Abstract
Objective
Patients with chronic obstructive pulmonary disease (COPD) commonly present with cardiovascular disease (CVD). We investigated the association between COPD exacerbations and major cardiovascular (CV) events in a COPD population with a history of CVD.
Methods
This population-based and register-based cohort study identified all Danish COPD patients aged ≥40 years who visited a hospital-based, pulmonary outpatient clinic for COPD between 1st January, 2010, and 31st December, 2016, from a nationwide COPD registry. Patients with a history of a major CV event 36‒6 months prior to their COPD measurement date and no CV event 6 months before this date were included. During a 6-month assessment period, the risks of a new CV event (hospitalization with fatal/non-fatal stroke, myocardial infarction, or heart failure) and moderate and severe COPD exacerbations were evaluated. Odds ratios with 95% confidence intervals for CV events and death were estimated using adjusted logistic regression models.
Results
Of the 1501 COPD patients included, 55% experienced a COPD exacerbation and 13% experienced both an exacerbation and a CV event during follow-up (6 months). The odds of a CV event were 1.5 times higher in patients with a moderate exacerbation and more than 6-times higher in those with a severe exacerbation vs patients with no exacerbation(s). The majority of CV events occurred within 30 days post exacerbation in patients who experienced both an exacerbation and a CV event. In total, 113 patients died during the study period: 28% of deaths were caused by CVD and 72% by reasons other than CVD, mostly COPD.
Conclusion
In patients with known CVD, severe COPD exacerbations are associated with increased odds of major CV events that occur within 30 days post exacerbation, highlighting the need to prevent exacerbations in COPD patients with concomitant CVD to potentially improve both respiratory and CV health.
Keywords: concomitant cardiovascular disease, respiratory health, cardiovascular health, prevention, real-world evidence
Introduction
Chronic obstructive pulmonary disease (COPD) is a heterogeneous and progressive disease affecting approximately 384 million people worldwide.1 Multimorbidity is prevalent in people with COPD. Cardiovascular disease (CVD) is particularly common and associated with an increased risk of hospitalization and mortality.2,3 In fact, COPD has been associated with a 2‒3-fold increase in the risk of CVD (congestive heart failure, coronary artery disease, ischemic stroke, and arrhythmias) independent of age, sex, smoking history, and other confounders and cardiovascular death in general occurs in approximately 30% of COPD patients.4
Of all the comorbidities associated with COPD, interactions between the cardiovascular system and COPD are of particular interest since this interplay could lead to fatal outcomes. Individuals with both COPD and CVD experience worse clinical outcomes than those with either COPD or CVD as regards quality of life, dyspnea, exercise tolerance,5 and the risk of hospitalization and mortality.6 Compared to individuals without COPD, those with COPD have a 50% increased risk of stroke,7 a 40% increased risk of acute myocardial infarction,8 and an increased risk of heart failure (pooled odds ratio, OR 2.57),9 suggesting a vulnerable population of patients. The natural history of COPD in many individuals is characterized by acute exacerbations, which can increase the negative impact on the cardiovascular system in individuals with risk factors for or diagnosed with CVD.10 Studies have shown the relationship between acute exacerbations and cardiovascular events in the vicinity of exacerbation.6,10,11
The relationship between CVD and exacerbations of COPD, however, is less defined,7,12 particularly in a real-world setting, where, to our knowledge, real-world data examining the association between COPD exacerbations and major cardiovascular events in a COPD population with a history of CVD are either not available or have not been broadly examined. While these diseases may share both mechanistic and biochemical pathways, many factors may be at play.7 Moreover, novel therapies are lacking to target CVD in COPD patients, least of all to reduce the number of premature deaths, as well as dedicated guidelines for these patients (and CVD patients with COPD) that require high-quality evidence.7 The aim of our study, therefore, was to investigate the association between acute COPD exacerbations and severe acute cardiovascular (CV) events in a vulnerable COPD population with a history of CVD using a large and comprehensive, real-world population database.
Methods
Study Design and Data Sources
In this population-based cohort study, data from several comprehensive national Danish health registries were linked: the National Hospital Registry covering all inpatient hospitalizations since 1977 and all outpatient visits since 1995 with mandatory registration by the treating physician; the National COPD Registry, including all COPD patients followed in outpatient specialist clinics in Denmark since 2008; the National Prescription Registry, including all prescriptions redeemed at pharmacies since 1995 using anatomical therapeutic chemical (ATC) codes; the Civil Registration System for information on vital status, migration, and cohabitation; and, the Cause of Death Registry. Data linkage was performed by Statistics Denmark using an individual’s personal identification number, and data were pseudo-anonymized before analysis. This study is purely registry-based, and all micro-data is anonymized, so no informed consent was needed. According to Danish law, no ethical approval is required for register research, data access was approved and delivered by Statistics Denmark (project number 704,702). All analyses were performed at a secure research infrastructure server at Statistics Denmark, which has been set up to comply with the General Data Protection Regulation (GDPR) and the Danish Data Protection Agency guidelines for research on sensitive data.
Study Population
This study included all Danish patients with COPD (age ≥40 years) who had visited a hospital-based, pulmonary outpatient clinic due to COPD between 1st January, 2010, and 31st December, 2016, and all of whom had an ICD-10 code J43 or J44. The first visit at which a complete set of clinical measurements (modified Medical Research Council [mMRC], forced expiratory flow [FEV1], body mass index [BMI], and smoking history) was registered, was regarded as the COPD measurement date (index date/baseline; defined as “COPD measurement” from here on in). Patients with incomplete measurements were excluded from the data set to avoid missing data (Supplementary Figure 1). To be eligible for inclusion, patients had to have a history of CVD defined as having experienced a major CV event (hospitalization with primary diagnosis of stroke [ICD-10 code I61‒I64], myocardial infarction [I21], or heart failure [I50]) during the 36‒6-month period prior to COPD measurement. Patients experiencing a CV event within 6 months prior to this date were excluded to avoid potential misclassification of endpoints, eg, the recording of a follow-up or late discharge date of a previous CV event rather than a new CV event (Supplementary Figure 1).
Cardiovascular Events and Mortality
Cardiovascular events were defined as requiring hospitalization with a primary diagnosis of fatal/non-fatal stroke (ICD-10 code I61‒I64), myocardial infarction (I21), or heart failure (I50). Cardiovascular death was defined as ICD-10 codes I00‒I99 as the cause of death. Death due to causes other than CVD included all causes of death reported using ICD-10 main codes during the follow-up period, excluding CV events.
The risk of fatal and non-fatal CV events or death due to any cause other than CVD during a 6-month prospective follow-up period starting from COPD measurement was evaluated in COPD patients with a history of a major CV event (Supplementary Figure 2).
Chronic Obstructive Pulmonary Disease Exacerbations
Moderate exacerbations were defined as redeeming a course of oral corticosteroids (OCS) (a maximum of 20 defined daily doses of 25 mg prednisolone [ATC code H02AB06] or prednisone [ATC code H02AB07]) with or without concomitant prescription of antibiotics. If patients collected more than one package of OCS on the same day, the event was still classed as one exacerbation.
Severe exacerbations were defined as a) hospitalizations or emergency visits with ICD-10 code J40–44 as the primary diagnosis or b) J13–18 (pneumonia) or J96 (respiratory insufficiency) as the primary diagnosis in combination with a secondary diagnosis of J40–44 as coded in the National Hospital Registry. Recurrent exacerbations within 28 days were considered to be one exacerbation. Patients with both a moderate and a severe exacerbation within 28 days were classed as having a severe exacerbation (the start date was designated as the date of the first occurring exacerbation).
All patients were retrospectively evaluated to determine their exacerbation history during a 6-month period before occurrence of the event of interest (a fatal/non-fatal CV event, death from causes other than CVD, or from the end of the assessment window for patients still alive and with no event). This design ensured that all patients had a 6-month period where exacerbation history, as well as timely clinical information, was captured retrospectively (Supplementary Figure 2).
Statistical Analyses
The clinical baseline measurements of COPD, including mMRC, FEV1, BMI, and smoking history, were assessed at COPD measurement and are reported as means (standard deviation [SD]) for continuous variables and absolute and relative frequencies for categorical variables. Prescribed COPD medications collected from pharmacies were assessed during the 6-month period prior to COPD measurement and presented as absolute and relative frequencies to ensure that all relevant combinations of COPD medication usage were captured. Respiratory antibiotics, OCS, and CVD medications were assessed 12 months before COPD measurement.
Patients were stratified into the following groups: 1) no CV event + no exacerbation; 2) no CV event + exacerbation; 3) fatal/non-fatal CV event + no exacerbation; 4) fatal/non-fatal CV event + exacerbation; and, 5) death due to non-CV event. To explore the association between COPD exacerbations and odds (with corresponding 95% confidence intervals) of CV events or death due to other causes than CVD we use multivariate logistic regression models were applied to estimate ORs with 95% confidence intervals (CIs) for CV events and death, adjusted for age, gender, BMI, mMRC, FEV1, exacerbation history, smoking, diabetes medication, and cohabitation status. Additionally, the number of days from hospital discharge for the most recent exacerbation until a severe CV event (fatal/non-fatal) occurred, stratified by any exacerbation and severe exacerbations, respectively, were assessed descriptively.
Results
A total of 2869 patients with both COPD and a history of major CV events 36 months prior to COPD measurement were identified. Of these, 1368 experienced a CV event in the 6-month period prior to COPD measurement and were excluded, leaving a study population of 1501 patients with COPD (mean age 73.5 years, 42% female) (Table 1, Supplementary Figure 2). A total of 81 (5.4%) patients died during the 6-month follow-up period due to causes other than CVD.
Table 1.
Patient Characteristics Assessed at COPD Measurement
| n | % | |
|---|---|---|
| Patients | 1501 | |
| Females | 632 | 42.1 |
| Mean age (years, SD) | 73.5 (9.2) | |
| mMRC | ||
| 1 | 75 | 5.0 |
| 2 | 280 | 18.7 |
| 3 | 449 | 29.9 |
| 4 | 402 | 26.8 |
| 5 | 288 | 19.2 |
| FEV1 | ||
| ≥80 | 69 | 4.6 |
| 50‒79 | 634 | 42.2 |
| 30‒49 | 578 | 38.5 |
| 1‒29 | 218 | 14.5 |
| BMI | ||
| <18.5 | 105 | 7.0 |
| 18.5‒24 | 526 | 35.0 |
| 25‒29 | 463 | 30.8 |
| 30‒34 | 256 | 17.1 |
| 35+ | 151 | 10.1 |
| Smoking status | ||
| Previous smoker | 978 | 65.2 |
| Smoking | 456 | 30.4 |
| Never smoked | 67 | 4.4 |
Notes: COPD measurement (date of COPD measurement/baseline) represented the study index date, ie, the date of a patient’s first visit at which a complete set of clinical measurements (mMRC, FEV1, BMI, and smoking history) was registered.
Abbreviations: BMI, body mass index; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory flow; mMRC, modified Medical Research Council; SD, standard deviation.
At the time of COPD measurement, 75% of patients had a mMRC ≥3; over half (53%) had a FEV1 <50%, the majority (58%) had a BMI ≥25; and, almost all were smokers (30%) or previous smokers (65%) (Table 1).
Prior to COPD measurement, most patients had redeemed a prescription for at least one CVD medication: 96% collected anti-hypertensives, almost 70% collected anti-dyslipidemia drugs, and 30% collected anticoagulants. Inhaled maintenance COPD treatments were collected by 80.1% of patients, including long-acting beta-2-agonists (LABAs) and/or long-acting muscarinic antagonists (LAMAs) (16.5%), and inhaled corticosteroids (ICS), LABAs and LAMAs (42.8%). Oral corticosteroids were collected by 41.4% of patients and respiratory antibiotics by 69.6% (Table 2).
Table 2.
Medication Collected by Patients from Pharmacy
| Prescription Drugs | All | |
|---|---|---|
| n | % | |
| Inhaled COPD medications (6 months prior to COPD measurement) | ||
| ● LAMAs | 147 | 9.8 |
| ● LABAs | 33 | 2.2 |
| ● ICS | 32 | 2.1 |
| ● LABAs + LAMAs | 67 | 4.5 |
| ● LABAs + ICS | 281 | 18.7 |
| ● LABAs + LAMAs + ICS | 643 | 42.8 |
| ● SABAs | 40 | 2.7 |
| ● SABAs and other R03a medication | 7 | 0.5 |
| ● Other R03a medication | 19 | 1.3 |
| ● No inhaled COPD medication | 232 | 15.5 |
| Other COPD treatments (12 months prior to COPD measurement) | ||
| ● Respiratory antibioticsb | 1044 | 69.6 |
| ● OCS | 622 | 41.4 |
| CVD medication (12 months prior to COPD measurement) | ||
| ● Anti-dyslipidemics | 1040 | 69.3 |
| ● Antihypertensives | 1445 | 96.3 |
| ● Antiplatelets | 1089 | 72.6 |
| ● Anticoagulants | 457 | 30.4 |
| ● Other CV medication | 451 | 30.0 |
| ● Diabetes medication | 354 | 23.6 |
Notes: aR03: R03AL01, R03AL02, R03CC02, R03CC03, R03CC12, R03DA04; bRespiratory antibiotics: amoxicillin and enzyme inhibitor (ATC-code J01CR02), amoxicillin (J01CA04), pivampicillin (J01CA02), phenoxymethylpenicillin (J01CE02), macrolides (J01FA01, J01FA06, J01FA09, J01FA10).
Abbreviations: COPD, chronic obstructive pulmonary disease; CV, cardiovascular; ICS, inhaled corticosteroids; LABA, long-acting beta-2-agonist; LAMA, long-acting muscarinic antagonist; OCS, oral corticosteroids; SABA, short-acting beta-2-agonist.
During the retrospective assessment period, a total of 820 (55%) patients experienced a moderate or severe COPD exacerbation and 267 (17.8%) experienced a fatal/non-fatal CV event during the study period (Table 3). Overall, 197 (13.1%) of included patients experienced both an exacerbation and a CV event, 70 (4.7%) a CV event without an exacerbation, 556 (37%) an exacerbation without a CV event, and 597 (39.8%) had neither an exacerbation nor a CV event (Table 3). Of the patients who experienced both a CV event and an exacerbation, more had a severe exacerbation (66.0%), whereas the proportion of patients with moderate exacerbations was higher in the no CV event + exacerbation group (79.3%) (Table 3).
Table 3.
Exacerbations of COPD and Fatal or Non-Fatal CV Events During the Assessment Period
| All Patients | ||||
|---|---|---|---|---|
| n | % | Meanb | SD | |
| N | 1501 | 100.0 | ||
| No CV event + no exacerbation | 597 | 39.8 | ||
| No CV event + exacerbationa | 556 | 37.0 | ||
| Moderate exacerbation | 441 | 79.3 | 1.1 | 0.8 |
| Severe exacerbation | 175 | 31.5 | 0.4 | 0.6 |
| CV event + no exacerbation | 70 | 4.7 | ||
| Fatal CV event | 10 | 14.3 | ||
| Heart failure | 38 | 54.3 | ||
| Stroke | 11 | 15.7 | ||
| Myocardial infarction | 11 | 15.7 | ||
| CV event + exacerbationa | 197 | 13.1 | ||
| Moderate exacerbation | 126 | 64.0 | 0.9 | 0.8 |
| Severe exacerbation | 130 | 66.0 | 0.9 | 0.8 |
| Fatal CV event | 22 | 11.2 | ||
| Heart failure | 124 | 62.9 | ||
| Stroke | 28 | 14.2 | ||
| Myocardial infarction | 23 | 11.7 | ||
| Death due to non-CV event | 81 | 5.4 | ||
| No exacerbation before death | 14 | 17.3 | ||
| Exacerbation before death | 67 | 82.7 | 1.6 | 1.0 |
Notes: aExcluding exacerbations that occur before death from causes other than a CV event (n=67). CV events and mortality were assessed prospectively while exacerbations were assessed retrospectively. bMean refers to the mean number of exacerbations per patient in our study, taking into account all patients (with and without exacerbations).
Abbreviations: COPD, chronic obstructive pulmonary disease; CV, cardiovascular; SD, standard deviation.
In total, 113 patients died during the assessment period, with 32 (28.3%) deaths due to CVD and the remaining 81 (71.7%) deaths were attributed to reasons than other CVD (Table 3), mostly COPD (59%).
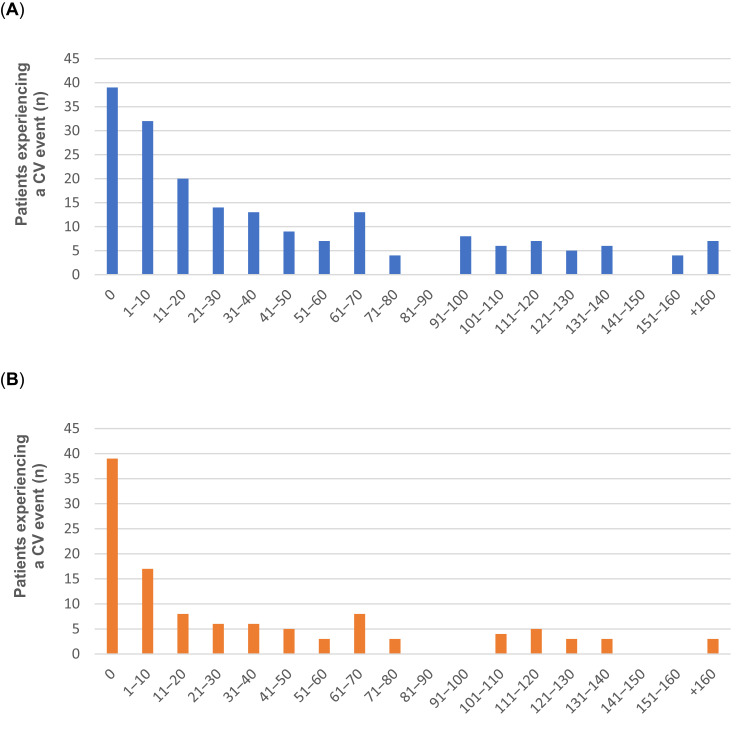
More than half of the patients (53.3%) had a CV event within 30 days after experiencing a moderate or severe COPD exacerbation (Figure 1A), and almost two-thirds (59.3%) had a CV event within 30 days after experiencing a severe exacerbation (Figure 1B).
Figure 1.
Duration (days) from hospital discharge for the most recent COPD exacerbation to severe CV event (fatal/non-fatal) for (A) any exacerbations in a total of 197 patients, and for (B) severe exacerbations only in a total of 118 patients. Duration (days) from hospital discharge for the most recent COPD exacerbation. In both instances (A and B), fewer than three observations were not reported, and Day 0 indicates that both the COPD exacerbation and the CV event occurred during the same hospital stay. Duration (days) from hospital discharge for the most recent COPD exacerbation.
Abbreviations: COPD, chronic obstructive pulmonary disease; CV, cardiovascular.
The odds of having a CV event (fatal/non-fatal) after a moderate exacerbation were 1.5 (OR; 95% CI: 1.0‒2.1) and 6.4 (OR; 95% CI: 4.5‒9.1) after a severe exacerbation vs patients with no exacerbations. Furthermore, the odds of dying due to reasons other than CVD after a moderate exacerbation were 1.4 (OR; 95% CI: 0.6‒3.0) and 11.2 (OR; 95% CI: 6.0‒21.1) after a severe exacerbation (Table 4). The odds of having a non-fatal CV event after a moderate exacerbation were 1.5 (OR; 95% CI: 1.0‒2.2) and 6.9 (OR; 95% CI: 4.8‒10.0) after a severe exacerbation, and the odds of a fatal CV event were 1.4 (OR; 95% CI: 0.6‒3.5) and 3.9 (OR; 95% CI: 1.6‒9.1) after a moderate and severe exacerbation, respectively.
Table 4.
Multivariate Logistic Regression Model of CV Events (Fatal and Non-Fatal) or Death Due to a Cause Other Than a CV Event
| Parameter | CV Event (Fatal and Non-Fatal) | Death Due to Other Cause | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | CI 95% | P-value | OR | CI 95% | P-value | |||
| LCL | UCL | LCL | UCL | |||||
| Severe exacerbation | 6.4 | 4.5 | 9.1 | <0.0001 | 11.2 | 6.0 | 21.1 | <0.0001 |
| Moderate exacerbation only | 1.5 | 1.0 | 2.1 | 0.0338 | 1.4 | 0.6 | 3.0 | 0.4548 |
| No exacerbation | Ref. | |||||||
| FEV1 <50 severe‒very severe | 0.8 | 0.6 | 1.1 | 0.2771 | 1.7 | 0.9 | 3.1 | 0.0734 |
| FEV1 50+ mild‒moderate | Ref. | |||||||
| mMRC high 3‒5 | 1.3 | 0.9 | 1.9 | 0.1539 | 3.0 | 1.2 | 7.9 | 0.0226 |
| MRC low 1‒2 | Ref. | |||||||
| BMI <18.5 | 1.2 | 0.6 | 2.1 | 0.6463 | 3.2 | 1.6 | 6.5 | 0.0012 |
| BMI 25‒29 | 1.0 | 0.7 | 1.4 | 0.9553 | 0.5 | 0.3 | 1.0 | 0.0573 |
| BMI 30‒34 | 0.7 | 0.5 | 1.1 | 0.1654 | 0.3 | 0.1 | 0.8 | 0.0105 |
| BMI 35+ | 0.8 | 0.5 | 1.4 | 0.4624 | 0.5 | 0.2 | 1.4 | 0.1927 |
| BMI 18.5‒24 | Ref. | |||||||
| Smoking | 1.1 | 0.8 | 1.5 | 0.7174 | 1.2 | 0.7 | 2.1 | 0.4828 |
| Never smoked | Ref. | |||||||
| Diabetes medication 1-year prior to COPD measurementa | 1.4 | 1.0 | 1.9 | 0.0556 | 2.1 | 1.2 | 3.7 | 0.0111 |
| Age | 1.0 | 1.0 | 1.0 | 0.5064 | 1.0 | 1.0 | 1.1 | 0.1169 |
| Female | 0.7 | 0.5 | 0.9 | 0.0073 | 0.6 | 0.4 | 1.0 | 0.0701 |
| Cohabitation status | 1.0 | 0.7 | 1.3 | 0.7821 | 0.6 | 0.3 | 1.0 | 0.0441 |
Notes: aCOPD measurement (baseline) represented the study index date, ie, the date of a patient’s first visit at which a complete set of clinical measurements (mMRC, FEV1, BMI, and smoking history) was registered, Diabetes medication; ICD-10 code A10.
Abbreviations: BMI, body mass index; CI, confidence interval; CV, cardiovascular; FEV1, forced expiratory flow; mMRC, modified Medical Research Council; LCI, lower confidence limit; UCI, upper confidence limit.
Discussion
In this nationwide, observational study of patients with COPD and a history of CVD in Denmark, we found that over half of all patients experienced a COPD exacerbation during a 6-month follow-up. Of these, more than 50% experienced a major CV event within a 30-day post-exacerbation period. The adjusted odds of experiencing a major CV event were 6.4 times higher in patients with a severe exacerbation and 1.5 times higher in those with a moderate exacerbation vs patients without COPD exacerbation. Almost all patients had collected one or more types of CVD medication, whereas one in five had no collection of inhaled COPD maintenance medication during the 6-month period prior to COPD measurement.
Our comprehensive and novel, real-world data both confirm and advance increasing evidence supporting the association of COPD exacerbations with major CV events. Post hoc analysis of the SUMMIT study, a randomized clinical trial in patients with COPD, showed that the risk of CV events (eg, death from CVD, myocardial infarction, and stroke) after an acute COPD exacerbation was increased, particularly in the first 30 days post exacerbation.10 A four-fold greater hazard ratio within 30 days after any exacerbation and a 10-fold increased hazard ratio after a severe exacerbation with an elevated risk up to 1 year after exacerbation was reported.10 Moreover, a recent report from Denmark showed that the risk of major adverse cardiac events (MACE) increases almost four-fold following acute exacerbation onset compared to periods without exacerbations in the same individuals (OR: 3.70; 95% CI: 3.60–3.80).11 In a large, population-based COPD study, Goto et al13 showed that acute COPD exacerbations were associated with increased 30-day and 1-year incidences of an acute CV event. Furthermore, a systematic literature review of seven studies found an increased risk of CV events after a COPD exacerbation, although none of these were deemed eligible for meta-analysis.14
Interestingly, in our study, 55% of patients experienced a COPD exacerbation during a 6-month follow-up period, which reflects that we investigated a select and very vulnerable population of COPD patients with a history of CVD. This exacerbation rate is slightly higher than reported by Hurst et al15 and may be explained by the higher mMRC, higher age, and lower FEV1 percentage of patients in our study indicating a vulnerable population compared to those in the study of Hurst et al.15 Since COPD and CVD share common risk factors, including smoking, sedentary lifestyle, and unhealthy diet, they frequently occur together. Established cardiovascular disease and risk factors of CVD, such as ischemic heart disease, diabetes, or atrial fibrillation, are the most common comorbidities in COPD. Besides the progression of COPD over time, even CVD becomes more prevalent with increasing COPD severity and advancing age,16 suggesting a negative bidirectional interaction between COPD and CV conditions. In one study in 476 patients hospitalized for severe exacerbation, 43% had echocardiographic-confirmed heart failure and around 50% were previously undiagnosed and untreated.17 There is currently no routine to screen for CVD in patients with COPD and the value of screening—especially in an outpatient setting—may lie in identifying this vulnerable population.
Moreover, several mechanisms may link COPD, and particularly COPD exacerbations, with a high risk of CV events. In addition to hypoxemia that may occur during an exacerbation, negative mechanical CV effects, and a prothrombotic inflammatory state are plausible explanations.18–20 Static and dynamic hyperinflation during exacerbation leads to increased intrathoracic pressure, which compromises ventricular filling. Tachycardia and hypertension during an exacerbation increase cardiac afterload. All these factors reduce the ejection fraction. Additionally, acute exacerbations of COPD are characterized by increasing pulmonary inflammation that can “spill over” into the systemic circulation and trigger MACE. Mediators include pro-inflammatory cytokines, such as tumor necrosis factor α and interleukins 1, 6, and 8. These promote a systemic inflammatory and prothrombotic state with increased levels of fibrinogen and C-reactive protein that activate the vascular endothelium and platelets, triggering endothelial dysfunction and rupture of susceptible plaques.18–20 Short courses of oral corticosteroids at a daily dose of 40 mg prednisolone equivalent for 5‒7 days are routine in the treatment of acute exacerbations. However, Bazell et al21 have shown that treatment with daily doses of over 1000 mg prednisolone equivalent was associated with a higher incidence of events that may be OCS-related, including CVD and heart failure. While we lack data on the total accumulated OCS doses, it is possible that patients in our study receiving large doses of steroids to treat acute COPD could have contributed to our results.
In our study, 15.5% of COPD patients did not collect inhaled maintenance COPD treatment from the pharmacy during the 6-month period prior to COPD measurement. We have reported previously on inhaled maintenance medication under-treatment in COPD patients classified as GOLD Group B, where almost one-third was untreated.22 In fact, studies from Sweden have shown that a considerable proportion of subjects at high risk of exacerbations did not receive treatment to prevent future exacerbations23 and that approximately 35% of COPD patients hospitalized due to a severe exacerbation were not on maintenance inhalation treatment during the year before exacerbation onset, with a substantial proportion (40%) continuing without treatment after discharge.24 Furthermore, a substantial proportion of patients on maintenance bronchodilation treatment alone continued with unchanged treatment 1 year after discharge.24 Under-treatment and under-management of patients with COPD have also been described by Sandelowsky et al,25 where only one-third of patients had a follow-up visit after a severe COPD exacerbation. Under-treatment and delay in drug optimization after an exacerbation may be explained by various reasons, such as patient and doctor behavior or organizational barriers between primary and secondary care. While inadequate/incorrect risk-characterization of COPD combined with fear of adverse events associated with inhaled medications may lead to under-treatment of patients with COPD and consequently increase the risk of exacerbations,20 comorbid CVD is itself an independent risk factor for patients experiencing COPD exacerbations.16,26 Clearly, there are issues with both under- and over-treatment in this population and further studies exploring the use of ICS in COPD are warranted.
Several studies advocate a rationale for screening and monitoring of patients with COPD to detect CVD and thus reduce the risk of future CV outcomes.3,12,20 Our study also suggests that there is a need to optimize COPD treatment to avoid exacerbations and, potentially, CV events. We do not have data to confirm if these patients are adequately treated for their CVD, but our study indicates that there is room to improve their COPD treatment. The lack of relevant COPD treatment in particular is highly problematic because the benefits of relevant inhalation treatment, including a reduced rate of exacerbations, have been demonstrated.27–31 We do not know if the patients were prescribed inhalation medications but failed to collect them or if the medications were either not prescribed or unwanted by patients. Considering both the high collection rate of CV medications and reimbursement rate of patients’ pharmaceutical expenses in Denmark, however, the most likely explanation is under-treatment of COPD. Historically, GOLD D patients have received the most attention regarding future risk to prevent future exacerbations and death.1 The nationwide cohort study by Gedebjerg et al,32 however, showed that CVD-related mortality was equal in groups B and D, and more recent studies by Løkke et al22 and Marott et al33 showed that GOLD B patients with just one moderate exacerbation in the preceding year have a significantly higher risk of future exacerbations and death than those without exacerbations. Considering the high risk of both exacerbations and CV events, timely optimization of the treatment and care of patients with COPD is a clinical necessity, especially if patients have comorbid CVD or CV risk factors. Thus, the clinical implication of our study is that outpatient assessment of these high-risk patients in a joint venture (cardio-respiratory) is required to ensure optimal treatment with the aim of avoiding these devastating exacerbations.
High-quality, mandatory nationwide registry data, and personal identification numbers that allow linkage of individual data provide solid and unique data. They are major strengths of our study, as are the size of the COPD patient population and the relatively frequent outcomes of interest that we believe support sufficient power to report reliable effect estimates of the association between COPD exacerbations and odds of CV events or death due to other causes than CVD. Furthermore, using prospectively collected data reported by the treating physician reduced the risk of information bias, and the use of discharge diagnoses for COPD exacerbations and CV events reduced the risk of misclassification of diagnoses recorded at the admission to the hospital. Moreover, nationwide coverage and virtually complete follow-up limited selection bias.
Nevertheless, some limitations should be considered when interpreting the results. Excluding COPD patients with CV events in the 6 months prior to COPD measurement (the index date) could have introduced selection bias and thus limited the representativeness of findings. Additionally, data retrieval was limited to variables registered in the database and reported medications were based on prescription collections at pharmacy that do not necessarily reflect actual medication use. Moreover, our population was included when first assessed and potentially first diagnosed with COPD at the outpatient clinic, which partly explains why some had not purchased any COPD medication prior to inclusion. The diagnosis and treatment of COPD may have improved since our inclusion period (2010‒2016). The follow-up period for exacerbations and CV events was only 6 months; while this may be considered too short, we found that most CV events occurred within 30 days after exacerbation. Additionally, we were unable to disentangle the order of events in patients who experienced both a COPD exacerbation and a CV event during the same hospital admission (ie, Day 0 in Figure 1). Finally, the external validity of our findings, especially with regard to the high proportion of exacerbations and mortality, is limited to represent similar selected populations of COPD patients with a known history of major CV events (ie, stroke, MI, and heart failure during 36‒6 months prior to COPD diagnosis) and should not be extrapolated to all COPD patients.
Conclusion
In patients with known CVD, severe COPD exacerbations are associated with increased odds of major CV events, which occurred within 30 days post exacerbation in most patients. Furthermore, 15.5% COPD patients do not collect inhaled maintenance treatments, indicating under-treatment. COPD is a multisystem disease due to its common risk factors, namely smoking and patient lifestyle and behavior. COPD patients in a stable phase have an elevated cardiopulmonary risk. This study provides real-world evidence highlighting that prevention of exacerbations in patients with COPD and concomitant CVD may improve respiratory outcomes and prevent CV events. The heterogeneity and dynamic complexity of COPD and its comorbidities justify the need for better routine follow-up and a precision medicine approach aimed at improving patient assessment.
Acknowledgments
Dr Grażyna Söderbom, Klipspringer AB, is acknowledged for editorial support sponsored by AstraZeneca.
Funding Statement
This study and editorial support was sponsored by AstraZeneca.
Abbreviations
ATC, anatomical therapeutic chemical; BMI, body mass index; CI, confidence interval; COPD measurement, COPD measurement/index date, baseline; COPD, chronic obstructive pulmonary disease; CV, cardiovascular; CVD, cardiovascular disease; FEV1, forced expiratory flow; ICS, inhaled corticosteroids; LABA, long-acting beta-2-agonist; LAMA, long-acting muscarinic antagonist; MACE, major adverse cardiac events; mMRC, modified Medical Research Council; OCS, oral corticosteroids; OR, odds ratio; SABA, short-acting beta-2-agonist, SD, standard deviation.
Data Sharing Statement
The dataset supporting the conclusions of this article is available from public registries upon request and approval of access to national authorities.
Ethics Approval and Informed Consent
This study was performed in accordance with the Declaration of Helsinki, the International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use Good Clinical Practices, Good Pharmacoepidemiology Practice, and the applicable legislation on non-interventional studies and/or observational studies. All data accessed complied with relevant data protection and privacy regulations.
Consent for Publication
All authors have read and approve the final manuscript and consent to publish these data.
Author Contributions
All authors significantly contributed to the work reported in terms of study conception, design and execution or data acquisition, analysis, and interpretation or all of these areas; participated in drafting, revising, or critically reviewing the manuscript; approved the final manuscript for publication; agreed on the journal to which the manuscript was submitted; and, agreed to be accountable for all aspects of the work.
Disclosure
A.L., J.L., R.I., and O.H. report no conflict of interests with respect to this study. P.L. has participated in advisory boards for AstraZeneca, Boehringer Ingelheim, Chiesi, and GSK and has received research grants from AstraZeneca, Boehringer Ingelheim, and GSK. G.T. and G.S. are full-time employees of AstraZeneca. The authors report no other conflicts of interest in this work.
References
- 1.GOLD, Global Initiative for Chronic Obstructive Lung Disease [homepage on the Internet]. Global strategy for the diagnosis, management and prevention of COPD report; 2022. Available from: https://goldcopd.org. Accessed October 11, 2022.
- 2.Chetty U, McLean G, Morrison D, Agur K, Guthrie B, Mercer SW. Chronic obstructive pulmonary disease and comorbidities: a large cross-sectional study in primary care. Br J Gen Pract. 2017;67(658):e321–e328. doi: 10.3399/bjgp17X690605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andell P, Koul S, Martinsson A, et al. Impact of chronic obstructive pulmonary disease on morbidity and mortality after myocardial infarction. Open Heart. 2014;1(1):e000002. doi: 10.1136/openhrt-2013-000002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berry CE, Wise RA. Mortality in COPD: causes, risk factors, and prevention. COPD. 2010;7(5):375‒382. doi: 10.3109/15412555.2010.510160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller J, Edwards LD, Agustí A, et al. Comorbidity, systemic inflammation and outcomes in the ECLIPSE cohort. Respir Med. 2013;107(9):1376‒1384. doi: 10.1016/j.rmed.2013.05.001 [DOI] [PubMed] [Google Scholar]
- 6.Donaldson GC, Hurst JR, Smith CJ, Hubbard RB, Wedzicha JA. Increased risk of myocardial infarction and stroke following exacerbation of COPD. Chest. 2010;137(5):1091‒1097. doi: 10.1378/chest.09-2029 [DOI] [PubMed] [Google Scholar]
- 7.Morgan AD, Zakeri R, Quint JK. Defining the relationship between COPD and CVD: what are the implications for clinical practice? Ther Adv Respir Dis. 2018;12:1753465817750524. doi: 10.1177/1753465817750524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schneider C, Bothner U, Jick SS, Meier CR. Chronic obstructive pulmonary disease and the risk of cardiovascular diseases. Eur J Epidemiol. 2010;25(4):253‒260. doi: 10.1007/s10654-010-9435-7 [DOI] [PubMed] [Google Scholar]
- 9.Chen W, Thomas J, Sadatsafavi M, FitzGerald JM. Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(8):631‒639. doi: 10.1016/S2213-2600(15)00241-6 [DOI] [PubMed] [Google Scholar]
- 10.Kunisaki KM, Dransfield MT, Anderson JA, et al. Exacerbations of chronic obstructive pulmonary disease and cardiac events. a post hoc cohort analysis from the SUMMIT randomized clinical trial. Am J Respir Crit Care Med. 2018;198(1):51‒57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reilev M, Pottegård A, Lykkegaard J, Søndergaard J, Ingebrigtsen TS, Hallas J. Increased risk of major adverse cardiac events following the onset of acute exacerbations of COPD. Respirology. 2019;24(12):1183‒1190. doi: 10.1111/resp.13620 [DOI] [PubMed] [Google Scholar]
- 12.Ingebrigtsen TS, Marott JL, Vestbo J, Nordestgaard BG, Lange P. Coronary heart disease and heart failure in asthma, COPD and asthma-COPD overlap. BMJ Open Respir Res. 2020;7(1):e000470. doi: 10.1136/bmjresp-2019-000470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goto T, Shimada YJ, Faridi MK, Camargo CA, Hasegawa K. Incidence of acute cardiovascular event after acute exacerbation of COPD. J Gen Intern Med. 2018;33(9):1461‒1468. doi: 10.1007/s11606-018-4518-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Müllerová H, Marshall J, De Nigris E, et al. Association between COPD exacerbations and acute cardiovascular events: a systematic literature review. Ther Adv Respir Dis. 2022;16:17534666221113647. doi: 10.1177/17534666221113647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hurst JR, Vestbo J, Anzueto A, et al. Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128‒1138. doi: 10.1056/NEJMoa0909883 [DOI] [PubMed] [Google Scholar]
- 16.Westerik JA, Metting EI, van Boven JF, Tiersma W, Kocks JW, Schermer TR. Associations between chronic comorbidity and exacerbation risk in primary care patients with COPD. Respir Res. 2017;18(1):31. doi: 10.1186/s12931-017-0512-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hesse K, Bourke S, Steer J. Heart failure in patients with COPD exacerbations: looking below the tip of the iceberg. Respir Med. 2022;196:106800. doi: 10.1016/j.rmed.2022.106800 [DOI] [PubMed] [Google Scholar]
- 18.Rabe KF, Hurst JR, Suissa S. Cardiovascular disease and COPD: dangerous liaisons? Eur Respir Rev. 2018;27(149):180057. doi: 10.1183/16000617.0057-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Decramer M, Janssens W. Chronic obstructive pulmonary disease and comorbidities. Lancet Respir Med. 2013;1(1):73‒83. doi: 10.1016/S2213-2600(12)70060-7 [DOI] [PubMed] [Google Scholar]
- 20.Crisan L, Wong N, Sin DD, Lee HM. Karma of cardiovascular disease risk factors for prevention and management of major cardiovascular events in the context of acute exacerbations of chronic obstructive pulmonary disease. Front Cardiovasc Med. 2019;6:79. doi: 10.3389/fcvm.2019.00079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bazell C, Pollack M, Comellas AP, et al. A 4-year retrospective claims analysis of oral corticosteroid use and health conditions in newly diagnosed medicare FFS patients with COPD. Int J Chron Obstruct Pulmon Dis. 2022;17:2635‒2652. doi: 10.2147/COPD.S373590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Løkke A, Hilberg O, Lange P, et al. Disease trajectories and impact of one moderate exacerbation in GOLD B COPD patients. Int J Chron Obstruct Pulmon Dis. 2022;17:569‒578. doi: 10.2147/COPD.S344669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Larsson K, Ekberg-Jansson A, Stridsman C, Hanno M, Vanfleteren LEGW. Adherence to treatment recommendations for chronic obstructive pulmonary disease - results from the Swedish national airway register. Int J Chron Obstruct Pulmon Dis. 2021;16:909‒918. doi: 10.2147/COPD.S300299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Janson C, Nwaru BI, Wiklund F, Telg G, Ekström M. Management and risk of mortality in patients hospitalised due to a first severe COPD exacerbation. Int J Chron Obstruct Pulmon Dis. 2020;15:2673‒2682. doi: 10.2147/COPD.S276819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sandelowsky H, Janson C, Wiklund F, Telg G, de Fine Licht S, Ställberg B. Lack of COPD-related follow-up visits and pharmacological treatment in Swedish primary and secondary care. Int J Chron Obstruct Pulmon Dis. 2022;17:1769‒1780. doi: 10.2147/COPD.S372266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hurst JR, Skolnik N, Hansen GJ, et al. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur J Intern Med. 2020;73:1‒6. doi: 10.1016/j.ejim.2019.12.014 [DOI] [PubMed] [Google Scholar]
- 27.Papi A, Vestbo J, Fabbri L, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076‒1084. doi: 10.1016/S0140-6736(18)30206-X [DOI] [PubMed] [Google Scholar]
- 28.Rabe KF, Martinez FJ, Ferguson GT, et al. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. New Eng J Med. 2020;383(1):35‒48. doi: 10.1056/NEJMoa1916046 [DOI] [PubMed] [Google Scholar]
- 29.Martinez FJ, Rabe KF, Ferguson GT, et al. Reduced all-cause mortality in the ETHOS trial of budesonide/glycopyrrolate/formoterol for chronic obstructive pulmonary disease. A randomized, double-blind, multicenter, parallel-group study. Am J Respir Crit Care Med. 2021;203(5):553‒564. doi: 10.1164/rccm.202006-2618OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lipson DA, Barnhart F, Brealey N, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. NEJM. 2018;378(18):1671‒1680. doi: 10.1056/NEJMoa1713901 [DOI] [PubMed] [Google Scholar]
- 31.Lipson DA, Crim C, Criner GJ, et al. Reduction in all-cause mortality with fluticasone furoate/umeclidinium/vilanterol in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2020;201(12):1508‒1516. doi: 10.1164/rccm.201911-2207OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gedebjerg A, Szépligeti SK, Wackerhausen LH, et al. Prediction of mortality in patients with chronic obstructive pulmonary disease with the new global initiative for chronic obstructive lung disease 2017 classification: a cohort study. Lancet Respir Med. 2018;6(3):204‒212. doi: 10.1016/S2213-2600(18)30002-X [DOI] [PubMed] [Google Scholar]
- 33.Marott JL, Çolak Y, Ingebrigtsen TS, Vestbo J, Nordestgaard BG, Lange P. Exacerbation history, severity of dyspnoea and maintenance treatment predicts risk of future exacerbations in patients with COPD in the general population. Respir Med. 2022;192:106725. doi: 10.1016/j.rmed.2021.106725 [DOI] [PubMed] [Google Scholar]