Abstract
The scapulothoracic, acromioclavicular and sternoclavicular joints play a fundamental role in the shoulder function. Shoulder complex kinematics have been studied with different methods using: goniometers, 2 static radiographs, 3D motion analyzers (invasive or noninvasive) and digital inclinometers. Goniometers have been used traditionally to assess scapular rotation in relation to the thorax. The intrinsic limit of multiple static two-dimensional shoulder radiographs is the attempt of describing in two what is occurring in three dimensions. Technology innovations have led to the development of the 3D shoulder complex kinematics analysis ETS (Electromagnetic tracking systems) using sensors (invasive bone-pin markers or noninvasive skin surface marker) stitched to the scapula/clavicula, thorax, and humerus. Despite being uncomfortable, invasive 3D motion cortical pins analyzers still represent the current gold standard for tracking shoulder complex kinematics. Therefore, access to three-dimensional biomechanical instrumentations for collecting kinematic data represents an active problem for many physicians. A precise, easy to use and low-cost non-invasive method able to draw and analyze the kinematics of the shoulder complex has not been developed yet. Further researches are necessary to design a new non-invasive method able to draw and analyze the kinematics of the scapula and the whole shoulder complex, precisely.
Keywords: scapulothoracic, acromioclavicular, sternoclavicular, Shoulder complex
Shoulder Complex kinematics
No other joint has a range of motion as wide as that of the shoulder complex. The shoulder girdle to move properly requires the combined motions of 4 joints: the scapulothoracic (ST), sternoclavicular (SC), acromioclavicular AC) and glenohumeral (GH). 1
The ST joint is a complex anatomical structure having a fundamental role in the function of the shoulder. Due to the absence of osseous or ligamentous connections with the thorax, the scapula is kept in position by its muscular attachments to the head, vertebral column and sternum, including the rhomboid major, rhomboid minor, elevator scapulae, subclavius, trapezius, serratus anterior, and pectoralis minor muscles. 1
The scapulothoracic joint is characterized by the rotation and translation of the scapula on the surface of the rib cage. Abduction-adduction and elevation-depression locate the origin of the joint reference frame on the rib cage surface. 2
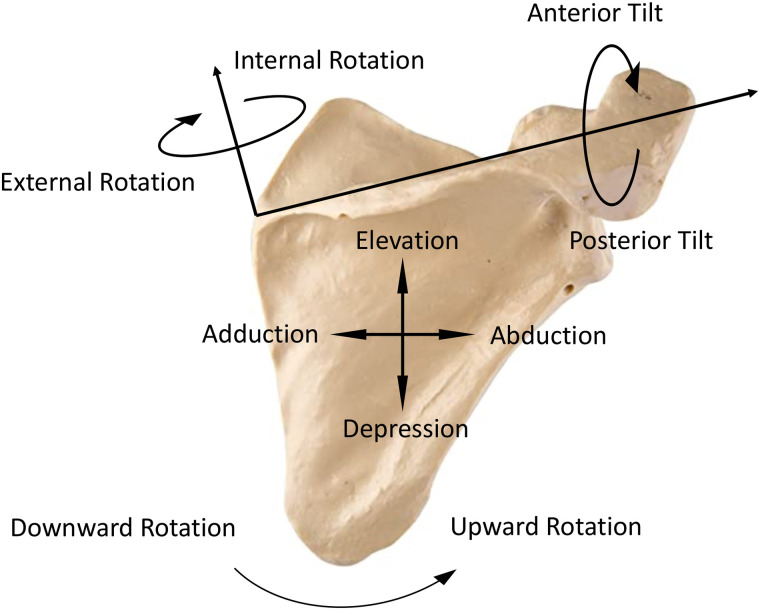
Scapula rotates in 3 planes: upward/downward and internal/external rotations relatively in the scapular and transverse plane and anterior/posterior tilting in the sagittal plane (Figure 1). 3
Figure 1.
Motions of the scapula are defined as internal-external rotation, upward-downward rotation and anterior-posterior tilting.
Ludewig et al. 4 showed that at rest, the scapula is located on the thoracic surface with 5.4° and 41.1° of relatively upward and internal rotation and 13.5° of anterior tilt.
The scapula moves on the rib cage and rotates in the three planes to maintain congruity with it. 2
The sum of anterior translation and internal rotation is usually referred to as scapular protraction. Whereas the sum of posterior translation and external rotation is referred to as scapular retraction. 1
While elevating the arm the normal scapulothoracic motions involve posterior tilting, upward and either internal or external rotation. 5
The opposite rotations are carried out while lowering the arm. No significant differences have been outlined in posterior tilting, and upward or internal-external rotation between dominant and non-dominant arms in healthy patients. 6
According to Yano et Al., 6 healthy patients might be divided into two groups relating to the type of scapular motion. The first group is characterized by a downward rotation of the scapula at the initial phase of elevation and an upward rotation at the terminal phase of lowering. Whereas the second group has a scapula rotating only upward and not rotating downward respectively during the initial phase of elevation and terminal phase of lowering.
Altered scapular motion and position have been termed scapular dyskinesis, may be the cause or the consequence of a shoulder injury, exacerbating shoulder symptoms. 7
This condition, which affects shoulder function, might be caused by multiple factors: thoracic kyphosis, clavicle fracture, AC instability, cervical radiculopathy, long thoracic or spinal accessory nerve palsy and periscapular muscles tightness.
Decreased upward and internal rotation might be caused by decreased serratus anterior activation. A tight pectoralis minor limits scapular posterior tilt or external rotation.
Inhibition of the subscapularis, lower trapezius and serratus anterior, coupled with increased activation of pectoralis minor and latissimus dorsi, have been demonstrated to place the scapula in a protracted position.
In other cases, dyskinesis might cause several types of shoulder diseases such as impingement (decreasing the subacromial space), instability (increasing the strain on the anterior or posterior GH ligaments), frozen shoulder and rotator cuff (RC) lesions.3,7
The Scapular upward rotation, which is the predominant scapular motion during shoulder elevation, and the posterior tilting, are thought to be functionally fundamental to avoid the humeral head and the RC tendons impinging under the anterior aspect of the acromion during shoulder elevation. 3
The dynamic alteration of the humeral head and acromion positions may create increased pressure within the subacromial space, leading to bursal impingement and/or rotator cuff tear. 7
It may also affect the glenohumeral contact pressure: a scapular position in increased downward and internal rotation, which is frequently seen in patients with dyskinesis, leads to a greater contact pressure of the humerus with the posterosuperior glenoid.
The altered position and motion of internal rotation and anterior tilt is believed to change GH alignment, placing increased tensile strain on the anterior ligaments.
Debated is whether the observed scapular dyskinesis is a cause or an effect (compensation) for rotator cuff pathology. Several studies have demonstrated an increased scapular upward rotation in patients with demonstrated rotator cuff tears. 8
The theory according to which the increased scapular upward rotation in patients with RCT may be compensatory, in an attempt to increase arm elevation seems most likely. 8
The scapular winging is referred to as the raising of the medial and inferior or lateral border off the surface of the rib cage, with the medial being the more common type. Medial winging is frequently the result of serratus anterior paralysis from injury to the long thoracic nerve. Lateral winging might be caused by trapezius paralysis due to spinal accessory nerve injury. However, acute traumatic tears of the serratus anterior, trapezius, and rhomboids off of the scapula are important and under-recognized causes of scapular winging. 9
Acromioclavicular joint motion is referred to as the motion of the scapula relative to the clavicle. The laxity of the Acromioclavicular joint alters the clavicle-scapular link, which needs to be rigid to work properly. As the arm is elevated overhead, the scapula motion relative to the clavicle is characterized by internal rotation, upward and posterior tilting. 4
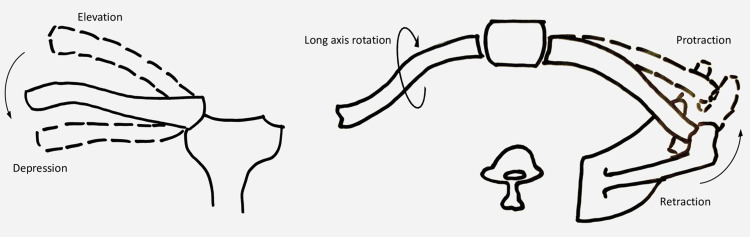
Furthermore, the motions of the clavicle relative to the thorax (Sternoclavicular joint) are referred to as protraction-retraction, elevation-depression and anterior-posterior long-axis rotation. (Figure 2)4,10
Figure 2.
Motion permitted at the sternoclavicular joint: elevation-depression, protraction-retraction, and anterior-posterior long-axis rotation.
The mean clavicular position at rest includes modest elevation, retraction and neutral long-axis rotation. 10
The coupled and coordinated movement between the humerus and the scapula, allowing placement of the arm in the optimum position and achievement of the proper motion to accomplish tasks, is very important in the scapulohumeral rhythm.
Due to the direct mechanical contact of the scapula to the clavicle, the motion of the scapula relative to the thorax is enabled only by combined and simultaneous motion at the acromioclavicular and sternoclavicular joints. 10
Since the motion takes place at the glenohumeral joint, the position of the scapula is relatively unchanged during the first 30 degrees of abduction. To contribute 40 degrees to abduction approximately, the scapula and clavicle rotate counterclockwise about an axis that extends from the sternoclavicular joint to the medial edge of the scapular spine. The sternoclavicular joint gets rigid at approximately 100 degrees of abduction and continued counter-clockwise rotation of the scapula occurs about the acromioclavicular joint, this action contributes an additional 20 degrees to abduction. 1
Therefore the complete scapulothoracic upward rotation, which occurs during humeral elevation, is achieved in a greater percentage through the acromioclavicular joint, with upward rotation of the scapula relative to the clavicle resulting in a total of 40°of scapulothoracic upward rotation, and also through the sternoclavicular joint (motion of the clavicle relative to the thorax). 1
From the initial resting position, the motion at the sternoclavicular joint during elevation is characterized by increasing elevation, posterior axial rotation of the clavicle relative to the thorax and retraction.10,11
Both posterior long-axis rotation at the SC joint and elevation occur with upward rotation of the scapula on the thorax. Also, protraction and retraction of the clavicle at the SC joint occur with respectively scapular internal and external rotation whereas posterior long-axis rotation of the clavicle at the SC joint occur with scapular posterior tipping.4,12
Clinical evaluation
The ability for surgeons to collect relevant kinematic data depends on the validity and reliability of the instrumentation being utilized. To obtain a real understanding of physiologic and non-physiologic movement, the ability to measure shoulder complex kinematics objectively is the key and could assist surgeons in a more precise diagnosis and management of shoulder dysfunction. Frontal (anterior-posterior) and sagittal (lateral) views should be evaluated in Shoulder complex evaluation. 13
Observation of resting shoulder complex position, useful to evaluate possible side-to-side asymmetry, can be utilized with the patient positioning both hands on ipsilateral hips relaxed beside his body. 13
The patient must raise repeatedly the arms to the maximal elevation, extending the elbows in the scapular, sagittal, and coronal plane and subsequently letting them down to the starting position. 14
Analysis of different rotational motions of the shoulder complex is carried out comparing dominant and nondominant arms. 13
Defective scapular positioning patterns might be revealed by the addition of weights during shoulder movements.
Because the coordination of movements and much of the stability of the scapula to the thorax is determined by the active participation of scapulohumeral and axioscapular muscles, a fatigue protocol might be performed by the subjects before the examination to facilitate the finding of the dysfunction. 14 Series of arm elevation with sub-maximal loads and holding the push-up plus position are performed until fatigue is apparent. 14
It appears difficult to accurately measure and distinguish shoulder kinematics between symptomatic and asymptomatic individuals due to several factors which include shoulder mechanics associated with the movement of muscle, fat and skin to the scapula. 2
The scapular examination can be performed from the posterior aspect in almost the totality of the cases. The medial border of the scapula should be located parallel to the thorax midline. 1
Observation of scapular positioning, mainly motion of the medial border, occurring during shoulder movement allows surgeons to diagnose scapular dyskinesis. Protrusion of any aspect of the medial scapular border on the symptomatic side is classified as “yes” (protrusion detected) or “no” (protrusion not detected). 15
Palpating the movement of the lower angle of the scapula is easy and might be a useful method to diagnose scapular dyskinesis. Asymmetry seems to be frequent either in symptomatic and asymptomatic individuals. 1
The Scapular Assistance Test (SAT) evaluates scapular and acromial involvement in subacromial impingement.
The examiner manually stabilizes and pushes gently, relatively the superior border and inferior medial angle of the scapula as the arm moves during forward and abduction to eliminate or modify the impingement symptoms. The examiner assists serratus anterior and lower trapezius muscle activity during scapular upward rotation as the arm is elevated.
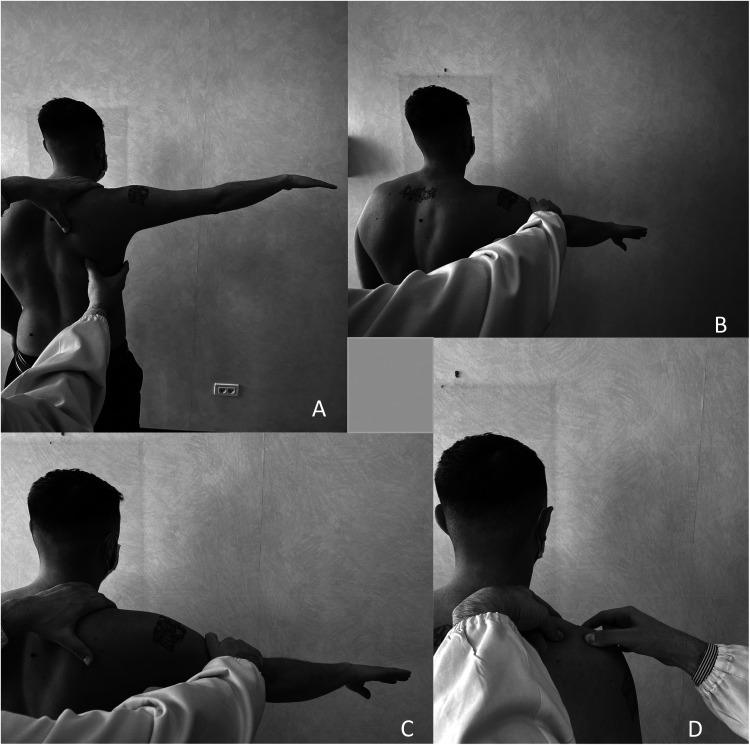
A positive test is defined by the relief of the pain related to the arc of impingement and ROM increased (Figure 3).
Figure 3.
A) The scapular assistance test The Examiner stabilizes the superior border of the scapula and assists Serratus anterior and lower trapezius muscles during scapular upward rotation. B) The Scapular Retraction Test (Phase 1). The Examiner performs an Empty can manual muscle test to assess supraspinatus muscle strength. C) The Scapular Retraction Test (Phase 2). The Examiner stabilizes the medial scapular border and reapplies the muscle test D) Clinical Assessment of acromioclavicular joint laxity in a patient with suspected scapular dyskinesis. The clavicle is stabilized, and an anteroposterior force is applied to the distal end of the acromion.
The Scapular Retraction Test (SRT) involves two phases. An Empty can manual muscle test is performed by the examiner to study supraspinatus muscle strength (Figure 4). Subsequently, the test is repeated with the examiner manually stabilizing the scapula in a retracted position on the thorax. This position confers a stable base of origin for the rotator cuff and often will improve tested rotator cuff strength. The test is positive when supraspinatus strength increases with the scapula in the retracted position (Figure 3). 16
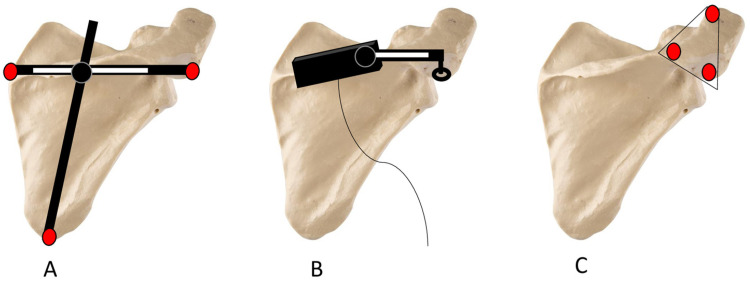
Figure 4.
Schematic diagram showing a subject with scapula locator (A), scapula tracker (B), and acromial method (C).
The Lateral Scapular Slide Test (LSST) is performed to detect scapular asymmetry. The distances individuated from the inferior angle of the scapula and the closest spinous process placed at the same level are measured on both sides while holding three arm positions. Firstly, the patient maintains the arms down by the sides, then actively places both hands on the ipsilateral hips with the humerus positioned in medial rotation at ± 45°of abduction. In the end, the patient, extending both elbows, actively elevates and maximally internally rotates with thumbs down both arms at or below 90°in the coronal plane. 13
For Scapular Winging the diagnosis is made clinically. The alignment of the scapula is assessed from behind and compared side to side for asymmetry. Stabilization of the scapula against the thorax will relieve the discomfort and improve forward flexion. The evaluation of serratus anterior dysfunction includes also the scapular assistance test, simulating the serratus anterior muscle and the Serratus Anterior Test, which is carried out by asking the patient to face a wall and then push against the it with flat palms. 9
The stability of the SC and AC joints should be also evaluated. AP laxity of the AC joint is clinically determined by stabilizing the clavicle with one hand while grasping and mobilizing the acromion with the other hand in an AP direction (Figure 3). 15
Therefore, the clavicle should be assessed for shortening, angulation, or malrotation.
Imaging instruments
Shoulder complex kinematics has been studied clinically and radiographically with different methods.
Goniometers have been used traditionally to assess scapular rotation in relation to the thorax. 13
Furthermore, mainly in the past, participants were exposed to radiographs to assess static two-dimensional motions of the shoulder complex. This method has the intrinsic limit of describing in two what is occurring in the three dimensions.17,18
The obstacle in tracking the movements of the scapula appears to be the main obstacle to analyzing three-dimensional shoulder movements. As previously said, differently from the superior and inferior extremity segments, the scapula rotates and glides right below layers of skin and soft tissues. 18
Technology innovations have led to an invasive or noninvasive 3D shoulder complex kinematics analysis both using electromagnetic tracking systems (ETS). 6
Through ETSs the physicians can individuate the position and orientation of sensors in space. 19
This technology comprises a low-frequency electromagnetic field transmitter, some sensors (receivers), a stylus (digitizer) palpating and digitizing landmarks to create a local coordinate system (LCS) based on the shoulder complex anatomy, and a system unit. All the points of reference are located on the surface and could be positioned instantly with the digitizer connected to the magnetic tracking device. The center of the humeral head represents the only exception, which must be individuated as the least-moving point of the humerus in relation to the scapula when the humerus is moved through short arcs. 3
The Recommendations of the International Society of Biomechanics delineate the LCS. Incisura jugularis, xiphoid process, the C7 and T8 spinous process are used as thoracic landmarks; lateral epicondyle, medial epicondyle and the glenohumeral rotation center are used as humeral landmarks; the acromial angle, trigonum spinae, inferior angle and coracoid process are used as scapular landmarks. Clavicular points of reference include the anterosuperior SC and AC joints on the proximal and distal clavicle respectively. 3
Electromagnetic sensors (invasive bone-pin marker20,21 or noninvasive skin surface marker) stitched to the scapula/clavicula, thorax, and humerus are used to individuate shoulder complex kinematics in the three dimensions.
Studies define ETS as valid and reliable to collect, for the shoulder complex, static and dynamic kinematic data. 22
The noninvasive markers are placed on the skin over different anatomical landmarks enabling the measurement of the anatomical segment kinematics. 22
However, since the position of noninvasive skin markers might be offset from the exact location of bony points of reference, invasive transcutaneous cortical pins still represent the current gold standard for tracking shoulder complex kinematics.
Although cortical pins provide a way to directly collect bone kinematic data, they are not comfortable for the patient. 21
Three ETS noninvasive methods have been described to draw scapula orientation: Scapula locator, Scapula tracker method, and acromial method. (Figure 4)17,18
The validity of new methods is usually assessed by comparing data being collected concurrently with the gold standard invasive approach. Estimation of skin motion artifact is represented by the differences between bone and skin-based measurements. 17
The Scapula locator consisted of a housing supporting three rods, being placed on the posterolateral acromial angle, the inferior angle of the scapula, and the root of the scapular spine. An electromagnetic sensor allows the orientation of the locator relative to the thorax, using ETS during quasi-static trials. Participants move to and hold selected positions at the same time the scapula locator is used to gather orientation data. (Figure 4A)22,23
The Scapula tracker method involves the development of a personalized scapular tracker consisting of three parts: a base, an adjustable arm, and a footpad. The base is stitched to the skin, right over the spine of the scapula. The arm lengthens from the base reaching the acromion and it is affixed to it via the footpad. An ETS sensor is linked to the base allowing dynamic tracking of three-dimensional scapular kinematics. (Figure 4B)17,22
The Acromial method is a skin-fixed method using an ETS sensor adhered to the postero-lateral side of the acromion. This site results very accurately for scapula tracking because of the vicinity of the acromion to the skin, moving closely with it (Figure 4C).
This method, as opposed to the scapula locator and the scapula tracker, is more comfortable, permits dynamic tracking of the scapula without restricting the motions of subjects and does not necessitate personalized designed equipment.17,18,22
Two other methods have been proposed to analyze shoulder complex dynamics, instead of electromagnetic systems: a video motion capture analysis utilizing reflective cutaneous markers adhered to the skin and digital inclinometers.18,24
Despite the digital inclinometer has neither the ability to record three-dimensional nor dynamic shoulder movements, it provides clinically meaningful measures of complex two-dimensional shoulder kinematic data. 13
Current clinical practice
Careful clinical physical examination mainly discriminates among patients demonstrating or not scapular dyskinesis, therefore modifying the treatment approach. The presence of dyskinesis as part of the etiology of shoulder symptoms will be a key component for rehabilitation, with mobilization and strengthening of respectively the tight anterior and periscapular stabilizer muscles.
A positive SAT, which is assessed in patients with altered upward rotation and anterior/posterior tilt, might explain in part the shoulder symptoms and would lead to an adapted treatment including increased flexibility in pectoralis minor and short head of the biceps. 7
In patients with positive SRT, the treatment is modified to improve scapular stability as the first step in the rehabilitation process. 7
However, the qualitative physical methods assessing scapular dyskinesis have been assessed by several authors and have not showed high reliability values, limiting their use in clinical practice.25,26 This has led to search for new methods with higher reliability values.
Although several techniques have been proposed to evaluate and study quantitatively the scapular motion, there is still limited understanding of this joint kinetics and its relationship with the risk of rotator cuff, glenoid labrum and subacromial bursae injury. This is the main reason explaining why those methods are still used mainly for research purpose. Furthermore, unlike studies evaluating qualitative methods, which are of moderate methodological quality, the studies assessing quantitative methods for scapular dyskinesis diagnosis are of low methodological quality.25,26
Greater investigation is necessary to deepen the physiologic scapular motion and position before those will be used worldwide for clinical diagnosis.
An increased knowledge of scapular motion with better biomechanical models will assist in the diagnostic challenge surrounding shoulder pain of unknown etiology and aid in the development of specific treatment strategies, with a “menu à la carte” for each of the factor leading to scapular dyskinesis.
Conclusion
Existing literature studying three-dimensional scapular orientation during humeral elevation, varies in: instrumentation used, planes of analysis, definitions of axis orientations, measuring range, trunk position, types of subjects and the use of static versus dynamic motion. Invasive Cortical Pins still represent the current gold standard for tracking shoulder complex kinematics despite being uncomfortable.
Therefore, access to three-dimensional biomechanical instrumentations for collecting kinematic data represents an active problem for many physicians. Also, the time needed to use ETS seems to be excessive to use in a daily working routine. Doctors should have access to simple instrumentations which are either cost-effective and practical. 22
Further research is necessary to design a new non-invasive method able to draw and analyze the kinematics of the scapula and the whole shoulder complex, precisely and with a high reliability.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Edoardo Giovannetti de Sanctis https://orcid.org/0000-0002-6012-1651
References
- 1.Frank RM, Ramirez J, Chalmers PNet al. et al. Scapulothoracic anatomy and snapping scapula syndrome. Anat Res Int 2013; 2013: 635628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seth A, Matias R, Veloso AP, et al. A biomechanical model of the scapulothoracic joint to accurately capture scapular kinematics during shoulder movements. PLoS One 2016; 11: e0141028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borstad JD, Ludewig PM. Comparison of scapular kinematics between elevation and lowering of the arm in the scapular plane. Clin Biomech (Bristol, Avon) 2002; 17: 650–659. [DOI] [PubMed] [Google Scholar]
- 4.Ludewig PM, Phadke V, Braman JPet al. et al. Motion of the shoulder complex during multiplanar humeral elevation. J Bone Joint Surg Am 2009; 91: 378–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Umehara J, Yagi M, Hirono Tet al. et al. Relationship between scapular initial position and scapular movement during dynamic motions. PLoS One 2019; 14: e0227313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yano Y, Hamada J, Tamai K, et al. Different scapular kinematics in healthy subjects during arm elevation and lowering: glenohumeral and scapulothoracic patterns. J Shoulder Elbow Surg 2010; 19: 209–215. [DOI] [PubMed] [Google Scholar]
- 7.Kibler WB, Ludewig PM, McClure PWet al. et al. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘scapular summit’. Br J Sports Med 2013; 47: 877–885. [DOI] [PubMed] [Google Scholar]
- 8.Barcia AM, Makovicka JL, Group MS, et al. Scapular motion in the presence of rotator cuff tears: a systematic review. J Shoulder Elbow Surg 2021; 30: 1679–1692. [DOI] [PubMed] [Google Scholar]
- 9.Didesch JT, Tang P. Anatomy, etiology, and management of scapular winging. J Hand Surg Am 2019; 44: 321–330. [DOI] [PubMed] [Google Scholar]
- 10.Ludewig PM, Behrens SA, Meyer SMet al. et al. Three-dimensional clavicular motion during arm elevation: reliability and descriptive data. J Orthop Sports Phys Ther 2004; 34: 140–149. [DOI] [PubMed] [Google Scholar]
- 11.Sahara W, Sugamoto K, Murai Met al. et al. 3D Kinematic analysis of the acromioclavicular joint during arm abduction using vertically open MRI. J Orthop Res 2006; 24: 1823–1831. [DOI] [PubMed] [Google Scholar]
- 12.Teece RM, Lunden JB, Lloyd ASet al. et al. Three-dimensional acromioclavicular joint motions during elevation of the arm. J Orthop Sports Phys Ther 2008; 38: 181–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Struyf F, Nijs J, Mottram Set al. et al. Clinical assessment of the scapula: a review of the literature. Br J Sports Med 2014; 48: 883–890. [DOI] [PubMed] [Google Scholar]
- 14.Miachiro NY, Camarini PM, Tucci HTet al. et al. Can clinical observation differentiate individuals with and without scapular dyskinesis? Braz J Phys Ther 2014; 18: 282–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kibler WB, Sciascia A, Wilkes T. Scapular dyskinesis and its relation to shoulder injury. J Am Acad Orthop Surg 2012; 20: 364–372. [DOI] [PubMed] [Google Scholar]
- 16.Kibler WB, Sciascia A, Dome D. Evaluation of apparent and absolute supraspinatus strength in patients with shoulder injury using the scapular retraction test Am J Sports Med 2006; 34: 1643–1647. [DOI] [PubMed] [Google Scholar]
- 17.Karduna AR, McClure PW, Michener LA, et al. Dynamic measurements of three-dimensional scapular kinematics: a validation study. J Biomech Eng 2001; 123: 184–190. [DOI] [PubMed] [Google Scholar]
- 18.Hoard RW, 2nd, Janes WE, Brown JMet al. et al. Measuring scapular movement using three-dimensional acromial projection. Shoulder Elbow 2013; 5: 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roy JS, Moffet H, Hebert LJet al. et al. The reliability of three-dimensional scapular attitudes in healthy people and people with shoulder impingement syndrome. BMC Musculoskelet Disord 2007; 8: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McClure PW, Michener LA, Sennett BJ, et al. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg 2001; 10: 269–277. [DOI] [PubMed] [Google Scholar]
- 21.Bourne DA, Choo AM, Regan WDet al. et al. Three-dimensional rotation of the scapula during functional movements: an in vivo study in healthy volunteers. J Shoulder Elbow Surg 2007; 16: 150–162. [DOI] [PubMed] [Google Scholar]
- 22.Hannah DC, Scibek JS. Collecting shoulder kinematics with electromagnetic tracking systems and digital inclinometers: a review. World J Orthop 2015; 6: 783–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson GR, Stuart PR, Mitchell S. A method for the measurement of three-dimensional scapular movement. Clin Biomech (Bristol, Avon) 1993; 8: 269–273. [DOI] [PubMed] [Google Scholar]
- 24.Janes WE, Brown JM, Essenberg JM, et al. Development of a method for analyzing three-dimensional scapula kinematics. Hand 2012; 7: 400–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paraskevopoulos E, Papandreou M, Gliatis J. Reliability of assessment methods for scapular dyskinesis in asymptomatic subjects: a systematic review. Acta Orthop Traumatol Turc 2020; 54: 546–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lange T, Struyf F, Schmitt Jet al. et al. The reliability of physical examination tests for the clinical assessment of scapular dyskinesis in subjects with shoulder complaints: a systematic review. Phys Ther Sport 2017; 26: 64–89. [DOI] [PubMed] [Google Scholar]