Abstract
Aim
To quantitatively synthesize the correlation between posttraumatic growth and resilience among breast cancer patients and explore the potential moderators affecting the relation.
Design
A meta‐analysis of cross‐sectional studies.
Methods
This meta‐analysis followed the Preferred Reporting Items for Systematic Review and Meta‐Analyses 2020 guidelines. This meta‐analysis was carried out by searching Chinese and English databases of China National Knowledge Infrastructure, WANFANG DATA, Chongqing VIP Information Co., Ltd., PubMed, Embase, Web of Science, and PsycINFO from inception to February 25, 2022. Pooled Pearson's correlation coefficients between posttraumatic growth and resilience was calculated by the Stata software (version 17.0) using the random effects model.
Results
Seventeen studies including 4156 breast cancer patients were identified. A high positive correlation was found between posttraumatic growth and resilience (r = 0.448, 95% CI: 0.370–0.519, p < 0.001), and region and publication type significantly moderated the relation.
Keywords: breast cancer, meta‐analysis, posttraumatic growth, resilience, review
1. INTRODUCTION
As early as 2020, the International Agency for Research on Cancer stated in a report that breast cancer has officially replaced lung cancer as the number one cancer in the world (Sung et al., 2021). National cancer centre in February 2022 reported that female malignant tumours showed the highest incidence rate among breast cancer, with about 43,000 new cases (Xia et al., 2022). Although the global five‐year survival rate of people with breast cancer after diagnosis is >70% (Maajani et al., 2019), a breast cancer diagnosis and its associated treatment can strongly effect people's mental health, prompting stress and arousing a series of negative psychological responses, such as anxiety (Perez‐Tejada et al., 2021), depression (Kim & Park, 2021), fear of recurrence (Soriano et al., 2021), and trauma post‐stress disorder (Yan et al., 2021). However, some studies have informed that cancer patients often experience positive psychological changes as their cancer develops, known as posttraumatic growth (PTG) (Hamama‐Raz et al., 2019; Mostarac & Brajković, 2021). And evidence signifies that PTG is relatively common in people with breast cancer (Faustova, 2020; Karimzadeh et al., 2021). Meanwhile, research have discovered that resilience is a critical factor affecting PTG among breast cancer patients (Cai & Shi, 2015; Li et al., 2019; Shi et al., 2022). But the magnitude of the relationship between PTG and resilience in people with breast cancer is still in literature a controversial topic.
1.1. Background
In the beginning, coined by Tedeschi and Calhoun (1996), PTG is defined as the positive psychological changes that an individual can perceive in their struggle with a traumatic incident (Tedeschi & Calhoun, 2004). Unlike responses to tiny or everyday pressure sources and normal growth and developmental processes (Linley & Joseph, 2004), PTG is a person's efforts to control the effect of trauma on their lives and attempts to cope with their experiences and their consequences (Hirooka et al., 2017; Tedeschi & Calhoun, 2004). It usually was assessed by the Posttraumatic Growth Inventory (PTGI) (Tedeschi & Calhoun, 1996), which includes the five dimensions of new possibilities, relating to others, spiritual change, personal strength, and appreciation of life and comprises 21 items scored on a six‐point Likert‐type scale, with high scores indicating positive growth. Meanwhile, some Chinese scholars have localized this scale and formed different versions of this scale. For example, Dong et al. (2013) retained the contents of the original scale to the greatest extent, with 21 items in the Chinese version PTGI (PTGI‐21); Geng et al. (2011) and Wang et al. (2011) deleted item 18 of the original scale, and there were 20 items in the Chinese version PTGI (PTGI‐20); Lu et al. (2015) deleted the dimension of spiritual change in the original scale, and the Chinese version PTGI has 19 items in total (PTGI‐19).
Resilience, as a structure which is different from but associated to PTG, is usually delimited as an individual's well‐adjusted process in the face of trauma, adversity, tragedy, threat, or other major pressure stress, or a person's ability to bounce back after experiencing difficulties (VanMeter & Cicchetti, 2020). As a feature, it mainly was regarded as a bunch of individual traits, such as hardiness, optimism, high self‐esteem, and positive effect, which enables persons to deal with and be suit for challenges which menace their survival, function, or future development (Connor & Davidson, 2003). And some researchers have developed some instruments to measure the degree of resilience. Generally, resilience usually is surveyed by the Connor‐Davidson Resilience Scale (CD‐RISC) (Connor & Davidson, 2003), which includes the three dimensions of strength, tenacity, and optimism and comprises 25 items scored on a five‐point Likert‐type scale. High scores show the high degree of psychological resilience. Meanwhile, it was translated and revised by Yu and Zhang (2007). Subsequently, Campbell‐Sills and Stein (2007) extracted 10 entries from the CD‐RISC to form a simplified version of CD‐RISC (CD‐RISC‐10), which consists of 10 items scored on a four‐point Likert scale. Equally, the 14 items Resilience Scale (RS‐14) is also widely applied to survey the degree of resilience (Wagnild, 2009). It is composed of two dimensions of personal ability and acceptance of self and life, a total of 14 items rated on a five‐point Likert‐type scale. The higher the score, the higher the level of resilience. It has been translated and revised by many countries, such as China (Tian & Hong, 2013), Italy (Cuoco et al., 2021), Poland (Surzykiewicz et al., 2018), etc.
Although many studies have investigated the link between PTG and resilience in people with breast cancer, the PTG–resilience association is controversial. First, from the perspective of concept, Tedeschi and Calhoun (2004) believed that, unlike the superficially similar concept of resilience, PTG had a quality of transformation or a qualitative change in functioning. Second, Hobfoll et al. (2007) conceptualized PTG in terms of action‐centred growth, and equated growth with resilience, or argued that it was superior to the consequences of resilience. Third, Westphal and Bonanno (2007) placed PTG in a broader framework of individual differences in response to potential trauma, argued however, that many if not most people are resilient in the face of trauma and that resilient outcomes typically give little need or opportunity for PTG. Fourth, cross‐sectional results on the relationship between PTG and resilience in people with breast cancer are mixed. For example, some researchers found that there was a strong link between PTG and resilience (r = 0.572, 0.748, 0.650) (Jia et al., 2015; Shi et al., 2019; Yan et al., 2019); some scholars' studies found a moderate connection between PTG and resilience (r = 0.381, 0.379, 0.301) (Ding, 2020; Li, 2019; Wang et al., 2017); Lu (2014) and Zhang (2021) both found that there was a low relation between resilience and PTG (r = 0.249, 0.157); Darabos et al., (2021) found that there was no association between PTG and resilience among cancer patients. Therefore, the first aim of our meta‐analysis was to investigate the magnitude of the relationship between PTG and resilience in people with breast cancer.
Meanwhile, we also examined whether the connection between PTG and resilience in people with breast cancer might be due to the influence of potential moderators such as age, cancer stage, region, publication type, resilience measurement tools, and PTG measurement tools. First, previous studies have identified that younger breast cancer survivors experience a deeper impact from cancer, reporting greater emotional distress than older survivors (Bártolo et al., 2020; Kroenke et al., 2004). According to the psychological theory proposed by Janoff‐Bulman (2006), with the increase in psychological stress, they tend to feel that their level of adaptation to the disease becomes worse and avoid treatment (Borgi et al., 2020), which is detrimental to PTG. Hence, the relationship between PTG and resilience in people with breast cancer may vary depending on the age. Second, region may confound the association between PTG and resilience. Due to the socioeconomic disparities in different areas of China, the eastern region has better healthcare and social sources compared with the central and northeastern regions (Wang et al., 2022). Breast cancer patients in the eastern region may be more likely to receive medical and social support, and thus are more resourceful to cope with stress and achieve optimal adjustment than those in other areas. Therefore, the correlation between PTG and resilience may vary based on the region. Third, in general, researches with interesting findings are often easier to be published, so published journal articles may magnify the real relation between variables (Sterne et al., 2000). To this end, we included dissertations that were not officially published in journals and divided the publication types into two categories, journal and dissertation, to examine the moderating effect of publication type on the relationship between PTG and resilience. Fourth, considering that the dimensions and items of each resilience measurement tool are different, then we believed that resilience measurement could be a factor that adjust the correlation between PTG and resilience in breast cancer patients. Finally, considering the measurement of PTG, since it forms scales with different items after its sinicization, and at the same time, there are differences in dimensions, therefore, it may be a moderating factor affecting the relationship between PTG and resilience.
2. THE REVIEW
2.1. Aims
The objective of this study was to quantitatively synthesize the correlation between PTG and resilience among people with breast cancer and explore the potential moderators affecting the relation.
2.2. Design
The meta‐analysis was carried out and written based on the Preferred Reporting Items for Systematic Review and Meta‐Analyses (PRISMA) 2020 guidelines (Page et al., 2021), from searching articles, extracting results and describing the systematic processes. Moreover, the protocol has been registered in PROSPERO (ID: CRD42022313866).
2.3. Search methods
Seven databases were searched by us for studies on the correlation between PTG and resilience in people with breast cancer published from inception to February 25, 2022: China National Knowledge Infrastructure (CNKI), WANFANG DATA, Chongqing VIP Information Co., Ltd. (VIP), PubMed, Embase, Web of Science, and PsycINFO. The search string comprised three elements: (a) breast cancer, (b) posttraumatic growth, and (c) resilience. For the Chinese databases, the search terms included “breast cancer” OR “breast tumour” AND “posttraumatic growth” OR “stress‐related growth” OR “benefit finding” AND “resilience” OR “mental resilience” OR “mental toughness” OR “mental vulnerability”. For the English databases, the search strategy in PubMed could be seen in Appendix A.
2.4. Search criteria
Two reviewers screened independently all the literature records by following the selection criteria for possibly eligible articles: (1) the study design was a cross‐sectional survey; (2) it reported either Pearson's product–moment coefficients r or t, β, χ2 and F values which could be transformed into r values.; (3) there was no restriction on posttraumatic growth scale and resilience scale; (4) participants were diagnosed with breast cancer; (5) it was written in Chinese or English; (6) it excluded the conference abstracts; (7) it also excluded the studies with low quality or obvious data mistakes; and (8) when multiple publications came from the same dataset, we employed the one published in the journal, if the journal articles did not involve the intact dataset yet, we employed the primitive dissertation with an analysis of the full dataset.
2.5. Quality appraisal
The methodological quality of all researches was evaluated all alone by two reviewers by using the 9‐item Joanna Briggs Institution Critical Appraisal Checklist (Munn et al., 2015). The criteria for the cross‐sectional study included 9 items. The 9 assessment items are as follows: (1) Was the sample frame appropriate to address the target population? (2) Were study participants sampled in an appropriate way? (3) Was the sample size adequate? (4) Were the study subjects and the setting described in detail? (5) Was the data analysis conducted with sufficient coverage of the identified sample? (6) Were valid methods used for the identification of the condition? (7) Was the condition measured in a standard, reliable way for all participants? (8) Was there appropriate statistical analysis? (9) Was the response rate adequate, and if not, was the low response rate managed appropriately? “Yes”, “No”, “Unclear” and “Not Applicable” were the answer options for each item, with 1 point for “Yes” and 0 points for the rest. Higher scores reported better methodological quality. Furthermore, we resolved doubts or disagreements that arise in the quality assessment of the literature by focusing discussions (among at least three persons) or by asking for third‐party expert's opinions.
2.6. Data extraction
Two reviewers independently picked up data using a purpose‐designed form, and discrepancy arising from the extraction process were addressed by discussion. We coded the collected studies for the following traits: author information, publication year, region, publication type, participant characteristics, sample size, the Pearson's association coefficients between PTG and resilience, instruments applied to survey the level of resilience, and instruments applied to survey the degree of PTG. The principles of coding are as follows: first, if studies did not report correlation coefficients r but reported F, t, χ2, and β values, according to corresponding formula, they were transformed to r values: r=, r=, and r=, r = β × 0.98 + 0.05 (β ≥ 0); r = β × 0.98–0.05 (β < 0) [−0.5 < β < 0.5] (Card, 2012). Second, effect sizes were extracted using independent samples, with each independent sample being coded once. In case that multiple effect sizes were acquired for resilience and PTG in the identical sample, we only selected the total effect size.
2.7. Synthesis
We calculated the pooled Pearson's correlation coefficients and their corresponding 95% confidence intervals (CIs) between PTG and resilience by using the inverse variance method (Moles, 2009). Specifically, we transformed Fisher's z to r, weighted in view of the sample size with 95% confidence intervals (CIs): Z = 0.5*ln [(1 + r)/(1− r)]. Among them, VZ = 1/n − 3 is the variance of Z, and SEZ = square root of (1/n − 3) is the standard deviation of Z. As suggested by Lipsey and Wilson (2001), effect size r values of 0.10, 0.25, and 0.40 correspond to low, moderate, and high correlations, respectively. Moreover, we applied Cochran's Q and I 2 statistics to appraise the heterogeneity across researches (Higgins et al., 2003). The between‐study heterogeneity was statistically interesting when p < 0.05 or I 2 > 75%. Then, we would use the random effects model to compute the summary Pearson's association coefficient. Else, we would apply the fixed effects model.
Meanwhile, a large degree of heterogeneity suggested potential moderation effects (Lipsey & Wilson, 2000). The moderating effect analysis involved two forms. (1) When the moderating variable was a continuous variable, we used meta‐regression analysis to check whether the result was significant. (2) When the moderating variable was a categorical variable, we used subgroup analysis to test whether the result was significant. Furthermore, to assess the impact of personal studies on the summary association coefficients, and to examine the stability of the correlation between PTG and resilience, we carried on a sensitivity analysis by sequentially removing one research for each turn. Funnel plots were employed to detect possible publication bias. Besides, Egger's linear regression test was performed to help us to pass judgement for publication bias (Egger, 1997). All statistical analyses were carried on using Stata software (version 17.0).
3. RESULTS
3.1. Study characteristics and quality appraisal
We retrieved initially a total of 223 articles. Subsequently, through moving duplicates, the search produced 164 studies. By reading the titles and abstracts, we excluded a total of 136 studies. We then evaluated the full text of 28 studies for eligibility and eventually included 17 studies (see Figure 1 for the flow chart on the studies selection process). Table 1 summarized the features of the involved studies. A total of 17 cross‐sectional surveys with 4156 participants were contained, all from articles published after 2014. The survey sample size scoped from 78 to 789 participants. All the articles were derived from China. The results of the quality appraisal are shown in Table 1. We considered all involved researches were of medium to high quality (total score ≥6).
FIGURE 1.
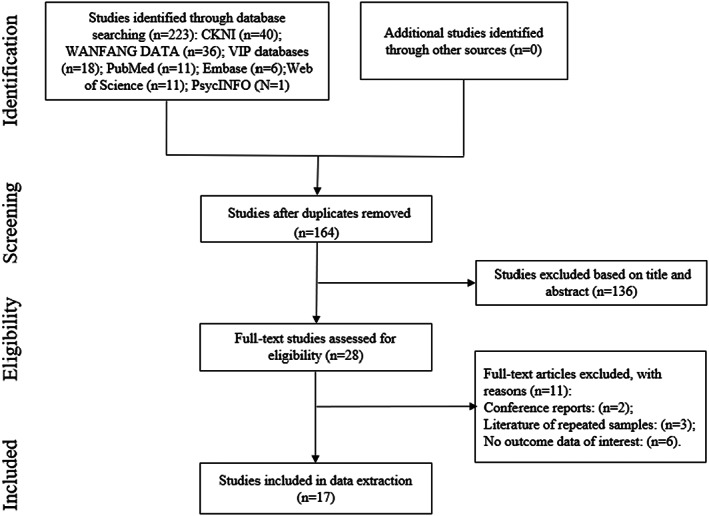
Flow chart of the study selection process
TABLE 1.
Characteristics of the 17 studies included in the meta‐analysis
| Study author (year) | Region | Publication type | Mean age | r | N | Resilience measurement | PTG measurement | JBI score |
|---|---|---|---|---|---|---|---|---|
| Lu, 2014 | Northeastern | Dissertation | 50.47 | 0.249 | 159 | CD‐RISC | PTGI‐19 | 8 |
| Cai & Shi, 2015 | Northeastern | Journal | 50.75 | 0.383 | 101 | CD‐RISC | PTGI‐20 | 7 |
| Jia et al., 2016 | Eastern | Journal | 46.78 | 0.572 | 303 | CD‐RISC | PTGI‐20 | 9 |
| Lei et al., 2017 | Eastern | Journal | 46.78 | 0.434 | 350 | CD‐RISC | PTGI‐20 | 8 |
| Wang et al., 2017 | Eastern | Journal | 43.2 | 0.381 | 120 | CD‐RISC | PTGI‐21 | 7 |
| Liu et al., 2018 | N/A | Journal | 49 | 0.350 | 108 | FRAS‐C | PTGI‐SF | 7 |
| Yu et al., 2018 | Eastern | Journal | N/A | 0.491 | 302 | CD‐RISC‐10 | PTGI‐20 | 8 |
| Li, 2019 | Central | Dissertation | N/A | 0.379 | 244 | CD‐RISC | PTGI‐21 | 8 |
| Li et al., 2019 | Central | Journal | N/A | 0.386 | 224 | CD‐RISC | PTGI‐21 | 9 |
| Shi et al., 2019 | Eastern | Journal | N/A | 0.748 | 160 | RS‐14 | PTGI‐21 | 6 |
| Yan et al., 2019 | Eastern | Journal | 49.91 | 0.650 | 180 | CD‐RISC | PTGI‐21 | 8 |
| Ding, 2020 | Eastern | Journal | N/A | 0.301 | 299 | CD‐RISC‐10 | PTGI‐20 | 7 |
| Geng et al., 2020 | Eastern | Journal | 49.16 | 0.491 | 302 | CD‐RISC‐10 | PTGI‐20 | 8 |
| Zhu & Liu, 2020 | Central | Journal | 41.28 | 0.502 | 78 | RS‐14 | PTGI‐21 | 8 |
| Tu et al., 2020 | Eastern | Journal | 51.54 | 0.610 | 201 | CD‐RISC | PTGI‐21 | 7 |
| Zhang, 2021 | Central | Dissertation | 47 | 0.157 | 236 | CD‐RISC | PTGI‐20 | 8 |
| Shi et al., 2022 | Northeastern | Journal | 53.28 | 0.307 | 789 | RS‐14 | PTGI‐21 | 8 |
Note: N/A=Not reported.
Abbreviations: CD‐RISC, Connor‐Davidson Resilience Scale; FRAS‐C, Shortened Chinese Version of the Family Resilience Assessment Scale; CD‐RISC‐10, Simplified CD‐RISC was compiled by Campbell‐Sills; RS‐14, 14‐item Resilience Scale; PTGI‐21, Posttraumatic Growth Inventory. PTGI‐19, 19‐items PTGI; PTGI‐20, 20‐items PTGI; PTGI‐SF, Short Form of the Posttraumatic Growth Inventory.
3.2. Pooled analyses
As demonstrated in Figure 2 and Table 2, the homogeneity test for 17 single samples revealed significant heterogeneity in the selected studies (Q = 139.13; p < 0.001; I 2 = 88.5%) and likely moderation effects, so we employed a random‐effects model. The random‐effects model indicated a significant association of 0.448 (95% CI: 0.370–0.519) between PTG and resilience. In addition, the association between resilience and PTG was steady, as demonstrated by the Z value of 10.171 and p < 0.001.
FIGURE 2.
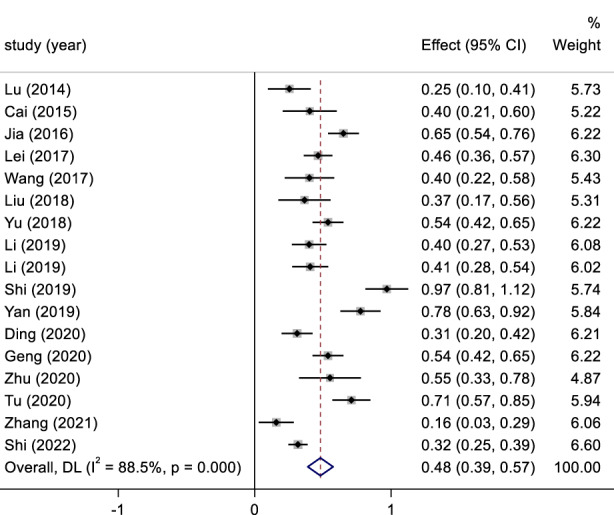
Forest plots for the correlation between posttraumatic growth and resilience
TABLE 2.
Random‐model of the correlation between PTG and resilience
| K | N | Mean r effect size | 95% CI for r | Homogeneity test | Test of null (two tailed) | |||
|---|---|---|---|---|---|---|---|---|
| Q(r) | p | I 2 | Z‐value | p | ||||
| 17 | 4156 | 0.448 | [0.370, 0.519] | 139.13 | 0.00 | 88.5% | 10.171 | <0.001 |
3.3. Moderating effect test
In this study, the moderating effect of four variables was tested: participant's age, region, publication type, and tool for measuring resilience and PTG (Tables 3 and 4). Subgroup analysis signalled that region and publication type significantly adjusted the correlation between PTG and resilience in people with breast cancer (Table 3). However, resilience measurement and PTG measurement did not moderate the correlation between resilience and PTG (QB = 0.41; df = 2, p > 0.05; QB = 1.14; df = 1, p > 0.05). Meanwhile, meta‐regression analysis showed that the moderating effects of age on PTG and resilience were not significant (p > 0.05).
TABLE 3.
Subgroup analysis of the summary correlation between PTG and resilience
| Between‐group effect (QB) | K | N | Mean r effect size | 95% CI for r | Homogeneity test within each group (QW) | I 2 (%) | |
|---|---|---|---|---|---|---|---|
| Region | 15.87*** | ||||||
| Northeastern | 3 | 1,049 | 0.306 | [0.250, 0.360] | 1.35 | 0.0 | |
| Eastern | 9 | 2,217 | 0.531 | [0.439, 0.613] | 65.87*** | 87.9 | |
| Central | 4 | 782 | 0.350 | [0.212, 0.475] | 12.88** | 76.7 | |
| Publication type | 8.02** | ||||||
| Journal | 14 | 3,517 | 0.484 | [0.404, 0.556] | 107.19*** | 87.9 | |
| Dissertation | 3 | 639 | 0.265 | [0.124, 0.396] | 6.94* | 71.2 | |
| Resilience measurement | 0.41 | ||||||
| CD‐RISC | 10 | 2,118 | 0.433 | [0.329, 0.527] | 70.55*** | 87.2 | |
| CD‐RISC‐10 | 3 | 903 | 0.432 | [0.304, 0.544] | 10.18** | 80.4 | |
| RS‐14 | 3 | 1,027 | 0.544 | [0.170, 0.781] | 56.60*** | 96.5 | |
| PTG measurement | 1.14 | ||||||
| PTGI‐21 | 8 | 1996 | 0.510 | [0.377, 0.623] | 87.94*** | 92.0 | |
| PTGI‐20 | 7 | 1893 | 0.414 | [0.307, 0.510] | 42.48*** | 85.9 |
Abbreviations: CD‐RISC, Connor‐Davidson Resilience Scale; CD‐RISC‐10, Simplified CD‐RISC was compiled by Campbell‐Sills; RS‐14, 14‐item Resilience Scale; PTGI‐21, Posttraumatic Growth Inventory. PTGI‐20, 20‐items PTGI.
*p < 0 .05, **p < 0.01, ***p < 0.001.
TABLE 4.
Univariate regression analysis of age (random effects model)
| Variables | K | B | SE | 95%CI | t | p |
|---|---|---|---|---|---|---|
| Age | 12 | −0.002 | 0.018 | [−0.041, 0.038] | −0.09 | 0.929 |
Region significantly regulated the link between PTG and resilience (QB = 15.87, df = 2, p < 0.001). Specifically, the positive relation between PTG and resilience was the highest in Eastern China (r = 0.531, 95% CI: 0.439–0.613), smaller in Central China (r = 0.350, 95% CI: 0.212–0.475)and the smallest in Northeastern China (r = 0.306, 95% CI: 0.250–0.360).
Publication type significantly adjusted the relationship between PTG and resilience (QB = 8.02, df = 1, p < 0.01). The positive correlation between PTG and resilience was larger in journal articles (r = 0.484, 95% CI: 0.404–0.556) than in dissertations (r = 0.265, 95% CI: 0.124–0.396).
3.4. Sensitivity analysis
To assess the stability of our findings, we conducted a sensitivity analysis by sequentially moving one single research for each turn and then recomputing the summary association coefficients. The sensitivity analysis for the summary association coefficients between PTG and resilience indicated tiny changes, suggesting that our results were steady (see Figure 3).
FIGURE 3.
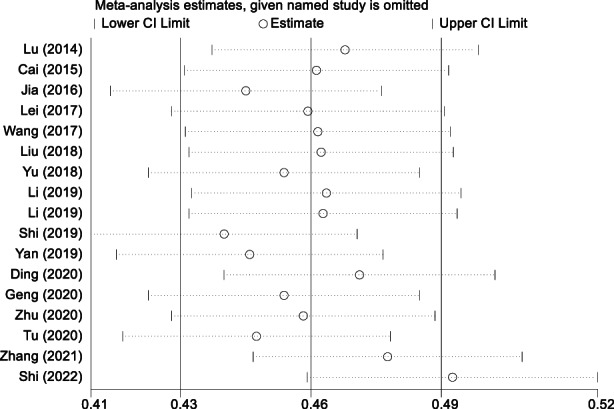
Sensitivity analyses of the 17 studies included in the meta‐analysis
3.5. Publication bias
The funnel plot demonstrated that the 17 effect sizes of the connection between PTG and resilience of people with breast cancer were basically evenly released on both sides of the overall effect sizes, implying no publication bias (see Figure 4). Besides, Egger's linear regression exhibited no significant bias (t17 = 1.16, p = 0.263) (see Figure 5). This finding suggested that the overall connection between PTG and resilience was stable in this study.
FIGURE 4.
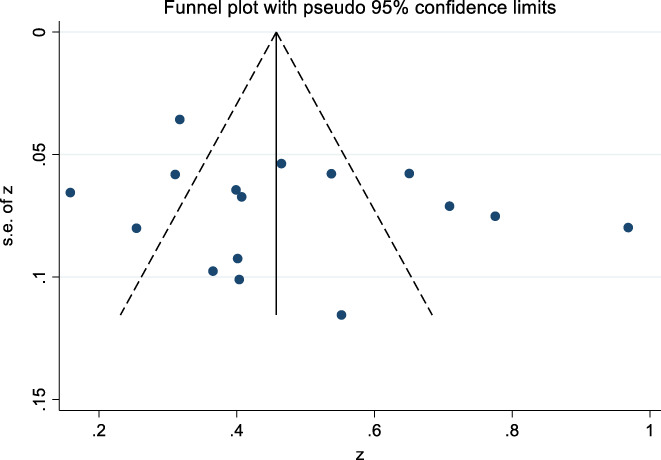
Funnel plot of the association of posttraumatic growth and resilience
FIGURE 5.
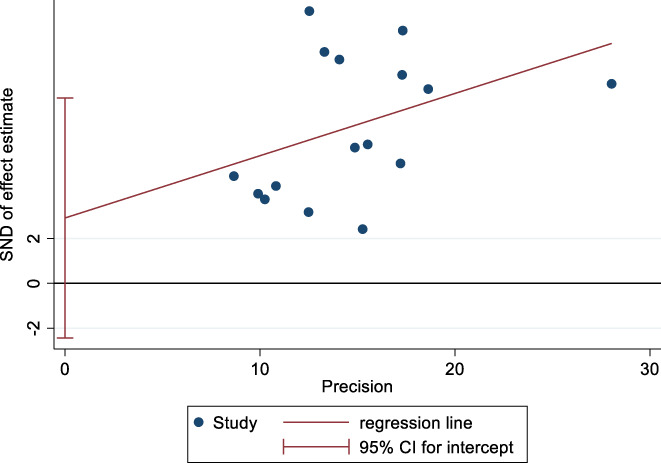
Egger's test of the 17 studies included in the meta‐analysis
4. DISCUSSION
4.1. The relationship between MPA and resilience
As far as we know, it was the first meta‐analysis to explore the pooled correlation coefficients of PTG with resilience in people with breast cancer. Our meta‐analysis indicated that resilience had a high degree of positive connection with PTG in people with breast cancer, which was consistent with the findings of most researchers on the relation between breast cancer patients' PTG and resilience (Geng et al., 2020; Lei et al., 2017; Zhu & Liu, 2020). This result suggests that good psychological resilience can help patients make full use of their higher positive and optimistic cognition and emotional regulation to cope effectively after suffering from cancer events, and promote patients' psychological recovery and better self‐growth (Lei et al., 2017). At the same time, this result also shows that for breast cancer patients, it is possible to promote PTG by improving their psychological resilience. First of all, families and caregivers should understand and care for patients more, help them eliminate bad emotions, and face disease treatment with a good attitude (Zhu & Liu, 2020). Second, when working, medical staff should not only focus on the patient's physical recovery but also pay attention to the patient's psychological state and PTG level (Romeo et al., 2017). For maladaptive patients, they should give psychological comfort and counselling in time to help patients establish a positive and optimistic attitude and cognition, enabling patients to better adapt to physical changes and integrate into society more quickly. Third, the government can encourage professional medical institutions to hold regular lectures and symposiums to increase the ways for patients to seek psychological counselling.
4.2. Moderation effects
4.2.1. The moderating role of age
Meta‐regression revealed that the moderating effect of age on the relationship between PTG and resilience in people with breast cancer was not significant, which was not consistent with the result of a previous study (Boyle et al., 2017). The reason for this result might be that the majority of the study population we included were middle‐aged breast cancer patients, with a small age span. Hence, the relationship between the two was not significantly different. Additionally, cancer is a serious threat to individuals at all ages. Meanwhile, some authors have suggested that individual stress from cancer also stimulates individuals to adapt to the disease and gain growth (Pascoe & Edvardsson, 2013; Rankin et al., 2020). Therefore, it may lead less variation in the relationship between PTG and resilience.
4.2.2. The moderating role of region
According to the results of the subgroup analysis, region had a moderating effect on the relation between PTG and resilience in people with breast cancer, which was consistent with our previous hypothesis. We found that the positive correlation between PTG and resilience was the highest in Eastern China, smaller in Central China, and the smallest in Northeastern China. The reason for this phenomenon may be, compared with Northeastern China and Central China, Eastern China has the most developed economy. The more developed the economy, people's life pressure is relatively greater, and breast cancer patients need to play a good role as parents, children, and other identities while enduring physical pain, they are under greater pressure. And previous studies have shown that excessive stress is not conducive to the individual's ability to adjust and adapt (Borgi et al., 2020; Ye et al., 2020), which in turn is not conducive to PTG, thus, it may cause the differences in the relation between PTG and resilience in people with breast cancer in these regions.
4.2.3. The moderating role of publication type
In general, studies with significant findings are more easily to be published, thereby exaggerating the true relationship between variables. To reduce publication bias, meta‐analyses should include unpublished studies (Sterne et al., 2000). In our study, we found that publication type also had a significant adjusting effect on the relation between resilience and PTG in people with breast cancer. The correlation coefficients between breast cancer patients' PTG and resilience reported in different types of researches were different, and the level of association reported in journal articles was higher than that informed in dissertations. On the one hand, this difference may be correlated to the quality of the studies and the rigour of the review. On the other hand, since the number of dissertations included is much smaller than the number of journal articles, this may also have some influence on the results of this research.
4.2.4. The moderating role of resilience measurement
However, our study showed that although between PTG and resilience was the highest in using the RS‐14, smaller in using the CD‐RISC‐10, and the smallest in using the CD‐RISC, the difference was not significant. The reason for this result may be that although the dimensions of the three resilience measurement tools are different and the number of measurement questions is also different, they all have high reliability and validity (the Cronbach a coefficient of the CD‐RISC, CD‐RISC‐10, and RS‐14 are 0.910, 0.928, and 0.776, respectively) (Campbell‐Sills & Stein, 2007; Connor & Davidson, 2003; Wagnild, 2009), all of which can truly measure the level of psychological resilience. In addition, due to the multidimensional structure of the resilience scale, the relationship between different dimensions of resilience and PTG among people with breast cancer can be further explored in the future.
4.2.5. The moderating role of PTG measurement
Meanwhile, our study also showed that the tools for measuring PTG did not significantly moderate the relation between PTG and resilience among people with breast cancer. This may be because although the content and length of the PTGI‐21 and the PTGI‐20 are slightly different, they both refer to the PTGI standard, so all of their content basically covers the important parts of PTG (Dong et al., 2013; Geng et al., 2011; Tedeschi & Calhoun, 1996; Wang et al., 2011), such as new possibilities, related to others, personal strength, appreciation for life, and spiritual change. Therefore, the effect of the relationship between PTG and resilience was not significantly different. Furthermore, to ensure the accuracy and stability of the results when analysing the moderating effect of the measurement tool in this study, for the subgroup analysis, we excluded subgroups with a single effect size. Therefore, it remains to be further confirmed in the future whether the relation between PTG and resilience in breast cancer patients is affected by the use of less personal testing tools.
4.3. Limitations and prospects
Unlike previous studies on the relationship between PTG and resilience in people with breast cancer, this study adopted the method of meta‐analysis to investigate the relation between breast cancer patients' PTG and resilience, clarifying the controversy about the magnitude of the correlation between them in empirical studies. However, this study still has some limitations. First, in view of the limited number of the involved researches, subgroup analysis based on some moderating variables should be explained with caution to some degree, at the same time, in the future, more empirical studies can be selected to further probe the relation between PTG and resilience among breast cancer patients. Second, since the included studies were all Chinese samples, due to the uniqueness of the Chinese economy, culture, and history, whether these results are applicable to other countries requires further investigation. Third, this study focused on the influence of certain moderator variables on the relationship between breast cancer patients' PTG and resilience. Other potential moderator variables, such as type of surgery, and time since diagnosis, should also be analysed in the future.
5. CONCLUSION
Although the limitations referred above, all available evidence stands by the high correlation between PTG and resilience. The summary Pearson's correlation coefficient was 0.448. This meant that people with breast cancer with the high level of resilience were more likely to have PTG. And region and publication type moderated the positive correlation between PTG and resilience, while age, resilience measurement, and PTG measurement did not play a role in regulating both. In the future, more empirical researches can be selected to further quest the connection between PTG and resilience among people with breast cancer.
6. IMPACT
This meta‐analysis gives solid evidence that there was a high positive connection between PTG and resilience among people with breast cancer. This also reminds medical staff that they should pay more attention to the psychological state of people with breast cancer in their work, find out the psychological problems of patients in time and help them solve them, so as to encourage patients to face life positively and optimistically.
AUTHOR CONTRIBUTIONS
Conceptualization: XW and HH; Methodology: XW and HH.; Software: QP, YZ, and YD; Validation: HW, JW, and GL; Formal Analysis: XW and HH; Data Curation: XW; Writing – Original Draft Preparation: XW and HH; Writing – Review & Editing: XW, Nancy XY and CC; Supervision: GL and CC; Project Administration: CC; Funding Acquisition: CC.
FUNDING INFORMATION
This work was supported by Henan graduate education reform and quality improvement project (Grant NO. YJS2021AL074); Henan University Undergraduate teaching reform Research and Practice Key projects (Grant NO. HDXJJG2020‐25); Henan ProvinceFederation of Social Science Circles Investigation Topic: “Henan Youth Research on the Current Situation of Social and Emotional Competence and the Cultivation Mechanism” (Grant NO. SKL‐2022‐55).
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICAL APPROVAL
This article does not contain studies involving human participants performed by any of the authors.
DISCLOSURE
Haitao Huang was the co‐first author.
ACKNOWLEDGEMENTS
The authors would like to thank all the participants of the study.
APPENDIX A. The search strategy in PubMed
#1 Search: “Breast Neoplasms”[Mesh] Sort by: Most Recent
#2 Search: ((((((((((((((((((((((((((((((((((((Breast Neoplasm[Title/Abstract]) OR (Neoplasm, Breast[Title/Abstract])) OR (Neoplasms, Breast[Title/Abstract])) OR (Breast Tumour[Title/Abstract])) OR (Breast Tumours[Title/Abstract])) OR (Tumour, Breast[Title/Abstract])) OR (Tumours, Breast[Title/Abstract])) OR (Breast Cancer[Title/Abstract])) OR (Cancer, Breast[Title/Abstract])) OR (Mammary Cancer[Title/Abstract])) OR (Mammary Cancers[Title/Abstract])) OR (Cancer, Mammary[Title/Abstract])) OR (Cancers, Mammary[Title/Abstract])) OR (Malignant Neoplasm of Breast[Title/Abstract])) OR (Breast Malignant Neoplasm[Title/Abstract])) OR (Breast Malignant Neoplasms[Title/Abstract])) OR (Malignant Tumour of Breast[Title/Abstract])) OR (Breast Malignant Tumour[Title/Abstract])) OR (Breast Malignant Tumours[Title/Abstract])) OR (Cancer of Breast[Title/Abstract])) OR (Cancer of the Breast[Title/Abstract])) OR (Mammary Carcinoma, Human[Title/Abstract])) OR (Mammary Carcinomas, Human[Title/Abstract])) OR (Carcinoma, Human Mammary[Title/Abstract])) OR (Carcinomas, Human Mammary[Title/Abstract])) OR (Human Mammary Carcinoma[Title/Abstract])) OR (Human Mammary Carcinomas[Title/Abstract])) OR (Mammary Neoplasm, Human[Title/Abstract])) OR (Mammary Neoplasms, Human[Title/Abstract])) OR (Human Mammary Neoplasm[Title/Abstract])) OR (Human Mammary Neoplasms[Title/Abstract])) OR (Neoplasm, Human Mammary[Title/Abstract])) OR (Neoplasms, Human Mammary[Title/Abstract])) OR (Breast Carcinoma[Title/Abstract])) OR (Breast Carcinomas[Title/Abstract])) OR (Carcinoma, Breast[Title/Abstract])) OR (Carcinomas, Breast[Title/Abstract])
#3 Search: #1 OR #2
#4 Search: “Posttraumatic Growth, Psychological”[Mesh] Sort by: Most Recent
#5 Search: ((((((((Growth, Psychological Posttraumatic[Title/Abstract]) OR (Psychological Posttraumatic Growth[Title/Abstract])) OR (Post‐traumatic Growth, Psychological[Title/Abstract])) OR (Growth, Psychological Post‐traumatic[Title/Abstract])) OR (Post traumatic Growth, Psychological[Title/Abstract])) OR (Psychological Post‐traumatic Growth[Title/Abstract])) OR (Psychological Post‐traumatic Growths[Title/Abstract])) OR (Posttraumatic Growth[Title/Abstract])) OR (Growth, Posttraumatic[Title/Abstract])
#6 Search: #4 OR #5
#7 Search: “ Resilience, Psychological “[Mesh] Sort by: Most Recent
#8 Search: ((Psychological Resilience [Title/Abstract]) OR (Resiliency, Psychological [Title/Abstract])) OR (Psychological Resiliency [Title/Abstract])
#9 Search: #7 OR #8
#10 Search: #3 AND #6 AND #9
Wan, X. , Huang, H. , Peng, Q. , Yu, N. X. , Zhang, Y. , Ding, Y. , Wu, H. , Hao, J. , Lu, G. , & Chen, C. (2023). A meta‐analysis on the relationship between posttraumatic growth and resilience in people with breast cancer. Nursing Open, 10, 2734–2745. 10.1002/nop2.1540
Contributor Information
Guangli Lu, Email: kfwangli0915@126.com.
Chaoran Chen, Email: kfccr@126.com.
DATA AVAILABILITY STATEMENT
The data that support the findings of the study are available from the corresponding author upon reasonable request.
REFERENCES
- Bártolo, A. , Neves, M. , Carvalho, B. , Reis, S. , Valério, E. , Santos, I. M. , & Monteiro, S. (2020). Fertility under uncertainty: Exploring differences in fertility‐related concerns and psychosocial aspects between breast cancer survivors and non‐cancer infertile women. Breast Cancer, 27(6), 1177–1186. 10.1007/s12282-020-01124-w [DOI] [PubMed] [Google Scholar]
- Borgi, M. , Collacchi, B. , Ortona, E. , & Cirulli, F. (2020). Stress and coping in women with breast cancer:Unravelling the mechanisms to improve resilience. Neuroscience and Biobehavioral Reviews, 119, 406–421. 10.1016/j.neubiorev.2020.10.011 [DOI] [PubMed] [Google Scholar]
- Boyle, C. C. , Stanton, A. L. , Ganz, P. A. , & Bower, J. E. (2017). Posttraumatic growth in breast cancer survivors: Does age matter? Psycho‐Oncology, 26, 800–807. 10.1002/pon.4091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai, Y. , & Shi, T. (2015). Correlation ananlysis between posttraumatic growth and resilience in patients with breast cancer after surgery. Chinese Nursing Research, 29(35), 4409–4411. 10.3760/cma.j.issn.1672-7088.2015.16.001 [DOI] [Google Scholar]
- Campbell‐Sills, L. , & Stein, M. B. (2007). Psychometric analysis and refinement of the Connor‐davidson resilience scale (CD‐RISC): Validation of a 10‐item measure of resilience. Journal of Traumatic Stress, 20(6), 1019–1028. 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- Card, N. A. (2012). Applied Meta‐Analysis for Social Science Research: Applied Meta‐Analysis for Social Science Research.
- Connor, K. M. , & Davidson, J. R. (2003). Development of a new resilience scale: The connor‐davidson resilience scale (CD‐RISC). Depression and Anxiety, 18(2), 76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Cuoco, S. , Carotenuto, I. , Cappiello, A. , Bisogno, R. , Picillo, M. , Pellecchia, M. T. , Barone, P. , & Erro, R. (2021). Reliability and validity of the novel Italian version of the 14‐item resilience scale (RS‐14) in adults. Neurological Sciences, 1–9, 3079–3087. 10.1007/s10072-021-05784-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darabos, K. , Renna, M. E. , Wang, A. W. , Zimmermann, C. F. , & Hoyt, M. A. (2021). Emotional approach coping among young adults with cancer: Relationships with psychological distress, posttraumatic growth, and resilience. Psychooncology, 30(5), 728–735. 10.1002/pon.5621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding, B. R. (2020). The mediating effect of resilience on posttraumatic growth and coping styles of breast cancer patients. Modern Nurse, 27(12), 41–44. 10.19791/j.cnki.1006-6411.2020.34.016 [DOI] [Google Scholar]
- Dong, L. , Hu, Y. , Xu, G. , & Huang, J. (2013). Reliability and validity of the Chinese version of post‐traumatic growth inventory scale in breast cancer survivors. Journal of Nursing Science, 28(22), 21–23. 10.3870/hlxzz.2013.22.021 [DOI] [Google Scholar]
- Egger, M. (1997). Bias in meta‐analysis detected by a simple, graphical test. BMJ (Clinical researched), 315(7109), 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faustova, A. G. (2020). Dataset on posttraumatic growth in women survived breast cancer. Data in Brief, 33, 106468. 10.1016/j.dib.2020.106468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geng, Q. , Zhang, P. , Cui, D. , Guo, Y. , Wang, B. , & Zhang, A. (2020). Mediating role of attention bias in posttraumatic growth and resilience of breast cancer patients. Nursing Science, 9(3), 209–215. 10.12677/NS.2020.93033 [DOI] [Google Scholar]
- Geng, Y. , Xu, Q. , Liu, H. , & Xu, X. (2011). Reliability and validity of the Chinese version of the post‐traumatic growth scale in survivors of multiple trauma. Chinese Journal of Nursing, 46(10), 1003–1005. 10.3761/j.issn.0254-1769.2011.10.023 [DOI] [Google Scholar]
- Hamama‐Raz, Y. , Pat‐Horenczyk, R. , Roziner, I. , Perry, S. , & Stemmer, S. M. (2019). Can posttraumatic growth after breast cancer promote positive coping?‐a cross‐lagged study. Psychooncology, 28(4), 767–774. 10.1002/pon.5017 [DOI] [PubMed] [Google Scholar]
- Higgins, J. , Thompson, S. G. , Decks, J. J. , & Altman, D. G. (2003). Measuring inconsistency in meta‐analyses. British Medical Journal, 327(7414), 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirooka, K. , Fukahori, H. , Ozawa, M. , & Akita, Y. (2017). Differences in posttraumatic growth and grief reactions among adolescents by relationship with the deceased. Journal of Advanced Nursing, 73(4), 955–965. 10.1111/jan.13196 [DOI] [PubMed] [Google Scholar]
- Hobfoll, S. E. , Hall, B. J. , Canetti‐Nisim, D. , Galea, S. , Johnson, R. J. , & Palmieri, P. A. (2007). Refining our understanding of traumatic growth in the face of terrorism: Moving from meaning cognitions to doing what is meaningful. Applied Psychology‐an International Review‐Psychologie Appliquee‐Revue Internationale, 56(3), 345–366. 10.1111/j.1464-0597.2007.00292.x [DOI] [Google Scholar]
- Janoff‐Bulman, R. (2006). Schema‐change perspectives on posttraumatic growth. In Calhoun L. G., & Tedeschi R. G. (Eds.), Handbook of posttraumatic growth: Research and practice. Erlbaum. [Google Scholar]
- Jia, X. , Cheng, L. , Yang, F. , Sun, Y. , & Liu, Y. (2015). Study on the relationship of post‐traumatic growth with self‐care efficacy and psychological resilience in patients with breast cancer. Chinese Journal of Practical Nursing, 31(36), 2742–2745. 10.3760/cma.j.issn.1672-7088.2015.36.003 [DOI] [Google Scholar]
- Karimzadeh, Y. , Rahimi, M. , Goodarzi, M. A. , Tahmasebi, S. , & Talei, A. (2021). Posttraumatic growth in women with breast cancer: Emotional regulation mediates satisfaction with basic needs and maladaptive schemas. European Journal of Psychotraumatology, 12(1), 1943871. 10.1080/20008198.2021.1943871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, K. , & Park, H. (2021). Factors affecting anxiety and depression in young breast cancer survivors undergoing radiotherapy. European Journal of Oncology Nursing, 50, 101898. 10.1016/j.ejon.2021.101898 [DOI] [PubMed] [Google Scholar]
- Kroenke, C. H. , Rosner, B. , Chen, W. Y. , Kawachi, I. , Colditz, G. A. , & Holmes, M. D. (2004). Functional impact of breast cancer by age at diagnosis. Journal of Clinical Oncology, 22, 1849–1856. 10.1200/JCO.2004.04.173 [DOI] [PubMed] [Google Scholar]
- Lei, P. , Gao, Y. , & Yang, F. (2017). Study on the relationship of post‐traumatic growth with self‐care efficacy and psychological resilience in patients with breast cancer. Modern Preventive Medicine, 44(13), 2392–2395 +2410. [Google Scholar]
- Li, L. , Kang, F. , Li, Z. , & Tian, W. (2019). Mediating effect of anxiety, depression and resilience on post‐traumatic growth of breast cancer patients. Chinese Nursing Research, 33(6), 960–965. 10.12102/j.issn.1009-6493.2019.06.011 [DOI] [Google Scholar]
- Li, L. B. (2019). A model study on the relationship between psychosomatic symptoms, resilience and post‐traumatic growth in patients with breast cancer during chemotherapy. (Master's dissertation, Shanxi Medical University. [Google Scholar]
- Linley, P. A. , & Joseph, S. (2004). Positive change following trauma and adversity: A review. Journal of Traumatic Stress, 17(1), 11–21. [DOI] [PubMed] [Google Scholar]
- Lipsey, M. W. , & Wilson, D. B. (2000). Practical Meta‐Analysis.
- Lipsey, M. W. , & Wilson, D. B. (2001). The way in which intervention studies have Ȝpersonality” and why it is important to meta‐analysis. Evaluation & The Health Professions, 24(3), 236–524. 10.1177/016327870102400302 [DOI] [PubMed] [Google Scholar]
- Liu, Y. , Li, Y. , Chen, L. , Li, Y. , Qi, W. , & Yu, L. (2018). Relationships between family resilience and posttraumatic growth in breast cancer survivors and caregiver burden. Psychooncology, 27(4), 1284–1290. 10.1002/pon.4668 [DOI] [PubMed] [Google Scholar]
- Lu, J. (2014). A pilot study of intervention to enhance posttraumatic growth for breast cancer based on exploring the related factors. (Master's dissertation, Dalian Medical University. [Google Scholar]
- Lu, J. , Shi, T. , & Li, H. (2015). Correlation of posttraumatic growth with psychological resilience, social support and self‐efficacy in breast cancer patients. Chinese Journal of Practical Nursing, 31(16), 1171–1174. 10.3760/cma.j.issn.1672-7088.2015.16.001 [DOI] [Google Scholar]
- Maajani, K. , Jalali, A. , Alipour, S. , Khodadost, M. , Tohidinik, H. R. , & Yazdani, K. (2019). The global and regional survival rate of women with breast cancer: A systematic review and meta‐analysis. Clinical Breast Cancer, 19(3), 165–177. 10.1016/j.clbc.2019.01.006 [DOI] [PubMed] [Google Scholar]
- Moles, D. (2009). Introduction to meta‐analysis. John Wiley & Sons, Inc. [Google Scholar]
- Mostarac, I. , & Brajković, L. (2021). Life after facing cancer: Posttraumatic growth, meaning in life and life satisfaction. Journal of Clinical Psychology in Medical Settings, 29, 92–102. 10.1007/s10880-021-09786-0 [DOI] [PubMed] [Google Scholar]
- Munn, Z. , Moola, S. , Lisy, K. , Riitano, D. , & Tufanaru, C. (2015). Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. International Journal of Evidence‐Based Healthcare, 13(3), 147–153. 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo‐Wilson, E. , McDonald, S. , … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe, L. , & Edvardsson, D. (2013). Benefit finding in cancer: A review of influencing factors and health outcomes. European Journal of Oncology Nursing, 17(6), 760–766. 10.1016/j.ejon.2013.03.005 [DOI] [PubMed] [Google Scholar]
- Perez‐Tejada, J. , Labaka, A. , Vegas, O. , Larraioz, A. , Pescador, A. , & Arregi, A. (2021). Anxiety and depression after breast cancer: The predictive role of monoamine levels. European Journal of Oncology Nursing, 52, 101953. 10.1016/j.ejon.2021.101953 [DOI] [PubMed] [Google Scholar]
- Rankin, K. , Le, D. , & Sweeny, K. (2020). Preemptively finding benefit in a breast cancer diagnosis. Psychology & Health, 35(5), 613–628. 10.1080/08870446.2019.1664740 [DOI] [PubMed] [Google Scholar]
- Romeo, A. , Ghiggia, A. , Tesio, V. , Di Tella, M. , Torta, R. , & Castelli, L. (2017). Post‐traumatic growth, distress and attachment style among women with breast cancer. Journal of Psychosocial Oncology, 35, 309–322. 10.1080/07347332.2017.1289291 [DOI] [PubMed] [Google Scholar]
- Shi, J. , Sznajder, K. K. , Liu, S. , Xie, X. , Yang, X. , & Zheng, Z. (2022). Resilience and posttraumatic growth of patients with breast cancer during the COVID‐19 pandemic in China: The mediating effect of recovery. Frontiers in Psychology, 12, 811078. 10.3389/fpsyg.2021.811078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, Y. , Zhuang, J. , Zhang, Q. , & Ma, L. (2019). The mediating effect of marital intimate relationship between psychological resilience and post‐traumatic growth for patients after breast cancer surgery. Journal of Qilu Nursing, 25(20), 16–19. [Google Scholar]
- Soriano, E. C. , Otto, A. K. , LoSavio, S. T. , Perndorfer, C. , Siegel, S. D. , & Laurenceau, J. P. (2021). Fear of cancer recurrence and inhibited disclosure: Testing the social‐cognitive processing model in couples coping with breast cancer. Annals of Behavioral Medicine, 55(3), 192–202. 10.1093/abm/kaaa043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne, J. , Gavaghan, D. , & Egger, M. (2000). Publication and related bias in meta‐analysis. Journal of Clinical Epidemiology, 53(11), 1119–1129. 10.1016/S0895-4356(00)00242-0 [DOI] [PubMed] [Google Scholar]
- Sung, H. , Ferlay, J. , Siegel, R. L. , Laversanne, M. , Soerjomataram, I. , Jemal, A. , & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3), 209–249. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- Surzykiewicz, J. , Konaszewski, K. , & Wagnild, G. (2018). Polish version of the resilience scale (RS‐14): A validity and reliability study in three samples. Frontiers in Psychology, 9, 2762. 10.3389/fpsyg.2018.02762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedeschi, R. G. , & Calhoun, L. G. (1996). The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. 10.1007/bf02103658 [DOI] [PubMed] [Google Scholar]
- Tedeschi, R. G. , & Calhoun, L. G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15(1), 1–18. 10.1207/s15327965pli1501_01 [DOI] [Google Scholar]
- Tian, J. , & Hong, J. S. (2013). Validation of the Chinese version of the resilience scale and its cutoff score for detecting low resilience in Chinese cancer patients. Support Care Cancer, 21(5), 1497–1502. 10.1007/s00520-012-1699-x [DOI] [PubMed] [Google Scholar]
- Tu, P. C. , Yeh, D. C. , & Hsieh, H. C. (2020). Positive psychological changes after breast cancer diagnosis and treatment: The role of trait resilience and coping styles. Journal of Psychosocial Oncology, 38(2), 156–170. 10.1080/07347332.2019.1649337 [DOI] [PubMed] [Google Scholar]
- VanMeter, F. , & Cicchetti, D. (2020). Resilience. Handbook of Clinical Neurology, 173, 67–73. 10.1016/b978-0-444-64150-2.00008-3 [DOI] [PubMed] [Google Scholar]
- Wagnild, G. (2009). A review of the resilience scale. Journal of Nursing Measurement, 17(2), 105–113. 10.1891/1061-3749.17.2.105 [DOI] [PubMed] [Google Scholar]
- Wang, J. , Chen, Y. , Wang, Y. , & Liu, X. (2011). Revision of the posttraumatic growth inventory and testing its reliability and validity. Journal of Nursing Science, 26(14), 26–28. 10.3870/hlxzz.2011.14.026 [DOI] [Google Scholar]
- Wang, L. , Chen, L. , & Li, Y. (2022). Digital economy and urban low‐carbon sustainable development: The role of innovation factor mobility in China. Environmental Science and Pollution Research International, 29(32), 48539–48557. 10.1007/s11356-022-19182-2 [DOI] [PubMed] [Google Scholar]
- Wang, Y. , Yuan, Y. , & Ge, M. (2017). Investigation and correlation study on posttraumatic growth, psychological resilience and quality of life of breast cancer patients. Journal of Qilu Nursing, 23(12), 26–28. [Google Scholar]
- Westphal, M. , & Bonanno, G. A. (2007). Posttraumatic growth and resilience to trauma: Different sides of the same coin or different coins? Applied Psychology‐an International Review‐Psychologie Appliquee‐Revue Internationale, 56(3), 417–427. 10.1111/j.1464-0597.2007.00298.x [DOI] [Google Scholar]
- Xia, C. , Dong, X. , Li, H. , Cao, M. , Sun, D. , He, S. , Yang, F. , Yan, X. , Zhang, S. , Li, N. , & Chen, W. (2022). Cancer statistics in China and United States, 2022: Profiles, trends, and determinants. Chinese Medical Journal, 135(5), 584–590. 10.1097/cm9.0000000000002108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan, H. , Xu, C. , Qi, M. , Zhang, S. , & Li, R. (2019). Correlation between post traumatic growth, social support and resilience in patients with breast cancer. Chinese Journal of Modern Nursing, 25(21), 2674–2679. [Google Scholar]
- Yan, Z. , Zhang, Q. , Chang, L. , Liu, Y. , & Li, Y. (2021). Dyadic effects of family resilience on post‐traumatic stress symptoms among breast cancer patients and their primary family caregivers: A cross‐sectional study. European Journal of Oncology Nursing, 53, 101998. 10.1016/j.ejon.2021.101998 [DOI] [PubMed] [Google Scholar]
- Ye, Z. , Yang, X. , Zeng, C. , Wang, Y. , Shen, Z. , Li, X. , & Lin, D. (2020). Resilience, social support, and coping as mediators between COVID‐19‐related stressful experiences and acute stress disorder among college students in China. Applied Psychology Health and Well‐Being, 12(4), 1074–1094. 10.1111/aphw.12211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, W. , Zhang, A. , Xia, S. , & Liu, H. (2018). Mediating role of resilience in posttraumatic growth and miserable emotion among breast cancer patients. Modern Preventive Medicine, 45(10), 1827–1831. [Google Scholar]
- Yu, X. , & Zhang, J. (2007). Factor analysis and psychometric evaluation of the Connor‐Davidson resilience scale (CD‐RISC) with Chinese people. Social Behavior and Personality, 35(1), 19–30. 10.2224/sbp.2007.35.1.19 [DOI] [Google Scholar]
- Zhang, X. M. (2021). Relationship between posttraumatic growth, psychological resilience, social support and molecular typing In breast cancer patients. (Master's dissertation, Bengbu Medical College). [Google Scholar]
- Zhu, J. , & Liu, Y. (2020). Analysis on positive psychological factors and their correlation in primary medical staff with breast cancer. Chinese Journal of Industrial Medicine, 33(02), 164–166. 10.13631/j.cnki.zggyyx.2020.02.022 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of the study are available from the corresponding author upon reasonable request.


