the events carried out for MSM and LGBT and with the ease of movement and travel across the globe, the probability of further spreading the disease is anticipated. We recommend to postpone or cancel sex parties until the Mpox outbreak ends due to the following reasons: 1) The relation between these events and the emergence of Mpox has been well documented. We should not forget that the two-sex rave parties in Spain and Belgium likely led to the outbreak of Mpox in Europe. 2) It is not expected in the atmosphere of such events, particularly chemsex parties [39], to strictly adhere to guidelines of safe sex practice, particularly in light of the fact that the use of a condom is not enough to avoid Mpox transmission [14], and 3) so far, data about effective treatment or vaccine prophylaxis are limited. Just like during the pandemic of COVID-19, it is likely to stop such gatherings and events until the epidemic retreats.
Groups that should never be ignored
It is well established that elderly and immunocompromised individuals are in significant danger of acquiring the disease. Both categories currently exist and are on an ongoing rise. Recent reports from the USA and most comparable countries reveal an increased life expectancy, leading to a higher percentage of the elderly population [41]. Moreover, the number of immunocompromised individuals is on the continuous upsurge. Examples are people living with HIV who are not on treatment, patients with severe underlying diseases, e.g., cancer, autoimmune disorders, and others receiving advanced treatment interventions that, despite being lifesaving, are immunity-compromising. When considering the catastrophic outcome of the infection in children and pregnant women, there is the potential for increased health impact with a broader spread in all these vulnerable groups.
The front liners
HCWs are the backbone of effective healthcare services provided to Mpox patients and are one of the vulnerable groups to catch the infection. In one study of 1130 HCWs, 50% were more concerned about Mpox than COVID-19, especially in relation to the possible progression into a new pandemic [42]. During the Mpox outbreak, they must be provided with all relevant information and training, as well as vaccines, to protect themselves and continue to provide critical care, comfort, and compassion to patients.
Mpox vaccine challenges
Some countries may maintain strategic reserves of the older smallpox vaccines; first generation, from the Smallpox Eradication Programme (SEP), which ended in 1980. HCWs and high-risk close contacts of Mpox virus may be offered this vaccine as PPV or PEPV, a procedure that is not recommended as it does not meet acceptable standards. When vaccination is the only option, complete information about the risk/benefits, and probable side effects should be fully provided to vaccinees. The availability of the new second- and third-generation vaccines for smallpox, which are safer and some of which may be helpful for Mpox, are providing more convenient alternatives, e.g., MVA-BN [36]. Unfortunately, the supply of newer vaccines is limited, and access strategies are under discussion. It is to be emphasized that all decisions around immunization with smallpox or Mpox vaccines should be made on a case-by-case basis, within a framework of conjoint research and randomized clinical trial protocols with standardized data collection tools for clinical and outcome data.
So far, the 2022 Mpox outbreak is a new paradigm in human-poxvirus interaction since the eradication of smallpox in 1980. This infectious disease is the latest to be added to the list of public health emergencies of international concern. There are demonstrated key needs to refocus on the understanding of Mpox as a significant member of orthopoxviruses and to develop specific interventions to prevent and manage.
Areas for future research
Following the current outbreak, epidemiological and clinical reports raise many questions that await answers and call for further research. Most of the previous research on Mpox has focused predominantly on clade I, leaving many aspects related to clade II (the cause of the current outbreak) less well understood. Regarding the mode of transmission, which is the cornerstone of outbreak spread and hence its control, many inquiries still exist as we discussed in a previous work [43]. There is still no clear information on specific routes of animal-to-human transmission as well as the range of potential reservoir hosts. The potential for a peri-domestic cycle of Mpox and the implications of such a cycle are also unknown. It remains unclear what proportion of cases in this outbreak present atypically or are asymptomatic, and to what extent these cases contribute to disease transmission. The transmission efficiency in heterosexual relationships or between women, women who have sex with women and non- binary women [44] continues to call for further studies. In the current outbreak, there have been multiple reports of the initial misdiagnosis or underdiagnosis of patients who were later confirmed to have Mpox due to many causes. So continuous updates of case definitions are mandatory, and the development of better diagnostics should be prioritized. Finally, antivirals and vaccines designed for the treatment and prevention Mpox should be developed within a framework of collaborative research, including randomized controlled trials.
Conclusions and recommendations
All factors that help further the spread of Mpox disease do exist. Unless appropriate measures for combating the virus are implemented, it will not be possible to go out of the dark tunnel. In all countries, all those having a relationship with health services, whether administratively or technically, social sector partners, academicians, and research partners have to respond quickly to control the further spread of the multi-country outbreak of Mpox. A rapid strategic preventive movement must be brought about before the virus can embed itself as a human pathogen with dynamic person-to-person transmission in any previously affected or newly affected areas.
Declaration of Competing Interest
None.
References
- 1.World Health Organization [WHO]. Multi-country monkeypox outbreak in non-endemic countries. Available at: 〈https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON385〉. [Accessed 30th August 2022].
- 2.World Health Organization [WHO]. Clinical management and infection prevention and control for monkeypox: Interim rapid response guidance. Updated 10th June. Available at: 〈https://www.who.int/publications/i/item/WHO-MPOX-Clinical-and-IPC-2022.1〉. [Accessed 6th August 2022].
- 3.Amer F.A., Hammad N.M., Wegdan A.A., ElBadawy N.E., Pagliano P., Rodríguez-Morales A.J. Growing shreds of evidence for monkeypox to be a sexually transmitted infection. Infez Med. 2022;30(3):323–327. doi: 10.53854/liim-3003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Antinori A., Mazzotta V., Vita S., Carletti F., Tacconi D., Lapini L.E., et al. Epidemiological, clinical and virological characteristics of four cases of monkeypox support transmission through sexual contact, Italy, May 2022. Eur Surveill. 2022;27(22) doi: 10.2807/1560-7917.ES.2022.27.22.2200421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.European Centre for Disease Prevention and Control [ECDC]. European Centre for Disease Prevention and Control Factsheet for health professionals on monkeypox. Updated 21 September 2022. Available at (〈https://www.ecdc.europa.eu/en/all-topics-z/monkeypox/factsheet-health-professionals〉). [Accessed 6th October 2022].
- 6.Bragazzi N.L., Woldegerima W.A., Iyaniwura S.A., Han Q., Wang X., Shausan A., et al. Knowing the unknown: the underestimation of monkeypox cases. Insights and implications from an integrative review of the literature. Front Microbiol. 2022;13 doi: 10.3389/fmicb.2022.1011049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.European Centre for Disease Prevention and Control [ECDC]. Monkeypox multi-country outbreak rapid risk assessment; 2022. Available at: 〈https://www.ecdc.europa.eu/sites/default/files/documents/Monkeypox-multi-country-outbreak.pdf〉. [Accessed 6th October 2022].
- 8.Adler H., Gould S., Hine P., Snell L.B., Wong W., Houlihan C.F., et al. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis. 2022;22(8):1153–1162. doi: 10.1016/S1473-3099(22)00228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chittick G., Morrison M., Brundage T., Nichols W.G. Short-term clinical safety profile of brincidofovir: a favorable benefit–risk proposition in the treatment of smallpox. Antivir Res. 2017;143:269–277. doi: 10.1016/j.antiviral.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization [WHO]. Multi-country outbreak of Mpox, External Situation report # 17–2 March 2023. Available at: 〈https://www.who.int/publications/m/item/multi-country-outbreak-of-mpox--external-situation-report---17---2-march-2023〉. [Accessed 22 March 2023].
- 11.World Health Organization [WHO]. WHO Director-General declares the ongoing monkeypox outbreak a Public Health Emergency of International Concern. Available at: 〈https://www.who.int/europe/news/item/23-07-2022-who-director-general-declares-the-ongoing-monkeypox-outbreak-a-public-health-event-of-international-concern〉. [Accessed 4th October 2022].
- 12.Centre for Disease Prevention and Control [CDC]. Monkeypox, pets in the home updated; 2022 Available at: 〈https://www.cdc.gov/poxvirus/monkeypox/prevention/pets-in-homes.html〉. [Assecced 7th February 2023].
- 13.European Centre for Disease Prevention and Control [ECDC]. Navigating monkeypox: considerations for gay and bisexual men and other men who have sex with men; 2022. Available at: 〈https://www.ecdc.europa.eu/sites/default/files/documents/Navigating-monkeypox-considerations-for-gay-bisexual-and-MSM.pdf〉. [Accessed 6th October].
- 14.Centre for Disease Prevention and Control [CDC]. Safer sex, social gatherings, and monkeypox. Updated December 16, 2022. Available at: 〈https://www.cdc.gov/poxvirus/monkeypox/prevention/sexual-health.html〉. [Accessed 10 February 2023].
- 15.Gould S., Atkinson B., Onianwa O., Spencer A., Furneaux J., Grieves J., et al. NHS England airborne high consequence infectious diseases network. Air and surface sampling for monkeypox virus in a UK hospital: an observational study. Lancet Microbe. 2022;(22):S2666–S5247. doi: 10.1016/S2666-5247(22)00257-9.00257-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zachary K.C., Shenoy E.S. Monkeypox transmission following exposure in healthcare facilities in nonendemic settings: low risk but limited literature. Infect Control Hosp Epidemiol. 2022;43(7):920–924. doi: 10.1017/ice.2022.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vaughan A., Aarons E., Astbury J., Brooks T., Chand M., Flegg P., et al. Human-to-human transmission of monkeypox virus, United Kingdom, October 2018. Emerg Infect Dis. 2020;26(4):782–785. doi: 10.3201/eid2604.191164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization (WHO). Laboratory biosafety manual, 4th edition. Geneva. Available at: 〈https://www.who.int/publications/i/item/9789240011311〉. [Accessed 30 July 2022].
- 19.Mpox contact tracing classification and vaccination matrix: version 17 (23 January 2023) 〈https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1130558/monkeypox-contact-tracing-classification-and-vaccination-matrix-version-17-23-january-2023.pdf〉.
- 20.Centre of Disease Prevention and Control [CDC]. Monkeypox in multiple countries: travel notice. Available at: 〈https://wwwnc.cdc.gov/travel/diseases/monkeypox〉. [Accessed 5th Februry 2023].
- 21.Di Giulio D.B., Eckburg P.B. Human monkeypox: an emerging zoonosis. Lancet Infect Dis. 2004;4(1):15–25. doi: 10.2217/17460913.2.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seang S., Burrel S., Todesco E., Leducq V., Monsel G., Le Pluart D., et al. Evidence of human-to-dog transmission of monkeypox virus. Lancet. 2022 doi: 10.1016/S0140-6736(22)01487-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shepherd W., Beard P.M., Brookes S.M., et al. The risk of reverse zoonotic transmission to pet animals during the current global monkeypox outbreak, United Kingdom, June to mid-September 2022. Eur Surveill: Bull Eur sur Les Mal Transm = Eur Commun Dis Bull. 2022;27(39) doi: 10.2807/1560-7917.es.2022.27.39.2200758. [PMID: 36177868; PMCID: PMC9524050] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Insurance Information Institute. Available at: 〈https://www.iii.org/fact-statistic/facts-statistics-pet-ownership-and-insurance〉. [Accessed 30 July 2022].
- 25.Neville V., Mounty J., Benato L., Hunter K., Mendl M., Paul E.S. Pet rat welfare in the United Kingdom: the good, the bad and the ugly. Vet Rec. 2021;189(6) doi: 10.1002/vetr.559. [DOI] [PubMed] [Google Scholar]
- 26.Public Health Agency of Canada [PHAC]. Interim guidance on infection prevention and control for suspect, probable or confirmed monkeypox within healthcare settings. Available at: 〈https://www.canada.ca/en/public-health/services/diseases/monkeypox/health-professionals/interim-guidance-infection-prevention-control-healthcare-settings.html〉. [Accessed 8th July 2022].
- 27.Vancouvre Costal Health. Point-of-care risk assessment (PCRA). Available at: 〈http://ipac.vch.ca/Documents/Routine%20Practices/PCRA%20Algorithm.pdf〉. [Accessed 5th August 2022].
- 28.Centre for Disease Prevention and Control [CDC]. Disinfecting home and other non-healthcare settings. Available at: 〈https://www.cdc.gov/poxvirus/monkeypox/if-sick/home-disinfection.html〉. [Accessed 5th September2022].
- 29.World Health Organization [WHO]. Vaccines and immunization for monkeypox. Interim guidance; 2022. Available at: 〈https://www.who.int/publications/i/item/WHO-MPX-Immunization〉. [Accessed 7 Februaury 2023].
- 30.World Health Organization [WHO]. Guidance on regulations for the transport of infectious substances 2019–2020. Geneva: WHO. Available at: 〈https://www.who.int/publications/i/item/WHO-WHE-CPI-2019.20〉. [Accessed 5th August 2022].
- 31.Centre of Disease Prevention and Control [CDC]. Monkeypox: laboratory procedures and biosafety guideline. Available at: 〈https://www.cdc.gov/poxvirus/monkeypox/lab-personnel/lab-procedures.html〉. [Accessed 5th August 2022].
- 32.Amer F. Hospital infection control; Part I. 3rd ed. LAP LAMBERT Academic Publishing; 2017. pp. 146–170. [Isolation] [Google Scholar]
- 33.Smoliga J.M. Mpox and monkeypox virus: special considerations for athletes in contact sports. Sports Med. 2023 doi: 10.1007/s40279-023-01812-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sah R., Alshahrani N.Z., Shah P., Mohanty A., Rouniyar R., Shah S., et al. FIFA World Cup 2022 in Qatar: mitigating the risk of imported infections amid the COVID-19 pandemic, monkeypox outbreak and other emerging diseases. Travel Med Infect Dis. 2022;50 doi: 10.1016/j.tmaid.2022.102450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cocco N., Sebastiani T., Giuliani R., Cereda D., D'Arminio Monforte A., Tavoschi L., et al. Monkeypox epidemic in prisons: how to prevent it. Lancet. 2022;22 doi: 10.1016/j.lanepe.2022.100530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pittman P.R., Hahn M., Lee H.C.S., Koca C., Samy N., Schmidt D., et al. Phase 3 efficacy trial of modified vaccinia Ankara as a vaccine against smallpox. N Engl J Med. 2019;381(20):1897–1908. doi: 10.1056/NEJMoa1817307. [DOI] [PubMed] [Google Scholar]
- 37.Kozlov Y.M. How deadly is monkeypox? What scientists know. Nature. 2022;609:663. doi: 10.1038/d41586-022-02931-1. [DOI] [PubMed] [Google Scholar]
- 38.Patel A., Bilinska J., Tam J.C.H., Fontoura D.D.S., Mason C.Y., Anna Daunt A., et al. Clinical features and novel presentations of human monkeypox in a central London centre during the 2022 outbreak: descriptive case series. BMJ. 2022;378 doi: 10.1136/bmj-2022-072410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Santoro P., Rodríguez R., Morales P., Morano A., Morán M. One “chemsex” or many? Types of chemsex sessions among gay and other men who have sex with men in Madrid, Spain: findings from a qualitative study. Int J Drug Policy. 2020;82 doi: 10.1016/j.drugpo.2020.102790. [102790. 33, 34] [102790. 33, 34] [DOI] [PubMed] [Google Scholar]
- 40.Program for LGBTQ Health Home About Health Education. Key health concerns for MSM (Men Who have Sex with Men). Available at: 〈https://www.vumc.org/lgbtq/key-health-concerns-msm-men-who-have-sex-men〉. [Accessed 7th August 2022].
- 41.Jared Ortaliza G.R., Satheeskumar V., Amin K.. Health & wellbeing. How does U.S. life expectancy compare to other countries? Available at: 〈https://www.healthsystemtracker.org/chart-collection/u-s-life-expectancycomparecountries/#Life%20expectancy%20at%20birth%20in%20years,%201980-2020%C2%A0〉. [Accessed 4th August 2022].
- 42.Ajman F., Alenezi S., Alhasan K., Saddik B., Alhaboob A., Altawil E.S., et al. Healthcare workers' worries and monkeypox vaccine advocacy during the first month of the WHO monkeypox alert: cross-sectional survey in Saudi Arabia. Vaccines. 2022;10(9):1408. doi: 10.3390/vaccines10091408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sah R., Reda A., Abdelaal A., Mohanty A., Siddiq A., Alshahrani N.Z., et al. A potential monkeypox pandemic: are we making the same mistakes as COVID-19? New Microbes New Infect. 2022;49–50 doi: 10.1016/j.nmni.2022.101030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rodriguez-Morales A.J., Amer F. Monkeypox virus infection in women and non-binary people: uncommon or neglected? Lancet. 2022;400(10367):1903–1905. doi: 10.1016/S0140-6736(22)02396-0. [DOI] [PMC free article] [PubMed] [Google Scholar]