This cohort study investigates the association of long-term exposure to multiple air pollutants and incident depression and anxiety.
Key Points
Question
What are the associations of long-term exposure to low levels of multiple air pollutants with incident depression and anxiety?
Findings
In this cohort study of 389 185 participants, estimated joint exposure to multiple air pollutants was associated with increased risk of depression and anxiety, and the exposure-response curves were nonlinear.
Meaning
Results of this study suggest an association between long-term exposure to low levels of multiple air pollutants and depression and anxiety.
Abstract
Importance
Air pollution is increasingly recognized as an important environmental risk factor for mental health. However, epidemiologic evidence on long-term exposure to low levels of air pollutants with incident depression and anxiety is still very limited.
Objectives
To investigate the association of long-term joint exposure to multiple air pollutants with incident depression and anxiety.
Design, Setting, and Participants
This prospective, population-based cohort study used data from the UK Biobank. The participants were recruited between March 13, 2006, and October 1, 2010, and included individuals who had never been diagnosed with depression or anxiety at baseline and had full information on exposure and covariates. Data were analyzed from May 1 to October 10, 2022.
Exposures
Annual mean air pollution concentrations of particulate matter (PM) with aerodynamic diameter of 2.5 μm or less (PM2.5) and PM with aerodynamic diameter between 2.5 μm and 10 μm (PM2.5-10). Nitrogen dioxide (NO2) and nitric oxide (NO) were estimated for each participant’s residential address using the land use regression model, and joint exposure to air pollution reflected by air pollution score was calculated by principal components analysis.
Main Outcomes and Measures
Incidence of diagnosed depression (F32-F33) and anxiety (F40-F48) were ascertained with International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes.
Results
During a median (IQR) follow-up of 10.9 (10.1-11.6) years, among 389 185 participants (mean [SD] age, 56.7 [8.1] years, 205 855 female individuals [52.9%]), a total of 13 131 and 15 835 patients were diagnosed with depression and anxiety, respectively. The median (IQR) concentration of pollutants was as follows: PM2.5, 9.9 (9.3-10.6) μg/m3; PM2.5-10, 6.1 (5.8-6.6) μg/m3; NO2, 26.0 (21.3-31.1) μg/m3; and NO, 15.9 (11.6-20.6) μg/m3. Long-term estimated exposure to multiple air pollutants was associated with increased risk of depression and anxiety, and the exposure-response curves were nonlinear, with steeper slopes at lower concentrations and plateauing trends at higher exposure. The hazard ratios (HRs) and 95% CIs for depression and anxiety were 1.16 (95% CI, 1.09-1.23; P < .001) and 1.11 (95% CI, 1.05-1.17; P < .001) in the highest quartile compared with the lowest quartile of air pollution score, respectively. Similar trends were shown for PM2.5, NO2, and NO. Subgroup analysis showed the association between PM2.5 and anxiety tended to be higher in male individuals than in female individuals (quartile 4: male individuals, 1.18; 95% CI, 1.08-1.29; female individuals, 1.07; 95% CI, 1.00-1.14; P = .009).
Conclusions and Relevance
Study results suggest that estimates of long-term exposure to multiple air pollutants was associated with increased risk of depression and anxiety. The nonlinear associations may have important implications for policy making in air pollution control. Reductions in joint exposure to multiple air pollutants may alleviate the disease burden of depression and anxiety.
Introduction
Mental health disorders are a leading and growing cause of disability, accounting for 125 million disability-adjusted life-years (DALYs) worldwide, the seventh leading cause of DALYs in 2019.1 Depressive and anxiety disorders are of particular concern as they are the most prevalent mental health disorders, ranking first and second leading causes of DALYs among mental health disorders in 2019.2 Depressive and anxiety disorders commonly coexist,3 and evaluating them together would be important to identify early symptoms and promote primary prevention for mental health. Given that the disease burden of depressive and anxiety disorders is surging,2 identifying the modifiable environmental risk factors of the anxiety and depression and developing preventive interventions constitute an urgent public health priority.
Ambient air pollution is a major worldwide health issue.4 Growing epidemiologic evidence shows a link between air pollution and mental health disorders.5,6,7 Several studies indicated that short-term exposure to air pollution was associated with increased risk of hospitalization or outpatient visits of depression8,9,10 as well as anxiety.11,12,13 Evidence of long-term effects has emerged with conflicting findings,14,15,16,17,18,19,20,21 and only 3 studies have explored the long-term effects of air pollution on incidence of depression in the general population.19,20,21 Evidence on the long-term effects on incidence of anxiety are lacking. Importantly, the only available studies on risk of incident depression in the general population were conducted in regions with high air pollution concentrations, which exceeded annual values in UK air quality standards.19,20,21 The question, therefore, remains whether long-term exposure to air pollution at low levels would cause increased incidence risk of depression and anxiety disorders.
Additionally, previous studies assessed the associations of depression and anxiety with air pollution focusing on individual air pollutants separately.14,15,16,17,18,19,20,21 However, ambient air pollution consists of both particulate matter and gaseous pollutants, and assessing the health effects of multiple air pollutants as a whole has been increasingly recognized.22,23 Nevertheless, no one study has, as yet and to our knowledge, investigated long-term joint exposure to various air pollutants with the incidence risk of depression and anxiety.
Taking advantage of the large sample size of over nearly one-half million adults and the detailed information about individual characteristics, lifestyles, area-level covariates, and individual air pollution data in the UK Biobank, we prospectively assessed the associations of long-term exposure to air pollution with the risk of incident depression and anxiety. An air pollution score, which included the main air pollutants in the UK, was generated to assess the joint exposure to multiple air pollutants.
Methods
Study Design and Population
The UK Biobank is a large, population-based prospective study, with the study protocol described in detail previously.24 Information on sociodemographic characteristics, lifestyles, and health data was collected. The UK Biobank has approval from the North West Multicentre Research Ethics Committee, and participants have provided written consent. Because of the publicly available and deidentified data, ethical approval was waived from Peking University institutional review board. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
Participants diagnosed with anxiety or depression at baseline and during follow-up were confirmed according to the first occurrence of health outcomes in the UK Biobank, which is identified through linkage to self-report (based on physician diagnosis and subsequently checked with nurses), inpatient hospital data, primary care, and death records and defined by 3-character International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes. Race and ethnicity data are commonly used to reflect the basic demographic characteristics of the study participants, and the related data on race and ethnicity were collected from the UK Biobank dataset. The specific race and ethnic groups included in this study were Asian (Indian, Pakistani, Bangladeshi, or any other Asian background except Chinese), Black, Chinese, multiracial, White, and other race or ethnicity. Race and ethnicity data were not a requirement of the funding body.
Among the participants recruited between March 13, 2006, and October 1, 2010, participants diagnosed with depression or anxiety at baseline were excluded. In addition, we excluded participants with missing information of air pollution exposure or covariates in the main analysis.
Air Pollution Assessment
Air pollution estimates for particulate matter (PM) with aerodynamic diameter of 2.5 μm or less (PM2.5), PM with aerodynamic diameter between 2.5 μm and 10 μm (PM2.5-10), nitrogen dioxide (NO2), and nitrogen oxides (NOx) were modeled for each participant’s residential address using land use regression model, which developed as part of the European Study of Cohorts for Air Pollution Effects.25 Centrally and locally available geographic information system–derived variables such as traffic intensity, population, and land use were evaluated to model spatial variation of mean annual air pollution concentrations at baseline with a land use regression model. The median model-explained variance (R2) was 71% for PM2.5, 68% for PM2.5-10, 82% for NO2, and 78% for NOx.26,27 The NO concentrations were calculated by subtracting NO2 from NOx according to the previous study.28 To assess the joint exposure to multiple air pollutants, we calculated an air pollution score with principal components analysis considering high correlations among air pollutants.29
Outcome Identification
Follow-up occurrences of depression and anxiety were ascertained by the ICD-10 codes F32-F33 and F40-F48, respectively.30 The details of ICD-10 codes were as follows: F32, depressive episode; F33, recurrent depressive disorder; F40, phobic anxiety disorders; F41, other anxiety disorders; F42, obsessive-compulsive disorder; F43, reaction to severe stress and adjustment disorders; F44, dissociative (conversion) disorders; F45, somatoform disorders; and F48, other neurotic disorders.
Covariates
A directed acyclic graph was drawn to discern which covariates are confounders (eFigure 1 in Supplement 1).31,32 Sociodemographic factors (age, sex, race and ethnicity, length of time at residence, and assessment center), socioeconomic status (Townsend deprivation index, education level, and employment status), and local environmental exposure (24-hour weighted average noise, and proximity to major roads) were collected at baseline. The detailed information for covariates is described in eMethods in Supplement 1.
Statistical Analysis
Characteristics of the study population were presented as mean with SD or median with IQR for continuous variables and as number (percentage) for categorical variables.
Follow-up time was calculated from baseline until the date of diagnosis of depression or anxiety, loss to follow-up, death, or February 29, 2020, whichever came first. Cox proportional hazard models were conducted to estimate the hazard ratios (HRs) and 95% CIs for the associations of individual air pollutants and air pollution score in quartiles with incidence of depression and anxiety. Model 1 was the crude model that only adjusted for age, sex, and assessment center. Model 2 was the main model, which further adjusted for race and ethnicity, length of time at residence, Townsend deprivation index, education level, employment status, 24-hour weighted average noise, and proximity to major roads. The assumption of proportional hazards was tested by Schoenfeld residuals, and no violation of this assumption was observed. Addictive hazards model was used to estimate interactions among air pollutants on the addictive scale.33 Based on the Akaike information criterion,34 we used restricted cubic spline functions with 3 knots to depict the exposure-response curves between air pollution and risk of depression and anxiety.
We hypothesized that the association of air pollution with depression or anxiety may be modified by age, sex, length of time at residence, and education level. We performed a subgroup analysis with HRs and 95% CIs estimated from the strata. Group comparisons were assessed by P values for interaction term. A Bonferroni-corrected 2-sided P value of .004 was used as the significance threshold for the 12 interaction analyses due to multiple comparisons.
Furthermore, several sensitivity analyses were conducted to verify the robustness of results. First, multiple imputation using chained equations by exposures and covariates was conducted considering the protentional bias of missing data. Second, we further adjusted for household income to control for potential confounders of household-level socioeconomic status. Third, green space percentage in 1000-m buffer was further adjusted as a possible local environment exposure confounder. Fourth, we used income score and housing score to replace Townsend deprivation index, which might not be weighted appropriately.35 Fifth, considering that the coexistence of depression and anxiety for the same person in follow-up might overestimate the effect, we ignored the second depression outcome for the same person if follow-up anxiety was diagnosed first, and vice versa. Sixth, to minimize the influence of reverse causation, we excluded depression and anxiety cases that occurred in the first 2 years of follow-up. Additionally, we compared the results of using baseline exposure estimates with the use of time-varying PM2.5 from global estimates and long-term trends.36 All statistical analyses were performed with R software, version 3.6.3 (R Project for Statistical Computing). Data were analyzed from May 1 to October 10, 2022.
Results
A total of 389 185 participants (mean [SD] age, 56.7 [8.1] years, 205 855 female individuals [52.9%]; 183 330 male individuals [47.1%]) were included in the final analysis among whom 13 131 and 15 835 incident cases of depression and anxiety were identified, respectively, during a median (IQR) follow-up of 10.9 (10.1-11.6) years (eFigure 2 in Supplement 1). Participants from the following race and ethnicity groups were included: 7814 Asian (2.0%), 6788 Black (1.7%), 1255 Chinese (0.3%), 2306 multiracial (0.6%), 367 524 White (94.4%), and 3498 other (0.9%). The median (IQR) concentration of pollutants was as follows: PM2.5, 9.9 (9.3-10.6) μg/m3; PM2.5-10, 6.1 (5.8-6.6) μg/m3; NO2, 26.0 (21.3-31.1) μg/m3; and NO, 15.9 (11.6-20.6) μg/m3 (Table 1; detailed data in eTable 1 in Supplement 1), which were below the annual values for PM2.5 and NO2 in UK air quality standards (eTable 2 in Supplement 1). The Spearman correlations between air pollutants are shown (eTable 3 in Supplement 1). The censoring rates for participants (eTable 4 in Supplement 1) and cumulative survival curves for air pollutants and incident depression and anxiety are also provided (eFigure 3 in Supplement 1).
Table 1. Characteristics of the Study Population and Air Pollution Exposures Stratified by Depression and Anxiety.
| Characteristic | No. (%) | ||
|---|---|---|---|
| Participants (N = 389 185) | Depression cases (n = 13 131) | Anxiety cases (n = 15 835) | |
| Person-years | 4 124 737a/4 107 105b | 80 438 | 92 359 |
| Age, mean (SD), y | 56.7 (8.1) | 56.2 (8.4) | 56.4 (8.4) |
| <65 | 312 639 (80.3) | 10 516 (80.1) | 12 563 (79.3) |
| ≥65 | 76 546 (19.7) | 2615 (19.9) | 3272 (20.7) |
| Sex | |||
| Female | 205 855 (52.9) | 8031 (61.2) | 10 342 (65.3) |
| Male | 183 330 (47.1) | 5100 (38.8) | 5493 (34.7) |
| Race and ethnicity | |||
| Asian | 7814 (2.0) | 211 (1.6) | 294 (1.9) |
| Black | 6788 (1.7) | 196 (1.5) | 272 (1.7) |
| Chinese | 1255 (0.3) | 17 (0.1) | 26 (0.2) |
| Multiracial | 2306 (0.6) | 103 (0.8) | 116 (0.7) |
| White | 367 524 (94.4) | 12 481 (95.0) | 14 990 (94.7) |
| Other | 3498 (0.9) | 123 (0.9) | 137 (0.9) |
| Length of time at residence, y | |||
| <10 | 122 209 (31.4) | 4841 (36.9) | 5417 (34.2) |
| ≥10 | 266 976 (68.6) | 8290 (63.1) | 10 418 (65.8) |
| Townsend deprivation index, mean (SD) | –1.4 (3.0) | –0.7 (3.3) | –1.0 (3.2) |
| Education | |||
| University or college degree | 126 561 (32.5) | 3232 (24.6) | 4175 (26.4) |
| Otherc | 262 624 (67.5) | 9899 (75.4) | 11 660 (73.6) |
| Employment | |||
| Active | 228 728 (58.8) | 6726 (51.2) | 8566 (54.1) |
| Inactive | 160 457 (41.2) | 6405 (48.8) | 7269 (45.9) |
| 24-h Weighted average noise, median (IQR), dB | 54.9 (53.4-57.0) | 55.0 (53.5-57.1) | 54.9 (53.4-57.0) |
| Proximity to major roads, median (IQR), 1/km | 2.6 (1.3-6.0) | 2.8 (1.4-6.2) | 2.7 (1.4-6.1) |
| PM2.5, median (IQR), μg/m3 | 9.9 (9.3-10.6) | 10.1 (9.4-10.7) | 10.0 (9.4-10.6) |
| PM2.5-10, median (IQR), μg/m3 | 6.1 (5.8-6.6) | 6.1 (5.8-6.7) | 6.1 (5.8-6.6) |
| NO2, median (IQR), μg/m3 | 26.0 (21.3-31.1) | 26.9 (22.2-31.9) | 26.5 (21.8-31.3) |
| NO, median (IQR), μg/m3 | 15.9 (11.6-20.6) | 16.8 (12.3-21.5) | 16.5 (12.2-21.0) |
Abbreviations: NO, nitric oxide; NO2, nitrogen dioxide; PM2.5, particulate matter with aerodynamic diameter of 2.5 μm or less; PM2.5-10, particulate matter with aerodynamic diameter between 2.5 and 10 μm.
Depression.
Anxiety.
Other education includes advanced levels/advanced subsidiary levels or equivalent; general certificate of education ordinary levels/general certificate of secondary education or equivalent; certificate of secondary education or equivalent; national vocational qualification or higher national diploma or higher national certificate or equivalent; other professional qualifications, eg, nursing, teaching; and none of the above.
The exposure-response curves between air pollution score and incidence of depression and anxiety were nonlinear, with steeper slopes at lower levels and plateauing trends at higher exposure. Similar trends were shown for PM2.5, NO2, and NO (Figure 1 and Figure 2).
Figure 1. Exposure-Response Curves Between Air Pollution and Incidence of Depression.
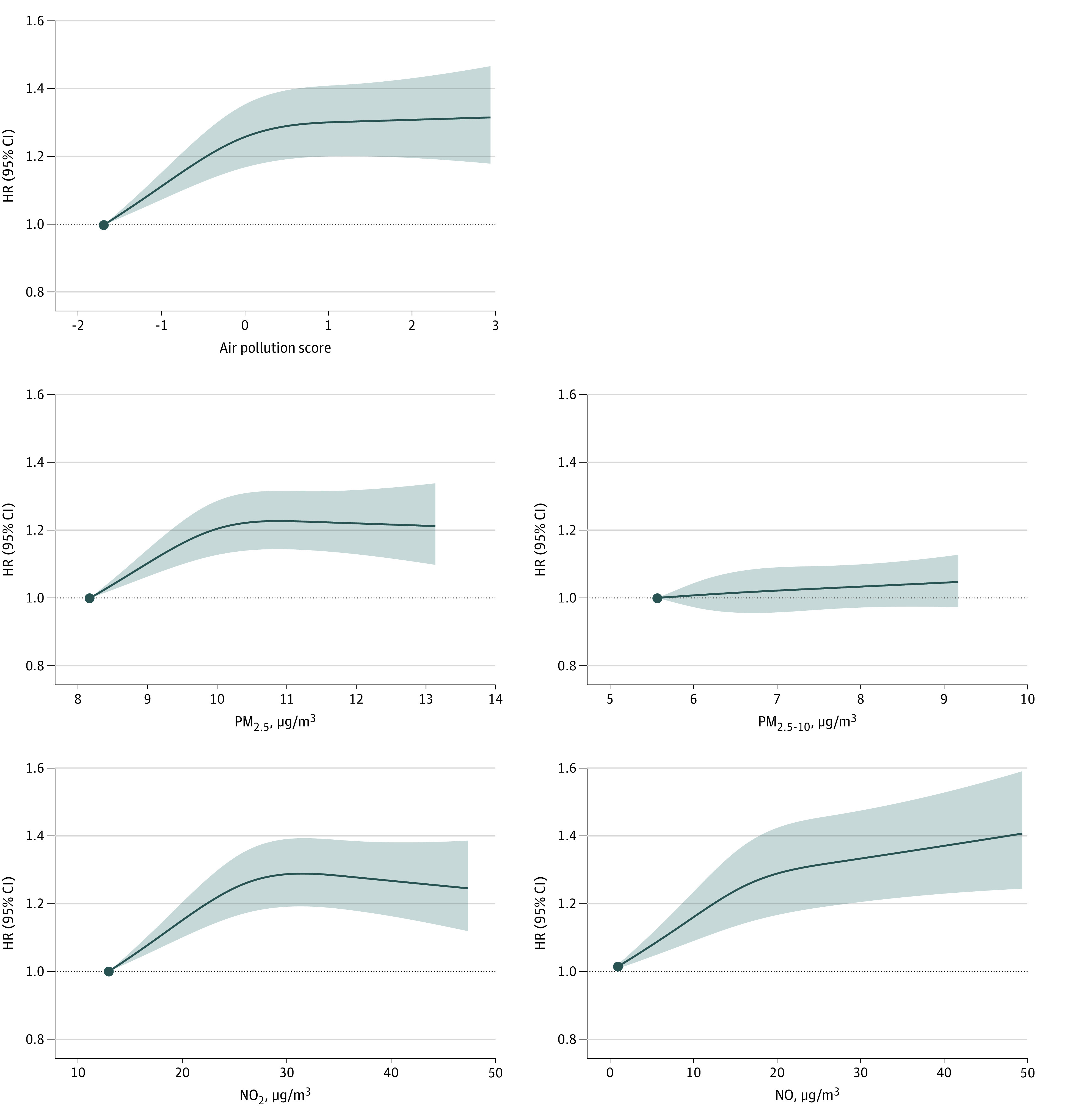
The models were adjusted for age, sex, assessment center, ethnicity, length of time at residence, Townsend deprivation index, education level, employment status, 24-hour weighted average noise, and proximity to major roads (main model). Air pollution levels range from the 0 to 99th percentiles. HR indicates hazard ratio; NO, nitric oxide; NO2, nitrogen dioxide; PM2.5, particulate matter with aerodynamic diameter of 2.5 μm or less; PM2.5-10, particulate matter with aerodynamic diameter between 2.5 and 10 μm.
Figure 2. Exposure-Response Curves Between Air Pollution and Incidence of Anxiety.
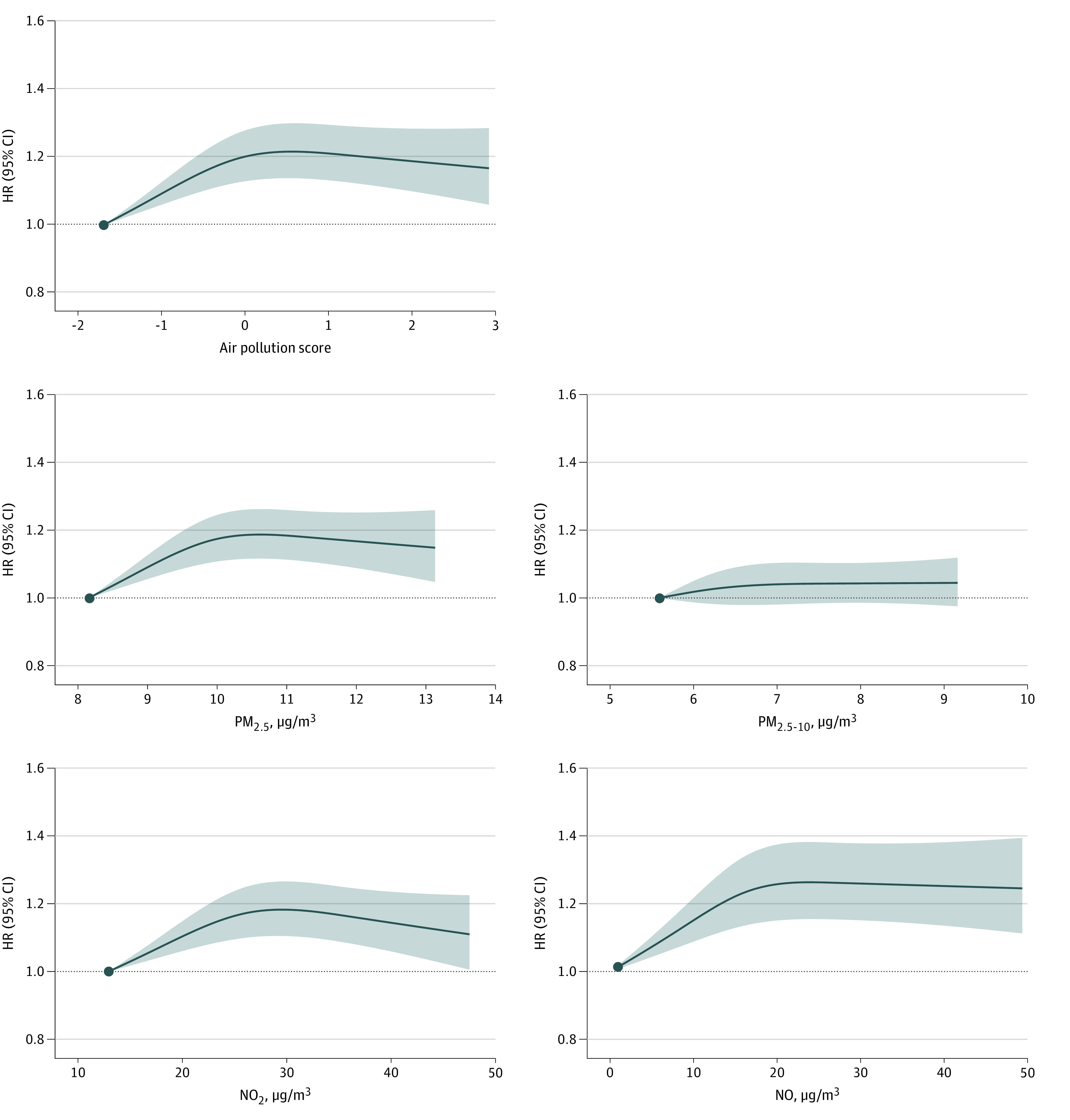
The models were adjusted for age, sex, assessment center, ethnicity, length of time at residence, Townsend deprivation index, education level, employment status, 24-hour weighted average noise, and proximity to major roads (main model). Air pollution levels range from the 0 to 99th percentiles. HR indicates hazard ratio; NO, nitric oxide; NO2, nitrogen dioxide; PM2.5, particulate matter with aerodynamic diameter of 2.5 μm or less; PM2.5-10, particulate matter with aerodynamic diameter between 2.5 and 10 μm.
For PM2.5, the HRs of depression were 1.09 (95% CI, 1.03-1.14; P = .002), 1.14 (95% CI, 1.08-1.20; P < .001), and 1.15 (95% CI, 1.08-1.21; P < .001) in quartile 2 to 4 compared with the lowest quartile in the main models. For NO2, the HRs were 1.11 (95% CI, 1.06-1.17; P < .001), 1.15 (95% CI, 1.09-1.22; P < .001), and 1.14 (95% CI, 1.07-1.21; P < .001) in quartile 2 to 4 compared with the lowest quartile. For NO, the HRs were 1.07 (95% CI, 1.02-1.13; P = .006), 1.11 (95% CI, 1.06-1.17; P < .001), and 1.12 (95% CI, 1.06-1.18; P < .001) in quartile 2 to 4 compared with the lowest quartile. However, nonsignificant elevated risk of depression associated with PM2.5-10 was observed. Similarly, increased associated risks of anxiety with PM2.5, NO2, and NO were also observed, although there was no association between PM2.5-10 and anxiety (Figure 3; detailed data in eTable 5 in Supplement 1). We did not find additive effects of joint exposure (eTable 6 in Supplement 1).
Figure 3. Association of Individual Air Pollutants With Incidence of Depression and Anxiety.
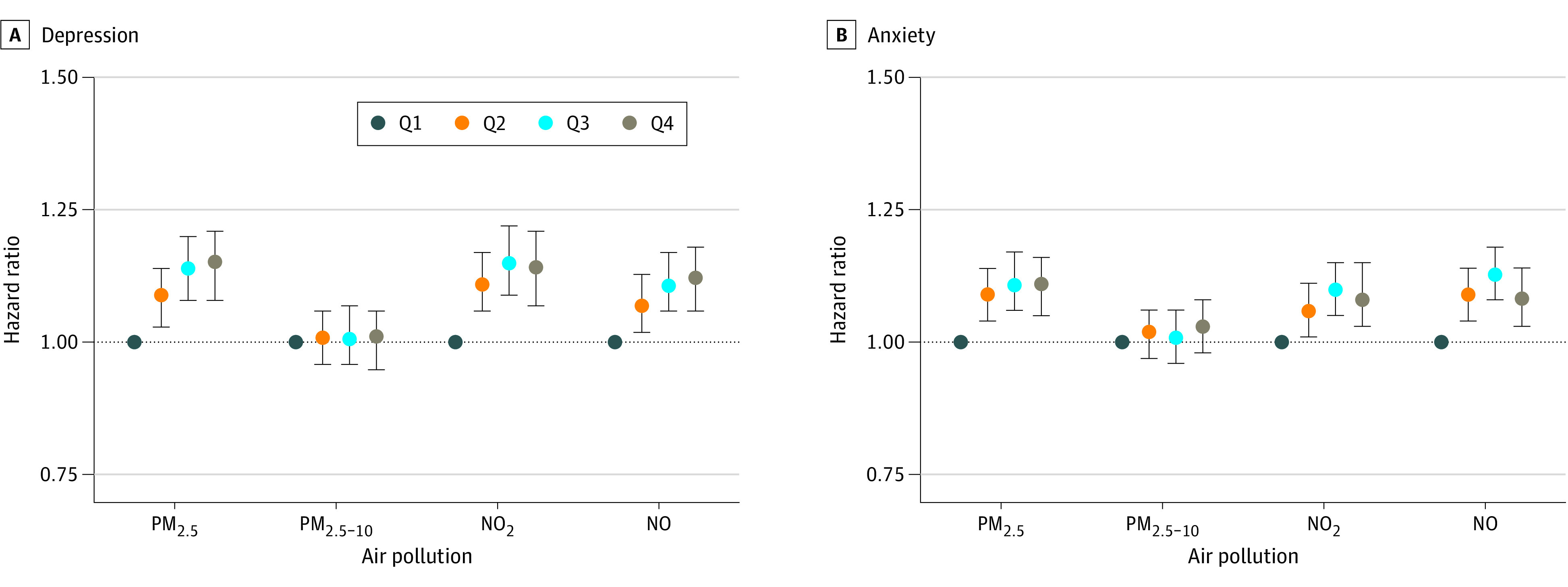
Association of air pollutants with incidence of depression (A) and anxiety (B). The models were adjusted for age, sex, assessment center, ethnicity, length of time at residence, Townsend deprivation index, education level, employment status, 24-hour weighted average noise, and proximity to major roads (main model). Pollutant levels for each quartile (Q) are as follows: (1) particulate matter with aerodynamic diameter of 2.5 μm or less (PM2.5): Q1, less than 9.3 μg/m3; Q2, 9.3 to 9.9 μg/m3; Q3, 9.9 to 10.6 μg/m3; and Q4, greater than or equal to10.6 μg/m3; (2) particulate matter with aerodynamic diameter between 2.5 and 10 μm (PM2.5-10): Q1, less than 5.8 μg/m3; Q2, 5.8 to 6.1 μg/m3; Q3, 6.1 to 6.6 μg/m3; and Q4, greater than or equal to 6.6 μg/m3; (3) nitrogen dioxide (NO2): Q1, less than 21.3 μg/m3; Q2, 21.3 to 26.0 μg/m3; Q3, 26.0 to 31.1 μg/m3; and Q4, greater than or equal to 31.1 μg/m3; and (4) nitric oxide (NO): Q1, less than 11.6 μg/m3; Q2, 11.6 to 15.9 μg/m3; Q3, 15.9 to 20.6 μg/m3; and Q4, greater than or equal to 20.6 μg/m3.
Considering the significant associations between PM2.5, NO2, NO, and depression and anxiety, we selected those air pollutants to construct an air pollution score. The first principal component, which contributed 85.5% of the total variance, was chosen to calculate the air pollution score. Compared with the lowest quartile of the air pollution score, the HRs of depression were 1.08 (95% CI, 1.02-1.14; P = .004), 1.17 (95% CI, 1.11-1.24; P < .001), and 1.16 (95% CI, 1.09-1.23; P < .001) in quartile 2 to 4. Similarly, the HRs of anxiety were 1.09 (95% CI, 1.04-1.14; P < .001), 1.14 (95% CI, 1.08-1.19; P < .001), and 1.11 (95% CI, 1.05-1.17; P < .001) in quartile 2 to 4 compared with the lowest quartile of air pollution score (Table 2).
Table 2. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollution Score.
| Quartile | Model 1a | Model 2b | ||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Depression, 0.32 (95% CI, 0.31-0.32) cases per 100 person-yearsc | ||||
| Quartiled | ||||
| 1 | 1 [Reference] | NA | 1 [Reference] | NA |
| 2 | 1.13 (1.08-1.19) | <.001 | 1.08 (1.02-1.14) | .004 |
| 3 | 1.31 (1.24-1.37) | <.001 | 1.17 (1.11-1.24) | <.001 |
| 4 | 1.44 (1.37-1.52) | <.001 | 1.16 (1.09-1.23) | <.001 |
| Anxiety, 0.39 (95% CI, 0.38-0.40) cases per 100 person-yearse | ||||
| Quartiled | ||||
| 1 | 1 [Reference] | NA | 1 [Reference] | NA |
| 2 | 1.12 (1.07-1.18) | <.001 | 1.09 (1.04-1.14) | <.001 |
| 3 | 1.21 (1.16-1.27) | <.001 | 1.14 (1.08-1.19) | <.001 |
| 4 | 1.26 (1.20-1.32) | <.001 | 1.11 (1.05-1.17) | <.001 |
Abbreviations: HR, hazard ratio; NA, not applicable.
Model 1 was adjusted for age, sex, and assessment center.
Model 2 was further adjusted for ethnicity, length of time at residence, Townsend deprivation index, education level, employment status, 24-hour weighted average noise, and proximity to major roads (main model).
Actual incidence rates of depression adjusted for age, sex, and assessment center.
Quartile 1, less than −0.6; quartile 2, −0.6 to −0.1; quartile 3, −0.1 to 0.5; quartile 4, greater than or equal to 0.5.
Actual incidence rates of anxiety adjusted for age, sex, and assessment center.
Subgroup analysis showed that the association between PM2.5 and risk of anxiety tended to be higher in male individuals compared with female individuals (quartile 4: male individuals, 1.18; 95% CI, 1.08-1.29; female individuals, 1.07; 95% CI, 1.00-1.14; P = .009) (eTable 7-10 in Supplement 1). The results were robust in sensitivity analysis (eTable 11-17 in Supplement 1).
Discussion
Results of this cohort study involving 389 185 participants during a median follow-up of 10.9 years showed for the first time, to our knowledge, that estimated long-term exposure to multiple air pollutants and joint air pollution exposure were associated with an increased risk of both incident depression and anxiety. These findings may fill the gap on the associations between air pollution exposure and mental health at air pollution concentrations below the annual values in UK air quality standards. Furthermore, the nonlinear exposure-response curves suggested that the risk of incident depression and anxiety tended to be steeper at lower air pollution levels and plateauing at higher exposures, which have important implications for policy making in air pollution control.
Recent time-series and case-crossover studies have documented associations between short-term air pollution exposure and hospitalization or outpatient visits for depression and anxiety,8,9,11,12,13 although few studies have investigated the long-term air pollution exposure and depression or anxiety with longitudinal study design, and the findings are inconsistent.14,15,16,17,18,19,20,21 For example, a longitudinal study from the National Social Life, Health and Aging Project in the US reported positive associations between air pollution and symptoms of depression and anxiety assessed by scales among 4008 individuals aged 57 to 85 years.16 The Nurses’ Health Study in the US also found that PM2.5 was associated with high symptoms of anxiety in the occupational population of 71 271 women.15 However, a study from Boston, Massachusetts, found no significant association between air pollution and depressive symptoms among 732 older adults.18 Furthermore, although most of these studies implied a positive association between air pollution and depression or anxiety, they focused on symptoms and prevalence identified by scales. To the best of our knowledge, only 3 studies have investigated the exposure to long-term air pollution with incidence of depression in the general population.19,20,21 However, all the studies were conducted in high-polluted areas with air pollution levels exceeding the annual values in UK air quality standards. Our findings indicate positive associations, which were consistent with 2 single-city studies in Korea and China, respectively,20,21 although a study conducted in Seoul and Suwon, South Korea, which identified incident depression by the Centre for Epidemiological Studies Depression scale (or a doctor’s diagnosis or medication use), found no association between PM2.5 and depression, partly due to a much shorter follow-up time of only 1 year.19 Compared with the limited evidence, our findings may fill in the gap in unknown evidence at low air pollution concentrations.
Furthermore, to our knowledge, this was the first prospective study to report significantly increased associated risk of both depression and anxiety with the air pollution score, which reflects joint exposure to multiple air pollutants. Nonlinear exposure-response curves were found, with steeper slope at lower air pollution levels and plateauing trends at higher exposure. Increased associated risk for both depression and anxiety was observed even at concentration levels below the annual values in UK air quality standards. Thus, the findings suggest that stricter standards or regulations for air pollution control are essential, and reductions in exposure to multiple air pollutants may alleviate the disease burden of depression and anxiety.
Air pollution exposure may affect the central nervous system by inflammatory and oxidative stress pathways through olfactory receptor neurons, the trigeminal nerve, or the systemic circulation.37 Particles such as PM2.5 may induce the release of proinflammatory mediators, enhance the production of reactive oxygen species, damage the blood-brain barrier, and cause hypothalamic-pituitary-adrenal (HPA)–axis activation.38,39 NO2, as a nitrogen-centered free radical, is responsible for initiating a signaling cascade, which also gives rise to oxidative stress40 and may contribute to the onset of depression and anxiety.38 Further research is needed to clarify the mechanisms that underlie the association between air pollution and mental health.
Subgroup analysis indicated that sex may play a role in modulating susceptibility to anxiety associated with PM2.5 exposure. An animal study also found the male mice are more susceptible than female mice to induced neuroinflammation following diesel exhaust particles exposure.41 Estrogen fluctuation in female individuals and differences in the HPA axis between male and female individuals may play a potential role in the associations; as a result, further explorations are still needed.42
Strengths and Limitations
Our study has several strengths. First, we assessed the associations of long-term exposure to multiple air pollutants below the annual values in UK air quality standards with incidence of both depression and anxiety based on prospective study design. Second, an air pollution score was calculated to evaluate the joint exposure to multiple air pollutants, which emphasized the importance of health risk assessment associated with multiple air pollutants exposure. Third, the large sample size of nearly 0.4 million adults and long follow-up time of 10.9 years provided us with a large number of outcome events and adequate statistical power to detect the risk of incident depression and anxiety associated with air pollution. Fourth, detailed information about individual- and area-level covariates are available in the UK Biobank, which contributes to minimizing confounding and detecting the susceptibility of the population.
Some limitations of our study should also be noted. First, although we considered particulate matter and gaseous pollutants including PM2.5, PM2.5-10, NO2, and NO, information on other air pollutants (eg, ozone, sulfur dioxide, and carbon monoxide) was not available. However, PM2.5 and NO2 are primary air pollutants in the UK,43 and we have incorporated them to assess the joint exposure to a combination of air pollutants. Second, air pollution exposure at baseline might not reflect its trends during follow-up. However, air pollution emissions remained relatively stable from 2010 to 2019.44 In addition, there is epidemiologic evidence indicating that using annual mean air pollutants at baseline showed similar associations with that using time-varying air pollutant,45,46 which is consistent with our sensitivity analysis. Third, there is a potential source of selection bias in the UK Biobank due to nonresponse of potential study participants.47 Future studies should take selection weights into account to address this potential source of bias if data are available. Fourth, some residual confounding was inevitable, although a series of individual- and area-level covariates were adjusted according to directed acyclic graph theory. Fifth, it is common that mental disorders cannot be diagnosed in time.48 Although we used available multiple-sources medical conditions, a proportion of the participants with anxiety and depression may not have been diagnosed, which may have underestimated the associations. Sixth, the participants in the UK Biobank are of mainly European descent, for which generalization to other populations should be undertaken with caution. Finally, reverse causality may still exist, although we did a sensitivity analysis by excluding cases that occurred in the first 2 years of follow-up, and the results were robust.
Conclusions
In this large-scale, population-based, prospective cohort study, results suggest that estimated long-term joint exposure to multiple air pollutants at low concentrations was associated with increased risk of incident depression and anxiety. Exposure-response curves showed nonlinear associations, with steeper slopes at lower levels and plateauing trends at higher exposure. Considering that many countries’ air quality standards are still well above the latest World Health Organization global air quality guidelines 2021, stricter standards or regulations for air pollution control should be implemented in the future policy making. Furthermore, the results may provide important evidence for the assessment of mental health associated with air pollution to be considered in the Global Burden of Disease.
eMethods
eTable 1. Description of Air Pollutants
eTable 2. Annual Guidelines for PM2.5 and NO2 in 2021 WHO Global Air Quality Guidelines and Standards in Other Countries
eTable 3. The Spearman Correlations Between Air Pollutants
eTable 4. Censoring Rates for Study Participants According to Categorical Air Pollutants
eTable 5. Associations of Incidence of Depression and Anxiety With Individual Air Pollutant
eTable 6. Interaction Between PM2.5, NO2, and NO for Depression and Anxiety in Additive Hazards Models
eTable 7. Subgroup Analysis and Effect Modification for the Association of Incidence of Depression and Anxiety With Air Pollution Score
eTable 8. Subgroup Analysis and Effect Modification for the Association of Incidence of Depression and Anxiety With PM2.5
eTable 9. Subgroup Analysis and Effect Modification for the Association of Incidence of Depression and Anxiety With NO2
eTable 10. Subgroup Analysis and Effect Modification for the Association of Incidence of Depression and Anxiety With NO
eTable 11. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Multiple Imputation
eTable 12. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Further Adjusting for Household Income
eTable 13. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Further Adjusting for Green Space Percentage
eTable 14. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Replacing Townsend Deprivation Index With Income Score and Housing Score
eTable 15. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Avoiding the Second Depression Outcome for the Same Person if Follow-up Anxiety Was Diagnosed First, and Vice Versa
eTable 16. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Excluding Depression and Anxiety Cases Occurred in the First 2 Years of Follow-up
eTable 17. Associations of Incidence of Depression and Anxiety With Time-Varying PM2.5
eFigure 1. Directed Acyclic Graph for the Association Between Air Pollution and Depression or Anxiety
eFigure 2. Flow Chart of Participants Included in the Study
eFigure 3. Cumulative Survival Curves for Air Pollutants and Incident Depression (A) and Anxiety (B)
Data Sharing Statement
References
- 1.GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-1222. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2019 Mental Disorders Collaborators . Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137-150. doi: 10.1016/S2215-0366(21)00395-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tiller JW. Depression and anxiety. Med J Aust. 2013;199(S6):S28-S31. doi: 10.5694/mja12.10628 [DOI] [PubMed] [Google Scholar]
- 4.Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389(10082):1907-1918. doi: 10.1016/S0140-6736(17)30505-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braithwaite I, Zhang S, Kirkbride JB, Osborn DPJ, Hayes JF. Air pollution (particulate matter) exposure, and associations with depression, anxiety, bipolar, psychosis and suicide risk: a systematic review and meta-analysis. Environ Health Perspect. 2019;127(12):126002. doi: 10.1289/EHP4595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borroni E, Pesatori AC, Bollati V, Buoli M, Carugno M. Air pollution exposure and depression: a comprehensive updated systematic review and meta-analysis. Environ Pollut. 2022;292(Pt A):118245. [DOI] [PubMed] [Google Scholar]
- 7.Newbury JB, Arseneault L, Beevers S, et al. Association of air pollution exposure with psychotic experiences during adolescence. JAMA Psychiatry. 2019;76(6):614-623. doi: 10.1001/jamapsychiatry.2019.0056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gu X, Guo T, Si Y, et al. Association between ambient air pollution and daily hospital admissions for depression in 75 Chinese cities. Am J Psychiatry. 2020;177(8):735-743. doi: 10.1176/appi.ajp.2020.19070748 [DOI] [PubMed] [Google Scholar]
- 9.Wang F, Liu H, Li H, et al. Ambient concentrations of particulate matter and hospitalization for depression in 26 Chinese cities: a case-crossover study. Environ Int. 2018;114:115-122. doi: 10.1016/j.envint.2018.02.012 [DOI] [PubMed] [Google Scholar]
- 10.Szyszkowicz M, Kousha T, Kingsbury M, Colman I. Air pollution and emergency department visits for depression: a multicity case-crossover study. Environ Health Insights. 2016;10:155-161. doi: 10.4137/EHI.S40493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou YM, Fan YN, Yao CY, et al. Association between short-term ambient air pollution and outpatient visits of anxiety: a hospital-based study in northwestern China. Environ Res. 2021;197:111071. doi: 10.1016/j.envres.2021.111071 [DOI] [PubMed] [Google Scholar]
- 12.Ma Y, Wang W, Li Z, et al. Short-term exposure to ambient air pollution and risk of daily hospital admissions for anxiety in China: a multicity study. J Hazard Mater. 2022;424(Pt B):127535. [DOI] [PubMed] [Google Scholar]
- 13.Yue JL, Liu H, Li H, et al. Association between ambient particulate matter and hospitalization for anxiety in China: a multicity case-crossover study. Int J Hyg Environ Health. 2020;223(1):171-178. doi: 10.1016/j.ijheh.2019.09.006 [DOI] [PubMed] [Google Scholar]
- 14.Kioumourtzoglou MA, Power MC, Hart JE, et al. The association between air pollution and onset of depression among middle-aged and older women. Am J Epidemiol. 2017;185(9):801-809. doi: 10.1093/aje/kww163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Power MC, Kioumourtzoglou MA, Hart JE, Okereke OI, Laden F, Weisskopf MG. The relation between past exposure to fine particulate air pollution and prevalent anxiety: observational cohort study. BMJ. 2015;350:h1111. doi: 10.1136/bmj.h1111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pun VC, Manjourides J, Suh H. Association of ambient air pollution with depressive and anxiety symptoms in older adults: results from the NSHAP study. Environ Health Perspect. 2017;125(3):342-348. doi: 10.1289/EHP494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang KC, Lo YC, Liao CC, Jou YY, Huang HB. Associations between symptoms of depression and air pollutant exposure among older adults: results from the Taiwan Longitudinal Study on Aging (TLSA). Front Public Health. 2022;9:779192. doi: 10.3389/fpubh.2021.779192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y, Eliot MN, Koutrakis P, et al. Ambient air pollution and depressive symptoms in older adults: results from the MOBILIZE Boston study. Environ Health Perspect. 2014;122(6):553-558. doi: 10.1289/ehp.1205909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Z, Zhao D, Hong YS, et al. Long-term particulate matter exposure and onset of depression in middle-aged men and women. Environ Health Perspect. 2019;127(7):77001. doi: 10.1289/EHP4094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim KN, Lim YH, Bae HJ, Kim M, Jung K, Hong YC. Long-term fine particulate matter exposure and major depressive disorder in a community-based urban cohort. Environ Health Perspect. 2016;124(10):1547-1553. doi: 10.1289/EHP192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wei F, Yu Z, Zhang X, et al. Long-term exposure to ambient air pollution and incidence of depression: a population-based cohort study in China. Sci Total Environ. 2022;804:149986. doi: 10.1016/j.scitotenv.2021.149986 [DOI] [PubMed] [Google Scholar]
- 22.Oakes M, Baxter L, Long TC. Evaluating the application of multipollutant exposure metrics in air pollution health studies. Environ Int. 2014;69:90-99. doi: 10.1016/j.envint.2014.03.030 [DOI] [PubMed] [Google Scholar]
- 23.Yu L, Liu W, Wang X, et al. A review of practical statistical methods used in epidemiological studies to estimate the health effects of multipollutant mixture. Environ Pollut. 2022;306:119356. doi: 10.1016/j.envpol.2022.119356 [DOI] [PubMed] [Google Scholar]
- 24.Sudlow C, Gallacher J, Allen N, et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3):e1001779. doi: 10.1371/journal.pmed.1001779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.European Union . ESCAPE: European Study of Cohorts for Air Pollution Effects. Accessed May 5, 2022. http://www.escapeproject.eu/
- 26.Eeftens M, Beelen R, de Hoogh K, et al. Development of land use regression models for PM(2.5), PM(2.5) absorbance, PM(10) and PM(coarse) in 20 European study areas; results of the ESCAPE project. Environ Sci Technol. 2012;46(20):11195-11205. doi: 10.1021/es301948k [DOI] [PubMed] [Google Scholar]
- 27.Beelen R, Hoek G, Vienneau D, et al. Development of NO2 and NOx land use regression models for estimating air pollution exposure in 36 study areas in Europe: the ESCAPE project. Atmos Environ. 2013;72:10-23. doi: 10.1016/j.atmosenv.2013.02.037 [DOI] [Google Scholar]
- 28.Cyrys J, Eeftens M, Heinrich J, et al. Variation of NO2 and NOx concentrations between and within 36 European study areas: results from the ESCAPE study. Atmos Environ. 2012;62:374-390. doi: 10.1016/j.atmosenv.2012.07.080 [DOI] [Google Scholar]
- 29.Abdi H, Williams LJ. Principal component analysis. Wiley Interdiscip Rev Comput Stat. 2010;2(4):433-459. doi: 10.1002/wics.101 [DOI] [Google Scholar]
- 30.Macpherson JM, Gray SR, Ip P, et al. Child maltreatment and incident mental disorders in middle and older ages: a retrospective UK Biobank cohort study. Lancet Reg Health Eur. 2021;11:100224. doi: 10.1016/j.lanepe.2021.100224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tennant PWG, Murray EJ, Arnold KF, et al. Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: review and recommendations. Int J Epidemiol. 2021;50(2):620-632. doi: 10.1093/ije/dyaa213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Westreich D, Greenland S. The table 2 fallacy: presenting and interpreting confounder and modifier coefficients. Am J Epidemiol. 2013;177(4):292-298. doi: 10.1093/aje/kws412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Turner MC, Cohen A, Burnett RT, et al. Interactions between cigarette smoking and ambient PM2.5 for cardiovascular mortality. Environ Res. 2017;154:304-310. doi: 10.1016/j.envres.2017.01.024 [DOI] [PubMed] [Google Scholar]
- 34.Rutherford MJ, Crowther MJ, Lambert PC. The use of restricted cubic splines to approximate complex hazard functions in the analysis of time-to-event data: a simulation study. J Stat Comput Simul. 2015;85(4):777-793. doi: 10.1080/00949655.2013.845890 [DOI] [Google Scholar]
- 35.Tomova GD, Arnold KF, Gilthorpe MS, Tennant PWG. Adjustment for energy intake in nutritional research: a causal inference perspective. Am J Clin Nutr. 2022;115(1):189-198. doi: 10.1093/ajcn/nqab266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hammer MS, van Donkelaar A, Li C, et al. Global estimates and long-term trends of fine particulate matter concentrations (1998-2018). Environ Sci Technol. 2020;54(13):7879-7890. doi: 10.1021/acs.est.0c01764 [DOI] [PubMed] [Google Scholar]
- 37.Block ML, Calderón-Garcidueñas L. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009;32(9):506-516. doi: 10.1016/j.tins.2009.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hahad O, Lelieveld J, Birklein F, Lieb K, Daiber A, Münzel T. Ambient air pollution increases the risk of cerebrovascular and neuropsychiatric disorders through induction of inflammation and oxidative stress. Int J Mol Sci. 2020;21(12):4306. doi: 10.3390/ijms21124306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9(1):46-56. doi: 10.1038/nrn2297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kelly FJ. Oxidative stress: its role in air pollution and adverse health effects. Occup Environ Med. 2003;60(8):612-616. doi: 10.1136/oem.60.8.612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ehsanifar M, Montazeri Z, Taheri MA, Rafati M, Behjati M, Karimian M. Hippocampal inflammation and oxidative stress following exposure to diesel exhaust nanoparticles in male and female mice. Neurochem Int. 2021;145:104989. doi: 10.1016/j.neuint.2021.104989 [DOI] [PubMed] [Google Scholar]
- 42.Cho J, Choi YJ, Suh M, et al. Air pollution as a risk factor for depressive episode in patients with cardiovascular disease, diabetes mellitus, or asthma. J Affect Disord. 2014;157:45-51. doi: 10.1016/j.jad.2014.01.002 [DOI] [PubMed] [Google Scholar]
- 43.The Lancet . UK air pollution and public health. Lancet. 2017;389(10082):1860. doi: 10.1016/S0140-6736(17)31271-0 [DOI] [PubMed] [Google Scholar]
- 44.Department for Environment Food and Rural Affairs . Air quality statistics: an annual update on concentrations of major air pollutants in the UK. Accessed October 1, 2022. https://webarchive.nationalarchives.gov.uk/ukgwa/20201225100256/https://www.gov.uk/government/statistics/air-quality-statistics
- 45.Qiu H, Schooling CM, Sun S, et al. Long-term exposure to fine particulate matter air pollution and type 2 diabetes mellitus in elderly: a cohort study in Hong Kong. Environ Int. 2018;113:350-356. doi: 10.1016/j.envint.2018.01.008 [DOI] [PubMed] [Google Scholar]
- 46.Wong CM, Lai HK, Tsang H, et al. Satellite-based estimates of long-term exposure to fine particles and association with mortality in elderly Hong Kong residents. Environ Health Perspect. 2015;123(11):1167-1172. doi: 10.1289/ehp.1408264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang JY. Representativeness is not representative: addressing major inferential threats in the UK Biobank and other big data repositories. Epidemiology. 2021;32(2):189-193. doi: 10.1097/EDE.0000000000001317 [DOI] [PubMed] [Google Scholar]
- 48.Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):603-613. doi: 10.1001/archpsyc.62.6.603 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
eTable 1. Description of Air Pollutants
eTable 2. Annual Guidelines for PM2.5 and NO2 in 2021 WHO Global Air Quality Guidelines and Standards in Other Countries
eTable 3. The Spearman Correlations Between Air Pollutants
eTable 4. Censoring Rates for Study Participants According to Categorical Air Pollutants
eTable 5. Associations of Incidence of Depression and Anxiety With Individual Air Pollutant
eTable 6. Interaction Between PM2.5, NO2, and NO for Depression and Anxiety in Additive Hazards Models
eTable 7. Subgroup Analysis and Effect Modification for the Association of Incidence of Depression and Anxiety With Air Pollution Score
eTable 8. Subgroup Analysis and Effect Modification for the Association of Incidence of Depression and Anxiety With PM2.5
eTable 9. Subgroup Analysis and Effect Modification for the Association of Incidence of Depression and Anxiety With NO2
eTable 10. Subgroup Analysis and Effect Modification for the Association of Incidence of Depression and Anxiety With NO
eTable 11. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Multiple Imputation
eTable 12. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Further Adjusting for Household Income
eTable 13. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Further Adjusting for Green Space Percentage
eTable 14. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Replacing Townsend Deprivation Index With Income Score and Housing Score
eTable 15. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Avoiding the Second Depression Outcome for the Same Person if Follow-up Anxiety Was Diagnosed First, and Vice Versa
eTable 16. Associations of Incidence of Depression and Anxiety With Exposure to Air Pollutants by Excluding Depression and Anxiety Cases Occurred in the First 2 Years of Follow-up
eTable 17. Associations of Incidence of Depression and Anxiety With Time-Varying PM2.5
eFigure 1. Directed Acyclic Graph for the Association Between Air Pollution and Depression or Anxiety
eFigure 2. Flow Chart of Participants Included in the Study
eFigure 3. Cumulative Survival Curves for Air Pollutants and Incident Depression (A) and Anxiety (B)
Data Sharing Statement


