Abstract
Background
A sedentary lifestyle and stress are major risk factors for cardiovascular disease (CVD). Since yoga involves exercise and is thought to help in stress reduction it may be an effective strategy in the primary prevention of CVD.
Objectives
To determine the effect of any type of yoga on the primary prevention of CVD.
Search methods
We searched the following electronic databases: the Cochrane Central Register of Controlled Trials (CENTRAL) (2013, Issue 11) in The Cochrane Library; MEDLINE (Ovid) (1946 to November Week 3 2013); EMBASE Classic + EMBASE (Ovid) (1947 to 2013 Week 48); Web of Science (Thomson Reuters) (1970 to 4 December 2013); Database of Abstracts of Reviews of Effects (DARE), Health Technology Assessment Database and Health Economics Evaluations Database (Issue 4 of 4, 2013) in The Cochrane Library. We also searched a number of Asian databases and the Allied and Complementary Medicine Database (AMED) (inception to December 2012). We searched trial registers and reference lists of reviews and articles, and approached experts in the field. We applied no language restrictions.
Selection criteria
Randomised controlled trials lasting at least three months involving healthy adults or those at high risk of CVD. Trials examined any type of yoga and the comparison group was no intervention or minimal intervention. Outcomes of interest were clinical CVD events and major CVD risk factors. We did not include any trials that involved multifactorial lifestyle interventions or weight loss.
Data collection and analysis
Two authors independently selected trials for inclusion, extracted data and assessed the risk of bias.
Main results
We identified 11 trials (800 participants) and two ongoing studies. Style and duration of yoga differed between trials. Half of the participants recruited to the studies were at high risk of CVD. Most of studies were at risk of performance bias, with inadequate details reported in many of them to judge the risk of selection bias.
No study reported cardiovascular mortality, all‐cause mortality or non‐fatal events, and most studies were small and short‐term. There was substantial heterogeneity between studies making it impossible to combine studies statistically for systolic blood pressure and total cholesterol. Yoga was found to produce reductions in diastolic blood pressure (mean difference (MD) ‐2.90 mmHg, 95% confidence interval (CI) ‐4.52 to ‐1.28), which was stable on sensitivity analysis, triglycerides (MD ‐0.27 mmol/l, 95% CI ‐0.44 to ‐0.11) and high‐density lipoprotein (HDL) cholesterol (MD 0.08 mmol/l, 95% CI 0.02 to 0.14). However, the contributing studies were small, short‐term and at unclear or high risk of bias. There was no clear evidence of a difference between groups for low‐density lipoprotein (LDL) cholesterol (MD ‐0.09 mmol/l, 95% CI ‐0.48 to 0.30), although there was moderate statistical heterogeneity. Adverse events, occurrence of type 2 diabetes and costs were not reported in any of the included studies. Quality of life was measured in three trials but the results were inconclusive.
Authors' conclusions
The limited evidence comes from small, short‐term, low‐quality studies. There is some evidence that yoga has favourable effects on diastolic blood pressure, HDL cholesterol and triglycerides, and uncertain effects on LDL cholesterol. These results should be considered as exploratory and interpreted with caution.
Plain language summary
Yoga to prevent cardiovascular disease
Background
Cardiovascular disease (CVD) is a global health burden. Nevertheless, it is thought that the risk of CVD can be lowered by changing a number of risk factors, such as by increasing physical activity and using relaxation to reduce stress, both of which are components of yoga. This review assessed the effectiveness of any type of yoga in healthy adults and those at high risk of CVD.
Study Characteristics
We searched scientific databases for randomised controlled trials (clinical trials where people are allocated at random to one of two or more treatments) looking at the effects of yoga on adults at high risk of developing CVD. We did not included people who had already had CVD (e.g. heart attacks and strokes). The evidence is current to December 2013.
Key Results
We found 11 trials (800 participants), none of them were large enough or of long enough duration to examine the effects of yoga on decreasing death or non‐fatal endpoints.There were variations in the style and duration of yoga and the follow‐up of the interventions ranged from three to eight months.The results showed that yoga has favourable effects on diastolic blood pressure, high‐density lipoprotein (HDL) cholesterol and triglycerides (a blood lipid), and uncertain effects on low‐density lipoprotein (LDL) cholesterol. None of the included trials reported adverse events, the occurrence of type 2 diabetes or costs. Longer‐term, high‐quality trials are needed in order to determine the effectiveness of yoga for CVD prevention.
Quality of the Evidence
These results should be considered as exploratory and interpreted with caution. This is because the included studies were of short duration, small and at risk of bias (where there was a risk of arriving at the wrong conclusions because of favouritism by the participants or researchers).
Background
Description of the condition
The number one cause of death and disability worldwide is cardiovascular disease (CVD) (WHO 2011). Around 29.6% of total global deaths can be attributed to CVD (WHO 2003). Indeed, in the United Kingdom 88,000 deaths per year are attributable to coronary heart disease and 43,000 deaths are caused by stroke (BHF 2012). In the United States, 35% of total deaths in 2010 were accounted for by CVD compared to 45% in Germany, 30% in Costa Rica, 31% in Denmark, 15% in Ethiopia, 48% in Greece, 32% in Japan, 26% in Mexico and 38% in China (WHO 2011a). It is estimated that by 2030 CVDs will account for almost 23.6 million deaths (WHO 2011).
There are many risk factors that contribute to the development of CVD. Many of these are related to lifestyle choices, such as physical inactivity, smoking, alcohol use and an unhealthy diet (WHO 2011). Whilst clinical treatments are effective in preventing and treating CVD, other strategies involving a healthy lifestyle and stress management have also been shown to be beneficial (Frishman 2005). One such strategy that involves both stress management and exercise is yoga.
As yoga has become increasingly popular as a form of exercise it may be an important intervention for the primary and secondary prevention of CVDs, since high levels of physical activity play a major role in preventing obesity and CVDs (Mendelson 2008). Indeed, there are a number of publications that show yoga to be beneficial for hypertension (Murugesan 2000), dyslipidaemia and atherosclerosis (Singh 2004). The systematic review by Innes et al also demonstrated that yoga improved metabolic risk factors such as blood pressure and lipids (Innes 2005). Furthermore, the psychological benefits of yoga have been established (Saper 2004), with yoga being used in stress reduction, a determinant for CVD (WHO 2011).
Description of the intervention
Yoga is defined in the Oxford Handbook of Complementary Medicine as an "ancient Indian practice involving postural exercises, breathing control and meditation" (Ernst 2008). It was founded in India over 5000 years ago and is believed to give the practitioner a union between their mind, body and spirit (Kappmeier 2006). It has its foundations in three basic components: Asana (posture), Pranayama (breathing) and Dhyana (mediation and devotion), all of which are integrated with each other (Riley 2004). There are six main branches of yoga: Bhakti yoga, Hatha yoga, Jnana yoga, Karma yoga, Mantra yoga and Raja yoga (Feuerstein 2011). Jnana yoga is the path of knowledge in which enlightenment is developed through the philosophical investigation of traditional yogic texts and scriptures (Carrico 2012). In Jnana yoga the practitioner contemplates life using rational thought which, it is believed, leads the mind towards higher levels of consciousness (Simpkins 2003). Karma yoga, however, teaches practitioners how to maintain their focus in everyday life (Simpkins 2003), by analysing their actions and thoughts in order to learn about different qualities of thinking and behaving. In doing this, the practitioner will learn how to channel their actions in the correct way and ultimately achieve an enlightened way of living (Simpkins 2003). Mantra yoga influences the human consciousness through sound and vibration (Simpkins 2003). It is thought that after many repetitions and practice the mantra will begin to recite itself within the practitioner's mind, leading them to enlightenment. Bhakti yoga is known as the yoga of devotion (Koay 2009). It involves "cultivating selfless love, pure giving and long devotion to God", which is expressed through chants, prayers and also services to humanity (Koay 2009). In Raja yoga, on the other hand, all three basic yoga components are used so that the practitioner can seek enlightenment through the mind. In this type of yoga enlightenment is sought through using meditation and techniques of attention, concentration and contemplation (Simpkins 2003). However, the most practised style of yoga in the West is Hatha (Hewitt 2001). Hatha yoga seeks enlightenment not through the mind, as in Raja yoga, but through the body. It can be practised in many styles, such as Bikram, Integral, Kundalini, Ashtanga and Iyengar, all of which have unique characteristics (Cook 2014).
The physical and psychological benefits of yoga have been acknowledged (Saper 2004). Evidence suggests that yoga can be applied to manage and reduce the symptoms of a number of conditions. For instance, yoga has been found to relieve perceived pain in those with rheumatoid arthritis (Bosch 2009) and chronic back pain (Groessl 2008), as well as aiding in the management of those with urological disorders (Ripoll 2002). Yoga has also been found to be beneficial for depression, stress and insomnia (Granath 2006; Khalsa 2004; Lavey 2005; Woolery 2004).
How the intervention might work
High levels of exercise have been found to play a major role in preventing obesity, diabetes and CVD (Mendelson 2008; Mittal 2008). Therefore, as some forms of yoga, such as Hatha yoga, are considered a form of exercise it may help in CVD prevention. Evidence suggests that regular exercise can decrease the risk of dying from CVD (USHHS 1996), and it has been found to be beneficial when included in primary and secondary prevention strategies (Lavie 2009). This is because physical activity has favourable effects not only on CVD risk factors but also on CVD symptoms, a person's functional capacity, physiology and quality of life (ACSM 2010; AHA 2011). Furthermore, yoga is a moderately safe, gentle choice for promoting general health and emotional well‐being, especially for those whose lifestyle is sedentary (Lau 2012).
However, the benefits and degree of improvement in physical health from yogic practices will vary according to how the individual practises yoga. For instance, if the individual practises all poses intensely and continuously then cardiorespiratory fitness will improve, whereas if the individual only practises a single pose then improvements may be made in muscular strength, flexibility and posture (Lau 2012). Furthermore, Hagins et al state that when the metabolic cost is averaged out across a whole session of Hatha yoga, it only represents a low level of exercise. This does not meet the recommendations for levels of physical activity developed for improving or maintaining general health and CVD fitness (Hagins 2007). However, studies suggests that regular yogic training leads to significant improvements in cardiovascular endurance and anaerobic power and therefore is useful in improving exercise tolerance (Bera 1993; Madanmohan 2004; Muralidhara 1982). As such, yoga can be used in patients who are sedentary to improve exercise tolerance gradually and, with regular practice, strengthen the cardiovascular system.
As well as being beneficial in terms of exercise, yoga may also help to reduce stress (AHA 2011), a determinant of CVD (WHO 2011). It does this by creating a physiological sequence of events in the body as a result of changes in posture, breathing or both, which reduces the stress response (Woodyard 2011). Proposed physiological mechanisms include reducing the reactivity of the sympathetic nervous system (Innes 2007), counteracting the activity of the aroused autonomic nervous system (ANS), reversing it back to a relaxed state, or both (Levine 2000; Michalsen 2005).
Why it is important to do this review
Few randomised controlled trials have directly investigated the effectiveness of yoga for the primary prevention of CVD, even though yoga has the potential to help in CVD prevention. Furthermore, few systematic reviews examining the effectiveness of yoga are available. Those that do exist mainly focus on secondary prevention (Innes 2005; Lau 2012). Therefore, a comprehensive systematic review is needed, which thoroughly examines the most up to date evidence to determine whether yoga is effective in preventing CVD in those who are healthy or who have CVD risk factors.
Objectives
To determine the effect of any type of yoga on the primary prevention of CVD.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials.
Types of participants
Healthy adults (18 years old or over) of all ages from the worldwide general population and those at moderate to high risk of CVD (Perk 2012). As the review focused on the primary prevention of CVD we excluded those who had experienced a previous myocardial infarction, stroke, revascularisation procedure (coronary artery bypass grafting (CABG) or percutaneous transluminal coronary angioplasty (PTCA)), and those with angina or angiographically defined coronary heart disease.
Types of interventions
Trials investigating any type of yoga. The definition of yoga was that provided by Ernst 2008, in which yoga is seen as involving three components: postural exercises, breathing control and meditation.
Multifactorial intervention studies (including dietary or other additional interventions) were not included in this review in order to avoid confounding. We also focused on follow‐up periods of three months or more. We considered follow‐up to be the time elapsed since the start of the intervention and therefore we excluded any trials with an intervention period of less than 12 weeks. We also only considered trials where the comparison group was either given no intervention or minimal intervention (for example, leaflets with no person to person intervention or reinforcement).
Types of outcome measures
Primary outcomes
Cardiovascular mortality
All‐cause mortality
Non‐fatal endpoints such as myocardial infarction, CABG, PTCA, angina or angiographically defined coronary heart disease, stroke, carotid endarterectomy or peripheral arterial disease (PAD)
Secondary outcomes
Changes in blood pressure (systolic and diastolic blood pressure) and blood lipids (total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides)
Occurrence of type 2 diabetes as a major CVD risk factor
Quality of life
Adverse effects (as defined by the authors of the included trials)
Costs
Search methods for identification of studies
Electronic searches
We searched the following electronic databases:
Cochrane Central Register of Controlled Trials (CENTRAL) (2013, Issue 11) in The Cochrane Library;
MEDLINE (Ovid) (1946 to November week 3 2013);
EMBASE Classic + EMBASE (Ovid) (1947 to 2013 Week 48);
Web of Science (Thomson Reuters, including the Social Sciences Citation Index (SSCI) and the Conference Proceedings Citation Index ‐ Science (CPCI‐S) (1970 to 4 December 2013);
Database of Abstracts of Reviews of Effects (DARE), Health Technology Assessment Database and Health Economics Evaluations Database (Issue 4 of 4, 2013) in The Cochrane Library;
AMED (Inception to 22 October 2012).
We used medical subject headings (MeSH) or equivalent and text word terms. We used the Cochrane sensitivity‐maximising randomised controlled trial (RCT) filter for MEDLINE (Lefebvre 2011), and used adaptations of it for EMBASE and Web of Science.
There were no language restrictions.
We tailored the searches to individual databases (Appendix 1).
Searching other resources
In addition, we checked reference lists of reviews and retrieved articles for additional studies.
We searched the metaRegister of controlled trials (mRCT) (www.controlled‐trials.com/mrct), Clinicaltrials.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (http://apps.who.int/trialsearch/) for ongoing trials (search date 5 November 2012). We also searched OpenGrey for grey literature (http://www.opengrey.eu/) and the following Asian databases: KoreaMed (www.koreamed.org), DBPIA (www.dbpia.co.kr/), Korean studies information service system (http://kiss.kstudy.com/index.asp), Oasis (http://oasis.kiom.re.kr) and China National Knowledge Infrastructure (CNKI) (www.cnki.net/) from their inception to 21 December 2012.
We performed citation searches on key articles and used Google Scholar to search for further studies. We contacted experts in the field for unpublished and ongoing trials and contacted authors where necessary for any additional information.
Data collection and analysis
Selection of studies
From the searches, two review authors (LH, JH, MD) independently reviewed the title and abstract of each paper. Following the initial screen, we obtained the full text of potentially relevant studies and two review authors (LH, MD) independently selected relevant studies using predetermined inclusion criteria. In all cases we resolved disagreements about study inclusion by consensus and consulted a third review author (KR) if disagreements persisted.
Data extraction and management
Two review authors (LH, MD) independently extracted data using a proforma. We contacted chief investigators to provide additional relevant information if necessary. We extracted details of the study design, participant characteristics, study setting, intervention and outcome data (including details of outcome assessment, adverse effects and methodological quality (randomisation, blinding and attrition)) from each included study. We resolved disagreements about extracted data by consensus with a third review author (KR) being consulted if disagreements persisted.
Assessment of risk of bias in included studies
Two review authors (LH, MD) assessed risk of bias independently by examining the random sequence generation and allocation concealment, description of drop‐outs and withdrawals (including analysis by intention‐to‐treat), blinding (participants, personnel and outcome assessment) and selective outcome reporting in each trial (Higgins 2011).
Measures of treatment effect
We processed data in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For continuous outcomes we compared net changes (i.e. intervention group minus control group differences) and calculated a mean difference (MD) and 95% CI for each study.
Assessment of heterogeneity
For each outcome we conducted tests of heterogeneity (using the Chi2 test of heterogeneity and the I2 statistic). Where there was no heterogeneity we performed a fixed‐effect meta‐analysis. If we detected substantial heterogeneity (I2 greater than 50%), we looked for possible explanations for this (for example, participants and intervention). If the heterogeneity could not be explained, we considered the following options: providing a narrative overview and not aggregating the studies at all or using a random‐effects model with appropriate cautious interpretation.
Subgroup analysis and investigation of heterogeneity
It was our intention to stratify results according to baseline risk, type of yoga, and time and duration of yoga, but there were not sufficient trials for us to perform these analyses.
Sensitivity analysis
We performed sensitivity analysis by excluding studies at high risk of bias (e.g. those with loss to follow‐up of more than 20% without intention‐to‐treat analysis). We intended to examine the effects of publication bias using funnel plots and tests of asymmetry (Egger 1997), but these could not be carried out due to the small number of trials included in the review.
Results
Description of studies
Results of the search
The electronic searches generated 2151 hits (1465 after de‐duplication). Screening of titles and abstracts identified 204 papers to go forward for formal inclusion and exclusion. Of these, 11 randomised controlled trials (16 papers) met the inclusion criteria. We also identified two ongoing trials. The study flow diagram is presented in Figure 1.
1.
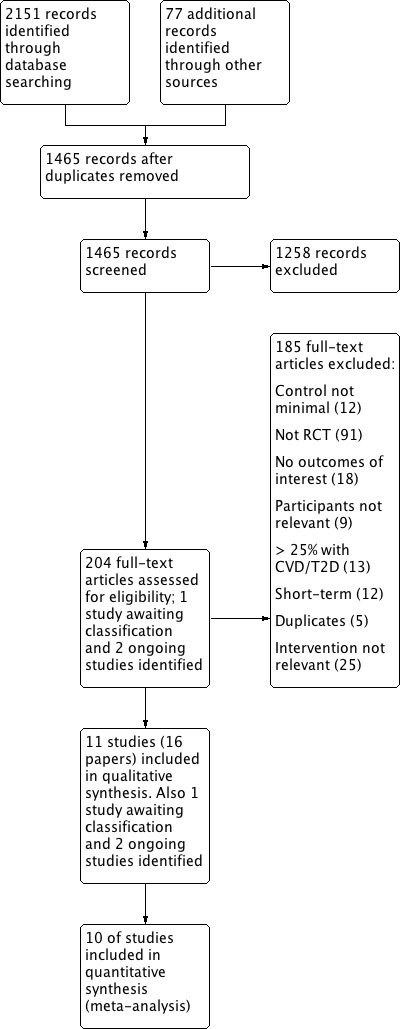
Study flow diagram.
Included studies
Details of studies included in the review are provided in the Characteristics of included studies table. Eleven trials (16 papers) with 800 participants randomised met the inclusion criteria. Four of the 11 trials recruited only female participants (Kim 2012; Kim 2013; Lee 2012; Monika 2012), and one trial recruited only male participants (Mahajan 1999). The health status of participants varied between studies; one study recruited females with metabolic syndrome (Kim 2013); one study recruited essential hypertensives (Latha 1991); one study recruited women with menstrual irregularities (Monika 2012); one study recruited healthy premenopausal women (Kim 2012); one study recruited males with hypertension and high cholesterol (Mahajan 1999); one study recruited HIV‐infected participants (Cade 2010); another study recruited obese postmenopausal women (Lee 2012); one study recruited non‐exercisers with a family history of type 2 diabetes and at least one cardio‐metabolic risk factor (Yang 2011), and the remaining three studies recruited healthy participants (394 participants) (Blumenthal 1989; Ray 2001; Wolever 2012).
Five of the trials were conducted in the USA (472 participants) (Blumenthal 1989; Cade 2010; Kim 2012; Wolever 2012; Yang 2011), four trials in India (271 participants) (Latha 1991; Mahajan 1999; Monika 2012; Ray 2001), one trial in South Korea (16 participants) (Lee 2012), and one trial did not provide country information (Kim 2013). The follow‐up periods also varied between studies. Three studies had a follow‐up period of three months (Kim 2013; Wolever 2012; Yang 2011); one study had a follow‐up period of 14 weeks (Mahajan 1999); two studies had a four‐month follow‐up (Blumenthal 1989; Lee 2012); two studies had a follow‐up period of five months (Cade 2010; Ray 2001); two studies had a six‐month follow‐up (Latha 1991; Monika 2012); and the remaining study had a follow‐up period of eight months (Kim 2012).
Duration and type of yoga varied between the 11 included studies. In six studies yoga was practised for one hour either for three days a week (Ray 2001), three days a week on non‐consecutive days for 16 weeks (Lee 2012), two times a week every two to three days for three months (Yang 2011), two to three times a week for 20 weeks (Cade 2010), for 64 sessions on Mondays and Wednesdays for eight months (Kim 2012), or for two or more days a week for four months (Blumenthal 1989). In one study yoga was practised twice weekly for six months (Latha 1991), whilst in another study yoga was practised for 35 to 40 minutes a day for five days a week in the morning for six months (Monika 2012). In another study yoga was practised for 12 weeks (Kim 2013). In the remaining two studies yoga was practised either for 12 hours in 12 weeks (Wolever 2012), or for four days at a residential camp with one hour of practice at home every day (Mahajan 1999). Five studies stated that yoga was taught by a qualified instructor (Kim 2012; Monika 2012; Ray 2001; Wolever 2012; Yang 2011), and four studies stated that participants were encouraged to practise at home (Cade 2010; Mahajan 1999; Wolever 2012; Yang 2011). Two studies used Ashtanga yoga (Cade 2010; Kim 2012), one study used Hatha yoga (Ray 2001), one study practised Vinyasa yoga (Yang 2011), and one study used Viniyoga (Wolever 2012). Five studies did not state which type of yoga they used (Blumenthal 1989; Kim 2013; Latha 1991; Lee 2012; Mahajan 1999). In the remaining study (Monika 2012), the intervention involved yoga Nidra. This differs from the types of yoga performed in the other included studies as the focus was not on yoga as a whole but on yoga meditation whilst in a particular pose. Yoga Nidra was performed whilst in the Shavasana pose and involved an awareness of breath and meditation practices.
One study is awaiting classification because clarification was needed about the control group. We contacted the authors for this information. Details of this study are provided in the Characteristics of studies awaiting classification table. This trial examined 12 weeks of yoga therapy in patients with essential hypertension (Punita 2011). We identified two ongoing trials looking at yoga. Details for these trials are given in the Characteristics of ongoing studies table. The first trial examines the effects of yoga in male and female office and manual workers in Sweden (NCT01305096). The outcomes measured include blood pressure and the anticipated start date was March 2011. The second trial examines the effect of yoga in patients with metabolic syndrome with outcome measures of blood pressure, quality of life, stress and insulin sensitivity. No anticipated end date was provided for this study (Cohen 2008).
Excluded studies
Details and reasons for exclusion of the studies that most closely missed the inclusion criteria are given in the Characteristics of excluded studies table. Reasons for exclusion for the majority of studies included the control group not receiving a minimal intervention or no intervention, no relevant outcomes reported and the studies not being randomised controlled trials. Some studies were also short‐term, with less than three months follow‐up (see Figure 1).
Risk of bias in included studies
Details for each included trial are presented in the 'Risk of bias' tables in the Characteristics of included studies and summaries are presented in Figure 2 and Figure 3.
2.
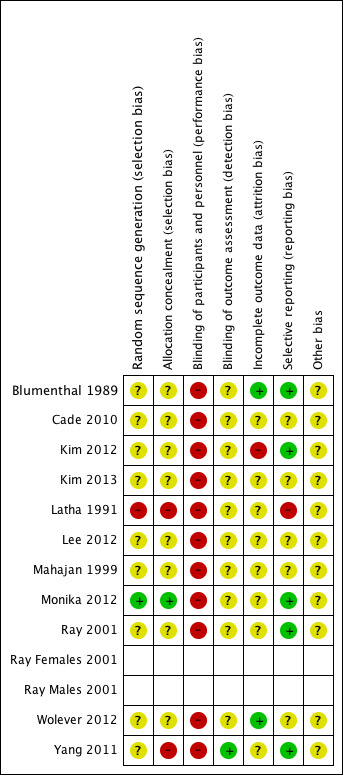
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
3.
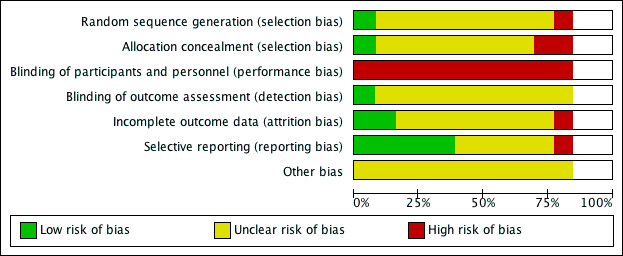
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
The methods of random sequence generation were unclear in nine of the 11 included studies (Blumenthal 1989; Cade 2010; Kim 2012; Kim 2013; Lee 2012; Mahajan 1999; Ray 2001; Wolever 2012; Yang 2011). In the remaining two studies the methods of random sequence generation were stated. In one study, we judged these methods to be at low risk of bias as a statistician not associated with the study generated the randomisation scheme and opaque envelopes were used (Monika 2012). The other study used open allocation and so we judged this to be at high risk of bias (Latha 1991). The methods of allocation concealment were unclear in eight of the 11 included studies (Blumenthal 1989; Cade 2010; Kim 2012; Kim 2013; Lee 2012; Mahajan 1999; Ray 2001; Wolever 2012). In one study, we judged the method of allocation concealment stated to be at low risk of bias (Monika 2012), whilst in the remaining two studies we judged the method of allocation concealment to be at high risk of bias (Latha 1991; Yang 2011).
Blinding
We considered blinding of participants and personnel to be high risk in all 11 of the included studies as it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise. The blinding of outcome assessment was unclear in 10 of the 11 included studies (Blumenthal 1989; Cade 2010; Kim 2012; Kim 2013; Latha 1991; Lee 2012; Mahajan 1999; Monika 2012; Ray 2001; Wolever 2012). The remaining study stated that outcome assessors were blind and so we judged it to be at low risk of bias (Yang 2011).
Incomplete outcome data
In eight of the 11 included studies we judged the reporting of incomplete outcome data to be unclear because there was insufficient information to judge (Cade 2010; Latha 1991; Lee 2012; Mahajan 1999; Yang 2011), no information was provided (Kim 2013), or they did not report the reasons for losses to follow‐up (Monika 2012; Ray 2001). Two of the 11 included studies reported losses to follow‐up and had a similar number of losses between the intervention and control arms (Blumenthal 1989; Wolever 2012). In the remaining study, we judged the reporting of incomplete outcome data to be high risk of bias as there were large numbers of losses to follow‐up with a high number of losses reported in the intervention arm (Kim 2012).
Selective reporting
For five of the 11 included trials the risk of bias of selective reporting was unclear as there was insufficient information available for a judgement to be made (Cade 2010; Kim 2013; Lee 2012; Mahajan 1999; Wolever 2012). We judged five of the included studies to be at low risk of bias as these studies clearly stated the primary and secondary outcomes and reported their results (Blumenthal 1989; Kim 2012; Monika 2012; Ray 2001; Yang 2011). We judged one study to be at high risk of bias as no blood pressure measurements were provided for the control group (Latha 1991).
Other potential sources of bias
For all included studies there was insufficient information to judge the risk of bias from other potential sources.
Effects of interventions
Cardiovascular and all‐cause mortality
None of the included studies provided cardiovascular or all‐cause mortality data.
Non‐fatal Endpoints
None of the included studies provided clinical event data.
Cardiovascular risk factors
Blood pressure
Nine of the 11 included studies measured blood pressure (Cade 2010; Kim 2012; Kim 2013; Latha 1991; Lee 2012; Monika 2012; Ray 2001; Wolever 2012; Yang 2011). Useable data for meta‐analysis were not available for one study (Latha 1991), as no data for the control group were provided, only changes since baseline for the yoga group. In this study, systolic blood pressure was significantly reduced by yoga (mean difference (MD) ‐5.71 mmHg, P < 0.01) and diastolic blood pressure was also reduced but this did not reach statistical significance (mean difference ‐3.71 mmHg, P reported to be non‐significant). The other eight studies could not be combined as there was substantial heterogeneity between trials (I2 = 81%) (Analysis 1.1) (485 participants). Two studies showed a significant reduction in systolic blood pressure with the intervention (Lee 2012; Ray Males 2001), and six studies showed yoga to reduce systolic blood pressure but this did not reach statistical significance (Cade 2010; Kim 2013; Monika 2012; Ray Females 2001; Wolever 2012; Yang 2011). The remaining study showed a significant increase in systolic blood pressure (MD 2.20, 95% confidence interval (CI) 0.16 to 4.24) (Kim 2012).
1.1. Analysis.
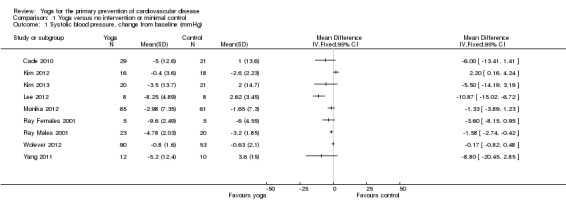
Comparison 1 Yoga versus no intervention or minimal control, Outcome 1 Systolic blood pressure, change from baseline (mmHg).
For diastolic blood pressure (444 participants), we found moderate heterogeneity between studies (I2 = 58%) so we performed a random‐effects meta‐analysis. From the pooled analysis, yoga was found to significantly lower diastolic blood pressure (MD ‐2.90, 95% CI ‐4.52 to ‐1.28) (Analysis 1.2). Results were similar for the fixed‐effect model but we reported the random‐effects results as the effect estimate is more conservative with wider confidence intervals. Sensitivity analysis, removing studies with high risk of bias based on incomplete outcome data (those with loss to follow‐up of more than 20% without intention‐to‐treat analysis), retained seven studies and statistical significance (MD ‐3.38 mmHg, 95% CI ‐4.88 to ‐1.88).
1.2. Analysis.
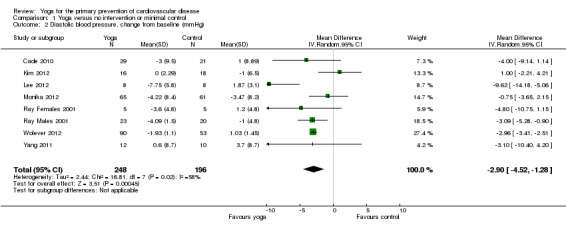
Comparison 1 Yoga versus no intervention or minimal control, Outcome 2 Diastolic blood pressure, change from baseline (mmHg).
Lipid levels
Five trials measured total cholesterol (207 participants) (Blumenthal 1989; Cade 2010; Lee 2012; Mahajan 1999; Yang 2011). Data for these trials could not be pooled as there was significant heterogeneity (I2 = 71%) (Analysis 1.3). Two studies showed a significant reduction in total cholesterol with yoga (Lee 2012; Mahajan 1999). In the three remaining studies (Blumenthal 1989; Cade 2010; Yang 2011), there was some variation in the direction of effect, but individually each found no clear evidence of an effect of yoga on total cholesterol (MD 0.33 mmol/l, 95% CI ‐0.13 to 0.79 (Blumenthal 1989), MD ‐0.16 mmol/l, 95% CI ‐0.68 to 0.36 (Cade 2010), MD ‐0.11 mmol/l, 95% CI ‐0.93 to 0.71 (Yang 2011)). Five trials also measured low‐density lipoprotein (LDL) cholesterol (Blumenthal 1989; Cade 2010; Lee 2012; Mahajan 1999; Yang 2011). We found moderate heterogeneity between studies (I2 = 62%) so we performed a random‐effects meta‐analysis. From the pooled analysis, yoga was found to have no effect on LDL cholesterol (MD ‐0.09 mmol/l, 95% CI ‐0.48 to 0.30) (Analysis 1.4). Results were similar for the fixed‐effect model but, as with diastolic blood pressure, we reported the random‐effects results as the effect estimate is more conservative with wider confidence intervals.
1.3. Analysis.
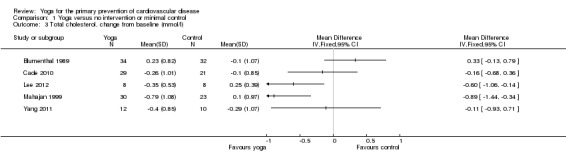
Comparison 1 Yoga versus no intervention or minimal control, Outcome 3 Total cholesterol, change from baseline (mmol/l).
1.4. Analysis.
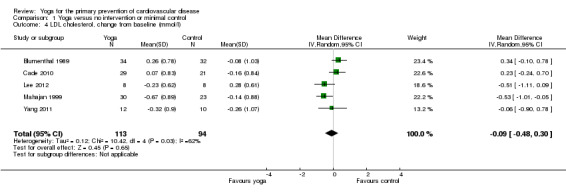
Comparison 1 Yoga versus no intervention or minimal control, Outcome 4 LDL cholesterol, change from baseline (mmol/l).
Five of the 11 included studies measured high‐density lipoprotein (HDL) cholesterol (Blumenthal 1989; Cade 2010; Lee 2012; Mahajan 1999; Yang 2011). From the pooled analysis (207 participants) we found that HDL cholesterol significantly increased with yoga (MD 0.08 mmol/l, 95% CI 0.02 to 0.14) (Analysis 1.5). All five trials also measured triglyceride levels and we pooled data for these five (207 participants). Overall, yoga was found to lower triglyceride levels significantly (mean difference ‐0.27 mmol/l, 95% CI ‐0.44 to ‐0.11) (Analysis 1.6).
1.5. Analysis.
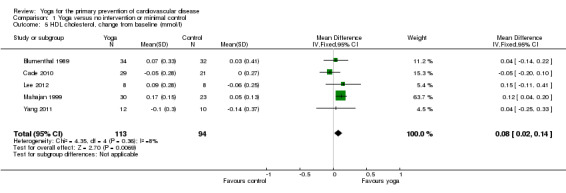
Comparison 1 Yoga versus no intervention or minimal control, Outcome 5 HDL cholesterol, change from baseline (mmol/l).
1.6. Analysis.
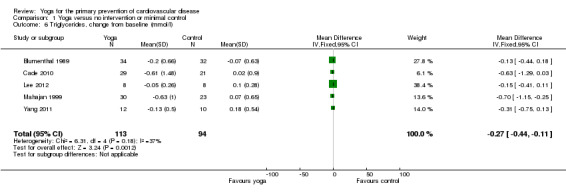
Comparison 1 Yoga versus no intervention or minimal control, Outcome 6 Triglycerides, change from baseline (mmol/l).
Occurrence of type 2 diabetes
None of the 11 included studies provided data on the occurrence of type 2 diabetes.
Quality of life
Quality of life was measured in three of the included studies (Blumenthal 1989; Cade 2010; Ray 2001). In one study (Ray 2001), subjective well‐being at five months was better for women participants in the yoga group (mean 100.0, standard error of the mean (SEM) 11.44) than in the control group (mean 99.04, SEM 9.65), whilst for men subjective well‐being was better in the control group (mean 101.75, SEM 12.55) than in the yoga group (mean 98.4, SEM 12.72). In another study (Cade 2010), absolute Medical Outcome Study ‐ SF36 scores at 20 weeks were the same between the standard care group and the yoga group (73 ± 25 versus 75 ± 24). In the remaining study (Blumenthal 1989), quality of life was measured by a perceived change questionnaire that measured perceived change in mood, personality, physical and social functioning. In this study, participants in the yoga group saw themselves as improving on a number of psychological and behavioural dimensions compared to participants in the wait‐list control group after four months.
Adverse effects
None of the 11 included studies provided information about adverse events.
Costs
None of the 11 included studies provided data on costs.
Discussion
Summary of main results
We identified 11 trials that randomised 800 participants in studies with a duration of three months or more from the 1465 papers screened; 10 of them provided useable data for meta‐analysis. For the remaining study no control group data were provided and its report gave no contact details to elicit further information. We identified two ongoing trials.
None of the trials measured clinical events as they were relatively short‐term and conducted in mainly healthy participants. Small beneficial effects were seen in the five trials that measured triglycerides, the five trials that measured diastolic blood pressure and the five trials that measured high‐density lipoprotein (HDL) cholesterol. For low‐density lipoprotein (LDL) cholesterol, yoga had uncertain effects. For systolic blood pressure and total cholesterol, heterogeneity between trials precluded meta‐analyses. Three trials looked at the effects of yoga on quality of life but the results were inconclusive. No studies reported adverse events and the occurrence of type 2 diabetes. Costs were also not examined in any of the included studies.
The gaps in the published literature are highlighted by the results of this review. There is a lack of reliable, strong evidence on the effects of yoga on clinical events, blood pressure and lipid levels and for the primary prevention of cardiovascular disease (CVD). As such, more trials are needed in order to clarify the potential benefits of yoga for CVD risk factors. Furthermore, the trials included in this review were quite small, at risk of bias and short‐term. Longer, larger, rigorously conducted trials should be carried out to verify or refute the potential benefits of yoga for the primary prevention of CVD.
Overall completeness and applicability of evidence
The review included adults participants who were at varying levels of CVD risk and included both men and women. Most of the trials were conducted in developed countries. None of the 11 included studies examined our primary outcomes as participants were predominantly healthy and trials were small and relatively short‐term in follow‐up. We were also not able to examine the effects of baseline CVD risk, type of yoga or intervention intensity due to the limited number of included studies.
The effectiveness of yoga could not be rigorously assessed since only three trials (174 participants) assessed cardiovascular risk factors at six or more months. The remaining eight studies were shorter‐term so it is unclear if any effects of yoga could be sustained. Furthermore, the 11 included trials were limited in the information that they provided. The majority of the included trials did not state what type of yoga was being assessed or which yoga components were included, and had few details about intervention frequency, duration or physiological intensity. Consequently, we are unable to say which types of yoga are effective in preventing CVD and if the frequency, duration and physiological intensity of yoga impact on its effectiveness.
The 11 included studies varied in the health status of participants. Around half of participants (399 randomised) were classified as at high risk of CVD and were recruited in seven trials (Cade 2010; Kim 2013: Latha 1991; Lee 2012; Mahajan 1999; Monika 2012; Yang 2011), whilst the remaining four trials recruited healthy participants. Due to this variability the applicability of this review's findings to different populations is uncertain. There was also considerable variability in the yoga interventions in the included studies. Studies differed in the intensity of the yoga intervention, with practice ranging from two times a week to five times a week, for 35 minutes to an hour for 12 to 32 weeks. Yoga instructors were also used in some of the included trials and some encouraged practice at home.The type of yoga taught also differed between studies with two studies using Ashtanga yoga (Cade 2010; Kim 2012), one study using Hatha yoga (Ray 2001), one study using yoga Nidra (Monika 2012), one study using Vinyasa yoga (Yang 2011), and one study using Viniyoga (Wolever 2012). The remaining studies did not state which type of yoga they used (Blumenthal 1989; Kim 2013; Latha 1991; Lee 2012; Mahajan 1999). Due to the variability in yoga interventions and the lack of reported detail, we were unable to assess the effectiveness of each type of yoga or to assess intervention intensity. Therefore we cannot say which type of yoga is best at reducing CVD risk and by how much, or for how long yoga should be practised to be able to see reductions in CVD risk factors.
The two ongoing trials will add to the evidence but more longer‐term trials are needed.
Quality of the evidence
Overall, the trials included in this review were at some risk of bias meaning that the results should be treated with caution. In nine of the 11 included trials the methods of random sequence generation were not stated or unclear, whilst in eight trials the details of allocation concealment were not stated. All 11 trials did not state if participants and personnel were blinded and in 10 trials it was unclear whether outcome assessors were blinded. However, it is difficult, if not impossible, to blind participants and personnel to behavioural lifestyle interventions such as yoga. Risk of bias related to incomplete outcome data was unclear in eight trials, low in two trials but high in one trial. We judged bias due to selective outcome reporting to be high in one study, low in five studies and unclear in five studies. For all studies there was insufficient information to judge the risk of other biases.
Small study bias is also a risk in this review since most of the included trials were very small. Furthermore, we were unable to examine the effects of publication bias in funnel plots due to the limited number of trials included in the review. However, small trials are often conducted with less methodological rigour, more likely to be carried out in selected populations and have been shown to report larger beneficial effects than larger trials (Nüesch 2010; Sterne 2000; Sterne 2001). Therefore, the results of this review need to be interpreted with this in mind.
There was a high degree of heterogeneity between trials, from different sources (participants, type of yoga, duration of intervention and follow‐up, outcome data), which precluded statistical pooling for some outcomes. Therefore, our findings should be interpreted with the inconsistency between studies in mind.
Potential biases in the review process
We conducted a comprehensive search across major databases for interventions involving yoga. We also screened systematic review reference lists and contacted authors when necessary. However, from corresponding with authors we did not receive further unreported information or data from three trials, which limited our analysis. Two review authors carried out all screening, inclusion and exclusion and data abstraction independently. Two review authors also conducted data entry and analysis.
Our decision to restrict this review to interventions only investigating yoga avoided the potential confounding effects of other behavioural interventions on our outcomes, for instance interventions that focused on weight loss. However, this limited the number of trials eligible for inclusion. Furthermore, the small number of trials on which this review is based, limitations in reporting methodological rigour, an unclear risk of bias in most trials and sparse or no data for primary and secondary outcomes means that the findings of this review, to date, are limited.
Agreements and disagreements with other studies or reviews
To our knowledge, no other systematic review including only randomised controlled trials has been carried out solely to examine the effects of yoga in adults for the primary prevention of CVD. Other systematic reviews have looked at yoga for secondary prevention of coronary heart disease in adults (Innes 2005; Lau 2012), or have looked at yoga in relation to type 2 diabetes, cancer or physical functioning and health‐related quality of life in older adults (Aljasir 2010; Harder 2012; Patel 2012). One review did not find any randomised controlled trials that examined the effectiveness of yoga for patients with coronary heart disease that were eligible for inclusion (Lau 2012). Another review found some evidence to suggest that yoga reduced insulin resistance syndrome‐related risk factors for CVD and may help in CVD management (Innes 2005). However, this review could not draw any firm conclusions due to the methodological and other limitations of the included studies.
In the current review, trials were also small and heterogeneous. We found substantial heterogeneity between trials for lipid level measurements and for systolic blood pressure. There were differences between the included studies in the characteristics of participants, sample size, intensity of yoga, type of yoga and the duration of follow‐up.
Authors' conclusions
Implications for practice.
Only a few trials met the inclusion criteria for this review and no trials reported our primary outcome. Small beneficial effects were seen in the five trials that measured triglycerides, the five trials that measured high‐density lipoprotein (HDL) cholesterol and the five trials that measured diastolic blood pressure, which is promising. This is because small reductions in cardiovascular disease (CVD) risk factors throughout a whole population may lead to large reductions in CVD incidence (Emberson 2004). For low‐density lipoprotein (LDL) cholesterol, yoga was found to have uncertain effects. However, the trials included in this review were at some risk of bias and as such should be treated with caution. In order to confirm or refute the findings of this review methodologically rigorous trials are needed that examine cardiovascular disease and its risk factors over the longer term.
Given the limited evidence to date, we are unable to determine the effects of yoga in the primary prevention of CVD.
Implications for research.
Currently, there is a lack of evidence from randomised controlled trials that solely examine the effects of yoga for the primary prevention of CVD, particularly over the long term. Such trials are essential to examine the effects of yoga on our primary outcome, CVD events. Future trials should aim to examine the effects of yoga over longer time periods so that the potential benefits of yoga for CVD prevention can be rigorously assessed.
No trials were identified that reported adverse events or economic evaluations of yoga and only three trials reported health‐related quality of life outcomes. Furthermore, there was a lack of information in the included studies about the type of yoga assessed or which components of yoga were included, and few details about the frequency of yoga, duration of the intervention and physiological intensity. Future trials should report all of these details so that the best treatment parameters can be established and so that the effectiveness of yoga and its components can be rigorously assessed. Future trials should also report methods of sequence generation, allocation concealment and methods of blinding, as such details again were scarcely reported in the trials included in this review.
What's new
| Date | Event | Description |
|---|---|---|
| 30 June 2014 | Amended | Minor correction to plain language summary |
Acknowledgements
We are grateful to Nicole Martin and Jo Abbot for conducting the searches for this review. We would also like to acknowledge Dr Yarasheski for providing additional data from their trial (Cade 2010).
Appendices
Appendix 1. Search strategies 2013
CENTRAL
#1 MeSH descriptor Yoga explode all trees #2 MeSH descriptor Relaxation Therapy explode all trees #3 yoga #4 asana #5 pranayama #6 dhyana #7 meditat* #8 MeSH descriptor Meditation explode all trees #9 hatha #10 ananda #11 ashtanga #12 bikram #13 iyengar #14 integral near/5 yoga #15 kripalu #16 kundalini #17 power near/5 yoga #18 sivananda #19 vinyasa #20 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19) #21 MeSH descriptor Cardiovascular Diseases explode all trees #22 (cardio*) #23 (cardia*) #24 (heart*) #25 (coronary*) #26 angina* #27 (ventric*) #28 (myocard*) #29 (pericard*) #30 (isch?em*) #31 (emboli*) #32 arrhythmi* #33 (thrombo*) #34 atrial next fibrillat* #35 (tachycardi*) #36 (endocardi*) #37 (sick next sinus) #38 MeSH descriptor Stroke explode all trees #39 (stroke or stokes) #40 (cerebrovasc*) #41 (cerebral next vascular) #42 apoplexy #43 (brain near/2 accident*) #44 ((brain* or cerebral or lacunar) near/2 infarct*) #45 MeSH descriptor Hypertension explode all trees #46 (hypertensi*) #47 (peripheral next arter* next disease*) #48 ((high or increased or elevated) near/2 blood pressure) #49 MeSH descriptor Hyperlipidemias explode all trees #50 (hyperlipid*) #51 (hyperlip?emia*) #52 (hypercholesterol*) #53 (hypercholester?emia*) #54 (hyperlipoprotein?emia*) #55 (hypertriglycerid?emia*) #56 MeSH descriptor: [Arteriosclerosis] explode all trees #57 MeSH descriptor: [Cholesterol] explode all trees #58 cholesterol #59 "coronary risk factor*" #60 MeSH descriptor: [Blood Pressure] this term only #61 "blood pressure" #62 #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 or #55 or #56 or #57 or #58 or #59 or #60 or #61 #63 #20 and #62
MEDLINE OVID
1. Yoga/ 2. Relaxation Therapy/ 3. yoga.tw. 4. asana.tw. 5. pranayama.tw. 6. dhyana.tw. 7. meditat*.tw. 8. Meditation/ 9. hatha.tw. 10. ananda.tw. 11. ashtanga.tw. 12. bikram.tw. 13. iyengar.tw. 14. (integral adj5 yoga).tw. 15. kripalu.tw. 16. kundalini.tw. 17. (power adj5 yoga).tw. 18. sivananda.tw. 19. vinyasa.tw. 20. or/1‐19 21. exp Cardiovascular Diseases/ 22. cardio*.tw. 23. cardia*.tw. 24. heart*.tw. 25. coronary*.tw. 26. angina*.tw. 27. ventric*.tw. 28. myocard*.tw. 29. pericard*.tw. 30. isch?em*.tw. 31. emboli*.tw. 32. arrhythmi*.tw. 33. thrombo*.tw. 34. atrial fibrillat*.tw. 35. tachycardi*.tw. 36. endocardi*.tw. 37. (sick adj sinus).tw. 38. exp Stroke/ 39. (stroke or stokes).tw. 40. cerebrovasc*.tw. 41. cerebral vascular.tw. 42. apoplexy.tw. 43. (brain adj2 accident*).tw. 44. ((brain* or cerebral or lacunar) adj2 infarct*).tw. 45. exp Hypertension/ 46. hypertensi*.tw. 47. peripheral arter* disease*.tw. 48. ((high or increased or elevated) adj2 blood pressure).tw. 49. exp Hyperlipidemias/ 50. hyperlipid*.tw. 51. hyperlip?emia*.tw. 52. hypercholesterol*.tw. 53. hypercholester?emia*.tw. 54. hyperlipoprotein?emia*.tw. 55. hypertriglycerid?emia*.tw. 56. exp Arteriosclerosis/ 57. exp Cholesterol/ 58. cholesterol.tw. 59. "coronary risk factor*".tw. 60. Blood Pressure/ 61. blood pressure.tw. 62. or/21‐61 63. 20 and 62 64. randomized controlled trial.pt. 65. controlled clinical trial.pt. 66. randomized.ab. 67. placebo.ab. 68. drug therapy.fs. 69. randomly.ab. 70. trial.ab. 71. groups.ab. 72. 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 73. exp animals/ not humans.sh. 74. 72 not 73 75. 63 and 74
EMBASE OVID
1. Yoga/ 2. Relaxation Therapy/ 3. yoga.tw. 4. asana.tw. 5. pranayama.tw. 6. dhyana.tw. 7. meditat*.tw. 8. Meditation/ 9. hatha.tw. 10. ananda.tw. 11. ashtanga.tw. 12. bikram.tw. 13. iyengar.tw. 14. (integral adj5 yoga).tw. 15. kripalu.tw. 16. kundalini.tw. 17. (power adj5 yoga).tw. 18. sivananda.tw. 19. vinyasa.tw. 20. or/1‐19 21. exp cardiovascular disease/ 22. cardio*.tw. 23. cardia*.tw. 24. heart*.tw. 25. coronary*.tw. 26. angina*.tw. 27. ventric*.tw. 28. myocard*.tw. 29. pericard*.tw. 30. isch?em*.tw. 31. emboli*.tw. 32. arrhythmi*.tw. 33. thrombo*.tw. 34. atrial fibrillat*.tw. 35. tachycardi*.tw. 36. endocardi*.tw. 37. (sick adj sinus).tw. 38. exp cerebrovascular disease/ 39. (stroke or stokes).tw. 40. cerebrovasc*.tw. 41. cerebral vascular.tw. 42. apoplexy.tw. 43. (brain adj2 accident*).tw. 44. ((brain* or cerebral or lacunar) adj2 infarct*).tw. 45. exp hypertension/ 46. hypertensi*.tw. 47. peripheral arter* disease*.tw. 48. ((high or increased or elevated) adj2 blood pressure).tw. 49. exp hyperlipidemia/ 50. hyperlipid*.tw. 51. hyperlip?emia*.tw. 52. hypercholesterol*.tw. 53. hypercholester?emia*.tw. 54. hyperlipoprotein?emia*.tw. 55. hypertriglycerid?emia*.tw. 56. exp Arteriosclerosis/ 57. exp Cholesterol/ 58. cholesterol.tw. 59. "coronary risk factor*".tw. 60. Blood Pressure/ 61. blood pressure.tw. 62. or/21‐61 63. 20 and 62 64. random$.tw. 65. factorial$.tw. 66. crossover$.tw. 67. cross over$.tw. 68. cross‐over$.tw. 69. placebo$.tw. 70. (doubl$ adj blind$).tw. 71. (singl$ adj blind$).tw. 72. assign$.tw. 73. allocat$.tw. 74. volunteer$.tw. 75. crossover procedure/ 76. double blind procedure/ 77. randomized controlled trial/ 78. single blind procedure/ 79. 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 80. (animal/ or nonhuman/) not human/ 81. 79 not 80 82. 63 and 81
Web of Science
#19 #18 AND #17 #18 TS=((random* or blind* or allocat* or assign* or trial* or placebo* or crossover* or cross‐over*)) #17 #16 AND #7 #16 #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 #15 TS=(arteriosclerosis or cholesterol or "coronary risk factor*" or "blood pressure") #14 Topic=(hyperlipid* or hyperlip?emia* or hypercholesterol* or hypercholester?emia* or hyperlipoprotein?emia* or hypertriglycerid?emia*) #13 Topic=(high near/2 "blood pressure" or increased near/2 "blood pressure" or elevated near/2 "blood pressure") #12 Topic=(brain* near/2 infarct or cerebral near/2 infarct or lacunar near/2 infarct* or hypertensi* or "peripheral arter* disease*") #11 Topic=("cerebral vascular" or apoplexy or brain near/2 accident*) #10 Topic=("atrial fibrillat*" or tachycardi* or endocardi* or "sick sinus" or stroke or stokes or cerebrovasc*) #9 Topic=(myocard* or pericard* or isch?em* or emboli* or arrhythmi* or thrombo*) #8 Topic=(cardio* or cardia* or heart* or coronary* or angina* or ventric*) #7 #6 OR #5 OR #4 OR #3 OR #2 OR #1 #6 Topic=(sivananda or vinyasa) #5 Topic=(kripalu or kundalini) #4 Topic=(integral near/5 yoga) #3 Topic=(hatha or ananda or ashtanga or bikram or iyengar) #2 Topic=(asana or pranayama or dhyana or meditat*) #1 Topic=(yoga)
AMED
1. Yoga/ 2. Relaxation Therapy/ 3. Yoga.tw. 4. asana.tw. 5. pranayama.tw. 6. dhyana.tw. 7. meditat*.tw. 8. Meditation/ 9. hatha.tw. 10. ananda.tw. 11. ashtanga.tw. 12. bikram.tw. 13. iyengar.tw. 14. (integral adj5 yoga).tw. 15. kripalu.tw. 16. kundalini.tw. 17. (power adj5 yoga).tw. 18. sivavavda.tw. 19. vinyasa.tw. 20. or/1‐19 21. cardio*.tw. 22. cardia*.tw. 23. heart*.tw. 24. coronary*.tw. 25. angina*.tw. 26. ventric*.tw. 27. myocard*.tw. 28. pericard*.tw. 29. isch?em*.tw. 30. emboli*.tw. 31. arrhythmi*.tw. 32. thrombo*.tw. 33. atrial fibrillat*.tw. 34. tachycardi*.tw. 35. endocardi*.tw. 36. (sick adj sinus).tw. 37. exp Stroke/ 38. (stroke or strokes).tw. 39. cerebrovasc*.tw. 40. cerebral vascular.tw. 41. apoplexy.tw. 42. (brain adj2 accident*).tw. 43. ((brain* or cerebral or lacunar) adj2 infarct*).tw. 44. exp Hypertension/ 45. hypertensi*.tw. 46. peripheral arter* disease*.tw. 47. ((high or increased or elevated) adj2 blood pressure).tw. 48. hyperlipid*.tw. 49. hyperlip?emia*.tw. 50. hypercholesterol*.tw. 51. hypercholester?emia*.tw. 52. hyperlipoprotein?emia*.tw. 53. hypertriglycerid?emia*.tw. 54. or/21‐53 55. randomized controlled trial.pt. 56. controlled clinical trial.pt. 57. randomized.ab. 58. placebo.ab. 59. randomly.ab. 60. trial.ab. 61. groups.ab. 62. 55 or 56 or 57 or 58 or 59 or 60 or 61 63. exp animals/ not humans.sh. 64. 62 not 63 65. 20 and 54 and 64 66. arteriosclerosis.tw. 67. cholesterol.tw. 68. cholest*.tw. 69. or/21‐53,66‐68 70. 20 and 64 and 69
CNKI
1. 瑜伽 (3849)
2. 心血管疾病 (31,751)
3. 冠心病 (119,627)
4. 高血压 (216,118)
5. 高血脂 (12,658)
6. 心绞痛 (53,121)
7. 心肌梗死 (60,303)
8. 心律失常 (73,634)
9. 心力衰竭 (60,061)
10. 心肌缺血 (38,661)
11. 动脉粥样硬化 (51,704)
12. 冠状动脉疾病 (15,653)
13. 中风 (30,152)
14. 脑卒中 (43,507)
15. 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 (593,994)
16. 对照 (963,149)
17. 随机 (702,107)
18. 16 or 17 (1,291,457)
19. 1 and 15 and 18 (1)
KoreaMed
1. 요가:0
DBPIA
Yoga AND cardiovascular disease
Yoga AND hypertension
Yoga AND stroke
Yoga AND hyperlipidemia
Yoga AND angina
Yoga AND coronary
요가 AND 심혈관:
요가 AND 고혈압:
요가 AND 중풍:
요가 AND 고지혈증:
요가 AND 협심증:
요가 AND 심근경색:
Korean studies information service system
Yoga AND cardiovascular disease
Yoga AND hypertension
Yoga AND stroke
Yoga AND hyperlipidemia
Yoga AND angina
Yoga AND coronary
요가 AND 심혈관
요가 AND 고혈압
요가 AND 중풍
요가 AND 고지혈증
요가 AND 협심증
요가 AND 심근경색
OASIS
요가:0
Clinicaltrials.gov
1. Cardio* 2. Yoga
WHO ICTRP
1. Cardio* 2. Yoga
ISRCTN Register
1. Cardio* 2. Yoga
Data and analyses
Comparison 1. Yoga versus no intervention or minimal control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Systolic blood pressure, change from baseline (mmHg) | 9 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Diastolic blood pressure, change from baseline (mmHg) | 8 | 444 | Mean Difference (IV, Random, 95% CI) | ‐2.90 [‐4.52, ‐1.28] |
| 3 Total cholesterol, change from baseline (mmol/l) | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 LDL cholesterol, change from baseline (mmol/l) | 5 | 207 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.48, 0.30] |
| 5 HDL cholesterol, change from baseline (mmol/l) | 5 | 207 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [0.02, 0.14] |
| 6 Triglycerides, change from baseline (mmol/l) | 5 | 207 | Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.44, ‐0.11] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Blumenthal 1989.
| Methods | RCT | |
| Participants | Men and women who were healthy and free from coronary disease were recruited via advertisements on TV, radio, in local newspapers and from the Duke aging centre subject registry. 101 participants were randomly assigned to 3 arms: aerobic exercise; yoga; wait‐list control Inclusion criteria: healthy and free from coronary disease, at least 60 years old, sedentary, did not engage in regular exercise. 34 participants were randomised to yoga and 34 participants were randomised to the wait‐list control The study was published in the USA |
|
| Interventions | Yoga group: 60 minutes of supervised yoga at least twice a week for 16 weeks Wait‐list control: did not receive any form of treatment. Instructed not to change their physical activity habits and specifically not to engage in any aerobic exercise Follow‐up was 4 months |
|
| Outcomes | Lipid levels, QoL and blood pressure | |
| Notes | We contacted the author twice for extra information on blood pressure and lipid levels. The author did not respond | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States conditional randomisation procedure but does not provide any details of the randomisation procedure used |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not stated but it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No ITT analysis but drop‐outs and loss to follow‐up are low, with reasons reported |
| Selective reporting (reporting bias) | Low risk | All outcomes stated were reported |
| Other bias | Unclear risk | Insufficient information to judge |
Cade 2010.
| Methods | RCT | |
| Participants | HIV‐infected men and women who were 18 to 70 years old were recruited from a clinical trials unit and local infectious diseases clinics. 60 participants were randomly assigned to 2 arms ‐ yoga practice or standard care Inclusion criteria: documented HIV status, stable and with no plans to change current cART, CD4+ T‐cell count > 2000 cells/ml, plasma HIV RNA < 15,000 copies/ml and at least 1 of the following CVD risk factors: dyslipidaemia, central adiposity, glucose intolerance/insulin resistance or hypertension Exclusion criteria: chronic hepatitis B or active hepatitis C virus infection, diabetes, male hypogonadism, hypo‐ or hyperthyroidism, pregnant or plans to become pregnant, prior MI, unstable angina, heart failure, coronary artery disease, resting ST‐segment depression > 1 mm, coronary artery bypass graft or stroke and active substance abuse 34 participants were randomised to yoga and 26 to standard care The paper was published in the USA |
|
| Interventions | Yoga group: Ashtanga Vinyasa yoga was taught and practised. This follows progressive steps that required adherence, self control, mental focus, self awareness and physical resilience. All sessions emphasised the proper use of aligned postures, controlled breathing, focused gaze and the regulation of prana through the use of bandhas, strength building, increased flexibility, large muscle movement, asymmetrical movements and restorative relaxation. Yoga sessions were standardised and were held 2 to 3 times/week for approximately 60 minutes/session for 20 weeks. Participants initially received individual instruction but were then encouraged to practise at home (at least once a week) Standard care: regular routine visits to their physician, no added physical activity, no changes in cART and no added medications for hyperglycaemia, hyperlipidaemia or hypertension Follow‐up was 20 weeks |
|
| Outcomes | Blood pressure, lipid levels, QoL | |
| Notes | We contacted authors for extra blood pressure and lipid data for each point at which these were measured. The authors responded with the data requested | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not stated but it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to judge |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge |
| Other bias | Unclear risk | Insufficient information to judge |
Kim 2012.
| Methods | RCT | |
| Participants | Healthy premenopausal women who were 35 to 50 years old were recruited from the University of Oklahoma and the surrounding city area by flyers, adverts in local newspapers and mail. 47 participants were randomly assigned to 2 arms: yoga exercise group and control group Inclusion criteria: free of chronic back or joint problems, cardiovascular disease, non‐smokers, not pregnant, not taking antihypertensive drugs, not taking hormonal contraception, medically stable, ambulatory and capable of undergoing physical strength testing/training 27 participants were randomised to yoga and 20 participants were randomised to the control group The paper was published in the USA |
|
| Interventions | Yoga group: Ashtanga yoga was taught Mondays and Wednesdays from 6.30 to 7.30 am. 64 sessions were provided over 8 months. Each session lasted 60 minutes, which consisted of 15 minutes warm‐up, 35 minutes of postures and 10 minutes cool‐down with relaxation. Dynamic and static stretching was introduced during the warm‐up at the beginning with either sitting, supine or standing postures. A certified yoga instructor led all yoga sessions and precisely taught postures with consistent instructions. Session intensity was progressively increased by adding the number of Sun Salutations and jumping during the 8‐month intervention. All yoga postures were followed by the English name Control group: encouraged to maintain normal daily physical activity Follow‐up was 8 months |
|
| Outcomes | Blood pressure | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not stated but it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 40% lost to follow‐up in intervention group and 10% in control group. Also no intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All outcomes stated were reported |
| Other bias | Unclear risk | Insufficient information to judge |
Kim 2013.
| Methods | RCT | |
| Participants | 41 women with metabolic syndrome were randomised to a yoga or control group. 20 participants were randomised to yoga and 21 participants were randomised to the control group The country of publication was not stated | |
| Interventions | Yoga: yoga exercise for 12 weeks Control group: wait‐list Follow‐up was 12 weeks |
|
| Outcomes | Systolic blood pressure | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to judge |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge |
| Other bias | Unclear risk | Insufficient information to judge |
Latha 1991.
| Methods | RCT | |
| Participants | Essential hypertensive patients aged between 45 and 70 years who were attending outpatients at the hypertension clinic at Madras general hospital were recruited. 14 participants were randomised to yoga and thermal biofeedback or to the control group Inclusion criteria: on antihypertensive medication and free from any other abnormalities or pathological conditions 7 patients were randomised to yoga and 7 patients were randomised to the control group The country of publication was India |
|
| Interventions | Yoga: participants were told briefly about the nature of training and time of sessions. They practised selected breathing techniques and asanas that were taught by one of the investigators. Participants met twice a week for 6 months Control group: met once a week in the clinical setting to have blood pressure recorded and to have a general talk. They received the same amount of attention as the yoga group Follow‐up was 6 months |
|
| Outcomes | Blood pressure | |
| Notes | No contact details provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Odd and even numbers |
| Allocation concealment (selection bias) | High risk | Open allocation so trial recruiters knew what the next treatment option was |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not stated but it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information provided |
| Selective reporting (reporting bias) | High risk | No blood pressure measurements are provided for the control group at the end of the intervention period |
| Other bias | Unclear risk | Insufficient information to judge |
Lee 2012.
| Methods | RCT | |
| Participants | Healthy postmenopausal female volunteers who were 54.50 ± 2.75 years with more than 36% body fat were recruited from Busan, Korea. 16 women were randomly assigned to 2 arms: yoga exercise group or a "no exercise " control Inclusion criteria: postmenopausal, asymptomatic of any illness or disease, free from any acute or chronic injury, sedentary and were healthy nonsmokers using no medication 8 participants were randomised to yoga and 8 participants were randomised to the "no exercise" control The trial was conducted in South Korea |
|
| Interventions | Yoga group: yoga was taught and practised 3 times a week for 60 minutes a session on non‐consecutive days for 16 weeks. All sessions emphasised the proper use of aligned postures and breathing techniques and maintaining the body through the use of large muscle movements, asymmetrical movements and restorative relaxation "No exercise" group: instructed to take no exercise Follow‐up was 16 weeks |
|
| Outcomes | Blood pressure and lipid levels | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not stated but it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Hip circumference was stated as a measure but was not reported. There is also insufficient information to judge |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge |
| Other bias | Unclear risk | Insufficient information to judge |
Mahajan 1999.
| Methods | RCT | |
| Participants | Men aged 56 to 59 years with either angina or 1 or more coronary risk factor were recruited. They were divided into those with angina and those with coronary risk factors and 93 participants were randomised to 2 groups: yoga or conventional therapy Inclusion criteria: coronary risk factors included those with hypertension (BP > 140/90) for 6 months but on stable antihypertensive treatment for at least 6 weeks, history of smoking more than 9 cigarettes a day, cholesterol level above 250 mg/dl as diagnosed twice in previous year Exclusion criteria: those with unstable angina pectoris, left ventricular failure, cardiomegaly, ventricular arrhythmia or any other systemic disease. Overall, 41 participants were randomised to receive the conventional therapy and 52 participants were randomised to yoga. For the participants with coronary risk factors, 23 participants were randomised to conventional therapy and 30 to yoga The country of publication was India |
|
| Interventions | Yoga group: the participants spent 4 days at a yoga residential camp where they underwent training in various yogic lifestyle techniques. The programme consisted of yogic rejuvenating practices, stretching postures of asanas, pranayama, preksha dhyan, meditation and progressive muscle relaxation. The participants were asked to continue the programme at home for 1 hour daily which included half an hour of meditation, relaxation and half an hour of asanas. Participants visited the yoga centre every 2 weeks for evaluation and compliance Conventional therapy: managed with conventional therapy with control of risk factors. Diet control and moderate aerobic exertion as routinely advised The follow‐up period was 14 weeks |
|
| Outcomes | Lipid levels | |
| Notes | We emailed the authors for extra information on the control group but they did not respond | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not stated but it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to judge |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge |
| Other bias | Unclear risk | Insufficient information to judge |
Monika 2012.
| Methods | RCT | |
| Participants | Women 28.08 ± 7.43 years of age with menstrual irregularities visiting the department of Gynecology, CSMMU, Lucknow were recruited into the study. 150 participants were randomised to 2 arms: yoga and medication or medication alone 75 participants were randomised to the yoga group and 75 participants were randomised to the control group The country of publication was India |
|
| Interventions | Yoga: yoga Nidra sessions were guided by well‐educated and trained instructors that had been selected by an expert committee. The sessions were free and all necessary facilities were provided to the participants. The total duration of practice was 35 to 40 minutes a day for 5 days a week in the morning for 6 months. Practice was done in the department of physiology CSMMU UP, Lucknow Control: non‐yoga. Given medication (tranexamic acid, ethamsylate, madroxy progesterone, norethisterone ethinyl estradiol, levonorgestrel). Medication was provided to both groups The follow‐up period was 6 months |
|
| Outcomes | Blood pressure | |
| Notes | We emailed authors twice for extra information on the control group. However, the email address was not recognised and no other contact details were available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator |
| Allocation concealment (selection bias) | Low risk | Statistician not associated with the study generated randomisation scheme. They also used opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not stated but it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No intention‐to‐treat analysis performed and no reasons for losses provided |
| Selective reporting (reporting bias) | Low risk | All outcomes stated were reported |
| Other bias | Unclear risk | Insufficient information to judge |
Ray 2001.
| Methods | RCT | |
| Participants | Participants were electronic fellowship course students and mechanical engineering fellowship students. 54 participants were randomised to 2 arms: yoga and nothing Inclusion criteria: healthy, 22 to 25 years old 28 participants were randomised to yoga (23 male, 5 female: male age 23.6 ± 0.5, female age 22.6 ± 1.5) and 26 participants were randomised to the control (21 male, 5 female: male age 22 ± 1.07, female age 22.8 ± 0.58) Country of publication was India |
|
| Interventions | Yoga group: trained in selected yoga exercises (Hatha yoga) for 1 hour every alternate day of the week. All yogic practices were performed under the guidance of 3 qualified yoga instructors Control group: given nothing; after 5 months were instructed in yoga Follow‐up: 5 months |
|
| Outcomes | Blood pressure, subjective well‐being | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not stated but it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No ITT analysis and no reasons provided for drop‐outs or those lost to follow‐up. Also no written details of numbers lost to follow‐up. More information needed |
| Selective reporting (reporting bias) | Low risk | All outcomes stated were reported |
| Other bias | Unclear risk | Insufficient information to judge |
Ray Females 2001.
| Methods | See above information | |
| Participants | — | |
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
Ray Males 2001.
| Methods | See above information | |
| Participants | — | |
| Interventions | — | |
| Outcomes | — | |
| Notes | — | |
Wolever 2012.
| Methods | Pilot RCT | |
| Participants | Participants were employees of a national insurance carrier who volunteered. 239 participants were randomised to 4 arms: yoga; mindfulness online; mindfulness in person; no stress management intervention Inclusion criteria: scored 16 or higher on the 10‐item Perceived Stress Scale (PSS) Exclusion criteria: they had an arrhythmia requiring medication or a pacemaker, pregnant, heavy smoker, heavy nicotine gum chewer or heavily chewed tobacco, were on medications that would affect heart rate, had a major medical condition or psychological disorder, reported significant current or previous yoga or meditation experience or participated in an extended meditation or yoga retreat of more than 2 days in the past 5 years 90 participants were randomised to yoga (73.3% female; 92.2% not Hispanic/Latino, 7.8% Hispanic/Latino) and 53 participants were randomised to the control involving no stress management (81.1% female; 90.6% not Hispanic/Latino, 9.4% Hispanic/Latino) Country of publication was the USA |
|
| Interventions | Yoga group: 12‐week, 12‐hour programme developed by the American Viniyoga Institute (AVI) that progressively introduced tools for managing stress including asanas, breathing techniques, guided relaxation, mental techniques and education about starting home practice. Yoga was taught by an AVI‐trained teacher and the classes were offered at two work sites: one in Hartford, CT and the other in Walnut Creek, CA. Instructional handouts were provided to educate participants on home practice and shorter "yoga breaks" for home and at work. Half of the participants also received a DVD to support home practice. No stress management group: received the same assessments as the yoga group but did not received a stress management intervention. They were given a list of resources available to all employees that included discounted fitness programmes, chair massage sessions, employee assistance programmes, behavioural health services for depression and wellness coaching opportunities The follow‐up period was 12 weeks |
|
| Outcomes | Blood pressure | |
| Notes | After completion all participants received USD 75 and a USD 75 gift card for a massage therapy studio | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not stated but it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Used intention‐to‐treat analysis and provided numbers of losses to follow‐up. Numbers were similar between groups |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge |
| Other bias | Unclear risk | Insufficient information to judge |
Yang 2011.
| Methods | Pilot RCT | |
| Participants | Male and female participants were recruited via automated voicemail messages that were delivered to university employees, flyers posted in hospital outpatient waiting rooms and advertisements in local newspapers. 25 participants were randomised to 2 arms: yoga and health education materials Inclusion criteria: between 45 and 65 years old, non‐exercisers for the previous 12 months, have a family history of type 2 diabetes and at least 1 of the following cardio‐metabolic risk factors: impaired fasting glucose, pre‐hypertension, overweight/obese or abnormal level of cholesterol Exclusion criteria: those who were pregnant, used any drug to reduce their blood cholesterol level, BP or glucose, or had a physical disability that would limit their ability to practise yoga 13 participants were randomised to yoga and 12 were randomised to the health education materials (2 male, 21 female; 19 white, 2 black, 1 Hispanic, 1 Native American) Country of publication was the USA |
|
| Interventions | Participants in both groups were asked to maintain their current activity levels during the intervention Yoga group: 3‐month Vinyasa yoga intervention programme developed and led by a certified yoga instructor who is a PhD certified nurse. Vinyasa yoga is an evolving form of Hatha yoga but Vinyasa is more fitness‐based. The programme included various physical postures and each movement was combined with various breathing patterns. Each 1‐hour session began with a warm‐up (5 to 7 minutes) and ended with a relaxation period (10 minutes). To guide and facilitate home practice participants were provided with a CD of the yoga instructions recorded by the instructor. Group sessions were held twice a week with 2 to 3 days between sessions. There was no certain amount of frequency required Health education materials group: general health education materials mailed to their home every 2 weeks for 3 months. Included content about risk factors for type 2 diabetes and its prevention, tips for healthy eating out, CVD risk factors, consuming a balanced diet and engaging in physical activity Follow‐up period was 3 months |
|
| Outcomes | Blood pressure and lipid levels | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | High risk | To avoid disappointment with group assignment participants were informed of randomisation when they first contacted the project office for the initial telephone screening |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not stated but it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Measurements done by staff who were blinded to group assignment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to judge |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in methods were reported |
| Other bias | Unclear risk | Insufficient information to judge |
BP: blood pressure cART: combination antiretroviral therapy HIV: human immunodeficiency virus ITT: intention‐to‐treat MI: myocardial infarction QoL: quality of life RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agte 2011 | Not a RCT |
| Bock 2012 | No relevant outcome and intervention was multifactorial |
| Chaya 2006 | Not a RCT |
| Chen 2006 | No relevant outcomes |
| Duraiswamy 2007 | Control not minimal |
| Harinath 2004 | Control not minimal |
| Madanmohan 2008 | Not a RCT |
| McCaffrey 2005 | Not a RCT |
| Priya 2012 | Not a RCT |
| Telles 2004 | Not a RCT |
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Punita 2011.
| Methods | Randomised controlled trial with 2 arms |
| Participants | Patients with essential hypertension from JIPMER outpatient department |
| Interventions | Experimental: supervised yoga training consisting of static postures, breathing and relaxation techniques 3 times a week for 12 weeks. Also given antihypertensive drugs Control: antihypertensive drugs only Lifestyle modifications like dietary pattern, physical activity, cessation of smoking and alcohol were advised to both groups |
| Outcomes | Blood pressure |
| Notes | We contacted the authors for information on lifestyle advice to see what form this took and if it was minimal |
Characteristics of ongoing studies [ordered by study ID]
Cohen 2008.
| Trial name or title | Not known |
| Methods | Randomised controlled trial with 2 arms |
| Participants | Men and women aged 30 to 65 years who had metabolic syndrome |
| Interventions | Experimental: yoga, 3‐hour introductory class followed by 90‐minute session twice a week during weeks 1 to 5 and weekly during weeks 6 to 10. All sessions were taught by 2 yoga certified instructors Control: no intervention during the study |
| Outcomes | Blood pressure, weight, height, insulin sensitivity, stress, SF‐36, CES‐D |
| Starting date | No information available |
| Contact information | Beth Cohen Department of Veterans Affairs Medical Center General Internal Medicine (111A1) 4150 Clement Street San Francisco, CA 94121 Beth.Cohen@ucsf.edu |
| Notes | — |
NCT01305096.
| Trial name or title | Not known |
| Methods | Randomised controlled trial with 2 arms |
| Participants | Men and women who are 25 to 60 years old, healthy, not doing regular, planned physical activity that makes them out of breath or sweaty, yoga novices, office and manual workers |
| Interventions | Experimental: yoga inversions group ‐ 8 weeks of yoga classes held 2 times a week for 1 hour. The classes will consist of yoga inversions, other yoga postures and deep, slow breathing Control: no intervention ‐ conduct lives as usual |
| Outcomes | Heart rate variability, anthropometric variables, common symptoms in general practice, level of sleepiness, blood pressure, hand grip strength, relaxation and recovery, perceived stress, self rated health, perceived exertion, satisfaction with life, level of work‐family conflict |
| Starting date | March 2011 |
| Contact information | Per Wandell, Professor, Karolinska Institutet |
| Notes | — |
CES‐D: Center for Epidemiologic Studies Depression Scale
Differences between protocol and review
It was our intention to perform stratified analysis to examine the effects of baseline risk, duration of yoga and type of yoga but the review included an insufficient number of trials to do this. We also intended to create funnel plots to assess publication bias. These will be addressed in future updates of this review when more evidence is available. It was also our intention to include only studies with a six‐month follow‐up. However, as such studies were lacking, we changed the review to include studies with a follow‐up of three months or more.
In the review, substantial heterogeneity was defined but this was not defined within the protocol. We added this definition at the request of an external reviewer. The outcome "costs" was also added to the review so that resource use could be examined if data were available.
Contributions of authors
All authors contributed to protocol development. The Trials Search Co‐ordinators of the Cochrane Heart Group ran the searches and MS conducted the searches for the Asian databases. LH and MD/JH screened the titles and abstracts and assessed studies for formal inclusion and exclusion. LH and MD abstracted data and assessed methodological rigour. LH and KR conducted the analysis and wrote the first draft of the review. All authors contributed to later drafts.
Sources of support
Internal sources
Warwick Medical School, University of Warwick, UK.
External sources
NIHR Cochrane Programme Grant, UK.
Karen Rees is also supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care West Midlands at University Hospitals Birmingham NHS Foundation Trust, UK.
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Blumenthal 1989 {published data only}
- Blumenthal JA, Emery CF, Madden DJ, George LK, Coleman RE, Riddle MW, et al. Cardiovascular and behavioural effects of aerobic exercise training in healthy older men and women. Journal of Gerontology 1989;44(5):M147‐57. [DOI] [PubMed] [Google Scholar]
Cade 2010 {published and unpublished data}
- Cade T, Reeds DN, Mondy KE, Overton T, Grassino J, Tucker S, et al. Yoga lifestyle intervention reduces blood pressure in HIV‐infected adults with cardiovascular disease risk factors. HIV Medicine 2010;11(6):379‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2012 {published data only}
- Kim SJ, Bemben MG, Bemben DA. Effects of an 8‐month yoga intervention on arterial compliance and muscle strength in premenopausal women. Journal of Sports Science and Medicine 2012;11(2):322‐30. [PMC free article] [PubMed] [Google Scholar]
Kim 2013 {published data only}
- Kim HN, Kim KS, Kim SW. Effects of yoga on sexual function in women with metabolic syndrome. European Journal of Internal Medicine 2013;24:e104. [DOI] [PubMed] [Google Scholar]
- Kim HN, Ryu J, Kim KS, Song SW. Effects of yoga on sexual function in women with metabolic syndrome: a randomized controlled trial. Journal of Sexual Medicine 2013;10:2741‐51. [DOI] [PubMed] [Google Scholar]
Latha 1991 {published data only}
- Latha, Kaliappan KV. Yoga, Pranayama, thermal biofeedback techniques in the management of stress and high blood pressure. Journal of Indian Psychology 1991;9(1 and 2):36‐46. [Google Scholar]
Lee 2012 {published data only}
- Lee JA, Kim JW, Kim DY. Effects of yoga exercise on serum adiponectin and metabolic syndrome factors in obese postmenopausal women. Menopause 2012;19(3):296‐301. [DOI] [PubMed] [Google Scholar]
Mahajan 1999 {published data only}
- Mahajan AS, Reddy KS, Sachdeva U. Lipid profile of coronary risk subjects following yogic lifestyle intervention. Indian Heart Journal 1999;51(1):37‐40. [PubMed] [Google Scholar]
Monika 2012 {published data only}
- Monika, Singh U, Ghildiyal A, Kala S, Srivastava N. Effect of Yoga Nidra on physiological variables in patients of menstrual disturbances of reproductive age group. Indian Journal of Physiology and Pharmacology 2012;56(2):161‐7. [PubMed] [Google Scholar]
Ray 2001 {published data only}
- Ray US, Mukhopadhyaya S, Purkayastha SS, Asnani V, Tomer OS, Prashad R, et al. Effect of yogic exercises on physical and mental health of young fellowship course trainees. Indian Journal of Physiology and Pharmacology 2001;45(1):37‐53. [PubMed] [Google Scholar]
Ray Females 2001 {published data only}
- Ray US, Mukhopadhyaya S, Purkayastha SS, Asnani V, Tomer OS, Prashad R, et al. Effect of yogic exercises on physical and mental health of young fellowship course trainees. Indian Journal of Physiology and Pharmacology 2001;45(1):37‐53. [PubMed] [Google Scholar]
Ray Males 2001 {published data only}
- Ray US, Mukhopadhyaya S, Purkayastha SS, Asnani V, Tomer OS, Prashad R, et al. Effect of yogic exercises on physical and mental health of young fellowship course trainees. Indian Journal of Physiology and Pharmacology 2001;45(1):37‐53. [PubMed] [Google Scholar]
Wolever 2012 {published data only}
- Wolever RQ, Bobinet KJ, McCabe K, Mackenzie ER, Fekete E, Kusnick CA. Effective and viable mind‐body stress reduction in the workplace: a randomized controlled trial. Journal of Occupational Health Psychology 2012;17(2):246‐58. [DOI] [PubMed] [Google Scholar]
Yang 2011 {published data only}
- Yang K, Bernardo LM, Sereika SM, Conroy MB, Balk J, Burke LE. Utilization of 3‐month yoga program for adults at high risk for type 2 diabetes: a pilot study. Evidence‐Based Complementary and Alternative Medicine 2011;2011:257891. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Agte 2011 {published data only}
- Agte VV, Jahagirdar MU, Tarwadi KV. The effects of Sudarshan Kriya Yoga on some physiological and biochemical parameters in mild hypertensive patients. Indian Journal of Physiology & Pharmacology 2011;55(2):183‐7. [PubMed] [Google Scholar]
Bock 2012 {published data only}
- Bock BC, Morrow KM, Becker BM, Williams DM, Tremont G, Gaskins RB, et al. Yoga as a complementary treatment for smoking cessation: rationale, study design and participant characteristics of the Quitting‐in‐Balance study. BMC Complementary and Alternative Medicine 2010;10(14):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaya 2006 {published data only}
- Chaya MS, Kurpad AV, Nagendra HR, Nagarathna R. The effect of long term combined yoga practice on the basal metabolic rate of healthy adults. BMC Complementary and Alternative Medicine 2006;6(28):1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2006 {published data only}
- Chen KM, Tsen WS, Ting LF, Huang GF. Development and evaluation of a yoga exercise programme for older adults. Journal of Advanced Nursing 2007;57(4):432‐41. [DOI] [PubMed] [Google Scholar]
Duraiswamy 2007 {published data only}
- Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add‐on treatment in the management of patients with schizophrenia ‐ a randomized controlled trial. Acta Psychiatrica Scandinavica 2007;116(3):226‐32. [DOI] [PubMed] [Google Scholar]
Harinath 2004 {published data only}
- Harinath K, Malhotra AS, Pal K, Prasad R, Kumar R, Kain TC, et al. Effects of Hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. Journal of Alternative and Complementary Medicine 2004;10(2):261‐8. [DOI] [PubMed] [Google Scholar]
Madanmohan 2008 {published data only}
- Madanmohan, Mahadevan SK, Balakrishnan S, Gopalakrishnan M, Prakash ES. Effect of six weeks yoga training on weight loss following step test, respiratory pressures, handgrip strength and handgrip endurance in young healthy subjects. Indian Journal of Physiology and Pharmacology 2008;52(2):164‐70. [PubMed] [Google Scholar]
McCaffrey 2005 {published data only}
- McCaffrey R, Ruknui P, Hatthakit U, Kasetsomboon P. The effects of yoga on hypertensive persons in Thailand. Holistic Nursing Practice 2005;19(4):173‐80. [DOI] [PubMed] [Google Scholar]
Priya 2012 {published data only}
- Priya SA. Effect of shavasana training on basal heart rate and blood pressure in young healthy volunteers. Biomedicine 2012;32(1):25‐8. [Google Scholar]
Telles 2004 {published data only}
- Telles S, Joshi M, Dash M, Raghuraj P, Naveen KV, Nagendra HR. An evaluation of the ability to voluntarily reduce the heart rate after a month of yoga practice. Integrative Physiological & Behavioral Science 2004;39(2):119‐25. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Punita 2011 {published data only}
- Punita P, Madanmohan T, Swaminathan RP. Effect of 12 week yoga therapy on cardiac autonomic functions in patients of essential hypertension. Indian Journal of Physiology and Pharmacology 2011;55(5):42‐3. [Google Scholar]
References to ongoing studies
Cohen 2008 {published data only}
- Cohen BE, Chang AA, Grady D, Kanaya AM. Restorative yoga in adults with metabolic syndrome: a randomized controlled pilot trial. Metabolic Syndrome and Related Disorders 2008;6(3):223‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT01305096 {published data only}
- Wandell P. Effects of yoga on objective and self‐reported health indicators among female and male office and manual workers. http://clinicaltrials.gov/ct2/show/NCT01305096 accessed 24/9/12.
Additional references
ACSM 2010
- American College of Sports Medicine. ACSM's Resource Manual for Guidelines for Exercise Testing and Prescription. 6th Edition. Philadelphia: Wolters Kluwer Health/Lippincott Williams and Wilkins, 2010. [Google Scholar]
AHA 2011
- American Heart Association (AHA). Physical activity improves quality of life. http://www.heart.org/HEARTORG/GettingHealthy/Physical Activity/StartWalking/Physical‐activity‐improves‐quality‐of‐life_UCM_307977_Article.jsp (accessed 1 April 2012).
Aljasir 2010
- Aljasir B, Bryson M, Al‐Shehri B. Yoga practice for the management of type II diabetes mellitus in adults: a systematic review. Evidence‐based Complementary and Alternative Medicine 2010;7(4):399‐408. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bera 1993
- Bera TK, Rajapurkar MV. Body composition, cardiovascular endurance and anaerobic power of yogic practitioner. Indian Journal of Physiology and Pharmacology 1993;37(3):225‐8. [PubMed] [Google Scholar]
BHF 2012
- British Heart Foundation. Our Heart Disease Facts. http://www.bhf.org.uk/media/news‐from‐the‐bhf/bhf‐facts.aspx (accessed 29 March 2012).
Bosch 2009
- Bosch PR, Traustadottir T, Howard P, Matt KS. Functional and physiological effects of yoga in women with rheumatoid arthritis: a pilot study. Alternative Therapies in Health and Medicine 2009;15(4):24‐31. [PubMed] [Google Scholar]
Carrico 2012
- Carrico M. The Branches of Yoga from Yoga Journal's Yoga Basics. http://www.yogajournal.com/basics/157 (accessed 26 June 2012).
Cook 2014
- Cook J. Not All Yoga Is Created Equal. http://www.yogajournal.com/basics/165 (accessed 7/5/14).
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Emberson 2004
- Emberson J, Whincup P, Morris R, Walker M, Ebrahim S. Evaluating the impact of population and high‐risk strategies for the primary prevention of cardiovascular disease. European Heart Journal 2004;25(6):484‐91. [DOI] [PubMed] [Google Scholar]
Ernst 2008
- Ernst E, Pittler MH, Wider B, Boddy K. Oxford Handbook of Complementary Medicine. Oxford: Oxford University Press, 2008. [Google Scholar]
Feuerstein 2011
- Feuerstein G. The Path of Yoga: An Essential Guide to its Principles and Practices. 2nd Edition. Boston: Shambhala Publications Inc, 2011. [Google Scholar]
Frishman 2005
- Frishman WH, Weintraub MI, Micozzi MS. Complementary and Integrative Therapies for Cardiovascular Disease. St Louis, Mo: Elsevier/Mosby, 2005. [Google Scholar]
Granath 2006
- Granath J, Ingvarsson S, Thiele U, Lundberg U. Stress management: a randomized study of cognitive behavioural therapy and yoga. Cognitive Behaviour Therapy 2006;35(1):3‐10. [DOI] [PubMed] [Google Scholar]
Groessl 2008
- Groessl EJ, Weingart KR, Aschbacher K, Pader L, Naxi S. Yoga for veterans with chronic low‐back pain. Journal of Alternative and Complementary Medicine 2008;14(9):1123‐9. [DOI] [PubMed] [Google Scholar]
Hagins 2007
- Hagins M, Moore W, Rundle A. Does practicing Hatha yoga satisfy recommendations for intensity of physical activity which improves and maintains health and cardiovascular fitness?. BMC Complementary and Alternative Medicine 2007;7(40):1‐9. [DOI: 10.1186/1472-6882-7-40] [DOI] [PMC free article] [PubMed] [Google Scholar]
Harder 2012
- Harder H, Parlour L, Jenkins V. Randomised controlled trials of yoga interventions for women with breast cancer: a systematic literature review. Supportive Care in Cancer 2012;20(12):3055‐64. [DOI] [PubMed] [Google Scholar]
Hewitt 2001
- Hewitt J. The Complete Yoga Book. New York: Schocken Books Inc, 2001. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. The Cochrane Collaboration.
Innes 2005
- Innes K, Bourguignon C, Taylor A. Risk indices associated with the insulin resistance syndrome, cardiovascular disease and possible protection with yoga: a systematic review. Journal of the American Board of Family Medicine 2005;18(6):491‐519. [DOI] [PubMed] [Google Scholar]
Innes 2007
- Innes KE, Vincent HK. The influence of yoga based programmes on risk profiles in adults with type 2 diabetes mellitus: a systematic review. Evidence Based Complementary and Alternative Medicine 2007;4(4):469‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kappmeier 2006
- Kappmeier KL, Ambrosini DM. Instructing Hatha Yoga. Champaign, IL: Human Kinetics, 2006. [Google Scholar]
Khalsa 2004
- Khalsa SBS. Treatment of chronic insomnia with yoga: a preliminary study with sleep‐wake diaries. Applied Psychophysiology and Biofeedback 2004;29(4):269‐78. [DOI] [PubMed] [Google Scholar]
Koay 2009
- Koay J, Barenholtz T. The Science and Philosophy of Teaching Yoga and Yoga Therapy. USA: SUNYOGA/YogaSense, 2009. [Google Scholar]
Lau 2012
- Lau HLC, Kwong JSW, Yeung F, Chau PH, Woo J. Yoga for secondary prevention of coronary heart disease. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD009506] [DOI] [PubMed] [Google Scholar]
Lavey 2005
- Lavey R, Sherman T, Muesser KT, Osborne DD, Currier M, Wolfe R. The effects of yoga on mood in psychiatric inpatients. Psychiatric Rehabilitation Journal 2005;28(4):399‐402. [DOI] [PubMed] [Google Scholar]
Lavie 2009
- Lavie C, Thomas R, Squies R, Allison T, Milani R. Exercise training and cardiac rehabilitation in primary and secondary prevention of coronary heart disease. Mayo Clinic Proceedings 2009;84(4):373‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levine 2000
- Levine M. The Positive Psychology of Buddhism and Yoga: Paths to a Mature Happiness: with a Special Application to Handling Anger. Mahwah, NJ: Lawrence Erlbaum Publishers, 2000. [Google Scholar]
Madanmohan 2004
- Madanmohan, Udupa K, Bhavanani AB, Shatapathy C, Sahai A. Modulation of cardiovascular response to exercise by yoga training. Indian Journal of Physiology and Pharmacology 2004;48(4):461‐5. [PubMed] [Google Scholar]
Mendelson 2008
- Mendelson D. Metabolic Syndrome and Psychiatric Illness: Interactions, Pathophysiology, Assessment and Treatment. Amsterdam, Boston: Elsevier/Academic Press, 2008. [DOI] [PubMed] [Google Scholar]
Michalsen 2005
- Michalsen A, Grossman P, Acil A, Langhorst J, Ludtke R, Esch T, et al. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three‐month intensive yoga program. Medical Science Monitor 2005;11(12):555‐61. [PubMed] [Google Scholar]
Mittal 2008
- Mittal S. The Metabolic Syndrome in Clinical Practice. London: Springer, 2008. [Google Scholar]
Muralidhara 1982
- Muralidhara DV, Ranganathan KV. Effect of yoga practice on cardiac recovery index. Indian Journal of Physiology and Pharmacology 1982;26:279‐83. [PubMed] [Google Scholar]
Murugesan 2000
- Murugesan R, Govindarajalu N, Bera TK. Effect of selected yoga practices in the management of hypertension. Indian Journal of Physiology and Pharmacology 2000;44:207‐10. [PubMed] [Google Scholar]
Nüesch 2010
- Nüesch E, Trelle S, Reichenbach S, Rutjes AW, Tschannen B, Altman DG, et al. Small study effects in meta‐analyses of osteoarthritis trials: meta‐epidemiological study. BMJ 2010;341:c3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patel 2012
- Patel NK, Newstead AH, Ferrer RL. The effects of yoga on physical functioning and health related quality of life in older adults: a systematic review and meta‐analysis. Journal of Alternative and Complementary Medicine 2012;18(10):902‐17. [DOI] [PubMed] [Google Scholar]
Perk 2012
- Perk J, Backer G, Gohlke H, Graham I, Reiner Z, Verschuren WM, et al. European guidelines on cardiovascular disease prevention in clinical practice: full text. The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). European Heart Journal 2012; Vol. 33:1635–1701. [http://www.escardio.org/guidelines‐surveys/esc‐guidelines/GuidelinesDocuments/guidelines‐CVD‐prevention.pdf] [DOI] [PubMed]
Riley 2004
- Riley D. Hatha yoga and the treatment of illness. Alternative Therapies in Health and Medicine 2004;10(2):20‐1. [PubMed] [Google Scholar]
Ripoll 2002
- Ripoll E, Mahowald D. Hatha yoga therapy management of urologic disorders. World Journal of Urology 2002;20:306‐9. [DOI] [PubMed] [Google Scholar]
Saper 2004
- Saper RB, Eisenberg DM, Davis RB, Culpepper L, Phillips RS. Prevalence and patterns of adult yoga use in the United States: results of a national survey. Alternative Therapies in Health and Medicine 2004;10(2):44‐9. [PubMed] [Google Scholar]
Simpkins 2003
- Simpkins CA, Simpkins A. Yoga Basics. North Clarendon: Tuttle Publishing, 2003. [Google Scholar]
Singh 2004
- Singh S, Malhotra V, Singh KP, Madhu SV, Tandon OP. Role of yoga in modifying certain cardiovascular functions in type 2 diabetic patients. Journal of the Association of Physicians of India 2004;52:203‐6. [PubMed] [Google Scholar]
Sterne 2000
- Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta‐analysis: power of statistical tests and prevalence in the literature. Journal of Clinical Epidemiology 2000;53:1119‐29. [DOI] [PubMed] [Google Scholar]
Sterne 2001
- Sterne JA, Egger M, Smith GD. Systematic reviews in health care: investigating and dealing with publication and other biases in meta‐analysis. BMJ 2001;323:101‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
USHHS 1996
- US Department of Health and Human Services. Physical Activity and Health: A report of the Surgeon General. Atlanta GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, 1996. [Google Scholar]
WHO 2003
- World Health Organization. The World Health Report: 2003: Shaping the Future. Switzerland: World Health Organization, 2003. [Google Scholar]
WHO 2011
- World Health Organization. Media Centre: Cardiovascular Diseases (CVDs). http://www.who.int/mediacentre/factsheets/fs317/en/index.html (accessed 29 March 2012).
WHO 2011a
- World Health Organization. Noncommunicable diseases and mental health. http://www.who.int/nmh/countries/en/index.html (accessed 26 June 2012).
Woodyard 2011
- Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. International Journal of Yoga 2001;4:49‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Woolery 2004
- Woolery A, Myers H, Sternlieb B, Zeltzer L. A yoga intervention for young adults with elevated symptoms of depression. Alternative Therapies in Health and Medicine 2004;10(2):60‐3. [PubMed] [Google Scholar]


