Abstract
Background:
Marijuana legalization occurred gradually in Colorado through political processes.
Objectives:
This review aimed at describing the history of marijuana legalization and correlated shifts in product availability, use patterns, and risk perceptions and describes associated emerging concerns with this process for adolescents and young adults.
Methods:
This review focuses on the history of marijuana legalization and correlated shifts in product availability, use patterns, and risk perceptions.
Results:
Along with the legalization of marijuana, there has been strong commercialization characterized by the widespread development of dispensaries, new products including edibles and concentrates, and an overall lowering of the “price per serving” of marijuana. While the frequency of marijuana use among adolescents does not appear to have shifted substantially, young adult patterns of use have demonstrated an increase in usage. A substantial shift has occurred in the increasing use of concentrates and high potency products. Emerging concerns related to high potency products include increased acute care visits, prevalence and outcomes of comorbid mental health disorders, cannabis-induced psychosis, driving while high, marijuana-related lung injuries, and increased use during pregnancy. Yet, there are also potential medical uses of marijuana.
Conclusion:
To date, scientific evidence of the mental or physical effects of high potency products is currently very limited. Clinical issues related to the treatment of marijuana use and comorbid psychiatric disorders in youth are discussed with a focus on how low risk perceptions influence treatment considerations.
Keywords: Marijuana, cannabis, Δ-9-tetrahydrocannabinol, adolescent, young adult, marijuana legalization, cannabis-induced psychosis, E-cigarette and vaping associated lung injury (EVALI)
1. INTRODUCTION
Marijuana legalization in Colorado occurred through a process of gradual liberalization and relaxation of marijuana policies. In 2000, Colorado legalized medical marijuana and required a physician recommendation (Hopfer, 2014). During 2009, the Department of Justice released the Ogden Memo, deferring enforcement of federal bans on marijuana in legalized states (Ogden, 2009). Over the next two years, the number of individuals with a physician referral for medical marijuana increased 30-fold (Salomonsen-Sautel et al., 2014). In 2012, Colorado legalized recreational marijuana, and recreational sales began in January 2014. Since 2009, the federal government has continued with its policy of “non-interference” and the state’s marijuana industry has continued to expand.
While states continue to expand the liberalization of marijuana policy, policy changes have occurred well ahead of scientific evidence addressing safety and risk or potential medicinal uses (Carnevale, 2018). The paucity of evidentiary guidance likely contributes to many parent’s and provider’s discomfort in talking to adolescents about the consequences and health effects of marijuana use (Brooks et al., 2017; Bull et al., 2017). Consequently, the challenge facing clinicians and researchers is to develop scientifically based responses and provide evidence to guide future policy and regulation.
Recently, a body of literature has started to emerge that explores the impact of marijuana policy liberalization and highlights emerging public health concerns. Herein, we will review the status of marijuana availability in Colorado. Next, we will review the prevalence of marijuana use among adolescents and young adults and changes in modes of use and risk perceptions. We will then explore emerging public health considerations, including acute health care (emergency department) contacts, comorbid mental health disorders including cannabis-induced psychosis, marijuana-related lung injuries, use during pregnancy, and potential medicinal uses. Finally, we will discuss the treatment implications of marijuana legalization for comorbid mental health and other substance use disorders. A review of the evidence will highlight a continuance of changes in availability and behavior regarding marijuana use that outpace research and outline public health concerns that require further study.
2. MARIJUANA PRODUCTS AND SALES IN COLORADO
2.1. Widespread Availability of Dispensaries
As of April 1st, 2020 Colorado lists a total of 1,686 businesses with marijuana licenses that employ 40,257 individuals (Colorado Deparrtment of Revenue, 2020a). Of those, 582 cultivators and 587 stores are licensed to produce and sell recreational marijuana. While direct advertising to minors is banned by Colorado law, the majority of dispensaries maintain an online presence with minimal age verification requirements (Bierut et al., 2017). Of dispensaries surveyed by Bierut et al., only 5% required users to enter their birthdate and 54% required the user to click “yes” to verify age. Several dispensaries also maintain profiles on social media platforms, with young adults aged 20-29 years old being the most common demographic and 15% of followers being younger than 20 years old.
While cannabis use is categorized as medical or recreational, products generally are not exclusive to a category. Recreational use is more frequent, and the vast majority of medical users also report recreational cannabis use (Pacula et al., 2016). Additionally, Salomonsen-Sautel et al., identified substantial diversion of marijuana from registered medical users to 74% of adolescents entering substance use treatment (Salomonsen-Sautel et al., 2012). Adolescents who reported medical marijuana diversion were more likely also to report very easy availability, no friend disapproval of regular cannabis use, and use of cannabis at least 20 times per month in the past year (Thurstone et al., 2011). Thus, classification as medical or recreational is primarily a legal designation authorizing dispensary sales of marijuana.
Implementation of dispensaries, rather than dichotomous indicators of marijuana laws, are positively associated with recreational marijuana use and abuse among adolescents and young adults (Pacula et al., 2015). In the first year of commercialization of marijuana sales, perceived ease of access among high school students increased significantly from 46.5% to 52.1% (Healthy Kids Colorado Survey, HKCS, p < 0.0001) (Harpin et al., 2018). Further, commercialization may be a primary contributing factor for decreasing perceived harm from marijuana use (Brooks-Russell et al., 2019), increasing Δ-9-tetrahydrocannabinol (THC) potency (Sevigny et al., 2014), and marijuana-involved driving and motor vehicle fatalities (Aydelotte et al., 2019).
2.2. Increased THC Potency
Over the past two decades, THC potency, THC:cannabidiol (CBD) ratio, and products and modes of use have changed significantly (Chandra et al., 2019; Mehmedic et al., 2010; Smart et al., 2017; Wilson et al., 2019). Marijuana preparations confiscated in the United States showed an increasing trend of THC concentration from 3.4% in 1993 to 8.8% in 2008 (Mehmedic et al., 2010) and 17.7% by 2017 (Chandra et al., 2019). Concentrates have also shown a sharp increase in THC concentration, from a mean concentration of 6.7% in 2008 to 55.7% in 2017 (Chandra et al., 2019). Wax or shatter is one form of concentrates that has increased in prevalence. Wax is solidified, highly concentrated THC formulations that are used by dabbing, the flash vaporization of the concentrate by applying it to a hot surface. In states with legalized recreational marijuana use, average THC concentrations are likely higher than these national samples, and commercialization of dispensaries may have the most significant impact on increasing THC potency (Sevigny et al., 2014). In one survey of products in Washington state in 2016, the average THC concentration was 20.6% in flower-based products and 68.7% in extracts (Smart et al., 2017). In Colorado, sampled concentrates as part of the state’s monitoring system routinely have THC concentrations as high as 90-95% (Orens et al., 2015).
Similar to the national trend, concentrates have increased in market share from 11.6% in 2014 to 23.4% by 2017 (Orens et al., 2018). In response to nonlethal overdoses from ingestion of edibles, Colorado implemented guidelines for THC dose equivalent per serving (10 mg) and packaging. Table 1 presents the average potency and 1-ounce marijuana equivalent for bud or flower, edibles, and concentrates in Colorado in 2015 (Orens et al., 2015).
Table 1.
Marijuana products and dose equivalency.
| Product | Average THC Potency | 1-ounce Equivalent1 | Mode of Use |
|---|---|---|---|
| Bud/flower | 17.1% | 1 ounce | Smoke |
| Edibles | Variable | 83 10 mg servings | Ingest |
| Concentrates | 62.1% | 7.72 grams | Vaporize, dab |
Amount of product with THC equivalency of 1 ounce of bud/flower
2.3. Increased Sales and Decreased Price Per Serving
Once marijuana became legal for recreational consumption, tracking the number of legal marijuana users became more complicated as individuals were no longer being registered unless they had medical marijuana cards. Tax revenue from marijuana sales has shown a steady increase since 2014. Table 2 below presents the year-by-year increase in Colorado marijuana tax and fee revenue (Colorado Department of Revenue, 2020b).
Table 2.
Colorado revenue from marijuana taxes, licenses, and fees.
| Calendar Year | Annual Revenue |
|---|---|
| 2015 | $130,411,173 |
| 2016 | $193,604,810 |
| 2017 | $247,368,473 |
| 2018 | $266,529,637 |
| 2019 | $302,458,426 |
An analysis of the Colorado marijuana market conducted in 2017 revealed a steady decrease in the “price-per-serving” of marijuana since recreational legalization in 2014 (Orens et al., 2018). The average cost of a 57.1 mg serving of inhaled THC from adult use flower decreased 50.8%, from $3.68 in 2014 to $1.81 in 2017. A serving of THC from medical flower decreased 40% from a 2014 average of $1.79 to $1.11 in 2017. In both cases, the rate of decline in price-per-serving outpaced the price-per-gram declines due to a combination of falling flower prices and increasing potency from 2014 through 2017. The cost of a serving of THC from concentrated extract products exhibited the largest decrease of all marijuana products in both markets. The average price of a serving of THC from concentrates fell 61.7%, from $4.70 in 2014 to $1.80 in 2017, while a serving from medical concentrates fell 57.0%, from $3.28 in 2014 to $1.41 in 2017.
2.4. Prevalence of Marijuana Use in Adolescents and Young Adults
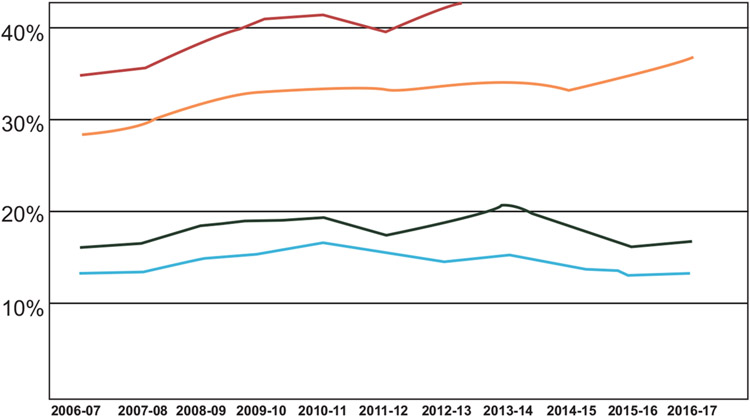
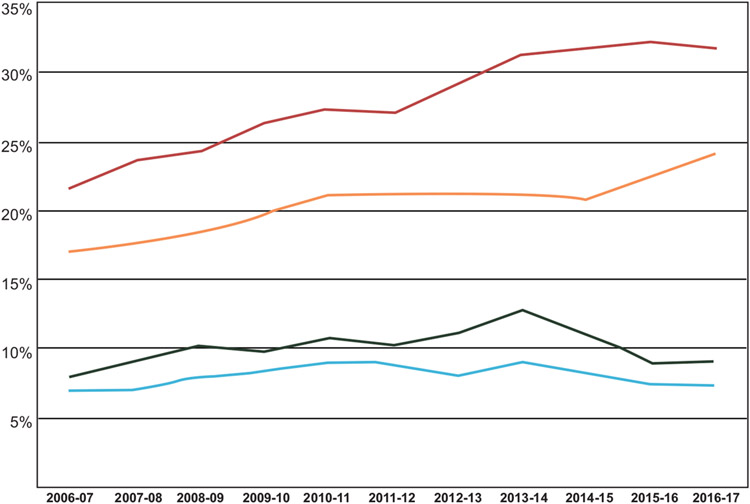
Analysis of Monitoring the Future, a biennial survey of substance use among 8th, 10th, and 12th grade students, found that states with legalized medical marijuana have a higher prevalence of adolescent marijuana use compared with states where marijuana is not legal (15.87% vs 13.27%, OR 1.27, 95% CI 1.07-1.51, p=0.0057; Hasin, Wall, et al., 2015; Sarvet et al., 2018). Comparing Colorado with neighboring states in the West region using the National Survey on Drug Use and Health ( Substance Abuse and Mental Health Services Administration, 2018), higher rates of past year (Fig. 1) and past 30-day (Fig. 2) marijuana use are observed among Colorado adolescents and young adults. While the prevalence of marijuana use has remained relatively steady among adolescents, a significant increase has been observed in both the past year and past 30-day use among young adults. The prevalence of daily or almost daily users is also higher among Colorado adolescents, compared with the national average (Jones et al., 2018). Of note, 20% of marijuana users may account for up to 80% of consumption by some estimates (Vogel, 2018).
Fig. (1). Past year marijuana use in Colorado compared to the West region.
Prevalence of past year use of marijuana is presented by year from 2006-2017 by age group and state or region: 1) Colorado residents aged 18-25 years (red), 2) residents of other West region states aged 18-25 years (yellow), 3) Colorado residents aged 11-17 years (green), and 4) residents of other West region states aged 11-17 years (blue). (A higher resolution / colour version of this figure is available in the electronic copy of the article).
Fig. (2). Past 30-day marijuana use in Colorado compared to the West region.
Prevalence of past 30-day use of marijuana is presented by year from 2006-2017 by age group and state or region: 1) Colorado residents aged 18-25 years (red), 2) residents of other West region states aged 18-25 years (yellow), 3) Colorado residents aged 11-17 years (green), and 4) residents of other West region states aged 11-17 years (blue). (A higher resolution / colour version of this figure is available in the electronic copy of the article).
The Colorado Department of Public Health and Environment (CDPHE) conducts the HKCS, a survey of high school students biennially. While the survey has been impacted by lower-than-expected response rates in the past two editions, age of first use has remained steady since 2013, with 82.1% first using cannabis before age 16 years (Ghosh et al., 2017). Since legalization of recreational marijuana, the prevalence of past 30-day use of marijuana has remained essentially steady, whereas past 30-day use of alcohol, tobacco cigarettes, and prescription drugs have continued to decline. The highest rates of past 30-day marijuana use have been reported among young adults (18-25 years, 26.1%) and high school juniors and seniors (26.3% and 27.8%, respectively). Groups with a higher prevalence of past 30-day marijuana use include adolescents who identified as gay, lesbian, or bisexual (30,9% vs 18.2% for heterosexual peers), adolescents of multiple races (27.1%), and Native Hawaiian/Pacific Islander adolescents (23.1%). Other characteristics associated with a higher prevalence of past 30-day use include male gender, older age, lower perceived harmfulness or wrongfulness, earlier age of initiation (≤ 13 years old), and current cigarette or alcohol use (Johnson et al., 2016). While legalization of medical or recreational marijuana use has not been associated with further increases in the prevalence of adolescent marijuana use ( Colorado Department of Public Health and Environment, 2018; Cerda et al., 2017; Jones et al., 2018), significantly higher rates of adolescent marijuana abuse/dependence after legalization of medical marijuana have been reported (Schuermeyer et al., 2014).
2.5. Modes of Use: Increase in Rates of Dabbing and Ingesting Edibles
The modes of use of marijuana have also changed over the past decade. Adolescents who consume marijuana by more than one mode tend to combine smoking with other high potency products, including ingesting, vaporizing, and/or dabbing (Schneider et al., 2019). Male high school students are more likely to report vaping, dabbing, and ingesting edibles compared to females (Tormohlen, Brooks-Russell, Ma et al., 2019). Of adolescents who responded to the 2017 HKCS, 35.6% reported ingesting edibles, 34.4% reported dabbing, and 20.3% reported vaping. Over the preceding two years, dabbing (7.6%) and ingesting edibles (9.8%) as the usual method of use increased significantly (from 4.3% and 2.1%, respectively) to their highest level (Colorado Department of Public Health and Environment, 2018). Ingesting edibles was more common among youth who accessed marijuana at a public event or school (Johnson et al., 2016).
The HKCS found the prevalence of vaping remained essentially stable from 2015-2017 (Tormohlen, Schneider, Johnson et al., 2019). The prevalence of vaping increases with age, up to three-fold higher among 12th graders compared to 9th graders, and it is highest among Asian and White adolescents (Johnson et al., 2016). A higher prevalence of vaping was also associated with the diversion of medical marijuana (OR 3.4, 95% CI 2.0-5.6).
2.6. Changing Risk Perceptions
Overall, there has been a significant decrease in adolescent perceptions of harm from marijuana use (Schuermeyer et al., 2014). Colorado adolescents and young adults were less likely to feel adults disapprove of smoking marijuana once or twice a week or to feel smoking marijuana once or twice a week presented a great health risk (Schuermeyer et al., 2014). While the change in perceived risk, and the significance of the change, differ by age and study sample (Cerda et al., 2017; Harpin et al., 2018), some important findings have been reported. First, because marijuana is often described as “natural” and medical uses are often touted, many adolescents and young adults view it as less harmful and less addictive than other drugs and medications, including antidepressants, anxiolytics, and opioid pain medications (Popova et al., 2017). Of licensed retailers surveyed by Bierut et al., the majority made health claims regarding marijuana use (Bierut et al., 2017). Common conditions cited include anxiety, cancer, depression, diabetes, insomnia, pain, post-traumatic stress disorder, and skin irritation. Conversely, none of the retail stores listed harmful or adverse effects of cannabis use.
Concerning signs and symptoms of cannabis use disorder, individuals often identify emotional or mental dependence on marijuana and habitual urges to use (Popova et al., 2017). In a study of perceived harm, Popova et al. found respondents described physiologic changes due to use, though they generally did not identify tolerance as signs of addiction or report withdrawal symptoms. Of concern, multiple respondents discussed using higher potency products to overcome tolerance to achieve getting high.
Second, there may be changing perceptions regarding the risks of combustible marijuana products compared to higher potency products. In the 2015 HKCS survey, adolescents who reported higher perceived parental disapproval, wrongfulness, or harm from marijuana use were less likely to consume marijuana by modes other than smoking (Tormohlen, Brooks-Russell, Ma et al., 2019). Conversely, in the 2013 HKCS survey, Johnson et al., found that higher perceived harmfulness was associated with an increased likelihood of ingesting edibles or vaping, whereas lower perceived harmfulness is associated with smoking (Johnson et al., 2016). Adolescents who reported high perceived wrongfulness of marijuana use were also less likely to vape. The differences between the 2013 and 2015 surveys may in part highlight changing perceptions regarding the risk of combustible marijuana products. Similarly, a survey of young adults aged 18-26 years old found that combustible products were perceived as more dangerous than vaporizers and edibles (Popova et al., 2017). The risk of unintentional overdose with these higher potency products was also perceived to be lower than the health risks of using a combustible product.
3. PUBLIC HEALTH CONSIDERATIONS
3.1. Increase in Unintentional Pediatric Exposures
Legalization of marijuana in Colorado has been associated with increases in marijuana-related regional poison center (RPC) calls, ED or urgent care visits, and hospitalizations for all age groups (Wang et al., 2017). Per the Colorado Hospital Association, ED visits and hospitalizations with marijuana poisoning billing codes have continued to rise since legalization (20.8 per 100,000 hospitalizations and 20.3 per 100,000 ED visits in 2017) (Colorado Department of Public Health and Environment, 2018). The greatest increase in the number of unintentional marijuana exposures was observed in children less than 9 years old (Wang et al., 2017). By 2017, calls to the regional poison control center due to unintentional exposure in children 0-8 years old increased 10-fold, after having remained steady for the preceding decade (Wang et al., 2020; Wang et al., 2014). The majority (60-74%) of these children were subsequently seen by health care professionals, with an overall admission rate of 16% (Wang, 2017; Wang et al., 2014). When compared to non-legal states, exposures in legal states led to more major effects (OR 2.1, 95% CI 1.4-3.1) and critical care admissions (OR 3.4, 95% CI 1.8-6.5; (Wang, 2017). Edible marijuana products accounted for 65.6% of exposures, followed by smokable products at 23.4% (Wang, 2017). The most common sources of THC ingested by minors include cookies, brownies, cake, popcorn, gummies, tootsie rolls, and other edible products (Heizer et al., 2018).
To date, little is known about risks from passive exposure to second-hand smoke, though many carcinogens common to cigarette smoke have been identified (Lee et al., 1976a, 1976b; Moir et al., 2008). Yet, a significant number of children who live in a home where marijuana is smoked daily within the home have detectable levels of THC or its metabolites (Wilson et al., 2018).
3.2. Adolescent and Young Adult Acute Health Care Contacts
Adolescents and young adults have experienced significant increases in intentional exposures resulting in acute medical care (Wang et al., 2017). The annual rate of marijuana-related ED and urgent care visits for adolescents aged 13-20 years old increased from 1.8 per 1,000 visits in 2005 to 4.9 per 1,000 visits in 2015 (Wang et al., 2018). According to Colorado Hospital Association data, in the past year, ED visits were highest among young adults aged 18-25 years old (2,352 per 100,000 ED visits) and hospitalizations with marijuana-related billing codes remain the highest among youth aged 9-17 years old (7,974 per 100,000 hospitalizations; (Colorado Department of Public Health and Environment, 2018). Higher rates of ED visits and hospitalizations have been reported in males and Black patients.
A recent study showed even regular and heavy users inaccurately estimate the amount of cannabis prepared or used (Prince et al., 2018). Not surprisingly, the number of ED visits related to cannabis use by out-of-state visitors rose sharply after commercialization of cannabis sales (Kim et al., 2016). In response to the risk posed by edible cannabis products, Colorado emergently introduced measures to reduce unintentional overdose, including limitations on the maximum THC content per package, demarcated servings, and universal symbols on packaging labels (Ghosh et al., 2017; Vogel, 2018). Over the time period of legalization of recreational cannabis use and commercialization of cannabis sales, a flattening of the curve in the prevalence of Colorado residents presenting to the ED for cannabis-related problems was observed, suggesting a learning curve initially during more widely available cannabis use and change in product potency (Kim et al., 2016).
3.3. Comorbid Mental Health Disorders
A review of the Colorado Hospital Association ED discharge data showed a five-fold higher prevalence of mental health diagnoses in marijuana-associated ED visits compared to visits without marijuana between 2012-2014 (Hall et al., 2018). The most prevalent disorders were mood (6.78%) and anxiety (3.82%) disorders, followed by schizophrenia spectrum disorders (2.96%) and suicide or intentional self-inflicted injury (2.79%). Of note, the prevalence ratio of schizophrenia spectrum disorders was 9.18 (95% CI 8.66-9.75) and of suicide or intentional self-inflicted injury was 7.96 (95% CI 7.49-8.46) compared to ED visits without marijuana codes. A review of tertiary care ED and urgent care visits at a Colorado children’s hospital system from 2005-2015 found 4,202 episodes of care (Wang et al., 2018). Sixty-two percent of patients were diagnosed with cannabis use, abuse, or misuse. Additionally, 71% received a comorbid psychiatric diagnosis, with the most common being depression (39%) or mood disorder (22%). Twelve percent had co-ingested ethanol, with other substances reported in 4% or fewer visits.
Overall, cross-sectional studies have shown one-third of adolescents with a substance use disorder meet the criteria for a comorbid psychiatric disorder, with up to 80% of adolescents entering substance use treatment having significant psychiatric symptoms (Robinson & Riggs, 2016). Adolescent marijuana use is associated with depression and anxiety disorders, as well as earlier onset of mania or psychosis (reviewed in Levine et al., 2017). Marijuana use is also associated with a higher risk of suicidal ideation (OR 1.50, 95% CI 1.11-2.03) and suicide attempt (OR 3.46, 95% CI 1.53-7.84) (Gobbi et al., 2019).
Comorbid cannabis use disorder and psychiatric disorders also have poorer treatment outcomes, increased treatment dropout, and earlier time to relapse for substance use (Cornelius et al., 2004; Hersh et al., 2013; White et al., 2004). Further, high-potency THC concentrates may also be associated with poorer mental health outcomes and higher use of illicit substances (Chan et al., 2017), though one other study did not find significant differences in mental health outcomes (Prince & Conner, 2019). While multiple associations between marijuana use and mental health have been established, there are notable overlapping factors, including poor parental monitoring, early childhood loss and family disruption, and trauma and multiple shared neurophysiologic changes (Brady & Sinha, 2005; Kendler et al., 2003; Libby et al., 2005; Volkow, 2004).
3.4. Cannabis-induced Psychosis
Of particular concern among comorbid psychiatric disorders is the increased risk of early onset schizophrenia and cannabis-induced psychosis. Prior to legalization of medical marijuana, a case series reported a temporal association between marijuana use and psychosis (Clark, 1994), now referred to as cannabis-induced psychosis (Hudak et al., 2015; Rolland et al., 2013). The prevalence of cannabis-induced psychosis is unknown. However, the majority of those who use marijuana do not develop signs or symptoms of psychosis. It seems individuals with the highest vulnerability to cannabis-induced psychosis are those with a familial risk for psychosis or schizophrenia (Hiemstra et al., 2018; Kendler et al., 2019). Primary risk factors may be high THC potency, duration of use, and initiation of marijuana use at a younger age (Di Forti et al., 2015; Di Forti et al., 2009; Di Forti et al., 2014; Keller et al., 2016; Large & Nielssen, 2017; Murray et al., 2016; Pierre, 2017; Pierre et al., 2016; Rabin & George, 2017). Further, adolescent initiation of marijuana use is associated with early onset psychotic disorder in a dose-dependent fashion and associated with poorer course of illness and functional outcomes (reviewed in Bagot et al., 2015). Neuroimaging findings suggest early use of marijuana may alter cortical maturation in susceptible adolescents (French et al., 2015), though the underlying mechanism of cannabis-induced psychosis is unknown.
3.5. Increase in Driving While High and Marijuana-related Motor Vehicle Fatalities
Overall, the percent of adolescents riding in a vehicle driven by someone who had been using marijuana or driving when they had been using has remained steady from 2011 (21.7%) to 2017 (19.7%) (Colorado Department of Public Health and Environment, 2018). While studies show individuals drive at slower speeds when high, a counterpoint often cited by the marijuana industry, such driving may also represent a danger on the highway (Vogel, 2018). Marijuana use affects multiple tasks important to driving safety, including attention, reaction time, and motor skills and has been shown to result in increases in lateral position deviation and slower driving (reviewed in Aydelotte et al., 2019). In adolescents, recent marijuana use, including less-than-weekly use, is associated with increased impairment and risk of motor vehicle collisions (MVC) (Colorado Department of Public Health and Environment, 2018). Driver impairment has been demonstrated at blood THC levels as low as 2-5 ng/mL or after orally ingesting more than 10 mg of THC. The estimated impact of driving impairment is up to 6 hours for smoking and 8 hours for ingesting up to 18 mg of THC.
One key factor associated with increasing rates of marijuana-related driving incidents and fatalities may be the commercialization of recreational marijuana sales (Aydelotte et al., 2017; Aydelotte et al., 2019). Medical marijuana laws have been associated with up to a doubling of the prevalence of driving while under the influence of marijuana by 2013 (Fink et al., 2020). Yet, following the legalization of recreational marijuana use, the proportion of drivers in fatal motor vehicle crashes who were THC-positive in Colorado was decreasing (Salomonsen-Sautel et al., 2014), which may be attributed to increased enforcement efforts (Sevigny, 2018). Following the commercialization of recreational marijuana sales, however, the number of driving under the influence (DUI) citations where marijuana was reported as the impairing substance increased by 16% between 2014 and the first 10 months of 2016 (Ghosh et al., 2017). Simultaneously, there was an increasing trend in proportion of marijuana-positive drivers in fatal MVC and an 80% increase in fatalities that tested positive for marijuana (Salomonsen-Sautel et al., 2014). Analysis of MVC fatalities found an increase of 0.8 fatalities per billion vehicle miles traveled after legalization of recreational marijuana use and an increase of 1.3 fatalities per billion vehicle miles traveled when comparing MVC in the period between legalization and commercialization with MVC after commercialization (Aydelotte et al., 2019).
3.6. Marijuana-related Lung Injuries
Recently, there has been increasing concern about marijuana-related pulmonary injuries. The most common marijuana-related pulmonary injuries are bronchospasms, pneumothorax, and aspergillus infection (McGraw et al., 2018). Acute and chronic pulmonary injuries in adolescents and young adults have been associated with contaminated marijuana products, including talcum (Scheel et al., 2012), formaldehyde and phencyclidine (Gilbert et al., 2013), and other chemicals (Moatemri et al., 2016). Three cases of an adolescent male with eosinophilic pneumonia with silica-induced pneumoconiosis and acute hypersensitivity pneumonitis associated with recent cannabis inhalation were reported in Colorado in 2018 (McGraw et al., 2018). In 2019, a multistate outbreak of electronic cigarette or vaping product-use associated lung injury (EVALI) cases was reported, with 805 cases and 12 deaths reported to the Centers for Disease Control (CDC) through September 2019 (Perrine et al., 2019; Schier et al., 2019). Seventy-seven percent of patients reported using THC-containing products in the 30 days preceding the onset of symptoms. Over half of patients were younger than 25 years old (54.2%), and 23.9% of patients were 25-34 years old. EVALI cases were reported in previously healthy individuals and resulted in acute lung injuries, often necessitating intubation or intensive care admissions (Civiletto et al., 2020; Perrine et al., 2019; Schier et al., 2019). Subsequent analyses of recovered cartridges implicated vitamin E acetate, a diluent used in some cannabis oil products (Duffy et al., 2020). Other cases of marijuana-related lung injury have been reported, including exogenous lipoid pneumonia or chemical pneumonitis (Gay et al., 2020), acute lung injury mimicking atypical pneumonia (Stephens et al., 2020), and diffuse alveolar hemorrhage (Alqahtani et al., 2019).
3.7. Increased Use During Pregnancy
Marijuana use before pregnancy (15.2%), during pregnancy (7.8%), and while breastfeeding (4.4%) trended upward from 2014-2018 (Colorado Department of Public Health and Environment, 2018). The American College of Obstetricians and Gynecologists strongly recommend against the use of marijuana during pregnancy or lactation (Committee on Obstetric Practice, 2017). Yet, of Colorado dispensaries surveyed by Dickson et al., 69% recommended marijuana products for the treatment of morning sickness (Dickson et al., 2018). Marijuana use during pregnancy is highest among younger moms aged 15-19 years (13.3%) and 20-24 years (12.3%) compared with moms that are 25-34 years or older than 34 years (5.3% and 3.4%, respectively). Marijuana use is also higher among women with unintended pregnancies compared to women with intended pregnancies (10.4% vs 4.1%). THC rapidly crosses the placenta, with cord blood THC levels measured three to six times lower than that found in maternal blood (Blackard & Tennes, 1984). There is a greater transfer of THC early in pregnancy, at a time when the fetus may be most vulnerable to the neurodevelopmental consequences of exposure and some women may not know they are pregnant. THC also concentrates in breast milk (Atkinson et al., 1988; Perez-Reyes & Wall, 1982), though the degree to which and how long after cessation of use has yet to be determined.
The endocannabinoid system, through which THC exerts its effects, is present in the fetus as early as 16-22 days gestation and is fundamental to neurodevelopment (Campolongo et al., 2011; American College of Obstetrics and Gynecology, 2017; Szutorisz et al., 2014; Volkow et al., 2017). The effects of exogenous cannabinoids on neurodevelopment have not been well-characterized, yet it is of great concern. Human studies of prenatal marijuana exposure have also raised concerns for lower birth weight, smaller head circumference, and higher stillbirth rate (Campolongo et al., 2011; American College of Obstetrics and Gynecology, 2017; Volkow et al., 2017). Children exposed in utero also exhibit cognitive and behavioral deficits, impairments in executive functioning, lower processing speed and visual problem solving, and increased impulsivity and externalizing behaviors (Goldschmidt et al., 2012; Szutorisz et al., 2014). It is important to note there are multiple confounders in studying prenatal marijuana exposure, including comorbid use of alcohol or tobacco and demographic, social, and psychological factors among participants most likely to participate in these studies.
4. POTENTIAL MEDICAL USES OF CANNABIS
In addition to the recreational market, a growing number of Americans use marijuana for medicinal purposes (Hasin, Saha, et al., 2015; Substance Abuse and Mental Health Services Administration, 2017). In Colorado, the most common medical condition cited for medical marijuana referrals is severe pain, with the exception of children younger than 11 (seizures). As of March 2020, there were 21,400 registered adolescents and young adults with medical marijuana referrals (Table 3). A medical evaluation and registration with the state is mandatory for a medical marijuana referral, though no ongoing monitoring or counseling is required.
Table 3.
Colorado medical marijuana referrals by age.
| Age Group | Number (% of Total Registry) | Most Common Condition |
|---|---|---|
| 11-17 | 168 (0.21%) | Severe pain |
| 18-20 | 3,598 (4.40%) | Severe pain |
| 21-30 | 17,634 (21.58%) | Severe pain |
A recent National Academy of Sciences, Engineering, and Medicine review reported marijuana affects a wide range of organ systems, including the central nervous system, gastrointestinal system, and immune system, among others (Maccarrone et al., 2015; National Academies of Science, 2017). Marijuana has been implicated in chronic illnesses, including bronchitis, cardiovascular disease, some cancers, metabolic syndrome, and psychiatric illness (National Academies of Science, 2017; Volkow et al., 2014). However, there is also preliminary evidence it may be efficacious for other medical conditions. Relatively small controlled trials of marijuana or cannabinoid derivatives in patients have shown potential efficacy for appetite regulation, muscle spasticity, nausea, pain, and seizures (Ben Amar, 2006; Watson et al., 2000). Animal studies investigating anti-inflammatory properties of cannabinoids suggest they may also be efficacious for some inflammatory diseases, including the gastrointestinal tract (Esposito et al., 2013; Nagarkatti et al., 2009). To date, the FDA has approved two pharmaceutical-grade forms of CBD (Epidiolex) for seizures associated with Lennox-Gastaut or Dravet syndromes and THC (Marinol and Syndros) for anorexia associated with AIDS (Food and Drug Administration, 2020). The use of marijuana or plant-derived products has not been federally approved.
Proponents of medical marijuana legalization often suggest a substitution effect with opioids that might result in fewer opioid related deaths in medical marijuana states. However, a recent review identified a non-significant reduction compared with states where marijuana is not legal, including a modest reduction of 7% in opioid overdose mortality and 6% reduction in opioid prescriptions among Colorado Medicaid and managed care enrollees (Chihuri & Li, 2019).
5. TREATMENT IMPLICATIONS OF MARIJUANA LEGALIZATION
The adolescent and young adult treatment implications of marijuana legalization for psychiatry can be divided into a number of areas: 1) the treatment of cannabis use disorder, 2) the treatment of other substance use or psychiatric conditions where marijuana use may be worsening or exacerbating the condition but the patient does not wish to discontinue use, and 3) the situations where the patient reports that marijuana use has beneficial/medicinal effects and requests a medical marijuana referral or the provider’s approval for continued use.
The greatest area of scientific consensus for marijuana use is that it is harmful for adolescents, particularly in domains of cognitive functioning, the development of psychosis, and effects on long-term social adjustment (Volkow et al., 2016). For young adults, there is a broad literature that associates marijuana use with a range of negative psychosocial outcomes; however, whether marijuana is a cause of these psychosocial outcomes or a marker for other associated conditions remains unclear. However, the “medical” legal status for marijuana is unusual and creates unique perception and status issues for marijuana compared to other substances. Despite tobacco use being associated with weight loss (Audrain-McGovern & Benowitz, 2011) and alcohol having some anxiolytic properties (Gilman et al., 2008), neither have a general sense of medical approval nor legal status as medicinal.
Similar to the treatment of alcohol use disorder in adults, the treatment of cannabis use disorder under the conditions of legalization remains fairly straightforward, with marijuana identified as the “problem substance.” Cannabis use disorder is primarily addressed with psychosocial treatments such as motivational interviewing, contingency management, and cognitive behavioral therapy. For cannabis use disorder, the primary decision to be made is whether a “harm reduction” or “abstinence” model is the primary treatment goal (Potter et al., 2019; Stockings et al., 2016). As abstinence models typically apply to the use of any substance, marijuana use is incompatible with this treatment model. Harm reduction treatment plans may focus on reduction in the amount or frequency of use and identifying how the substance is influencing the patient’s functioning.
In adolescents with comorbid psychiatric disorders, cannabis use disorder should be treated in an integrated fashion due to the interaction between disorders (Hinckley & Riggs, 2019). Recently, Arias et al., demonstrated a relationship between decreasing cannabis use and decreasing depression symptoms in adolescents receiving psychosocial intervention for cannabis use disorder (Arias et al., 2020). When considering pharmacotherapy, it is typically indicated only for comorbid conditions, such as depression or anxiety. Analysis of treatment outcomes of adolescents receiving outpatient motivational interviewing and cognitive behavioral therapy indicates overall treatment remains effective in a state with legalized cannabis (LeNoue et al., 2017). Few studies have investigated the efficacy and safety of psychopharmacologic agents in adolescents with cannabis use disorder (Cornelius et al., 2010; Hinckley & Riggs, 2019; Riggs et al., 2007; Winhusen et al., 2011).
There has been particular concern regarding comorbid ADHD and marijuana use. ADHD has been associated with increased use of marijuana and other substances through young adulthood, as well as more impairing symptoms of ADHD (Bidwell et al., 2014; Molina et al., 2018). Marijuana has been shown to cause neuropsychological impairment, including inattention. However, the interaction between marijuana use and ADHD remains unclear. Research suggests the relationship between childhood ADHD and later marijuana use may be due to shared familial environment and genetics rather than a causal relationship (Elkins et al., 2018). To date, few studies of medications for ADHD have included patients with comorbid substance use. One study of osmotic-release methylphenidate found it is generally well-tolerated in adolescents with substance use disorders (Riggs et al., 2011; Wilens & Upadhyaya, 2007), though its efficacy for ADHD is unclear. It is also unclear if medical stimulant use in comorbid ADHD may reduce the risk of substance use (Hammerness et al., 2017; Riggs et al., 2011). Inconsistent findings may be due to a tendency to underdose stimulants in those with substance use disorders (Skoglund et al., 2017). Further, pharmacologic treatment of ADHD does not appear to increase the risk for SUD (Wilens & Upadhyaya, 2007). While there is much we do not know, clinicians should decide they would consider prescribing controlled substances for ADHD with comorbid marijuana use and if prescribing would be conditional upon concurrent substance use monitoring and/or treatment.
6. CONCLUSION
When patients seek a medical marijuana referral or provider approval to use marijuana, clinicians should have an established policy. While many youth report using marijuana to self-treat depression, anxiety, insomnia, or other mental health conditions, a recent meta-analysis found scarce evidence that pharmaceutical-grade cannabinoid products improve mental health disorders (Black et al., 2019). The American Psychiatric Association (APA) issued a position statement in opposition to the use of marijuana as medicine, citing the lack of scientific evidence supporting marijuana as medicine, that no medications are currently smoked, that dosages consumed are unclear, and that ballot initiatives should not form the basis for medical decision making (American Psychiatric Association, 2019). While the American Academy of Child and Adolescent Psychiatry (AACAP) has encouraged more scientific evaluation to determine whether there is a medical indication for marijuana in children and adolescents (American Academy of Child and Adolescent Psychiatry, 2012), the organization has issued statements opposing medical marijuana dispensing to adolescents and more recently opposing the use of marijuana in autism spectrum disorder (American Academy of Child and Adolescent Psychiatry 2019). Further, the American Academy of Pediatrics opposes medical marijuana outside of the regulatory process of the US Food and Drug Administration (American Academy of Pediatrics, 2015). Thus, institutions and providers should consider the risks and benefits of recommending marijuana for medicinal use to determine a priori guidelines.
7. FUTURE DIRECTIONS
In summary, while marijuana legalization has outpaced scientific research, recent studies highlight changing trends in the availability, potency, and modes of use, and risk perceptions and raise emerging public health concerns that warrant further investigation. Commercialization of marijuana in Colorado created an environment of increasing availability and increasing THC potency and decreasing price per serving. The acute and chronic effects of high potency THC exposure are unknown, as are differences in route of consumption. Yet, clinically, increased acute care encounters, cannabis-induced psychosis, EVALI and recent EVALI-related deaths, and the incidence of comorbid mental health conditions are of great public health concern. As potency increases and price decreases, higher doses of THC are more readily available to adolescents. Demand for marijuana, as with other intoxicating substances, is responsive to monetary price and legal risk (Aston et al., 2017; Hunt & Pacula, 2017; Pacula & Lundberg, 2014; Smart et al., 2017).
While it does not appear the prevalence of use has changed among adolescents, there is a paucity of baseline data prior to marijuana legalization, complicating pre- and post-legalization analyses (Ghosh et al., 2017). Further, studies differ in findings of use prevalence based on analysis and dataset (Dilley et al., 2019). It might also be that no post-legalization increase in prevalence was observed because public opinion and perceived acceptance and risk may have already shifted (Palamar et al., 2014), resulting in an environment where legalization is feasible. Insufficient data provides a challenge to further elucidating the relationship between the evolution of social acceptance, legalization, and prevalence of use.
Further, it remains to be seen how changes in risk perception will affect prevalence and frequency of use, and it is unknown if changes in risk perception contribute to the increasing use of high-potency products among adolescents. However, individual and societal perceptions and beliefs do influence marijuana consumption patterns. As demonstrated by Popova et al., combustible products and manufactured or chemically manipulated products are viewed as more harmful (Popova et al., 2017). It is likely that concerns about combustible and chemically manipulated products are driven by years of public health campaigns and knowledge about the risks of tobacco smoking. Thus, informed, evidence-based public health campaigns regarding marijuana use may be an effective tool for influencing marijuana use.
The impact of marijuana on mental health and other substance use disorders remains largely unknown. While associations between cannabis and psychosis have been demonstrated, a causal relationship is difficult to establish due to limitations of methodology and the prevalence of marijuana use in adolescents. Yet, marijuana use, as with other substance use, also leads to lower treatment compliance and more adverse outcomes in adolescents with mental health disorders. Further studies are also needed to understand the impact of marijuana legalization on the use of other substances, including alcohol, tobacco, and opioids.
In this first decade of marijuana legalization, policy and public opinion have outpaced, and even superseded science and public health. Emerging studies raise the concern that such an approach may have negatively impacted youth and the public. As outlined in this qualitative review, marijuana research, particularly with products consumed by the public, is in its nascency. As such, quantitative investigations are not yet feasible. Other reports that may be of interest and expand on the scope of data in this review include the NIDA National Advisory Council on Drug Abuse cannabis policy research recommendations (Carnevale, 2018), the National Academy of Sciences report (Maccarrone et al., 2015; National Academies of Science, 2017), and the Rocky Mountain High Intensity Drug Trafficking Area impact report (Rocky Mountain High Intensity Drug Trafficking Area, 2020). It is vital for the research and medical community to respond with evidence supported by research to address public health concerns and guide future policies and regulations. The outcomes of these studies are fundamental to evidence-based, public health awareness campaigns that will inform universal prevention strategies and selective interventions, as well as youth and parent education.
ACKNOWLEDGEMENTS
Drs. Hinckley and Hopfer receive research funding from the National Institute on Drug Abuse, the Colorado Clinical Sciences and Translational Institute, and the University of Colorado Department of Psychiatry.
LIST OF ABBREVIATIONS
- ADHD
Attention deficit/hyperactivity disorder
- CBD
Cannabidiol
- ED
Emergency department
- EVALI
e-cigarette and vaping related lung injury
- HKCS
Healthy Kids Colorado Survey
- MVC
Motor vehicle collision
- OR
Odds ratio
- RPC
Regional poison control center
- THC
Δ-9-tetrahydrocannabinol
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
REFERENCES
- American Academy of Child and Adolescent Psychiatry. (2012). Medical marijuana. Available from: https://www.aacap.org
- American Academy of Child and Adolescent Psychiatry. (2019). Use of medical marijuana in children and adolescents with autism spectrum disorder for core autism symptoms or co-occurring emotional or behavioral problems. Available from: https://www.aacap.org
- American College of Obstetrics and Gynecology (2017). Committee Opinion No. 722: Marijuana use during pregnancy and lactation. Obstet. Gynecol, 130(4), e205–e209. 10.1097/AOG.0000000000002354 [DOI] [PubMed] [Google Scholar]
- Alqahtani A, Ammari Z, Ramahi A, Said Ahmed TS, Klada E (2019). Cannabis smoking-induced diffuse alveolar hemorrhage. Cureus, 11(7), e5089. 10.7759/cureus.5089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2019). Position statement in opposition to cannabis as medicine. Available from: https://www.psychiatry.org
- Arias AJ, Hammond CJ, Burleson JA, Kaminer Y, Feinn R, Curry JF, Dennis ML (2020). Temporal dynamics of the relationship between change in depressive symptoms and cannabis use in adolescents receiving psychosocial treatment for cannabis use disorder. J. Subst. Abuse Treat, 117, 108087. 10.1016/j.jsat.2020.108087 [DOI] [PubMed] [Google Scholar]
- Aston ER, Farris SG, MacKillop J, Metrik J (2017). Latent factor structure of a behavioral economic marijuana demand curve. Psychopharmacology (Berl.), 234(16), 2421–2429. 10.1007/s00213-017-4633-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson HC, Begg EJ, Darlow BA (1988). Drugs in human milk. Clinical pharmacokinetic considerations. Clin. Pharmacokinet, 14(4), 217–240. 10.2165/00003088-198814040-00003 [DOI] [PubMed] [Google Scholar]
- Audrain-McGovern J, Benowitz NL (2011). Cigarette smoking, nicotine, and body weight. Clin. Pharmacol. Ther, 90(1), 164–168. 10.1038/clpt.2011.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aydelotte JD, Brown LH, Luftman KM, Mardock AL, Teixeira PGR, Coopwood B, Brown CVR (2017). Crash fatality rates after recreational marijuana legalization in Washington and Colorado. Am. J. Public Health, 107(8), 1329–1331. 10.2105/AJPH.2017.303848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aydelotte JD, Mardock AL, Mancheski CA, Quamar SM, Teixeira PG, Brown CVR, Brown LH (2019). Fatal crashes in the 5 years after recreational marijuana legalization in Colorado and Washington. Accid. Anal. Prev, 132, 105284. 10.1016/.aap.2019.105284 [DOI] [PubMed] [Google Scholar]
- Bagot KS, Milin R, Kaminer Y (2015). Adolescent initiation of cannabis use and early-onset psychosis. Subst. Abus, 36(4), 524–533. 10.1080/08897077.2014.995332 [DOI] [PubMed] [Google Scholar]
- Ben Amar M (2006). Cannabinoids in medicine: A review of their therapeutic potential. J. Ethnopharmacol, 105(1-2), 1–25. 10.1016/j.jep.2006.02.001 [DOI] [PubMed] [Google Scholar]
- Bidwell LC, Henry EA, Willcutt EG, Kinnear MK, Ito TA (2014). Childhood and current ADHD symptom dimensions are associated with more severe cannabis outcomes in college students. Drug Alcohol Depend, 135, 88–94. 10.1016/j.drugalcdep.2013.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierut T, Krauss MJ, Sowles SJ, Cavazos-Rehg PA (2017). Exploring marijuana advertising on Weedmaps, a popular online directory. Prev. Sci, 18(2), 183–192. 10.1007/s11121-016-0702-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black N, Stockings E, Campbell G, Tran LT, Zagic D, Hall WD, Farrell M, Degenhardt L (2019). Cannabinoids for the treatment of mental disorders and symptoms of mental disorders: A systematic review and meta-analysis. Lancet Psychiatry, 6(12), 995–1010. 10.1016/S2215-0366(19)30401-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackard C, Tennes K (1984). Human placental transfer of cannabinoids. N. Engl. J. Med, 311(12), 797. 10.1056/NEJM198409203111213 [DOI] [PubMed] [Google Scholar]
- Brady KT, Sinha R (2005). Co-occurring mental and substance use disorders: The neurobiological effects of chronic stress. Am. J. Psychiatry, 162(8), 1483–1493. 10.1176/appi.ajp.162.8.1483 [DOI] [PubMed] [Google Scholar]
- Brooks-Russell A, Ma M, Levinson AH, Kattari L, Kirchner T, Anderson Goodell EM, Johnson RM (2019). Adolescent marijuana use, marijuana-related perceptions, and use of other substances before and after initiation of retail marijuana sales in Colorado (2013-2015). Prev. Sci, 20(2), 185–193. 10.1007/s11121-018-0933-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks E, Gundersen DC, Flynn E, Brooks-Russell A, Bull S (2017). The clinical implications of legalizing marijuana: Are physician and non-physician providers prepared? Addict. Behav, 72, 1–7. 10.1016/j.addbeh.2017.03.007 [DOI] [PubMed] [Google Scholar]
- Bull SS, Brooks-Russell A, Davis JM, Roppolo R, Corsi K (2017). Awareness, perception of risk and behaviors related to retail marijuana among a sample of Colorado youth. J. Community Health, 42(2), 278–286. 10.1007/s10900-016-0253-z [DOI] [PubMed] [Google Scholar]
- Campolongo P, Trezza V, Ratano P, Palmery M, Cuomo V (2011). Developmental consequences of perinatal cannabis exposure: Behavioral and neuroendocrine effects in adult rodents. Psychopharmacology (Berl.), 214(1), 5–15. 10.1007/s00213-010-1892-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnevale J (2018). Recommendations for NIDA's cananbis policy research agenda: Report from the Cannabis Policy Research Workgroup. Available from: https://www.drugabuse.gov/sites/default/files/nacda_cannabis_policy_research_workgroup_report_feb_2018.pdf [Google Scholar]
- Cerdá M, Wall M, Feng T, Keyes KM, Sarvet A, Schulenberg J, O’Malley PM, Pacula RL, Galea S, Hasin DS (2017). Association of state recreational marijuana laws with adolescent marijuana use. JAMA Pediatr., 171(2), 142–149. 10.1001/jamapediatrics.2016.3624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan GCK, Hall W, Freeman TP, Ferris J, Kelly AB, Winstock A (2017). User characteristics and effect profile of butane hash oil: An extremely high-potency cannabis concentrate. Drug Alcohol Depend., 178, 32–38. 10.1016/j.drugalcdep.2017.04.014 [DOI] [PubMed] [Google Scholar]
- Chandra S, Radwan MM, Majumdar CG, Church JC, Freeman TP, ElSohly MA (2019). New trends in cannabis potency in USA and Europe during the last decade (2008-2017). Eur. Arch. Psychiatry Clin. Neurosci, 269(1), 5–15. 10.1007/s00406-019-00983-5 [DOI] [PubMed] [Google Scholar]
- Chihuri S, Li G (2019). State marijuana laws and opioid overdose mortality. Inj. Epidemiol, 6, 38. 10.1186/s40621-019-0213-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Civiletto CW, Aslam S, Hutchison J (2020). Electronic delivery (vaping) of cannabis and nicotine.StatPearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430685/ [PubMed] [Google Scholar]
- Clark RR (1994). Marijuana use associated with first episode of psychiatric illness in an adolescent population. Am. J. Addict, 3(1), 67–71. 10.1111/j.1521-0391.1994.tb00228.x [DOI] [Google Scholar]
- Colorado Department of Public Health and Environment. (2020). Medical marijuana registry program statistics. Available from: https://www.colorado.gov/pacific/cdphe/data
- Colorado Department of Public Health and Environment. (2018). Monitoring heatlh concerns related to marijuana in Colorado. Available from: https://colorado.gov/marijuanahealthinfo
- Colorado Department of Revenue. (2020). MED resources and statistics. a Available from: https://www.colorado.gov/pacific/enforcement/med-resources-and-statistics
- Colorado Department of Revenue. (2020). Marijuana tax data. b Available from: https://www.colorado.gov/pacific/revenue/colorado-marijuana-tax-data
- Committee on Substance Abuse, Committee on Adolescence; (2015). The impact of marijuana policies on youth: Clinical, research, and legal update. Pediatrics, 135(3), 584–587. 10.1542/peds.2014-4146 [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Bukstein OG, Douaihy AB, Clark DB, Chung TA, Daley DC, Wood DS, Brown SJ (2010). Double-blind fluoxetine trial in comorbid MDD-CUD youth and young adults. Drug Alcohol Depend., 112(1-2), 39–45. 10.1016/j.drugalcdep.2010.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius JR, Maisto SA, Martin CS, Bukstein OG, Salloum IM, Daley DC, Wood DS, Clark DB (2004). Major depression associated with earlier alcohol relapse in treated teens with AUD. Addict. Behav, 29(5), 1035–1038. 10.1016/j.addbeh.2004.02.056 [DOI] [PubMed] [Google Scholar]
- Di Forti M, Marconi A, Carra E, Fraietta S, Trotta A, Bonomo M, Bianconi F, Gardner-Sood P, O’Connor J, Russo M, Stilo SA, Marques TR, Mondelli V, Dazzan P, Pariante C, David AS, Gaughran F, Atakan Z, Iyegbe C, Powell J, Morgan C, Lynskey M, Murray RM (2015). Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: A case-control study. Lancet Psychiatry, 2(3), 233–238. 10.1016/S2215-0366(14)00117-5 [DOI] [PubMed] [Google Scholar]
- Di Forti M, Morgan C, Dazzan P, Pariante C, Mondelli V, Marques TR, Handley R, Luzi S, Russo M, Paparelli A, Butt A, Stilo SA, Wiffen B, Powell J, Murray RM (2009). High-potency cannabis and the risk of psychosis. Br. J. Psychiatry, 195(6), 488–491. 10.1192/bjp.bp.109.064220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Forti M, Sallis H, Allegri F, Trotta A, Ferraro L, Stilo SA, Marconi A, La Cascia C, Reis Marques T, Pariante C, Dazzan P, Mondelli V, Paparelli A, Kolliakou A, Prata D, Gaughran F, David AS, Morgan C, Stahl D, Khondoker M, MacCabe JH, Murray RM (2014). Daily use, especially of high-potency cannabis, drives the earlier onset of psychosis in cannabis users. Schizophr. Bull, 40(6), 1509–1517. 10.1093/schbul/sbt181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickson B, Mansfield C, Guiahi M, Allshouse AA, Borgelt LM, Sheeder J, Silver RM, Metz TD (2018). Recommendations from cannabis dispensaries about first-trimester cannabis use. Obstet. Gynecol, 131(6), 1031–1038. 10.1097/AOG.0000000000002619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilley JA, Richardson SM, Kilmer B, Pacula RL, Segawa MB, Cerdá M (2019). Prevalence of cannabis use in youths after legalization in Washington state. JAMA Pediatr., 173(2), 192–193. 10.1001/jamapediatrics.2018.4458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy B, Li L, Lu S, Durocher L, Dittmar M, Delaney-Baldwin E, Panawennage D, LeMaster D, Navarette K, Spink D (2020). Analysis of cannabinoid-containing fluids in illicit vaping cartridges recovered from pulmonary injury patients: Identification of vitamin E acetate as a major diluent. Toxics, 8(1), E8. 10.3390/toxics8010008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkins IJ, Saunders GRB, Malone SM, Keyes MA, McGue M, Iacono WG (2018). Associations between childhood ADHD, gender, and adolescent alcohol and marijuana involvement: A causally informative design. Drug Alcohol Depend., 184, 33–41. 10.1016/j.drugalcdep.2017.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito G, Filippis DD, Cirillo C, Iuvone T, Capoccia E, Scuderi C, Steardo A, Cuomo R, Steardo L (2013). Cannabidiol in inflammatory bowel diseases: A brief overview. Phytother. Res, 27(5), 633–636. 10.1002/ptr.4781 [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration. (2020). FDA regulation of cannabis and cannabis-derived products, including cannabidiol (CBD). Available from: https://www.fda.gov/news-events/public-health-focus/fda-regulation-cannabis-and-cannabis-derived-products-including-cannabidiol-cbd#approved
- Fink DS, Stohl M, Sarvet AL, Cerda M, Keyes KM, Hasin DS (2020). Medical marijuana laws and driving under the influence of marijuana and alcohol. Addiction, 115(10), 1944–1953. 10.1111/add.15031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- French L, Gray C, Leonard G, Perron M, Pike GB, Richer L, Séguin JR, Veillette S, Evans CJ, Artiges E, Banaschewski T, Bokde AW, Bromberg U, Bruehl R, Buchel C, Cattrell A, Conrod PJ, Flor H, Frouin V, Gallinat J, Garavan H, Gowland P, Heinz A, Lemaitre H, Martinot JL, Nees F, Orfanos DP, Pangelinan MM, Poustka L, Rietschel M, Smolka MN, Walter H, Whelan R, Timpson NJ, Schumann G, Smith GD, Pausova Z, Paus T (2015). Early cannabis use, polygenic risk score for schizophrenia and brain maturation in adolescence. JAMA Psychiatry, 72(10), 1002–1011. 10.1001/jamapsychiatry.2015.1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gay B, Field Z, Patel S, Alvarez RM, Nasser W, Madruga M, Carlan SJ (2020). Vaping-induced lung injury: A case of lipoid pneumonia associated with E-cigarettes containing cannabis. Case Rep. Pulmonol, 2020, 7151834. 10.1155/2020/7151834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh TS, Vigil DI, Maffey A, Tolliver R, Van Dyke M, Kattari L, Krug H, Reed JK, Wolk L (2017). Lessons learned after three years of legalized, recreational marijuana: The Colorado experience. Prev. Med, 104, 4–6. 10.1016/j.ypmed.2017.02.021 [DOI] [PubMed] [Google Scholar]
- Gilbert CR, Baram M, Cavarocchi NC (2013). “Smoking wet”: Respiratory failure related to smoking tainted marijuana cigarettes. Tex. Heart Inst. J, 40(1), 64–67. [PMC free article] [PubMed] [Google Scholar]
- Gilman JM, Ramchandani VA, Davis MB, Bjork JM, Hommer DW (2008). Why we like to drink: A functional magnetic resonance imaging study of the rewarding and anxiolytic effects of alcohol. J. Neurosci, 28(18), 4583–4591. 10.1523/JNEUROSCI.0086-08.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J, Ware M, Marmorstein N, Cipriani A, Dendukuri N, Mayo N (2019). Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: A systematic review and meta-analysis. JAMA Psychiatry, 76(4), 426–434. 10.1001/jamapsychiatry.2018.4500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt L, Richardson GA, Willford JA, Severtson SG, Day NL (2012). School achievement in 14-year-old youths prenatally exposed to marijuana. Neurotoxicol. Teratol, 34(1), 161–167. 10.1016/j.ntt.2011.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall KE, Monte AA, Chang T, Fox J, Brevik C, Vigil DI, Van Dyke M, James KA (2018). Mental health-related emergency department visits associated with cannabis in Colorado. Acad. Emerg. Med, 25(5), 526–537. 10.1111/acem.13393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammerness P, Petty C, Faraone SV, Biederman J (2017). Do stimulants reduce the risk for alcohol and substance use in youth with ADHD? A secondary analysis of a prospective, 24-month open-label study of osmotic-release methylphenidate. J. Atten. Disord, 21(1), 71–77. 10.1177/1087054712468051 [DOI] [PubMed] [Google Scholar]
- Harpin SB, Brooks-Russell A, Ma M, James KA, Levinson AH (2018). Adolescent marijuana use and perceived ease of access before and after recreational marijuana implementation in Colorado. Subst. Use Misuse, 53(3), 451–456. 10.1080/10826084.2017.1334069 [DOI] [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Grant BF (2015). Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiatry, 72(12), 1235–1242. 10.1001/jamapsychiatry.2015.1858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O’Malley PM, Galea S, Pacula R, Feng T (2015). Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: Results from annual, repeated cross-sectional surveys. Lancet Psychiatry, 2(7), 601–608. 10.1016/S2215-0366(15)00217-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heizer JW, Borgelt LM, Bashqoy F, Wang GS, Reiter PD (2018). Marijuana misadventures in children: Exploration of a dose-response relationship and summary of clinical effects and outcomes. Pediatr. Emerg. Care, 34(7), 457–462. 10.1097/PEC.0000000000000770 [DOI] [PubMed] [Google Scholar]
- Hersh J, Curry JF, Becker SJ (2013). The influence of comorbid depression and conduct disorder on MET/CBT treatment outcome for adolescent substance use disorders. Int. J. Cogn. Ther, 6(4), 325–341. 10.1521/ijct.2013.6.4.325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiemstra M, Nelemans SA, Branje S, van Eijk KR, Hottenga JJ, Vinkers CH, van Lier P, Meeus W, Boks MP (2018). Genetic vulnerability to schizophrenia is associated with cannabis use patterns during adolescence. Drug Alcohol Depend., 190, 143–150. 10.1016/j.drugalcdep.2018.05.024 [DOI] [PubMed] [Google Scholar]
- Hinckley JD, Riggs P (2019). Integrated treatment of adolescents with co-occurring depression and substance use disorder. Child Adolesc. Psychiatr. Clin. N. Am, 28(3), 461–472. 10.1016/j.chc.2019.02.006 [DOI] [PubMed] [Google Scholar]
- Hopfer C (2014). Implications of marijuana legalization for adolescent substance use. Subst. Abus, 35(4), 331–335. 10.1080/08897077.2014.943386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudak M, Severn D, Nordstrom K (2015). Edible cannabis-induced psychosis: Intoxication and beyond. Am. J. Psychiatry, 172(9), 911–912. 10.1176/appi.ajp.2015.15030358 [DOI] [PubMed] [Google Scholar]
- Hunt P, Pacula RL (2017). Early impacts of marijuana legalization: An evaluation of prices in Colorado and Washington. J. Prim. Prev, 38(3), 221–248. 10.1007/s10935-017-0471-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RM, Brooks-Russell A, Ma M, Fairman BJ, Tolliver RL, Jr, Levinson, A.H. (2016). Usual modes of marijuana consumption among high school students in Colorado. J. Stud. Alcohol Drugs, 77(4), 580–588. 10.15288/jsad.2016.77.580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones J, Nicole Jones K, Peil J (2018). The impact of the legalization of recreational marijuana on college students. Addict. Behav, 77, 255–259. 10.1016/j.addbeh.2017.08.015 [DOI] [PubMed] [Google Scholar]
- Keller CJ, Chen EC, Brodsky K, Yoon JH (2016). A case of butane hash oil (marijuana wax)-induced psychosis. Subst. Abus, 37(3), 384–386. 10.1080/08897077.2016.1141153 [DOI] [PubMed] [Google Scholar]
- Kendler KS, Jacobson KC, Prescott CA, Neale MC (2003). Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. Am. J. Psychiatry, 160(4), 687–695. 10.1176/appi.ajp.160.4.687 [DOI] [PubMed] [Google Scholar]
- Kendler KS, Ohlsson H, Sundquist J, Sundquist K (2019). Prediction of onset of substance-induced psychotic disorder and its progression to schizophrenia in a Swedish national sample. Am. J. Psychiatry, 176(9), 711–719. 10.1176/appi.ajp.2019.18101217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HS, Hall KE, Genco EK, Van Dyke M, Barker E, Monte AA (2016). Marijuana tourism and emergency department visits in Colorado. N. Engl. J. Med, 374(8), 797–798. 10.1056/NEJMc1515009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Large M, Nielssen O (2017). Daily use of high-potency cannabis is associated with an increased risk of admission and more intervention after first-episode psychosis. Evid. Based Ment. Health, 20(2), 58. 10.1136/eb-2017-102630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee ML, Novotny M, Bartle KD (1976). Gas chromatography/mass spectrometric and nuclear magnetic resonance determination of polynuclear aromatic hydrocarbons in airborne particulates. Anal. Chem, 48(11), 1566–1572. a 10.1021/ac50005a037 [DOI] [PubMed] [Google Scholar]
- Lee ML, Novotny M, Bartle KD (1976). Gas chromatography/mass spectrometric and nuclear magnetic resonance spectrometric studies of carcinogenic polynuclear aromatic hydrocarbons in tobacco and marijuana smoke condensates. Anal. Chem, 48(2), 405–416. b 10.1021/ac60366a048 [DOI] [PubMed] [Google Scholar]
- LeNoue SR, Salomonsen-Sautel S, Min SJ, Thurstone C (2017). Marijuana commercialization and adolescent substance treatment outcomes in Colorado. Am. J. Addict, 26(8), 802–806. 10.1111/ajad.12634 [DOI] [PubMed] [Google Scholar]
- Levine A, Clemenza K, Rynn M, Lieberman J (2017). Evidence for the risks and consequences of adolescent cannabis exposure. J. Am. Acad. Child Adolesc. Psychiatry, 56(3), 214–225. 10.1016/j.jaac.2016.12.014 [DOI] [PubMed] [Google Scholar]
- Libby AM, Orton HD, Stover SK, Riggs PD (2005). What came first, major depression or substance use disorder? Clinical characteristics and substance use comparing teens in a treatment cohort. Addict. Behav, 30(9), 1649–1662. 10.1016/j.addbeh.2005.07.012 [DOI] [PubMed] [Google Scholar]
- Maccarrone M, Bab I, Biró T, Cabral GA, Dey SK, Di Marzo V, Konje JC, Kunos G, Mechoulam R, Pacher P, Sharkey KA, Zimmer A (2015). Endocannabinoid signaling at the periphery: 50 years after THC. Trends Pharmacol. Sci, 36(5), 277–296. 10.1016/j.tips.2015.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGraw MD, Houser GH, Galambos C, Wartchow EP, Stillwell PC, Weinman JP (2018). Marijuana medusa: The many pulmonary faces of marijuana inhalation in adolescent males. Pediatr. Pulmonol, 53(12), 1619–1626. 10.1002/ppul.24171 [DOI] [PubMed] [Google Scholar]
- Mehmedic Z, Chandra S, Slade D, Denham H, Foster S, Patel AS, Ross SA, Khan IA, ElSohly MA (2010). Potency trends of Δ9-THC and other cannabinoids in confiscated cannabis preparations from 1993 to 2008. J. Forensic Sci, 55(5), 1209–1217. 10.1111/j.1556-4029.2010.01441.x [DOI] [PubMed] [Google Scholar]
- Moatemri Z, Zaibi H, Dabboussi S, Mhamedi S, Aichaouia C, Khadhraoui M, Cheikh R (2016). [Alveolar haemorrhage following a cannabis water pipe]. Rev. Pneumol. Clin, 72(5), 316–319. 10.1016/j.pneumo.2016.03.002 [DOI] [PubMed] [Google Scholar]
- Moir D, Rickert WS, Levasseur G, Larose Y, Maertens R, White P, Desjardins S (2008). A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions. Chem. Res. Toxicol, 21(2), 494–502. 10.1021/tx700275p [DOI] [PubMed] [Google Scholar]
- Molina BSG, Howard AL, Swanson JM, Stehli A, Mitchell JT, Kennedy TM, Epstein JN, Arnold LE, Hechtman L, Vitiello B, Hoza B (2018). Substance use through adolescence into early adulthood after childhood-diagnosed ADHD: Findings from the MTA longitudinal study. J. Child Psychol. Psychiatry, 59(6), 692–702. 10.1111/jcpp.12855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray RM, Quigley H, Quattrone D, Englund A, Di Forti M (2016). Traditional marijuana, high-potency cannabis and synthetic cannabinoids: Increasing risk for psychosis. World Psychiatry, 15(3), 195–204. 10.1002/wps.20341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagarkatti P, Pandey R, Rieder SA, Hegde VL, Nagarkatti M (2009). Cannabinoids as novel anti-inflammatory drugs. Future Med. Chem, 1(7), 1333–1349. 10.4155/fmc.09.93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National academies of science, engineering, and medicine. (2017). The health effects of cannabis and cannabinoids: Current state of evidence and recommendations for research. T. N. A. Press. [PubMed] [Google Scholar]
- Ogden D (2009). Memorandum for selected United States attorneys on investigations and prosecutions in states authorizing the medical use of marijuana Department of Justice. Available from: https://www.justice.gov/sites/default/files/opa/legacy/2009/10/19/medical-marijuana.pdf [Google Scholar]
- Orens A, Light M, Lewandowski B, Rowberry J, Saloga C (2018). Market size and demand for marijuana in colorado 2017 market update. Available from: https://www.colorado.gov/pacific/sites/default/files/MED%20Demand%20and [Google Scholar]
- Orens A, Light M, Rowberry J, Matsen J, Lewandowski B (2015). Marijuana equivalency in proportion and disage: An assessment of physical and pharmacokinetic relationships in marijuana production and consumption in Colorado. Available from: https://www.colorado.gov/pacific/sites/default/files/MED%20Equivalency_Final%2008102015_1.pdf [Google Scholar]
- Pacula RL, Jacobson M, Maksabedian EJ (2016). In the weeds: A baseline view of cannabis use among legalizing states and their neighbours. Addiction, 111(6), 973–980. 10.1111/add.13282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Lundberg R (2014). Why changes in price matter when thinking about marijuana policy: A review of the literature on the elasticity of demand. Public Health Rev, 35(2), 1–18. 10.1007/bf03391701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Powell D, Heaton P, Sevigny EL (2015). Assessing the effects of medical marijuana laws on marijuana use: The devil is in the details. J. Policy Anal. Manage, 34(1), 7–31. 10.1002/pam.21804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Ompad DC, Petkova E (2014). Correlates of intentions to use cannabis among US high school seniors in the case of cannabis legalization. Int. J. Drug Policy, 25(3), 424–435. 10.1016/j.drugpo.2014.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Reyes M, Wall ME (1982). Presence of delta9-tetrahydrocannabinol in human milk. N. Engl. J. Med, 307(13), 819–820. 10.1056/NEJM198209233071311 [DOI] [PubMed] [Google Scholar]
- Perrine CG, Pickens CM, Boehmer TK, King BA, Jones CM, DeSisto CL, Duca LM, Lekiachvili A, Kenemer B, Shamout M, Landen MG, Lynfield R, Ghinai I, Heinzerling A, Lewis N, Pray IW, Tanz LJ, Patel A, Briss PA (2019). Characteristics of a multistate outbreak of lung injury associated with E-cigarette use, or vaping - United States, 2019. MMWR Morb. Mortal. Wkly. Rep, 68(39), 860–864. 10.15585/mmwr.mm6839e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierre JM (2017). Risk factors of increasingly potent cannabis: The joint effects of potency and frequency. Curr. Psychiatr, 16(2), 15–20. [Google Scholar]
- Pierre JM, Gandal M, Son M (2016). Cannabis-induced psychosis associated with high potency “wax dabs”. Schizophr. Res, 172(1-3), 211–212. 10.1016/j.schres.2016.01.056 [DOI] [PubMed] [Google Scholar]
- Popova L, McDonald EA, Sidhu S, Barry R, Richers Maruyama TA, Sheon NM, Ling PM (2017). Perceived harms and benefits of tobacco, marijuana, and electronic vaporizers among young adults in Colorado: Implications for health education and research. Addiction, 112(10), 1821–1829. 10.1111/add.13854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter K, Virtanen H, Luca P, Pacaud D, Nettel-Aguirre A, Kaminsky L, Ho J (2019). Knowledge and practice of harm-reduction behaviours for alcohol and other illicit substance use in adolescents with type 1 diabetes. Paediatr. Child Health, 24(1), e51–e56. 10.1093/pch/pxy075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince MA, Conner BT (2019). Examining links between cannabis potency and mental and physical health outcomes. Behav. Res. Ther, 115, 111–120. 10.1016/j.brat.2018.11.008 [DOI] [PubMed] [Google Scholar]
- Prince MA, Conner BT, Pearson MR (2018). Quantifying cannabis: A field study of marijuana quantity estimation. Psychol. Addict. Behav, 32(4), 426–433. 10.1037/adb0000370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabin RA, George TP (2017). Understanding the link between cannabinoids and psychosis. Clin. Pharmacol. Ther, 101(2), 197–199. 10.1002/cpt.421 [DOI] [PubMed] [Google Scholar]
- Riggs PD, Mikulich-Gilbertson SK, Davies RD, Lohman M, Klein C, Stover SK (2007). A randomized controlled trial of fluoxetine and cognitive behavioral therapy in adolescents with major depression, behavior problems, and substance use disorders. Arch. Pediatr. Adolesc. Med, 161(11), 1026–1034. 10.1001/archpedi.161.11.1026 [DOI] [PubMed] [Google Scholar]
- Riggs PD, Winhusen T, Davies RD, Leimberger JD, Mikulich-Gilbertson S, Klein C, Macdonald M, Lohman M, Bailey GL, Haynes L, Jaffee WB, Haminton N, Hodgkins C, Whitmore E, Trello-Rishel K, Tamm L, Acosta MC, Royer-Malvestuto C, Subramaniam G, Fishman M, Holmes BW, Kaye ME, Vargo MA, Woody GE, Nunes EV, Liu D (2011). Randomized controlled trial of osmotic-release methylphenidate with cognitive-behavioral therapy in adolescents with attention-deficit/hyperactivity disorder and substance use disorders. J. Am. Acad. Child Adolesc. Psychiatry, 50(9), 903–914. 10.1016/j.jaac.2011.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson ZD, Riggs PD (2016). Co-occurring psychiatric and substance use disorders. Child Adolesc. Psychiatr. Clin. N. Am, 25(4), 713–722. 10.1016/j.chc.2016.05.005 [DOI] [PubMed] [Google Scholar]
- Rocky mountain high intensity drug trafficking area. (2020). The legalization of marijuana in Colordao: The impact. Available from: https://www.thenmi.org/wp-content/uploads/2020/10/RMHIDTA-Marijuana-Report-2020-2.pdf
- Rolland B, Geoffroy PA, Jardri R, Cottencin O (2013). Aripiprazole for treating cannabis-induced psychotic symptoms in ultrahigh-risk individuals. Clin. Neuropharmacol, 36(3), 98–99. 10.1097/WNF.0b013e3182908330 [DOI] [PubMed] [Google Scholar]
- Salomonsen-Sautel S, Min SJ, Sakai JT, Thurstone C, Hopfer C (2014). Trends in fatal motor vehicle crashes before and after marijuana commercialization in Colorado. Drug Alcohol Depend, 140, 137–144. 10.1016/j.drugalcdep.2014.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomonsen-Sautel S, Sakai JT, Thurstone C, Corley R, Hopfer C (2012). Medical marijuana use among adolescents in substance abuse treatment. J. Am. Acad. Child Adolesc. Psychiatry, 51(7), 694–702. 10.1016/j.jaac.2012.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarvet AL, Wall MM, Fink DS, Greene E, Le A, Boustead AE, Pacula RL, Keyes KM, Cerdá M, Galea S, Hasin DS (2018). Medical marijuana laws and adolescent marijuana use in the United States: A systematic review and meta-analysis. Addiction, 113(6), 1003–1016. 10.1111/add.14136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheel AH, Krause D, Haars H, Schmitz I, Junker K (2012). Talcum induced pneumoconiosis following inhalation of adulterated marijuana, a case report. Diagn. Pathol, 7, 26. 10.1186/1746-1596-7-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schier JG, Meiman JG, Layden J, Mikosz CA, VanFrank B, King BA, Salvatore PP, Weissman DN, Thomas J, Melstrom PC, Baldwin GT, Parker EM, Courtney-Long EA, Krishnasamy VP, Pickens CM, Evans ME, Tsay SV, Powell KM, Kiernan EA, Marynak KL, Adjemian J, Holton K, Armour BS, England LJ, Briss PA, Houry D, Hacker KA, Reagan-Steiner S, Zaki S, Meaney-Delman D, Group, C.D.C.L.I.R. (2019). Severe pulmonary disease associated with electronic-cigarette-product use - interim guidance. MMWR Morb. Mortal. Wkly. Rep, 68(36), 787–790. 10.15585/mmwr.mm6836e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider KE, Tormohlen KN, Brooks-Russell A, Johnson RM, Thrul J (2019). Patterns of co-occurring modes of marijuana use among Colorado high school students. J. Adolesc. Health, 64(6), 807–809. 10.1016/j.jadohealth.2018.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuermeyer J, Salomonsen-Sautel S, Price RK, Balan S, Thurstone C, Min SJ, Sakai JT (2014). Temporal trends in marijuana attitudes, availability and use in Colorado compared to non-medical marijuana states: 2003-11. Drug Alcohol Depend., 140, 145–155. 10.1016/j.drugalcdep.2014.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevigny EL (2018). The effects of medical marijuana laws on cannabis-involved driving. Accid. Anal. Prev, 118, 57–65. 10.1016/j.aap.2018.05.023 [DOI] [PubMed] [Google Scholar]
- Sevigny EL, Pacula RL, Heaton P (2014). The effects of medical marijuana laws on potency. Int. J. Drug Policy, 25(2), 308–319. 10.1016/j.drugpo.2014.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skoglund C, Brandt L, D’Onofrio B, Larsson H, Franck J (2017). Methylphenidate doses in attention deficit/hyperactivity disorder and comorbid substance use disorders. Eur. Neuropsychopharmacol, 27(11), 1144–1152. 10.1016/j.euroneuro.2017.08.435 [DOI] [PubMed] [Google Scholar]
- Smart R, Caulkins JP, Kilmer B, Davenport S, Midgette G (2017). Variation in cannabis potency and prices in a newly legal market: Evidence from 30 million cannabis sales in Washington state. Addiction, 112(12), 2167–2177. 10.1111/add.13886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens D, Patel JK, Angelo D, Frunzi J (2020). Cannabis butane hash oil dabbing induced lung injury mimicking atypical pneumonia. Cureus, 12(2), e7033. 10.7759/cureus.7033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockings E, Hall WD, Lynskey M, Morley KI, Reavley N, Strang J, Patton G, Degenhardt L (2016). Prevention, early intervention, harm reduction, and treatment of substance use in young people. Lancet Psychiatry, 3(3), 280–296. 10.1016/S2215-0366(16)00002-X [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2017). Key substance use and mental health indicators in the United States: Results from the 2016 national survey on drug use and health. Available from: https://www.samhsa.gov/data/
- Substance abuse and mental health services administration. (2018). 2018 NSDUH annual national report Substance abuse and mental health services administration, center for behavioral health statistics and quality. Available from: https://www.samhsa.gov/data/report/2018-nsduh-annual-national-report [Google Scholar]
- Szutorisz H, DiNieri JA, Sweet E, Egervari G, Michaelides M, Carter JM, Ren Y, Miller ML, Blitzer RD, Hurd YL (2014). Parental THC exposure leads to compulsive heroin-seeking and altered striatal synaptic plasticity in the subsequent generation. Neuropsychopharmacology, 39(6), 1315–1323. 10.1038/npp.2013.352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurstone C, Lieberman SA, Schmiege SJ (2011). Medical marijuana diversion and associated problems in adolescent substance treatment. Drug Alcohol Depend., 118(2-3), 489–492. 10.1016/j.drugalcdep.2011.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tormohlen KN, Brooks-Russell A, Ma M, Schneider KE, Levinson AH, Johnson RM (2019). Modes of marijuana consumption among Colorado high school students before and after the initiation of retail marijuana sales for adults. J. Stud. Alcohol Drugs, 80(1), 46–55. 10.15288/jsad.2019.80.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tormohlen KN, Schneider KE, Johnson RM, Ma M, Levinson AH, Brooks-Russell A (2019). Changes in prevalence of marijuana consumption modes among Colorado high school students from 2015 to 2017. JAMA Pediatr., 173(10), 988–989. 10.1001/jamapediatrics.2019.2627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel L (2018). What really happened after Colorado legalized marijuana? CMAJ, 190(41), E1237–E1238. 10.1503/cmaj.109-5665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND (2004). The reality of comorbidity: Depression and drug abuse. Biol. Psychiatry, 56(10), 714–717. 10.1016/j.biopsych.2004.07.007 [DOI] [PubMed] [Google Scholar]
- Volkow ND, Baler RD, Compton WM, Weiss SR (2014). Adverse health effects of marijuana use. N. Engl. J. Med, 370(23), 2219–2227. 10.1056/NEJMra1402309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Compton WM, Wargo EM (2017). The risks of marijuana use during pregnancy. JAMA, 317(2), 129–130. 10.1001/jama.2016.18612 [DOI] [PubMed] [Google Scholar]
- Volkow ND, Swanson JM, Evins AE, DeLisi LE, Meier MH, Gonzalez R, Bloomfield MA, Curran HV, Baler R (2016). Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: A review. JAMA Psychiatry, 73(3), 292–297. 10.1001/jamapsychiatry.2015.3278 [DOI] [PubMed] [Google Scholar]
- Wang GS (2017). Pediatric concerns due to expanded cannabis use: Unintended consequences of legalization. J. Med. Toxicol, 13(1), 99–105. 10.1007/s13181-016-0552-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang GS, Banerji S, Contreras AE, Hall KE (2020). Marijuana exposures in Colorado, reported to regional poison centre, 2000-2018. Inj. Prev, 26(2), 184–186. 10.1136/injuryprev-2019-043360 [DOI] [PubMed] [Google Scholar]
- Wang GS, Davies SD, Halmo LS, Sass A, Mistry RD (2018). Impact of marijuana legalization in Colorado on adolescent emergency and urgent care visits. J. Adolesc. Health, 63(2), 239–241. 10.1016/j.jadohealth.2017.12.010 [DOI] [PubMed] [Google Scholar]
- Wang GS, Hall K, Vigil D, Banerji S, Monte A, VanDyke M (2017). Marijuana and acute health care contacts in Colorado. Prev. Med, 104, 24–30. 10.1016/j.ypmed.2017.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang GS, Roosevelt G, Le Lait MC, Martinez EM, Bucher-Bartelson B, Bronstein AC, Heard K (2014). Association of unintentional pediatric exposures with decriminalization of marijuana in the United States. Ann. Emerg. Med, 63(6), 684–689. 10.1016/j.annemergmed.2014.01.017 [DOI] [PubMed] [Google Scholar]
- Watson SJ, Benson JA Jr, Joy JE (2000). Marijuana and medicine: Assessing the science base: A summary of the 1999 Institute of Medicine report. Arch. Gen. Psychiatry, 57(6), 547–552. Available from: https://www.ncbi.nlm.nih.gov/pubmed/10839332 10.1001/archpsyc.57.6.547 [DOI] [PubMed] [Google Scholar]
- White AM, Jordan JD, Schroeder KM, Acheson SK, Georgi BD, Sauls G, Ellington RR, Swartzwelder HS (2004). Predictors of relapse during treatment and treatment completion among marijuana-dependent adolescents in an intensive outpatient substance abuse program. Subst. Abus, 25(1), 53–59. 10.1300/J465v25n01_08 [DOI] [PubMed] [Google Scholar]
- Wilens TE, Upadhyaya HP (2007). Impact of substance use disorder on ADHD and its treatment. J. Clin. Psychiatry, 68(8), e20. 10.4088/JCP.0807e20 [DOI] [PubMed] [Google Scholar]
- Wilson J, Freeman TP, Mackie CJ (2019). Effects of increasing cannabis potency on adolescent health. Lancet Child Adolesc. Health, 3(2), 121–128. 10.1016/S2352-4642(18)30342-0 [DOI] [PubMed] [Google Scholar]
- Wilson KM, Torok MR, Wei B, Wang L, Lowary M, Blount BC (2018). Marijuana and tobacco coexposure in hospitalized children. Pediatrics, 142(6), e20180820. 10.1542/peds.2018-0820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winhusen TM, Lewis DF, Riggs PD, Davies RD, Adler LA, Sonne S, Somoza EC (2011). Subjective effects, misuse, and adverse effects of osmotic-release methylphenidate treatment in adolescent substance abusers with attention-deficit/hyperactivity disorder. J. Child Adolesc. Psychopharmacol, 21(5), 455–463. 10.1089/cap.2011.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]