Abstract
Background
Nursing home hospital avoidance programmes have contributed to a reduction in unnecessary emergency transfers but a description of the core components of the programmes has not been forthcoming. A well‐operationalised health‐care programme requires clarity around core components to evaluate and replicate the programme. Core components are the essential functions and principles that must be implemented to produce expected outcomes.
Objectives
To identify the core components of a nursing home hospital avoidance programme by assessing how the core components identified at one nursing home (Site One) translated to a second nursing home (Site Two).
Methods
Data collected during the programme's implementation at Site Two were reviewed for evidence of how the core components named at Site One were implemented at Site Two and to determine if any additional core components were evident. The preliminary updated core components were then shared with seven evaluators familiar with the hospital avoidance programme for consensus.
Results
The updated core components were agreed to include the following: Decision Support Tools, Advanced Clinical Skills Training, Specialist Clinical Support and Collaboration, Facility Policy and Procedures, Family and Care Recipient Education and Engagement, Culture of Staff Readiness, Supportive Executive and Facility Management.
Conclusion
This study launches a discussion on the need to identify hospital avoidance programme core components, while providing valuable insight into how Site One core programme components, such as resources, education and training, clinical and facility support, translated to Site Two, and why modifications and additions, such as incorporating the programme into facility policy, family education and executive support were necessary, and the ramifications of those changes. The next step is to take the eight core component categories and undertake a rigorous fidelity assessment as part of formal process evaluation where the components can be critiqued and measured across multiple nursing home sites. The core components can then be used as evidence‐based building blocks for developing, implementing and evaluating nursing home hospital avoidance programmes.
Keywords: aged, hospitals, nursing homes, process assessment, health care, skilled nursing facilities
SUMMARY STATEMENT OF IMPLICATIONS FOR PRACTICE.
What does this research add to existing knowledge of gerontology?
This research fills a gap in the literature by describing the core components of a nursing home hospital avoidance programme and their importance.
This research provides insight into how a nursing home programme was adapted to suit local culture at a second site and the impact this had on the programme's core components.
What are the implications of this new knowledge for nursing care with older people?
Attention and resources will be directed towards the core components of hospital avoidance programmes that are needed to successfully keep nursing home residents with deteriorating health out of the hospital.
Nursing home nurses will reimagine their roles and the level of care provided when an evidence‐based hospital avoidance programme is introduced.
How could the findings be used to influence policy or practice or research or education?
The findings will bring awareness to the importance of identifying the core components of a hospital avoidance programme, especially if the programme is to be available at different locations.
The findings will initiate a discussion and further research around the core components of a hospital avoidance programme.
The findings will provide a framework for replicating and comparing hospital avoidance programmes.
1. INTRODUCTION
Efforts to reduce hospital transfers from nursing homes has had some success. In the United States, where national initiatives to improve the quality of care and reduce unnecessary hospitalisations have been instituted, the number of transfers of nursing home residents with advanced illnesses have declined (McCarthy et al., 2020). Similar reductions in transfers have been recognised internationally (Graverholt et al., 2014), including Austria (Kada et al., 2017), Australia (Carter et al., 2020; Dai et al., 2021; Hullick et al., 2021; Testa et al., 2021). This is welcomed news because the hospital environment is not fully conducive to caring for older persons (Parke et al., 2014). Older persons often experience delirium (Marcantonio, 2017), pressure injuries (Dwyer et al., 2014), falls (Dolan et al., 2021) and nosocomial infections (Kaye et al., 2014) during hospitalisation that can lead to further medical complications (Creditor, 1993; Dwyer et al., 2014; Zisberg et al., 2015). In particular, physical activity, nutrition and continence care are often suboptimal, contributing to immediate and post‐hospitalisation functional decline in older persons (Zisberg et al., 2015). Medication‐related problems also arise during hospitalisation due to medication reconciliation issues and the prescribing of medications that are not suitable for older persons (Beers Criteria Update Expert Panel, 2019). The risks are well noted, and efforts are underway by organisations such as the Geriatric Emergency Department Collaborative (GEDC) to improve the quality of care provided to older persons in the emergency department and hospital settings (The Geriatric Emergency Department Collaborative, 2022).
Yet attention must still be made to avoiding unnecessary and inappropriate emergency hospital transfers from nursing homes in the first place (Lemoyne et al., 2019). Half of all nursing home residents are hospitalised at least once in the last year of life (Xing et al., 2013). Hospitalisation is costly. The Australian Medical Association (2021) estimated that during the first 6 months of 2021 there were over 27,000 possibly avoidable hospital admissions of persons from nursing homes, requiring approximately 160,00 hospital patient days for an estimated cost $AU 312 million. Some transfers can be avoided when programmes are in place that equip nursing staff with the skills and resources to identify and address risk factors (Hallgren et al., 2016) and provide a higher level of care (Trahan et al., 2016). Different models of care for hospital avoidance programmes have been developed to address the high rate of emergency room visits experienced by older persons from nursing homes. Hospital avoidance, subacute care (O'Neill et al., 2018), quality improvement and INTERACT (Ouslander et al., 2014) admission avoidance (Crilly et al., 2011) and INTERCARE (Zúñiga et al., 2019) are just some of the names given to these programmes that provide specific care pathways, training, diagnostic equipment and communication instruction to expedite early detection of deteriorating health and allow for care to be provided in the nursing home instead of the hospital. While these types of programmes all aim to reduce unnecessary hospital transfers and some have reported success, the extent to which the core components of these programmes are similar or differ is not well defined or understood, making comparisons between programmes with positive or negative outcomes difficult to assess. Core components are ‘the essential functions and principles that define the programme and are judged as being necessary to produce outcomes in a typical service setting and the associated elements and intervention activities’ (Blase & Fixsen, 2013, p.3).
A widely recognised and reported programme that aims to reduce unnecessary hospitalisations is the U.S. based Interventions to Reduce Acute Care Transfers INTERACT II quality improvement programme that trains and supports nursing home staff in early identification of health problems (Ouslander et al., 2014). The programme includes corporate and facility leadership education, nursing staff education, communication tools, care paths and advance care planning tools (Ouslander et al., 2014). Nursing homes that utilised INTERACT II reported up to a 24% reduction in hospitalisations (Ouslander et al., 2011). However, a later study involving 85 nursing homes determined that the training and support provided by the programme did not result in a statistically significant effect on transfers or hospitalisations (Kane et al., 2017). The authors questioned whether programme delivery differences across the different nursing homes may have been a factor and the extent of support and training may have been insufficient (Kane et al., 2017). This lack of consistency and interpretation of the delivery of the components are the reason why the core components of a hospital programme, and how they should be delivered, is needed to achieve the expected outcome of a reduction in unnecessary hospitalisations.
When a programme is introduced to reduce hospital transfers in a residential nursing home, a clear understanding of the core components will help to ensure limited and appropriate resources are properly allocated towards these items and outcomes accurately interpreted (Blase & Fixsen, 2013). If adaptations to the core components are made to suit the local context they need to be described and evaluated to determine if they have had either a positive or negative impact on the programme's success or effectiveness (Augustsson et al., 2015; Pérez et al., 2016). The evaluation may lead to amendments to the core components. Thus, identification of the core components has a wider application to not only an aid in comparing the programmes but in the development of best practices.
This article reports on an opportunity to formulate a list of the core components of a nursing‐home‐driven hospital avoidance programme by assessing how an initial list of core components identified at one nursing home (Site One) was translated to a second nursing home (Site Two).
1.1. Background on the Programme
In 2013, nursing and managerial staff at Site One, a 94‐bed nursing home in regional Queensland, Australia, with input from other healthcare professionals in the community, developed a pilot hospital avoidance programme named the Sub Acute Care Programme, which will be herewith referred to as the Programme. The nursing home managers identified a high number of hospital transfers were occurring and received funding to develop a model of care for delivering subacute care within the nursing home. Subacute care within the study setting was defined as a point when the resident requires ‘…more intensive treatments, interventions and frequent assessment for a complex condition that does not require hospitalisation’ (Dwyer et al., 2017). The Programme aimed to prevent potentially avoidable transfers of older persons to hospital and to decrease length of hospital stay for residents admitted. The Programme sought to achieve this by upskilling and empowering nursing staff with the required resources to detect and act upon signs of deteriorating health. The Programme employed a three‐step ‘traffic light’ system to detect, assess and treat common clinical conditions known to lead to hospitalisation of nursing home residents.
The Theory of Planned Behaviour served as the theoretical framework for the evaluation of the Programme and helped to gauge nursing staff response to the change in practice (Ajzen, 1991). After reviewing research on similar programmes and reflecting on their own experience, the Programme developers identified the core components of the programme prior to the Programme's launch. These core components are described in Table 1.
TABLE 1.
Site One Programme core components
| Initial Programme Core components | Operational description of the components |
|---|---|
| Decision support tools | RADD index™: A flip‐chart guide to help staff identify and proactively manage changes in a resident's condition related to eight conditions. |
| Resident Early Warning Observation chart: Resident observation chart, track and trigger tool for documenting vital signs | |
| SBAR (Situation, Background, Assessment, Recommendation) Communication tool | |
| Advanced Care Planning | |
| Clinical Management Guidelines: Urinary Tract Infection, chest pain, dyspnoea, constipation delirium, dehydration, falls, palliative care | |
| Advanced Clinical Policies & Procedures | |
| Advanced clinical skills training | Initial mandatory face‐to‐face workshops on: Sub Acute Programme, tools and resources, new equipment; and eight conditions that commonly lead to hospitalisation: urinary tract infection, chest pain, dyspnoea, constipation, delirium, dehydration, falls, palliative care |
| Specialist clinical support and collaboration | Access to clinical support from medical personnel Health Specialist In‐Reach team; Clinical lead Nurses; Nurse Practitioner; Geriatrician; Wound Specialist; Clinical Champions |
| Diagnostic medical equipment | Diagnostic equipment not typically found in nursing home setting that can be used to assess and manage clinical deterioration |
Outcome measures of the success of the Programme included pre‐ and post‐comparisons of medical record data on rates of hospital admissions, length of hospital stay, the number of residents receiving sub‐acute care and staff engagement. Subsequent to the introduction of the Programme at study Site One, there was a statistically significant increase in the frequency of subacute care delivered by nursing staff, and decreased number of hospital transfers and length of hospital stays (Parkinson et al., 2015). Data from focus group interviews indicated nursing staff believed that they benefitted from the structure and support provided by the Programme (O'Neill et al., 2017; Parkinson et al., 2015). The structure and support provided in the Programme helped nursing staff to detect signs of deterioration of the resident early and to respond appropriately (O'Neill et al., 2017). Nursing staff had a significantly more positive attitude towards early detection of deteriorating resident health and provision of sub‐acute care after the introduction of the Programme (O'Neill et al., 2018).
Given these successes, the Programme was subsequently implemented at a second affiliated nursing home (Site Two), with one objective being to evaluate how the core components of the Program were translated from one site to the next. During the first year after implementation of the Programme at Site Two, 112 sub‐acute episodes were recorded, hospital admissions were reduced by 19% and there was a 31% reduction in length of hospital stay (Carter et al., 2020). The Programme is currently being implemented and evaluated across 12 nursing homes as part of an Australian government initiative to reduce unnecessary hospitalisation of nursing home residents (Australian Government Department of Health, 2019). Given the evidence that the Programme has achieved the expected outcomes and to facilitate successful replication/scalability of the Programme at subsequent sites, confirmation of the core components is required.
Thus, the aim of this study was to clarify the core components of the Programme by examining the core components as they were translated from Site One to Site Two. Research questions asked were as follows:
What adaptations were made to the Site One core components?
Were the adaptations perceived to have a positive or negative impact?
Should any adaptations or additions be integrated into the core components?
1.2. Design
Identification of the core components was just one area of focus during the year‐long evaluation of the implementation of the Programme at Site Two. The researchers adopted a pragmatic action research approach that followed a Plan, Do, Study, Act cycle, which is an iterative four‐stage model used to guide implementation and evaluation of quality improvement initiatives in healthcare (Taylor et al., 2014). The research coordinator organised monthly meetings, and the data were collected from these meetings, as well as from interviews, reflections, training sessions and site visits that were undertaken throughout the year to discuss and review the implementation process. The frequent meetings and reviews of the process lead to actions being taken to further facilitate the Programme's integration into Site Two.
To further facilitate the implementation process and organise the data collected, the integrated version of the Promoting Action on Research Implementation in Health Services framework, referred to as the i‐PARIHS framework, was utilised (Harvey & Kitson, 2016). The theoretical antecedents of i‐PARIHS focus on what is being implemented, who is targeted, the characteristics of the implementation site and the implementation process itself (Harvey & Kitson, 2016).
1.3. Study setting and participants
Site One and Site Two are owned by the same regional not‐for‐profit aged care provider but are located in two geographically distant areas of regional Queensland, Australia. The differences between the two sites are outlined in Table 2. A key difference between the two sites was the availability of medical support. Site One had access to affiliated General Physicians (GPs) plus hospital‐based Nurse Practitioners (NPs) and eventually their own NP; while Site Two did not have this level of support and relied on GPs affiliated with the facility. Clinical lead nurses were assigned to provide clinical guidance around the Programme at both sites when the programme was introduced.
TABLE 2.
Demographic comparison of Site One and Site Two
| Features | Site One | Site Two |
|---|---|---|
| Community Population (2016) | 49,573 (Australian Bureau of Statistics, 2016) | 51,102 (Australian Bureau of Statistics, 2017) |
| Number of beds | 94 | 95 |
| Medical support providers | Residential Aged Care hospital outreach team comprising; hospital‐based nurse practitioners, General Practitioners serving nursing home population, a Nurse Practitioner on staff (midway through pilot introduction) | General Practitioners serving nursing home population. |
Abbreviations: AU, Australia; QLD, Queensland.
Participants in the overall implementation study included the members of the nursing home staff and external researchers. The researchers were invited by the manager to participate in the implementation of the Programme because of their research expertise and ability to provide an objective evaluation of the Programme. The participants' input is documented in the various data collected from the implementation team meetings, interviews, reflections and focus groups. The seven participants conducting the evaluation of the core components were purposefully chosen by the research coordinator because of their in‐depth knowledge of the implementation process and evaluation of the Programme at both sites and are referred to as the evaluators. The evaluators include three external researchers and four nursing home staff. Table 3 further describes the participants and their roles including the following: nursing home staff, involvement in the implementation process, serving as external researchers or evaluators and whether or not their input was collected during the implementation process and included in the data set.
TABLE 3.
Participant roles and credentials
| Credentials | Nursing home staff | Involved in implementation process | External researchers | Included in data set | Evaluator |
|---|---|---|---|---|---|
| PhD, RN | x | x | x | x | |
| PhD | x | x | x | x | |
| PhD, RN | x | x | x | x | |
| PhD Candidate, RN | x | x | x | ||
| Manager, RN | x | x | x | x | |
| Chief Clinical Officer, RN | x | x | x | x | |
| Facilities Manager, RN | x | x | x | x | |
| RN, NP | x | x | x | x | |
| PhD, Health economist | x | x | x | ||
| Clinical Nurse, RN | x | x | x | ||
| Clinical Nurse Manager, RN | x | x | x | ||
| Senior Research Fellow, Implementation Scientist, RN | x | x | x | ||
| Senior Research Fellow, Health Economics | x | x | x | ||
| Research Project Manager | x | x | x | ||
| Professor, Health Economics, PhD | x | x | x | ||
| Professorial Research Fellow, RN | x | x | x | ||
| 2 RNs, 3 ENs, 3AINs, 1 Speech clinician | x | x |
Abbreviations: AIN, Assistant in Nursing; EN, Enrolled nurse; NP, Nurse Practitioner; PhD, Doctor of Philosophy; RN, Registered Nurse.
1.4. Ethical considerations
The University Human Research Ethics Committee approved this research (H14/01–012). Participation was voluntary. Signed consent forms were obtained from the primary subjects and the evaluators.
2. MATERIALS AND METHODS
Data were collected over the course of one year during the implementation of the Programme at Site Two. Consistent with the pragmatic actions approach (Taylor et al., 2014), various modes of data were collected to document the implementation process. Table 4 describes the data collection methods from the implementation team meetings, participant interviews/focus groups, reflections and staff surveys that provided a rich history of the implementation process and the insight into how the Programme core components were translated to the second site.
TABLE 4.
Description of data collection methods
| Team meetings (n = 44) | Monthly team meetings were recorded and transcribed as a valuable source of project process information. All team meetings began with an open reflection on activities and progress report by all team members to capture important data. This data were used to guide the implementation process. The three teams were as follows: Health economics group, research group, implementation group |
| Participant interviews / focus groups (n = 17) |
Qualitative interviews were undertaken with external and internal facilitators, staff and resident family to identify past relevant experiences, and barriers and facilitators to the programme. Questions included: Who do you think is going to be most affected by (the Programme)? How do you think (the Programme) will fit into (this facility)? Who will most likely accept it? Resist? Will it require significant changes in the current system of delivery of care? Will it present a challenge to people's ways of thinking? Will it enhance the resident experience? Could it introduce greater efficiency in the provision of care? Who are the formal and informal leaders? Do they support the changes? Are they providing motivation and support? Do you think the current culture supports innovation and change? Why? What is your past experience of introducing changes? Any training in project implementation? What mechanisms are in place to support learning and embedding changes into routine practice? |
| Reflections (n = 6) | Similar to the team meeting open reflections, team members were asked to provide reflection on events, site visits and activities they attended. A guide was provided that included questions based on the Gibb's model of reflection that included:
|
| Staff surveys | A pre‐program 20‐question survey adapted from the Readiness to Change Assessment (ORCA) and the Alberta Context Tool and Context Assessment List was made available to the nursing home staff to provide insight into the context within which the programme was about to be introduced by assessing organisational culture, leadership and staff perceptions related to learning and evaluation. Using a Likert scale, the questions assessed 3 categories: Evaluation, Leadership and Culture. Simple descriptive statistics were generated for the pre‐programme survey responses. |
The data from these sources were collected and organised using the i‐PARIHS framework by the research coordinator. Given the vast amount of data collected in Step One, illustrative concepts and summaries were used to describe the findings. Figure 1 illustrates the five steps followed in the data assembly and analysis process for purposes of this study.
FIGURE 1.
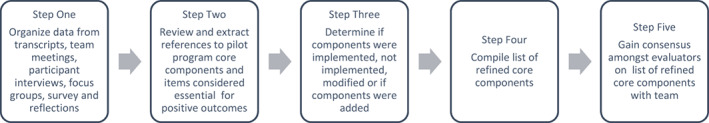
Overview of the five‐step data collection and analysis process
2.1. Step One
Summaries from all sources of data were categorised consistent with the i‐PARIHS framework for successful implementation: innovation, recipients, facilitation and context (Harvey & Kitson, 2015; See Table 5).
TABLE 5.
Categories of the i‐PARIHS framework (Harvey & Kitson, 2015)
| Innovation | How the evidence is adapted in diverse ways to suit a particular situation. |
| Recipients | People affected by and who influence implementation at both the individual and collective team level. |
| Facilitation | Concerns the role of the facilitators and the facilitation process. |
| Context | Expressed as the different contextual layers including micro‐, meso‐ and macro‐context level that act to aid or inhibit implementation. |
2.2. Step Two
Using the initial Core Components from Site One as a framework, the research coordinator independently reviewed the i‐PARIHS framed data and extracted references to Site One core components and sought to identify if there were any additional components of the Programme that emerged as being essential to the Programme's success.
2.3. Step Three
After reviewing the results of Step Two, the research coordinator followed a three‐step assessment approach provided by Pérez et al. (2016) to assess the initial core components and how these translated to Site Two. The components were defined by whether they had been implemented, not implemented or if there had been any omissions, modifications, or additions and their perceived impact, either negative or positive and also any perceptions of the balance between adaptation and adherence (Pérez et al., 2016). This step addresses the research questions.
2.4. Step Four
A list of the refined core components was assembled.
2.5. Step Five
To check the credibility of the refined core components, a Core Component Credibility Survey was developed and emailed to the seven evaluators. The survey listed the identified core components and included columns for evaluators to agree or disagree that the items listed are core components. Respondents were invited to add comments or suggest other items. The survey sought to validate the accuracy of the core components and to determine if the evaluators believed they corroborated their experiences (Lincoln & Guba, 1985). The survey was available for two weeks. Using a consensus approach, the responses were then discussed by the evaluators to confirm the final refined core components.
3. RESULTS
Table 6 illustrates Step Three and how the components were operationalised, delivered and implemented at Sites One and Two, and lists the core items at each site. All four categories of the initial core components were operationalised at Site Two; however, due to the contextual differences between sites, not all Site One core components items were readily translated to Site Two and some required modifications. These modifications were consistent with the plan, do, study act cycle (Taylor et al., 2014) and were made at the discretion of the Site Two on‐site facilitators who lead the Programme implementation due to their local operational knowledge. Of the nine specific operational components (column 2, Table 6), two were not introduced, seven were implemented, with all requiring some element of modification; four new core component categories were added (column 1, Table 6). The core items added included: facility policy and procedures; family and care recipient education and engagement; culture of staff readiness; supportive executive and facility management.
TABLE 6.
Program component evaluation
| Site one core component categories | Operational description of the components | Delivery method (Site One) | Implemented as intended at Site Two (yes/no) | Moderators descriptor of adaptation modified? Omitted? Added components? | Reviewer ‐ negative or positive impact | Refined core components descriptions |
|---|---|---|---|---|---|---|
| Decision‐support tools | RADD index ™: A flip‐chart guide to help staff identify and proactively manage changes in a resident's condition related to eight conditions. |
Introduced at mandatory initial face‐to‐face intensive training session Posted at all work stations. |
Yes |
MODIFIED: Introduced at non‐mandatory introductory meeting; reinforced at regularly scheduled staff meetings. Posted at all work stations. |
Nursing staff benefitted from having guidelines available to follow when a resident's health deteriorated. Facilitators acknowledge the necessity of having this decision‐support guide. | Clinical decision‐making guidelines (or protocol) for managing acute deterioration are needed for staff to follow. |
| Resident Early Warning Observation chart: track and trigger tool for documenting vital signs | Introduced in initial face‐to‐face training session with staff. Available at all work stations. | Yes |
MODIFIED/ ADDED COMPONENTS: Initially seen to conflict with current documentation of vital signs but eventually introduced, along with a policy document outlining its usage |
A track and trigger tool is needed to detect changes in observations / vital signs. Facility policy is needed to support usage. | Track and trigger tool to monitor vital signs is needed to identify changes | |
| SBAR (Situation, Background, Assessment, Recommendation) Communication tool | Introduced during mandatory training | Yes |
MODIFIED/ADDED COMPONENT: Staff were trained to use the tool and it was posted at all workstations. A SBAR‐based fax form was developed to use with GP offices. |
A standardised communication tool, such as SBAR, is needed to facilitate effective communication; the tool was used to create a fax form to communicate resident deterioration between the nursing home and GP or other medical service. | Use of standard communication tool (such as SBAR) for written and oral communication | |
| Advanced Care Planning | Introduced during mandatory training | No | Omitted in initial introduction | |||
| Clinical Management Guidelines: UTI, chest pain, dyspnea, constipation delirium, dehydration, falls, palliative care | Based on current procedures; Introduced in the initial mandatory training. | No |
Omitted: Maintained their own clinical management guidelines. |
Guidelines on clinical care requirements are important and should be linked to the advanced clinical skills training. | Clinical Management Guidelines linked with advanced clinical skills training. | |
| Advanced Clinical Policies & Procedures | Introduced during pilot implementation | Yes | Introduced during programme implementation. | Nursing staff asked for policies to support the use of the programme tools and steps undertaken. Policies were seen as important in supporting nursing staff in their clinical care. | Policies and procedures are needed to support the use of the decision support tools and programme pathways. | |
| Advanced clinical skills training | Initial mandatory face‐to‐face workshops on: Sub Acute Program, tools and resources, new equipment; and eight conditions that commonly lead to hospitalisation: UTI, chest pain, dyspnoea, constipation, delirium, dehydration, falls, palliative care | Training on the programme and eight conditions provided in one mandatory session. Emphasis was given on the idea the programme requires a behaviour change in practice around managing the conditions. | Yes | MODIFIED: Initial training was not provided on all topics; facility decided to introduce training as needed; utilised ‘on the job’ learning and ‘point of care training.’ Training sessions on chest pain, UTI and bladder scanning provided after programme commenced. | Mandatory pre‐programme introduction face‐to‐face training with nursing staff is necessary on the topics identified as contributing to hospitalisations; the mandatory training must include clarification of the term subacute, along with practical examples of application to the various conditions to help staff better understand what is required for early detection and response. | Mandatory initial face‐to‐face training on early identification of deterioration and response (around main conditions leading to transfer); must include a clear definition and description of subacute and subacute care requirements. |
| Specialist clinical support and collaboration | Access to clinical support from medical personnel Health Specialist In‐Reach team; Clinical lead Nurses; NP; Geriatrician; Wound Specialist; Clinical Champions | Ongoing clinical support from NP/RAC team, Clinical Nurse Lead, Clinical Champions, GPs | Yes | MODIFIED: Two clinical nurse leaders appointed; NP available but from distance and not utilised; no Clinical Champions; GP support sought; GP Practice Nurses identified as essential for support. |
The programme requires an on‐site strong clinical leader who can implement the clinical guidelines, provide training on the tools and resources, and support staff; the person must be enthusiastic and knowledgeable and have full support from management. Clinical Champions should be considered to help engage staff and provide support but their role must be clear. External clinicians and their associates available for support must be identified and engaged (Example: GPs and their Practice Nurses) |
Knowledgeable and enthusiastic on‐site clinical leader(s); Clinical Champions (optional); external stakeholders' engagement and support must be identified and sought (i.e., GPs, NPs, GP Practice Nurses, RAC team) |
| Diagnostic medical equipment | Diagnostic equipment not typically found in nursing home setting that can be used to assess and manage clinical deterioration | All equipment available when programme commenced; training provided. Equipment included: ECG machine, bladder scanner, infusion pumps, pulse oximeters, vital sign monitors. | Yes | MODIFIED: Equipment available in stages, along with training. | Diagnostic medical equipment helps to support the decision‐making process and may even lead to shorter hospital length of stay. Equipment seen as important but staff need clinical support while learning to use it; equipment is costly and if cost prohibitive should not forestall introduction of the programme | Diagnostic medical equipment (optional item) |
| Core items added | ||||||
| Facility policy and procedures | Yes |
ADDED: Identified a need to have facility policy and procedures around early identification of deteriorating health and providing subacute care |
Practice changes around providing subacute care in the nursing home must be supported with written policies and procedures. | Facility policy and procedures on early identification of deteriorating health and providing subacute care | ||
| Family and care recipient education and engagement | Yes |
ADDED: Identified family and care recipient support as important to the programme implementation and success. |
Families can insist on transfers and therefore require a good understanding of the nursing home's increase capacity to manage an unwell resident; outreach activities are required. | Family and care recipient education and engagement around the SAC programme. | ||
| Culture of staff readiness to change | Yes |
ADDED: Culture of staff readiness for change. Assessed by administering a questionnaire derived from Organisational Readiness to Change Assessment (ORCA), the Alberta Context Tool and the Context Assessment Index |
Staff need to be willing to embrace the change in practice. | Culture of staff readiness to change | ||
| Supportive executive and facility management | Yes |
ADDED: Supportive executive and facility management. |
Management support was seen as required for the successful implementation of the programme. | Supportive executive and facility management. | ||
Abbreviations: ECG, electrocardiogram machine; GP, general practitioners; NPs, Nurse Practitioners; RAC, Residential Acute Care; RADD, Residential Acute Deterioration Decision; UTI, urinary tract infection.
Table 7 presents the refined core components, including optional components, of the Programme agreed upon by the seven evaluators responding to the Core Component Credibility Survey. These items are viewed by the evaluators as essential to the hospital avoidance programme to produce the expected outcome of a reduction in unnecessary hospitalisations.
TABLE 7.
Refined core components of the Programme
| Decision Support tools |
| ‐‐Clinical decision‐making guidelines for managing acute deterioration |
| ‐‐Track and trigger tool to monitor vital signs |
| ‐‐Use of standard communication tool (such as SBAR) |
| Advanced clinical skills training |
| ‐‐Initial mandatory face‐to‐face training on early identification of deterioration and response (around main conditions leading to hospital transfers) |
| ‐‐Clear definition and description of subacute and subacute care requirements |
| ‐‐Training on clinical management of conditions identified as likely to result in hospitalisation (i.e. UTIs, chest pain, falls, delirium, dehydration, dyspnoea, palliative care, constipation) |
| Specialist clinical support and collaboration |
| ‐‐Knowledgeable and enthusiastic on‐site clinical leader(s) |
| ‐‐Clinical Champions (optional) |
| ‐‐External stakeholders' engagement and support (i.e. GPs, NPs, GP Practice Nurses, RAC team) |
| Diagnostic medical equipment (i.e. bladder scanners, ECG machines, vital sign monitors) (optional) |
| Facility policy and procedures on early identification of deteriorating health and providing subacute care |
| Culture of staff readiness to change |
| Supportive executive and facility management |
| Family and care recipient education and engagement around subacute programme |
Abbreviations: ECG, Electrocardiogram; GP, General Physician; NPs, Nurse Practitioner; RAC, Residential Aged Care; SBAR, Situation, Background, Assessment, Recommendation (communication tool); UTI, urinary tract infection.
3.1. Learnings about modifying core components
Consistent with the i‐PARHIS framework, modifications to a programme may be necessary to address local contextual needs (Kitson & Harvey, 2016). To accommodate the local cultural context, modifications were made to the Programme both prior to the programme launch at Site Two and during the implementation phase (Table 6). The Site Two implementation teams' reflections and the subsequent modifications provided insight into local culture, why adaptations occurred and how such changes influenced full Programme implementation and adoption. In Research Meeting #44, a senior researcher stated: ‘In hindsight, all this is about fidelity. You don't know it until you run it twice. You can assume what the core elements are and put that in place at the next site. You allow for adaptability. You engage those stakeholders at the new site and let them make some decisions, yet you didn't know the core elements needed to really be the core elements until you tried it at another place’.
As an example, at Site One a suite of decision‐support tools was developed to guide nursing staff in identifying and responding to signs of deteriorating health. One of the main tools was an evidence‐based Resident Early Warning Observation chart designed to assist staff in recognising, interpreting and initiating a response to a resident's deteriorating health. This chart is a track and trigger tool for documenting vital signs. Site Two did not initially adopt this chart because a traditional general observation chart was already in place for documenting vital signs and additional documentation, albeit an evidence‐based early warning observation chart, was perceived to be neither warranted nor welcomed. With time and further education on how these charts track trends and help detect early signs of clinical deterioration, the Resident Early Warning Observation chart was introduced along with a site‐specific policy on when and how to use it. Hence, the existing system for documenting vital signs did not change but this tool was added and was reinforced as being a core component.
Another area where modifications were made and then later corrected was clinical skills training. Site One had an initial mandatory full day, face‐to‐face training session for nursing staff that covered all aspects of the Programme, including the decision‐support tools and eight conditions that typically lead to hospitalisation. At Site Two, clinical skills training was delivered as a series of ‘on the job’ and ‘point of care’ training sessions. These staggered training sessions were organised on an as‐needed basis or as new equipment arrived. Our study found this latter approach to be less effective in changing staff behaviour and supporting timely recognition of clinical deterioration. Training was more focused on operating the equipment versus the overall objective, which was the early recognition of clinical deterioration and resident safety.
Approximately five months following the commencement of the Programme at the Site Two, an external facilitator noted that study site staff categorisation of ‘subacute cases’ recorded in the administrative data was not consistent with the Programme's definition. Because nursing staff had been detecting and responding to deteriorating health prior to the programme's implementation, and there were protocols and practices already in place, it was difficult for the nursing staff to grasp what was meant by subacute care versus regular care for health problems. In Health Economics Meeting (#28) the Manager, RN reported that in a review of the data nurses were entering all cases into the database and not clarifying which ones were subacute care versus regular incidents:
(Nurses) should be reporting on only those residents that they are actually providing more advanced care than previously. What they were doing was putting all the falls in and not really doing anything more. … They just did their obs (vital signs) and that was it. Had to provide more advanced clinical care than observations. Not just same old same old. … If monitoring or doing ECG then it would be subacute.
Steps were immediately taken to address the misunderstanding. The implementation and research teams determined the misunderstanding could have been avoided if the decision‐support tools and a mandatory intensive training session had occurred prior to the Programme's launch during the mandatory face‐to‐face training, as had occurred at Site One.
In Meeting #44, Manager RN said: ‘We did full day intensive training up front at (Site One) and offered that at (Site Two) but they weren't keen at the time’. It was agreed during that discussion that mandatory, up front intensive training would help to ensure that nursing staff were well educated in early detection around specific conditions and had a clear understanding as to what subacute care is and that it required a higher level of clinical care than had been previously provided. Therefore, because of this incident, and recognition that it might happen at other nursing homes, initial mandatory face‐to‐face training was reinforced as a core component. This incident also highlighted the need for assessing the nursing staff readiness and willingness to change their views on how care is delivered in the nursing home. Nursing staff need to recognise the change in their roles and responsibilities in recognising and responding to early signs of deteriorating health amongst the residents.
The implementation and research teams recognised early that the level of clinical support available at Site Two differed from Site One. Therefore, they knew they had to identify and work with existing stakeholders and formulate modifications to suit the local model of care. At Site One, access to clinical support was available from health care providers within an outreach team, clinical lead nurses, a nurse practitioner, General Practitioners (GPs) and Clinical Champions; whereas Site Two relied solely on GPs affiliated with the nursing home for support and guidance. Because first contact with the GPs was through the nursing staff at the GP's office, the clinical nurse leads and site manager took steps to engage this cohort with the Programme. In the process, they uncovered a gap in the communication between the GP and nursing home and collaboratively developed a fax form to alert the GP office that the nursing home had a resident with deteriorating health in need of immediate attention. Through this exercise, it became clear that specialist clinical support and collaboration is site specific, and stakeholders need to be identified and engaged to support positive outcomes.
There was also disagreement during implementation at Site Two over inclusion of clinical implementation leaders, which we labelled as ‘Clinical Champions’, as core components. The Clinical Champions at Site One were selected by management from the nursing staff and provided with additional training to lead and support the nursing staff during the introduction of the Programme. Site Two opted not to assign Clinical Champions. In an interview, the NP, RN noted ‘We learned (at Site One) the Champions did not work because it was too easy for the staff to pass care onto the Champions’. During discussion, the evaluators felt that the Clinical Champions would have played an important role in supporting the clinical nurse leads at the Site Two and should be considered an optional core item for future sites. The comments below support this recommendation:
In meeting #23, CCO, RN said: ‘Champs drove the programme (at Site One) initially. We questioned the benefits. Hearing here I'm thinking they were a critical success factor’.
Meeting #24 – Manager, RN – ‘In original project we had really strong clinical leadership. What I'm seeing is we need to have that. Without, you're not seeing the change happen that you would expect to happen’.
The diagnostic medical equipment called for as part of the Programme (electrocardiogram machine, bladder scanner, infusion pumps, pulse oximeters and vital sign monitors) are not typically found in the nursing home setting. Unlike Site One, where the equipment was introduced up front, the equipment at Site Two was introduced at different stages of implementation with training on how to use the equipment. Diagnostic equipment was valued core components at Site One; however, the evaluators recognised that diagnostic medical equipment is expensive and therefore may not be an option for some nursing homes. Therefore, it was decided that the equipment should be an optional core component. On the responses to the Core Component Credibility Survey, an evaluator noted: ‘Whilst the diagnostic equipment can aid the decision‐making process, the costs may be prohibitive for some facilities. The key is for staff to be skilled and confident in clinical assessment to identify and assess changes early, for observations to be monitored and tracked, GP notified, a timely response from the GP and early interventions and management of deterioration’.
Furthermore, four core components were added after implementation and review at Site Two. The first was the inclusion of the Programme in the facility policy and procedures. Staff needed assurance that the practice changes around providing subacute care in the nursing home were supported by documented policy and procedures. A policy outlining the requirements for staff providing care to residents receiving Subacute Care was adopted. It outlined: definitions of terms roles, policy and procedures. The second addition was a culture of readiness to change.
At Site One, there was a recognition that all levels of staff need to be willing to embrace change in practice and that managers in particular must fully support the programme; however, these items were not listed as being core components until their value was reinforced throughout discussions around the implementation process at Site Two. At Site Two, consenting staff completed a survey based on the Organisational Readiness to Change Assessment (ORCA; Humphreys et al., 2012) prior to the introduction of the Programme to assess their willingness to change their practice. The survey results showed that the staff felt the nursing home was ready to undertake the intervention. This step was viewed as key to determining whether efforts to change practice would be embraced by the staff and should be considered prior to the introduction of any new programme. The third added core component was family and care recipient education and engagement. Nursing home residents and their family members are often involved in hospital transfer decisions and have the power to insist that a transfer takes place when a resident is unwell (O'Neill et al., 2015). This power struggle between what the family wants and what the healthcare providers perceive is needed often leaves the nursing staff feeling powerless (O'Neill et al., 2015). Therefore, the evaluators agreed family members had to feel confident that the care available in the nursing home is appropriate and comparable to what their loved one would receive in the hospital setting. A brochure was created at Site Two to provide information to family members and residents regarding the higher‐level of care available. Staff also talked about the programme at family meetings. This component was seen as requisite for positive programme outcomes.
4. DISCUSSION
The process of identifying the core components of this novel nursing home hospital avoidance programme serves to bring attention to the need to identify core components, so that similar programmes can be evaluated and compared to establish best practices. This pilot study clarified essential core components and provided valuable insights into how the core components were translated, why modifications were necessary and the ramifications of those changes. The appraisal captured information about the components from a variety of perspectives over the course of a year‐long study, resulting in a better understanding of the challenges of programme implementation and the importance of future monitoring around the core components. Similar to the findings of Östlund et al. (2015), consideration of the core components led to a deeper understanding and knowledge of the Programme. Adaptations to the original core components were perceived to be both positive and negative. Some of the adaptations led to strengthening aspects of the core components. The evaluation also helped identify core components that were initially overlooked and reinforced why this type of evaluation is valuable.
It was also clear from this evaluation that although both facilities were operated by the same nursing home company, there were considerable differences in available human and non‐human resources between sites. Some of the differences were not evident until well after the programme was launched. This highlights the need to fully assess the resources available before introducing a programme to ensure the outcome expectations can be achieved. We refer again here to the INTERACT reference in the introduction where programme outcomes were not achieved across 85 nursing home sites and a possible barrier included scarce resources (Kane et al., 2017). In this study, we were aware of some of the differences in resources and expectations between the two sites before we launched the Programme at Site Two and determined that allowing the differences to unfold would help us to better understand the programme and the core components. As a result, one of the key learnings from our study was that the timing and content of the advanced clinical skills training should not be compromised.
Because nursing home nurses are already involved in detection of deteriorating health and response, there needs to be a clear understanding from the start that the adoption of a hospital avoidance programme requires the earliest detection and a higher level of resident care. This awareness is best achieved if the definition of subacute is clearly described, and training is provided on early detection and the expected higher level of care prior to launching the programme. Nurses, in particular, must be clear on the higher‐level care requirements and responsibilities assigned when a new programme is introduced (Carusone et al., 2006). Furthermore, access to a clinical nurse lead who is available to answer questions and concerns about unwell residents can improve nursing staff knowledge and clinical skills during the transition (Carusone et al., 2006). INTERCARE assigns a nurse to this role (Zúñiga et al., 2019). We concur that this role is important and should be viewed as a core component. This is an example of where definition of the roles and responsibilities of this lead person would be helpful in evaluating their contribution across different hospital avoidance programmes.
Another important learning from this study was the importance of informing and engaging families and care recipients in the Programme. Families play a key role in resident care and deciding on whether care should be provided at a hospital versus the nursing home and this power influences nursing practice and decision‐making (O'Neill et al., 2015). Family decision makers benefit from interventions that are inclusive (Carnahan et al., 2017). Nurses need to include families in patient care (Aerens et al., 2021). Participation will help families feel confident that the higher level of care available in the nursing home is safe and appropriate. Thus, family and care recipient education and engagement should be an essential core component in a hospital avoidance programme.
Finally, the pragmatic action research approach used in this study reinforces the need to monitor and evaluate a programme during its implementation and to measure its effectiveness. This step is required to build evidence‐based practices.
4.1. Limitations
The evaluation of the translation of the core components of this hospital avoidance programme from Site One to Site Two was complex because many factors were evaluated during the implementation process, including the process itself. This study included monthly meetings and reflections amongst a diverse team of researchers, nursing home staff and programme implementation experts. We understand the limitations of using internal evaluators but believe their conclusions were evidence‐based and guided by the learnings from the implementation process. Nursing home residents and their family members were made aware of the programme, but we recognise their inclusion in the planning and implementation would have been an asset to the overall programme.
5. CONCLUSIONS
Hospital avoidance programmes are needed to prevent unnecessary emergency transfers from nursing homes. The Programme is a nursing‐home initiated hospital avoidance programme that has reduced hospital transfers and length of hospital stays. Implementing the Programme at a second site provided an opportunity to refine and strengthen the core components of the programme. In the process, some of the challenges of programme implementation and adaptation to suit local context have been identified. The foundational core components of a successful hospital avoidance programme have been determined to be: decision‐support tools, advanced clinicals skills training, specialist clinical support and collaboration, facility policies and procedures, family education, a culture of readiness to change and supportive executive and facility management. The next step is to take these core components and undertake a rigorous fidelity assessment as part of a formal process evaluation where the components can be critiqued and measured across multiple nursing home sites in order to solidify the core components.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
FUNDING INFORMATION
This work received financial support from a grant from the Australian Centre for Health Services Innovation. PresCare, a regional not‐for‐profit aged care provider in Queensland, Australia, supported this research at its facilities.
ACKNOWLEDGEMENTS
This work received financial support from a grant from the Australian Centre for Health Services Innovation. PresCare, a regional not‐for‐profit aged care provider in Queensland, Australia, supported this research at its facilities. Open access publishing facilitated by Central Queensland University, as part of the Wiley ‐ Central Queensland University agreement via the Council of Australian University Librarians.
O’Neill, B. J. , Dwyer, T. , Parkinson, L. , Reid‐Searl, K. , & Jeffrey, D. (2023). Identifying the core components of a nursing home hospital avoidance programme. International Journal of Older People Nursing, 18, e12493. 10.1111/opn.12493
DATA AVAILABILITY STATEMENT
Due to ethical concerns, supporting data cannot be made openly available.
REFERENCES
- Aerens, S. , Lepoudre, S. , Verstappen, L. , Vanhoucke, A.‐L. , Malfait, S. , & Van Humbeeck, L. (2021). Family participation in the care of older hospitalised patients: Patients', family caregivers' and nurses' preferences on family caregivers performing care tasks. International Journal of Older People Nursing, 17(3), e12440. 10.1111/opn.12440 [DOI] [PubMed] [Google Scholar]
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes., 50(2), 179–211. [Google Scholar]
- Augustsson, H. , von Thiele Schwarz, U. , Stenfors‐Hayes, T. , & Hasson, H. (2015). Investigating variations in implementation fidelity of an organizational‐level occupational health intervention. International Journal of Behavioral Medicine, 22(3), 345–355. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics . (2016). 2016 census QuickStats (Rockhampton) . https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/SED30071?opendocument
- Australian Bureau of Statistics . (2017). 2016 census QuickStats (Maryborough) . https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/SED30051?opendocument
- Australian Government Department of Health . (2019). $11.7 million investment to keep Australians out of hospital . https://www.health.gov.au/ministers/the‐hon‐greg‐hunt‐mp/media/117‐million‐investment‐to‐keep‐australians‐out‐of‐hospital
- Australian Medical Association . (2021). AMA putting health care back into aged care report . https://www.ama.com.au/articles/report‐putting‐health‐care‐back‐aged‐care
- Beers Criteria Update Expert Panel . (2019). American Geriatrics Society 2019 updated AGS beers criteria for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society, 67(4), 674–694. [DOI] [PubMed] [Google Scholar]
- Blase, K. , & Fixsen, D. (2013). Core intervention components: Identifying and operationalizing what makes programs work. ASPE Research Brief US Department of Health and Human Services. [Google Scholar]
- Carnahan, J. L. , Fowler, N. R. , & Unroe, K. T. (2017). Supporting family decision makers for nursing home residents: A promising approach. JAMA Internal Medicine, 177(1), 32–33. 10.1001/jamainternmed.2016.7065 [DOI] [PubMed] [Google Scholar]
- Carter, H. , Lee, X. , Dwyer, T. , O'Neill, B. , Jeffrey, D. , Doran, C. , Parkinson, L. , Osborne, S. , Reid‐Searl, K. , & Graves, N. (2020). The effectiveness and cost effectiveness of a hospital avoidance program in a residential aged care facility: A prospective cohort study and modelled decision analysis. BMC Geriatrics, 20(1), 1–9. 10.1186/s12877-020-01904-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carusone, S. C. , Loeb, M. , & Lohfeld, L. (2006). A clinical pathway for treating pneumonia in the nursing home: Part I: The nursing perspective. Journal of the American Medical Directors Association, 7(5), 271–278. 10.1016/j.jamda.2005.11.004 [DOI] [PubMed] [Google Scholar]
- Creditor, M. C. (1993). Hazards of hospitalization of the elderly. Annals of Internal Medicine, 118(3), 219–223. 10.7326/0003-4819-118-3-199302010-00011 [DOI] [PubMed] [Google Scholar]
- Crilly, J. , Chaboyer, W. , Wallis, M. , Thalib, L. , & Polit, D. (2011). An outcomes evaluation of an Australian Hospital in the Nursing Home admission avoidance programme. Journal of Clinical Nursing, 20(7/8), 1178–1187. 10.1111/j.1365-2702.2010.03371.x [DOI] [PubMed] [Google Scholar]
- Dai, J. , Liu, F. , Irwanto, D. , Kumar, M. , Tiwari, N. , Chen, J. , Xu, Y. , Smith, M. , & Chan, D. K. (2021). Impact of an acute geriatric outreach service to residential aged care facilities on hospital admissions. Aging Medicine (Milton [N.S.W]), 4(3), 169–174. 10.1002/agm2.12176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan, H. , Slebodnik, M. , & Taylor‐Piliae, R. (2021). Older adults' perceptions of their fall risk in the hospital: An integrative review. Journal of Clinical Nursing, 1–14. 10.1111/jocn.16125 [DOI] [PubMed] [Google Scholar]
- Dwyer, R. , Gabbe, B. , Stoelwinder, J. U. , & Lowthian, J. (2014). A systematic review of outcomes following emergency transfer to hospital for residents of aged care facilities. Age and Ageing, 43(6), 759–766, 758p. 10.1093/ageing/afu117 [DOI] [PubMed] [Google Scholar]
- Dwyer, T. , Reid‐Searl, K. , O'Neill, B. , Parkinson, L. , & Bullock, K. (2017). EDDIE: Early detection of deterioration in elderly: Clinical guide for nursing staff working in aged care. Central Queensland University. [Google Scholar]
- Geriatric Emergency Department Collaborative . (2022). About the geriatric emergency department collaborative . https://gedcollaborative.com/about/
- Graverholt, B. , Forsetlund, L. , & Jamtvedt, G. (2014). Reducing hospital admissions from nursing homes: A systematic review. BMC Health Services Research., 14, 1–9. 10.1186/1472-6963-14-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallgren, J. , Ernsth Bravell, M. , Mölstad, S. , Östgren, C. J. , Midlöv, P. , & Dahl Aslan, A. K. (2016). Factors associated with increased hospitalisation risk among nursing home residents in Sweden: A prospective study with a three‐year follow‐up. International Journal of Older People Nursing, 11(2), 130–139. 10.1111/opn.12107 [DOI] [PubMed] [Google Scholar]
- Harvey, G. , & Kitson, A. (2015). PARIHS re‐visited: Introducing the i‐PARIHS framework. In Harvey G. & Kitson A. (Eds.), Implementing evidence‐based practice in healthcare: A facilitation guide (pp. 25–46). Routledge. [Google Scholar]
- Harvey, G. , & Kitson, A. (2016). PARIHS revisited: From heuristic to integrated framework for the successful implementation of knowledge into practice. Implementation Science, 11, 33. 10.1186/s13012-016-0398-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hullick, C. J. , Hall, A. E. , Conway, J. F. , Hewitt, J. M. , Darcy, L. F. , Barker, R. T. , Oldmeadow, C. , & Attia, J. R. (2021). Reducing hospital transfers from aged care facilities: A large‐scale stepped wedge evaluation. Journal of the American Geriatric Society, 69(1), 201–209. 10.1111/jgs.16890 [DOI] [PubMed] [Google Scholar]
- Humphreys, J. , Harvey, G. , Coleiro, M. , Butler, B. , Barclay, A. , Gwozdziewicz, M. , O'Donoghue, D. , & Hegarty, J. (2012). A collaborative project to improve identification and management of patients with chronic kidney disease in a primary care setting in greater Manchester. BMJ Quality & Safety, 21(8), 700–708. 10.1136/bmjqs-2011-000664 [DOI] [PubMed] [Google Scholar]
- Kada, O. , Janig, H. , Likar, R. , Cernic, K. , & Pinter, G. (2017). Reducing avoidable hospital transfers from nursing homes in Austria: Project outline and baseline results. Gerontology and Geriatric Medicine, 3, 2333721417696671. 10.1177/2333721417696671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane, R. L. , Huckfeldt, P. , Tappen, R. , Engstrom, G. , Rojido, C. , Newman, D. , Yang, Z. , & Ouslander, J. (2017). Effects of an intervention to reduce hospitalizations from nursing homes: A randomized implementation trial of the INTERACT program. JAMA Internal Medicine., 177(9), 1257–1264. 10.1001/jamainternmed.2017.2657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye, K. S. , Marchaim, D. , Chen, T. Y. , Baures, T. , Anderson, D. J. , Choi, Y. , Sloane, R. , & Schmader, K. E. (2014). Effect of nosocomial bloodstream infections on mortality, length of stay, and hospital costs in older adults. Journal of the American Geriatrics Society, 62(2), 306–311. 10.1111/jgs.12634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitson, A. L. , & Harvey, G. (2016). Methods to succeed in effective knowledge translation in clinical practice. Journal of Nursing Scholarship, 48(3), 294–302. 10.1111/jnu.12206 [DOI] [PubMed] [Google Scholar]
- Lemoyne, S. E. , Herbots, H. H. , De Blick, D. , Remmen, R. , Monsieurs, K. G. , & Van Bogaert, P. (2019). Appropriateness of transferring nursing home residents to emergency departments: A systematic review. BMC Geriatrics, 19(1), 17. 10.1186/s12877-019-1028-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln, Y. S. , & Guba, E. G. (1985). Naturalistic inquiry. Sage. [Google Scholar]
- Marcantonio, E. (2017). Delerium in hospitalized older adults. New England Journal of Medicine., 377(15), 1456–1466. 10.1056/NEJMcp1605501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy, E. P. , Ogarek, J. A. , Loomer, L. , Gozalo, P. L. , Mor, V. , Hamel, M. B. , & Mitchell, S. L. (2020). Hospital transfer rates among US nursing home residents with advanced illness before and after initiatives to reduce hospitalizations. JAMA Internal Medicine, 180(3), 385–394. 10.1001/jamainternmed.2019.6130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neill, B. , Dwyer, T. , Reid‐Searl, K. , & Parkinson, L. (2017). Managing the deteriorating nursing home resident after the introduction of a hospital avoidance programme: A nursing perspective. Scandinavian Journal of Caring Sciences., 31(2), 312–322. 10.1111/scs.12349 [DOI] [PubMed] [Google Scholar]
- O'Neill, B. , Parkinson, L. , Dwyer, T. , & Reid‐Searl, K. (2015). Nursing home nurses' perceptions of emergency transfers from nursing homes to hospital: A review of qualitative studies using systematic methods. Geriatric Nursing, 36(6), 423–430. 10.1016/j.gerinurse.2015.06.001 [DOI] [PubMed] [Google Scholar]
- O'Neill, B. J. , Dwyer, T. , Reid‐Searl, K. , & Parkinson, L. (2018). Nursing staff intentions towards managing deteriorating health in nursing homes: A convergent parallel mixed‐methods study using the theory of planned behaviour. Journal of Clinical Nursing, 27(5–6), e992–e1003. 10.1111/jocn.14119 [DOI] [PubMed] [Google Scholar]
- Östlund, U. , Bäckström, B. , Lindh, V. , Sundin, K. , & Saveman, B.‐I. (2015). Nurses' fidelity to theory‐based core components when implementing family health conversations ‐ a qualitative inquiry. Scandinavian Journal of Caring Sciences, 29(3), 582–590. 10.1111/scs.12178 [DOI] [PubMed] [Google Scholar]
- Ouslander, J. G. , Bonner, A. , Herndon, L. , & Shutes, J. (2014). The interventions to reduce acute care transfers (INTERACT) quality improvement program: An overview for medical directors and primary care clinicians in long term care. Journal of the American Medical Directors Association, 15(3), 162–170. 10.1016/j.jamda.2013.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouslander, J. G. , Lamb, G. , Tappen, R. , Herndon, L. , Diaz, S. , Roos, B. A. , Grabowski, D. C. , & Bonner, A. (2011). Interventions to reduce hospitalizations from nursing homes: Evaluation of the INTERACT II collaborative quality improvement project. Journal of the American Geriatrics Society, 59(4), 745–753. 10.1111/j.1532-5415.2011.03333.x [DOI] [PubMed] [Google Scholar]
- Parke, B. , Hunter, K. F. , Bostrom, A. M. , Chambers, T. , & Manraj, C. (2014). Identifying modifiable factors to improve quality for older adults in hospital: A scoping review. International Journal of Older People Nursing, 9(1), 8–24. 10.1111/opn.12007 [DOI] [PubMed] [Google Scholar]
- Parkinson, L. , O'Neill, B. , Dwyer, T. , & Reid‐Searl, K. (2015). Recognising and responding to the deteriorating aged care client: Evaluation of PresCare sub acute care project (final report to PresCare) .
- Pérez, D. , Van der Stuyft, P. , del Carmen Zabala, M. , Castro, M. , & Lefèvre, P. (2016). A modified theoretical framework to assess implementation fidelity of adaptive public health interventions. Implementation Science, 11(1), 91. 10.1186/s13012-016-0457-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, M. , McNicholas, C. , Nicolay, C. , Darzi, A. , Bell, D. , & Reed, J. E. (2014). Systematic review of the application of the plan–do–study–act method to improve quality in healthcare. BMJ Quality & Safety, 23(4), 290–298. 10.1136/bmjqs-2013-001862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa, L. , Hardy, J. E. , Jepson, T. , Braithwaite, J. , & Mitchell, R. J. (2021). Health service utilisation and health outcomes of residential aged care residents referred to a hospital avoidance program: A multi‐site retrospective quasi‐experimental study. Australasian Journal of Ageing., 40(3), e244–e253. 10.1111/ajag.12906 [DOI] [PubMed] [Google Scholar]
- Trahan, L. M. , Spiers, J. A. , & Cummings, G. G. (2016). Decisions to transfer nursing home residents to emergency departments: A scoping review of contributing factors and staff perspectives. Journal of the American Medical Directors Association, 17(11), 994–1005. 10.1016/j.jamda.2016.05.012 [DOI] [PubMed] [Google Scholar]
- Xing, J. , Mukamel, D. B. , & Temkin‐Greener, H. (2013). Hospitalizations of nursing home residents in the last year of life: Nursing home characteristics and variation in potentially avoidable hospitalizations. Journal of the American Geriatrics Society, 61(11), 1900–1908. 10.1111/jgs.12517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zisberg, A. , Shadmi, E. , Gur‐Yaish, N. , Tonkikh, O. , & Sinoff, G. (2015). Hospital‐associated functional decline: The role of hospitalization processes beyond individual risk factors. Journal of the American Geriatrics Society, 63(1), 55–62. 10.1111/jgs.13193 [DOI] [PubMed] [Google Scholar]
- Zúñiga, F. , De Geest, S. , Guerbaai, R. A. , Basinska, K. , Nicca, D. , Kressig, R. W. , Zeller, A. , Wellens, N. I. , De Peitro, C. , Vlaeyen, E. , & Desmedt, M. (2019). Strengthening geriatric expertise in swiss nursing homes: INTERCARE implementation study protocol. Journal of the American Geriatrics Society, 67(10), 2145–2150. 10.1111/jgs.16074 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to ethical concerns, supporting data cannot be made openly available.


