Abstract
Aims
Osteoarthritis (OA) is a prevalent joint disorder with inflammatory response and cartilage deterioration as its main features. Dihydrocaffeic acid (DHCA), a bioactive component extracted from natural plant (gynura bicolor), has demonstrated anti-inflammatory properties in various diseases. We aimed to explore the chondroprotective effect of DHCA on OA and its potential mechanism.
Methods
In vitro, interleukin-1 beta (IL-1β) was used to establish the mice OA chondrocytes. Cell counting kit-8 evaluated chondrocyte viability. Western blotting analyzed the expression levels of collagen II, aggrecan, SOX9, inducible nitric oxide synthase (iNOS), IL-6, matrix metalloproteinases (MMPs: MMP1, MMP3, and MMP13), and signalling molecules associated with nuclear factor-kappa B (NF-κB) and mitogen-activated protein kinase (MAPK) pathways. Immunofluorescence analysis assessed the expression of aggrecan, collagen II, MMP13, and p-P65. In vivo, a destabilized medial meniscus (DMM) surgery was used to induce mice OA knee joints. After injection of DHCA or a vehicle into the injured joints, histological staining gauged the severity of cartilage damage.
Results
DHCA prevented iNOS and IL-6 from being upregulated by IL-1β. Moreover, the IL-1β-induced upregulation of MMPs could be inhibited by DHCA. Additionally, the administration of DHCA counteracted IL-1β-induced downregulation of aggrecan, collagen II, and SOX9. DHCA protected articular cartilage by blocking the NF-κB and MAPK pathways. Furthermore, DHCA mitigated the destruction of articular cartilage in vivo.
Conclusion
We present evidence that DHCA alleviates inflammation and cartilage degradation in OA chondrocytes via suppressing the NF-κB and MAPK pathways, indicating that DHCA may be a potential agent for OA treatment.
Cite this article: Bone Joint Res 2023;12(4):259–273.
Keywords: Dihydrocaffeic acid, Osteoarthritis, Chondrocyte, Inflammation, MAPK, NF-κB, cartilage degradation, inflammation, Chondrocytes, collagen II, western blotting, aggrecan, MMP13, knee joints, interleukin 6, articular cartilage
Article focus
We hypothesized that dihydrocaffeic acid (DHCA) could alleviate osteoarthritis (OA) progression.
Key messages
DHCA was proved to possess the anti-inflammation and anti-cartilage degradation properties in OA chondrocytes.
DHCA alleviated OA progression via inhibiting the nuclear factor-kappa B (NF-κB) and mitogen-activated protein kinase (MAPK) pathways.
Strengths and limitations
The strength of this study is that we are the first to present evidence that DHCA alleviates inflammation and cartilage degradation in OA chondrocytes in vitro and in vivo by suppressing the NF-κB and MAPK pathways, indicating that DHCA may be a potential agent for OA treatment.
The limitation of this study is that in vivo evidence of chondroprotective mechanism of DHCA on OA needs to be addressed in the future.
Introduction
Osteoarthritis (OA) is a common age-related degenerative disease which mainly affects 10% of males and 18% of females aged over 60 years old, and about 240 million individuals worldwide.1-3 It is believed that the incidence of OA will double in the middle of the 20th century, leaving behind significant social and financial difficulties.4 In addition to subchondral osteosclerosis and osteophytes, the pathophysiology of OA includes the breakdown of articular cartilage, with pain and dysfunction as its main clinical manifestations.5 Due to the lack of understanding of the mechanism and effective measures, the OA treatment mainly focuses on anti-inflammation and protection of articular cartilage, and joint prosthesis arthroplasty surgery, as a ultimate treatment, is applicable to end-stage OA patients.6
Numerous physiological and mechanical factors such as trauma, obesity, inheritance, sex, and mechanical stress contribute to the OA progression.7-9 Inflammation is considered as a major contributor to the symptoms of OA, as well as the degradation of articular cartilage.10 Inflammatory cytokines like interleukin-1β (IL-1β) induces apoptosis of chondrocytes, initiates overproduction of catabolic components, such as thrombospondin motifs (ADAMTS) and matrix metalloproteinases (MMPs), and reduces the production of metabolic components, such as aggrecan and collagen II. These changes will lead to degradation of extracellular matrix (ECM) in articular cartilage.11 Measures to inhibit the release of inflammatory cytokines can effectively improve OA.12
In recent years, more and more attention has been paid to the research of active components in plants found in common diseases, such as artemisinin against malaria.13 Dihydrocaffeic acid (DHCA), as a main bioactive component in gynura bicolor, possesses anti-inflammatory and anti-oxidative properties in various diseases.14,15 However, the precise effect of DHCA in OA is still unknown, and the potential mechanism by which DHCA inhibits inflammation and cartilage degradation in IL-1β-induced mouse chondrocytes was examined in this study.
In this study, we show that DHCA downregulated the inflammatory response (inducible nitric oxide synthase (iNOS) and IL-6) and catabolic response (MMPs), while upregulating the anabolic response (aggrecan, collagen II, and SOX9) in IL-1β-induced OA chondrocyte in vitro studies. Furthermore, the effects of DHCA on inhibiting catabolism and promoting anabolism were also verified by immunohistochemistry (IHC) in destabilized medial meniscus (DMM) OA mice model. Additionally, DHCA mitigated the destruction of articular cartilage by blocking the NF-κB and MAPK pathways. We thus identify, for the first time, the chondroprotective role of DHCA in OA through its suppression of NF-κB and MAPK pathways and provide a potential agent for OA treatment.
Methods
Predict the pharmacological targets of DHCA
The potential drug targets of DHCA were acquired from Pharmmapper (East China University of Science and Technology, China). The candidate genes were further identified using the Uniprot database.16
Enrichment analyses
R packages “clusterProfiler”, “enrichplot”, and “ggplot2” were used to perform the Gene Ontology (GO) enrichment analysis and Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analysis.
The PPI networks
Metascape was used to identify transcription factors and represent the network of protein-protein interaction (PPI) analysis.17
Reagents
Dihydrocaffeic acid (HY-N2406) was obtained from MedChemExpress (MCE, USA). Recombinant mouse IL-1β was purchased from R&D Systems (USA). Dulbecco’s modified Eagle medium F12 (DMEM/F12) was obtained from HyClone (USA). Fetal bovine serum was purchased from BioInd (Biological Industries, Israel). Primary antibodies for western blotting were as follows: Proteintech (China) supplied primary antibodies against glyceraldehyde 3-phosphate dehydrogenase (GAPDH) (60004-1-Ig, 1:10,000), IL-6 (21865-1-AP, 1:500), MMP1 (10371-2-AP, 1:500), MMP13 (18165-1-AP, 1:1,000), collagen II (28459-1-AP, 1:1,000), and aggrecan (13880-1-AP, 1:1,000). Cell Signalling Technology (CST, USA) provided the iNOS (13120, 1:1,000), SOX9 (82630, 1:1,000), p-IκBα (2859, 1:1,000), IκBα (4814, 1:1,000), p-IKKα/β (2697, 1:1,000), IKKα (61294, 1:1,000), IKKβ (8943, 1:1,000), p-P65 (3033, 1:1,000), P65 (8242, 1:1,000), p-ERK (4370, 1:1,000), ERK (4695, 1:1,000), p-P38 (4511, 1:1,000), P38 (8690, 1:1,000), p-JNK (4668, 1:1,000), and JNK (9252, 1:1,000) antibodies. Primary antibody against MMP3 (BM4074, 1:1,000) and secondary antibodies came from Boster (China). Primary antibodies for immunofluorescence staining were collagen II (Proteintech, 28459-1-AP, 1:50), aggrecan (Proteintech, 13880-1-AP, 1:100), MMP13 (Proteintech, 18165-1-AP, 1:50), and P65 (CST, 8242, 1:400). Primary antibodies for IHC staining were collagen II (Proteintech, 28459-1-AP, 1:800), aggrecan (Proteintech, 13880-1-AP, 1:200), and MMP13 (Proteintech, 18165-1-AP, 1:50).
Murine chondrocyte isolation and culture
Primary chondrocytes were extracted from knee joints of five-day-old C57BL/6 J mice. Briefly, the fur and skin were cleaned, then the mice were killed and disinfected in 75% alcohol. After that the ankle joint was clamped with a tweezer, the skin at the front of knee joint was cut with a microscissor, the fascia tissue around the knee joint was peeled off, the joint capsule was opened and the cartilage granules were obtained. Remove the adipose and synovial tissue around the cartilage granules which are hyaluronic and flexible. Next, the cartilage granules from the knee joints were cut into pieces with a microscissor. Cartilage granules were digested with 0.25% trypsin for 30 minutes and 0.25% type II collagenase for six hours at 37°C. Afterwards, the primary chondrocytes were cultured in a DMEM/F12 medium containing 10% fetal bovine serum in a humid environment (37°C, 5% CO2). Chondrocytes of the first or second passage were employed in subsequent experiments.
Viability of chondrocytes
To assess the viability of chondrocytes, we used a cell counting kit-8 (CCK-8, Boster). Chondrocytes (5,000 cells/well) were seeded in a 96-well plate with six replicates. After the cells had adhered, they were given treatment with 5 ng/ml IL-1β for different time durations (0, 3, 6, 12, 24, and 48 hours) or with 40 μM DHCA for 24 hours. Then, the cells received a CCK-8 solution (100 μl, 10%) after the medium had been withdrawn, and were incubated in an incubator at 37°C for one hour without any light. Absorbance was determined at 450 nm using a microplate reader from Thermo Fisher Scientific (Finland).
Western blotting
Chondrocytes from each treatment group were lysed with radioimmunoprecipitation assay (RIPA) (Boster) buffer, which contains 1% protease inhibitor and 1% phosphatase inhibitor for 15 minutes on ice. Then, lysed protein samples were gathered and centrifuged (12,000 g, 30 minutes, 4°C). After that, a bicinchoninic acid (BCA) assay kit (Boster) was employed to quantify the protein content of each sample after collecting the supernatant after centrifugation. In electrophoresis on a polyacrylamide-sodium dodecyl sulfate gel (SDS-PAGE), multiple proteins were isolated and subsequently transferred to polyvinylidene difluoride (PVDF) membranes (Millipore, USA). Next, the membranes were incubated with 5% skim milk for one hour at room temperature to inhibit any potential permeability, and treated with primary antibodies for more than 14 hours at 4°C, followed by one hour of treatment with secondary antibodies at room temperature. Protein bands were visualized using a Western ECL System (Boster), and images were captured using a Bio-Rad scanner (USA).
Quantitative reverse transcription polymerase chain reaction
Cells in a six-well plate were exposed to DHCA (40 µM) or IL-1β (5 ng/ml) for 24 hours after reaching 80% confluence. The catabolism and anabolism of chondrocytes at gene levels were assessed using quantitative reverse transcription polymerase chain reaction (qRT-PCR) analysis. The total RNA is extracted and purified with the aid of an RNA extraction kit (Omega Bio-Tek, USA). The quality of the RNA samples was evaluated with microplate reader. Next, a complementary DNA (cDNA) synthesis kit (Yeasen, China) was employed to synthesize the cDNA, which was then amplified by a qRT-PCR kit (Yeasen). The comparative 2−ΔΔCt method was selected to reflect the levels of various gene expressions. Table I displays the primer sequences that were used in the experiment.
Table I.
Primer sequence used in quantitative reverse transcription polymerase chain reaction experiment.
| Gene | Sequence |
|---|---|
| Aggrecan | Forward: 5’-AGGTGTCGCTCCCCAACTAT-3’ |
| Reverse: 5’-CTTCACAGCGGTAGATCCCAG-3’ | |
| Collagen II | Forward: 5’-GGCCAGGATGCCCGAAAATTA-3’ |
| Reverse: 5’-CGCACCCTTTTCTCCCTTGT-3’ | |
| SOX9 | Forward: 5’-AGGAAGTCGGTGAAGAACGG-3’ |
| Reverse: 5’-GGACCCTGAGATTGCCCAGA-3’ | |
| MMP3 | Forward: 5’-ACTCCCTGGGACTCTACCAC-3’ |
| Reverse: 5’-GGTACCACGAGGACATCAGG-3’ | |
| MMP13 | Forward: 5’-TGATGGACCTTCTGGTCTTCTGG-3’ |
| Reverse: 5’-CATCCACATGGTTGGGAAGTTCT-3’ | |
| iNOS | Forward: 5’-GACCCAGAGACAAGCCTAC-3’ |
| Reverse: 5’-GTGAGCTGGTAGGTTCCTG-3’ | |
| IL-6 | Forward: 5’-AGTTGCCTTCTTGGGACTG-3’ |
| Reverse: 5’-CCACGATTTCCCAGAGAAC-3’ | |
| GAPDH | Forward: 5’-CTCCCACTCTTCCACCTTCG-3’ |
| Reverse: 5’-TTGCTGTAGCCGTATTCATT-3’ |
GAPDH, glyceraldehyde 3-phosphate dehydrogenase; IL-6, interleukin 6; iNOS, inducible nitric oxide synthase; MMP, matrix metalloproteinase.
Chondrocytes stained with toluidine blue
Following the manufacturer’s instruction, toluidine blue agent (Solarbio, China) was employed to examine the chondrocytes’ external characteristics. In a six-well plate, chondrocytes reaching 80% confluence were exposed to DHCA (40 µM) or IL-1β (5 ng/ml) for 24 hours. Then, the pre-treated chondrocytes were fixed with 4% paraformaldehyde for 15 minutes at room temperature, and stained with toluidine blue dye for 24 hours. Subsequently, the excess dye was removed and the cells were washed with phosphate-buffered saline (PBS). Then, the morphological features of chondrocytes with DHCA and IL-1β treatment were detected by an Evos Fl Auto microscope (Life Technologies, USA).
Immunofluorescence
Chondrocytes were planted at a density of 1 × 104 cells per well in a 24-well plate. In either the presence or absence of 40 µM DHCA, IL-1β (5 ng/ml) was used to treat the cells. For 15 minutes at room temperature, the cells were fixed with 4% paraformaldehyde. Then, cell membranes were punched using a 0.2% Triton X-100 solution for five minutes, and blocked with 5% bovine serum albumin (BSA) for 30 minutes. After that, collagen II, aggrecan, MMP13, and P65-specific antibodies were used to treat the cells overnight at 4°C. After being washed three times with PBS, the cells were incubated with Cy3/Fitc-conjugated secondary antibodies for one hour at 37°C in the dark. The DAPI was left to soak into the cell nuclei for a full ten minutes. The immunofluorescence images were captured using an Evos Fl Auto fluorescent microscope (Life Technologies).
Destabilized medial meniscus-induced mice OA models
The C57BL/6 J mice (five mice in each cage) had free access to water and food in a specific pathogen-free environment, a constant temperature (22°C), and 12 hours of alternating light and dark. An intraperitoneal injection of pentobarbital (35 mg/kg) was used to sedate the mice. Then, the medial meniscus of the right knee was surgically destabilized to establish the destabilization of the medial meniscus (DMM)-induced OA models. In sham surgery, only the joint capsule was cut without medial meniscus instability surgery. The SHAM, DMM, and DMM + DHCA groups were randomly formed from 24 eight-week-old male C57BL/6 J mice. DHCA was dissolved in co-solvents such as 40% polyethylene glycol300 (PEG300), 10% DMSO, 5% Tween-80, and 45% saline according to manufacturer guidance, and 10 μl DHCA (0.0036 mg/kg) was intra-articular administered to the mice in the DMM + DHCA group. The identical volume (10 μl) of vehicle (40% PEG300, 10% DMSO, 5% Tween-80, and 45% saline) was intra-articularly injected into the mice in the SHAM and DMM groups. For eight weeks straight, the injection was administered twice every week. The samples of their knee joints were taken for later research. An ARRIVE checklist is included to prove compliance with the ARRIVE guidelines.
Radiograph examination and histological evaluation
The sacrificed mice’s right knee joints were extracted from muscle tissue and a radiograph examination was performed by a digital X-ray machine (Kubtec Model XPERT.8; KUB Technologies, USA). After that, the knee joint samples were kept for 24 hours in 4% paraformaldehyde, then decalcified for 30 days in a 10% EDTA solution before being embedded in paraffin wax. Prior to being stained with haematoxylin and eosin (H&E) and safranin O/fast green, the samples were divided into pieces that were 5 μm thick. A blinded method was employed to evaluate the progression of OA using a score assigned by the Osteoarthritis Research Society International (OARSI).18 Histochemistry required deparaffinization, rehydration, and blocking for one hour in BSA containing 0.1% Triton X-100, staining the slices with diaminobenzidine, and counterstaining with haematoxylin after being incubated with anti-MMP13, -collagen II, and -aggrecan antibodies. Using fluorescent microscopy, pictures were taken (Evos Fl Auto; Life Technologies).
Statistical analysis
Data were shown as the mean and standard deviation (SD) for independent experiments and analyzed using GraphPad Prism 8 (GraphPad, USA). A one-way analysis of variance was used to compare all of the research groups, and independent-samples t-test and Bonferroni’s test were used for a post hoc comparison. To denote statistical significance, p < 0.05 was used.
Results
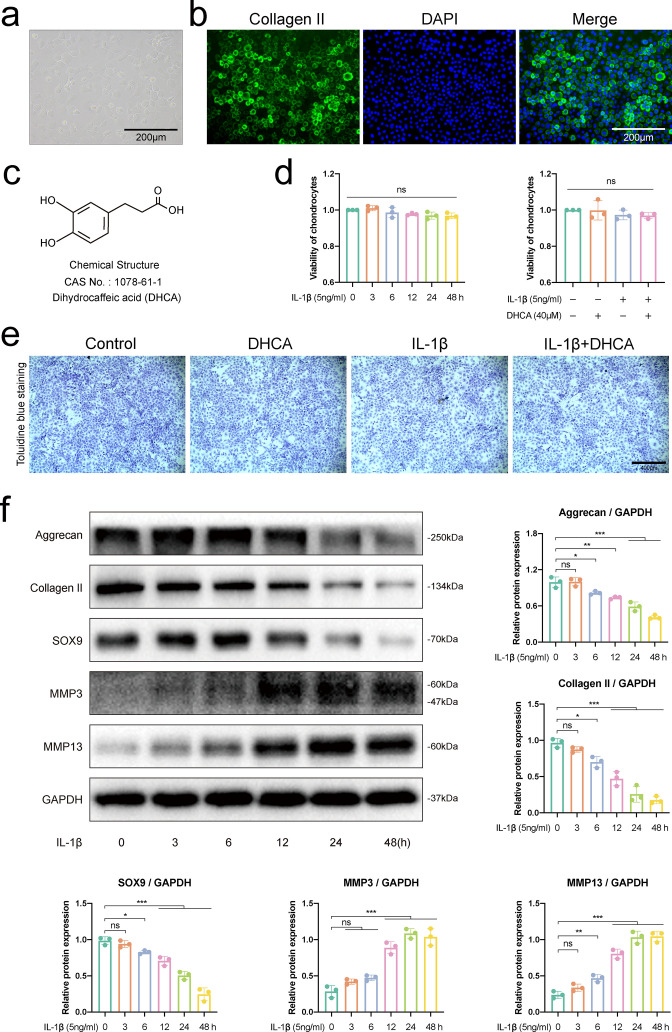
Identification of chondrocytes
Proteoglycan and collagen II make up the ECM of chondrocytes, which are the only cells that make up articular cartilage.19 To detect mouse chondrocytes, we therefore used phase contrast microscopy, immunofluorescence, and toluidine blue staining. As shown in Figure 1a, chondrocytes showed typical paving stone-like changes in cell morphology, which were round or polygonal. Immunofluorescence staining showed that the target cells were rich in collagen II (Figure 1b). Toluidine blue staining reflects the content of proteoglycan (Figure 1e). Combined with where the cells come from, we determined that the cells obtained from the knee joint are chondrocytes.
Fig. 1.
Identification of chondrocytes, detection of cell viability, and selection of proper time of interleukin-1β (IL-1β) stimulation on chondrocytes. a) Morphology of primary mouse chondrocytes under phase contrast microscope. b) Immunofluorescence analysis showed that the cytoplasm of primary mouse chondrocytes was rich in collagen II, which was stained with fluorescein isothiocyanate (FITC). c) Chemical structure of dihydrocaffeic acid (DHCA). d) Cell counting kit assesses the viability of chondrocytes treated with 5 ng/ml IL-1β for different time durations (0, 3, 6, 12, 24, and 48 hours) or with 40 μM DHCA for 24 hours. e) Toluidine blue staining of the chondrocytes treated with 40 μM DHCA or/and 5 ng/ml IL-1β for 24 hours. f) Western blot bands and quantitative analysis of mediators about anabolism (aggrecan, collagen II, and SOX9) and catabolism of chondrocytes (matrix metalloproteinase 3 (MMP3) and MMP13) in chondrocytes stimulated with 5 ng/ml IL-1β at different timepoints (0, 3, 6, 12, 24, and 48 hours). Data were presented as means and standard deviations (n = 3). GAPDH, glyceraldehyde 3-phosphate dehydrogenase; ns, no significance; *p < 0.05; **p < 0.01; ***p < 0.001.
Effect of DHCA on chondrocyte viability
In order to explore whether DHCA and/or IL-1β affects the viability of chondrocytes, CCK-8 assay was performed. The chemical structure of DHCA can be found in Figure 1c. As shown in Figure 1d, 5 ng/ml IL-1β at different time durations (0, 3, 6, 12, 24, and 48 hours) and DHCA at a concentration of 40 μM alone, or together with 5 ng/ml IL-1β for 24 hours did not affect the vitality of chondrocytes compared with the control group and the DHCA group. Additionally, when chondrocytes were exposed to 40 μM DHCA alone or together with 5 ng/ml IL-1β for 24 hours, toluidine blue staining failed to detect any apparent morphological alterations (Figure 1e).
Selection of proper time of IL-1β stimulation on chondrocytes
The balance between catabolism and anabolism, as well as chondrocyte homeostasis, are both impacted by the well-known major inflammatory cytokine IL-1β, which accelerates cartilage degradation.20 To determine the optimal time of IL-1β action, the following experiments were performed. First, the vitality of chondrocytes was tested with 5 ng/ml IL-1β at various time durations (0, 3, 6, 12, 24, and 48 hours), and Figure 1d demonstrates that there was no significant difference in the cytotoxicity of chondrocytes. Next, the effect of affected chondrocytes’ catabolism and anabolism at various stimulation periods of IL-1β was detected with western blot analysis. As shown in Figure 1f, collagen II, aggrecan, and SOX9, which are anabolic markers, declined over time, whereas MMP3 and MMP13, which are catabolic markers, were seen to rise over time. The decrease expression levels of aggrecan, collagen II, and SOX9 were obvious at 24 hours and 48 hours, while MMP3 and MMP13 reached their highest points at 24 hours. Thus, the stimulation duration of IL-1β on mouse chondrocytes that we ultimately chose was 24 hours.
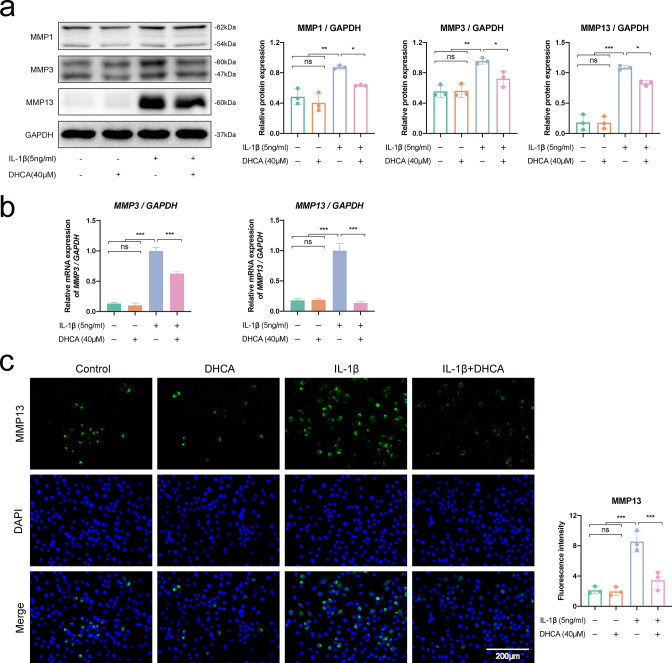
DHCA decreased IL-1β-induced upregulation of catabolic mediators in mouse OA chondrocytes
Matrix-degrading proteases, including aggrecanases and metalloproteinases (MMP1, MMP3, and MMP13), are known to be activated during the pathogenesis of OA.21,22 In response to IL-1β, chondrocytes produce the overexpression of catabolic enzymes, such as MMP1, MMP3, and MMP13, which aid in the degradation of ECM. Our western blot data demonstrated that treatment with DHCA significantly suppressed the expression of the abovementioned enzymes (Figure 2a). Furthermore, qRT-PCR analysis revealed that IL-1β triggered the overexpression of MMP1, MMP3, and MMP13 at gene levels, whereas DHCA reversed the upregulated trends in IL-1β-induced chondrocytes (Figure 2b). The results of western blot and qRT-PCR data about MMP13 were also verified by immunofluorescence analysis, as DHCA effectively decreased the elevated MMP13 in cytoplasm caused by IL-1β (Figure 2c). When seen collectively, these findings imply that DHCA may be a potent inhibitor of matrix-degrading proteases in mouse chondrocytes.
Fig. 2.
Dihydrocaffeic acid (DHCA) decreased interleukin-1β (IL-1β)-induced upregulation of catabolic mediators in mouse osteoarthritis (OA) chondrocytes. Chondrocytes were administrated with 40 μM DHCA or/and 5 ng/ml IL-1β for 24 hours. a) Western blot bands and quantitative analysis of catabolic-related proteins (matrix metalloproteinase 1 (MMP1), MMP3, and MMP13). b) Quantitative reverse transcription polymerase chain reaction (qRT-PCR) analysis of catabolic-related genes (MMP3 and MMP13) at the messenger RNA expression level. c) Immunofluorescence images (magnification: ×200) and quantitative analysis of the MMP13 expression. Data were presented as means and standard deviations (n = 3). DAPI, 4′,6-diamidino-2-phenylindole; GAPDH, glyceraldehyde 3-phosphate dehydrogenase; ns, no significance; *p < 0.05; **p < 0.01; ***p < 0.001.
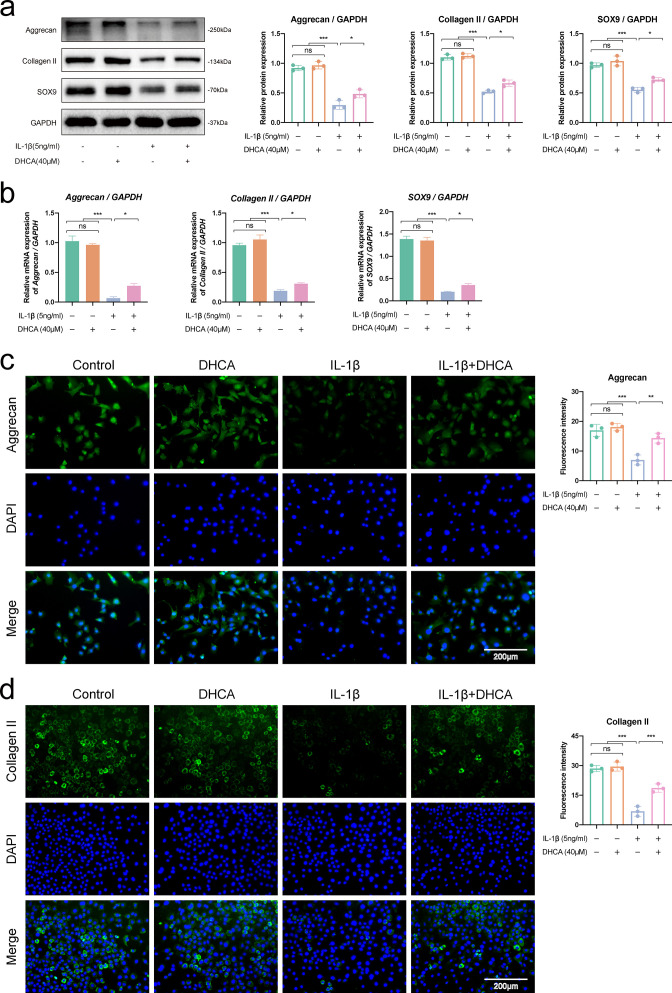
DHCA increased IL-1β-induced downregulation of anabolic mediators in mouse OA chondrocytes
Anabolism has a crucial protective role in preserving the homeostasis of cartilage. The most crucial mediators of chondrocytes metabolism are collagen II, aggrecan, and SOX9.23,24 Therefore, we investigated whether DHCA can restore the expression of aforementioned mediators in chondrocytes activated with IL-1β. As shown in Figures 3a and 3b, IL-1β stimulation drastically reduced the expression of aggrecan, collagen II, and SOX9 at both mRNA and protein levels in mouse chondrocytes. Conversely, DHCA markedly increased the anabolic mediators (aggrecan, collagen II, and SOX9) both at mRNA and protein levels in mouse IL-1β-induced chondrocytes. Additionally, immunofluorescence verified the expression level of aggrecan and collagen II that observed in western blot and qRT-PCR analysis (Figures 3c and 3d). These findings collectively suggest that, under the pathological conditions of inflammation, DHCA may exert cartilage protective effects by increasing the expression of anabolic mediators in chondrocytes.
Fig. 3.
Dihydrocaffeic acid (DHCA) increased interleukin-1β (IL-1β)-induced downregulation of anabolic mediators in mouse osteoarthritis (OA) chondrocytes. Chondrocytes were administrated with 40 μM DHCA or/and 5 ng/ml IL-1β for 24 hours. a) Western blot bands and quantitative analysis of anabolic-related proteins (aggrecan, collagen II, and SOX9). b) Quantitative reverse transcription polymerase chain reaction (qRT-PCR) analysis of anabolic-related genes (aggrecan, collagen II, and SOX9) at the mRNA expression level. c) and d) Immunofluorescence images and quantitative analysis of the expression of aggrecan and collagen II. Data were presented as means and standard deviations (n = 3). GAPDH, glyceraldehyde 3-phosphate dehydrogenase; ns, no significance; *p < 0.05; **p < 0.01; ***p < 0.001.
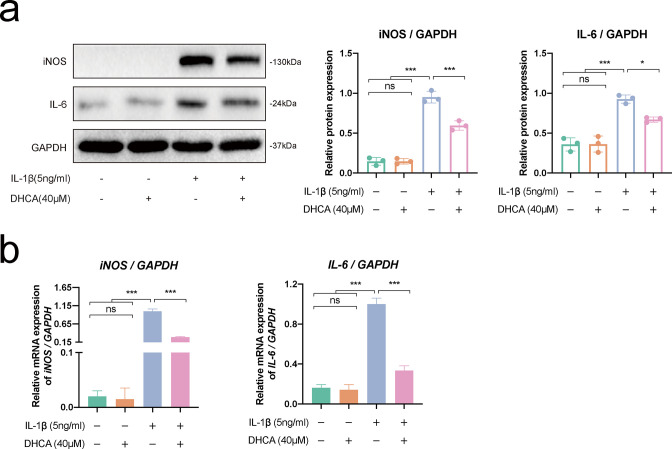
DHCA decreased IL-1β-induced upregulation of inflammatory mediators in mouse OA chondrocytes
It is acknowledged that inflammation acts as a significant contributor to the pathophysiology of OA.25 We explored how DHCA affected the expression of inflammatory mediators induced by IL-1β in OA chondrocytes. The expression levels of specific inflammatory mediators (iNOS and IL-6) were assessed using western blot and qRT-PCR analysis after chondrocytes were stimulated with 5 ng/ml of IL-1β or with 40 µM DHCA for 24 hours. Data revealed that IL-1β upregulated the expression levels of iNOS and IL-6 compared with the control group and the DHCA group. However, DHCA greatly decreased these expressions of inflammatory mediators in IL-1β-induced chondrocytes (Figure 4a). In addition, the mRNA expression of IL-6 and iNOS dramatically rose after IL-1β stimulation, and decreased with the DHCA treatment in IL-1β-induced chondrocytes (Figure 4b). Together, these findings suggest that DHCA possess anti-inflammatory properties in IL-1β-induced chondrocytes.
Fig. 4.
Dihydrocaffeic acid (DHCA) decreased interleukin-1β (IL-1β)-induced upregulation of inflammatory mediators in mouse osteoarthritis (OA) chondrocytes. Chondrocytes were administrated with 40 μM DHCA or/and 5 ng/ml IL-1β for 24 hours. a) Western blot bands and quantitative analysis of inflammation-related proteins (inducible nitric oxide synthase (iNOS) and IL-6). b) Quantitative reverse transcription polymerase chain reaction (qRT-PCR) analysis of inflammation-related genes (iNOS and IL-6) at the mRNA expression level. Data were presented as means and standard deviations (n = 3). GAPDH, glyceraldehyde 3-phosphate dehydrogenase; ns, no significance; *p < 0.05; **p < 0.01; ***p < 0.001.
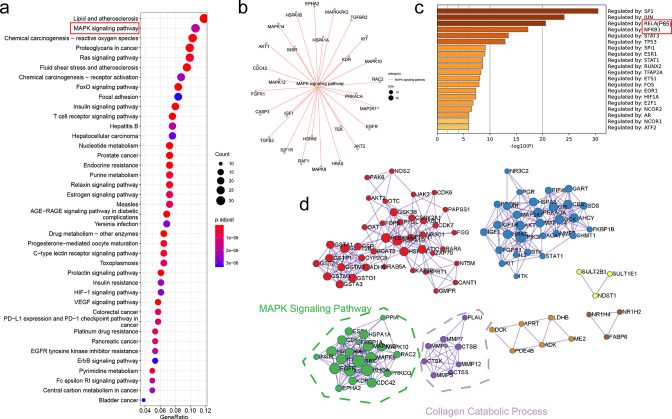
Bioinformatics analysis illustrated that DHCA might regulate NF-κB/MAPK signalling pathway
Bioinformatics analysis plays an important role in finding potential diagnostic markers of OA.26 To explore the underlying mechanism by which DHCA modulates OA, we analyzed the potential drug targets of DHCA. Overall, 294 drug targets were identified by means of the Pharmmapper database. KEGG analysis suggested that the MAPK signalling pathway might be regulated by DHCA, and 28 DHCA targets were enriched to MAPK pathway (Figures 5a and 5b). Transcription factors analysis indicated that RELA (P65) and NFKB1 played an important role in regulating DHCA targets, which suggested P65 NF-κB pathway might be regulated by DHCA (Figure 5c). Further PPI analysis validated that MAPK pathway was highly enriched; additionally, DHCA might affect collagen catabolic process, which was consistent with our previous conclusions (Figure 5d).
Fig. 5.
Bioinformatics analysis illustrated that dihydrocaffeic acid (DHCA) might regulate nuclear factor-kappa B (NF-κB) and mitogen-activated protein kinase (MAPK) signalling pathway. a) DHCA targets were frequently enriched in the MAPK pathway. b) 28 genes were enriched in the MAPK pathway. c) According to transcription factors (TF) analysis, RELA (P65) and NFKB1 were identified as key TFs. d) PPI analysis of DHCA targets illustrated that the MAPK pathway and collagen catabolic process were involved. AGE-RAGE, advanced glycosylation end products-receptor for advanced glycosylation end products; HIF-1, hypoxia-inducible factor 1; VEGF, vascular endothelial growth factor.
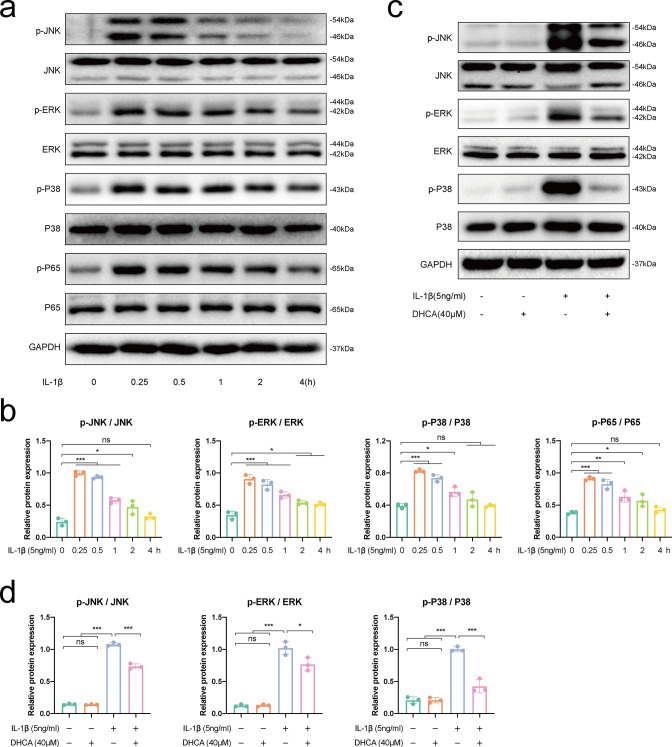
Determining the best time for IL-1β-induced activation of the NF-κB/MAPK signalling pathway
The earliest events that contribute to the development of OA are the transduction of NF-κB and MAPK signal pathways. According to a recent study, preventing the aforementioned two signalling pathways from being activated via IL-1β slows down the degradation of the cartilage.27 To determine the ideal activation timepoints of the aforementioned two pathways induced by IL-1β at different time durations (0, 0.25, 0.5, 1, 2, and 4 hours), we therefore examined proteins associated with the pathways. As shown in Figures 6a and 6b, the NF-κB and MAPK pathways were activated by IL-1β in a time-dependent manner, with the peak of activation happening at 0.25 hours after stimulation, and fading thereafter. Therefore, chondrocytes stimulated with IL-1β for 0.25 hours was chosen in subsequent study of the two pathways.
Fig. 6.
The early activation of nuclear factor-kappa B (NF-κB) and mitogen-activated protein kinase (MAPK) signalling pathway induced by interleukin-1β (IL-1β). Chondrocytes were administrated with 5 ng/ml IL-1β at different time durations (0, 0.25, 0.5, 1, 2, and 4 hours). a) Western blot bands and b) quantitative analysis of proteins associated with the NF-κB (p-P65, P65) and MAPK (p-JNK, JNK, p-ERK, ERK, p-P38, and P38) pathways. Dihydrocaffeic acid (DHCA) inhibited IL-1β-induced activation of the MAPK signalling pathway. Chondrocytes were treated with 40 μM DHCA for 24 hours or/and 5 ng/ml IL-1β for 0.25 hours. c) Western blot bands and d) quantitative analysis of proteins associated with the MAPK pathway. Data were presented as means and standard deviations (n = 3). GAPDH, glyceraldehyde 3-phosphate dehydrogenase; ns, no significance; *p < 0.05; **p < 0.01; ***p < 0.001.
DHCA inhibited IL-1β-induced activation of the MAPK signalling pathway
Next, we identified the molecular mechanism underlying the chondroprotective actions of DHCA. Recent research reveals that the MAPK pathway, which includes the signal transducers P38 kinase, c-Jun NH2-terminal kinase (JNK), and extracellular signal-regulated kinase (ERK),28 have been activated to regulate the IL-1β-mediated MMP expressions.29 To ascertain if DHCA exerts its chondroprotective effects by inhibiting MAPKs, we measured the phosphorylation levels of JNK, ERK, and P38 (p-JNK, p-ERK, and p-P38) in IL-1β-activated murine chondrocytes. The results showed that within 0.25 hours of IL-1β administration, the MAPK pathway including JNK, ERK, and P38 was activated in chondrocytes, as the expression level of p-JNK, p-ERK, and p-P38 were elevated. However, the activation trends were inhibited when mouse chondrocytes were pretreated with DHCA (Figures 6c and 6d). According to these findings, DHCA modulates the activation of MAPK signalling pathway under pathological circumstances, which has a chondroprotective impact.
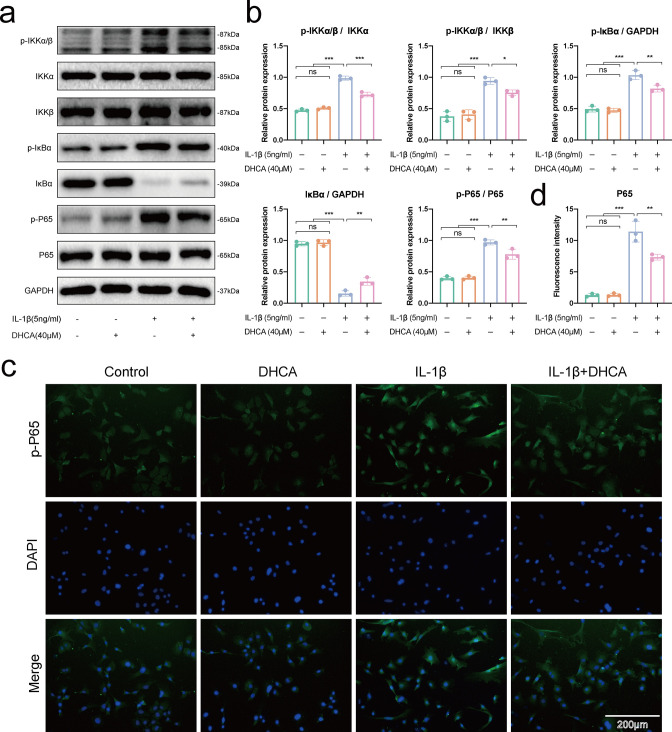
DHCA suppressed IL-1β-induced activation of the NF-κB signalling pathway
The generation of catabolic mediator is stimulated by IL-1β, as well as IL-6 and iNOS, through transcriptional regulation, while NF-κB is a signal pathway mainly regulated by transcription factors, thus we next investigated the role of NF-κB transcription factor in chondrocyte metabolism.30 We discovered that within 15 minutes of treatment, IL-1β increased the phosphorylation levels of IKKα/β, IκBα, and P65 (p-IKKα/β, p-IκBα, and p-P65), and the degradation of IκBα in mice chondrocytes. However, the treatment with DHCA reversed these alterations (Figures 7a and 7b). Moreover, when p-P65 accumulates in the nucleus, it can act as a downstream effector protein of NF-κB pathway activation. Immunofluorometric assay revealed that p-P65 was restricted to the cytoplasm of healthy chondrocytes, but the propensity of p-P65 to migrate into the nucleus was elevated following IL-1β treatment of chondrocytes. However, by using DHCA, the amount of p-P65 that accumulated in the nucleus decreased (Figures 7c and 7d). These findings collectively imply that, under pathological circumstances, DHCA exhibits chondroprotective effects by controlling the NF-κB signalling pathways in mouse chondrocytes.
Fig. 7.
Dihydrocaffeic acid (DHCA) suppressed interleukin-1β (IL-1β)-induced activation of the nuclear factor-kappa B (NF-κB) signalling pathway. Chondrocytes were treated with 40 μM DHCA for 24 hours or/and 5 ng/ml IL-1β for 0.25 hours. a) Western blot bands and b) quantitative analysis of proteins associated with the NF-κB pathway. c) Immunofluorescence images (magnification: ×200) and d) quantitative analysis of the expression of p-P65. Data were presented as means and standard deviations (n = 3). GAPDH, glyceraldehyde 3-phosphate dehydrogenase; IKK, inhibitor of nuclear factor-κB (IκB) kinase; ns, no significance; *p < 0.05; **p < 0.01; ***p < 0.001.
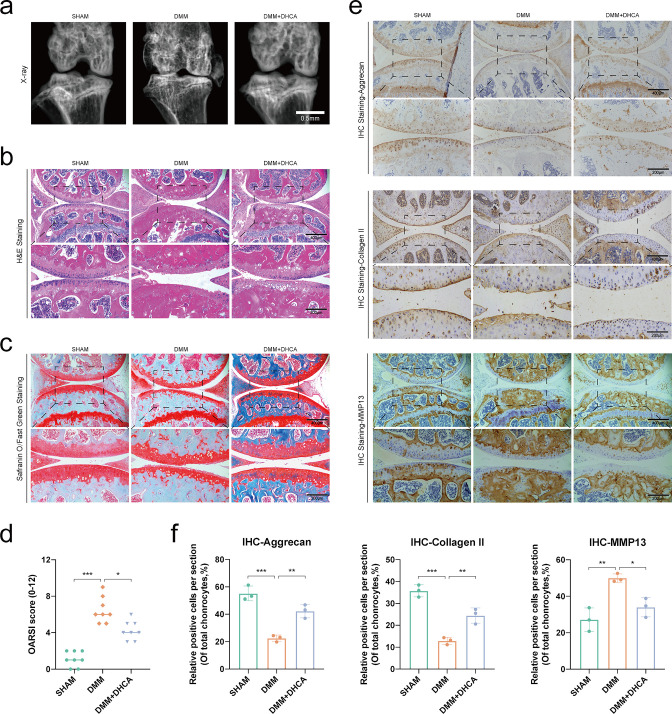
DHCA attenuated cartilage degradation in vivo
Eight weeks after DMM surgery or intra-articular DHCA injection, mice were killed and the knee joints were obtained. The knee joint samples among the three groups underwent radiograph assessment, and were stained with H&E and safranin O/fast green to determine the extent of the cartilage damage. The DMM group demonstrated OA-like features, such as the roughness and unevenness of the articular cartilage surface, the damage of articular cartilage, and the formation of osteophytes. While in the DMM + DHCA group, we found that DHCA mitigated cartilage deterioration when measured by radiograph, H&E, and safranin O/fast green staining. As shown in Figure 8a, the knee joint surface in the SHAM group was smooth, with a wider joint space, without osteophyte formation and osteosclerosis, while the DMM group exhibited obvious OA changes, such as joint space narrowing, osteophyte formation, bone cystic change, etc. However, the above OA changes in DMM + DHCA group were alleviated to a certain extent. Furthermore, in Figures 8b and 8c, the DMM group exhibited an uneven, rough, and damaged cartilage surface compared with the SHAM group, whereas the DMM + DHCA group showed a full and smooth cartilage surface. Additionally, we evaluated the severity of OA by calculating OARSI scores, and data revealed that the DMM group received a higher score than that of the SHAM group, whereas the DMM + DHCA group exhibited a lower score compared with the DMM group (Figure 8d). Moreover, the three groups’ IHC results for aggrecan, collagen II, and MMP13 supported the in vitro experiment. In the mouse DMM-induced OA models, DHCA treatment boosted aggrecan and collagen II expression, and decreased MMP13 production (Figures 8e and 8f). In conclusion, the outcomes of the in vivo studies revealed that DHCA could slow the development of OA in DMM mice.
Fig. 8.
Dihydrocaffeic acid (DHCA) attenuated mouse knee cartilage degradation in vivo. a) Radiograph, b) haematoxylin and eosin (H&E) staining, and c) Safranin O/fast green staining of the knee articular cartilage among the SHAM, DMM, and DMM + DHCA group (magnification: ×100 for 400 μm, ×200 for 200 μm). d) Osteoarthritis Research Society International (OARSI) scoring analysis demonstrated the degree of cartilage degradation (n = 8). e) Immunohistochemical (IHC) staining and f) quantitative analysis of positive chondrocytes about anabolism (aggrecan and collagen II) and catabolism (MMP13) (n = 3). Data were presented as means and standard deviations. *p < 0.05; **p < 0.01; ***p < 0.001.
Discussion
OA, one of the most prevalent joint diseases associated with the elderly, is a heterogeneous, complicated, multifactorial illness.31,32 The present strategies for OA are symptomatic treatment which cannot be used to cure the OA.33 These treatment methods include reducing the movement of the affected joints, and medical and surgical treatment. However, serious side-effects are frequently experienced with medication therapy for OA.34 Moreover, the surgical treatment is mostly joint prosthesis arthroplasty surgery, leaving patients with unpredictable psychological pressure, and placing a huge economic burden on the society.35 Exploring the pathological mechanism of OA and searching for drugs without side-effects have become the urgent areas to be solved by the current research institute. A growing body of research indicates that natural substances may be able to treat OA with few negative effects.36 DHCA, a bioactive component extracted from Gynura bicolor, has been proved to have anti-inflammatory properties.14 However, inflammation is considered as a pathogenic factor of OA. This study aimed to investigate how DHCA affects chondrocyte inflammation brought on by IL-1β. Our findings demonstrated that DHCA prevented an IL-1β-induced inflammatory response, and cartilage degradation, by preventing the activation of NF-κB and MAPK signalling pathways.
Previous research believed that inflammatory mediators, including iNOS and IL-6, are crucial mediators in the progression of OA.37 Studies revealed that iNOS and IL-6 levels were shown to be elevated in OA patients.38,39 Moreover, research has confirmed that it is the production of these inflammatory factors that leads to the emergence of clinical symptoms, such as pain and swelling. Anti-inflammatory treatment, such as oral administration of non-steroidal anti-inflammatory drugs, can alleviate patients’ clinical discomfort.40 Our data demonstrated that DHCA decreased the expression of inflammatory mediators, such as iNOS and IL-6, in IL-1β-stimulated chondrocytes, implying that DHCA possesses anti-inflammatory properties.
The importance of NF-κB signalling pathway in controlling inflammatory mediators has been well established.41,42 The aggravation of OA is closely related to the activation of this pathway, and inhibiting activation has been shown to improve OA.43-45 NF-κB is often found in the cytoplasm and coupled to the inhibitor of NF-κB (IκB). When cells were being triggered by IL-1β, IκB protein such as IκBα was phosphorylated and destroyed, together with the nucleus translocation of NF-κB P65, which ultimately regulates the production of inflammatory mediators.46-48 In this study, we discovered that DHCA prevented the activation of NF-κB signalling pathway in IL-1β chondrocytes. In addition, MAPK signalling pathway is also closely related to inflammation and is associated with the progression of OA.49 Proteins at the key nodes of the P38, JNK, and ERK MAPK signalling pathways are phosphorylated and activated when IL-1β stimulates chondrocytes,50 which are consistent with our experimental results. Strategies of suppressing the MAPK signalling pathway could alleviate the OA progression.51 Our data found evidence of DHCA’s impact on MAPK activation, as DHCA inhibited IL-1β-induced P38, JNK, and ERK MAPK activation. Overall, our findings revealed that DHCA prevented IL-1β-induced activation of the NF-κB and MAPK signalling pathways.
In addition to inflammatory response, cartilage deterioration is another main feature of OA. The balance of chondrocyte metabolism is a crucial factor to maintaining cartilage homeostasis. Cartilage degeneration includes the imbalance of anabolism and catabolism in chondrocytes, such as the weakening of anabolism and/or enhancement of catabolism, which will lead to the increased degradation of ECM on the surface of cartilage and contribute to cartilage deterioration and OA formation.52,53 MMPs, such as MMP1, MMP3, and MMP13, are important catabolic enzymes, the overexpression of which target collagen II and aggrecan for degradation.54-56 However, the most important enzymes of anabolism are collagen II and aggrecan, which could maintain the physiological structure of ECM. The reduction of their synthesis will cause the degradation of ECM.57 However, the above-mentioned inflammatory response is one of the main pathogenic factors leading to the imbalance of chondrocyte metabolism. Excessive pro-inflammatory factors will trigger the upregulation of catabolic enzymes and downregulation of anabolic enzymes in chondrocytes, and ultimately contribute to the degradation of ECM, the deterioration of cartilage, and the occurrence of OA.58-60 Our in vitro experiments confirmed that DHCA maintains the metabolic balance of chondrocytes by inhibiting inflammatory response. In addition, DMM method was a commonly used surgical strategy for establishing the OA cartilage. In our in vivo study, H&E and safranin O/fast green staining data revealed that the SHAM group showed a full and smooth cartilage surface, with a considerable thickness of cartilage and without any cartilage damage. However, the DMM group experienced pronounced cartilage loss and erosion, whereas the DHCA-treated group experienced a reduction in these changes, indicating that DHCA treatment slowed down the progression of OA in vivo. Furthermore, the IHC staining for the protein expression of anabolic-related indicators (aggrecan and collagen II) and catabolic-related indicators (MMP13) supported the in vitro experiment, as DHCA treatment boosted aggrecan and collagen II expression and decreased MMP13 production. This supported OARSI results and histochemical findings, pointing to the protective role of DHCA in the mouse DMM model. Therefore, strategies of inhibiting inflammation can effectively improve the progression of OA.
In summary, our findings indicated that DHCA reduced the inflammatory reaction and deterioration of cartilage brought on by IL-1β via suppressing the NF-κB and MAPK pathways through in vivo and in vitro tests, implying that DHCA might be a promising agent for OA treatment.
Author contributions
R. Lu: Conceptualization, Data curation, Formal analysis, Methodology, Writing – review & editing.
Y-G. Wang: Data curation, Formal analysis, Methodology, Writing – original draft.
Y. Qu: Data curation, Formal analysis, Writing – original draft.
S-X. Wang: Formal analysis, Methodology, Validation, Data curation.
C. Peng: Methodology, Validation, Data curation.
H. You: Data curation, Validation, Funding acquisition, Writing – review & editing, Writing – original draft.
W. Zhu: Conceptualization, Data curation, Writing – review & editing, Supervision.
A. Chen: Conceptualization, Data curation, Funding acquisition, Project administration, Writing – review & editing.
Funding statement
The authors disclose receipt of the following financial or material support for the research, authorship, and/or publication of this article: The National Natural Science Foundation of China (No. 81772390) and Wu JiePing Medical Foundation (No. 320.6750.2020-03-07) provided funding for this work.
ICMJE COI statement
The authors declare that they have no conflict of interest.
Data sharing
The authors will make the raw data necessary to support this article's conclusion available without excessive delay.
Acknowledgements
We wish to thank all of those who generously agreed to be interviewed for this research.
Ethical review statement
The Institutional Animal Care and Use Committee of Tongji Hospital Tongji Medical College, Huazhong University of Science and Technology (Wuhan, China) evaluated and approved the animal study.
Open access funding
The open access funding for this study was provided by the National Natural Science Foundation of China (No. 81772390) and Wu JiePing Medical Foundation (No. 320.6750.2020-03-07).
Supplementary material
ARRIVE checklist, and schematic diagram of dihydrocaffeic acid improving mouse osteoarthritis.
© 2023 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Contributor Information
Rui Lu, Email: hblurui2020@163.com.
Ying-Guang Wang, Email: d202082001@hust.edu.cn.
Yunkun Qu, Email: m202076278@hust.edu.cn.
Shan-Xi Wang, Email: wangshanxi0210@163.com.
Cheng Peng, Email: chengpeng2015@tjh.tjmu.edu.cn.
Hongbo You, Email: hbyou360@hotmail.com.
Wentao Zhu, Email: wentao-zhu@hotmail.com.
Anmin Chen, Email: anminchen@hust.edu.cn.
References
- 1. Glyn-Jones S, Palmer AJR, Agricola R, et al. Osteoarthritis. Lancet. 2015;386(9991):376–387. doi: 10.1016/S0140-6736(14)60802-3. [DOI] [PubMed] [Google Scholar]
- 2. Nelson AE. Osteoarthritis year in review 2017: clinical. Osteoarthritis Cartilage. 2018;26(3):319–325. doi: 10.1016/j.joca.2017.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. He C-P, Chen C, Jiang X-C, et al. The role of AGEs in pathogenesis of cartilage destruction in osteoarthritis. Bone Joint Res. 2022;11(5):292–300. doi: 10.1302/2046-3758.115.BJR-2021-0334.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wallace IJ, Worthington S, Felson DT, et al. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc Natl Acad Sci U S A. 2017;114(35):9332–9336. doi: 10.1073/pnas.1703856114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745–1759. doi: 10.1016/S0140-6736(19)30417-9. [DOI] [PubMed] [Google Scholar]
- 6. Bonnet CS, Walsh DA. Osteoarthritis, angiogenesis and inflammation. Rheumatology (Oxford) 2005;44(1):7–16. doi: 10.1093/rheumatology/keh344. [DOI] [PubMed] [Google Scholar]
- 7. Morales-Ivorra I, Romera-Baures M, Roman-Viñas B, Serra-Majem L. Osteoarthritis and the Mediterranean diet: A systematic review. Nutrients. 2018;10(8):1030. doi: 10.3390/nu10081030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eitner A, Wildemann B. Diabetes - osteoarthritis and joint pain. Bone Joint Res. 2021;10(5):307–309. doi: 10.1302/2046-3758.105.BJR-2021-0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jiang L, Zhu X, Rong J, et al. Obesity, osteoarthritis and genetic risk: The rs182052 polymorphism in the ADIPOQ gene is potentially associated with risk of knee osteoarthritis. Bone Joint Res. 2018;7(7):494–500. doi: 10.1302/2046-3758.77.BJR-2017-0274.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sellam J, Berenbaum F. The role of synovitis in pathophysiology and clinical symptoms of osteoarthritis. Nat Rev Rheumatol. 2010;6(11):625–635. doi: 10.1038/nrrheum.2010.159. [DOI] [PubMed] [Google Scholar]
- 11. Hosseinzadeh A, Kamrava SK, Joghataei MT, et al. Apoptosis signaling pathways in osteoarthritis and possible protective role of melatonin. J Pineal Res. 2016;61(4):411–425. doi: 10.1111/jpi.12362. [DOI] [PubMed] [Google Scholar]
- 12. Mei L, Wang H, Chen J, et al. Self-assembled lyotropic liquid crystal gel for osteoarthritis treatment via anti-inflammation and cartilage protection. Biomater Sci. 2021;9(21):7205–7218. doi: 10.1039/d1bm00727k. [DOI] [PubMed] [Google Scholar]
- 13. Tu Y. Artemisinin-a gift from traditional Chinese medicine to the world (Nobel lecture) Angew Chem Int Ed Engl. 2016;55(35):10210–10226. doi: 10.1002/anie.201601967. [DOI] [PubMed] [Google Scholar]
- 14. Oliveira MM, Ratti BA, Daré RG, et al. Dihydrocaffeic acid prevents UVB-induced oxidative stress leading to the inhibition of apoptosis and MMP-1 expression via p38 signaling pathway. Oxid Med Cell Longev. 2019;2019:2419096. doi: 10.1155/2019/2419096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Baeza G, Sarriá B, Mateos R, Bravo L. Dihydrocaffeic acid, a major microbial metabolite of chlorogenic acids, shows similar protective effect than a yerba mate phenolic extract against oxidative stress in HepG2 cells. Food Res Int. 2016;87:25–33. doi: 10.1016/j.foodres.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 16. UniProt Consortium UniProt: the universal protein knowledgebase in 2021. Nucleic Acids Res. 2021;49(D1):D480–D489. doi: 10.1093/nar/gkaa1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhou Y, Zhou B, Pache L, et al. Metascape provides a biologist-oriented resource for the analysis of systems-level datasets. Nat Commun. 2019;10(1):1523. doi: 10.1038/s41467-019-09234-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578–1589. doi: 10.1016/j.joca.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 19. Sandell LJ, Aigner T. Articular cartilage and changes in arthritis. An introduction: cell biology of osteoarthritis. Arthritis Res. 2001;3(2):107–113. doi: 10.1186/ar148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier JP, Fahmi H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol. 2011;7(1):33–42. doi: 10.1038/nrrheum.2010.196. [DOI] [PubMed] [Google Scholar]
- 21. Goldring MB. Articular cartilage degradation in osteoarthritis. HSS J. 2012;8(1):7–9. doi: 10.1007/s11420-011-9250-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yang J, Zhou Y, Liang X, Jing B, Zhao Z. MicroRNA-486 promotes a more catabolic phenotype in chondrocyte-like cells by targeting SIRT6: possible involvement in cartilage degradation in osteoarthritis. Bone Joint Res. 2021;10(7):459–466. doi: 10.1302/2046-3758.107.BJR-2019-0251.R4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Orhan C, Juturu V, Sahin E, et al. Undenatured type II collagen ameliorates inflammatory responses and articular cartilage damage in the rat model of osteoarthritis. Front Vet Sci. 2021;8:617789. doi: 10.3389/fvets.2021.617789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Liu ZM, Shen PC, Lu CC, Chou SH, Tien YC. Suramin enhances chondrogenic properties by regulating the p67phox/PI3K/AKT/SOX9 signalling pathway. Bone Joint Res. 2022;11(10):723–738. doi: 10.1302/2046-3758.1110.BJR-2022-0013.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sokolove J, Lepus CM. Role of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretations. Ther Adv Musculoskelet Dis. 2013;5(2):77–94. doi: 10.1177/1759720X12467868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yang J, Fan Y, Liu S. ATF3 as a potential diagnostic marker of early-stage osteoarthritis and its correlation with immune infiltration through bioinformatics analysis. Bone Joint Res. 2022;11(9):679–689. doi: 10.1302/2046-3758.119.BJR-2022-0075.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ran J, Ma C, Xu K, et al. Schisandrin B ameliorated chondrocytes inflammation and osteoarthritis via suppression of NF-κB and MAPK signal pathways. Drug Des Devel Ther. 2018;12:1195–1204. doi: 10.2147/DDDT.S162014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kim EK, Choi EJ. Compromised MAPK signaling in human diseases: an update. Arch Toxicol. 2015;89(6):867–882. doi: 10.1007/s00204-015-1472-2. [DOI] [PubMed] [Google Scholar]
- 29. Kimura H, Yukitake H, Suzuki H, et al. The chondroprotective agent ITZ-1 inhibits interleukin-1beta-induced matrix metalloproteinase-13 production and suppresses nitric oxide-induced chondrocyte death. J Pharmacol Sci. 2009;110(2):201–211. doi: 10.1254/jphs.09076fp. [DOI] [PubMed] [Google Scholar]
- 30. Haseeb A, Ansari MY, Haqqi TM. Harpagoside suppresses IL-6 expression in primary human osteoarthritis chondrocytes. J Orthop Res. 2017;35(2):311–320. doi: 10.1002/jor.23262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zheng L, Zhang Z, Sheng P, Mobasheri A. The role of metabolism in chondrocyte dysfunction and the progression of osteoarthritis. Ageing Res Rev. 2021;66:101249. doi: 10.1016/j.arr.2020.101249. [DOI] [PubMed] [Google Scholar]
- 32. Loeser RF, Goldring SR, Scanzello CR, Goldring MB. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum. 2012;64(6):1697–1707. doi: 10.1002/art.34453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Katz JN, Arant KR, Loeser RF. Diagnosis and treatment of hip and knee osteoarthritis: A review. JAMA. 2021;325(6):568–578. doi: 10.1001/jama.2020.22171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. O’Neil CK, Hanlon JT, Marcum ZA. Adverse effects of analgesics commonly used by older adults with osteoarthritis: focus on non-opioid and opioid analgesics. Am J Geriatr Pharmacother. 2012;10(6):331–342. doi: 10.1016/j.amjopharm.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Xie F, Kovic B, Jin X, He X, Wang M, Silvestre C. Economic and humanistic burden of osteoarthritis: A systematic review of large sample studies. Pharmacoeconomics. 2016;34(11):1087–1100. doi: 10.1007/s40273-016-0424-x. [DOI] [PubMed] [Google Scholar]
- 36. Zhao H, Zhang T, Xia C, et al. Berberine ameliorates cartilage degeneration in interleukin-1β-stimulated rat chondrocytes and in a rat model of osteoarthritis via Akt signalling. J Cell Mol Med. 2014;18(2):283–292. doi: 10.1111/jcmm.12186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Xu Z, Ke T, Zhang Y, Guo L, Chen F, He W. Danshensu inhibits the IL-1β-induced inflammatory response in chondrocytes and osteoarthritis possibly via suppressing NF-κB signaling pathway. Mol Med. 2021;27(1):80. doi: 10.1186/s10020-021-00329-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Koch B, Baum W, Burmester GR, et al. Prostaglandin E2, interleukin 1 and gamma interferon production of mononuclear cells of patients with inflammatory and degenerative joint diseases. Z Rheumatol. 1989;48(4):194–199. [PubMed] [Google Scholar]
- 39. Laavola M, Leppänen T, Hämäläinen M, et al. IL-6 in osteoarthritis: Effects of pine stilbenoids. Molecules. 2018;24(1):109. doi: 10.3390/molecules24010109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. da Costa BR, Pereira TV, Saadat P, et al. Effectiveness and safety of non-steroidal anti-inflammatory drugs and opioid treatment for knee and hip osteoarthritis: network meta-analysis. BMJ. 2021;375:2321. doi: 10.1136/bmj.n2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yang P, Han Y, Gui L, et al. Gastrodin attenuation of the inflammatory response in H9c2 cardiomyocytes involves inhibition of NF-κB and MAPKs activation via the phosphatidylinositol 3-kinase signaling. Biochem Pharmacol. 2013;85(8):1124–1133. doi: 10.1016/j.bcp.2013.01.020. [DOI] [PubMed] [Google Scholar]
- 42. Joh EH, Gu W, Kim DH. Echinocystic acid ameliorates lung inflammation in mice and alveolar macrophages by inhibiting the binding of LPS to TLR4 in NF-κB and MAPK pathways. Biochem Pharmacol. 2012;84(3):331–340. doi: 10.1016/j.bcp.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 43. He L, Pan Y, Yu J, Wang B, Dai G, Ying X. Decursin alleviates the aggravation of osteoarthritis via inhibiting PI3K-Akt and NF-kB signal pathway. Int Immunopharmacol. 2021;97:107657. doi: 10.1016/j.intimp.2021.107657. [DOI] [PubMed] [Google Scholar]
- 44. Cao Y, Tang S, Nie X, et al. Decreased miR-214-3p activates NF-κB pathway and aggravates osteoarthritis progression. EBioMedicine. 2021;65:103283. doi: 10.1016/j.ebiom.2021.103283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zhang Y, Lu R, Huang X, et al. Circular RNA MELK promotes chondrocyte apoptosis and inhibits autophagy in osteoarthritis by regulating MYD88/NF-κB signaling axis through microRNA-497-5p. Contrast Media Mol Imaging. 2022;2022:1–13. doi: 10.1155/2022/7614497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jeon J, Lee JH, Park KA, et al. Brazilin selectively disrupts proximal IL-1 receptor signaling complex formation by targeting an IKK-upstream signaling components. Biochem Pharmacol. 2014;89(4):515–525. doi: 10.1016/j.bcp.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 47. Heyninck K, Lahtela-Kakkonen M, Van der Veken P, Haegeman G, Vanden Berghe W. Withaferin A inhibits NF-kappaB activation by targeting cysteine 179 in IKKβ. Biochem Pharmacol. 2014;91(4):501–509. doi: 10.1016/j.bcp.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 48. Wang L, Xu Y, Yu Q, et al. H-RN, a novel antiangiogenic peptide derived from hepatocyte growth factor inhibits inflammation in vitro and in vivo through PI3K/AKT/IKK/NF-κB signal pathway. Biochem Pharmacol. 2014;89(2):255–265. doi: 10.1016/j.bcp.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 49. Liu F, Li L, Lu W, et al. Scutellarin ameliorates cartilage degeneration in osteoarthritis by inhibiting the Wnt/β-catenin and MAPK signaling pathways. Int Immunopharmacol. 2020;78:105954. doi: 10.1016/j.intimp.2019.105954. [DOI] [PubMed] [Google Scholar]
- 50. Akhtar N, Haqqi TM. Epigallocatechin-3-gallate suppresses the global interleukin-1beta-induced inflammatory response in human chondrocytes. Arthritis Res Ther. 2011;13(3):R93. doi: 10.1186/ar3368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lu R, Yu X, Liang S, et al. Physalin A inhibits MAPK and NF-κB signal transduction through integrin αVβ3 and exerts chondroprotective effect. Front Pharmacol. 2021;12:761922. doi: 10.3389/fphar.2021.761922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lv Z, Xu X, Sun Z, et al. TRPV1 alleviates osteoarthritis by inhibiting M1 macrophage polarization via Ca2+/CaMKII/Nrf2 signaling pathway. Cell Death Dis. 2021;12(6):504. doi: 10.1038/s41419-021-03792-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Fujii Y, Liu L, Yagasaki L, Inotsume M, Chiba T, Asahara H. Cartilage Homeostasis and Osteoarthritis. Int J Mol Sci. 2022;23(11):6316. doi: 10.3390/ijms23116316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wang M, Sampson ER, Jin H, et al. MMP13 is a critical target gene during the progression of osteoarthritis. Arthritis Res Ther. 2013;15(1):R5. doi: 10.1186/ar4133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Malemud CJ. Inhibition of MMPs and ADAM/ADAMTS. Biochem Pharmacol. 2019;165:33–40. doi: 10.1016/j.bcp.2019.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Liu Z, Wang H, Wang S, Gao J, Niu L. PARP-1 inhibition attenuates the inflammatory response in the cartilage of a rat model of osteoarthritis. Bone Joint Res. 2021;10(7):401–410. doi: 10.1302/2046-3758.107.BJR-2020-0200.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Luo Y, Sinkeviciute D, He Y, et al. The minor collagens in articular cartilage. Protein Cell. 2017;8(8):560–572. doi: 10.1007/s13238-017-0377-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ren C, Jin J, Hu W, et al. Betulin alleviates the inflammatory response in mouse chondrocytes and ameliorates osteoarthritis via AKT/Nrf2/HO-1/NF-κB axis. Front Pharmacol. 2021;12:754038. doi: 10.3389/fphar.2021.754038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wang T, He C. Pro-inflammatory cytokines: The link between obesity and osteoarthritis. Cytokine Growth Factor Rev. 2018;44:38–50. doi: 10.1016/j.cytogfr.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 60. Zhou Y, Li J, Xu F, Ji E, Wang C, Pan Z. Long noncoding RNA H19 alleviates inflammation in osteoarthritis through interactions between TP53, IL-38, and IL-36 receptor. Bone Joint Res. 2022;11(8):594–607. doi: 10.1302/2046-3758.118.BJR-2021-0188.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]