Abstract
Background
There is widespread agreement amongst clinicians that people with non‐specific low back pain (NSLBP) comprise a heterogeneous group and that their management should be individually tailored. One treatment known by its tailored design is the McKenzie method (e.g. an individualized program of exercises based on clinical clues observed during assessment).
Objectives
To evaluate the effectiveness of the McKenzie method in people with (sub)acute non‐specific low back pain.
Search methods
We searched CENTRAL, MEDLINE, Embase and two trials registers up to 15 August 2022.
Selection criteria
We included randomized controlled trials (RCTs) investigating the effectiveness of the McKenzie method in adults with (sub)acute (less than 12 weeks) NSLBP.
Data collection and analysis
We used standard methodological procedures expected by Cochrane.
Main results
This review included five RCTs with a total of 563 participants recruited from primary or tertiary care. Three trials were conducted in the USA, one in Australia, and one in Scotland. Three trials received financial support from non‐commercial funders and two did not provide information on funding sources. All trials were at high risk of performance and detection bias. None of the included trials measured adverse events.
McKenzie method versus minimal intervention (educational booklet; McKenzie method as a supplement to other intervention ‐ main comparison)
There is low‐certainty evidence that the McKenzie method may result in a slight reduction in pain in the short term (MD ‐7.30, 95% CI ‐12.04 to ‐2.56; 2 trials, 328 participants) but not in the intermediate term (MD ‐5.00, 95% CI ‐14.29 to 4.29; 1 trial, 180 participants).
There is low‐certainty evidence that the McKenzie method may not reduce disability in the short term (MD ‐2.74, 95% CI ‐7.52 to 2.04; 2 trials, 328 participants) nor in the intermediate term (MD ‐0.87, 95% CI ‐7.31 to 5.57; 1 trial, 180 participants).
McKenzie method versus manual therapy
There is low‐certainty evidence that the McKenzie method may not reduce pain in the short term (MD ‐8.67, 95% CI ‐27.37 to 10.02; 3 trials, 298 participants) and may result in a slight increase in pain in the intermediate term (MD 7.00, 95% CI 0.70 to 13.30; 1 trial, 235 participants).
There is low‐certainty evidence that the McKenzie method may not reduce disability in the short term (MD ‐4.98, 95% CI ‐15.00 to 5.04; 3 trials, 298 participants) nor in the intermediate term (MD 4.30, 95% CI ‐0.72 to 9.32; 1 trial, 235 participants).
McKenzie method versus other interventions (massage and advice)
There is very low‐certainty evidence that the McKenzie method may not reduce disability in the short term (MD 4.00, 95% CI ‐15.44 to 23.44; 1 trial, 30 participants) nor in the intermediate term (MD 10.00, 95% CI ‐8.95 to 28.95; 1 trial, 25 participants).
Authors' conclusions
Based on low‐ to very low‐certainty evidence, the treatment effects for pain and disability found in our review were not clinically important. Thus, we can conclude that the McKenzie method is not an effective treatment for (sub)acute NSLBP.
Keywords: Adult, Humans, Acute Pain, Acute Pain/therapy, Exercise Therapy, Low Back Pain, Low Back Pain/therapy, Quality of Life, Treatment Outcome
Plain language summary
Is the McKenzie method effective for the treatment of (sub)acute non‐specific low back pain?
Key messages
The McKenzie method may result in little to no benefit in pain and disability in people with (sub)acute non‐specific low back pain in the short term (closest to two weeks) and in the intermediate term (closest to three months). The McKenzie method is not an effective treatment for (sub)acute non‐specific low back pain. We do not know whether the McKenzie method leads to any side effects as none of the trials included in this review measured any side effects.
What is (sub)acute non‐specific low back pain?
Non‐specific low back pain (NSLBP) is the most common type of back pain and consists of pain or discomfort in the lower back that is not caused by an identifiable disease or problem (e.g. fracture, cancer, infection, nerve root pain, etc.). NSLBP is considered (sub)acute when it lasts for up to 12 weeks.
What is the McKenzie method?
The McKenzie method is a treatment applied by trained healthcare providers (typically physiotherapists) for the care of people with NSLBP. It comprises an individualized program of exercises based on clinical clues (changes in pain location or restricted movement), observed during the assessment. It also includes the teaching of postures and home exercises to encourage people to control their symptoms by themselves.
What did we want to find out?
We wanted to find out if the McKenzie method is effective for people with (sub)acute NSLBP.
What did we do?
We searched for studies that looked at the McKenzie method compared to minimal intervention (e.g. a small booklet with information on spinal pain) (main comparison) or other treatments for (sub)acute NSLBP. We were interested in knowing if the McKenzie method could reduce pain and disability in the short term (closest to two weeks) and in the intermediate term (closest to three months). We compared and summarized the results of the studies and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find?
We found five studies on a total of 536 people. Two studies compared the McKenzie method to minimal intervention, three compared it to manual therapy, (i.e. hands‐on therapy provided by a clinician) and one compared it to other interventions (back massage and advice). All five studies were conducted in high‐income countries (three in the USA, one in Australia, and one in Scotland). Three of them were funded by non‐commercial sources and two did not provide information on funding sources.
Our main comparison of the McKenzie method versus minimal intervention found that the McKenzie method may result in a slight reduction in pain and disability (0‐ to 100‐point scale, lower scores mean less pain and less disability):
‐ Pain: improved by 7.30 points (12.04 better to 2.56 better) in the short term (2 trials, 328 participants); and improved by 5.00 points (14.29 better to 4.29 worse) in the intermediate term (1 trial, 180 participants). ‐ Disability: improved by 2.74 points (7.52 better to 2.04 worse) in the short term (2 trials, 328 participants); and improved by 0.87 points (7.31 better to 5.57 worse) in the intermediate term (1 trial, 180 participants).
Our second comparison of the McKenzie method versus manual therapy found that the McKenzie method may not reduce pain or disability (0‐ to 100‐point scale, lower scores mean less pain and less disability):
‐ Pain: improved by 8.67 points (27.37 better to 10.02 worse) in the short term (3 trials, 298 participants); and worsened by 7.00 points (0.70 worse to 13.30 worse) in the intermediate term (1 trial, 235 participants). ‐ Disability: improved by 4.98 points (15.00 better to 5.04 worse) in the short term (3 trials, 298 participants); and worsened by 4.30 points (0.72 better to 9.32 worse) in the intermediate term (1 trial, 235 participants).
Our third comparison of the McKenzie method versus other interventions (back massage and advice) found that the McKenzie method may not reduce disability (0‐ to 100‐point scale, lower scores mean less disability):
‐ Disability: worsened by 4.00 points (15.44 better to 23.44 worse) in the short term (1 trial, 30 participants); and worsened by 10.0 points (8.95 better to 28.95 worse) in the intermediate term (1 trial, 25 participants).
None of the trials included in the review measured unwanted effects.
What are the limitations of the evidence?
We are not confident in the evidence because there weren't enough studies, the studies were small, and we have concerns about how some of the studies were conducted.
How up‐to‐date is this evidence?
This review included trials published up to 15 August 2022.
Summary of findings
Summary of findings 1. McKenzie therapy compared with minimal intervention for (sub)acute low back pain.
| McKenzie therapy compared with minimal intervention for acute and subacute low back pain | |||||
|
Patient or population: patients with non‐specific acute and subacute low back pain Settings: primary care Intervention: McKenzie therapy Comparison: minimal intervention (educational booklet; McKenzie method as a supplement to other intervention) | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of participants (trials) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Minimal intervention | McKenzie therapy | ||||
|
Pain intensity: short‐term (closest to 2 weeks) NRS (scale from 0‐100, 0 is no pain) |
The mean pain in the control group was 25.00 pointsa | The mean pain in the intervention group was 7.30 points better (12.04 points better to 2.56 better) | 328 participants (2 trials) |
⊕⊕⊝⊝ Lowb,c | McKenzie may result in a slight reduction in pain at short‐term. |
|
Pain intensity: intermediate‐term (closest to 3 months) NRS (scale from 0‐100, 0 is no pain) |
The mean pain in the control group was 32.00 pointsd | The mean pain in the intervention group was 5.00 points better (14.29 points better to 4.29worse) | 180 participants (1 trial) |
⊕⊕⊝⊝ Lowb,c | McKenzie may not reduce pain at intermediate‐term. |
|
Disability: short‐term (closest to 2 weeks) RMDQ (scale from 0‐100, 0 is no disability) |
The mean disability in the control group was 21.25 pointsa | The mean disability in the intervention group was 2.74 points better (7.52 points better to 2.04 worse) | 328 participants (2 trials) |
⊕⊕⊝⊝ Lowb,c | McKenzie may not reduce disability at short‐term. |
|
Disability: intermediate‐term (closest to 3 months) RMDQ (scale from 0‐100, 0 is no disability) |
The mean disability in the control group was 18.69 pointsd | The mean disability in the intervention group was 0.87 points better (7.31 points better to 5.57 worse) | 180 participants (1 trial) |
⊕⊕⊝⊝ Lowb,c | McKenzie may not reduce disability at intermediate‐term. |
| Adverse events | See comment | See comment | ‐ | ‐ | None of the included trials measured adverse events |
| *The basis for the assumed risk is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; NRS: numerical rating scale; RMDQ: Roland Morris Disability Questionnaire | |||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty; we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aMean value in minimal intervention group at short‐term follow‐up from Machado 2010 bDowngraded by one level due to risk of bias (lack of information about random allocation and lack of blinding of outcome assessment) cDowngraded by one level due to imprecision (wide 95% CI, including the possibility of a small or no effect and important benefit) dMean value in minimal intervention group at intermediate‐term follow‐up from Cherkin 1998
Summary of findings 2. McKenzie therapy compared with manual therapy for (sub)acute low back pain.
| McKenzie therapy compared with manual therapy for acute and subacute low back pain | |||||
|
Patient or population: patients with non‐specific acute and subacute low back pain Settings: primary care or outpatient physical therapy clinic Intervention: McKenzie therapy Comparison: manual therapy | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of participants (trials) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Manual therapy | McKenzie therapy | ||||
|
Pain intensity: short‐term (closest to 2 weeks)a Multiples scales (scale from 0‐100, 0 is no pain) |
The mean pain in the control group was 19.00 pointsb | The mean pain in the intervention groups was 8.67 points (27.37 better to 10.02 worse) | 298 participants (3 trials) | ⊕⊕⊝⊝ Lowc,d | McKenzie may not reduce pain at short‐term. |
|
Pain intensity: intermediate‐term (closest to 3 months) NRS (scale from 0‐100, 0 is no pain) |
The mean pain in the control group was 20.00 pointsb | The mean pain in the intervention group was 7.00 points worse (0.70 worse to 13.30 worse) | 235 participants (1 trial) |
⊕⊕⊝⊝ Lowc,d | McKenzie may result in a slight increase in pain. |
|
Disability: short‐term (closest to 2 weeks)a Multiples scales (scale from 0‐100, 0 is no disability) |
The mean disability in the control group was 16.10 pointsb | The mean disability in the intervention groups was 4.98 points better (15.00 better to 5.04 worse) | 298 participants (3 trials) |
⊕⊕⊝⊝ Lowc,d | McKenzie may not reduce disability at short‐term. |
|
Disability: intermediate‐term (closest to 3 months) RMDQ (scale from 0‐100, 0 is no disability) |
The mean disability in the control group was 13.50 pointsb | The mean disability in the intervention group was 4.30 points worse (0.72 better to 9.32 worse) | 235 participants (1 trial) |
⊕⊕⊝⊝ Lowc,d | McKenzie may not reduce disability at intermediate‐term. |
| Adverse events | See comment | See comment | ‐ | ‐ | None of the included trials measured adverse events. |
| *The basis for the assumed risk is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; NRS: numerical rating scale; RMDQ: Roland Morris Disability Questionnaire | |||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | |||||
aPain measured with NRSor visual analogue scale (VAS). Disability measured with RMDQ and Oswestry disability index (ODI) bMean value in manual therapy group at short‐term and intermediate‐term follow‐up from Cherkin 1998 cDowngraded by one level due to risk of bias (lack of information about random allocation, lack of allocation concealment, lack of blinding of outcome assessment, and intention‐to‐treat analysis) dDowngraded by one level due to imprecision (wide 95% CI, including the possibility of a small or no effect and important benefit)
Summary of findings 3. McKenzie therapy compared with other interventions for (sub)acute low back pain.
| McKenzie therapy compared with other interventions for acute and subacute low back pain | |||||
|
Patient or population: patients with non‐specific acute and subacute low back pain Settings: primary care Intervention: McKenzie therapy Comparison: back massage and standard back care advice | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of participants (trials) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Non‐specific back massage and standard back care advice | McKenzie therapy | ||||
| Pain intensity: short‐term (closest to 2 weeks) | See comment | See comment | ‐ | ‐ | None of the included trials measured pain at short‐term follow‐up. |
| Pain intensity: intermediate‐term (closest to 3 months) | See comment | See comment | ‐ | ‐ | None of the included trials measured pain at intermediate‐term follow‐up. |
|
Disability: short‐term (closest to 2 weeks) ODI (scale from 0‐100, 0 is no disability) |
The mean disability in the control group was 34.00 pointsa | The mean disability in the intervention group was 4.00 points worse (15.44 points better to 23.44 worse) | 30 participants (1 trial) |
⊕⊝⊝⊝ Verylowb,c | The evidence is very uncertain about the effect of McKenzie on disability at short‐term. |
|
Disability: intermediate‐term (closest to 3 months) ODI (scale from 0‐100, 0 is no disability) |
The mean disability in the control group was 20.00 pointsa | The mean disability in the intervention group was 10.00 points worse (8.95 points better to 28.95 worse) | 25 participants (1 trial) |
⊕⊝⊝⊝ Verylowb,c | The evidence is very uncertain about the effect of McKenzie on disability at intermediate‐term. |
| Adverse events | See comment | See comment | ‐ | ‐ | None of the included trials measured adverse events. |
| *The basis for the assumed risk is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; ODI: Oswestry Disability Index. | |||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | |||||
aMean value in other interventions group (back massage and standard back care advice) at short‐ and intermediate‐term follow‐up from Gillan 1998. bDowngraded by two levels due to risk of bias (lack of allocation concealment, lack of blinding of outcome assessment, incomplete outcome data, and lack of intention‐to‐treat analysis). cDowngraded by one level due to imprecision (wide 95% CI, including the possibility of a small or no effect and important benefit).
Background
Low back pain affects a significant proportion of the adult population and is considered a major health problem in high‐income, as well as in low‐ and middle‐income countries (Koes 2006; Maher 2017). The lifetime prevalence of low back pain has been estimated at 39% and this condition is known to pose a multifactorial impact on individuals' lives (Hoy 2010; Hoy 2012). The direct and indirect costs of this condition to societies are overwhelming, reaching more than USD 100,000 million per year (Indrakanti 2011). Moreover, the Global Burden of Disease study has consistently ranked low back pain as the leading cause of years lived with disability since 1990 (GBD 2019 Diseases and Injuries Collaborators).
Description of the condition
Low back pain is defined as pain or discomfort between the lower ribs and the gluteal folds, with or without leg pain (Van Tulder 2006). For most people with low back pain, the primary pathological process cannot be identified, and they are considered to have “non‐specific low back pain” (NSLBP) (Koes 2006). NSLBP can be classified according to the duration of the pain episode into acute NSLBP (pain lasting for six weeks or less), (sub)acute NSLBP (pain lasting from six to shorter than 12 weeks' duration), or chronic NSLBP (pain that persists for 12 weeks or more) (Koes 2006). People with (sub)acute NSLBP are generally grouped with those with acute NSLBP (Chou 2007). Recent evidence suggests that the natural and clinical course of NSLBP is not as favorable as previously thought (Itz 2013). Although people with low back pain improve markedly within the first six weeks, further improvements in symptoms are slow, with low to moderate levels of pain and disability still being present after one year in a significant proportion of individuals (Costa 2012). Clinical practice guidelines recommend that first‐line care for people with an acute episode of NSLBP should comprise general advice about self‐management and oral non‐steroidal anti‐inflammatory drugs (NSAIDs) at the lowest effective dose, and for the shortest time possible (ACP 2017; NICE 2016). The prescription of weak opioids (with or without paracetamol) is also recommended when people do not tolerate or respond to an NSAID. The Clinical Guidelines Committee of the American College of Physicians (ACP) recommends the use of superficial heat over the lower back, manual therapy, and acupuncture as second‐line care (ACP 2017). The National Institute for Health and Care Excellence (NICE) also recommend manual therapy for these people (e.g. spinal manipulation, mobilization, massage), but in conjunction with self‐management and group exercises (NICE 2016). At present, clinical practice guidelines do not include the McKenzie method among non‐pharmacological modalities for the management of people with (sub)acute NSLBP.
Randomized controlled trials (RCTs) have provided some support for the identification of clinical presentations that may indicate a greater likelihood of people with NSLBP in benefiting from specific treatments, including customized exercise programs (Brennan 2006; Childs 2004; Fritz 2003). For example, a pattern of pain response known as centralization appears to distinguish between people who are likely to respond to exercises performed in specific directions, particularly flexion or extension of the spine (Aina 2004; McKenzie 2003a). Centralization can be observed in approximately 70% of people with acute NSLBP and is defined as the phenomenon by which pain moves to a more proximal position in the spine before being ultimately abolished (Aina 2004). Robin McKenzie originally described this phenomenon in 1981 (McKenzie 1981), along with a method to classify and treat people with NSLBP named Mechanical Diagnosis and Therapy (MDT).
Description of the intervention
The McKenzie method uses history‐taking and symptomatic and mechanical responses to spinal loading strategies (e.g. centralization, or changes in range of motion, or both) to classify people into one of three McKenzie syndromes (derangement, dysfunction, or postural syndrome) and to determine the ideal management for each person with NSLBP (McKenzie 2003a; McKenzie 2003b). People not exhibiting one of the three McKenzie syndromes, such as those whose symptoms have been caused by a serious disease or trauma, or who present a chronic pain syndrome, are classified as 'other' and referred to appropriate non‐McKenzie treatments and practitioners (McKenzie 2003a). After classification, a customized treatment, including specific exercises that resemble the loading strategies used during assessment, is applied in conjunction with postural advice and education on self‐management skills (McKenzie 2003a). Some of the loading strategies applied during assessment and treatment (manual techniques can also be used as part of continuous force progression) in the McKenzie method are listed in Appendix 1. The core component of the McKenzie method is exercise, but education and postural training (which can be assisted by the use of a lumbar roll) also play a significant role (McKenzie 2003a; McKenzie 2003b). The main role of the educational component is to encourage people to use simple self‐management strategies to control their pain (McKenzie 2003a; McKenzie 2003b). Treat Your Own Back (McKenzie 2011) is McKenzie’s handbook for people with back pain, detailing the methods and exercises he developed. For a brief description of each McKenzie syndrome and their matching treatment programs, see Machado 2005. For a detailed account of all the procedures of this method, please refer to McKenzie’s textbooks (McKenzie 2003a; McKenzie 2003b).
How the intervention might work
Each McKenzie syndrome corresponds to different potential underlying mechanisms that are targeted by McKenzie’s individualized treatment program. The McKenzie Institute International has briefly described these mechanisms as follows: “the derangement syndrome involves mechanical obstruction to movement within the joint. Dysfunction syndrome involves pain caused by the mechanical loading of structurally impaired soft tissues and in postural syndrome pain develops from prolonged overloading of tissue” (www.mckenzieinstitute.org/clinicians/mckenzie-method/). The resolution of mechanical obstruction (e.g. disc herniation), soft tissue impairment (e.g. adaptive shortening or scarring), and tissue overloading (e.g. excessive thoracic hyperkyphosis or lumbar lordosis) have long been used as the conceptual model for treatment in the McKenzie method. However, due to the lack of empirical support for a clear patho‐anatomical diagnosis in people with NSLB, the understanding of how this method works is increasingly shifting to a model focused solely on clinical clues observed during clinical assessment (Hartvigsen 2018).
Why it is important to do this review
Despite the general idea that exercise prescription for NSLBP should match a set of clinical clues observed during clinical assessment (an approach also known as subgrouping of NSLBP), the evidence from previous systematic reviews on the effectiveness of the most popular subgrouping scheme for NSLBP (i.e. the McKenzie method), is inconsistent (Clare 2004; Lam 2018; Machado 2006). For example, two reviews found small, short‐term effects on pain and disability favoring the McKenzie method over other treatments for people with mostly (sub)acute NSLBP (Clare 2004; Machado 2006). However, no benefits were reported for people with the same condition in a more recent review (Lam 2018). Although inconsistencies like this may be related to how reviews group trials reporting on different comparisons or duration of symptoms for analysis, another concern is that some reviews have included trials investigating generic, non‐classification‐based interventions that do not reflect the original principles of the McKenzie method. Thus, a review that summarizes the evidence for the effects of the McKenzie method in people with NSLBP by considering only studies that truly represent the principles of the original method is needed. Two Cochrane Reviews were designed to overcome the limitations of previous studies conducted on this topic. This review focuses on (sub)acute NSLBP. The second one is focused on chronic NSLBP (Garcia 2012).
Objectives
To evaluate the effectiveness of the McKenzie method in people with (sub)acute non‐specific low back pain.
Methods
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials (RCTs) with clearly outlined, appropriate methods of randomization (e.g. computer‐generated random sequence). We did not include quasi‐randomized trials (e.g. randomization by date of birth).
Types of participants
We included trials in adults of either sex with (sub)acute NSLBP. At the time of allocation to trial groups, participants must have presented with a (sub)acute episode of NSLBP lasting for shorter than 12 weeks' duration. We excluded trials not reporting the duration of participants’ symptoms. We included trials in a mix of participants with (sub)acute and chronic symptoms, if data for the (sub)acute sample were reported separately. We excluded trials in participants with specific pathologic entities (e.g. spinal stenosis, radicular syndrome, scoliosis), ‘red flags’ for serious spinal pathology, spinal surgery in the previous six months, pregnancy, or severe cardiovascular or metabolic diseases. We also excluded trials aimed at primary prevention of NSLBP.
Types of interventions
We included trials evaluating the effectiveness of the McKenzie method, regardless of how the exercise regimen was named in each publication (i.e. McKenzie method, mechanical diagnosis and therapy (MDT), end‐range exercises, active range of motion exercises, etc.) as long as they followed the original principles described by the developer of the method (e.g. management or treatment strategy in line with the evaluation and classification, including repeated or sustained end‐range movements of the spine or postural education, or both; McKenzie 2003a; McKenzie 2003b). To assist with this decision, we sought advice from an expert of the McKenzie method. We contacted trial authors for further information when necessary.
Our comparisons of interest were:
McKenzie method versus minimal intervention (main comparison): waiting list control, placebo or inert controls, or both, brief educational interventions or booklets, or McKenzie method as a supplement to other intervention (i.e. manual therapy plus McKenzie versus manual therapy alone);
McKenzie method versus manual therapy (i.e. spinal manipulative therapy (SMT), vertebral mobilization, massage);
McKenzie method versus other types of exercise therapy (excluding McKenzie principles); and
McKenzie method versus all other interventions.
The decision to combine no intervention and minimal intervention in the same comparison group and the choice of the main comparison were post‐protocol decisions and are stated in the Differences between protocol and review section.
Types of outcome measures
We chose all major and minor outcomes according to the published protocol (Machado 2012).
Major outcomes
Pain intensity, measured as mean improvement from baseline, recorded using a visual analogue scale (VAS) or numerical rating scale
Disability, measured as mean improvement from baseline, recorded using the Oswestry Disability Index (ODI), the Roland Morris Disability Questionnaire (RMDQ), or another scale for back‐specific disability
Adverse events
Minor outcomes
General health status (as reported in the trials)
Future visits to healthcare professionals
Return to work
Patient satisfaction (as reported in the trials)
Timing of outcome assessments
We recorded outcomes in the short term (closest to two weeks) and intermediate term (closest to three months). The primary time point is short term.
Search methods for identification of studies
Electronic searches
We searched the following databases and trial registries, without language restrictions, from inception to 15 August 2022:
Cochrane Central Register of Controlled Trials (CENTRAL, which includes the Cochrane Back and Neck (CBN) Review Group trials register; Cochrane Register of Studies (CRS));
MEDLINE Ovid (1946 to 15 August 2022); and
Embase Ovid (1974 to 15 August 2022).
CINAHL (Cumulative Index to Nursing and Allied Health Literature; 1982 to 15 August 2022);
Physiotherapy Evidence Database (PEDro to 15 August 2022);
LILACS (Latin American and Caribbean Health Sciences Literature; 1982 to 15 August 2022);
Scientific Electronic Library Online (SciELO);
PubMed;
ClinicalTrials.gov (www.clinicaltrials.gov; searched 15 August 2022); and
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 15 August 2022).
The complete search strategies for all databases are described in Appendix 2.
Searching other resources
We conducted a manual search of reference lists of all included trials and previous systematic reviews (Clare 2004; Lam 2018; Machado 2006). We also screened the reference list from the McKenzie Institute International website (www.mckenziemdt.org). Personal communication with content experts complemented our search strategy.
Data collection and analysis
Selection of studies
Two review authors (ANG and MOA) independently screened all search results. We screened titles and abstracts first, before we obtained full texts of every potentially relevant study to judge whether it was eligible for inclusion. We resolved any disagreements by consensus, and a third review author (LMC) arbitrated, if necessary.
Data extraction and management
Two review authors (ANG and MOA) independently extracted data using a pre‐piloted standardized data extraction sheet. We extracted relevant information under the following domains:
publication data (authors, journal, volume, issue, year, pages, sources of funding);
number and characteristics of participants, characteristics of experimental and control groups, presence of co‐interventions; and
measures used to assess major and minor outcomes, time of assessment, number of participants assessed, and results for the assessment of major and minor outcomes at each relevant time point.
Assessment of risk of bias in included studies
Two review authors (ANG and MOA) independently assessed the risk of bias of included trials using the Cochrane risk of bias tool, as recommended by the Back and Neck Group (Furlan 2015). We rated each of the 13 items on the list as ‘yes’ (low risk of bias), ‘no’ (high risk of bias), or ‘unsure’ (unclear risk of bias). We resolved any disagreements through consensus, and a third review author (LMC) arbitrated, if necessary. The complete list of sources of risk of bias and the instructions for risk of bias assessments are described in Table 4 and Table 5, respectively. We based our decision on the overall risk of bias for each trial on ratings of the following key quality criteria:
1. Sources of risk of bias.
| Bias domain | Source of bias | Possible answers |
| Selection | (1) Was the method of randomization adequate? | Yes/No/Unsure |
| Selection | (2) Was the treatment allocation concealed? | Yes/No/Unsure |
| Performance | (3) Was the patient blinded to the intervention? | Yes/No/Unsure |
| Performance | (4) Was the care provider blinded to the intervention? | Yes/No/Unsure |
| Detection | (5) Was the outcome assessor blinded to the intervention? | Yes/No/Unsure |
| Attrition | (6) Was the dropout rate described and acceptable? | Yes/No/Unsure |
| Attrition | (7) Were all randomized participants analyzed in the group to which they were allocated? | Yes/No/Unsure |
| Reporting | (8) Are reports of the study free of suggestion of selective outcome reporting? | Yes/No/Unsure |
| Selection | (9) Were the groups similar at baseline regarding the most important prognostic indicators? | Yes/No/Unsure |
| Performance | (10) Were co interventions avoided or similar? | Yes/No/Unsure |
| Performance | (11) Was the compliance acceptable in all groups? | Yes/No/Unsure |
| Detection | (12) Was the timing of the outcome assessment similar in all groups? | Yes/No/Unsure |
| Other | (13) Are other sources of potential bias unlikely? | Yes/No/Unsure |
2. Instructions for risk of bias assessments.
| Item should be rated as “yes” (low risk of bias) only if the following is present: | |
| 1 | Random (unpredictable) assignment sequence (i.e. tossing a coin for studies with 2 groups or rolling a dice if ≥ 2 groups; drawing balls of different colours or ballots with group labels from a dark bag; using a computer‐generated random sequence, preordered opaque sealed envelopes or sequentially‐ordered vials; making a telephone call to central office). Group assignments by alternation, birth date, social insurance or security number, date of invitation to participate, or hospital registration number are not adequate (i.e. non‐random). |
| 2 | Assignment generated by an independent person, who does not participate in decisions about participant’s eligibility (i.e. does not have access to information about trial participants and has no influence on the assignment sequence or any decision about eligibility). |
| 3 | Index and comparison treatments are indistinguishable (i.e. treatments look the same), or treatments are distinguishable but blinding of trial participants was tested and found to be successfully achieved. |
| 4 | Index and comparison treatments are indistinguishable (i.e. treatments look the same), or treatments are distinguishable but blinding of care providers was tested and found to be successfully achieved. |
| 5 | Index and comparison treatments are indistinguishable (i.e. treatments look the same), or treatments are distinguishable but blinding of outcome assessors was tested and found to be successfully achieved. Blinding success should be assessed for each primary outcome separately. This item should also be rated as ‘yes’ (low risk of bias) if: ‐ Item 3 (participant blinding) is rated as ‘yes’ and either the outcome is self‐reported (i.e. pain and disability) or treatment or adverse effects cannot be identified during face‐to‐face assessment; ‐ Item 4 (blinding of care providers) is rated as ‘yes’ and the outcome is a clinical or therapeutic event assessed by the care provider (i.e. use of co‐intervention, hospitalization length, treatment failure, etc); ‐ Treatment/adverse effects cannot be identified during contactless outcome assessment (i.e. review of health administrative data, radiographs, magnetic resonance imaging, etc). |
| 6 | Number of dropouts and withdrawals does not exceed 20% at short‐term follow‐up or 30% at long‐term follow‐up, or both, and reasons for dropout and withdrawal are given and do not indicate substantial bias (N.B. these percentages are arbitrary, not supported by literature). |
| 7 | Data from all randomized patients are reported and analyzed in the group of original allocation, irrespective of treatment noncompliance or co‐interventions. |
| 8 | All the results from pre‐specified outcomes are adequately reported. To make this judgment, the full trial report should be compared to its published protocol pr registration. In the absence of a protocol/registration, this item should be rated as ‘yes’ only if there is sufficient information in the full trial report to support the absence of selective outcome reporting. |
| 9 | Experimental and control groups are similar at baseline regarding demographic factors, duration and severity of complaints, percentage of patients with neurological symptoms, and primary outcome measure(s). |
| 10 | There are no co‐interventions or co‐interventions are similar between experimental and control groups. |
| 11 | The reviewer determines if treatment compliance is acceptable according to data reported on intensity, duration and frequency of sessions for both index and comparison treatment(s). For example, physiotherapy treatment is usually administered over multiple sessions. This item is not relevant for single‐session treatments (i.e. surgery). |
| 12 | Timing of assessment is the same in experimental and control group(s) for all primary outcomes. |
| 13 | Other types of bias are absent. Examples of other sources of potential bias include (but are not limited to) the use of an outcome measure that lacks validity (i.e. does not measure what it intends to measure) and disclosed or suspected undisclosed conflict of interest (COI). For example, the COI statement of an industry‐sponsored trial must explicitly state that funders had no role in data collection or statistical analyses. |
random allocation (item 1):
allocation concealment (item 2):
blinding of outcome assessors (item 5):
acceptable dropout rate (item 6); and
intention‐to‐treat analysis (item 7).
We considered the trial to be at high risk of bias if any of these five criteria had been assessed as ‘unsure’ or ‘no’. We made this choice as part of a set of post‐protocol decisions, which are listed in Differences between protocol and review.
Measures of treatment effect
For each included trial, we estimated treatment effects measured on a continuous scale by the difference between group means (MD) and the 95% confidence interval (CI) at specific time points, or by the difference in change scores between groups, according to available data. We converted continuous measures assessing the same construct into a common 0‐ to 100‐point scale (e.g. pain scores measured on a 0‐ to 10‐point scale were multiplied by 10). We calculated treatment effects for dichotomous outcome as risk ratios (RR) and 95% CI. We classified the effect according to its magnitude as small (MD less than 10 points on a 0‐ to 100‐point scale; RR < 1.25 or > 0.8), moderate (MD of 10 to 20 points on a 0‐ to 100‐point scale; RR 1.25 to 2.0, or 0.5 to 0.8), or large (MD > 20 points on a 0‐ to 100‐point scale; RR > 2.0 or < 0.5) (Rubinstein 2012). We considered effects of at least moderate magnitude (i.e. ≥ 10 points or RR ≥ 1.25 or ≤ 0.8) as clinically important (Saragiotto 2016). The classification of the effect size according to its magnitude was part of a set of post‐protocol decisions (please see Differences between protocol and review).
For dichotomous outcomes, we also provided the absolute percent difference and the relative percent change from baseline between experimental and control groups. We calculated the absolute percent change from the difference in the risks between the intervention and control group, as calculated in GRADEpro (GRADEpro GDT), and we expressed this as a percentage. We calculated the relative percent change as the RR minus 1 and expressed it as a percentage. Additionally, in the presence of a clinically important effect, we reported the number needed to treat for an additional beneficial outcome (NNTB) or number needed to treat for an additional harmful outcome (NNTH). For dichotomous outcomes, we calculated the NNTB or NNTH from the control group event rate and the risk ratio using the Visual Rx NNT calculator (Cates 2008). For continuous measures, we calculated the NNTB using the Wells calculator (available at the Cochrane Musculoskeletal Group Editorial office, musculoskeletal.cochrane.org). The decision to report the absolute and relative effects was a post‐protocol decision, and it is described in Differences between protocol and review.
Unit of analysis issues
For all included trials, the unit of analysis was the individual. We made a post‐protocol decision to follow the guidance on cluster‐RCTs and cross‐over trials in sections 16.3 and 16.4 of the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2011). However, we did not find any trial with these designs to include in the review. For trials comparing multiple treatments against the McKenzie method, we combined comparison groups to create a single pair‐wise comparison, or we selected only one comparison group, depending on the nature of the treatment. The latter (selection of one comparison group) was part of a set of post‐protocol decisions, listed in Differences between protocol and review.
Dealing with missing data
Where measures of central tendency and dispersion were reported in the included trials, we calculated means and standard deviations (SDs) using the methods described in the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2011). In cases where measures of dispersion were not reported, we attempted to obtain additional data by contacting the trial authors. If we were unable to obtain this information, we used SDs from baseline assessments or the pooled SD of the remaining trials (Machado 2009). In trials reporting results of both intention‐to‐treat and per‐protocol analyses, we used the former, except for the analysis of adverse events. In cases where there were missing participants due to dropout, we addressed the potential impact of the missing data in our assessment of risk of bias.
Assessment of heterogeneity
We assessed the presence of between‐trial statistical heterogeneity using the Chi² test and I² statistic (Higgins 2003). We considered I² values above 75% as indicative of considerable statistical heterogeneity. We assessed clinical heterogeneity among trials in multiple planned subgroup analyses, as described below.
Assessment of reporting biases
We followed simple strategies to prevent and identify potential reporting biases. To minimize publication bias, we performed a comprehensive search strategy in multiple databases. We also searched for trials investigating the effectiveness of the McKenzie method but naming the method differently (e.g. “physical therapy”, “flexion and extension exercises”, etc.). We also searched online registries of clinical trials (ClinicalTrials.gov and International Clinical Trials Registry Platform [ICTRP]) for trials that were completed but have not yet been published, in order to identify a potential publication bias. Additionally, we assessed selective outcome reporting along with the risk of bias assessments by checking for inconsistencies between the protocol and the trial report, or within the published report.
Data synthesis
Where there were at least two sufficiently homogenous trials comparing the effect of the McKenzie method with a comparison group of a similar nature, we performed a meta‐analysis to obtain a pooled estimate of the effect with a 95% CI. We used a random‐effects model in all meta‐analyses (this was a post‐protocol decision as listed in Differences between protocol and review). We used Review Manager 2020 for the analysis.
Subgroup analysis and investigation of heterogeneity
We planned to evaluate possible clinical heterogeneity among the synthesized primary outcomes (i.e. pain and disability) through subgroup analyses if there were a sufficient number of trials (Higgins 2011). We planned to perform these analyses in subsets of trials to investigate whether the magnitude of the effects of the McKenzie method differ among populations with distinct clinical presentations. We planned to independently evaluate two clinical features: (1) duration of the NSLBP episode and (2) presence of centralization. We planned to do a subgroup analysis of acute and (sub)acute NSLBP if trials separately included participants with acute or (sub)acute NSLBP or if data were separately presented for acute and (sub)acute participants. We planned to perform a subgroup analysis by centralization, as it is believed to indicate a more favourable prognosis (Donelson 1990; Long 1995; Karas 1997; Sufka 1998; Werneke 1999; Werneke 2001). It also appears to identify people who respond better to the McKenzie method (Brennan 2006; Fritz 2003). For subgroup analysis, trials must have reported that the majority of participants who received the McKenzie method (i.e. at least 80%) presented the centralization phenomenon, a clear directional preference during the evaluation, or were classified as having a ‘derangement syndrome’(McKenzie 2003a; McKenzie 2003b). We attempted to contact the authors of the original trials to acquire subgroup data when needed.
We planned to use the formal test for subgroup interactions in Review Manager 2020 and use caution in the interpretation of subgroup analyses as advised in section 9.6 of the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2011).
Sensitivity analysis
We planned a sensitivity analysis to explore the robustness of effect estimates by excluding from the analysis those trials judged to have a high risk of bias.
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach to assess the overall certainty of the evidence for each outcome from a group of trials reporting on the same comparison, as recommended in the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2011), and adapted in the updated CBN method guidelines (Furlan 2015). We rated the certainty of the evidence as high, moderate, low, or very low, according to the performance of the trials against five domains:
study design and risk of bias;
inconsistency (considerable between‐group statistical heterogeneity (i.e. I² > 75%));
indirectness (inability to generalize);
imprecision (insufficient or imprecise data); and
publication bias.
We set the certainty of the evidence at high when trials with a low risk of bias provided results for the outcome, and we reduced it by a level for each domain not met (Appendix 3).
We generated summary of findings (SoF) tables to report results of data synthesis, following the recommendations of the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2011), and GRADE guidelines (Guyatt 2013). We created SoF tables including the two primary outcomes (pain intensity and disability at short‐term (2 weeks) and intermediate‐term follow‐ups) and adverse events for each of the investigated comparisons. We made decisions about the outcomes and time points to be included in SoF tables as part of a set of post‐protocol decisions, which are listed under Differences between protocol and review.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
Results of the search
The search strategy identified a total of 2370 records (including 39 registered trials). After de‐duplication, 1522 records remained. Of these, we assessed 85 full‐text articles for eligibility. We included five trials that fulfilled all inclusion criteria (Cherkin 1998; Gillan 1998; Machado 2010; Schenk 2003; Schenk 2012). We identified three ongoing trials (ACTRN12616000735459; CTRI/2017/01/007683; RBR‐4yz96t). We present the study flow diagram in Figure 1.
1.
Study flow diagram
Included studies
The five trials included in this review were conducted in high‐income countries: three trials were conducted in the USA (Cherkin 1998; Schenk 2003; Schenk 2012), one in Australia (Machado 2010), and one in Scotland (Gillan 1998). All trials were published in English.
Three trials received funding from non‐commercial funders (Cherkin 1998; Gillan 1998; Machado 2010). The remaining two trials failed to provide information on potential funding sources (Schenk 2003; Schenk 2012).
Trial participants
The sample size for each included trial ranged from 25 to 321, totaling 563 participants. Three trials recruited participants from primary care (Cherkin 1998; Gillan 1998; Machado 2010). Two trials recruited participants from tertiary care (Schenk 2003; Schenk 2012). Machado 2010 and Schenk 2012 reported exclusively on acute NSLBP while Cherkin 1998, Gillan 1998, and Schenk 2003 included a mix of participants with acute and subacute NSLBP. All trials included participants of both sexes.
Cherkin 1998 and Machado 2010 reported that participants allocated to the group treated with the McKenzie method were classified as having one of the three McKenzie syndromes (derangement, dysfunction, and postural syndrome). In Cherkin 1998, 92% were classified as having derangement (no information was provided for the classification of the remaining 8%), while in Machado 2010, 94% and 6% were classified as having derangement and dysfunction syndrome, respectively. One trial included only participants with derangement syndrome (Schenk 2003). The remaining three trials did not provide information on participants' classification.
Interventions
Details of the interventions in each trial are presented in the Characteristics of included studies table. Treatment was applied during three to nine sessions, which were distributed over three days to four weeks. Four included trials did not provide information about treatment duration (Gillan 1998; Machado 2010; Schenk 2003; Schenk 2012).
In four trials, the McKenzie method was delivered by highly trained clinicians who had demonstrated competency in the method (i.e. attained a credentialed status; Gillan 1998; Machado 2010; Schenk 2003; Schenk 2012). In the remaining trial, only one of 13 clinicians applying the method had not completed an advanced credentialing program (Cherkin 1998). In two trials, clinicians had more than 10 years of clinical experience with the McKenzie method (Cherkin 1998; Schenk 2003). In Machado 2010, credentialed physiotherapists had also attended a training session with a senior McKenzie educator prior to the commencement of the study. Two trials did not provide information about clinicians' experience (Gillan 1998; Schenk 2012). All included trials were considered to use treatment procedures that reflected the original principles of the McKenzie method. In two trials, participants in the McKenzie method group also received a copy of McKenzie’s Treat Your Own Back book and a lumbar support (original McKenzie lumbar roll) (Cherkin 1998; Machado 2010). No information about the use of the book or lumbar roll was provided in the remaining trials, and none of the trials reported the use of manual techniques as part of continuous force progression during treatment with the McKenzie method.
Two trials compared the McKenzie method to our main comparison (i.e. minimal intervention (Cherkin 1998; Machado 2010)). In one trial, the minimal intervention consisted of an educational booklet informing about potential causes, prognosis, and management of NSLBP (Cherkin 1998). In another trial, first‐line care was applied to both study groups, and the McKenzie method was provided in addition to first‐line care in participants in the experimental group (Machado 2010).
Three trials compared the McKenzie method to manual therapy (Cherkin 1998; Schenk 2003; Schenk 2012). Cherkin 1998 used chiropractic manipulation, Schenk 2003 used joint mobilization, and Schenk 2012 used spinal thrust manipulation. The remaining trial compared the McKenzie method to other interventions, including non‐specific back massage in addition to standard back care advice (Gillan 1998). None of the included trials compared the McKenzie method to other types of exercises.
Major outcomes
Pain intensity and disability were assessed in all the included trials, except in Gillan 1998.
Pain intensity
Pain was measured on a numeric rating scale (NRS) in three trials (Cherkin 1998; Machado 2010; Schenk 2012). Schenk 2003 measured pain on a visual analogue scale (VAS). We converted all pain outcomes to a 0‐ to 100‐point scale (zero indicates no pain and 100 indicates the worst pain possible).
Disability
Disability was measured by the Roland‐Morris Disability Questionnaire (RMDQ) in two trials (Cherkin 1998; Machado 2010). Three trials used the Oswestry Disability Index (ODI) to measure disability (Gillan 1998; Schenk 2003; Schenk 2012). We converted all disability outcomes to a 0‐ to 100‐point scale (zero indicates no disability and 100 indicates severe disability).
Adverse events
None of the included trials reported any adverse events.
Minor outcomes
Two trials assessed the need for future visits to healthcare professionals (Cherkin 1998; Machado 2010). None of the trials assessed general health status, return to work, and patient satisfaction.
Follow‐up
All trials assessed at least one outcome in the short term (closest to two weeks), and two trials provided data on assessments in the intermediate term (closest to three months) (Cherkin 1998; Gillan 1998).
Excluded studies
After full‐text screening, we excluded 17 trials (Arab 2016; Brennan 2006; Buswell 1982; Dettori 1995; Elnaagar 1991; Erhard 1994; Hosseinifar 2013; Kayani 2021; Lohana 2021; Long 2004; Malmivaara 1995; Mayer 2005; Srivastava 2020; Stankovic 1990; Stankovic 1995; Waqqar 2016; Yamim 2016). We judged that these trials did not follow the original principles of the McKenzie method (e.g. management or treatment strategy in line with the evaluation and classification, including repeated or sustained end‐range movements of the spine or postural education, or both).
The exclusion of the other 60 trials was due to the following reasons: trial did not include people with NSLBP (n = 5) (Mahmoudzadeh 2016; Nwuga 1985; Ponte 1984; Thackeray 2016; Van Ravensberg 2005); trial included people with chronic NSLBP (n = 20) (Ali 2013; Bid 2017; Callaghan 1994; Cuesta‐Vargas 2011; Garcia 2013; Garcia 2018; Halliday 2016; Hasanpour 2017; Helmhout 2004; Mannion 1999; Mbada 2014; Mbada 2017; Mazloum 2016; Moncelon 2015; Murtezani 2015; Petersen 2002; Petersen 2007; Petersen 2011; Rasmussen 2008; Sakai 2008); trial included people with NSLBP of mixed duration and it was impossible to separate data from those with (sub)acute NSLBP (n = 7) (Bonnet 2011; Manca 2007; Miller 2005; Moffet 2006; Nechvátal 2022; Paatelma 2008; RBR‐5mcvt6); trial was not an RCT (n = 7) (ACTRN12613000267752; Apeldoorn 2010; Apeldoorn 2016; Dimaggio 1987; Fernando 1991; Foster 2010; Mujic 2004); trial proposed McKenzie treatment in both groups (n = 3) (UMIN000018380; Szulc 2015; Udermann 2004); trial evaluated the effectiveness of other interventions (n = 17) (Ali 2002; Apeldoorn 2010; Apeldoorn 2012; Apeldoorn 2012b; CTRI/2012/07/002774; Djavid 2007; Hahne 2011; Helmhout 2008; IRCT201107197057N1; Nazzal 2013; NCT01794962; Powers 2008; Rittweger 2002; Skargen 1997; Skargen 1998; Smith 2011; Yeung 2003); trial evaluated mixed intervention, the treatment group includes three types of exercise programmes and it is not possible to describe the results for McKenzie therapy individually (n = 1) (Sorensen 2010).
Risk of bias in included studies
We based the decision on the overall risk of bias for each trial on ratings of the following key quality criteria: random allocation, allocation concealment, blinding of outcome assessors, acceptable dropout rate, and intention‐to‐treat analysis. We judged all included trials to be at high risk of bias as they rated 'no' or 'unsure' for at least one of these criteria. Figure 2 describes the percentage of trials with a low, unclear, or high risk of bias for each of these criteria. Figure 3 presents the results of the risk of bias assessment for individual trials. Additional details about risk of bias judgments are shown in the Characteristics of included studies table.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
We judged four trials to be at low risk of selection bias as randomization was adequately described (Gillan 1998; Machado 2010; Schenk 2003; Schenk 2012). One trial did not report sufficient information that could confirm the use of an adequate randomization procedure (Cherkin 1998). We attempted to contact the trial author, but because we were not able to obtain any additional information, we deemed the trial to be at unclear risk of bias for random sequence generation.
Two trials met the criterion for allocation concealment and we judged them to be at low risk of bias (Cherkin 1998; Machado 2010). We judged the remaining three trials to be at high risk of bias for allocation concealment (Gillan 1998; Schenk 2003; Schenk 2012).
Blinding
All included trials failed to meet the three criteria for blinding: that is, they were rated ‘no’ for blinding of participants, care providers, and outcome assessors. Although some trials have reported that outcome assessors were kept blinded to group allocation, we still considered these trials to be at high risk of bias for this criterion since their index and comparison treatments were not indistinguishable, and all their primary outcomes were self‐reported (see Table 5).
Incomplete outcome data
All four trials provided adequate information about missing data and had no more than 20% or 30% of data missing for short‐, intermediate‐, or long‐term follow‐ups, respectively, and we therefore considered them to be at low risk of attrition bias (Cherkin 1998; Machado 2010; Schenk 2003; Schenk 2012). One trial exceeded the 20% cut‐off for dropouts at its short‐term follow‐up and we considered it to be at high risk of attrition bias (Gillan 1998).
Intention‐to‐treat analysis
Three trials met the criterion for intention‐to‐treat analysis and we considered them to be at low risk of bias (Cherkin 1998; Machado 2010; Schenk 2003). The analyses of the remaining trials were not based on intention‐to‐treat principles and we considered them to be at high risk of bias (Gillan 1998; Schenk 2012).
Selective reporting
It was impossible to determine if reporting bias was present in three trials without a published or registered protocol (Cherkin 1998; Gillan 1998; Schenk 2003). Therefore, we judged these trials to be at unclear risk of bias. Two trials pre‐specified outcomes in their published protocols and we judged both to be at low risk of reporting bias (Machado 2010; Schenk 2012).
Group similarity at baseline
All included trials met the criterion for group similarity; that is, the experimental and control groups were similar regarding the most important prognostic factors at baseline (Cherkin 1998; Gillan 1998; Machado 2010; Schenk 2003; Schenk 2012).
Co‐interventions
Two trials reported that co‐interventions were not allowed and we therefore considered them to be at low risk of bias (Schenk 2003; Schenk 2012). We judged one trial to be at high risk of bias due to unbalanced co‐interventions between experimental and control groups (Cherkin 1998). We judged another trial to be at unclear risk of bias because it failed to provide information about co‐interventions, and we could not obtain additional information after contacting the trial author (Gillan 1998).
Compliance
Treatment compliance was found to be acceptable in four trials (Gillan 1998; Machado 2010; Schenk 2003; Schenk 2012). In one trial, treatment compliance was not balanced between index and comparison treatments (Cherkin 1998).
Timing of assessment
In all five trials, assessments were performed at the same time in experimental and control groups, for all primary outcomes (Cherkin 1998; Gillan 1998; Machado 2010; Schenk 2003; Schenk 2012). We considered them to be at low risk of bias.
Other potential sources of bias
We judged one trial to be at high risk of bias because participants were allowed to cross‐over from the index to comparison treatment (and from comparison treatment to index treatment) at the second week visit if there was no improvement with the originally assigned treatment (Schenk 2012). We judged the other four included trials to be at low risk of other bias (Cherkin 1998; Gillan 1998; Machado 2010; Schenk 2003).
Effects of interventions
See: Table 1; Table 2; Table 3
See: Table 1; Table 2; Table 3.
McKenzie method versus minimal intervention
See: Table 1 (main comparison).
Major outcomes
There is low‐certainty evidence (downgraded one level due to risk of bias and one level due to imprecision) from two trials that the McKenzie method may result in a slight reduction (not clinically important) in pain at short‐term when compared to minimal intervention (Cherkin 1998; Machado 2010). MD was 7.30 points better (95% CI 12.04 better to 2.56 better; 328 participants) after the McKenzie method. At intermediate‐term, there is low‐certainty evidence (downgraded one level due to risk of bias and one level due to imprecision) from Cherkin 1998, that the McKenzie method may not reduce pain when compared to minimal intervention. MD was 5.00 points better (95% CI 14.29 better to 4.29 worse; 180 participants) after the McKenzie method (Analysis 1.1).
1.1. Analysis.

Comparison 1: McKenzie method versus minimal intervention, Outcome 1: Pain intensity
There is low‐certainty evidence (downgraded one level due to risk of bias and one level due to imprecision) from two trials that the McKenzie method may not reduce disability at short‐term when compared to minimal intervention (Cherkin 1998; Machado 2010). MD was 2.74 points better (95% CI 7.52 better to 2.04 worse, 328 participants) after McKenzie method. At intermediate‐term, there is low‐certainty evidence (downgraded one level due to risk of bias and one level due to imprecision) from Cherkin 1998, that the McKenzie method may not reduce disability when compared to minimal intervention. MD was 0.87 points better (95% CI 7.31 better to 5.57 worse; 180 participants) after McKenzie method (Analysis 1.2).
1.2. Analysis.

Comparison 1: McKenzie method versus minimal intervention, Outcome 2: Disability
Adverse events were not measured in any included trial.
Minor outcomes
There is low‐certainty evidence (downgraded one level due to risk of bias and one level due to imprecision) from Machado 2010, that the McKenzie method may result in large and clinically important reduction of additional health care at short‐term compared to minimal intervention (RR 0.27; 95% CI 0.11 to 0.70; 139 participants), corresponding to an absolute difference of 19% fewer healthcare usage (23% fewer to 8% fewer), and relative difference of 73% fewer healthcare usage (89% fewer to 30% fewer). In the same trial, the NNTH is 5 (3 to 14) participants treated with minimal intervention for one additional health care use (Analysis 1.3).
1.3. Analysis.

Comparison 1: McKenzie method versus minimal intervention, Outcome 3: Future visits to healthcare professionals
General health status and return to work were not measured in any included trial.
Subgroup analyses
Subgroup analysis assessing the duration of the NSLBP episode (acute versus subacute) was not possible because trials included only participants with acute NSLBP. Subgroup analysis assessing the presence of centralization (centralization versus no centralization) was not possible due to the lack of data.
Sensitivity analyses
A sensitivity analysis to explore the robustness of effect estimates was not possible as all included trials were at high risk of bias.
McKenzie method versus manual therapy
See: Table 2.
Major outcomes
There is low‐certainty evidence (downgraded one level due to risk of bias and one level due to imprecision) from three trials that the McKenzie method may not reduce pain at short‐term when compared to manual therapy (Cherkin 1998; Schenk 2003; Schenk 2012). MD was 8.67 points better (95% CI 27.37 better to 10.02 worse; 298 participants) after McKenzie method. At intermediate‐term, there is low‐certainty evidence (downgraded one level due to risk of bias and one level due to imprecision) from Cherkin 1998, that the McKenzie method may result in little increase (not clinically important) in pain when compared to manual therapy. MD was 7.00 points worse (95% CI 0.70 worse to 13.30 worse; 235 participants) after McKenzie method (Analysis 2.1).
2.1. Analysis.

Comparison 2: McKenzie method versus manual therapy, Outcome 1: Pain intensity
There is low‐certainty evidence (downgraded one level due to risk of bias and one level due to imprecision) from three trials that the McKenzie method may not reduce disability at short‐term when compared to manual therapy (Cherkin 1998; Schenk 2003; Schenk 2012). MD was 4.98 points better (95% CI 15.00 better to 5.04 worse; three trials, 298 participants) after McKenzie method. There is low‐certainty evidence (downgraded one level due to risk of bias and one level due to imprecision) from Cherkin 1998, that the McKenzie method may not reduce disability at intermediate‐term when compared to manual therapy. MD was 4.30 points worse (95% CI 0.72 better to 9.32 worse; 235 participants) after McKenzie method (Analysis 2.2).
2.2. Analysis.

Comparison 2: McKenzie method versus manual therapy, Outcome 2: Disability
None of the trials measured adverse events.
Minor outcomes
None of the trials measured general health status, future visits to healthcare professionals, patient satisfaction, and return to work.
Subgroup analyses
Subgroup analysis assessing the duration of the NSLBP episode (acute versus subacute) was not performed due to an insufficient number of included trials (n = 2). Subgroup analysis assessing the presence of centralization (centralization versus no centralization) was not possible due to the lack of data.
Sensitivity analyses
A sensitivity analysis to explore the robustness of effect estimates was not possible as all included trials were at high risk of bias.
McKenzie method versus other interventions
See: Table 3.
Only one trial compared the McKenzie method with non‐specific low back massage plus standard back care advice (Gillan 1998).
Major outcomes
Because of very low‐certainty evidence (downgraded two levels due to risk of bias and one level due to imprecision) from Gillan 1998, the evidence is very uncertain about the effects of McKenzie method on disability at short‐ or intermediate‐term when compared to other interventions. MD was 4.00 points worse (95% CI 15.44 better to 23.44 worse; 30 participants) after McKenzie method at short‐term. At intermediate‐term, MD was 10.00 points worse (95% CI 8.95 better to 28.95 worse; 25 participants) after McKenzie method (Analysis 3.1).
3.1. Analysis.

Comparison 3: McKenzie method versus other interventions, Outcome 1: Disability
Pain and adverse events were not assessed in the trial reporting on this comparison.
Minor outcomes
General health status, future visits to healthcare professionals, patient satisfaction, and return to work were not assessed in the trial reporting on this comparison.
Subgroup analyses
Subgroup analyses were not possible as this comparison was based on only one trial.
Sensitivity analyses
Sensitivity analysis was not possible as this comparison was based on only one trial.
Discussion
Summary of main results
This Cochrane Review investigated the effectiveness of the McKenzie method for people with (sub)acute NSLBP. When compared to minimal intervention, there is low‐certainty evidence that the McKenzie method may result in a slight reduction (not clinically important) in pain in the short term. However, it appeared to have no effect on disability in the short term, nor on pain or disability in the intermediate term. When compared to manual therapy, there is low‐certainty evidence that the McKenzie method may not reduce pain in the short term or disability in the short and intermediate term (although it may result in a slight increase in pain at intermediate‐term follow‐up). Finally, because of very low‐certainty evidence, it is unclear if the McKenzie method reduces disability at all follow‐ups when compared to other interventions (back massage plus standard back care advice).
It was not possible to conduct subgroup analyses to explore clinical heterogeneity (e.g. different duration of NSLBP or presence of centralization) due to the insufficient number of studies included in each comparison. Additionally, given the high risk of bias of all studies included in this review, we could not perform sensitivity analysis to investigate the robustness of our estimates by excluding studies with high risk of bias from the analysis.
Overall completeness and applicability of evidence
The five trials included in this review were conducted in high‐income countries. Trials recruited middle‐aged participants from primary and tertiary care, who presented with NSLBP of acute (less than six weeks) or (sub)acute (less than three months) duration. We believe that these settings and participants are representative of the broader population, and that there is no obvious threat to the generalizability of the findings. The inclusion of trials in which the McKenzie method was delivered by credentialed clinicians further contributes to the generalizability of the findings, given that a proper implementation of the treatment would be expected by these highly trained health professionals.
Quality of the evidence
Assessments of the certainty of evidence using the GRADE approach indicated a large degree of uncertainty (very low‐ or low‐certainty evidence) in the results of this review. Imprecision was one important problem, as sample sizes were mostly small. Only a few trials reported on each of the investigated comparisons (e.g. from a total of 11 comparisons, only four included more than one trial). This resulted in estimates with wide confidence intervals that include the possibility of a small or no effect and important benefit. A high overall risk of bias also contributed to the uncertainty of evidence. When assessing the risk of bias of individual trials, we used a conservative approach to assess blinding of outcome assessors (it was considered present only if the participant was blinded), which acknowledges the self‐reported nature of the primary outcome measures investigated in this review.
Potential biases in the review process
It was not possible to assess publication bias using funnel plots due to the low number of included trials. When publication bias is present, it is expected that small negative trials are less likely to be published and small positive trials could then lead to an overestimation of the treatment effect. Given that trials included in our review showed mostly trivial effects favouring the McKenzie method, we consider that publication bias is unlikely.
We excluded a number of trials from this review. We excluded three trials because they analyzed data from participants with a mixed duration of NSLBP (acute, subacute, and chronic symptoms; Bonnet 2011; Miller 2005; Moffet 2006). We contacted trial authors, and they indicated it was not possible to separate the data. We minimized the risk of missing relevant trials by using a highly sensitive search strategy with no language restrictions.
We are confident that the estimates presented in this review are accurate. We followed rigorous methods in accordance with the most recent Cochrane guidelines (Furlan 2015). As some of the recommendations from these guidelines were released after the publication of the review protocol, we adapted the protocol in order to incorporate them. We have clearly described all changes in the Differences between protocol and review section. We have reported information about potential conflicts of interests and how we handled them during the review process in the Declarations of interest.
Agreements and disagreements with other studies or reviews
Three previous reviews investigated the effects of the McKenzie method for people with (sub)acute low back pain (Clare 2004; Lam 2018; Machado 2006). It is difficult to compare our findings because of their different methodological aspects. Clare 2004 evaluated NSLBP of mixed duration while Lam 2018 tested treatments that did not reflect McKenzie's original principles, as well as differences in the grouping of comparison treatments. Nevertheless, the small effects found in our review are somewhat consistent with the findings from these previous reviews. For instance, Clare 2004 found that the McKenzie method slightly reduced pain and disability in the short term when compared to other conservative treatments (NSAIDS, education, back massage and back care advice, strength training, and spinal mobilization). Machado 2006 concluded that the McKenzie method does not offer clinically important benefits in pain and disability when compared with passive therapies (including educational booklets, ice packs, and massage). Lam 2018 found moderate‐ to high‐certainty evidence that the McKenzie method is not clinically superior to other interventions (i.e. no intervention, education, or manual therapy) for reducing pain and disability in people with acute LBP.
We found that there is low‐certainty evidence that the McKenzie method may reduce healthcare use in the short term but not in the long term when compared to minimal intervention. Campos 2020 found promising findings regarding the effects of McKenzie‐based self‐management exercise and education compared to minimal intervention in reducing healthcare use when LBP recurs.
Authors' conclusions
Implications for practice.
At present, the McKenzie method is not listed among non‐pharmacological treatments recommended by clinical practice guidelines for the management of people with (sub)acute NSLBP (ACP 2017; NICE 2016). The Clinical Guidelines Committee of the American College of Physicians (ACP) strongly recommend that people with this condition are treated with superficial heat over the lower back, manual therapy, and acupuncture (ACP 2017). The 2016 guidelines from the National Institute for Health and Care Excellence (NICE) also recommend manual therapy (such as spinal manipulation, mobilization, and massage), but only as a treatment that is applied in conjunction with self‐management and exercise. However, exercises recommended in NICE guidelines comprise non‐tailored group exercises, differing substantially from those used in the McKenzie method (NICE 2016).
Our findings suggest that the McKenzie method is not an effective treatment for (sub)acute NSLBP, as we found that very low‐ to low‐certainty evidence demonstrated a minimal beneficial effect (or no effect) for pain and disability. Current clinical practice guideline recommendations should not change based on the results of this Cochrane Review.
Implications for research.
Despite the widespread belief that customized exercise programs enable better outcomes for people with NSLBP, treatment effects of the McKenzie method on pain and disability were generally very small or absent. Considering that all included trials were at high risk of bias and yet they did not demonstrate a clinically important benefit, it is unlikely that future low risk of bias studies will show different results.
The underestimation of treatment effects due to the inclusion of trials not adequately implementing the McKenzie method has been a major source of criticism of another review on this topic (Machado 2006). However, we are confident that this was not the case in our review, as we included trials in which the management of participants was in line with the evaluation and classification proposed by the McKenzie method.
The thoughtful design of future trials (and improved reporting) could reduce uncertainty by minimizing the risk of performance and detection bias. Although blinding of participants is particularly difficult in trials of non‐pharmacological treatments for NSLBP, the assessment of participants' baseline expectations of treatment may contribute to judgements on the risk of bias given their recognized role as treatment‐effect modifiers (Beasley 2017; Kalauokalani 2001). Additionally, the implementation of alternative strategies to maximize protocol adherence, such as the use of structurally equivalent comparison groups, could also reduce the likelihood of performance biases, such as imbalanced co‐interventions (Cherkin 1998). Finally, future trials on the effectiveness of the McKenzie method for (sub)acute NSLBP should incorporate the investigation of potential adverse events as well as participant‐reported outcomes that reflect both the personal and societal burden of (sub)acute NSLBP. One example of the latter is the assessment of additional healthcare use in trials that are fully powered for this outcome, which was analyzed in our review as a minor outcome.
What's new
| Date | Event | Description |
|---|---|---|
| 17 August 2023 | Amended | Minor text inconsistencies between sections corrected. |
History
Protocol first published: Issue 3, 2012 Review first published: Issue 4, 2023
Acknowledgements
We would like to thank the board of Directors of the McKenzie Institute International for providing feedback on whether treatment procedures reported in trials were a true reflection of McKenzie principles. We would also like to thank Rachel Mason from Spinal Publications NZ Ltd for the permission to reproduce the pictures from McKenzie's textbooks. We would also like to thank the institutions providing funding to the authors of this review. Alessandra Narciso Garcia was supported by Coordination for the Improvement of Higher Education Personnel (CAPES), Brazil and Matheus O Almeida was supported by São Paulo Research Foundation (FAPESP). Chung‐Wei Christine Lin is supported by a Leadership Fellowship of the National Health and Medical Research Council, Australia.
Appendices
Appendix 1. Loading strategies in the McKenzie method
1. Dynamic strategies
Dynamic loading strategies include repeated movements performed in different directions. While performing these repeated movements, patients are asked to report any changes in the intensity or location of their pain, such as centralization. A potential increase or decrease in the spinal range of motion is also assessed by the therapist.
Flexion in standing
With feet shoulder‐width apart and maintaining knee extension, the patient is asked to flex the spine as far as pain allows and to return to neutral standing (Figure 10A). This movement is then repeated up to 10 times.
4.
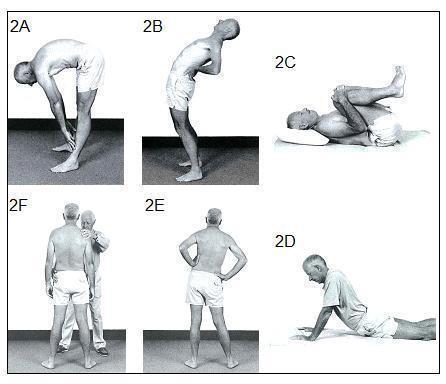
Dynamic loading strategies: 2A, flexion in standing; 2B, extension in standing, 2C, flexion in lying; 2D, extension in lying; 2E, side glide in standing, 2F, therapist‐assisted side glide in standing. Reproduced with permission of Spinal Publications NZ Ltd
Extension in standing
With feet shoulder‐width apart and maintaining knee extension, the patient is asked to place the hands at the lower back, to bend backwards as far as pain allows and to return to neutral standing (Figure 10B). This movement is then repeated up to 10 times.
Flexion in lying
Lying in supine with the feet resting flat on the plinth, the patient is asked to bring the knees up to the chest and to apply overpressure so maximum lumbar flexion is achieved (Figure 10C). The patient is then asked to return to the initial position and to repeat the movement up to 10 times.
Extension in lying
Lying prone with hands directly under the shoulders, the patient is asked to raise the upper body by extending the arms and maintaining the thighs and legs on the plinth (Figure 10D). The patient is then asked to return to the initial position and to repeat the movement up to 10 times.
Side glide in standing
Standing with the feet shoulder‐width apart and maintaining shoulders parallel to the ground, the patient is asked to move the hips to the left (left side gliding) or right (right side gliding) while their trunk remains in a neutral position (Figure 10E). The patient is then asked to return to the initial position and to repeat the movement up to 10 times. Therapist assistance may be needed to perform the movement (Figure 10F), particularly when there is a lateral shift deformity, which consists of an acute non‐structural misalignment of the spine (also known as sciatic scoliosis).
2. Static strategies
Static loading strategies include sustained postures that are held at end‐range for up to five minutes. Different postures may be used during the examination, including slouched sitting (Figure 11A), sitting erect, long sitting, standing slouched, standing erect, and lying prone in extension (Figure 11B).
5.
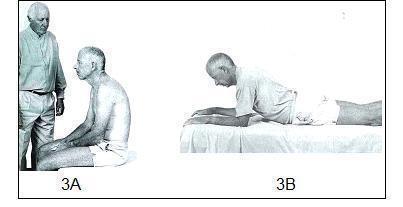
Static loading strategies: 3A, slouched sitting; 3B, lying prone in extension. Reproduced with permission of Spinal Publications NZ Ltd
3. Other strategies
When the above dynamic and static loading strategies fail to provide a clear symptom response to assist in the classification of low back pain, overpressure may be applied by the therapist. For example, while the patient performs extension in lying as described above, the therapist applies overpressure perpendicular to the spine still allowing the movement to occur (Figure 12A). The magnitude of the force applied by the therapist is dictated by the symptom response. For example, more pressure should be applied if this causes less pain. Another potential variation of this loading strategy is to perform the movement with the hips off‐centre, usually shifted away from the painful side (Figure 12B).
6.
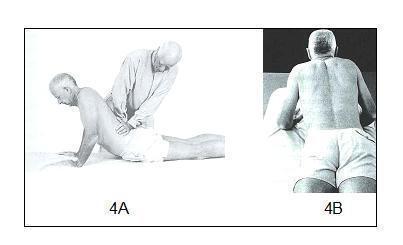
Other strategies: 4A, extension in lying with therapist overpressure; 4B, extension in lying with hips off‐centre. Reproduced with permission of Spinal Publications NZ Ltd
Appendix 2. Search strategies
CENTRAL
1 dorsalgia.tw,kf.
2 exp Back Pain/
3 (backache or back ache).tw,kf.
4 back pain.tw,kf.
5 exp Low Back Pain/
6 (lumb* adj3 pain).tw,kf.
7 coccyx.tw,kf.
8 coccydynia.tw,kf.
9 sciatica.tw,kf.
10 exp sciatic neuropathy/
11 spondylosis.tw,kf.
12 lumbago.tw,kf.
13 or/1‐12
14 McKenzie.tw,kf.
15 Mechanical Diagnosis.tw,kf.
16 end‐range.tw,kf.
17 active range of motion.tw,kf.
18 unloaded exercise.tw,kf.
19 directional preference.tw,kf.
20 extension exercise.tw,kf.
21 centralization.tw,kf.
22 or/14‐21
23 Physical Therapy Modalities/
24 subgroups.tw,kf.
25 23 and 24
26 22 or 25
27 13 and 26
MEDLINE
1 randomised controlled trial.pt.
2 controlled clinical trial.pt.
3 pragmatic clinical trial.pt.
4 comparative study.pt.
5 random*.ti,ab.
6 placebo.ab,ti.
7 drug therapy.fs.
8 trial.ab,ti.
9 groups.ab,ti.
10 or/1‐9
11 (animals not (humans and animals)).sh.
12 10 not 11
13 dorsalgia.tw,kf.
14 exp Back Pain/
15 (backache or back ache).tw,kf.
16 back pain.tw,kf.
17 exp Low Back Pain/
18 (lumb* adj3 pain).tw,kf.
19 coccyx.tw,kf.
20 coccydynia.tw,kf.
21 sciatica.tw,kf.
22 exp sciatic neuropathy/
23 spondylosis.tw,kf.
24 lumbago.tw,kf.
25 or/13‐24
26 McKenzie.tw,kf.
27 Mechanical Diagnosis.tw,kf.
28 end‐range.tw,kf.
29 active range of motion.tw,kf.
30 unloaded exercise.tw,kf.
31 directional preference.tw,kf.
32 extension exercise.tw,kf.
33 centralization.tw,kf.
34 or/26‐33
35 Physical Therapy Modalities/
36 subgroups.tw,kf.
37 35 and 36
38 34 or 37
39 12 and 25 and 38
Embase
1 Randomized Controlled Trial/
2 exp Controlled Clinical Trial/
3 Controlled Study/
4 Double Blind Procedure/
5 Single Blind Procedure/
6 crossover procedure/
7 placebo/
8 randomization/
9 random*.ti,ab.
10 placebo?.ti,ab.
11 allocat*.ti,ab.
12 assign*.ti,ab.
13 blind*.ti,ab.
14 (compare or comparing or compared or comparison or comparative).ti,ab.
15 (controlled adj7 (study or design or trial)).ti,ab.
16 (cross‐over or crossover).ti,ab.
17 ((singl* or doubl* or trebl* or tripl*) adj25 (blind* or mask*)).ti,ab.
18 trial.ti,ab.
19 or/1‐18
20 exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/
21 human/ or normal human/ or human cell/
22 20 and 21
23 20 not 22
24 19 not 23
25 dorsalgia.tw,kw.
26 (backache or back ache).tw,kw.
27 back pain.tw,kw.
28 exp LOW BACK PAIN/
29 exp BACKACHE/
30 (lumb* adj3 pain).tw,kw.
31 coccyx.tw,kw.
32 coccydynia.tw,kw.
33 sciatica.tw,kw.
34 sciatica/
35 exp ISCHIALGIA/
36 spondylosis.tw,kw.
37 lumbago.tw,kw.
38 or/25‐37
39 McKenzie.tw,kw.
40 Mechanical Diagnosis.tw,kw.
41 end‐range.tw,kw.
42 active range of motion.tw,kw.
43 unloaded exercise.tw,kw.
44 directional preference.tw,kw.
45 extension exercise.tw,kw.
46 centralization.tw,kw.
47 centralisation.mp.
48 or/39‐47
49 subgroups.tw,kw.
50 physiotherapy/
51 kinesiotherapy/ or movement therapy/
52 50 or 51
53 49 and 52
54 48 or 53
55 24 and 38 and 54
CINAHL
Last searched 16 April 2019
S65 S63 OR S64
S64 S62 AND EM 20160406‐20190416
S63 S62 Limiters ‐ Published Date: 20160401‐20190431
S62 S49 and S61
S61 S50 or S51 or S52 or S53 or S54 or S55 or S56 or S57 or S60
S60 S58 and S59
S59 (MH "Physical Therapy") OR (MH "Therapeutic Exercise")
S58 "subgroups"
S57 "centralization"
S56 "extension exercise"
S55 "directional preference"
S54 "unloaded exercise"
S53 "active range of motion"
S52 "end‐range"
S51 "Mechanical Diagnosis"
S50 "McKenzie"
S49 S28 and S48
S48 S35 or S43 or S47
S47 S44 or S45 or S46
S46 "lumbago"
S45 (MH "Spondylolisthesis") OR (MH "Spondylolysis")
S44 (MH "Thoracic Vertebrae")
S43 S36 or S37 or S38 or S39 or S40 or S41 or S42
S42 lumbar N2 vertebra
S41 (MH "Lumbar Vertebrae")
S40 "coccydynia"
S39 "coccyx"
S38 "sciatica"
S37 (MH "Sciatica")
S36 (MH "Coccyx")
S35 S29 or S30 or S31 or S32 or S33 or S34
S34 backache or "back ache"
S33 lumb* W3 pain
S32 back pain
S31 (MH "Low Back Pain")
S30 (MH "Back Pain+")
S29 "dorsalgia"
S28 S26 NOT S27
S27 (MH "Animals")
S26 S7 or S12 or S19 or S25
S25 S20 or S21 or S22 or S23 or S24
S24 volunteer*
S23 prospective*
S22 control*
S21 followup
S20 follow‐up
S19 S13 or S14 or S15 or S16 or S17 or S18
S18 (MH "Prospective Studies+")
S17 (MH "Evaluation Research+")
S16 (MH "Comparative Studies")
S15 latin square
S14 (MH "Study Design+") 1
S13 (MH "Random Sample")
S12 S8 or S9 or S10 or S11
S11 random*
S10 placebo*
S9 (MH "Placebos")
S8 (MH "Placebo Effect")
S7 S1 or S2 or S3 or S4 or S5 or S6
S6 triple‐blind
S5 single‐blind
S4 double‐blind
S3 trial or blind*
S2 "randomi?ed controlled trial*"
S1 (MH "Clinical Trials+")
2016 search
S62 S49 and S61
S61 S50 or S51 or S52 or S53 or S54 or S55 or S56 or S57 or S60
S60 S58 and S59
S59 (MH "Physical Therapy") OR (MH "Therapeutic Exercise")
S58 "subgroups"
S57 "centralization"
S56 "extension exercise"
S55 "directional preference"
S54 "unloaded exercise"
S53 "active range of motion"
S52 "end‐range"
S51 "Mechanical Diagnosis"
S50 "McKenzie"
S49 S28 and S48
S48 S35 or S43 or S47
S47 S44 or S45 or S46
S46 "lumbago"
S45 (MH "Spondylolisthesis") OR (MH "Spondylolysis")
S44 (MH "Thoracic Vertebrae")
S43 S36 or S37 or S38 or S39 or S40 or S41 or S42
S42 lumbar N2 vertebra
S41 (MH "Lumbar Vertebrae")
S40 "coccydynia"
S39 "coccyx"
S38 "sciatica"
S37 (MH "Sciatica")
S36 (MH "Coccyx")
S35 S29 or S30 or S31 or S32 or S33 or S34
S34 backache or "back ache"
S33 lumb* W3 pain
S32 back pain
S31 (MH "Low Back Pain")
S30 (MH "Back Pain+")
S29 "dorsalgia"
S28 S26 NOT S27
S27 (MH "Animals")
S26 S7 or S12 or S19 or S25
S25 S20 or S21 or S22 or S23 or S24
S24 volunteer*
S23 prospective*
S22 control*
S21 followup
S20 follow‐up
S19 S13 or S14 or S15 or S16 or S17 or S18
S18 (MH "Prospective Studies+")
S17 (MH "Evaluation Research+")
S16 (MH "Comparative Studies")
S15 latin square
S14 (MH "Study Design+")
S13 (MH "Random Sample")
S12 S8 or S9 or S10 or S11
S11 random*
S10 placebo*
S9 (MH "Placebos")
S8 (MH "Placebo Effect")
S7 S1 or S2 or S3 or S4 or S5 or S6
S6 triple‐blind
S5 single‐blind
S4 double‐blind
S3 clinical W3 trial
S2 "randomi?ed controlled trial*"
S1 (MH "Clinical Trials+")
PEDro
Last searched 16 April 2019
Abstract & Title: McKenzie
AND
Problem: Pain
AND
Body Part: lumbar spine, sacro‐iliac joint or pelvis
New records added since 6 April 2016
LILACS
Last searched 16 April 2019
Title, abstract, subject field: dor lombar AND tratamento
limit by year 2016 ‐ 2019
Title, abstract, subject field: (McKenzie AND (back pain OR backache OR lumbar pain OR lumbago OR dorsalgia OR sciatica))
limit by year 2016 ‐ 2019
2016 search
Title, abstract, subject field: dor lombar AND tratamento; limit to type of study: clinical trials, guideline, systematic reviews, cohort, health economic evaluation, health technology assessment, overview (all options present except case studies)
Title, abstract, subject field: McKenzie
SciELO
Last searched 16 April 2019
SciELO Network, all indexes: dor lombar AND tratamento
SciELO Network, all indexes: (McKenzie AND (back pain OR backache OR lumbar pain OR lumbago OR dorsalgia OR sciatica))
PubMed
Last searched 2016
(McKenzie AND (back pain OR backache Or lumbar pain OR lumbago OR dorsalgia OR sciatica) AND (pubstatusaheadofprint OR publisher[sb] or pubmednotmedline[sb]))
ClinicalTrials.gov
Last searched 16 April 2019
Advanced, Other terms field: (mckenzie AND (back pain OR backache OR lumbar pain OR lumbago OR dorsalgia OR sciatica))
First posted: 6 April 2016 ‐ 16 April 2019
2016 search
Advanced search, search terms field: (mckenzie AND (back pain OR backache OR lumbar pain OR lumbago OR dorsalgia OR sciatica))
WHO ICTRP
Last searched 16 April 2019
Basic search: McKenzie AND back pain OR McKenzie AND backache OR McKenzie and lumbago OR McKenzie AND lumbar pain OR McKenzie AND sciatica OR McKenzie AND dorsalgia
Selected studies with date of registration from 2016 to 2019
Appendix 3. GRADE approach to evidence synthesis
The certainty of evidence was categorized as follows:
High (⊙⊙⊙⊙): there are consistent findings among at least 75% of RCTs with no limitations of the study design; consistent, direct, and precise data, and no known or suspected publication biases. We are very confident that the true effect lies close to that of the estimate of the effect.
Moderate (⊙⊙⊙○): one of the domains is not met. We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low (⊙⊙○○): two of the domains are not met. Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect.
Very low (⊙○○○): three of the domains are not met. We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
The evidence available to answer each sub‐question was graded on the domains in the following manner:
Study design and risk of bias: refer to the results of the risk of bias assessment of the studies. If most studies (≥ 75% of studies) were classified as "low risk of bias", indicating no limitation, we did not downgrade. If most studies were classified as "unclear risk of bias", with no serious limitation (i.e. lack of allocation concealment, lack of intention‐to‐treat analysis, large loss to follow‐up), we did not downgrade. However, if most studies were classified as "unclear risk of bias", with serious limitations, we downgraded one level. If most studies were classified as "high risk of bias", indicating serious limitations, we downgraded one level. If most studies were classified as "high risk of bias", with very serious limitations, we downgraded two levels.
Inconsistency (heterogeneity): refers to unexplained heterogeneity of results. Results are considered inconsistent when: wide variance of point estimates across studies; minimal or no overlap of confidence intervals (CI); and by the results of the I² test. We downgraded one level if significant heterogeneity was presented by I² test ≥ 50%, and by two levels when heterogeneity was considerable (i.e. when I² ≥ 75%), unless there was a plausible explanation for the heterogeneity.
Indirectness (inability to generalize): refers to the extent to which the people, interventions, and outcomes in the trials are not representative of those defined in the inclusion criteria of the review; or that the results are based on an indirect comparison. We downgraded the certainty of evidence by one level if > 25% of the participants were outside the target group and by two levels when there was indirectness for two or more elements of the research question.
Imprecision (insufficient or imprecise data): refers to when studies included a low number of participants and events, and thus have a wide confidence interval for each outcome. We downgraded the certainty of evidence by one level if the 95% CI around the estimate of effect is sufficiently wide, including the possibility of a small or no effect and important benefit or harm. We downgraded by two levels when we judged we have a very serious imprecision.
Publication bias: refers to the probability of selective publication of trials and outcomes. We planned to use a funnel plot to estimate the likelihood of publication bias when there were more than 10 studies in a comparison. We downgraded one level if investigators failed to report studies (typically those that show no effect: publication bias) or outcomes (typically those that may be harmful or for which no effect was observed: selective outcome reporting bias) on the basis of results.
Data and analyses
Comparison 1. McKenzie method versus minimal intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Pain intensity | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1.1 Short‐term (closest to 2 weeks) | 2 | 328 | Mean Difference (IV, Random, 95% CI) | ‐7.30 [‐12.04, ‐2.56] |
| 1.1.2 Intermediate‐term (closest to 3 months) | 1 | 180 | Mean Difference (IV, Random, 95% CI) | ‐5.00 [‐14.29, 4.29] |
| 1.2 Disability | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.2.1 Short‐term (closest to 2 weeks) | 2 | 328 | Mean Difference (IV, Random, 95% CI) | ‐2.74 [‐7.52, 2.04] |
| 1.2.2 Intermediate‐term (closest to 3 months) | 1 | 180 | Mean Difference (IV, Random, 95% CI) | ‐0.87 [‐7.31, 5.57] |
| 1.3 Future visits to healthcare professionals | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.3.1 Short‐term (closest to 2 weeks) | 1 | 139 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.11, 0.70] |
Comparison 2. McKenzie method versus manual therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Pain intensity | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1.1 Short‐term (closest to 2 weeks) | 3 | 298 | Mean Difference (IV, Random, 95% CI) | ‐8.67 [‐27.37, 10.02] |
| 2.1.2 Intermediate‐term (closest to 3 months) | 1 | 235 | Mean Difference (IV, Random, 95% CI) | 7.00 [0.70, 13.30] |
| 2.2 Disability | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.2.1 Short‐term (closest to 2 weeks) | 3 | 298 | Mean Difference (IV, Random, 95% CI) | ‐4.98 [‐15.00, 5.04] |
| 2.2.2 Intermediate‐term (closest to 3 months) | 1 | 235 | Mean Difference (IV, Random, 95% CI) | 4.30 [‐0.72, 9.32] |
Comparison 3. McKenzie method versus other interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Disability | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1.1 Short‐term (closest to 2 weeks) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | 4.00 [‐15.44, 23.44] |
| 3.1.2 Intermediate‐term (closest to 3 months) | 1 | 25 | Mean Difference (IV, Random, 95% CI) | 10.00 [‐8.95, 28.95] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cherkin 1998.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Therapists from McKenzie group were trained at McKenzie Institute, and all but one therapist passed an advanced McKenzie credentialing examination. The chiropractors had 6 to 14 years of experience. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | We contacted the trial author and his response was: "This was done 20 years ago and I can't remember the details. All I can say is that we had a highly competent biostatistician in charge of the randomisation." |
| Allocation concealment (selection bias) | Low risk | "After baseline data had been collected, the subjects were randomly assigned without stratification to receive physical therapy, chiropractic manipulation, or an educational booklet with the use of sealed, opaque envelopes." |
| Blinding (performance bias and detection bias) All outcomes | High risk | The index and control groups are distinguishable for the patients. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The index and control groups are distinguishable for the care providers. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The primary outcomes are self‐reported outcomes, in which the patient (unblinded) is the outcome assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Between 89 and 96 percent of the subjects responded to each of the follow‐up questionnaires." |
| Intention to treat analysis | Low risk | Data were analysed according to the intention‐to‐treat principles. |
| Selective reporting (reporting bias) | Unclear risk | No protocol is available and the report does not include enough information to make this judgement. |
| Group similarity at baseline | Low risk | There were no differences among the three treatment groups in any baseline demographic characteristics or outcome measures. |
| Co‐interventions | High risk | The percentage of subjects who used back pain medication was different between groups (27% ‐ McKenzie group; 18% ‐ chiropractic group; 33% ‐ education group) |
| Compliance | High risk | The mean number of chiropractic visits exceeded the mean number of physical therapy visits (6.9 versus 4.6) |
| Timing of outcome assessment | Low risk | All patients were evaluated at the same time. |
| Other bias | Low risk | Free from other sources of bias |
Gillan 1998.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Patients were treated by a physiotherapist holding the McKenzie diploma in mechanical diagnosis and therapy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomly allocated, using a list of random numbers, to one of two groups for management". |
| Allocation concealment (selection bias) | High risk | A list of random numbers was used |
| Blinding (performance bias and detection bias) All outcomes | High risk | The index and control groups are distinguishable for the patients. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The index and control groups are distinguishable for the care providers. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The primary outcomes are self‐reported outcomes, in which the patient (unblinded) is the outcome assessor. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High and not balanced rate of withdrawals for short‐term follow‐up (30% in control group; 40% in McKenzie group, approximately) |
| Intention to treat analysis | High risk | Patients who withdrawn from the study were excluded from the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available and the report does not include enough information to make this judgement. |
| Group similarity at baseline | Low risk | There were no important differences among the groups in baseline demographic characteristics or outcome measures. |
| Co‐interventions | Unclear risk | No information on the text. We attempted to contact the authors, but our attempts were unsuccessful. |
| Compliance | Low risk | Both groups were attended 2 to 3 sessions during the first week and thereafter at the description of the therapist. |
| Timing of outcome assessment | Low risk | Patients in both groups were evaluated at same time |
| Other bias | Low risk | Free of other sources of bias |
Machado 2010.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Treatment was provided by physical therapists who had achieved the status of credentialed in McKenzie methods. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated randomisation sequence was used (randomisation permuted blocks of 4, 6 and 8) |
| Allocation concealment (selection bias) | Low risk | Sequentially, numbered, sealed and opaque envelopes were used. |
| Blinding (performance bias and detection bias) All outcomes | High risk | The index and control groups are distinguishable for the patients. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The index and control groups are distinguishable for the care providers. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The primary outcomes are self‐reported outcomes, in which the patient (unblinded) is the outcome assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The maximum number of participants lost to follow‐up in any time was 8 (5%) |
| Intention to treat analysis | Low risk | Data were analysed according to the intention to treat principles. |
| Selective reporting (reporting bias) | Low risk | All of the study's pre‐specified outcomes in the protocol have been reported. |
| Group similarity at baseline | Low risk | All demographic and clinical characteristics were similar between groups. |
| Co‐interventions | Low risk | Co‐interventions were equally applied across both groups. |
| Compliance | Low risk | Adherence rates were 66% over the first week and 74% over the treatment period. |
| Timing of outcome assessment | Low risk | Participants in both groups were evaluated at same time. |
| Other bias | Low risk | Free of other sources of bias |
Schenk 2003.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Participants were treated by the same physical therapist, who was certified in McKenzie method. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomization was used |
| Allocation concealment (selection bias) | High risk | The author was contacted and reported that the process of allocation concealment was carried out by drawing a slip of paper from a box. |
| Blinding (performance bias and detection bias) All outcomes | High risk | The index and control groups are distinguishable for the patients. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The index and control groups are distinguishable for the care providers. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The primary outcomes are self‐reported outcomes, in which the patient (unblinded) is the outcome assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no missing outcome data. |
| Intention to treat analysis | Low risk | There were no dropout or withdrawals and all patients were analysed in the groups to which they were allocated. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available and the report does not include enough information to make this judgement. |
| Group similarity at baseline | Low risk | Demographic and clinical characteristics are similar between groups. |
| Co‐interventions | Low risk | The trial author was contacted and reported that there were no co‐interventions. |
| Compliance | Low risk | All participants were seen for three physical therapy visits |
| Timing of outcome assessment | Low risk | Both groups were measured at same time |
| Other bias | Low risk | Free of other sources of bias |
Schenk 2012.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Both groups were treated by physical therapist with certification in McKenzie method | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned via a computerized random number generator". |
| Allocation concealment (selection bias) | High risk | The author was contacted and reported that the process of allocation concealment was carried out by alternating the assigned interventions. |
| Blinding (performance bias and detection bias) All outcomes | High risk | The index and control groups are distinguishable for the patients. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The index and control groups are distinguishable for the care providers. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The primary outcomes are self‐reported outcomes, in which the patient (unblinded) is the outcome assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals did not exceed 20% in the short term follow‐up. |
| Intention to treat analysis | High risk | Participants who crossed‐over were not included in the analysis. |
| Selective reporting (reporting bias) | Low risk | All of the study's pre‐specified outcomes in the protocol have been reported. |
| Group similarity at baseline | Low risk | Demographic and clinical characteristics were similar between groups. |
| Co‐interventions | Low risk | The author was contacted and reported that there were no co‐interventions. |
| Compliance | Low risk | "All subjects, regardless of enrolment, performed 10 repetitions of lumbar movements. Participants in the MDT group performed the repetitive movements in the DP on an hourly basis throughout the day, from session 3 until discharge as the home exercise program, a standard part of a MDT intervention. Those in the STM group performed lumbar flexion and extension in quadruped (‘cat and camel’) for 10 repetitions hourly throughout the day, from session 3 until discharge". |
| Timing of outcome assessment | Low risk | All participants were evaluated at the same time. |
| Other bias | High risk | Participants could cross‐over to the alternative at the week 2 visit if they failed to improve with the randomly assigned treatment. Participants were included if they met at least three of five of the selection criteria in clinical prediction rules. However, only those who met four of these criteria were retained for analysis. |
FABQ: Fear‐Avoidance Beliefs Questionnaire LBP: Low back pain MDT: Mechanical Diagnosis and Therapy NRS: Numerical Pain Rating Scale ODI: Oswestry Disability Index RMDQ: Roland Morris Disability Questionnaire STM: spinal manipulative therapy VAS: Visual Analogue Scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTRN12613000267752 | Not a randomised controlled trial. |
| Ali 2002 | The study used another intervention. |
| Ali 2013 | Chronic population |
| Apeldoorn 2012 | The study used other intervention. |
| Apeldoorn 2016 | Not a randomised controlled trial. |
| Arab 2016 | The study did not use the principles of original McKenzie therapy. |
| Bid 2017 | Chronic population |
| Bonnet 2011 | Mixed population |
| Brennan 2006 | The study did not use the principles of the original McKenzie therapy. |
| Buswell 1982 | The study did not use the principles of the original McKenzie therapy. |
| Callaghan 1994 | Chronic population |
| CTRI/2012/07/002774 | The study used another intervention. |
| Cuesta‐Vargas 2011 | Chronic population |
| Dettori 1995 | The study did not use the principles of the original McKenzie therapy. |
| Dimaggio 1987 | Not a randomised controlled trial. |
| Djavid 2007 | The study used another intervention. |
| Elnaagar 1991 | The study did not use the principles of the original McKenzie therapy. |
| Erhard 1994 | The study did not use the principles of the original McKenzie therapy. |
| Fernando 1991 | Not a randomised controlled trial. |
| Foster 2010 | Not a randomised controlled trial. |
| Garcia 2013 | Chronic population |
| Garcia 2018 | Chronic population |
| Hahne 2011 | The study used another intervention. |
| Halliday 2016 | Chronic population |
| Hasanpour 2017 | Chronic population |
| Helmhout 2004 | Chronic population |
| Helmhout 2008 | The study used other intervention. |
| Hosseinifar 2013 | The study did not use the principles of the original McKenzie method |
| IRCT201107197057N1 | The study used other intervention. |
| Kayani 2021 | The study did not use the principles of the original McKenzie therapy. |
| Lohana 2021 | The study did not use the principles of the original McKenzie therapy. |
| Long 2004 | The study did not use the principles of the original McKenzie therapy. |
| Mahmoudzadeh 2016 | Not non‐specific low back pain. |
| Malmivaara 1995 | The study did not use the principles of the original McKenzie therapy. |
| Manca 2007 | Mixed population |
| Mannion 1999 | Chronic population |
| Mayer 2005 | The study did not use the principles of the original McKenzie therapy. |
| Mazloum 2016 | Chronic population |
| Mbada 2014 | Chronic population |
| Mbada 2017 | Chronic population |
| Miller 2005 | Mixed population |
| Moffet 2006 | Mixed population |
| Moncelon 2015 | Chronic population |
| Mujic 2004 | Not a randomised controlled trial. |
| Murtezani 2015 | Chronic population |
| Nazzal 2013 | The study used another intervention. |
| NCT01794962 | The study used another intervention. |
| Nechvátal 2022 | Mixed population |
| Nwuga 1985 | Not non‐specific low back pain. |
| Paatelma 2008 | Mixed population |
| Petersen 2002 | Chronic population |
| Petersen 2007 | Chronic population |
| Petersen 2011 | Chronic population |
| Ponte 1984 | Not non specific low back pain (nerve root compromise). |
| Powers 2008 | The study used another intervention. |
| Rasmussen 2008 | Chronic population |
| RBR‐5mcvt6 | Mixed population |
| Rittweger 2002 | The study used another intervention. |
| Sakai 2008 | Chronic population |
| Skargen 1997 | The study used another intervention. |
| Skargen 1998 | The study used another intervention. |
| Smith 2011 | The study used another intervention. |
| Sorensen 2010 | Mixed intervention. The treatment group includes 3 types of exercise programmes and it is not possible to describe the results for McKenzie therapy individually. |
| Srivastava 2020 | The study did not use the principles of the original McKenzie therapy. |
| Stankovic 1990 | The study did not use the principles of the original McKenzie therapy. |
| Stankovic 1995 | The study did not use the principles of the original McKenzie therapy. |
| Szulc 2015 | Impossible to evaluate the treatment effect of McKenzie method, because both groups received treatment with McKenzie method. |
| Thackeray 2016 | Not non‐specific low back pain. |
| Udermann 2004 | Impossible to evaluate the treatment effect of McKenzie method, because both groups received treatment with McKenzie method. |
| UMIN000018380 | Both groups received treatment with McKenzie method. |
| Van Ravensberg 2005 | Not non‐specific low back pain. |
| Waqqar 2016 | The study did not use the principles of the original McKenzie therapy. |
| Yamim 2016 | The study did not use the principles of the original McKenzie therapy. |
| Yeung 2003 | The study used another intervention. |
Characteristics of ongoing studies [ordered by study ID]
ACTRN12616000735459.
| Study name | Comparison of two exercise approaches for the management of low back pain in the emergency department setting |
| Methods | Randomized controlled trial |
| Participants | • Acute low back pain • Age: 20‐50 years • Sex: male and female |
| Interventions | • Treatment group: McKenzie method and NSAIDS, paracetamol and opioids if necessary. • Control group: Management will include patient education and assurance, symptom relief by analgesia (NSAIDS, paracetamol, and opioids if necessary), as well as recommendation to stay as active as possible including return to work. |
| Outcomes | • Pain score (0‐10) • Roland Morris disability questionnaire (0‐24) |
| Starting date | May 2016 |
| Contact information | Mr Mahender Samtani (Mahender.Samtani@health.qld.gov.au) |
| Notes | Current status of the trial: recruiting ongoing |
CTRI/2017/01/007683.
| Study name | Effects of exercises on high reactivity of brain in chronic low back pain |
| Methods | Randomized controlled trial |
| Participants | • Chronic NSLBP • Age: 18‐50 years • Sex: male and female |
| Interventions | • Treatment group: McKenzie method • Control group: conventional physiotherapy intervention |
| Outcomes | • Central Sensitization Inventory • Pressure Pain Threshold • Roland Morris Disability Questionnaire • Fear Avoidance beliefs Questionnaire • Back flexors and Extensors endurance • Numerical Pain Rating Scale • Global rate of Change Scale |
| Starting date | January 2017 |
| Contact information | Bid Dibyendunarayan Dhrubaprasad (dnbid71@gmail.com) |
| Notes | Current status of the trial: recruiting ongoing |
RBR‐4yz96t.
| Study name | Comparative effects of core and Mckenzie stabilization exercises on non‐specific chronic low back pain in hospital workers of the Santa Luzia hospital of Capão Da Canoa |
| Methods | Randomized controlled trial |
| Participants | • Low back pain • Age: 18‐60 years • Sex: male and female |
| Interventions | • Treatment group: McKenzie method • Control group: CORE exercises |
| Outcomes | • Reduction of back pain assessed through the Visual Analog Pain Scale from preoperative to post intervention evaluations. • Improvement of the level of functionality by reducing the scores of the functional questionnaire of Roland Morris and Oswestry before and after intervention. |
| Starting date | August 2018 |
| Contact information | Marcelo Baptista Dohnert (mdohnert@hotmail.com) |
| Notes | Current status of the trial: recruiting completed |
NSAIDS: non‐steroidal anti‐inflammatory drugs NSLBP: non‐specific low back pain
Differences between protocol and review
As the period between the protocol publication and the review was long, most of the differences occurred to follow new recommendations proposed by the Cochrane Handbook and the Cochrane Back and Neck (CBN) Group (Furlan 2015).
In addition to including RCTs enrolling participants who have sought treatment for (sub)acute NSLBP, we also included trials recruiting adults with the target condition.
We combined no intervention and minimal intervention in the same comparison group.
We chose minimal intervention as the main comparison.
We added two databases (CINAHL and PubMed) and two trial registries (ClinicalTrials.gov and ICTRP) to the search strategy.
Instead of rating risk of bias using the criteria recommended by the Cochrane Back Review Group in 2009, we used 5 key criteria for this assessment: (1) random sequence generation, (2) allocation concealment, (3) blinding of outcome assessors, (4) acceptable dropout rate, (5) intention‐to‐treat analyses. We judged trials rated as “unclear” or “high risk” in at least one of these criteria to be at high risk of bias.
We adopted a random‐effects model for all meta‐analyses (instead of a fixed‐effect model in the presence of sufficient homogeneity), following the recommendation from the CBN method guideline (Furlan 2015).
We used the CBN method guideline to define the criteria to rate the overall certainty of evidence (Furlan 2015).
For unit of analysis issues, we planned to deal with cluster‐RCTS and crossover trials but we did not find any trials with these study designs to include in this review.
We classified the treatment effect as clinically important if it was at least of moderate magnitude (≥ 10 points of a continuous scale, or ≥ 1.25 RR ≤ 0.8).
We calculated the magnitude and relative treatment effects for the dichotomous outcomes and reported them in Effects of interventions. Additionally, for the outcomes that showed a clinically important difference between groups, we also reported the number needed to treat for an additional beneficial outcome (NNTB).
For the summary of findings (SoF) tables, we decided to include the following outcomes: pain intensity and disability at short‐term and intermediate‐term follow‐up, and adverse events. We also decided to present the results for all comparisons included in the review in the SoF tables. These decisions about SoF tables were not approached in the protocol.
Contributions of authors
Study concept and design: LMC, LACM, CLCW, MvT
Development of search strategy: LMC, LACM, CLCW, MvT
Searching for studies: LMC, CLCW, ANG, MOA
Study selection: LMC, CLCW, ANG, MOA
Data extraction: MOA, ANG and LMC
Data analysis: MOA, ANG
Drafting the manuscript: MOA, ANG
Critically revising manuscript for important intellectual content and providing final approval of the version to be submitted: all authors
Sources of support
Internal sources
No sources of support provided
External sources
-
National Health and Medical Research Council (NHMRC), Australia
CL is supported by the National Health and Medical Research Council (NHMRC), Australia.
Declarations of interest
LACM is the primary author of one of the trials included in this review, and a previous systematic review on the same topic. She was not involved in any decision regarding trial eligibility, data extraction, and risk of bias assessments for the present review.
MvT was the Coordinating Editor of Cochrane Back and Neck Review group (CBN), and is now on the Editorial Board of the group. CBN editors are required to conduct at least one Cochrane Review in order to ensure that they are familiar with the processes and commitment needed for these types of studies.
Edited (no change to conclusions)
References
References to studies included in this review
Cherkin 1998 {published data only}
- Cherkin DC, Deyo RA, Battie M, Street J, Barlow W. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. New England Journal of Medicine 1998;339(15):1021-9. [DOI: 10.1056/NEJM199810083391502] [DOI] [PubMed] [Google Scholar]
Gillan 1998 {published data only}
- Gillan MG, Ross JC, McLean IP, Porter RW. The natural history of trunk list, its associated disability and the influence of McKenzie management. European Spine Journal 1998;7(6):480-3. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Machado 2010 {published data only}
- Machado LA, Maher CG, Herbert RD, Clare H, McAuley JH. The effectiveness of the McKenzie method in addition to first-line care for acute low back pain: a randomized controlled trial. BMC Medicine 2010;8(10):1-10. [DOI: 10.1186/1741-7015-8-10] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schenk 2003 {published data only}
- Schenk RJ, Jozefczyk C, Kopf A. A randomized trial comparing interventions in patients with lumbar posterior derangement. Journal of Manual and Manipulative Therapy 2003;11(3):95-102. [DOI: 10.1179/106698103790826455] [DOI] [Google Scholar]
Schenk 2012 {published data only}
- Schenk R, Dionne C, Simon C, Johnson R. Effectiveness of mechanical diagnosis and therapy in patients with back pain who meet a clinical prediction rule for spinal manipulation. Journal of Manual and Manipulative Therapy 2012;20(1):43-9. [DOI: 10.1179/2042618611Y.0000000017] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
ACTRN12613000267752 {published data only}
- ACTRN12613000267752. A study to validate a classification algorithm for chronic low back pain participants using spinal injection as a comparison to measure improvement in symptoms. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=363664 first received 06 March 2013.
Ali 2002 {published data only}
- Ali AA. Management of the First Episode of Acute Low Back Pain: A Comparison Between Two Treatment Protocols [Doctoral thesis]. Denton (TX): Texas Woman's University, 2002. [Google Scholar]
Ali 2013 {published data only}
- Ali S, Ali SM, Memon KN. Effectiveness of core stabilization exercises versus McKenzie's exercises in chronic lower back pain. Medical Forum Monthly 2013;24(12):82-5. [Google Scholar]
Apeldoorn 2012 {published data only}
- Apeldoorn AO, Ostelo RW, De Vet HC, Van T, MW. Cost-effectiveness of a classification-based system for sub-acute and chronic low back pain. European Spine Journal 2012;21(7):1290-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apeldoorn AO, Van Helvoirt H, Fritz JM, De Vet HC, Van Tulder MW. The cost-effectiveness of a treatment-based classification system for low back pain: design of a randomised controlled trial and economic evaluation. BMC Musculoskeletal Disorders 2010;11(58):1-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apeldoorn AO, Van Helvoirt H, Fritz JM, Knol DL, Van Tulder MW, De Vet HC. A randomized controlled trial on the effectiveness of a classification-based system for subacute and chronic low back pain. Spine 2012;37(16):1347-56. [DOI] [PubMed] [Google Scholar]
- Apeldoorn AO, Van Helvoirt H, Knol D, De Vet HC, Van Tulder M. The cost-effectiveness of a treatment-based classification system for low back pain: results of a randomised controlled trial and economic evaluation. Physiotherapy 2011;97:eS76-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Apeldoorn 2016 {published data only}
- Apeldoorn AT, Helvoirt H, Meihuizen H, Tempelman H, Vandeput D, Knol, et al. The influence of centralization and directional preference on spinal control in patients with nonspecific low back pain. Journal of Orthopaedics and Sports Physical Therapy 2016;46(4):258-69. [PMID: ] [DOI] [PubMed] [Google Scholar]
Arab 2016 {published data only}
- Arab AM, Saadati H, Sheikhhoseini R. The effect of harmonic technique vs end range loading exercises on pain and disability in patients with non-specific chronic low back pain: a preliminary study. Journal of Chiropractic Medicine 2016;15(1):3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bid 2017 {published data only}
- Bid DD, Soni N, Yadav AS, Rathod PV. A study on central sensitivization in chronic non-specific low back pain. Indian Journal of Physiotherapy and Occupational Therapy 2017;11(4):165-75. [Google Scholar]
Bonnet 2011 {published data only}
- Bonnet F, Monnet S, Otero J. Short-time effects of a treatment according to the "directional preference" of low back pain patients: a randomized clinical trial [Effets a court terme d'un traitement selon la "preference directionnelle" de patients lombalgiques: essai controle randomise]. Kinesitherapie, la Revue 2011;11(112):51-9. [Google Scholar]
Brennan 2006 {published data only}
- Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute "nonspecific" low back pain: results of a randomized clinical trial. Spine 2006;31(6):623-3. [DOI: 10.1097/01.brs.0000202807.72292.a8] [DOI] [PubMed] [Google Scholar]
Buswell 1982 {published data only}
- Buswell J. Low back pain: a comparison of two treatment programmes. New Zealand Journal of Physiotherapy 1982;10(2):13-7. [Google Scholar]
Callaghan 1994 {published data only}
- Callaghan MJ. Evaluation of a back rehabilitation group for chronic low back pain in an out-patient setting. Physiotherapy 1994;80(10):677-81. [Google Scholar]
CTRI/2012/07/002774 {published data only}
- CTRI/2012/07/002774. A study on the incidence of upper back problem in patients with low back pain and the effect of different physiotherapy mobilization techniques in the management of back pain. http://ctri.nic.in first received 06 July 2012.
Cuesta‐Vargas 2011 {published data only}
- Cuesta-Vargas AC, Arroyo-Morales M, Diego-Acosta AM, Daly DJ. Exercise, manual therapy, and education with or without high-intensity deep-water running for nonspecific chronic low back pain: a pragmatic randomized controlled trial. American Journal of Physical Medicine and Rehabilitation 2011;90(7):526-34. [DOI] [PubMed] [Google Scholar]
Dettori 1995 {published data only}
- Dettori JR, Bullock SH, Sutlive TG, Franklin RJ, Patience T. The effects of spinal flexion and extension exercises and their associated postures in patients with acute low back pain. Spine 1995;20(21):2303-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Dimaggio 1987 {published data only}
- Dimaggio AV. The McKenzie program: exercise effective against back pain. Journal of Musculoskeletal Medicine 1987;12:63-74. [Google Scholar]
Djavid 2007 {published data only}
- Djavid GR, Ghasemi M, Hasan-Zadeh H, Sotoodeh-Manesh A, Pouryaghoub G. In chronic low back pain, low level laser therapy combined with exercise is more beneficial than exercise alone in the long term: a randomised trial. Australian Journal of Physiotherapy 2007;53(3):155-60. [DOI] [PubMed] [Google Scholar]
Elnaagar 1991 {published data only}
- Elnaggar IM, Sheikhzadeh A, Parnianpour M, Kahanovitz N. The effects of spinal flexion and extension exercises on low back pain severity and spinal mobility in chronic mechanical low back pain. Spine 1991;16(8):967-72. [DOI] [PubMed] [Google Scholar]
Erhard 1994 {published data only}
- Erhard RA, Cibulka MT. Relative effectiveness of an extension program and a combined program of manipulation and flexion and extension exercises in patients with acute low back syndrome. Physical Therapy 1994;74(12):1093-100. [DOI] [PubMed] [Google Scholar]
Fernando 1991 {published data only}
- Fernando CK. Conservative treatment of acute low-back pain, a prospective randomized trial: McKenzie method of treatment versus patient education in mini-back school. Spine 1991;16(3):391. [PubMed] [Google Scholar]
Foster 2010 {published data only}
- Foster N. McKenzie treatment for acute back pain added to first-line care does not result in appreciable clinical improvements. Journal of Physiotherapy 2010;56(2):135. [DOI] [PubMed] [Google Scholar]
Garcia 2013 {published data only}
- Garcia AN, Costa Lda C, da Silva TM, Gondo FL, Cyrillo FN, Costa RA, et al. Effectiveness of back school versus McKenzie exercises in patients with chronic nonspecific low back pain: a randomized controlled trial. Physical Therapy 2013;93(6):729-47. [PMID: ] [DOI] [PubMed] [Google Scholar]
Garcia 2018 {published data only}
- Garcia AN, Costa LCM, Hancock M, Souza F, Gomes G, Almeida M, et al. McKenzie method mechanical diagnosis and therapy was slightly more effective than placebo for pain, but not for disability, in patients with chronic nonspecific low back pain: a randomized placebo controlled trial with short and longer-term follow-up. British Journal of Sports Medicine 2018;52(9):594-600. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hahne 2011 {published data only}
- Hahne AJ, Surkitt LD, Richards MC, Chan AY, Thompson SL, Hinman RS, et al. Specific treatment of problems of the spine (STOPS): design of a randomised controlled trial comparing specific physiotherapy versus advice for people with subacute low back disorders. BMC Musculoskeletal Disorders 2011;12:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
Halliday 2016 {published data only}
- Halliday MH, Papas E, Hancoch MJ, Clare HA, Pinto RZ Robertson G, et al. A randomized controlled trial comparing the McKenzie method to motor control exercises in people with chronic low back pain and a directional preference. Journal of Orthopaedic and Sports Physical Therapy 2016;46(7):514-22. [DOI] [PubMed] [Google Scholar]
Hasanpour 2017 {published data only}
- Hasanpour-Dehkordi A, Dehghani A, Solari K. Comparison of the effects of pIlates and McKenzie training on pain and general health in men with chronic low back pain: a randomized trial. Indian Journal of Palliative Care 2017;23(1):36-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Helmhout 2004 {published data only}
- Helmhout PH, Harts CC, Staal JB, Candel MJ, Bie RA. Comparison of a high-intensity and a low-intensity lumbar extensor training program as minimal intervention treatment in low back pain: a randomized trial. European Spine Journal 2004;13(6):537-47. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Helmhout 2008 {published data only}
- Helmhout PH, Harts CC, Viechtbauer W, Staal JB, Bie RA. Isolated lumbar extensor strengthening versus regular physical therapy in an army working population with nonacute low back pain: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2008;89(9):1675-85. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hosseinifar 2013 {published data only}
- Hosseinifar MA, Behtash H, Amiri M, Sarrafzadeh J. The effects of stabilization and McKenzie exercises on transverse abdominis and multifidus muscle thickness, pain, and disability: a randomized controlled trial in nonspecific chronic low back pain. Journal of Physical Therapy Science 2013;25(12):1541-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
IRCT201107197057N1 {published data only}
- IRCT201107197057N1. Comparison between the effect of lumbar stabilization exercises with McKenzie's exercises on lumbo-pelvic stability and transverse abdominis and multifidus muscles thickness in patients with non-specific chronic low back pain. www.en.search.irct.ir/view/6617 first received 24 Aug 2012.
Kayani 2021 {published data only}
- Kayani S, Yasin MM, Naeem A, Arif AB, Mansoor SR, Majeed A. Effects of McKenzie method of mechanical diagnosis and therapy on lumbar range of movement and pain in patients with non-specific low back pain. Rawal Medical Journal 2021;46(1):224-7. [Google Scholar]
Lohana 2021 {published data only}
- Lohana DK, Ahmad U, Sharif F, Ahmad A, Gilane A, Atta S. Comparison of Mulligan sustained natural apophyseal glides verses McKenzie extension exercises on disability and functional outcomes in patients with acute nonspecific low back pain. Rawal Medical Journal 2021;46(2):469-72. [Google Scholar]
Long 2004 {published data only}
- Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine 2004;29(23):2593-602. [PMID: ] [DOI] [PubMed] [Google Scholar]
Mahmoudzadeh 2016 {published data only}
- Mahmoudzadeh A, Rezaeian ZS, Karimi A, Dommerholt J. The effect of dry needling on the radiating pain in subjects with discogenic low-back pain: a randomized control trial. Journal of Research in Medical Sciences 2016;21(86):1-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Malmivaara 1995 {published data only}
- Malmivaara A, Häkkinen U, Aro T, Heinrichs ML, Koskenniemi L, Kuosma E, et al. The treatment of acute low back pain: bed rest, exercises, or ordinary activity? New England Journal of Medicine 1995;332(6):351-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Manca 2007 {published data only}
- Manca AC, Torgerson DJ, Moffett JA, Mooney MP, Jackson DA, Eaton S. Randomized trial of two physiotherapy interventions for primary care back and neck pain patients: cost-effectiveness analysis. Rheumatology 2007;46(9):1495-501. [DOI] [PubMed] [Google Scholar]
Mannion 1999 {published data only}
- Mannion AF, Müntener M, Taimela S, Dvorak J. A randomized clinical trial of three active therapies for chronic low back pain. Spine 1999;24(23):2435-48. [PMID: ] [DOI] [PubMed] [Google Scholar]
Mayer 2005 {published data only}
- Mayer JM, Ralph L, Look M, Erasala GN, Verna JL, Matheson LN, et al. Treating acute low back pain with continuous low-level heat wrap therapy and/or exercise: a randomized controlled trial. Spine 2005;5(4):395-403. [DOI: 10.1016/j.spinee.2005.03.009] [DOI] [PubMed] [Google Scholar]
Mazloum 2016 {published data only}
- Mazloum V, Sahebozamani M, Barati A, Nakhaee N. Comparing the effects of pilates training and McKenzie exercises on core muscles cross-sectional area and strength in patients with chronic non-specific low back pain: a clinical trial. [Persian]. Journal of Mazandaran University of Medical Sciences 2016;26(143):48-61. [Google Scholar]
Mbada 2014 {published data only}
- Mbada CO, Ogunlade SO, Orimolade EA, Oladiran AB, Ogundele AO. Influence of McKenzie protocol and two modes of endurance exercises on health-related quality of life of patients with long-term mechanical low-back pain. Pan African Medical Journal 2014;17 Suppl 1:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mbada 2017 {published data only}
- Mbada C, Olaoye M, Ayanniyi O, Johnson O, Odole A, Dada O. Comparative efficacy of clinic-based and telerehabilitation application of McKenzie therapy in low-back pain. Archives of Physical Medicine and Rehabilitation 2017;98(10):e46-7. [DOI: ] [Google Scholar]
Miller 2005 {published data only}
- Miller ER, Schenk RJ, Karnes JL, Rousselle JG. A comparison of the McKenzie approach to a specific spine stabilization program for chronic low back pain. Journal of Manual and Manipulative Therapy 2005;13(2):103-12. [Google Scholar]
Moffet 2006 {published data only}
- Moffett JK, Jackson DA, Gardiner ED, Torgerson DJ, Coulton S, Eaton S, et al. Randomized trial of two physiotherapy interventions for primary care neck and back pain patients: 'McKenzie' vs brief physiotherapy pain management. Rheumatology 2006;45(12):1514-21. [DOI] [PubMed] [Google Scholar]
Moncelon 2015 {published data only}
- Moncelon S, Otero J. The McKenzie method of mechanical diagnosis and therapy in chronic low back pain with directional preference. Revue de Kinesitherapie 2015;15(160):31-7. [Google Scholar]
Mujic 2004 {published data only}
- Mujic SS, Sakota S, Avdic D. The effects of McKenzie and Brunkow exercise program on spinal mobility comparative study. Bosnian Journal of Basic Medical Sciences 2004;3(1):62-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murtezani 2015 {published data only}
- Murtezani A, Govori V, Meka VS, Ibraimi Z, Rrecaj S, Gashi S. A comparison of McKenzie therapy with electrophysical agents for the treatment of work related low back pain: a randomized controlled trial. Journal of Back and Musculoskeletal Rehabilitation 2015;28(2):247-53. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nazzal 2013 {published data only}
- Nazzal MA, Saadah LM, Al-Omari MA, Al-Oudat ZA, Nazzal MS, El-Beshari MY, et al. Management options of chronic low back pain: a randomized blinded clinical trial. Neurosciences 2013;18(2):152-9. [PubMed] [Google Scholar]
NCT01794962 {published data only}
- NCT01794962. Cognitive functional therapy versus manual therapy for non-specific low back pain. clinicaltrials.gov/ct2/show/NCT01794962 first received 20 February 2013.
Nechvátal 2022 {published data only}
- Nechvátal P, Hitrík T, Kendrova LD, Macej M. Comparison of the effect of the McKenzie method and spiral stabilization in patients with low back pain: a prospective, randomized clinical trial. Journal of Back and Musculoskeletal Rehabilitation 2022;35(3):641-7. [DOI] [PubMed] [Google Scholar]
Nwuga 1985 {published data only}
- Nwuga GV. Relative therapeutic efficacy of the Williams and Mckenzie protocols in back pain management. Physiotherapy Practice 1985;1:99-105. [Google Scholar]
Paatelma 2008 {published data only}
- Paatelma M, Kilpikoski S, Simonen R, Heinonen A, Alen M, Videman T. Orthopaedic manual therapy, McKenzie method or advice only for low back pain in working adults: a randomized controlled trial with one year follow-up. Journal of Rehabilitation Medicine 2008;40(10):858-63. [DOI] [PubMed] [Google Scholar]
Petersen 2002 {published data only}
- Petersen T, Kryger P, Ekdahl C, Olsen S, Jacobsen S. The effect of McKenzie therapy as compared with that of intensive strengthening training for the treatment of patients with subacute or chronic low back pain: a randomized controlled trial. Spine 2002;27(16):1702-9. [DOI] [PubMed] [Google Scholar]
Petersen 2007 {published data only}
- Petersen T, Larsen K, Jacobsen S. One-year follow-up comparison of the effectiveness of McKenzie treatment and strengthening training for patients with chronic low back pain: outcome and prognostic factors. Spine 2007;32(26):2948-56. [DOI] [PubMed] [Google Scholar]
Petersen 2011 {published data only}
- Petersen T, Larsen K, Nordsteen J, Olsen S, Fournier G, Jacobsen S. The McKenzie method compared with manipulation when used adjunctive to information and advice in low back pain patients presenting with centralization or peripheralization: a randomized controlled trial. Spine 2011;36(24):1999-2010. [DOI] [PubMed] [Google Scholar]
Ponte 1984 {published data only}
- Ponte DJ, Kent BE. A preliminary report on the use of the McKenzie protocol versus Williams protocol in the treatment of low back pain. Journal of Orthopaedic and Sports Physical Therapy 1984;6(2):130-9. [DOI] [PubMed] [Google Scholar]
Powers 2008 {published data only}
- Powers CM, Beneck GJ, Kulig K, Landel RF, Fredericson M. Effects of a single session of posterior-to-anterior spinal mobilization and press-up exercise on pain response and lumbar spine extension in people with nonspecific low back pain. Physical Therapy 2008;88(4):485-93. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rasmussen 2008 {published data only}
- Rasmussen J, Laetgaard J, Lindecrona AL, Qvistgaard E, Bliddal H. Manipulation does not add to the effect of extension exercises in chronic low-back pain (LBP). A randomized, controlled, double blind study. Joint Bone Spine 2008;75(6):708-13. [PMID: ] [DOI] [PubMed] [Google Scholar]
RBR‐5mcvt6 {unpublished data only}
- Daitx RB. Mckenzie Method and Core stabilization exercises in lumbar pain due to disc protrusion [Método Mckenzie e exercícios de estabilização do Core na dor lombar decorrente da protusão discal]. RBR 14 June 2019.
Rittweger 2002 {published data only}
- Rittweger J, Just K, Kautzsch K, Reeg P, Felsenberg D. Treatment of chronic lower back pain with lumbar extension and whole-body vibration exercise: a randomized controlled trial. Spine 2002;27(17):1829-34. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sakai 2008 {published data only}
- Sakai Y, Matsuyama Y, Nakamura H, Katayama Y, Imagama S, Ito Z, et al. The effect of muscle relaxant on the paraspinal muscle blood flow: a randomized controlled trial in patients with chronic low back pain. Spine 2008;33(6):581-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Skargen 1997 {published data only}
- Skargren EE, Carlsson PG, Gade M. Cost and effectiveness analysis of chiropractic and physiotherapy treatment for low back and neck pain. Six-months follow-up. Spine 1997;22(18):2167-77. [DOI] [PubMed] [Google Scholar]
Skargen 1998 {published data only}
- Skargren EG, Oberg BE. One-year follow-up comparison of the cost and effectiveness of chiropractic and physiotherapy as primary management for back pain. Subgroup analysis, recurrence, and additional health care utilization. Spine 1998;23(17):1875-83. [DOI] [PubMed] [Google Scholar]
Smith 2011 {published data only}
- Smith D, Bissell G, Bruce-Low S, Wakefield C. The effect of lumbar extension training with and without pelvic stabilization on lumbar strength and low back pain. Journal of Back and Musculoskeletal Rehabilitation 2001;24(4):241-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sorensen 2010 {published data only}
- Sorensen PH, Bendix T, Manniche C, Korsholm L, Lemvigh D, Indahl A. An educational approach based on a non-injury model compared with individual symptom-based physical training in chronic LBP: a pragmatic, randomised trial with a one-year follow-up. BMC Musculoskeletal Disorders 2010;11:212. [DOI: 10.1186/1471-2474-11-212] [DOI] [PMC free article] [PubMed] [Google Scholar]
Srivastava 2020 {published data only}
- Srivastava S, Kumar D, Mittal H, Dixit S, Nair A. Short-term effect of muscle energy technique and mechanical diagnosis and therapy in sacroiliac joint dysfunction: a pilot randomized clinical trial. Journal of Bodywork & Movement Therapies 2020;24(3):63-70. [DOI] [PubMed] [Google Scholar]
Stankovic 1990 {published data only}
- Stankovic RO. Conservative treatment of acute low-back pain. A prospective randomized trial: McKenzie method of treatment versus patient education in "mini back school". Spine 1990;15(2):120-3. [PubMed] [Google Scholar]
Stankovic 1995 {published data only}
- Stankovic RO. Conservative treatment of acute low back pain. A 5-year follow-up study of two methods of treatment. Spine 1995;20(4):469-72. [DOI] [PubMed] [Google Scholar]
Szulc 2015 {published data only}
- Szulc PM, Waszak M, Tomczak M, Cieslik K, Trzaska T. Impact of McKenzie method therapy enriched by muscular energy techniques on subjective and objective parameters related to spine function in patients with chronic low back pain. Medical Science Monitor 2015;21:2918-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thackeray 2016 {published data only}
- Thackeray A, Fritz JM, Childs JD, Brennan GP. The effectiveness of mechanical traction among subgroups of patients with low back pain and leg pain: a randomized trial. Journal of Orthopaedic and Sports Physical Therapy 2016;46(3):144-54. [DOI] [PubMed] [Google Scholar]
Udermann 2004 {published data only}
- Udermann BM, Donelson RG, Graves JE, Murray SR. Combining lumbar extension training with McKenzie therapy: effects on pain, disability, and psychosocial functioning in chronic low back pain patients. Gundersen Lutheran Medical Journal 2004;3(2):7-12. [Google Scholar]
UMIN000018380 {published data only}
- UMIN000018380. Randomized control trail to investigate if treatment effect for low back pain is enhanced by using LumoBack in addition to the McKenzie approach. https://center6.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000021285 first received 22 July 2015.
Van Ravensberg 2005 {published data only}
- Van Ravensberg CD, Oostendorp RA, Van Berkel LM, Scholten-Peeters GG, Pool JJ, Swinkels RA, et al. Physical therapy and manual physical therapy: differences in patient characteristics. Journal of Manual and Manipulative Therapy 2005;13(2):113-24. [Google Scholar]
Waqqar 2016 {published data only}
- Waqqar S, Shakil-ur Rehman S, Ahmad S. Mckenzie treatment versus mulligan sustained natural apophyseal glides for chronic mechanical low back pain. Pakistan Journal of Medical Sciences 2016;32(2):476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yamim 2016 {published data only}
- Yamin F, Rehman A, Aziz S, Zeya N, Choughley A. To compare the effectiveness of McKenzie exercises versus general conditioning exercises in low back pain. Indian Journal of Physiotherapy and Occupational Therapy 2016;10(1):82-9. [Google Scholar]
Yeung 2003 {published data only}
- Yeung CK, Leung MC, Chow DH. The use of electro-acupuncture in conjunction with exercise for the treatment of chronic low-back pain. Journal of Alternative and Complementary Medicine 2003;9(4):479-90. [PMID: ] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ACTRN12616000735459 {published data only}
- ACTRN12616000735459. Comparison of two exercise approaches for the management of low back pain in the emergency department setting.. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=370804 first received 03 June 2016.
CTRI/2017/01/007683 {published data only}
- CTRI/2017/01/007683. Effects of exercises on high reactivity of brain in chronic low back pain. http://ctri.nic.in/ first received 18 Jan 2016.
RBR‐4yz96t {published data only}
- RBR-4yz96t. Comparative effects of core and McKenzie stabilization exercises on non-specific chronic low back pain in hospital workers of the Santa Luzia Hospital of Capão Da Canoa. www.ensaiosclinicos.gov.br/rg/RBR-4yz96t first received 12 September 2018.
Additional references
ACP 2017
- Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Annals of Internal Medicine 2017;166(7):514-30. [DOI] [PubMed] [Google Scholar]
Aina 2004
Beasley 2017
- Beasley MJ, Ferguson-Jones EA, Macfarlane GJ. Treatment expectations but not preference affect outcome in a trial of CBT and exercise for pain. Canadian Journal of Pain 2017;1(1):161-70. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Campos 2020
- Campos TF, Pocovi NC, Maher CG, Clare HA, Silva TM, Hancock MJ. An individualised self-management exercise and education program did not prevent recurrence of low back pain but may reduce care seeking: a randomised trial. Journal of Physiotherapy 2020;66(3):166-73. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cates 2008 [Computer program]
- Dr.Christopher Cates EBM website. Visual Rx. Version 3. Dr.Christopher Cates EBM website, 2008.
Childs 2004
Chou 2007
Clare 2004
Costa 2012
- da C Menezes Costa L, Maher CG, Hancock MJ, McAuley JH, Herbert RD, Costa LO. The prognosis of acute and persistent low-back pain: a meta-analysis. Canadian Medical Association Journal 2012;184(11):613-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Donelson 1990
- Donelson R, Silva G, Murphy K. Centralization phenomenon: its usefulness in evaluating and treating referred pain. Spine 1990;15(3):211-3. [PubMed]
Flynn 2002
- Flynn T, Fritz J, Whitman J, Wainner R, Magel J, Rendeiro D, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine 2002;27(24):2835-42. [PMID: ] [DOI] [PubMed] [Google Scholar]
Fritz 2003
Furlan 2015
- Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, et al. 2015 Updated Method Guideline for Systematic Reviews in the Cochrane Back and Neck Group. Spine 2015;40(21):1660-73. [DOI] [PubMed] [Google Scholar]
Garcia 2012
- Narciso Garcia A, Menezes Costa LC, Almeida MO, Tulder MW, Lin CC, Hayden JA, Machado LAC. The McKenzie method for chronic non-specific low back pain. Cochrane Database of Systematic Reviews 2012, Issue 3 Art. No.: CD009712. [DOI] [PMC free article] [PubMed] [Google Scholar]
GBD 2019 Diseases and Injuries Collaborators
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396(10258):1204-22. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Hamilton (ON): McMaster University (developed by Evidence Prime), accessed 17 December 2020. Available at gradepro.org.
Guyatt 2013
- Guyatt GH, Thorlund K, Oxman AD, Walter SD, Patrick D, Furukawa TA, et al. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles-continuous outcomes. Journal of Clinical Epidemiology 2013;66(2):173-83. [DOI] [PubMed] [Google Scholar]
Hartvigsen 2018
- Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Lancet Low Back Pain Series Working Group. What low back pain is and why we need to pay attention. Lancet 2018;391(10137):2356-67. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Hoy 2010
- Hoy D, March L, Brooks P, Woolf A, Blyth F, Vos T, et al. Measuring the global burden of low back pain. Best Practice and Research Clinical Rheumatology 2010;24(2):155-65. [DOI] [PubMed] [Google Scholar]
Hoy 2012
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis and Rheumatology 2012;64(6):2028-37. [DOI] [PubMed] [Google Scholar]
Indrakanti 2011
- Indrakanti SS, Weber MH, Takemoto SK, Hu SS, Polly D, Berven SH. Value-based care in the management of spinal disorders: a systematic review of cost-utility analysis. Clinical Orthopaedics and Related Research 2011;470(4):1106-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Itz 2013
- Itz CJ, Geurts JW, Kleef M, Nelemans P. Clinical course of non-specific low back pain: a systematic review of prospective cohort studies set in primary care. European Journal of Pain 2013;17(1):5-15. [DOI] [PubMed] [Google Scholar]
Kalauokalani 2001
- Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine 2001;26(13):1418-24. [PMID: ] [DOI] [PubMed] [Google Scholar]
Karas 1997
Koes 2006
- Koes B, Van Tulder M, Thomas S. Diagnosis and treatment of low back pain. British Medical Journal 2006;332(775):1430-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lam 2018
- Lam OT, Strenger DM, Chan-Fee M, Pham PT, Preuss RA, Robbins SM. Effectiveness of the McKenzie method of mechanical diagnosis and therapy for treating low back pain: literature review with meta-analysis. Journal of Orthopaedic and Sports Physical Therapy 2018;48(6):476-90. [DOI] [PubMed] [Google Scholar]
Long 1995
- Long A. The centralization phenomenon: its usefulness as a predictor of outcome in conservative treatment of chronic low back pain (a pilot study). Spine 1995;20(23):2513-21. [PubMed]
Machado 2005
- Machado L, Maher C, Herbert R, Clare H, McAuley J. The McKenzie method for the management of acute non-specific low-back pain: design of a randomised controlled trial [ACTRN012605000032651]. BMC Musculoskeletal Disorders 2005;6:50. [DOI] [PMC free article] [PubMed]
Machado 2009
Maher 2017
- Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet 2017;389(10070):736-47. [PMID: ] [DOI] [PubMed] [Google Scholar]
McKenzie 1981
- McKenzie R. The Lumbar Spine: Mechanical Diagnosis and Therapy. New Zealand: Spinal Publications, 1981. [Google Scholar]
McKenzie 2003a
- McKenzie R, May S. The Lumbar Spine: Mechanical Diagnosis and Therapy. Vol. 1. New Zealand: Spinal Publications, 2003. [Google Scholar]
McKenzie 2003b
- McKenzie R, May S. The Lumbar Spine: Mechanical Diagnosis and Therapy. Vol. 2. New Zealand: Spinal Publications, 2003. [Google Scholar]
McKenzie 2011
- Robin McKenzie. Treat Your Own Back. Orthopedic Physical Therapy & Rehabilitation, 2011. [Google Scholar]
NICE 2016
- National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: assessment and management. Available from: nice.org.uk/guidance/ng59 2016. [PubMed]
Review Manager 2020 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.4. Copenhagen: The Cochrane Collaboration, 2020.
Rubinstein 2012
- Rubinstein SM, Terwee CB, Assendelft WJJ, De Boer MR, Van Tulder MW. Spinal manipulative therapy for acute low back pain. Cochrane Database of Systematic Reviews 2012;9:Art. No.: CD008880. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saragiotto 2016
- Saragiotto BT, Maher CG, Yamato TP, Costa LO, Menezes Costa LC, Ostelo RW, et al. Motor control exercise for chronic non-specific low-back pain. Cochrane Database of Systematic Reviews 2016, Issue 1. Art. No: CD012004. [DOI: 10.1002/14651858.CD012004] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sufka 1998
Van Tulder 2006
- Van Tulder M, Becker A, Bekkering T, Breen A, Gil del Real M, Hutchinson A, et al. European guidelines for the management of acute nonspecific low back pain in primary care. European Spine Journal 2006;15 Suppl 2:S169-91. [DOI] [PMC free article] [PubMed]
Werneke 1999
Werneke 2001
References to other published versions of this review
Machado 2006
Machado 2012
- Machado L, Lin C-WC, Clare H, Tulder MW. The McKenzie method for (sub)acute non-specific low-back pain. Cochrane Database of Systematic Reviews 2012, Issue 3. Art. No.: CD009711. Art. No: CD009711. [DOI: 10.1002/14651858.CD009711] [DOI] [PMC free article] [PubMed] [Google Scholar]


