ABSTRACT.
Tuberculosis (TB) and poverty are inextricably linked. Catastrophic costs of TB illness drive TB-affected households into worsening impoverishment and hamper treatment success. The WHO’s End TB Strategy recommends social protection for TB-affected households to mitigate financial shock and improve TB outcomes. This scoping review maps the landscape of social protection interventions for people with TB and their households in low- and middle-income countries with high TB burden. A systematic search of Medline, Embase, PubMed, and Web of Science for relevant articles was performed, supplemented with a gray literature search of key databases. Articles were included if they described social protection available to people with TB and TB-affected households in a low- or middle-income country. Data were synthesized in tabular form, and descriptive narrative outlined the successes and challenges of the social protection interventions identified. The search identified 33,360 articles. After abstract screening, 74 articles underwent full text screening, and 49 were included in the final analysis. Forty-three types of social protection were identified, of which 24 were TB specific (i.e., only people with TB were eligible). Varying definitions were used to describe similar social protection interventions, which limited cross-study comparison. Intervention successes included acceptability and increased financial autonomy among recipients. Challenges included delays in intervention delivery and unexpected additional bank transfer fees. A wide range of acceptable social protection interventions are available, with cash transfer schemes predominating. Use of standardized definitions of social protection interventions would facilitate consolidation of evidence and enhance design and implementation in future.
INTRODUCTION
Tuberculosis remains a global public health priority. It is predicted that there will be a 20% increase in TB deaths over the coming 5 years due to the impact of COVID-19.1 TB not only has devastating health implications but also severe socioeconomic impacts on those affected and their households. This socioeconomic burden falls mostly on poorer and vulnerable people and communities in low- and middle-income countries and perpetuates a cycle of poverty.2 An analysis by Silva et al. suggested that delays in achieving the World Health Organization’s 2015 End TB Strategy goals to reduce TB prevalence and mortality would have profound economic and health consequences, which would disproportionately affect sub-Saharan African countries.3 The major drivers of TB are undernutrition, poverty, diabetes, tobacco smoking, and household air pollution,4 which contribute to nearly half of the global TB burden. Such determinants need to be addressed urgently, including through social protection.5
When identified and treated early, TB is curable. However, there remain numerous challenges to completing treatment and achieving prolonged cure. The standard treatment regimen for drug-sensitive TB (DS-TB) lasts for 6 months. Drug-resistant TB (DR-TB) regimens are arduous, toxic, can involve injectable agents, can extend up to 24 months.6,7 The socioeconomic impacts of DS-TB and especially DR-TB are severe. Although all age groups are at risk, TB tends to affect adults in their most economically productive years. The economic devastation associated with loss of income and productivity, unemployment, and out-of-pocket medical costs (e.g., consultations, tests, pills) and nonmedical costs (e.g., food, travel) can make even “free” TB care expensive.8 Catastrophic costs (defined as total TB-related costs > 20% of a TB-affected household’s annual pre-TB income) can reduce the capacity of a household to cope with financial shocks and hamper access to and completion of TB treatment.8 According to the 2021 Global TB report, 45% and 87% of DS-TB and DR-TB-affected households incur catastrophic costs.9
The TB poverty cycle can be interrupted using social protection measures that alleviate poverty, reduce food insecurity and mitigate catastrophic costs of TB-affected households.10,11 Previous systematic reviews have examined the impact of social protection on the social determinants of TB.10–13 However, breadth and depth of exploration has been constrained by a limited evidence base and variable definitions or scope of what constitutes social protection. Moreover, since the introduction of the End TB strategy in 2015, which emphasized the importance of addressing the social determinants and consequences of TB and included a global Catastrophic Costs indicator, there has been a notable expansion of new evidence in the field.
This scoping review (ScR) will provide a much-needed assessment of the social protection interventions and programs available for people with TB and their households and evaluate the challenges and successes of their implementation including intervention design, recipients, and logistics of access, delivery, and receipt.
The aims of this ScR were to 1) establish what social protection interventions are available to people with TB and their households in low- and middle-income and/or TB high-burden countries, 2) describe the successes and challenges of implementation and delivery of available social protection interventions, and 3) inform the design of a systematic review and meta-analysis of the impact of social protection on TB and socioeconomic outcomes.
METHODS
To facilitate future similar reviews or related comparative reviews, this ScR used the recognized World Bank definition of social protection being “systems which seek to improve inequalities and reduce intergenerational poverty by seeking to help individuals and families, especially the poor and vulnerable, cope with crises and shocks, find jobs, improve productivity, invest in the health and education of their children and protect the aging population.”14 This umbrella term refers to interventions that include but are not limited to cash transfers, vouchers, food baskets, and nutritional supplementation.
The ScR was guided by the Arksey and O’Malley guidance and PRISMA ScR (PRISMA-ScR) extension checklist, which suggest inclusive search strategies of both the published and gray literature.15–17 A literature search was carried out in the research databases PubMed, Embase, Medline and Web of Science on March 10, 2021 (see supplemental materials for full search strategies). The eligibility criteria were defined using the PICOT approach outlined in Table 1. With regard to outcomes, the scoping review focused primarily on process outcome measures including successes and challenges of social protection interventions. As per a key aim of the ScR, impact outcome measures such as TB treatment outcome and catastrophic costs were also included as part of the eligibility criteria to identify studies with quantitative outcome data suitable for inclusion in a related systematic review and meta-analysis of the impact of social protection on TB and broader socioeconomic outcomes.
Table 1.
PICOT inclusion criteria
| Population | People with tuberculosis (TB) or living in TB-affected households (e.g., one or more household members with TB disease) were included. Countries classified by the World Bank as TB high-burden countries and/or low- and middle-income countries at the time the study was conducted were included. Countries classified as high income and/or non–high burden at the time of study were excluded. |
| Intervention | Standard TB care and access to at least one social protection intervention or program. In this context, access is defined as the receipt of services, not just the existence of a social protection intervention or program in a given area. |
| Control | People with TB receiving standard TB care who did not have access to any social protection intervention or program. |
| Outcomes |
|
| Time | All studies published from 2012 to present were considered. The time frame for study eligibility is based on the “World Bank’s Social Protection and Labour Strategy 2012–2022,” in which the World Bank focused their initiatives on reducing socioeconomic risk and strengthening social protection programs. Expanding the date range beyond this would have resulted in a yield of studies too great to manage. |
Articles were exported and managed in Covidence (covidence.org, Australia) and duplicate articles removed. Articles with relevant titles qualified for abstract screening. Abstracts screened as relevant to the topic and meeting eligibility criteria were selected for full text inclusion and review. Reference checking of articles eligible for full text review was conducted to identify additional studies missed in the initial search strategy. Two authors (M. H. and H. T.) were responsible for full text screening to minimize selection bias and enhance reliability and validity of this review. Each investigator screened every article once and, where there was disagreement, a third reviewer (T. W. and P. B. S.) acted as a tiebreaker. All observational, qualitative, interventional, and randomized studies meeting the eligibility criteria and written in English were included. All types of reviews and meta-analyses were excluded due to the inherent bias associated with secondary literature where authors have examined a topic and drawn their own conclusions.
For gray literature, searches were carried out in key repositories identified a priori by the ScR team (the WHO [who.int], International Labour Organization [ilo.org], Word Bank [worldbank.org], World Food Programme [WFP], wfp.org). The gray literature search was conducted on June 14, 2021, using Google Advanced and The Bielefield Academic Search Engine (BASE, Bielefeld University Library, Bielefeld, Germany). Results were exported as .CSV files to Microsoft Excel and stored using the GoogleChrome (Alphabet Inc., Mountain View, CA) extension SEOQuake (Semrush Inc., Trevose, PA). The time frame eligibility was defined based on the introduction of the Millennium Development Goals in 2000. Matching the time frame for gray literature to published literature limited the yield of documents to a very low number and, to accommodate this, the search criteria were expanded. Results were limited to documents written in English, pdf files and documents created between 2000 and 2021. Gray literature identified was deemed relevant and eligible if written in English between 2000 and 2021 and a PDF file that named a social protection program in a TB high-burden country or low- and middle-income country and included details of the intervention recipients. Documents were excluded if there were no details of a social protection intervention for people affected by TB or people living in TB-affected households. Finally, selected articles and documents were retrieved for data extraction. Information was inputted into a data extraction table, stored in Microsoft Excel. The data were synthesized in a combination of narrative and tabular format using simple descriptive quantitative analysis. Data were summarized into categories to facilitate the interpretation of findings and draw meaningful conclusions.20
A formal consultation exercise was not carried out within this ScR. Instead, the findings of this ScR were presented and discussed at relevant international partnerships and collaborations including the Social Protection Action Research and Knowledge Sharing network (SPARKS, www.sparksnetwork.ki.se) and related, active WHO Advisory Groups and Task Forces.
Ethics approval was not required for this ScR because primary data were not collected and the secondary data used was publicly available.
RESULTS AND FINDINGS
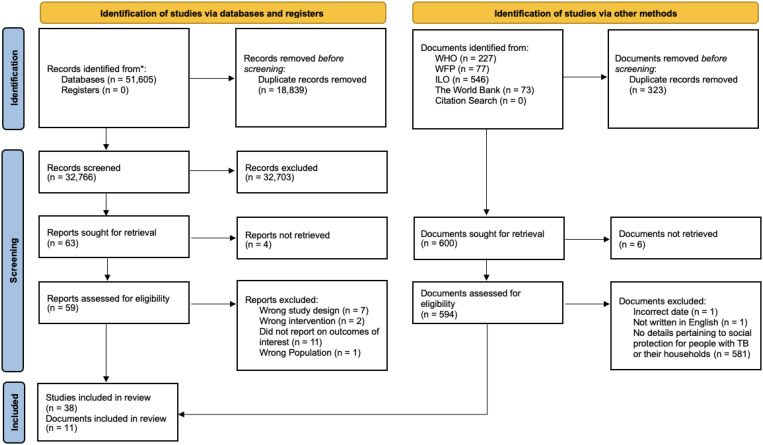
The search strategy identified 32,766 discrete articles that were screened according to the eligibility criteria of which 38 were included in this scoping review (Table 2). The gray literature search identified 594 documents that were assessed for eligibility, of which 11 were included in the review (Table 3). A flowchart of the screening and selection process is shown in Figure 1.
Table 2.
Characteristics of included studies
| Author (year) | Study design | Outcomes | Country | Setting | TB HBC | Income classification |
|---|---|---|---|---|---|---|
| Ciobanu et al.21 | Cohort | Treatment success; number of people with TB receiving incentives; types of incentives among those who received them | Moldova | Mixed | No | LMIC |
| Ukwaja et al.22 | Cohort | Treatment success; determinants of successful outcomes | Nigeria | Rural | Yes | LMIC |
| Oliosi et al.23 | Cohort | Treatment outcomes | Brazil | Urban | Yes | UMIC |
| Torrens et al.24 | Cohort | Treatment success | Brazil | Mixed | Yes | UMIC |
| Rohit et al.25 | Cohort | Treatment outcomes | India | Mixed | Yes | LMIC |
| Priedeman Skiles et al.26 | Cohort | Loss to follow-up; program impact on treatment default* | Ukraine | Mixed | Yes | LMIC |
| Klein et al.27 | Cohort | Treatment success | Argentina | Urban | Yes | UMIC |
| Malacarne et al.28 | Case–control | Treatment success | Brazil | Peri-urban | Yes | UMIC |
| Bhavesh et al.29 | Cohort | Utilization of social protection program; treatment success | India | Urban | Yes | LMIC |
| Mansour et al.30 | Cohort | Lost to follow-up (defined as unable to be located, never started treatment after diagnosis confirmed or treatment interrupted after > 2 months) | Kenya | Mixed | Yes | LMIC |
| Bhatt et al.31 | Cohort | Treatment success | India | Urban | Yes | LMIC |
| Samuel et al.32 | Cohort | Treatment success | India | Mixed | Yes | LMIC |
| Durovni et al.33 | Cohort | Treatment outcomes | Brazil | Urban | Yes | UMIC |
| Rudgard et al.34 | Cross-section survey | Financial hardship† | Brazil | Urban | Yes | UMIC |
| Chirico et al.35 | Case control | Clinical and epidemiological differences between people with TB included versus not included in the social protection regimen; treatment success | Argentina | Urban | Yes | UMIC |
| Zhao et al.36 | Observational | Financial burden of transportation; recipient’s perceptions of social protection intervention | China | Rural | Yes | UMIC |
| Soares et al.37 | Observational | Treatment success | Brazil | Urban | Yes | LMIC |
| Kaliakbarova et al.38 | Observational | Treatment success; recipient satisfaction with social protection program | Kazakhstan | Urban | Yes | UMIC |
| Rogers et al.39 | Cohort | Treatment success | Liberia | – | No | LIC |
| De Souza et al.40 | Ecological study | TB mortality rate, obtained by national databases41 | Brazil | – | Yes | UMIC |
| Reis-Santos et al.42 | Longitudinal database study | TB cure; broader clinical and social determinants of TB treatment outcomes | Brazil | Mixed | Yes | UMIC |
| Contreras et al.43 | Cohort | Socioeconomic needs of recipients of the social protection program “TB Cero”; how “TB Cero” social protection intervention addresses socioeconomic needs through qualitative evaluation | Peru | Peri-urban | No | UMIC |
| Ngamvithayapong-Yanai et al.44 | Observational | Treatment outcomes | Thailand | Urban | Yes | LMIC |
| Diaw et al.45 | Observational | Treatment outcomes; retention of recipients enrolled in program | Senegal | Rural | Yes | LIC |
| Wingfield et al.46 | Cohort study and RCT | Quantify prevalence of catastrophic costs; national TB control program-confirmed TB cure in people with TB | Peru | Urban | Yes | UMIC |
| Lutge et al.47 | Unblinded cluster RCT | Treatment outcomes; loss to follow-up and treatment failure rate | South Africa | Mixed | Yes | UMIC |
| Carter et al.48 | Quasi-experimental | TB treatment success | Brazil | Mixed | Yes | UMIC |
| Wei et al.49 | Quasi-experimental | Cost to person with TB‡; Cost-effectiveness of the social protection program | China | Urban | No | MIC |
| Wingfield et al.50 | RCT | Catastrophic costs | Peru | Urban | Yes | UMIC |
| Wingfield et al.51 | RCT | Initiation of TB preventive therapy; treatment success | Peru | Urban | Yes | UMIC |
| Ukwaja et al.52 | Qualitative | Recipients’ experience of social protection intervention | Nigeria | Urban | Yes | UMIC |
| Orlandi et al.53 | Qualitative | Perceived influence of social incentive on treatment adherence among healthcare professionals | Brazil | Urban | Yes | UMIC |
| George et al.54 | Qualitative | Analysis of support services available to people with TB | India | Rural | Yes | LMIC |
| Patel et al.55 | Mixed methods | Receipt of cash transfer; time to receipt of first cash transfer | India | Urban | Yes | LMIC |
| Yin et al.56 | Mixed methods | Treatment outcomes; TB treatment adherence§ | China | Urban | Yes | UMIC |
| Li et al.57 | Mixed methods | Access to TB diagnosis and treatment; affordability of TB treatment to person with TB | China | Urban | Yes | UMIC |
| Xiang et al.58 | Mixed methods | Reimbursement of out-of-pocket costs; catastrophic health expenditure¶ | China | Rural | Yes | UMIC |
| Sripad et al.59 | Mixed methods | Recipients’ perceptions of social protection program activities available to them; TB treatment adherenceǁ | Ecuador | Mixed | No | MIC |
HBC = high-burden country; LMIC = low- and middle-income countries; MIC = middle-income countries; RCT = randomized controlled study; TB = tuberculosis; UMIC = upper middle-income countries.
Treatment default was defined as anyone who missed treatment for more than 60 days per WHO standards.
Financial hardship = total costs exceeding 20% of preillness annual household income and/or relying on a negative financial coping strategy (i.e., taking a loan or selling assets); and/or total costs that are impoverishing (incurring total monthly costs that pushed preillness monthly household income per capita below Brazil’s 2016 poverty line [USD 48.6 per month]).
Patient costs = defined as direct medical (clinics, medicines, tests) and nonmedical (travel, food) out-of-pocket payments.
Adherence = taking medications 26 days per month up for up to 24 months.
Catastrophic health expenditure was defined as 10% of annual family income.
Adherence was measured using interruption; anytime during the entire treatment period that two doses of treatment were missed for at least 2 weeks but less than 2 consecutive months.
Table 3.
Characteristics of gray literature
| Author (year) | Document type | Document title | Country | TB HBC | Income classification |
|---|---|---|---|---|---|
| Loveleen et al.60 | Report | An Assessment of the Social Protection Needs and Gaps for Workers in Informal Employment in Myanmar | Myanmar | No | LMIC |
| Mahadevia61 | Working paper | Decent Work in Ahmedabad: An Integrated Approach | India | Yes | LMIC |
| World Bank62 | Report | The State of Social Safety Nets 2015 | Tajikistan | Yes | LMIC |
| Spray63 | Report | Leveraging Social Protection Programs for Improved Nutrition: Compendium of Case Studies Prepared for the Global Forum on Nutrition Sensitive Social-Protection Programs | Democratic Republic of Congo | Yes | LMIC |
| WHO64 | Report | National Strategic Plan for Ending TB 2020–2024, Timor-Leste | Timor-Leste | Yes | LMIC |
| Nurova65 | Project report | Support for Tuberculosis Patients and Their Families Standard Project Report 2016 | Tajikistan | Yes | LMIC |
| WFP66 | Report | Regional Bureau for Southern Africa | Lesotho | Yes | LMIC |
| Madagascar | No | LIC | |||
| Eswatini* | No | LMIC | |||
| Zambia | No | LMIC | |||
| WFP74 | Project report | Supporting Transition by Reducing Food Insecurity and Undernutrition Among the Most Vulnerable | Myanmar | No | LMIC |
| WFP67 | Project report | Standard Project Report 2015; World Food Programme in Congo | Democratic Republic of Congo | Yes | LMIC |
| WFP41 | Project evaluation | Responding to Humanitarian Needs and Strengthening Resilience to Food Insecurity | Zimbabwe | Yes | LMIC |
| Foster68 | PhD thesis | Structure and Agency in the Economics of Public Policy for TB Control | South Africa | Yes | UMIC |
HBC = high-burden country; LMIC = low- and middle-income countries; MIC = middle-income countries; TB = tuberculosis; UMIC = upper middle-income countries; WFP = World Food Programme.
In contrast with peer-reviewed publications included in this scoping review, gray literature lacks clear definitions of categories described in Table 2, reflecting data collected in peer-reviewed publications (author, study design, study outcomes).
Referred to in study as its previous name, Swaziland.
Figure 1.
Flow chart of identification, screening, and inclusion of studies included in the scoping review.
Study characteristics.
Most published studies (24/38, 61%) were observational. There was wide geographic distribution with studies from 15 low- and middle-income countries. Middle-income countries accounted for most included studies with only two being from low-income countries. Thirty-five (92%) studies were from TB high burden countries (HBC). Nearly half (17/38, 45%) of the studies were from South America, and 10 of these were based in Brazil. Most study settings were urban or periurban (21/38, 55%) with four from rural settings and 11 from more than mixed urban and rural settings.
Of the 11 gray literature documents included, 10 were reports from multilateral organizations (WHO, WFP, and ILO) and one was a PhD thesis. These documents described social protection programs from 11 countries, seven of which were TB HBCs.
Description of social protection programs.
Forty-three social protection programs were identified across the selected studies and are summarized in Table 4. Of the programs identified, 24 were described as TB-specific interventions, 15 were TB inclusive, and four were not classified. These social protection programs were grouped into three distinct categories including financial intervention, food support, and community participation. Financial interventions such as cash transfer tended to be designed to prevent out-of-pocket costs and lost income associated with TB illness and care. Food support and community participation were designed to alleviate the broader impacts of poverty such as food insecurity and malnutrition.
Table 4.
Summary of characteristics of social protection programs
| Social protection program (N = 43) | ||
|---|---|---|
| n | % | |
| Target recipient group | ||
| All people with TB | 17 | 40 |
| People with MDR-TB | 7 | 16 |
| TB and other diseases | 7 | 16 |
| TB-affected household | 5 | 12 |
| Not defined | 3 | 7 |
| People with TB/HIV | 1 | 2 |
| Migrants with TB | 1 | 2 |
| People with TB and food insecurity | 1 | 2 |
| People with DS-TB | 1 | 2 |
| Social protection type | ||
| Nutritional/food support | 13 | 30 |
| Conditional cash transfer | 12 | 28 |
| A combination of financial and nutritional/food support | 9 | 21 |
| Unconditional cash transfer | 5 | 12 |
| Other financial intervention | 2 | 4.5 |
| Community participation | 2 | 4.5 |
| Funding | ||
| Multilateral organization | 16 | 37 |
| Government | 13 | 30 |
| Mixed funding sources | 5 | 12 |
| Nongovernmental organization | 3 | 7 |
| Other | 6 | 14 |
| TB specific versus TB inclusive | ||
| Specific | 26 | 60 |
| Inclusive | 17 | 40 |
DS = drug susceptible; MDR = multidrug resistant; TB = tuberculosis.
The eligibility criteria that recipients had to meet to qualify for social protection were similar regardless of the type of social protection offered. Three overarching eligibility criteria were common to all programs: poverty and/or malnutrition, and/or an assessment by a healthcare or social work professional affiliated with the social protection program. Commonly, people with TB had to meet a specified poverty level to be eligible for the intervention. Two programs used other means of assessment including exposure to TB risk factors, and social assessment by a nonstatutory body of socially responsible citizens and volunteers chaired by local government.26,69 For seven of the programs, the eligibility criteria were undefined.
Financial support interventions.
The type, value, duration and mechanism of financial support and interventions varied greatly. Of the 19 programs that described a financial intervention, 12 used conditional cash transfer, five used unconditional cash transfer and two used a financial intervention other than cash transfer. For example, in Thailand, women of study-defined high socioeconomic status were engaged in social protection programs as financial supporters of those with TB and their households.44 Most financial support was given monthly, except for Nikshay Poshan Yojana, a conditional cash transfer program based in India, which made payments once every 2 months, these began only after 2 months of TB treatment is completed.25 Although most programs did not stipulate on what the cash or financial support had to be spent, a randomized study in South Africa offered US$15 in the form of a voucher, which could be redeemed in shops chosen by the clinic to monitor spending and prevent purchase of “harmful goods.”47 Other programs stated that the cash was intended to be used for nutrition or transport, but spending was in the autonomous control of the recipient.25,56
The size of cash transfers varied greatly from 8 USD in India for an unconditional cash transfer scheme to up to 20,000 USD55 in the form of insurance reimbursement in China57 (see supplemental material). Minimal evidence exists regarding the proportion of annual income that cash transfers represent and rationale behind the size of transfers, but there was some consensus among reports that the value should be large enough to mitigate against poverty-related TB risk factors and incentivize households to engage with the intervention, while being too small to potentially act as a perverse incentive.
Nonfinancial support interventions.
Sixteen distinct nonfinancial interventions were identified, the majority (13/16) of which were in the form of nutritional/food support. All nonfinancial support programs were based in Africa and Asia except for the Rocinha Intervention, which provided a supportive community health worker to people with TB in an urban settlement in Brazil.37
All nutritional/food support programs were funded by the WFP and targeted a range of TB populations. Six programs offered nutritional/food support to all people with TB, two specifically targeted people with TB and HIV, and two targeted people with DR-TB only. The content of nutrition/food support interventions varied from country to country but consisted of a core basic food parcel containing pulses, cereal, and vegetable oil. Programs aimed to provide the nutritional/food support at daily or monthly frequency and covered a proportion rather than the total food consumption of a TB-affected household.60,65
Community participation programs can be described as social protection or welfare programs that create a supportive network and environment that enables people with TB to adhere to and complete their treatment, adhere to preventive therapy, and avoid deepening impoverishment.37,38,69 These interventions consisted of a variety of activities including the implementation of educational activities in group settings37 and signposting people with TB to appropriate education and free, quality welfare programs.69
Some programs incorporated nonfinancial and financial social protection components as either combined or separate interventions. Various examples were identified with a range of approaches including but not limited to electronic vouchers, nutritional supplement, payment of school fees and home utilities, career counseling, transport subsidy, and provision of other materials (e.g., clothing and fuel).21,26,31,39,51,57,60,67
There was a lack of data on direct and indirect costs of delivering financial and especially nonfinancial interventions, which precluded comparative analysis of their budgetary feasibility or impact.
Funding and resources for social protection.
Funding sources for social programs were variable, but ensuring adequate, suitable funding was reported as essential for success, longevity, and sustainability of social protection programs. The most common source of funding was from multilateral organizations (16/43, 37%). Other sources included NGOs, central government, or a combination of sources. Those funded by central government generally did not report funding issues and had improved staff retention.37 Some pilot programs showed smooth transition to more stable, long-term funding despite initially precarious funding. For example, in Thailand, Ngamvithayapong-Yani et al. reported concerns due to receiving initial funding from the Stop TB partnership to provide financial and transportation support to people with TB. However, no long-term funding source was allocated, and when the short-term grant funding ended, wealthy local women were recruited to continue to support the intervention.44
Successes and challenges of implementation.
A review of the articles that provided evaluative commentary on the implementation of social protection interventions identified several barriers to implementation relating to three broad categories: the beneficiary, the provider, and the system by which the program was rolled out.
Challenges included those related to user access and provider shortcomings, authors commonly reported lack of awareness among recipients as a common reason for low coverage of social protection programs.25,29,38,61,67 Others acknowledged there were various administrative and logistical issues reported for the providers with a recurrent issue being delays in instalments of financial support25,41,55,59 and hidden or opaque “maintenance” or other charges of banks, which could adversely affect beneficiaries.47,51,52,55 Lutge et al. also noted the issues associated with mandatory bank accounts being an eligibility criterion because many individuals in low-resource settings do not have access to a bank and/or do not have their own bank accounts. Hence, the article suggested that the program itself needs to ensure that all potential recipients have a bank account to ensure equity. Lutge et al. also described “street-level bureaucrats” (i.e., individuals who are a subset of a public agency where civil servants have direct contact with the public) who determined who was “worthy” of receiving this intervention; however, the administration period was so long, it often exceeded the length of treatment and consequently this intervention was not widely available.47
Some successes were described by authors—for example, the associated emancipation of women through the financial responsibility of managing cash transfers and opening personal bank accounts to receive them.8 As well as the overarching acceptability of cash transfer interventions among studied populations, others cited the knock-on beneficial impacts that social protection had on social standing and financial autonomy.25,33,50
DISCUSSION
What social protection is available?
This ScR identified an array of social protection interventions, the language used to describe them, and their intended positive impact on people with TB and their affected households. Overall, 49 documents were identified, of which 43 detailed distinct social protection programs as defined by the World Bank. Most programs were based in middle-income countries with high TB burden. Of these, 24 were TB-specific programs, which focused exclusively on providing financial interventions.
This ScR used a single, recognized social protection definition from the World Bank to inform its search strategy. Despite this, the results showed that a unifying definition of social protection was lacking across studies. Authors used a variety of distinct definitions, and terminology was variable and overlapping to describe the same social protection program activities; this represented a challenge to conducting an effective literature search. For example, seven studies explicitly defined programs as “incentives” where other authors have defined the same interventions as social protection21,25,26,29,49,53,59 despite the term not being included in the key words of search strategies of related reviews.10,11,70 This is a necessary and important distinction because incentives offer reward for treatment rather than reduction of socioeconomic risk that is offered by social protection strategies, as per the World Bank definition used in this ScR.62
Consistent with previous studies, this ScR identified that although there was a broad range of TB-specific social protection programs and interventions, most offered financial support, predominantly through conditional cash transfers. Indeed, less than 10% of identified studies reported TB-specific social protection programs that offered nonfinancial support.
Although a variety of subjective values perceived to be relevant to the context and intervention were used to determine eligibility for social protection, poverty was generally assessed using quantitative data on socioeconomic position. The stringent criteria used to target beneficiaries illustrated the complicated relationship between poverty and TB. However, it also highlighted that design and implementation of relevant national policy should be informed by an understanding of the poverty-related socioeconomic barriers that potential recipients face to effectively access social protection programs.47
Successes and challenges of implementation.
Most studies were designed to measure success of interventions quantitatively based on the single outcome of TB treatment outcomes or TB treatment success. A minority of studies reported other outcome measures such as catastrophic costs incurrence or catastrophic health expenditure. However, some identified studies did narratively report implementation successes, which revealed some cross-cutting factors. Secure, adequate, and sustainable funding with robust infrastructure was reported as essential for successful implementation of social protection interventions.71 Importantly, these factors dictate both what programs people with TB and their households can access and also how they are able to access these programs. Further, adequate funding will be necessary to ensure cash transfers sufficiently mitigate the costs associated with TB illness and care. Rohit et al.25 and Wingfield et al.72 included evaluative commentary relating to charge-free, appropriate bank accounts to support sustainable cash transfer to prevent delay in transfer and reduce risk of theft or fraud.
Although the ethos of cash transfers is to promote equitable access to TB treatment services,73 this ScR demonstrated that there are several barriers to achieving equity in resource-limited settings.47 This is particularly the case if a program requires bank or electronic transfer of funds or distribution of food baskets, which can be logistically complex and difficult to deliver to underserved groups. Lack of political will, commitment, and sustainable long-term funding—all of which were considered to be out of the control of those delivering non-governmental social protection programs—were identified as threats to the longevity of interventions.
Ultimately, despite social protection being a key feature of the End TB Strategy, the dearth of pragmatic operational and implementation evidence or practical guidance and policy on social protection for people with TB and their households needs to be addressed, particularly with respect to delivery of social protection as part of broader mixed, integrated, or nonfinancial interventions.7 Realistic operationalization of social protection programs is discussed by Bustos et al., who noted that successful social protection programs rely on a network of groups in socio-political, relational, and operational contexts.71 In light of this, better process evaluation and implementation research is required in this field to support integration of social protection into routine practice and scale-up at national level.
Recommendations for the design of SR and MA.
Because this work was conducted to inform a systematic review, frequent meetings were held to refine the systematic review search strategy and inclusion criteria iteratively based on the interim findings of the scoping review. The gray literature review ensured that the ScR search strategy was as broad as possible and captured global and regional policy and practice documents that may not have been peer reviewed. The ScR led to some refinement and streamlining of the outcome measures to be used in the systematic review given that several of them, including food insecurity and multidimensional poverty indices, were not measured in any of the included studies. Additionally, the ScR suggested that a narrative synthesis analysis to examine the qualitative outcomes of studies included in the proposed meta-analysis may be of benefit to contextualize interpretation of their quantitative findings.
Descriptive narrative in this ScR pertaining to operational challenges and pragmatic implementation of social protection discovered valuable evaluative comments and revealed opportunity for formal analysis of the characteristics required for successful programs. Numerical assessment of thriving programs in the systematic review could offer a “blueprint” of updated guidance to improve program integration.
Strengths and limitations.
This ScR was planned to minimize the risk of bias and maintain high quality. The clear, recognized World Bank definition of social protection that was used allowed for a careful selection and high yield of papers, which adds much value in terms of standardizing the language used to describe social protection as per the World Bank definition and how this relates to existing interventions and studies. Although social protection has been part of the global health agenda since the beginning of the millennium, restricting the search from 2012 onward was a necessary limitation. Although some interventions may have been omitted, conclusions have been drawn from a large, broad yield of papers and therefore are likely representative of any additional social protection programs. The findings of this ScR clearly show that the terminology surrounding social protection is ill defined and unclear. Literature could have been missed in the review because the search strategy did not capture all the terminology used to describe social protection programs.
CONCLUSION
There remains a dearth of high-quality pragmatic trials, effectiveness implementation trials, and rigorous mixed-methods studies in this area, which are essential for assessing feasibility and impact of social protection programs. Such studies provide valuable information to guide policy and decision makers. Nevertheless, this ScR demonstrates the range of designs and mechanisms by which social protection can be distributed to mitigate against the socioeconomic impacts of TB. These findings have informed design and implementation of an ongoing systematic review to evaluate the impact of social protection on TB, health, and socioeconomic outcomes.
Supplemental files
Note: Supplemental material appears at www.ajtmh.org.
REFERENCES
- 1. Wingfield T, Karmadwala F, MacPherson P, Millington K, Walker N, Cuevas L, Squire S, 2021. Challenges and opportunities to end tuberculosis in the COVID-19 era. Lancet Respir Med 9: 556–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Burki TK, 2018. The global cost of tuberculosis. Lancet Respir Med 6: 13. [DOI] [PubMed] [Google Scholar]
- 3. Silva S, Arinaminpathy N, Atun R, Goosby E, Reid M, 2021. Economic impact of tuberculosis mortality in 120 countries and the cost of not achieving the Sustainable Development Goals tuberculosis targets: a full-income analysis. Lancet Glob Health 9: e1372–e1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization , 2020. Global Tuberculosis Report 2020. Geneva, Switzerland: WHO. [Google Scholar]
- 5. Lönnroth K, Jaramillo E, Williams BG, Dye C, Raviglione M, 2009. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc Sci Med 68: 2240–2246. [DOI] [PubMed] [Google Scholar]
- 6. Hargreaves JR, Boccia D, Evans CA, Adato M, Petticrew M, Porter JDH, 2011. The social determinants of tuberculosis: from evidence to action. Am J Public Health 101: 654–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization , 2015. The End TB Strategy. Geneva, Switzerland: WHO. [Google Scholar]
- 8. Wingfield T, Boccia D, Tovar M, Gavino A, Zevallos K, Montoya R, Lönnroth K, Evans CA, 2014. Defining catastrophic costs and comparing their importance for adverse tuberculosis outcome with multi-drug resistance: a prospective cohort study, Peru. PLoS Med 11: e1001675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization , 2021. Global Tuberculosis Report 2021. Geneva, Switzerland: WHO. [Google Scholar]
- 10. Andrade KVF, Nery JS, Souza RA, Pereira SM, 2018. Effects of social protection on tuberculosis treatment outcomes in low or middle-income and in high-burden countries: systematic review and meta-analysis. Cad Saude Publica 34: e00153116. [DOI] [PubMed] [Google Scholar]
- 11. Aragão FBA, Arcêncio RA, Fuentealba-Torres M, Carneiro TSG, Souza LLL, Alves YM, Fiorati RC, 2021. Impact of social protection programs on adults diagnosed with tuberculosis: systematic review. Rev Bras Enferm 74: e20190906. [DOI] [PubMed] [Google Scholar]
- 12. Richterman A, Steer-Massaro J, Jarolimova J, Luong Nguyen LB, Werdenberg J, Ivers LC, 2018. Cash interventions to improve clinical outcomes for pulmonary tuberculosis: systematic review and meta-analysis. Bull World Health Organ 96: 471–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. van Hoorn R, Jaramillo E, Collins D, Gebhard A, van den Hof S, 2016. The effects of psycho-emotional and socio-economic support for tuberculosis patients on treatment adherence and treatment outcomes—a systematic review and meta-analysis. PLoS One 11: e0154095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. The World Bank , 2021. The World Bank in Social Protection. Available at: https://www.worldbank.org/en/topic/socialprotection. Accessed January 29, 2023.
- 15. Arksey H, O’Malley L, 2005. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 8: 19–32. [Google Scholar]
- 16. Tricco AC. et al. , 2016. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol 16: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Levac D, Colquhoun H, O’Brien KK, 2010. Scoping studies: advancing the methodology. Implement Sci 5: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization , 2013. Definitions and Reporting Framework for Tuberculosis—2013 Revision: Updated December 2014 and January 2020. Geneva, Switzerland: WHO. [Google Scholar]
- 19. Sweeney S, Mukora R, Candfield S, Guinness L, Grant AD, Vassall A, 2018. Measuring income for catastrophic cost estimates: limitations and policy implications of current approaches. Soc Sci Med 215: 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Graneheim UH, Lundman B, 2004. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 24: 105–112. [DOI] [PubMed] [Google Scholar]
- 21. Ciobanu A, Domente L, Soltan V, Bivol S, Severin L, Plesca V, Van den Bergh R, Kumar AMV, de Colombani P, 2014. Do incentives improve tuberculosis treatment outcomes in the Republic of Moldova? Public Health Action 4: S59–S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ukwaja K, Alobu I, Gidado M, Onazi O, Oshi D, 2017. Economic support intervention improves tuberculosis treatment outcomes in rural Nigeria. Int J Tuberc Lung Dis 21: 564–570. [DOI] [PubMed] [Google Scholar]
- 23. Oliosi JGN. et al. , 2019. Effect of the Bolsa Familia Programme on the outcome of tuberculosis treatment: a prospective cohort study. Lancet Glob Health 7: e219–e226. [DOI] [PubMed] [Google Scholar]
- 24. Torrens AW, Rasella D, Boccia D, Maciel ELN, Nery JS, Olson ZD, Barreira DCN, Sanchez MN, 2016. Effectiveness of a conditional cash transfer programme on TB cure rate: a retrospective cohort study in Brazil. Trans R Soc Trop Med Hyg 110: 199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rohit A, Kumar AMV, Thekkur P, Shastri SG, Kumar RBN, Nirgude AS, Reddy MM, Ravichandra C, Somashekar N, Balu PS, 2020. Does provision of cash incentive to HIV-infected tuberculosis patients improve the treatment success in programme settings? A cohort study from South India. J Family Med Prim Care 9: 3955–3964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Priedeman Skiles M, Curtis SL, Angeles G, Mullen S, Senik T, 2018. Evaluating the impact of social support services on tuberculosis treatment default in Ukraine. PLoS One 13: e0199513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Klein K, Bernachea MP, Irribarren S, Gibbons L, Chirico C, Rubinstein F, 2019. Evaluation of a social protection policy on tuberculosis treatment outcomes: a prospective cohort study. PLoS Med 16: e1002788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Malacarne J, Kolte IV, Freitas LP, Orellana JDY, de Souza MLP, Souza-Santos R, Basta PC, 2018. Factors associated with TB in an indigenous population in Brazil: the effect of a cash transfer program. Rev Inst Med Trop São Paulo 60: e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bhavesh M, Bhautik M, Paresh D, 2020. Financial incentive—does this have impact on outcome of Tuberculosis? Indian J Community Health 32: 418–422. [Google Scholar]
- 30. Mansour O, Masini EO, Kim BJ, Kamene M, Githiomi MM, Hanson CL, 2018. Impact of a national nutritional support programme on loss to follow-up after tuberculosis diagnosis in Kenya. Int J Tuberc Lung Dis 22: 649–654. [DOI] [PubMed] [Google Scholar]
- 31. Bhatt R, Chopra K, Vashisht R, 2019. Impact of integrated psycho-socio-economic support on treatment outcome in drug resistant tuberculosis—a retrospective cohort study. Indian J Tuberc 66: 105–110. [DOI] [PubMed] [Google Scholar]
- 32. Samuel B. et al. , 2016. Relationship between nutritional support and tuberculosis treatment outcomes in West Bengal, India. J Tuberc Res 4: 213–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Durovni B, Saraceni V, Puppin MS, Tassinari W, Cruz OG, Cavalcante S, Coeli CM, Trajman A, 2018. The impact of the Brazilian Family Health Strategy and the conditional cash transfer on tuberculosis treatment outcomes in Rio de Janeiro: an individual-level analysis of secondary data. J Public Health (Oxf) 40: e359–e366. [DOI] [PubMed] [Google Scholar]
- 34. Rudgard WE, das Chagas NS, Gayoso R, Barreto ML, Boccia D, Smeeth L, Rodrigues LC, Lönnroth K, Williamson E, Maciel ELN, 2018. Uptake of governmental social protection and financial hardship during drug-resistant tuberculosis treatment in Rio de Janeiro, Brazil. Eur Respir J 51: 1800274. [DOI] [PubMed] [Google Scholar]
- 35. Chirico C, Iannizzotto A, Telles H, Valiante J, Rojas S, Etcheverria M, 2018. El amparo económico para mejorar el tratamiento de la tuberculosis. Buenos Aires, Argentina: Sociedad Iberoamericana de Información Científica (SIIC), 219–227. Available at: https://www.siicsalud.com/des/expertoimpreso.php/159135. Accessed January 29, 2023. [Google Scholar]
- 36. Zhao Q, Wang L, Tao T, Xu B, 2013. Impacts of the “transport subsidy initiative on poor TB patients” in rural China: a patient-cohort based longitudinal study in rural China. PLoS One 8: e82503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Soares EC, Vollmer W, Cavalcante S, Pacheco A, Saraceni V, Silva J, Neves G, Golub J, Efron A, Durovni B, 2013. Tuberculosis control in a socially vulnerable area: a community intervention beyond DOT in a Brazilian favela. Int J Tuberc Lung Dis 17: 1581–1586. [DOI] [PubMed] [Google Scholar]
- 38. Kaliakbarova G, Pak S, Zhaksylykova N, Raimova G, Temerbekova B, Hof S, 2013. Psychosocial support improves treatment adherence among MDR-TB patients: experience from East Kazakhstan. Open Infect Dis J 7: 60–64. [Google Scholar]
- 39. Rogers JH, Jabateh L, Beste J, Wagenaar BH, McBain R, Palazuelos D, Wickett E, Oswald C, Napier HG, Toomey-Garbo J, 2018. Impact of community-based adherence support on treatment outcomes for tuberculosis, leprosy and HIV/AIDS-infected individuals in post-Ebola Liberia. Glob Health Action 11: 1522150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. De Souza R, Nery JS, Rasella D, Guimarães Pereira R, Barreto ML, Rodrigues L, Pereira SM, 2018. Family health and conditional cash transfer in Brazil and its effect on tuberculosis mortality. Int J Tuberc Lung Dis 22: 1300–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. World Food Programme , 2014. Responding to Humanitarian Needs and Strengthening Resilience to Food Insecurity (Zimbabwe, Protracted Relief and Recovery Operation 200453; September 2012–March 2014). Available at: https://www.wfp.org/operations/200453-responding-humanitarian-needs-and-strengthening-resilience-food-insecurity. Accessed January 29, 2023.
- 42. Reis-Santos B, Shete P, Bertolde A, Sales CM, Sanchez MN, Arakaki-Sanchez D, Andrade KB, Gomes MGM, Boccia D, Lienhardt C, 2019. Tuberculosis in Brazil and cash transfer programs: a longitudinal database study of the effect of cash transfer on cure rates. PLoS One 14: e0212617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Contreras CC, Millones AK, Santa Cruz J, Aguilar M, Clendenes M, Toranzo M, Llaro K, Lecca L, Becerra MC, Yuen CM, 2017. Addressing tuberculosis patients’ medical and socio‐economic needs: a comprehensive programmatic approach. Trop Med Int Health 22: 505–511. [DOI] [PubMed] [Google Scholar]
- 44. Ngamvithayapong-Yanai J, Luangjina S, Nedsuwan S, Kantipong P, Wongyai J, Ishikawa N, 2013. Engaging women volunteers of high socioeconomic status in supporting socioeconomically disadvantaged tuberculosis patients in Chiang Rai, Thailand. Western Pac Surveill Response J 4: 34–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Diaw MM, Ndiaye M, Riccardi N, Ungaro R, Alagna R, Cirillo DM, Codecasa L, Viscoli C, Nicolini LA, Besozzi G, 2018. Implementing TB control in a rural, resource-limited setting: the stop-TB Italia project in Senegal. Multidiscip Respir Med 13: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wingfield T, Tovar MA, Huff D, Boccia D, Saunders MJ, Datta S, Montoya R, Ramos E, Lewis JJ, Gilman RH, 2016. Beyond pills and tests: addressing the social determinants of tuberculosis. Clin Med (Northfield Ill) 16: s79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lutge E, Lewin S, Volmink J, Friedman I, Lombard C, 2013. Economic support to improve tuberculosis treatment outcomes in South Africa: a pragmatic cluster-randomized controlled trial. Trials 14: 154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Carter DJ, Daniel R, Torrens AW, Sanchez MN, Maciel ELN, Bartholomay P, Barreira DC, Rasella D, Barreto ML, Rodrigues LC, 2019. The impact of a cash transfer programme on tuberculosis treatment success rate: a quasi-experimental study in Brazil. BMJ Glob Health 4: e001029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wei X, Zou G, Yin J, Walley J, Yang H, Kliner M, Mei J, 2012. Providing financial incentives to rural-to-urban tuberculosis migrants in Shanghai: an intervention study. Infect Dis Poverty 1: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wingfield T, Tovar MA, Huff D, Boccia D, Montoya R, Ramos E, Lewis JJ, Gilman RH, Evans CA, 2016. The economic effects of supporting tuberculosis-affected households in Peru. Eur Respir J 48: 1396–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wingfield T. et al. , 2017. A randomized controlled study of socioeconomic support to enhance tuberculosis prevention and treatment, Peru. Bull World Health Organ 95: 270–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ukwaja KN, Alobu I, Mustapha G, Onazi O, Oshi DC, 2017. “Sustaining the DOTS”: stakeholders’ experience of a social protection intervention for TB in Nigeria. Int Health 9: 112–117. [DOI] [PubMed] [Google Scholar]
- 53. Orlandi GM, Pereira ÉG, Biagolini REM, de Siqueira França FO, Bertolozzi MR, 2019. Social incentives for adherence to tuberculosis treatment. Rev Bras Enferm 72: 1182–1188. [DOI] [PubMed] [Google Scholar]
- 54. George LS, Rakesh PS, Sunilkumar M, Vijayakumar K, Kunoor A, Kumar VA, 2021. TB patient support systems in Kerala: a qualitative analysis. Indian J Tuberc 68: 9–15. [DOI] [PubMed] [Google Scholar]
- 55. Patel BH. et al. , 2019. Cash transfer scheme for people with tuberculosis treated by the National TB Programme in Western India: a mixed methods study. BMJ Open 9: e033158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Yin J, Wang X, Zhou L, Wei X, 2018. The relationship between social support, treatment interruption and treatment outcome in patients with multidrug-resistant tuberculosis in China: a mixed-methods study. Trop Med Int Health 23: 668–677. [DOI] [PubMed] [Google Scholar]
- 57. Li R, Ruan Y, Sun Q, Wang X, Chen M, Zhang H, Zhao Y, Zhao J, Chen C, Xu C, 2015. Effect of a comprehensive programme to provide universal access to care for sputum-smear-positive multidrug-resistant tuberculosis in China: a before-and-after study. Lancet Glob Health 3: e217–e228. [DOI] [PubMed] [Google Scholar]
- 58. Xiang L, Pan Y, Hou S, Zhang H, Sato KD, Li Q, Wang J, Tang S, 2016. The impact of the new cooperative medical scheme on financial burden of tuberculosis patients: evidence from six counties in China. Infect Dis Poverty 5: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sripad A, Castedo J, Danford N, Zaha R, Freile C, 2014. Effects of Ecuador’s national monetary incentive program on adherence to treatment for drug-resistant tuberculosis. Int J Tuberc Lung Dis 18: 44–48. [DOI] [PubMed] [Google Scholar]
- 60. Loveleen D, Anh QN, Tsuruga I, Ruck M, 2020. An Assessment of the Social Protection Needs and Gaps for Workers in Informal Employment in Myanmar. Geneva, Switzerland: International Labour Organization. [Google Scholar]
- 61. Mahadevia D, 2012. Decent Work in Ahmedabad: An Integrated Approach. Geneva, Switzerland: International Labour Organization. [Google Scholar]
- 62. World Bank , 2015. The State of Social Safety Nets 2015. Washington, DC: World Bank. Available at: https://openknowledge.worldbank.org/handle/10986/22101. Accessed January 29, 2023.
- 63. Spray AL, 2016. Leveraging Social Protection Programs for Improved Nutrition: Compendium of Case Studies Prepared for the Global Forum on Nutrition-Sensitive Social Protection Programs, 2015. Washington, DC: World Bank. [Google Scholar]
- 64. World Health Organization , 2020. National Strategic Plan for Ending TB 2020–2024, Timor-Leste. Geneva, Switzerland: WHO. [Google Scholar]
- 65. Nurova M, 2016. Support for Tuberculosis Patients and Their Families, Standard Project Report 2016. Rome, Italy: World Food Programme. [Google Scholar]
- 66. World Food Programme , 2012. Regional Bureau for Southern Africa. Available at: https://documents.wfp.org/stellent/groups/public/documents/op_reports/wfp252301.pdf. Accessed January 29, 2023. [Google Scholar]
- 67. World Food Programme , 2016. Country Programme—Congo (2015–2018). Standard Project Report 2016. Rome, Italy: WFP. [Google Scholar]
- 68. Foster N, 2019. Structure and Agency in the Economics of Public Policy for TB Control. Faculty of Health Sciences, Department of Public Health and Family Medicine, University of Cape Town, South Africa. Available at: http://hdl.handle.net/11427/31228. Accessed January 29, 2023.
- 69. Balakrishnan S, Manikantan J, Sreenivas A, Jayasankar S, Sunilkumar M, Rakesh PS, Karthickeyan DS, Mohandas CR, 2015. Social inclusion: an effort to end loss-to-treatment follow-up in tuberculosis. Indian J Tuberc 62: 230–234. [DOI] [PubMed] [Google Scholar]
- 70. Boccia D, Hargreaves J, Lönnroth K, Jaramillo E, Weiss J, Uplekar M, Porter JDH, Evans CA, 2011. Cash transfer and microfinance interventions for tuberculosis control: review of the impact evidence and policy implications. Int J Tuberc Lung Dis 15 ( Suppl 2 ): 37–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Bustos M, Luu K, Lau LL, Dodd W, 2022. Addressing tuberculosis through complex community-based socioeconomic interventions in low- and middle-income countries: a systematic realist review. Glob Public Health 17: 1924–1944. [DOI] [PubMed] [Google Scholar]
- 72. Wingfield T, Boccia D, Tovar MA, Huff D, Montoya R, Lewis JJ, Gilman RH, Evans CA, 2015. Designing and implementing a socioeconomic intervention to enhance TB control: operational evidence from the CRESIPT project in Peru. BMC Public Health 15: 810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Boccia D, Pedrazzoli D, Wingfield T, Jaramillo E, Lönnroth K, Lewis J, Hargreaves J, Evans CA, 2016. Towards cash transfer interventions for tuberculosis prevention, care and control: key operational challenges and research priorities. BMC Infect Dis 16: 307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. World Food Programme , 2012. Supporting Transition by Reducing Food Insecurity and Undernutrition among the Most Vulnerable. Available at: https://docs.wfp.org/api/documents/WFP-0000069855/download/?_ga=2.63000367.1003006815.1675348340-936112668.1675108384. Accessed January 29, 2023.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.