Abstract
Background
The Chicago Classification (CC) used to define esophageal motility disorders in high‐resolution manometry (HRM) has evolved over time. Our aim was to compare the frequency of motility disorders diagnosed with the last two versions (CCv3.0 and CCv4.0) and to evaluate symptoms severity according to the diagnoses.
Methods
From June to December 2020, patients who underwent esophageal HRM with swallows in supine and sitting positions were included. HRM studies were retrospectively analyzed using CCv3.0 and CCv4.0. Symptoms severity and quality of life were assessed with validated standardized questionnaires.
Key Results
Among the 130 patients included (73 women, mean age 52 years), motility disorder diagnoses remained unchanged in 102 patients (78%) with both CC. The 3 patients with esophago‐gastric junction outflow obstruction (EGJOO) with CCv3.0 were EGJOO, ineffective esophageal motility (IEM) and normal with CCv4.0. Twenty‐four out of 63 IEM diagnosed with the CCv3.0 (38%) turned into normal motility with the CCv4.0. Whatever the CC used, brief esophageal dysphagia questionnaire score was significantly higher in patients with EGJ relaxation disorders compared to those with IEM (25 (0–34) vs 0 (0–19), p = 0.01). Gastro‐Esophageal Reflux disease questionnaire (GERD‐Q) score was higher in patients with IEM with both CC compared to those who turned to normal with CCv4.0.
Conclusions and Inferences
While motility disorders diagnoses remained mainly unchanged with both CC, IEM was less frequent with CCv4.0 compared to CCv3.0. The higher GERD‐Q score in IEM patients with CCv4.0 suggests that CCv4.0 might identify IEM more likely associated with GERD.
Keywords: Chicago classification v4.0, dysphagia, esophageal motility disorders, high‐resolution manometry, ineffective esophageal motility, questionnaires
Applying the Chicago Classification v4.0 changed the diagnosis in 22% of patients but dysphagia score was still higher in patients with esophago‐gastric junction relaxation disorders compared to those with ineffective esophageal motility (IEM). The new definition of IEM might be more likely associated with gastro‐esophageal reflux disease.

Key points.
As expected, the application of the version 4 of the Chicago Classification did not change significantly the diagnosis of type I‐II achalasia, absent contractility, and distal esophageal spasm
Ineffective esophageal motility is less frequent with CCv4.0 compared to CCv3.0
Ineffective esophageal motility diagnosed with CCv4.0 might be more likely associated with gastro‐esophageal reflux disease
1. INTRODUCTION
Esophageal motility disorders might be responsible for symptoms such as dysphagia, regurgitation, or non‐cardiac chest pain. Upper gastro‐intestinal (GI) endoscopy with esophageal biopsies should be performed firstly in patients with esophageal symptoms in order to rule out obstructive disease and different causes of esophagitis (eosinophilic esophagitis, erosive reflux disease, pill or infectious esophagitis). If these examinations fail to explain symptoms, esophageal manometry is recommended to search for esophageal motility disorders. 1
High‐resolution manometry (HRM) is the gold standard to assess esophageal motility, and the Chicago Classification (CC) is used to define motility disorders. The first version of the Chicago Classification was published in 2009. 2 With the gain of clinical experience and growing publications over years, the CC was updated in 2012 and 2015 to become more clinically relevant. 3 , 4
With the version 3 of the CC (CCv3.0 published in 2015), the diagnosis of ineffective esophageal motility (IEM) was quite frequent and not always associated with symptoms. 4 The diagnosis of esophago‐gastric junction (EGJ) outflow obstruction with CCv3.0 was also questionable as many patients with this diagnosis have no obstructive symptoms and did not require any treatment. 5
These limitations were one of the reasons to propose a fourth version of the CC (CCv4.0). In this new iteration, a standard protocol was set up to improve technical consistency and diagnostic accuracy. Further, two major changes were made in the diagnostic criteria for IEM and EGJ outflow obstruction. 6 More than 70% ineffective swallows or at least 50% failed peristalsis in a context of normal integrated relaxation pressure (IRP) are required for the diagnosis of IEM in the CCv4.0 (vs more than 50% of ineffective swallows in the CCv3.0). Further, the diagnosis of EGJ outflow obstruction requires not only a median IRP above the upper limit of normal in both supine and sitting positions but also at least 20% of swallows with elevated intrabolus pressure (IBP) in supine position. Thus, diagnostic criteria becoming more stringent, we could expect a decreased frequency of IEM and EGJ outflow obstruction by applying the CCv4.0. These new diagnostic criteria could lead to more clinically relevant diagnosis compared to the CCv3.0.
The aim of the current study was to compare the frequency of motility disorders diagnosed with the last two versions of the Chicago Classification (CCv3.0 and CCv4.0) and to evaluate symptoms severity according to the motility disorders.
2. PATIENTS AND METHODS
2.1. Patients
Patients who underwent esophageal HRM in the Digestive Physiology department from June 2020 to December 2020 were retrospectively selected to participate to the study. Inclusion criteria were an age older than 18 years and a complete HRM protocol with 10 swallows in supine position and 5 in sitting position.
2.2. High‐resolution esophageal manometry protocol and analysis
Esophageal HRM was performed with ManoScan™ (Medtronic, Minneapolis MN). The manometry catheter was introduced transnasally within the esophagus. As proposed for the CCv4.0, the protocol consisted of a 30‐s baseline period (without swallowing) in the supine position, followed by ten 5‐ml swallows and two multiple rapid swallows (MRS) sequences (five 2‐ml swallows less than 2 s apart) in supine position. 6 Then, patient's position was changed to the sitting position and five 5‐ml swallows and a rapid drink challenge (RDC) test (200 ml water, ingested as fast as possible) were performed.
One single investigator (MS) retrospectively reviewed HRM studies with ManoView™ ESO v3.3 (Medtronic, Minneapolis, MN) and classified motility disorders according to the CCv3.0 and CCv4.0. Only swallows performed in supine position were analyzed to apply CCv3.0 while swallows performed in both supine and sitting positions were analyzed to apply CCv4.0. The CCv3.0 classified esophageal motility into 4 categories: EGJ relaxation disorders (achalasia and EGJ outflow obstruction), major disorders (absent contractility, distal esophageal spasm, and hypercontractile esophagus), minor disorders (IEM and fragmented peristalsis), and normal. 4 The CCv4.0 classified into 3 categories: EGJ disorders (achalasia and EGJ outflow obstruction), peristaltic disorders (absent contractility, distal esophageal spasm, hypercontractile esophagus, and IEM), and normal. 6 A contractile reserve was considered as present if the distal contractile integral of the contraction following the 5th swallow was augmented (compared to the mean DCI of the single swallows) for at least one of the MRS. Pan‐esophageal pressurization and esophageal shortening were analyzed during RDC. 7
2.3. Clinical data and questionnaires
Demographic data (age, body mass index [BMI], gender) and the indication of HRM were collected from patients' charts. When available, the results of upper GI endoscopy and esophageal pH ± impedance monitoring were noted.
Patients were requested to fill out questionnaires in the waiting room before HRM. The Gastro‐Esophageal Reflux Disease Questionnaire (GERD‐Q) was used to evaluate the presence and severity of GERD symptoms. 8 The Eckardt score usually used for patients with achalasia was systematically administrated to all patients referred for esophageal HRM to assess dysphagia and related symptoms and consequences. 9 Brief esophageal dysphagia questionnaire (BEDQ) and esophageal hypervigilance and anxiety scale (EHAS) recently validated in French were given to assess dysphagia frequency and severity and anxiety related to esophageal conditions, respectively. 10 , 11
2.4. Statistical analysis
Analyses were performed using IBM SPSS Statistics for Windows version 21.0 (IBM Corp., Armonk, N.Y.).
Continuous data were expressed as median (range) otherwise mentioned and categorical data as percentage. Non‐parametric tests (Mann–Whitney test and Kruskal–Wallis test) were used to compare continuous data, and chi 2 test was used to compare categorical data between the CCv3.0 and the CCv4.0. A p < 0.05 was considered significant.
3. RESULTS
3.1. Patients' characteristics
Among the 352 patients who underwent esophageal HRM within the study period, 132 fulfilled the inclusion criteria (73 women, mean age 52 years, range 17–89). The reason for exclusion was an incomplete manometry protocol in 220 patients (no swallow in sitting position). The manometry catheter did not pass through the EGJ in 2 patients, letting 130 patients for analysis. The characteristics of the 130 patients are summarized in Table 1.
TABLE 1.
Patients' characteristics
| Parameters | |
|---|---|
| Mean age (range) (years) | 52 (17–89) |
| Gender M/F n (%) | 57 (43)/73 (57) |
| Mean BMI (range) (kg/m2) | 25 (14–39) |
| Complete symptom questionnaire n (%) | 81 (62) |
| History of esophago‐gastric surgery n (%) | 17 (13) |
| Indications for manometry, n (%) | |
| Dysphagia | 45 (34) |
| Typical GERD symptoms | 59 (45) |
| Miscellaneous | 26 (20) |
Abbreviations: BMI, body mass index; GERD, gastro‐esophageal reflux disease.
3.2. Diagnoses according to the CCv3.0 and the CCv4.0
Diagnoses according to the CCv3.0 and the CCv4.0 are presented in Table 2. Using CCv3.0, 9 patients (7%) were diagnosed with EGJ relaxation disorders (achalasia or EGJ outflow obstruction), 7 (5%) with major motility disorders (6 absent contractility and 1 distal esophageal spasm), 63 (49%) with minor disorders (all of them were IEM) and 51 (39%) were normal. Using CCv4.0, 7 patients (5%) had EGJ relaxation disorders, 47 (36%) peristaltic disorders (6 absent contractility, 1 distal esophageal spasm, and 40 patients [85%] with IEM) and 76 (59%) were normal.
TABLE 2.
Diagnoses of motility disorders according to the Chicago Classification version 3.0 (CCv3.0) and version 4.0 (CCv4.0)
| CC v4.0 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Achalasia type I | Achalasia type II | Achalasia type III | EGJ outflow obstruction | Absent contraction | Distal Esophageal Spasm | IEM | Normal | Total | ||
| CC v3.0 | Achalasia I | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Achalasia II | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | |
| Achalasia III | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 2 | |
| EGJ outflow obstruction | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 3 | |
| Absent contraction | 0 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 6 | |
| Distal Esophageal Spasm | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | |
| IEM | 0 | 0 | 0 | 0 | 0 | 0 | 39 | 24 | 63 | |
| Normal | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 51 | 51 | |
| Total | 2 | 2 | 0 | 3 | 6 | 1 | 40 | 76 | 130 | |
Note: Discordances between the two classifications are highlighted in dark gray.
Bold values correspond to unchanged diagnosis with CCv3.0 and CCv4.0.
Abbreviations: EGJ, esophago‐gastric junction; IEM, ineffective esophageal motility.
Between the two classifications, the diagnosis remained unchanged in 102 patients (78%). In particular, the diagnoses of type I and type II achalasia, absent contractility, and distal esophageal spasm were not modified. The frequency of IEM was significantly reduced (49% of the studies with CCv3.0 vs 31% with CC v4.0, p < 0.01) and HRM was more likely normal with CCv4.0 compared to CCv3.0 (59% of normal studies vs 39%, p < 0.01).
Interestingly, the two patients with type III achalasia according to CCv3.0 turned into EGJ outflow obstruction when CCv4.0 was applied. The diagnosis change was related to the presence of a mix of premature and normal contractions in these patients (CCv4.0 requiring premature contractions alone or a mix of premature and absent contractions for the diagnosis of type III achalasia). These 2 patients had intermittent dysphagia. Timed barium swallow was recommended after HRM. However, none of them underwent this examination as dysphagia decreased spontaneously. Neither esophageal ultrasound endoscopy nor EndoFLIP™ were performed in these 2 patients.
Two of the three diagnoses of EGJ outflow obstruction with the CCv3.0 became normal or IEM with CCv4.0 because of a normal IRP in sitting position (the diagnosis of EGJ outflow obstruction with the CCv4.0 required elevated IRP in both supine and sitting positions). The patient who turned to normal motility had a moderate intermittent dysphagia (BEDQ score 19, Eckardt score 6) in a context of rheumatoid arthritis. Symptoms were finally related to temporo‐mandibular joint dysfunction and decreased with arthritis treatment. The patient who turned to IEM had regurgitation and heartburn but no dysphagia. He had grade B esophagitis on upper GI endoscopy. He was diagnosed with GERD. The patient with EGJ outflow obstruction on both CC was referred for regurgitation without heartburn. Upper GI endoscopy and barium swallow were normal as well as pH‐impedance monitoring off proton pump inhibitor. No EndFLIP™ was performed. Follow‐up data were not available for this patient.
Finally, among the 63 patients with IEM according to CCv3.0, 24 (38%) became normal with CCv4.0.
3.3. Questionnaires scores according to esophageal motility disorders
Whatever the version of the CC used, BEDQ score was significantly higher in patients with EGJ relaxation disorders (achalasia or EGJ outflow obstruction) compared to those with IEM (Table 3; Figures 1 and 2). This was also true for the group of patients with absent contractility or distal esophageal spasm compared to those with IEM and those with normal motility.
TABLE 3.
Symptomatic scores according to motility disorders diagnosed with the Chicago Classification version 3.0 (CCv3.0) and version v4.0 (CCv4.0)
| GERD‐Q | Eckardt score | BEDQ | EHAS | |
|---|---|---|---|---|
| Number of patients who completed the questionnaire | 81 | 76 | 75 | 77 |
| Motility disorders according to CC v3.0 | ||||
| EGJ disorders | 10 (6–12) | 6 (1–8)# | 22 (0–34)* | 31 (5–44) |
| Absent contractility/DES | 10 (4–15) | 4 (1–6) | 11 (10–37)*# | 23 (6–42) |
| IEM | 8 (3–16)# | 4 (0–9) | 1 (0–28) | 31 (0–60) |
| Normal | 7 (0–13) | 3 (0–11) | 3 (0–33) | 29 (6–55) |
| Motility disorders according to CC v4.0 | ||||
| EGJ disorders | 10 (6–12) | 7 (1–8) | 25 (0–34)*# | 32 (5–44) |
| Absent contractility/DES | 10 (4–15) | 4 (1–6) | 11 (10–37)*# | 23 (6–42) |
| IEM | 10 (6–16)# | 4 (1–9) | 0 (0–19) | 28 (8–45) |
| Normal | 7 (0–15) | 3 (0–11) | 3 (0–33) | 31 (0–60) |
Note: Data are expressed as median (range).
Abbreviations: EGJ, esophago‐gastric junction; DES, distal esophageal spasm; IEM, ineffective esophageal motility; GERD‐Q, gastro‐esophageal reflux disease questionnaire; BEDQ, brief esophageal dysphagia questionnaire; EHAS, esophageal hypervigilance and anxiety scale.
p < 0.05 vs IEM; #p < 0.05 vs normal.
FIGURE 1.
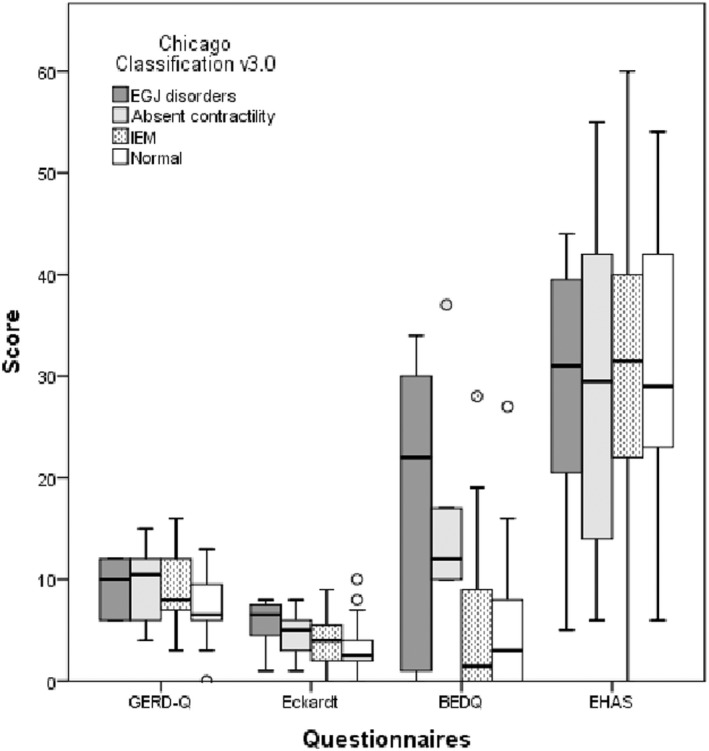
Box and Whisker plots for the 4 questionnaires scores (Gastro‐esophageal reflux disease questionnaire (GERD‐Q), Eckardt score, brief esophageal dysphagia questionnaire (BEDQ), Esophageal Hypervigilance and Anxiety Scale (EHAS)) and the motility disorders according to the Chicago Classification version 3.0 (CC v3.0) (esophago‐gastric junction (EGJ) disorders; absent contractility, ineffective esophageal motility (IEM) and normal motility). The center line denotes the median value while the box contains the 25th and 75th percentiles of the dataset. The whiskers mark the 5th and the 95th percentiles, and the dots are the outliers
FIGURE 2.
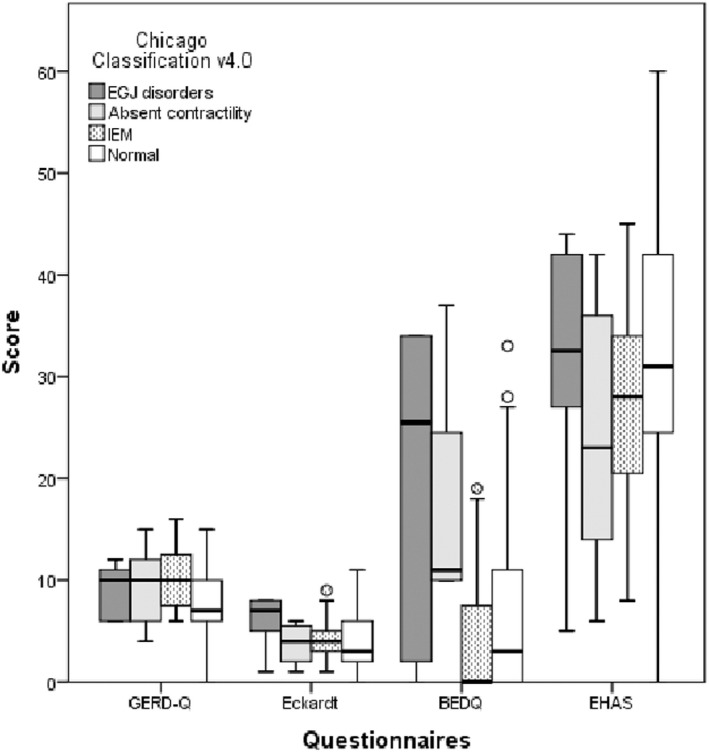
Box and Whisker plots for the 4 questionnaires scores (Gastro‐esophageal reflux disease questionnaire (GERD‐Q), Eckardt score, brief esophageal dysphagia questionnaire (BEDQ), Esophageal Hypervigilance and Anxiety Scale (EHAS)) and the motility disorders according to the Chicago Classification version 4.0 (CC v4.0) (esophago‐gastric junction (EGJ) disorders; absent contractility, ineffective esophageal motility (IEM), and normal motility). The center line denotes the median value while the box contains the 25th and 75th percentiles of the dataset. The whiskers mark the 5th and the 95th percentiles, and the dots are the outliers
Eckardt score was significantly higher in patients with EGJ relaxations disorders compared to those with normal motility only for CCv3.0.
EHAS score was never significantly different between the groups of motility disorders whatever the version of the CC.
GERD‐Q score was significantly higher in patients with IEM compared to those with normal motility in both versions of the CC.
3.4. Patients with IEM with the CC v3.0 and the CC v4.0
Among the 63 patients diagnosed with IEM according to CCv3.0, 39 (62%) were still classified as IEM according to CCv4.0 while 24 (38%) turned into normal. The GERD‐Q score was significantly higher in patients with IEM according to CCv4.0 compared to those who turned to normal (10 (6–16) vs 8 (3–15), p = 0.02) (Figure 3A). EHAS tended to be higher in patients who were normal with CCv4.0 compared to those who were diagnosed with IEM with both CC (38 (0–60) vs 28 (8–45), p = 0.06).
FIGURE 3.

Comparison of patients with ineffective esophageal motility (IEM) on both Chicago Classification (CC) (gray bars) and those with IEM on CCv3.0 and normal motility on CCv4.0 (white bars). Panel A represents Box and Whisker plots for the 4 questionnaires scores (Gastro‐esophageal reflux disease questionnaire (GERD‐Q), Eckardt score, Brief Esophageal Dysphagia Questionnaire (BEDQ), Esophageal Hypervigilance and Anxiety Scale (EHAS)). The center line denotes the median value while the box contains the 25th and 75th percentiles of the dataset. The whiskers mark the 5th and the 95th percentiles, and the dots are the outliers. Panel B represents the percentage of patients with pathological GERD diagnosed on upper gastro‐intestinal endoscopy and on pH‐(impedance) monitoring
A positive peristaltic response during MRS test (contractile reserve) was present in 30 out of 39 patients with IEM according to CCv4.0 (77%) and in all the 24 patients with IEM on CCv3.0 who became normal motility on CCv4.0 (p = 0.01).
Endoscopic data were available in 32 patients and reflux monitoring (pH +/− impedance monitoring) in 41 patients. The prevalence of erosive esophagitis was similar in IEM and normal motility according to CCv4.0 (p = 0.76) and pathological reflux was more likely diagnosed in IEM patients even if the difference was not statistically significant (p = 0.17) (Figure 3B).
3.5. Results of ajunct tests
Contractile inhibition was always present during MRS. Based on CCv4.0 criteria, all the 76 patients with normal HRM had a contractile reserve (100%) compared to 31 patients with IEM (30 IEM with CCv3.0 and 1 EGJ outflow obstruction with CCv3.0) (77%) and 3 patients with absent contractility (50%). In 2 patients with IEM on CCv4.0 and no contractile reserve, anti‐reflux surgery was contra‐indicated. Anti‐reflux surgery was performed in 2 patients with IEM and positive contractile reserve but not performed in 3 other patients with IEM and positive contractile reserve. Overall symptom scores were not different in patients with contractile reserve compared to those without.
Nine patients exhibited pan‐esophageal pressurization during RDC. According to CCv4.0, these patients were diagnosed as type I achalasia (n = 2; no pressurization at all for single swallows), type II achalasia (n = 2), EGJ outflow obstruction (n = 2, the 2 were type III achalasia with CCv3.0), distal esophageal spasm (n = 1), and normal (n = 2, 1 was EGJ outflow obstruction with CCv3.0 and 1 was also normal with CCv3.0). The patient with normal motility with both CC complained with intermittent dysphagia, no other abnormality was noted on HRM, upper GI endoscopy was normal but no esophageal biopsies were taken. Overall BEDQ score was significantly higher in patients with pan‐esophageal pressurization during RDC compared to those without (25 (2–34) vs 3 (0–37), p < 0.01). The other symptom scores were not different.
4. DISCUSSION
This study demonstrated that the use of the CCv4.0 instead of the CCv3.0 decreased significantly the frequency of IEM but did not affect the diagnosis of type I and type II achalasia, absent contractility, and distal esophageal spasm as expected. BEDQ score was higher in patients with EGJ disorders compared to those with IEM whatever the CC used. Finally, IEM diagnosed with the CCv4.0 criteria might be more likely associated with GERD symptoms than IEM defined with the CCv3.0 criteria, suggesting a more clinically relevant diagnosis with CCv4.0.
One goal of the new iteration of the CC was to refine motility disorders diagnoses to have disorders more likely associated with symptoms. The distribution of motility disorders was modified when CCv4.0 was applied but overall patients with EGJ relaxation disorders had higher BEDQ score whatever the CC used. However, due to a limited number of patients included in the study, the difference regarding BEDQ score among categories of motility disorders was not always statistically significant. This study is in line with the previous ones demonstrating the validity of BEDQ to depict significant esophageal motility disorders. 11 , 12 , 13
Overall only 2 patients out of 9 diagnosed with EGJ relaxation disorders (achalasia and EGJ outflow obstruction) with the CCv3.0 did not have an EGJ relaxation disorder with the CCv4.0. These 2 patients had an abnormal IRP only in supine position and instances of peristalsis (either normal or ineffective). Follow‐up data for these patients were in favor of an absence of clinically significant EGJ relaxation disorders and are an argument to justify the change of EGJ outflow obstruction definition. As expected applying CCv4.0 impacted also the diagnosis of type III achalasia but the 2 cases of type III achalasia with CCv3.0 remained in the group of patients with EGJ disorders with CCv4.0. Indeed these 2 cases turned into EGJ outflow obstruction with abnormal IRP in both supine and sitting positions and instances of normal esophageal peristalsis. Interestingly, these 2 patients improved over time without specific treatment. The third patient with EGJ outflow obstruction on CCv4.0 had EGJ outflow obstruction on CCv3.0 as well. Unfortunately, no follow‐up data were available for this patient. It is not possible to rule any conclusion regarding the yield of the refined definition of EGJ outflow obstruction due to the small number of patients and the low frequency of this diagnosis. Further, the CCv4.0 is more stringent for the diagnosis of type III achalasia resulting logically in a decreased frequency of type III achalasia. Type III achalasia was initially known to have worst outcome after treatment, 14 but the development of per oral endoscopic myotomy (POEM) changed this paradigm with similar response whatever the achalasia subtypes. 15 , 16 It remains to be determined if the CCv4.0 definition of type III achalasia will change patients' management.
Using CCv4.0 significantly decreased the number of patients diagnosed with IEM. More importantly, the current study suggests that the new definition of IEM might be more clinically relevant for GERD compared to the previous version. Indeed, patients with IEM tended to present more severe GERD symptoms as assessed by a higher GERD‐Q score in patients with IEM with both CC compared to those with IEM only with CCv3.0. This finding was supported by a higher percentage of pathological GERD on pH‐(impedance) monitoring in patients with persistent IEM compared to those who turned to normal (35% vs 13%) even if the difference was not statistically significant. Again this lack of significance might be related to the small sample size. These results are in line with the study of Rogers et al. demonstrating that the occurrence of more than 70% of ineffective swallows was more likely associated with abnormal reflux burden than the occurrence of at least 50% of ineffective swallows. 17
Interestingly, patients with IEM that turned into normal with the CCv4.0 tended to have a higher EHAS score than those with persistent IEM on CC v4.0. All these patients were referred for the work‐up of esophageal symptoms and the normality of HRM despite symptoms was in accordance with the diagnosis of functional symptoms. Recently, a Taiwanese study demonstrated that EHAS was associated with symptom severity and psychological stress but not with acid reflux burden or esophageal mucosal integrity. 18 The authors proposed to use EHAS to assess patient's outcome and satisfaction with a treatment. The elevation of EHAS score in patients with functional symptoms in the current study might be another reason to use EHAS for patients' evaluation.
One specificity of the CCv4.0 is to recommend the use of adjunct tests (MRS, RDC, solid swallows, etc.) to improve the diagnosis of esophageal motility disorders. MRS has 2 roles: identifying lack of inhibition and evaluating contractile reserve. We failed to observe any lack of inhibition, maybe because disorders associated with lack of inhibition (achalasia and DES) were rare in the current series. The presence of contractile reserve is of interest in patients with IEM referred for GERD as it might be associated with less dysphagia after anti‐reflux surgery compared to patients without contractile reserve. 19 Because of the lack of systematic follow‐up data, we cannot confirm the role of MRS. Only prospective studies could determine whether an absence of contractile reserve in a patient with IEM should contra‐indicate anti‐surgery. The second adjunct test, RDC, aims at identifying significant EGJ obstruction. Again our conclusions are impaired by the limited number of patients. Pan‐esophageal pressurization during RDC was observed in only 9 patients (7%) and was associated wither higher BEDQ score than in patients without pressurization. Seven of them were diagnosed as achalasia, EGJ outflow obstruction or DES based on the analysis of single swallows in supine and sitting position and the result of RDC did not change their management. In the 2 patients with normal motility, one with temporo‐mandibular joint dysfunction exhibited a resolution of dysphagia after treatment for rheumatoid arthritis and the other with mild dysphagia and normal upper GI endoscopy (without esophageal biopsies) was lost of follow‐up. Indeed, this small series is not powered to confirm the yield of adjunct tests. Overall in a random cohort of patients referred for esophageal HRM, the positivity of these tests might be not frequent. However, these tests are easy to perform and might be helpful in some instances. 19 , 20 Prospective studies might help to determine their role in patients' management.
Our study has several limitations. Firstly, it was a monocentric study with a limited number of patients. We cannot rule out a selection bias as well. The diagnoses of EGJ outflow obstruction and DES were rare, and no patient had hypercontractile esophagus in the current series. Then, it is not possible to conclude on the role of the new CC for the management of these patients. However, we observed a significant decrease of IEM as expected and an increase of normal HRM as a consequence. Secondly, questionnaires were not always completed by patients (62% of the patients filled the questionnaires vs 50% of the 220 patients excluded because of an incomplete HRM protocol). This low response rate is frequently observed in retrospective studies and might explain the lack of significance between groups. Despite that, BEDQ score was higher in patients with EGJ relaxation disorders compared to those with IEM.
In conclusion, EGJ relaxation disorders were associated with higher scores of dysphagia than IEM whatever the CC used. Due to the small number of patients, we cannot determine whether the new definition of EGJ outflow obstruction is able to identify patients who should benefit from treatment. Further studies with a large number of patients are required to address the yield of this definition for patients' management. Moreover, the current study confirmed that IEM was less frequently diagnosed with the CCv4.0 compared to the CCv3.0. Further studies are necessary to confirm that the CCv4.0 diagnosis of IEM is clinically relevant and a hallmark of GERD.
AUTHOR CONTRIBUTIONS
Performed the research: Morgane Sallette and Jamila Lenz; Designed the research study: Sabine Roman; Analyzed the data and wrote the paper: Morgane Sallette, François Mion, and Sabine Roman.
CONFLICT OF INTEREST
Morgane Sallette: nothing to declare. François Mion: consulting for Laborie. Jamila Lenz: support (conference attendance) from Celltrion. Sabine Roman: consulting for Dr Falk Pharma and Reckitt Benckiser; research support from Medtronic and Diversatek Healthcare.
Sallette M, Lenz J, Mion F, Roman S. From Chicago classification v3.0 to v4.0: Diagnostic changes and clinical implications. Neurogastroenterology & Motility. 2023;35:e14467. doi: 10.1111/nmo.14467
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Zerbib F, Omari T. Oesophageal dysphagia: manifestations and diagnosis. Nat Rev Gastroenterol Hepatol. 2014;12:322‐331. [DOI] [PubMed] [Google Scholar]
- 2. Pandolfino JE, Fox MR, Bredenoord AJ, Kahrilas PJ. High‐resolution manometry in clinical practice: utilizing pressure topography to classify oesophageal motility abnormalities. Neurogastroenterol Motil. 2009;21(8):796‐806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal esophageal pressure topography (EPT). Neurogastroenterol Motil. 2012;24(1):57‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160‐174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Biasutto D, Mion F, Garros A, Roman S. Rapid drink challenge test during esophageal high resolution manometry in patients with esophago‐gastric junction outflow obstruction. Neurogastroenterol Motil. 2018;30(6):e13293. [DOI] [PubMed] [Google Scholar]
- 6. Yadlapati R, Kahrilas PJ, Fox MR, et al. Esophageal motility disorders on high‐resolution manometry: Chicago classification version 4.0(©). Neurogastroenterol Motil. 2021;33(1):e14058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marin I, Cisternas D, Abrao L, et al. Normal values of esophageal pressure responses to a rapid drink challenge test in healthy subjects: results of a multicenter study. Neurogastroenterol Motil. 2017;29(6):e13021. [DOI] [PubMed] [Google Scholar]
- 8. Jones R, Junghard O, Dent J, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro‐oesophageal reflux disease in primary care. Aliment Pharmacol Ther. 2009;30(10):1030‐1038. [DOI] [PubMed] [Google Scholar]
- 9. Taft TH, Carlson DA, Triggs J, et al. Evaluating the reliability and construct validity of the Eckardt symptom score as a measure of achalasia severity. Neurogastroenterol Motil. 2018;30(6):e13287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roman S, Guadagnoli LA, Hastier A, et al. Validation of the French version of the esophageal hypervigilance and anxiety scale. Clin Res Hepatol Gastroenterol. 2021;45(2):101672. [DOI] [PubMed] [Google Scholar]
- 11. Roman S, Guadagnoli LA, Hastier A, et al. Validation in French of the brief esophageal dysphagia questionnaire in patients referred for esophageal manometry. Dysphagia. 2022;37(2):392‐398. [DOI] [PubMed] [Google Scholar]
- 12. Cisternas D, Taft T, Carlson DA, et al. Validation and psychometric evaluation of the Spanish version of brief esophageal dysphagia questionnaire (BEDQ): results of a multicentric study. Neurogastroenterol Motil. 2020;33:e14025. [DOI] [PubMed] [Google Scholar]
- 13. Carlson DA, Gyawali CP, Roman S, et al. Esophageal hypervigilance and visceral anxiety are contributors to symptom severity among patients evaluated with high‐resolution esophageal manometry. Am J Gastroenterol. 2020;115(3):367‐375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rohof WO, Boeckxstaens GE. Treatment of the patient with achalasia. Curr Opin Gastroenterol. 2012;28(4):389‐394. [DOI] [PubMed] [Google Scholar]
- 15. Ponds FA, Fockens P, Lei A, et al. Effect of peroral endoscopic myotomy vs pneumatic dilation on symptom severity and treatment outcomes among treatment‐naive patients with achalasia: a randomized clinical trial. Jama. 2019;322(2):134‐144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Werner YB, Hakanson B, Martinek J, et al. Endoscopic or surgical myotomy in patients with idiopathic achalasia. N Engl J Med. 2019;381(23):2219‐2229. [DOI] [PubMed] [Google Scholar]
- 17. Rogers BD, Rengarajan A, Mauro A, et al. Fragmented and failed swallows on esophageal high‐resolution manometry associate with abnormal reflux burden better than weak swallows. Neurogastroenterol Motil. 2020;32(2):e13736. [DOI] [PubMed] [Google Scholar]
- 18. Wong MW, Liu TT, Yi CH, et al. Oesophageal hypervigilance and visceral anxiety relate to reflux symptom severity and psychological distress but not to acid reflux parameters. Aliment Pharmacol Ther. 2021;54(7):923‐930. [DOI] [PubMed] [Google Scholar]
- 19. Hasak S, Brunt LM, Wang D, Gyawali CP. Clinical characteristics and outcomes of patients with Postfundoplication dysphagia. Clin Gastroenterol Hepatol. 2019;17(10):1982‐1990. [DOI] [PubMed] [Google Scholar]
- 20. Biasutto D, Roman S, Garros A, Mion F. Esophageal shortening after rapid drink test during esophageal high‐resolution manometry: a relevant finding? United European Gastroenterology Journal. 2018;6(9):1323‐1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


