Abstract
Telepresence robots are being increasingly used in long-term care (LTC) homes for virtual visits between families and residents. This study investigated the impacts and experiences of residents and their families using a telepresence robot (Double 3) for 4 to 12 months during the COVID-19 pandemic. A total of 51 participants were recruited through purposive sampling, including 9 residents, 15 family members, and 27 staff from 4 LTC homes in British Columbia, Canada. Conversational interviews were conducted with residents and family members. Focus groups and one-to-one interviews were held with frontline staff. Thematic analysis was performed, with five themes identified: (1) Stay connected, (2) Regain autonomy, (3) Relieve caregiver burden, (4) Environmental and technical issues, and (5) Scheduling concerns. In conclusion, telepresence robots helped maintain social connections between residents and families, despite the COVID-19 restrictions.
Keywords: telepresence robot, long-term care, technology, family, social isolation, social connection
Introduction
Residents in long-term care (LTC) are at risk of social isolation and reduced social connection due to shrinking social networks, communication, and physical challenges, and limited opportunities for social engagement and novel relationship-building (Boamah et al., 2021). During the COVID-19 pandemic, staff shortages, social distancing mandates, and the fluctuating pandemic situation have exacerbated the reduced social connection of residents, which has negative effects on their social, emotional, and mental well-being. Francis et al. (2019) and Cotten (2021) report that using technology to interact with others could positively promote social connectedness for older adults and enhance functioning, which is linked to a greater purpose in life, increased self-esteem, and wellness. However, LTC residents face challenges during video calls with families via tablets/computers (Hardy et al., 2022; Ickert et al., 2020). Many LTC homes have poor Internet connections and limited devices, which restricts the opportunity for virtual visits (Chu et al., 2022; Saad et al., 2022). Physical, cognitive, and sensory impairments of LTC residents also impede their independence in using technologies (Chu et al., 2021). Holding a tablet to enable video conferencing can be challenging for residents with dementia. Requiring staff to assist with calls can lead to a loss of privacy. Staffing shortages also make it difficult to schedule calls (Zamir et al., 2018). These challenges often lead to frustration for all involved (van de Baan et al., 2020; Zamir et al., 2018).
We have recently explored a more accessible option for virtual video calls by using telepresence robots (Double 3, 2022). Telepresence robots have three relative advantages compared to regular video and phone calls: (1) no effort is required on the resident’s side, (2) the mobility of the robot makes engagement of residents with dementia easier, and (3) family members can initiate calls without requiring staff assistance (Hung, Mann, et al., 2022; Hung, Wong, et al., 2022) (see Table 1). By increasing the number of virtual visits during everyday life, telepresence robots can enhance connections between residents and families by helping residents feel that they are not forgotten, their family bonds remain, and they are needed as part of their family. Virtual connection can support the value of older people, reinforcing that they matter in society. Rosenberg and McCullough (1981) explain the notion of mattering: (1) attention: the feeling that others pay attention to you, (2) importance: the belief that others care about you and what you do, and (3) dependence: the perception that others need you. The COVID-19 pandemic has exposed the problem of ageism and underappreciation of older people living in LTC. Helping residents and families stay connected is an important way of reminding everyone that older adults matter.
Table 1.
Advantages of Telepresence Robot over Telephone.
| Telepresence robot | Telephone |
|---|---|
| No need for staff members to schedule calls | Need for staff members to schedule calls, adding to workload |
| No need for resident to own phone | Resident needs to own phone or use staff member’s phone (creating conflict) |
| Activated by family member without resident needing to do anything to pick up call | Unless staff member has time to bring phone to resident, resident must have cognitive skills to recognize ringtone, mobility, and motor skills to physically look for and pick up the phone and press the right buttons correctly to respond to call |
| No need for resident to hold anything | Resident must have manual dexterity to hold phone at appropriate angle for relatively long periods of time |
| Large iPad screen makes it easy for family member and resident to see each other in their environments, thereby facilitating virtual visits | Small screen (mobile) or no screen (landline) makes it difficult for resident to see |
| Can be positioned remotely by family member (adjusting height, volume, and proximity) to ensure full visibility | Staff member needs be close to resident for the duration of the call to ensure resident does not accidentally re-position or drop the phone, or freeze the screen, thereby adding to workload |
| Privacy can be maintained between resident and family | Need for staff member’s assistance compromises resident-family privacy |
| No limit on number or length of virtual visits (calls) | Number and length of calls may be limited by staff workload/availability |
| Offers greater, sustained opportunity for family to observe changes in resident’s mood and behavior | Family remains reliant on resident’s ability and willingness to self-report mood and behavior |
| Can facilitate synchronous action and interactivity (e.g., exercising or eating together) | Can only facilitate conversation due to the need to hold phone; conversational turn-taking is often cognitively difficult for people with advanced dementia |
| Offers enhanced sense of presence and immersion in environment (visit) | Offers relatively limited chance to talk and listen (call) |
Although telepresence robots have the potential to reduce loneliness and social isolation, little is known about the use of telepresence robots among LTC residents and families (positive impact and challenges) during the COVID-19 pandemic. Previous studies evaluated the capabilities of telepresence robots prior to the pandemic to determine their ability to facilitate social interactions between individuals with dementia and their caregivers (Moyle et al., 2014, 2019). Prior research highlighted the positive reactions of participants to the use of telepresence robots for long-distance communication, promoting independent living, and providing memory aids. However, the impact of the stressful COVID-19 environment, such as isolation and prolonged anxiety, on telepresence robot usage and experiences has not been investigated. This study aims to fill this knowledge gap by examining the experiences of residents and family members using telepresence robots in long-term care homes during the COVID-19 pandemic.
Research questions:
What is the perceived positive impact of the telepresence robot on residents and their family members?
What are the challenges that residents and family members face in using the telepresence robot for virtual visits?
Methods
The study is descriptive qualitative, based on a thematic analysis of semi-structured conversational interviews with residents and family members, as well as focus groups with staff.
The Telepresence Robot for Family Virtual Visits
We used Double (Double Robotics, Inc., software version 3.0 as shown in Figure 1) to allow family members to connect to the robots via Wi-Fi and drive the robot remotely. Double online booking (Fleet Management) system was used to schedule virtual calls by sending a link to a family member’s email. Unlike voice-activated systems, calls are initiated by the family rather than the resident. Families can control the robot’s movements by clicking on arrow icons or using “click-to-drive” markings to guide the robot to their desired location. The robots are equipped with 3D sensors that allow them to navigate the environment and avoid obstacles. The height of the robot can be adjusted remotely, allowing families to see the faces of residents from the desired angle. Telephone or tablet video calls can be challenging for residents, as they may have difficulty holding their devices for an extended period and maintaining eye contact with their families. With the telepresence robot, families can adjust visuals and audio without requiring the resident to take any action, making it easier for them to remain engaged during virtual visits.
Figure 1.

A family virtual visit with the robot.
In the study, family members could use the robot anytime to contact residents. Robots were placed in resident rooms, except (for three residents) who were deemed unsafe to keep a robot in the room according to the families and staff. In such cases, the staff brought the robot to the residents when a call was scheduled. Our team utilized Collaborative Action Research (CAR) approach to involve both staff and families in various ways, such as seeking their input on the best location for the robot. Through these efforts, we found that most residents preferred to use the robot in stationary position at a shared space. In addition, the team also trained family members and staff about how to use the robot by using videos, written materials, and in-person demonstrations; the importance of charging the robot was emphasized to ensure the robot is available for use. The residents were informed about the purpose of the robot by their families and the research team. Training was not required for residents because they do not need to do anything to receive the virtual call.
Setting and Participants
The research was conducted from July 2021 to August 2022 at four urban LTC homes in British Columbia, Canada. Three homes are publicly funded. One home is non-profit and privately funded. We used purposive sampling (Braun & Clarke, 2021) to recruit residents and their family members, aiming to capture diverse racial backgrounds, various functional abilities and disabilities, different ethnicities, sex, gender, age, etc. Some participants were more fluent in linguistic expression; others had communication and cognitive difficulties in social interactions. The characteristics of resident participants are summarized in Table 2. Staff on the unit participated in one-to-one interviews and focus group discussions to provide more context about the telepresence robot use in the care home. The staffing ratio varied across four homes. Home 1 had a ratio of 1 staff member to 6 residents during the day and 1 to 20 in the evening. Home 2 had ratios of 1 to 6 during the day, 1 to 8 in the evening, and 1 to 25 at night. Across both day and evening, there was 1 nurse per 25 residents. At night, 1 nurse was assigned to every 50 residents. Home 3 had 3 nurses and 4 care aides (7 staff to 19 residents) during the day, 3 nurses and 3 care aides (6 staff to 19 residents) during the evening, and 2 nurses and 2 care aides (4 staff to 19 residents) during the night. Home 4 had 1 nurse and 2 to 3 care aides for 16 to 17 residents during both day and evening, and 1 staff (nurse or care aid) per care neighborhood (16–27 residents) during the night. Additionally, a registered nurse was available 24/7 in the care home.
Table 2.
Descriptive Characteristics of Study Participants (N = 9).
| Characteristics | N (%) |
|---|---|
| Age (years) | |
| 60–75 | 4 (44) |
| 76–85 | 2 (22) |
| Older than 85 | 3 (33) |
| Sex (self-report) | |
| Male | 5 (55) |
| Female | 4 (44) |
| Dementia | |
| Early | 2 (22) |
| Middle | 2 (22) |
| Late | 4 (44) |
| N/A | 1 (11) |
| Ethnicity | |
| Caucasian | 6 (66) |
| East Asian | 3 (33) |
The convenience sampling method was used to recruit staff participants. Staff experiences will be written about in a future paper.
Data Generation
Data generation involved (a) conversational interviews with residents and family members individually and together as dyads (Kindell et al., 2017), (b) focus groups (Morgan, 2002), and one-to-one interviews with interdisciplinary staff at the point of care. Each interview lasted 20 to 30 min. They were conducted by phone or in person, depending on the interviewee’s preference. We asked open-ended questions: What is your experience of using the robot for virtual calls? What did you like and dislike about it? What are the challenges and support you need? Focus groups (total: four) were held at each LTC home. They lasted 30 to 40 min. We asked the same questions as above. All participation was voluntary. Data saturation was determined by the sufficient data we gathered to answer the research questions (Braun & Clarke, 2021).
Data Analysis
Thematic analysis was performed in six steps, guided by Braun and Clarke (2022). Step 1: All authors (including patient and family partners totaling 11 people: including three patient partners) read and re-read the transcribed text to become familiar with the data. Step 2: One student author (GH) generated initial codes by using sensitized concepts in the literature (deductive approach) and concepts found in the data (inductive techniques). The academic supervisor (LH) reviewed the codes. Step 3: Initial themes were developed based on the codes and extracted data. Step 4: The whole team discussed the data and reviewed the themes. Step 5: Collectively, the research team refined the themes and selected extractions for quotations in the write-up. Step 6: The first author guided the student authors to write the first draft of the manuscript and all authors reviewed and made edits.
Ethical Considerations
Ethical approval was provided by the local University and Health Authority (Ethics ID: H22-00659). All family members and staff participants signed written informed consent forms. For resident participants, we obtained verbal consent (Black et al., 2010; Mann & Hung, 2018) or if needed, the family signed a written consent form for resident participants. Pseudonyms are used here to protect the participants’ identities. The robots do not have the function to record, so the privacy of individuals is protected. The only information that the family can access is the live conversation, which is no different from a face-to-face visit with the resident.
Results
We recruited 51 participants: 9 residents, their family members (15), and 27 staff from 4 LTC homes in British Columbia. See Table 2 for residents’ characteristics.
Our analysis identified five themes characterizing how families and residents felt about the use of telepresence robots in LTC. Three themes highlighted positive experiences while two themes focused on challenges.
Theme 1: “We are Together in Different Places”: The Robot Helps Residents Stay Connected to Their Families
With the covid-19 pandemic, many residents were impacted by social distancing mandates that threatened their social connection to loved ones. Many families did not live in the local area. Resident Rosie’s children used the robot with their mother and remarked:
The robot makes a big difference for me. To visit my mum, I have to get to the ferry and sometimes the ferry is cancelled. The robot saves a lot of troubles. I can now [virtually] visit her anytime and whenever I want. It is more convenient.
Resident George’s daughter said something similar:
Being an hour’s drive away makes it challenging for us to visit my dad in person but the robot is a great resource. He really enjoys seeing and talking to my daughter. We show him how she [granddaughter]rides a bike without training wheels or take him along whatever she’s doing.
Doing things together indicates the important value of the older person in the family, especially in the context of dementia: an isolating disease by nature, made worse by the pandemic’s physical distancing protocols.
Resident Max reflected on his experience:
The more I use it, the more I think I am able to enjoy it. I am a very fortunate man. I have an amazing wife and good kids. I like [it] when my boys call me. This is a cuddly robot, Kirby.
Max views the robot as a part of his family unit. “My sons and wife would call me with the help of Kirby.” His wife told us: “Using the robot adds to the sense of person because so much [of Max] gets taken away, through dementia.”
She further explained what the robot means to Max: “Connectivity. I mean his world is quite small right now. He’s adjusted to this new phase, living in long-term care and using the robot for calls. It’s been wonderful to see the change.”
Max’s wife emphasized how their connections through the robot helped reduce Max’s anxiety upon entry into the home. Staff also described that the robot helped Max; he became more engaged and cooperative, whereas before using the robot he was easily upset, leading to multiple falls.
Theme 2: “Freedom Makes a Big Difference”: The Robot Supports a Sense of Autonomy
With technology like Zoom and FaceTime, there’s a reliance on staff for assistance to connect the video call. This was especially difficult during COVID-19 due to staff shortages. The telepresence robot eliminates these burdens. Resident Bill’s daughter described: “It [robot] has been really helpful because he [my dad] doesn’t need to do anything. He wouldn’t be able to go to a screen and then turn it on. So, the fact that we can control everything is good.”
For Bill’s family, communication technology is needed as his daughters live overseas. However, options for technology are also limited by their father’s abilities. Bill would be unable to operate applications like Zoom on his own due to his limited physical capacity.
During the pandemic, many residents with dementia did not understand why family stopped visiting. Some thought they were abandoned. The virtual visits help reinforce experiences of care, love, and mattering to the resident. Rosie’s son recalled:
I haven’t seen her for a year since COVID. Then she wouldn’t talk to me anymore. I became a stranger to her before having the robot. Now I can see her every morning or so; she talks to me again.
Further, using the robot over time allowed families to better understand their resident’s abilities and to create personalized routines for positive engagement. Rosie’s daughter told us: “Every morning 10 to 11, I call her, and do exercise [with her through the robot] for 15 to 20 min. Then we drink a glass of water together. Now it’s almost like she’s expecting that; it becomes a routine.”
Theme 3: “We Can Have Peace of Mind”—the Robot Decreases Care Partner Burden
Many family members reported stress about COVID-19 infection and visiting restrictions. Many also had children and work responsibilities; they felt overwhelmed with conflicting responsibilities. George’s daughter described her experience:
I have a lot on my plate. I feel like I’m drowning in many ways as the juggle is quite hard these days with my kids, work and of course my dad being unwell. I am really grateful to have access to the robot as it allows me to see him.
Max’s wife also reported feeling burnout. She worried about Max a lot because he was quite unsettled. Thus, it was important for her to check on him daily via the robot. Something so simple as using the robot to view if Max was settled comfortably in bed, was important as it provided peace of mind. For Max’s wife, it seemed that the robot provides a way of reaching him in a time of need.
In LTC homes, families often express a desire to feel included in their loved one’s care. The pandemic’s social distancing mandates have made this inclusion difficult. This can produce care partner burden, as families worry if their loved ones are receiving the care that they need. With the telepresence robot, the family can remain present to support this care. For residents, the robot connects them to familiar, comforting faces. Rosie’s children highlighted feeling peace of mind. They described that because the robot allows them to visit their mom every day, they can observe her daily changes in mood, behavior, well-being, and her surroundings: “With the robot, I can see mom’s everyday changes, for example, getting tired or coughing or little thing. I can observe her surroundings and environment, like if she has a footrest nearby. Without the robot, we cannot have these updates.”
It was clear that our family participants felt the need to witness and experience what their loved one was going through in the care home. However, Rosie’s son did conclude that the robot cannot replace in-person visiting:
It’s a different thing even though you have the robot. To see [her] in person. . . I don’t think this can be replaced. It [In person] is a physical touch. We are humans, we like to touch and feel each other. There’s still a gap [between robot visits and in-person visits]. If I have the opportunity, I will visit her in person. However, the robot will help refresh her memory to talking to me.
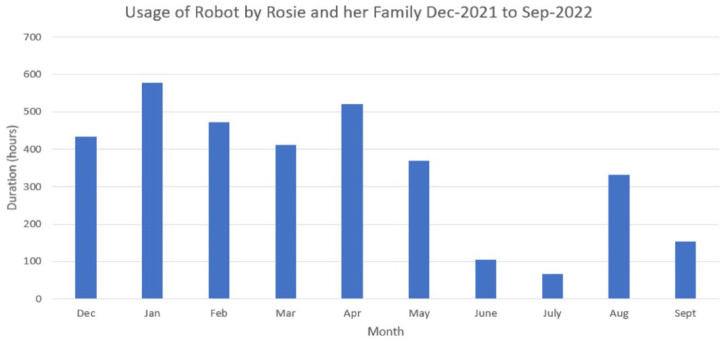
Figure 2 shows an example of the duration of time that the robot was utilized between the period of December 2021 and September 2022. The data shows that Rosie and her family used the robot for a total of 3,439 hr over a period of 10 months, which averages out to approximately 344 hr per month and 80 hr per week. The usage of robot was based on the availability of family member. We have explored the inconsistency in the trend of robot usage by Rosie’s family. Rosie’s family had fewer calls from June to August 2022, which was due to health issues and family responsibilities. In September 2022, the frequency of calls returned to 2 to 3 calls per week. This prompted our team to further investigate caregiver burden as a potential area of study.
Figure 2.
Usage of robot by Rosie’s family.
Challenge 1: “The Robot was Stuck”—Environmental Challenges in LTC
Several families faced difficulties driving and parking the robot due to space limitations in shared rooms. Multiple families found it challenging to correctly park the robot in the charging dock remotely; consequently, the robot could end up uncharged and unavailable for subsequent use.
In a shared space, it is also hard to predict whether a resident will have privacy to speak with the family. Max’s (resident in a shared room) family mentioned: “The sound was good on the robot, but the noise from TV next to us [from resident’s roommate] can make it somewhat difficult to hear.”
Challenge 2: “I Don’t Know Whether My Dad is Available or Not”—Residents’ Daily Routine During a Scheduled Call
Sometimes families call in the middle of care given by staff (e.g., toileting, washing). Even though residents can use the “end” button on the robot to exit the call, many do not seem to use it. George’s daughter explained that she wished there was a ring to notify her dad and the staff. Additionally, knowing the resident’s daily routine was important for scheduling calls. On one occasion, George’s daughter called her father while he was napping. She had to ask the staff to extend her visitation time. She expressed: “I don’t know whether my dad is available or not.”
Discussion
This study outlines the experiences shared by families and residents who used the robot in LTC over 4 to 12 months during the COVID-19 pandemic. Our findings offer in-depth insights to add to the literature, suggesting the value of using telepresence robots to address a pressing challenge of social isolation in LTC. Our family participants living overseas were able to remotely drive the robot, adjusting functions of the robot as needed, to talk with residents in LTC. The ease of controlling the robot on the family’s end helped to remove previous challenges that residents faced when using tablets/computers.
The robot’s ability to enhance social connectedness and family closeness was shared by many families. The freedom to have virtual visits is essential for maintaining relationships; the robot helps residents to maintain connections that remind them they are still included, valued, and loved, even though their physical surroundings have changed (Rosenberg & McCullough, 1981). The robot extended opportunities for everyday conversations that improved the residents’ feelings that their families pay attention to their needs, their living environment and the activities they engage in. With the enhanced sense of presence that families create via the robot, residents can feel that their space in the care home is not an isolated environment, but something collective that they can continue to share with loved ones. Moyle et al. (2019) wrote about the idea of collective immersion, as videos on the robot made visits feel authentic and engaging.
During covid-19, disruption of healthcare facilities and visitation restrictions hindered care routines, detrimentally impacting care partners (Messina et al., 2022). This created considerable stress for families, as it produced a sense of forced helplessness (Thirsk et al., 2022). In our study, it was evident that the robot supported family and residents. Bill’s family felt that the ability to control virtual visits on their end enabled their father with dementia to manage calls. Max’s wife highlighted the robot gave her peace of mind because she could check on her husband anytime to ensure his wellness. Rosie’s family emphasized that because they could engage with their mom every day, they could monitor and detect minor changes in her wellbeing, behavior, and attitude.
These findings support previous literature, which detail the enhanced applications for monitoring and security that telepresence robots have compared to other communication technologies (Moyle et al., 2019). Rosie’s daughter took advantage of the robot’s mobility to create a daily routine of exercise and water consumption. Although covid-19 restrictions function to limit families’ participation in visiting and care, the robot can help restore independence for families who want to be included in the care and daily life of residents. In addition, the worry and stress of future unknown situations may be lessened through the robot: several families shared that in the event of future unknown challenges, such as another lockdown, the robot provides a sense of security and peace of mind. Having a supportive tool that can connect families to residents at their convenience and control reduces worry about unforeseen events that may disrupt autonomy, connection, and stability.
Our findings contribute to previous literature by providing new insight into the benefits that the robot can bring to residents over a longer period of use. Time and routine are key factors that can enhance experiences with using robots. We found that many residents needed time to adapt to the robot. Rosie initially did not respond to her daughter’s prompts for exercise via the robot. Rosie’s daughter learned that it takes time for her mother to respond to her via the robot. This challenges the assumption that people with dementia cannot accept or learn to use the robot. In our study, some families questioned the residents’ ability to engage with the robot initially and became impressed that the virtual visits were well-accepted by residents. Our longer implementation period confirmed that through experience and practice, acceptance can be gained. This is significant, as there is so much stigmatization toward LTC homes and dementia.
Over the implementation period, several challenges emerged. Space limitations in resident rooms made it challenging to maneuver the robot remotely. To help support these families, our team held multiple in-person robot training sessions. We created instructional videos for families to have at hand for review of training. Over time, we learned that the robot also requires care: the robot must be monitored and maintained to ensure it is available for use at the family’s time of need. To prevent robot unavailability, we provided in-person training sessions and videos for staff as well, so that they could be familiarized with the robot and understand how to help the family if needed. Another challenge we noticed was that during initial days of robot deployment, scheduling was difficult. However, as time went on, families became more familiar with the daily routine of their loved ones. During covid outbreaks, the robot was especially helpful because residents were confined to their rooms. The robot was needed for families to routinely explain to residents about why they should stay in the room to reduce the spread of the virus. When a family was sick with COVID, the robot was also used by the resident to comfort their sick family member outside LTC as well.
Additionally, as reported by multiple other studies (Moyle et al., 2014, 2019), internet connectivity can be a challenge. Poor connectivity can lead to picture delays and sound distortions. To help support a smoother experience, our team provided an enhanced internet connection option to the LTC homes. This helped resolve some connectivity issues. However, strength of connection will also depend on the internet of the caller as well. Thus, it is important to consider if families can call from a location with adequate internet connectivity.
To further address these challenges, there is a need for structural and infrastructure support from management, as internet connectivity issues can be a challenge to technological implementation. Staff support and buy-in are also significant for robot engagement. Collaborating with family and residents to plan strategies to overcome challenges is important. The challenge of scheduling calls appropriately was overcome by integrating input from family, staff, and our team. Families communicated with staff to obtain residents’ weekly timetables, subsequently scheduling calls based on their availability. Thus, to optimize the experiences of residents and families, we must engage with care recipients and providers (residents and staff) to guide implementation. Future studies should seek to understand staff experience with robots as well; their close relationships with residents and opportunity for frequent in-person observation provides additional insight surrounding the robot’s impact on residents.
Strengths and Limitations
One strength of our study is that we collaborated meaningfully with patient and family partners in research planning, data collection, and analysis. Our patient and family partners have diverse experiences about dementia care in LTC settings. They provide a lived experience perspective to support the interpretation of data. Another strength is our long-term implementation and qualitative evaluation of robot use. A longer period of implementation helped to deepen insight into how positive impacts and challenges emerge over time. Adapting our methods to highlight the voices of residents and families was key to developing a deeper understanding of what the robot means to these participants. One limitation is the small population spread (racial backgrounds and ethnicity) that our study reports, as well as the risk of bias in using a purposive sampling method. The population in Canadian LTC is diverse. Our research setting was urban LTC, which limits any insight into how the technology usage may differ in remote and rural settings. Future research should examine how robot usage may vary depending on location, as well as racial, ethnic, and cultural backgrounds.
Conclusion
This study provides a rich understanding of the experiences and challenges that LTC residents and families face in using telepresence robots during the COVID-19 pandemic. Our findings indicate that telepresence robots in LTC can be a useful tool for families and residents. Older adults in early and later stages of dementia in the study were able to use the robot to connect with family. Future research should explore a more diverse population of participants to further understand how the use of telepresence can be optimized and personalized.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by funding from Vancouver Foundation Participatory Action Research Grant, VGH Foundation and RH Foundation. There were no financial, commercial, professional, or legal conflicts of interest related to this work. [Vancouver Foundation PAR Grant GR019971].
ORCID iDs: Lillian Hung  https://orcid.org/0000-0002-7916-2939
https://orcid.org/0000-0002-7916-2939
References
- Black B. S., Rabins P. V., Sugarman J., Karlawish J. H. (2010). Seeking assent and respecting dissent in dementia research. The American Journal of Geriatric Psychiatry, 18(1), 77–85. 10.1097/JGP.0b013e3181bd1de2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boamah S. A., Weldrick R., Lee T. J., Taylor N. (2021). Social isolation among older adults in long-term care: A scoping review. Journal of Aging and Health, 33(7–8), 618–632. 10.1177/08982643211004174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., Clarke V. (2021). To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qualitative Research in Sport, Exercise and Health, 13, 201–216. 10.1080/2159676X.2019.1704846 [DOI] [Google Scholar]
- Braun V., Clarke V. (2022). Conceptual and design thinking for thematic analysis. Qualitative Psychology, 9(1), 3–26. 10.1037/qup0000196 [DOI] [Google Scholar]
- Chu C. H., Ronquillo C., Khan S., Hung L., Boscart V. (2021). Technology recommendations to support person-centered care in long-term care homes during the COVID-19 pandemic and beyond. Journal of Aging & Social Policy, 33(4–5), 539–554. 10.1080/08959420.2021.1927620 [DOI] [PubMed] [Google Scholar]
- Chu C. H., Yee A., Stamatopoulos V. (2022). Poor and lost connections: Essential family caregivers’ experiences using technology with family living in long-term care homes during COVID-19. Journal of Applied Gerontology, 41(6), 1547–1556. 10.1177/07334648221081850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotten S. R. (2021). Chapter 23: Technologies and aging: Understanding use, impacts, and future needs. In Ferraro K. F., Carr D. (Eds.), Handbook of aging and the social sciences (pp. 373–392). Academic Press. [Google Scholar]
- Double Robotics. (2022). Double 3 overview. https://www.doublerobotics.com/double3.html
- Francis J., Rikard R. V., Cotten S. R., Kadylak T. (2019). Does ICT use matter? How information and communication technology use affects perceived mattering among a predominantly female sample of older adults residing in retirement communities. Information, Communication & Society, 22(9), 1281–1294. 10.1080/1369118X.2017.1417459 [DOI] [Google Scholar]
- Hardy M., Fanaki C., Savoie C., Dallaire C., Wilchesky M., Gallani M. C., Gagnon M., Laberge M., Voyer P., Côtéc A., Couture V., Dallaire B. (2022). Acceptability of videoconferencing to preserve the contact between cognitively impaired long-term care residents and their family caregivers: A mixed-methods study. Geriatric Nursing, 48, 65–73. 10.1016/j.gerinurse.2022.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung L., Mann J., Perry J., Berndt A., Wong J. (2022). Technological risks and ethical implications of using robots in long-term care. Journal of Rehabilitation and Assistive Technologies Engineering, 9, 20556683221106917. 10.1177/20556683221106917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung L., Wong J., Smith C., Berndt A., Gregorio M., Horne N. (2022). Facilitators and barriers to using telepresence robots in aged care settings: A scoping review. Journal of Rehabilitation and Assistive Technologies Engineering, 11(9), e051769. 10.1136/bmjopen-2021-051769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickert C., Rozak H., Masek J., Eigner K., Schaefer S. (2020). Maintaining resident social connections during COVID-19: Considerations for long-term care. Gerontology and Geriatric Medicine, 6, 233372142096266. 10.1177/2333721420962669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindell J., Keady J., Sage K., Wilkinson R. (2017). Everyday conversation in dementia: A review of the literature to inform research and practice. International Journal of Language & Communication Disorders, 52(4), 392–406. 10.1111/1460-6984.12298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann J., Hung L. (2018). Co-research with people living with dementia for change. Action Research, 17(4), 573–590. 10.1177/1476750318787 [DOI] [Google Scholar]
- Messina A., Lattanzi M., Albanese E., Fiordelli M. (2022). Caregivers of people with dementia and mental health during COVID-19: Findings from a cross-sectional study. BMC Geriatrics, 22, 56. 10.1186/s12877-022-02752-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan D. L. (2002). Focus group interviewing. In Gubrium J. F., Holstein J. A. (Eds.), Handbook of interview research: Context & method (pp. 141-160). Sage Publications. 10.4135/9781412973588 [DOI] [Google Scholar]
- Moyle W., Jones C., Cooke M., O’Dwyer S., Sung B., Drummond S. (2014). Connecting the person with dementia and family: A feasibility study of a telepresence robot. BMC Geriatrics, 14(7), 1–11. 10.1186/1471-2318-14-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyle W., Jones C., Dwan T., Ownsworth T., Sung B. (2019). Using telepresence for social connection: Views of older people with dementia, families, and health professionals from a mixed methods pilot study. Aging and Mental Health, 23(12), 1643–1650. 10.1080/13607863.2018.1509297 [DOI] [PubMed] [Google Scholar]
- Moyle W., Jones C., Sung B. (2019). Telepresence robots: Encouraging interactive communication between family carers and people with dementia. Australasian Journal on Ageing, 39(1), 127–133. 10.1111/ajag.12713 [DOI] [PubMed] [Google Scholar]
- Rosenberg M., McCullough B. C. (1981). Mattering: Inferred significance and mental health among adolescents. Research in Community & Mental Health, 2, 163–182. [Google Scholar]
- Saad A., Magwood O., Benjamen J., Haridas R., Hashmi S. S., Girard V., Sayfi S., Unachukwu U., Rowhani M., Agarwal A., Fleming M., Filip A., Pottie K. (2022). Health equity implications of the COVID-19 lockdown and visitation strategies in long-term care homes in Ontario: A mixed method study. International Journal of Environmental Research and Public Health, 19(7), 4275. 10.3390/ijerph19074275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thirsk L. M., Stahlke S., Perry B., Gordon B. (2022). #Morethanavisitor: Experiences of covid 19 visitor restrictions in Canadian long-term care facilities. Family Relations, 71, 1408–1427. 10.1111/fare.12712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Baan F., Aarts S., Verbeek H. (2020). Amidst the COVID-19 Pandemic: Video calling for connecting with family residing in nursing homes. IPA Bulletin, 8–12.
- Zamir S., Hennessy C. H., Taylor A. H., Jones R. B. (2018). Video-calls to reduce loneliness and social isolation within care environments for older people: An implementation study using collaborative action research. BMC Geriatrics, 18, 62. 10.1186/s12877-018-0746-y [DOI] [PMC free article] [PubMed] [Google Scholar]