Key Points
Question
What are the outcomes of nonoperative vs operative management of acute appendicitis in older adults, and are they different from what is seen in younger adults?
Findings
In this cohort study, nonoperative management of acute appendicitis in adults 65 years and older was associated with reduced complications, which was different than in those younger than 65 years.
Meaning
Nonoperative outcomes in this study were different in older versus younger adults with acute appendicitis; clinical trials should consider age in evaluating the best management approach for acute appendicitis.
This cohort study evaluates outcomes following nonoperative and operative treatment for acute appendicitis in older US adults.
Abstract
Importance
Although the incidence of acute appendicitis among adults 65 years and older is high, these patients are underrepresented in randomized clinical trials comparing nonoperative vs operative management of appendicitis; it is unclear whether current trial data can be used to guide treatment in older adults.
Objective
To compare outcomes following nonoperative vs operative management of appendicitis in older adults and assess whether they differ from results in younger patients.
Design, Setting, and Participants
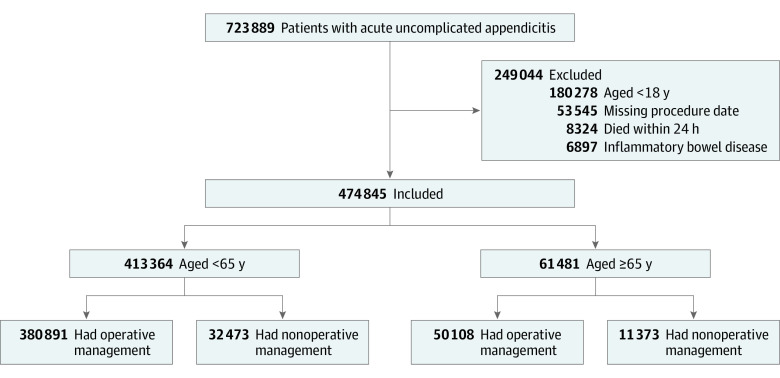
This retrospective cohort study used US hospital admissions data from the Agency for Healthcare Research and Quality’s National Inpatient Sample from 2004 to 2017. Of 723 889 adult patients with acute uncomplicated appendicitis, 474 845 with known procedure date who survived 24 hours postprocedure and did not have inflammatory bowel disease were included (43 846 who were treated nonoperatively and 430 999 with appendectomy) were included. Data were analyzed from October 2021 to April 2022.
Exposures
Nonoperative vs operative management.
Main Outcomes and Measures
The primary outcome was incidence of posttreatment complications. Secondary outcomes included mortality, length of stay, and inpatient costs. Differences were estimated using inverse probability weighting of the propensity score with sensitivity analysis to quantify effects of unmeasured confounding.
Results
The median (IQR) age in the overall cohort was 39 (27-54) years, and 29 948 participants (51.3%) were female. In patients 65 years and older, nonoperative management was associated with a 3.72% decrease in risk of complications (95% CI, 2.99-4.46) and a 1.82% increase in mortality (95% CI, 1.49-2.15) along with increased length of hospitalization and costs. Outcomes in patients younger than 65 years were significantly different than in older adults, with only minor differences between nonoperative and operative management with respect to morbidity and mortality, and smaller differences in length of hospitalization and costs. Morbidity and mortality results were somewhat sensitive to bias from unmeasured confounding.
Conclusions and Relevance
Nonoperative management was associated with reduced complications in older but not younger patients; however, operative management was associated with reduced mortality, hospital length of stay, and overall costs across all age groups. The different outcomes of nonoperative vs operative management of appendicitis in older and younger adults highlights the need for a randomized clinical trial to determine the best approach for managing appendicitis in older patients.
Introduction
Appendicitis has traditionally been treated with appendectomy, but there is growing evidence to support nonoperative management with antibiotics for uncomplicated appendicitis.1,2 However, randomized clinical trials of nonoperative vs operative management have primarily included patients younger than 65 years with limited comorbidities, while adults 65 years and older were underrepresented or excluded.1,3,4 Such underrepresentation is problematic because individuals 65 years and older will soon comprise 20% of the US population; although appendicitis is less common in older adults, incidence remains high; and older adults may be more difficult to treat when nonoperative management fails because of greater comorbidity burden.5 As a result, it is unclear if existing data can generalize to older adults and guide therapeutic decisions.
Our study aimed to compare nonoperative and operative management of uncomplicated acute appendicitis in older adults, since to our knowledge there are currently no data to estimate risks in this population. Additionally, we sought to determine if the risk-benefit profile in older adults was similar to that of the younger patients enrolled in prior clinical trials. We hypothesized that, compared to appendectomy, nonoperative management of acute appendicitis would be associated with similar morbidity and mortality but increased hospitalization length and costs for older adults and that nonoperative management in older adults would have a different risk-benefit profile than for younger adults. This study has implications for whether existing data are sufficient to inform decision-making in older adults with acute uncomplicated appendicitis.6
Methods
Setting and Population
This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline (eMethods in Supplement 1). After receiving approval from the institutional review board of the University of Texas Southwestern, we searched the National Inpatient Sample (NIS) database from 2004 to 2017. Patients were selected based on International Classification of Disease (ICD) codes for uncomplicated acute appendicitis (ICD Ninth Revision [9] 540 and Tenth Revision [10] K35) and included patients who were alive 24 hours after admission. Uncomplicated appendicitis was defined as without perforation, abscess, or peritonitis, as this mirrors prior research and excludes patients with an abscess or phlegmon, which would likely be managed nonoperatively. We also excluded individuals younger than 18 years, those with inflammatory bowel disease, those who underwent a procedure but were missing dates, and those who died within 24 hours of admission. See Figure 1 for information on patient selection. In total, missing data accounted for less than 10% of cases. Data were analyzed from October 2021 to April 2022.
Figure 1. Patient Selection.
Study Design and Database
This retrospective cohort study used the NIS, which provides information on individual hospitalizations and in-hospital follow-up. This database was developed by the Healthcare Cost and Utilization Project, is sponsored by the Agency for Healthcare Research and Quality, and is the largest publicly available inpatient database, encompassing data from all payers. It captures more than 7 million inpatient stays and represents 35 million hospitalizations. Collection and quality control information can be found at the Healthcare Cost and Utilization Project website.7
Independent Variable
The exposure of interest was nonoperative vs operative management of acute appendicitis. Operative management was defined as appendectomy (identified by ICD procedure codes for laparoscopic appendectomy, open appendectomy, exploratory laparotomy, ascending colectomy, or ileocecectomy) performed within 1 day of admission. Nonoperative management was defined as not having surgery consistent with appendectomy performed on day 0 or 1 of admission.
Because appendectomy may be delayed more than 1 day after admission, we conducted a sensitivity analysis to avoid misclassifications. We varied the definition of operative management to include surgery within 1 day, 2 or more days, and 3 or more days after admission and repeated all analyses. Since results were consistent, the results presented are based on the original classification.
Outcomes
The primary outcome was the incidence of postoperative complications: a composite variable based on validated ICD-9 and ICD-10 codes including wound complications, infection, urinary tract infection, pulmonary, gastrointestinal, cardiovascular, thromboembolism, cerebrovascular accident, kidney failure, and bleeding.8,9,10 For nonoperative patients, procedures (appendectomy, exploratory laparotomy, colonic resection, or interventional radiology drainage) that occurred more than 1 day after admission were considered complications. Secondary outcomes included mortality, length of hospitalization, and inpatient costs calculated using cost-charge ratios and inflation adjustment to the most recent year’s value.
Statistical Analysis
We grouped patients according to age and included analyses with the entire cohort, those younger than 65 years, and those 65 years and older, as this is a common designation for older age. For risk adjustment, we used inverse probability weighting of the propensity score with regression adjustment including all variables in the Table. This technique offers a more efficient use of the data than matching, has more flexibility within the common overlap region, and increases the chances of having an unbiased estimate in the setting of misspecification.11 Our balanced patient cohorts after adjusting with the propensity score are presented in the Table and eTable 1 in Supplement 1.
Table. Characteristics of Patients 65 Years and Older After Adjustment With Propensity Weighting.
| Characteristic | Propensity weighted cohorts, No. (%) | Standardized differences, % | ||
|---|---|---|---|---|
| Nonoperative management (n = 29 085) | Operative management (n = 29 324) | Unadjusted | Adjusted | |
| Age, mean (SD), y | 74.0 (7.1) | 73.9 (7.0) | 31.02 | 1.17 |
| Female | 14 902 (51.2) | 15 046 (51.3) | 0.74 | 0.21 |
| Male (reference) | 14 183 (48.8) | 14 278 (48.7) | NA | NA |
| Race and ethnicitya | ||||
| Asian | 1184 (4.1) | 1192 (4.1) | 1.61 | 0.03 |
| Black | 1548 (5.3) | 1560 (5.3) | 16.69 | 0.09 |
| Hispanic | 2236 (7.7) | 2215 (7.6) | 1.03 | 0.70 |
| Native American | 88 (0.3) | 91 (0.3) | 1.84 | 0.26 |
| White (reference) | 20 974 (72.1) | 21 201 (72.3) | NA | NA |
| Other | 647 (2.2) | 656 (2.2) | 2.77 | 0.15 |
| Unknown | 2408 (8.3) | 2410 (8.2) | 2.09 | 0.32 |
| Income quartile (based on zip code), $ | ||||
| ≤38 999 (reference) | 6390 (22.0) | 6360 (21.7) | NA | NA |
| 39 000-47 999 | 7139 (24.6) | 7176 (24.5) | 0.36 | 0.30 |
| 48 000-62 999 | 7198 (24.8) | 7333 (25.0) | 4.66 | 0.84 |
| ≥63 000 | 7774 (26.7) | 7873 (26.9) | 4.53 | 0.44 |
| Unknown | 583 (2.0) | 583 (2.0) | 0.69 | 0.10 |
| Primary payer | ||||
| Medicare (reference) | 24 712 (85.0) | 24 948 (85.1) | NA | NA |
| Medicaid | 577 (2.0) | 577 (2.0) | 2.03 | 2.36 |
| Private | 3511 (12.1) | 3500 (11.9) | 8.35 | 0.46 |
| Other | 284 (1.0) | 300 (1.0) | 1.59 | 0.60 |
| Hospital region | ||||
| Northeast (reference) | 6070 (20.9) | 6226 (21.2) | NA | NA |
| Midwest | 5566 (19.1) | 5504 (18.8) | 7.13 | 1.29 |
| South | 10 392 (35.7) | 10 492 (35.8) | 4.14 | 0.05 |
| West | 7057 (24.3) | 7102 (24.2) | 9.11 | 0.12 |
| Hospital size | ||||
| Small (reference) | 4832 (16.6) | 4824 (16.5) | NA | NA |
| Medium | 8182 (28.1) | 8237 (28.1) | 1.17 | 0.07 |
| Large | 16 071 (55.3) | 16 263 (55.5) | 2.09 | 0.49 |
| Location and teaching status of hospital | ||||
| Rural (reference) | 3804 (13.1) | 3843 (13.1) | NA | NA |
| Urban | ||||
| Nonteaching | 12 359 (42.5) | 12 638 (43.1) | 21.18 | 1.59 |
| Teaching | 12 922 (44.4) | 12 844 (43.8) | 21.33 | 1.70 |
| Diabetes | 5613 (19.3) | 5523 (18.8) | 9.63 | 1.70 |
| Chronic pulmonary disease | 5243 (18.0) | 5193 (17.7) | 13.89 | 1.21 |
| Congestive heart failure | 2905 (10.0) | 2877 (9.8) | 26.46 | 1.25 |
| Hypertension | 18 825 (64.7) | 18 829 (64.2) | 5.51 | 1.54 |
| Liver disease | 796 (2.7) | 788 (2.7) | 13.01 | 0.88 |
| Metastatic cancer | 743 (2.6) | 747 (2.6) | 21.24 | 0.56 |
| Peripheral vascular disorders | 1702 (5.9) | 1654 (5.6) | 12.37 | 1.41 |
| Kidney failure | 2755 (9.5) | 2711 (9.3) | 23.66 | 1.61 |
Abbreviation: NA, not applicable.
Race and ethnicity were gathered and categorized according to the National Inpatient Sample description of data elements.
Sensitivity Analyses
Because observational studies are subject to bias from unmeasured confounding, we conducted 2 analyses to assess robustness of findings to the effects of an unmeasured confounder. First, we used a probabilistic sensitivity analysis to assess how an unmeasured confounder could affect results for morbidity and mortality.12,13 For example, surgeons are presumably more likely to offer nonoperative management to patients whose age, comorbidity, or frailty would increase their risk of postoperative complications. We simulated the effects of an unmeasured confounder representing higher degrees of frailty or illness.14 We assumed it was present in 25% to 90% of the nonoperative patients, was twice as common in the nonoperative group, and increased the relative risk of morbidity and mortality by 1.1 to 4-fold. We simulated these effects 5000 times to estimate changes in the propensity score models. This generated a 95% simulation interval representing the difference between groups after accounting for unmeasured confounding. Each simulation is a random draw from a trapezoidal distribution with a random error component so that the prevalence and strength of the confounder varied between samples within the specified ranges.
The E-value represents the minimum strength of association between an unmeasured confounder and the outcome or exposure that could change a statistically significant result into a null result.15 This asks how strong an unmeasured confounder would have to be for a significant finding to be attributable to bias from the confounder rather than a real association between exposure and outcome, implying the original model would have estimated no effect if it had included the unmeasured confounder.
The NIS only includes information on the current hospitalization, so we are not able to comment on need for future appendectomy and subsequent complications in patients initially treated with nonoperative management, which may underestimate complications in the nonoperative group. To estimate this incidence, we used a 2-way deterministic sensitivity analysis wherein we varied (1) the nonoperative failure rate from 15% to 30% (the observed rate in recent trials) and (2) the postoperative complication rate after appendectomy from 11% to 15% (the rate in our operative cohort). The probability of incurring a complication from nonoperative failure requiring appendectomy was the joint probability of (1) and (2), which we compared to the observed difference in morbidity from our propensity-weighted analysis.
One criticism of nonoperative management in older adults is that appendiceal cancers may present as acute appendicitis, and nonoperative management will delay the diagnosis. To quantify the incidence of missed cancers in the nonoperative group, we used the National Surgical Quality Improvement Program Appendectomy database to identify rates of cancer diagnosed after appendectomy for acute appendicitis. Since the incidence in patients 65 years and older ranged from 1.7% to 3.9%, we used a β distribution to estimate appendiceal cancer incidence across 10 000 simulations, providing an expected mean incidence of missed cancers with a 95% simulation interval.
We also assessed whether the effects of nonoperative management were different in older vs younger adults. We estimated separate regression models for outcomes in older and younger adults then compared the coefficients for the estimated treatment effects to determine whether they differed at the P < .05 level, while accounting for differences in the variance-covariance matrix in each cohort via the cluster-adjusted sandwich estimator. This was done using the Stata suest command for seemingly unrelated estimation.16,17
We performed the analysis at additional age cutoffs and noted consistent results. As such, only results for patients 65 years and older are presented. Missingness was present in less than 10% of cases, and missing values consisted primarily of procedure dates, which are not amenable to imputation. Thus we conducted a complete case analysis. We used Stata version 17 (StataCorp) for analysis, with P < .05 considered significant.
Results
Patient Characteristics
We included 474 845 patients (median [IQR] age, 39 [27-54]; 29 948 [51.3%] female) with acute uncomplicated appendicitis (eTable 2 in Supplement 1). Of these, 43 846 (9.2%) underwent nonoperative management. The median (IQR) age of the nonoperative cohort was 49 (33-65) years compared to 38 (27-53) years for the operative cohort (P < .001). Patients 65 years and older accounted for 12.9% of the sample, and 18.4% were treated nonoperatively. By contrast, nonoperative management was substantially less common among younger patients (7.9%). Increasing comorbidity was associated with increased likelihood of nonoperative management (eTable 2 in Supplement 1). See eTable 3 in Supplement 1 for information on patient outcomes.
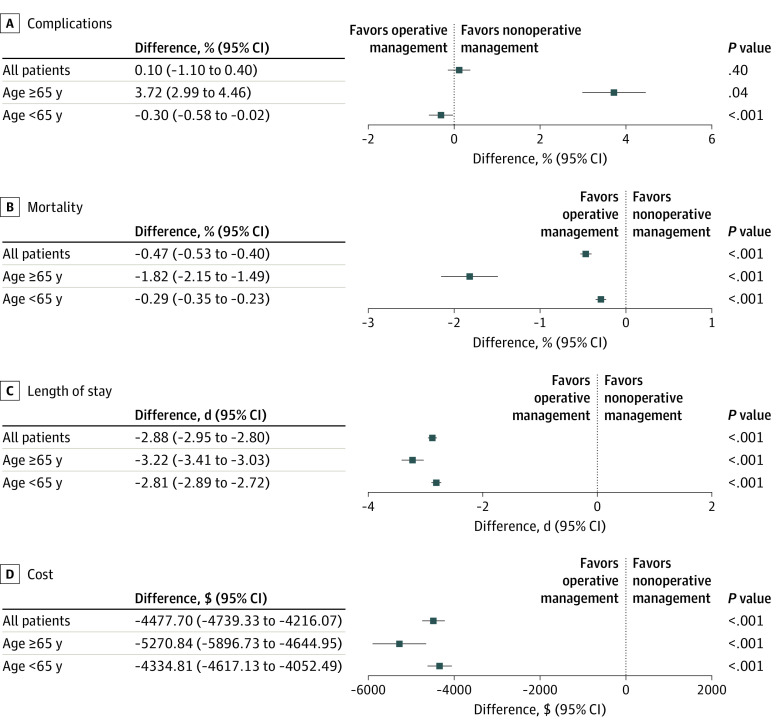
Association of Nonoperative Management With Fewer Complications in Older Adults
In patients 65 years and older, nonoperative management was associated with a 3.72% decrease in morbidity (95% CI, 2.99-4.46; P < .001) (Figure 2A). Probabilistic sensitivity analysis (eFigure 1 in Supplement 1) suggested that our initial results likely underestimated the morbidity reduction associated with nonoperative management because the bias-corrected 95% simulation interval was lower than the original estimate. Additionally, the E-value necessary to generate a null result was 2.2, indicating a result that was robust to moderate levels of unmeasured confounding. To address potential postdischarge complications from recurrent appendicitis, our 2-way deterministic sensitivity analysis found that if the rate of nonoperative failure was less than 30%, there was still a morbidity benefit with nonoperative management.
Figure 2. Mean Treatment Effect for Nonoperative vs Operative Management of Appendicitis by Age.
Association of Nonoperative Management With Increased Mortality in Older Adults
Nonoperative management was associated with a 1.82% increase in mortality (95% CI, 1.49-2.15; P < .001) for patients 65 years and older (Figure 2B). However, probabilistic sensitivity analysis suggested that these results were susceptible to the effects of unmeasured confounding and may not represent a reliable estimate of differences. Technically, the sensitivity analysis demonstrated a 95% simulation interval greater than 1 for nonoperative vs operative management (1.61-3.11; eFigure 2 in Supplement 1), but bias-corrected estimates shifted markedly closer to 1 than the propensity score analysis, and the E-value needed to generate a null result was 2.4. Taken together, these results suggest that unmeasured confounding has the potential to influence our original estimate.
Association of Nonoperative Management of Appendicitis With Increased Health Care Use in Older Adults
Patients 65 years and older who received nonoperative treatment had increased hospital length of stay by 3.22 days (95% CI, 3.03-3.41; P < .001) compared to those who underwent appendectomy (Figure 2C). This was consistent with higher hospital costs (Figure 2D) in the nonoperative group ($5270.84; 95% CI, $4644.95-$5896.73; P < .001).
Potential for Missed Appendiceal Cancer in Older Adults Treated Nonoperatively
To estimate the risk of missed appendiceal cancer, we ran 10 000 simulations. We found that in an unweighted cohort of 11 373 patients, the mean number of missed cancers was 341 (95% simulation interval, 239-441), assuming the incidence of cancer in a cohort aged 65 years and older ranged from 1.7%-3.9%.
Risk Profile of Nonoperative Management in Younger vs Older Patients
We formally tested whether each outcome differed between older and younger patients following nonoperative management. We found that for each outcome of interest, there was a significant difference in the treatment coefficient. The odds of developing a complication were greater with operative management for both age groups; however, those 65 years and older experienced increased odds of developing a complication (odds ratio [OR], 1.70; 95% CI, 1.58-1.83) relative to younger adults (OR, 1.07; 95% CI, 1.02-1.13), a significant difference (P < .001). Both age groups experienced reduced odds of mortality with operative management, but patients younger than 65 years had reduced odds of mortality relative to those 65 years and older who received operative management (OR, 0.16; 95% CI, 0.13-0.19 vs OR, 0.38; 95% CI, 0.33-0.43), a significant difference (P < .001). Our linear regression model found that older adults who received operative management were estimated to spend 3.09 fewer days in the hospital (95% CI, −3.21 to −2.98) and those younger than 65 years with operative management were estimated to spend 3.17 fewer days in the hospital (95% CI, −3.21 to −3.13), a significant difference (P < .001). The estimated costs associated with operative management were also significantly different between age groups (65 years and older, −$4924; 95% CI, −$5272.07 to −$4576 vs younger than 65 years, −$4904; 95% CI, −$5017 to −$4792; P < .001).
For individuals younger than 65 years, nonoperative management was associated with a 0.30% increase in postoperative complications (95% CI, 0.02-0.58; P = .04), a 0.29% increase in mortality (95% CI, 0.23-0.35; P < .001), a 2.81-day longer hospital length of stay (95% CI, 2.89-2.72; P < .001), and a $4334.81 increase in costs (95% CI, $4052.49-$4617.13). The probabilistic sensitivity analyses for the entire cohort is described in the eResults and eFigures 1 and 2 in Supplement 1.
Discussion
The key finding of our study is that the relative balance of risks and benefits with nonoperative vs operative management of acute appendicitis was noticeably different in older patients compared to prior randomized clinical trials, which included mostly younger patients. After simulating the effects of bias from unmeasured confounding, nonoperative management of appendicitis in older adults was associated with fewer short-term complications, equivocal differences in mortality, increased length of stay, and greater costs compared to appendectomy. By contrast, nonoperative management of appendicitis in younger adults was associated with no difference in morbidity, a small difference in mortality, and increased length of stay and costs (though smaller in magnitude than older adults). In short, we found that analyzing older and younger adults together obscured differences in outcomes. This suggests that when making decisions about appendicitis management in older adults, surgeons should be cautious about drawing on data from younger, healthier patients. Our finding is significant because we also found that nonoperative management of appendicitis has become routine for older adults, with nearly 20% being treated with antibiotics—twice the rate for younger patients. Since older adults are much more likely to receive nonoperative management, the underrepresentation of these patients in trials is concerning because there is a lack of evidence supporting this common clinical practice.
Our findings add to the growing body of literature examining the safety and efficacy of nonoperative management of acute appendicitis. The Comparison of Outcomes of Antibiotic Drugs and Appendectomy trial4 randomized 1552 patients with acute appendicitis to antibiotics vs appendectomy and found that nonoperative management was noninferior to appendectomy with respect to quality of life, despite increased risk of complications in the nonoperative arm. However, the mean age of participants was 38 years, only 8% of participants were 60 years or older, and the average Charlson score was 0.24, indicating a near absence of comorbidity. A meta-analysis of 11 randomized clinical trials by Yang et al18 noted that complications were generally lower with nonoperative management (odds ratio, 0.22-0.51), but nonoperative patients were more likely to require subsequent interventions (odds ratio, 9.58-14.29). Conversely, another meta-analysis19 included 1351 patients and found no difference in complications between surgical and antibiotic treatment. The above trials similar lack of representation of older adults and patients with comorbidities, with some trials deliberately excluding older patients.3,20,21 Given the known differences between older and younger adults, this raises concern about whether data from these trials can reasonably be used to guide treatment decisions for older adults.
This study represents an important step toward addressing the underrepresentation of older adults in clinical trials comparing nonoperative vs operative management of appendicitis. We used a nationally representative database, which facilitated analysis of outcomes for large numbers of older patients and increased external validity. We also made a strong effort to account for and quantify effects of unmeasured confounding that threaten valid inference from observational data. This approach was recommended in the STROBE guidelines, as findings from observational studies are biased by unmeasured confounding. Too often, authors dismiss this problem by arguing that the observed effect is large enough that it is unlikely to be affected by confounding; however, modern statistical tools allow us to test this assumption.12,15 If observational study results can only be changed by an unreasonably large unmeasured confounder, this provides confidence in the validity of its findings. However, if a small unmeasured confounder can nullify a result, then the result should be regarded skeptically.
Limitations
This study has limitations. First, although we applied rigorous techniques to account for unmeasured confounding, the accuracy of this approach depends on correctly approximating the potential effects of the confounder. It is possible that our estimates did not adequately correct for bias. However, we applied 2 separate techniques precisely because they have different underlying assumptions and could triangulate estimations of bias. Second, our data set was limited to information on the primary admission for treatment of appendicitis, so we were not able to directly evaluate differences in readmissions, postdischarge reintervention, or missed appendiceal cancer. As a result, we used simulation to assess how this missing data might affect our conclusions. However, despite our best efforts, it is possible that these long-term differences would erase any short-term gains of nonoperative management in older adults and this might be missed by our simulations. Due to database limitations, we were also unable to identify patients who had a fecalith, which has been shown to lead to differential outcomes with nonoperative management.22 Further, estimation of costs via cost-charge ratios may be conservative and can miss small differences in costs between groups. An additional weakness of the NIS is that we were unable to determine which aspects of care contributes to cost differences and could only perform a comparison of overall costs between nonoperative and operative management. Furthermore, it is possible that some patients who received nonoperative treatment were not offered surgery because their condition on admission was essentially terminal. Inclusion of such patients would artificially increase the risks of morbidity and mortality for the nonoperative group. Similarly, a patient could have been admitted with plans for appendectomy, but surgery was delayed. Under our classification scheme, they would have been classified as nonoperative failures because they appeared to require surgery after initial nonoperative management. We addressed the misclassification problem by varying our definition of what constituted nonoperative management and excluding patients who died within 24 hours of admission.
Conclusions
This cohort study found that nonoperative management was associated with reduced complications for older but not younger patients and that mortality, length of stay, and reduced hospital costs were associated with operative management (although the mortality difference was potentially subject to unmeasured confounding effects). Our study is not meant to be a definitive description of how nonoperative and operative management compare in the treatment of acute appendicitis among older adults. Instead, we sought to conduct a comprehensive study to evaluate whether it was reasonable to guide treatment of older adults based on prior clinical trials that mostly studied younger adults. Unsurprisingly, we found that outcomes in younger adults differed from those in older adults. This highlights the need to conduct a comprehensive randomized clinical trial of nonoperative vs operative management of appendicitis in older adults so that surgeons have relevant data to use when considering treatment options.
eFigure 1. A probabilistic sensitivity analysis - nonoperative management of acute appendicitis and complications
eFigure 2. A probabilistic sensitivity analysis - nonoperative management of acute appendicitis and mortality
eMethods. STROBE Statement—checklist of items that should be included in reports of observational studies
eResults. Full results from the sensitivity analysis
eTable 1. Standardized Differences and post-adjustment weights for the cohort following balancing using the propensity score
eTable 2. Unadjusted patient characteristics
eTable 3. Bivariate results of outcomes
Data sharing statement
References
- 1.Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313(23):2340-2348. doi: 10.1001/jama.2015.6154 [DOI] [PubMed] [Google Scholar]
- 2.Harnoss JC, Zelienka I, Probst P, et al. Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015: CRD42015016882). Ann Surg. 2017;265(5):889-900. doi: 10.1097/SLA.0000000000002039 [DOI] [PubMed] [Google Scholar]
- 3.Salminen P, Tuominen R, Paajanen H, et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA. 2018;320(12):1259-1265. doi: 10.1001/jama.2018.13201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flum DR, Davidson GH, Monsell SE, et al. ; CODA Collaborative . A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med. 2020;383(20):1907-1919. doi: 10.1056/NEJMoa2014320 [DOI] [PubMed] [Google Scholar]
- 5.Anderson LA, Goodman RA, Holtzman D, Posner SF, Northridge ME. Aging in the United States: opportunities and challenges for public health. Am J Public Health. 2012;102(3):393-395. doi: 10.2105/AJPH.2011.300617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haijanen J, Sippola S, Grönroos J, et al. ; APPAC study group . Optimising the antibiotic treatment of uncomplicated acute appendicitis: a protocol for a multicentre randomised clinical trial (APPAC II trial). BMC Surg. 2018;18(1):117. doi: 10.1186/s12893-018-0451-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agency for Healthcare Research and Quality . Healthcare Cost and Utilization Project databases. Published 2021. Accessed March 14, 2022. http://www.hcup-us.ahrq.gov/nisoverview.jsp
- 8.Balentine CJ, Naik AD, Robinson CN, et al. Association of high-volume hospitals with greater likelihood of discharge to home following colorectal surgery. JAMA Surg. 2014;149(3):244-251. doi: 10.1001/jamasurg.2013.3838 [DOI] [PubMed] [Google Scholar]
- 9.Balentine CJ, Mason MC, Richardson PJ, et al. Variation in postacute care utilization after complex surgery. J Surg Res. 2018;230:61-70. doi: 10.1016/j.jss.2018.04.052 [DOI] [PubMed] [Google Scholar]
- 10.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. doi: 10.1097/00005650-199801000-00004 [DOI] [PubMed] [Google Scholar]
- 11.Austin PC. The performance of different propensity-score methods for estimating differences in proportions (risk differences or absolute risk reductions) in observational studies. Stat Med. 2010;29(20):2137-2148. doi: 10.1002/sim.3854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Orsini N, Bellocco N, Bottai M, Wolk A, Greenland S. A tool for deterministic and probabilistic sensitivity analysis of epidemiologic studies. Stata J. 2008;8(1)29-48. doi: 10.1177/1536867X0800800103 [DOI] [Google Scholar]
- 13.Lash TL, Fox MP, Fink AK. Applying Quantitatice Bias Analysis to Epidemiologic Data. Springer; 2009. [Google Scholar]
- 14.Smith LH, VanderWeele TJ. Bounding bias due to selection. Epidemiology. 2019;30(4):509-516. doi: 10.1097/EDE.0000000000001032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268-274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 16.Weesie J. Seemingly unrelated estimation. Stata Manual; 2013. [Google Scholar]
- 17.Weesie J. Seemingly unrelated estimation and the cluster-adjusted sandwich estimator. ResearchGate . Accessed May 20, 2022. https://www.researchgate.net/publication/24137472_Seemingly_unrelated_estimation_and_the_cluster-adjusted_sandwich_estimator [Google Scholar]
- 18.Yang Z, Sun F, Ai S, Wang J, Guan W, Liu S. Meta-analysis of studies comparing conservative treatment with antibiotics and appendectomy for acute appendicitis in the adult. BMC Surg. 2019;19(1):110. doi: 10.1186/s12893-019-0578-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Podda M, Cillara N, Di Saverio S, et al. ; ACOI (Italian Society of Hospital Surgeons) Study Group on Acute Appendicitis . Antibiotics-first strategy for uncomplicated acute appendicitis in adults is associated with increased rates of peritonitis at surgery. a systematic review with meta-analysis of randomized controlled trials comparing appendectomy and non-operative management with antibiotics. Surgeon. 2017;15(5):303-314. doi: 10.1016/j.surge.2017.02.001 [DOI] [PubMed] [Google Scholar]
- 20.Vons C, Barry C, Maitre S, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011;377(9777):1573-1579. doi: 10.1016/S0140-6736(11)60410-8 [DOI] [PubMed] [Google Scholar]
- 21.Styrud J, Eriksson S, Nilsson I, et al. Appendectomy versus antibiotic treatment in acute appendicitis. a prospective multicenter randomized controlled trial. World J Surg. 2006;30(6):1033-1037. doi: 10.1007/s00268-005-0304-6 [DOI] [PubMed] [Google Scholar]
- 22.Ando T, Oka T, Oshima G, et al. Fecalith in the proximal area of the appendix is a predictor of failure of nonoperative treatment for complicated appendicitis in adults. J Surg Res. 2021;267:477-484. doi: 10.1016/j.jss.2021.06.015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. A probabilistic sensitivity analysis - nonoperative management of acute appendicitis and complications
eFigure 2. A probabilistic sensitivity analysis - nonoperative management of acute appendicitis and mortality
eMethods. STROBE Statement—checklist of items that should be included in reports of observational studies
eResults. Full results from the sensitivity analysis
eTable 1. Standardized Differences and post-adjustment weights for the cohort following balancing using the propensity score
eTable 2. Unadjusted patient characteristics
eTable 3. Bivariate results of outcomes
Data sharing statement