Abstract
This study examined Oregon’s early intervention (EI) and early childhood special education (ECSE) pipelines as a function of children’s intersecting ethnicity and home language(s) with a focus on children from Latino/a backgrounds with communication disorders. We found differences in children’s referral source and age of referral, likelihood of evaluation and placement, and type of placement for conditions related to communication, including autism spectrum disorder and hearing impairment. Results showed differences in EI and ECSE; however, disproportionality appeared greatest among Spanish-speaking Latino/a children and non-Latino/a children who spoke languages other than English compared to non-Latino/a English-speaking counterparts. Our findings suggest attending to children’s intersecting ethnicity and language backgrounds in referral, evaluation, and placement add nuance to examinations of disproportionality. Results also indicate that practices related to characterizing children’s communication disorders likely make substantial contributions to inequities in EI and ECSE. Precise identification of differences in service provision can lead to targeted policy and practice solutions to reduce structural barriers to care in EI/ECSE systems and improve equity, particularly as related to placement for children of color with communication concerns.
The United States Individuals with Disabilities Education Act (IDEA, 2004) mandates that states provide eligible children with disabilities early intervention (EI) and early childhood special education services (ECSE). To access services, children move along a pipeline that begins with a referral to IDEA Part C EI (birth to age 3) or IDEA Part B ECSE (ages 3 to 5). The process continues with evaluation and terminates with an eligibility decision that may result in special education placement. IDEA mandates that this pipeline be free of cultural and linguistic bias. Knowing how we are meeting this mandate with the growing population of children of color and who are learning languages other than English is especially important. Approximately 48% of children in EI and ECSE are from underrepresented racial, ethnic, and, relatedly, linguistic backgrounds (US Department of Education [DOE], 2022). Most (about 25%) are identified as Hispanic or Latino (herein: Latino/a). Latino/a children and children from non-White backgrounds are often learning languages other than or in addition to English at home (Romo et al., 2018). Ensuring less biased evaluation and services provision may be particularly challenging for Latino children when they are seen for communication concerns, which are common in EI and ECSE: 40% of children in EI (Hebbeler et al., 2007) and ECSE (US DOE, 2022) are eligible due to primary disorders in speech, language, and/or general communication. Additionally, 2% and 4% of children in EI qualify for a hearing impairment (HI) or social challenges (e.g., autism spectrum disorder [ASD]), presenting with concomitant disabilities in communication. In ECSE, approximately 40% of children qualify for developmental delay (often with communication delay), and 12% for ASD (US DOE, 2022). Thus, this study investigates adherence to equity across the EI/ECSE service pipeline with a specific emphasis on children who are Latino/a and who have communication concerns.
Disparities in EI and ECSE
Disproportionality in participation of non-White children in special education was first identified over 50 years ago (Dunn, 1968), and widespread inequities in EI and ECSE persist. Such inequities have been tied to differences in cultural perspectives on disability, decreased access to primary care, limited information available in languages other than English or bilingual providers, poor outreach to and collaboration with families, few culturally and linguistically appropriate evaluation tools, infrequent implementation of least-biased assessment practices, difficulties distinguishing disability from natural differences based on language exposure, culture, and/or experience, provider bias and discrimination toward children of color, and restrictive policies and funding (e.g., Hardin et al., 2009; Huerta et al., 2021; Sapiets et al., 2020; Wolfe & Durán, 2013; Zuckerman et al., 2014). Ultimately, systemic racism or the systematic, long-standing marginalization of communities of color within US institutions, underlies these challenges (Blanchard et al., 2021). Yet, despite efforts to address disproportionality in the 2004 reauthorization of IDEA (20 U.S.C. § 1418(d)(1); 2004) and a growing understanding of factors impacting equity in special education, the US Department of Education’s (2022) most recent report indicated continued disparities in EI/ECSE enrollment by child race and ethnicity. Dismantling structural racism to improve special education access for young children of color is necessary to support the developmental and academic outcomes of children with disabilities and meet IDEA mandates (Blanchard et al., 2021; Meek et al., 2020).
To develop targeted solutions which enhance equity for young children of color with communication concerns, we must precisely identify at which points in the EI/ECSE system, from referral to placement, outcomes differ for specific groups of children and families (Nalani et al., 2021). We also must use an intersectional lens that recognizes that children’s multiple marginalized identities interact in the production of discrimination and exclusion in EI/ECSE systems (Annamma et al., 2013; Love & Beneke, 2021). Simply defined, intersectionality is the idea that children’s race/ethnicity, linguistic background, and disability type (among other characteristics) “operate not as unitary, mutually exclusive entities, but as reciprocally constructing phenomena that in turn shape complex social inequities” (Collins, 2015; p. 2). In particular, attention to the home languages of Latino/a children with disabilities as well as their ethnic affiliations permits a nuanced understanding of the equity challenges faced by linguistic subgroups within this diverse population (i.e., families who speak primarily Spanish, primarily English, or both Spanish and English) and acknowledges the persistent institutional stigmatization of non-English languages (Rosa & Flores, 2017). However, prior studies of EI/ECSE disparities have largely focused on examining differences by child race/ethnicity alone at a single step in the EI/ECSE process. This research is reviewed next to provide foundational insight into the experiences of children with disabilities who are Latino/a.
The EI/ECSE Pipeline: From Referral to Placement
Children’s EI or ECSE encounter begins with a referral from anyone, including parents, teachers, or medical providers. Though variable, the average age of EI referral is 15.5 months (Hebbeler et al., 2007). Information is not available on age of referral to ECSE or on common referral sources in EI/ECSE. Following referral, children may receive a full developmental evaluation depending on state-specific regulations and/or parental preference. While ECSE evaluation rates have not been documented, the evaluation rates in EI appear to vary widely across states. Data from Massachusetts, Pennsylvania, Colorado, and Oregon suggest that anywhere between 5% and 88% of children referred to EI are evaluated (Atkins et al., 2020; Clements et al., 2008; Conroy et al., 2018; Jimenez et al., 2014; McManus et al., 2020). After evaluation, eligibility for IDEA services is determined per state-established criteria. If eligible, the EI/ECSE team (including parents) determines a disability category and places the child in services. Specific to eligibility for speech-language services, providers are expected to meet the challenge of distinguishing the natural influence of children’s home languages and cultures on early communication development from indicators of true disability (ASHA, n.d.; ASHA, 1993). Because communication and culture are closely intertwined (Duranti et al., 2011; Schieffelin & Ochs, 1986), this requires skillful administration of culturally- and linguistically-relevant approaches to make accurate diagnoses and appropriate eligibility and placement decisions. Failure to do so may lead to overdiagnosis, underdiagnosis, or misdiagnosis of disability, each of which can burden children and families (e.g., stigma, social isolation, reduced educational opportunities; Bianco, 2005; Green, 2003; Huang & Diamond, 2009) as well as special education systems (e.g., misallocation of resources).
Current research suggests that the disproportionality experienced by young children who are Latino/a varies by region of the country, child background, and EI versus ECSE systems. Regarding referrals, some studies show lower odds of referral for Latino/a children compared to White non-Latino/a peers (Clements et al., 2008; Delgado & Scott, 2006) whereas others show higher odds (Shapiro & Derrington, 2004). Clements et al. (2008) also showed slightly lower likelihood of EI referrals for mothers who spoke languages other than English. Similarly, regarding evaluation and placement, some studies find higher enrollment of Latino/a children (Clements et al., 2008) and children exposed to languages other than English (Shapiro & Derrington, 2004) in EI whereas others find no disproportionality in EI enrollment compared to White non-Latino/a children (McManus et al., 2020; Morgan et al., 2012). Results from studies of ECSE are more consistent: Latino/a children are often underrepresented in general special education eligibility (Delgado & Scott, 2006; Morrier & Gallagher, 2011; US DOE, 2022). It is less clear whether disparities exist in specific EI/ECSE placement categories: one study reported no differences between Latino/a children and White children in receiving a diagnosis in EI/ECSE for communication disorders (Morgan et al., 2012) whereas Morrier and Gallagher (2011) found that Latino/a children were less often categorized with speech or language impairment and ASD (but not HI) in ECSE. Morgan et al. (2012) found children whose primary language was not English were less likely to be diagnosed in EI/ECSE with a communication disorder.
Study Purpose
Overall, current literature on disparities in EI/ECSE provides an incomplete picture of services from referral to placement for children with multiple marginalized identities (i.e., non-White, multilingual, with disabilities) due to the (a) focus on a single step in the EI/ECSE pipeline instead of taking into account overall trajectories from referral to placement, (b) failure to consider the intersectionality of children’s ethnic and linguistic backgrounds simultaneously as related to such disparities, and (c) lack of examination of placement for communication disorders (CDs) specifically despite their prevalence. Addressing these gaps will guide EI/ECSE providers and policy makers to direct scant fiscal and personnel resources to addressing equity in steps of EI/ECSE pipeline for specific populations with CDs. Therefore, the purpose of this study is to fill a gap in the literature by investigating disparities faced by young children with CDs from underrepresented ethnic and linguistic backgrounds, highlighting children who are Latino/a given their growing representation in EI/ECSE. Our research questions were: do differences as a function of children’s ethnicity and home language(s) affect: (1) referral; (2) evaluation; (3) general placement; and, (4) type of communication placement? Based on prior research and theory, we hypothesized that disparities would be found by children’s ethnicity and language backgrounds in some, but not all, components of the EI and ECSE pipelines.
Methods
This study was a secondary data analysis of administrative data on child EI/ECSE service used in Oregon from 2016–2018. The goal of the study was to understand associations between child ethnicity and home language with referral, evaluation, general placement, and specific communication placements in EI/ECSE. Group-specific percentages were calculated and compared using ratios and differences as described in detail below. Estimates were adjusted for potentially confounding variables such as child sex, public health insurance eligibility, urbanicity, and EI/ECSE referral source, and compared the delivery of services to children from traditionally underrepresented ethnic and linguistic groups in Oregon to that of non-Latino/a children who spoke English only.
Setting
In 2018, 63% of Oregon’s children under age 18 were non-Hispanic White followed by 22% Hispanic/Latino (National Kids Count, n.d.). Approximately 15% of Oregon’s residents speak a language other than or in addition to English (US Census, n.d.). Oregon’s lead agency for EI and ECSE is the Department of Education (ODE); the same personnel administer Part C and Part B. To be EI eligible, children must have a documented medical condition with high likelihood of resulting in a developmental delay, meet criteria for a specific delay or disability category (e.g., ASD, HI), or present with a general delay in cognitive, physical, social or emotional, communication, or adaptive development (ORS 343.513; Oregon Administrative Rules [OAR]). To be ECSE eligible, children must meet criteria for one of twelve disability categories (ORS 343.475; OAR). All EI/ECSE eligible children in Oregon receive an Individualized Family Service Plan (IFSP).
Data Source
Data from all children with a primary EI/ECSE referral between 2016–2018 were analyzed. Data were extracted by ODE from ODE’s central electronic database, called ecWeb, used to log child and family demographics, referrals, evaluation outcomes, eligibility, IFSP components, and services for individual children. Fidelity is high as providers around the state use ecWeb to meet federal reporting requirements. The investigators’ respective Institutional Review Boards approved this study.
Variables
Child Demographic Variables.
The central independent variables concerned children’s ethnicity and home language(s). We created 5 mutually-exclusive groups using child ethnicity and home language(s) recorded in ecWeb per parent report.
Latino/a with primarily Spanish home language (i.e., Latino/a Spanish). Approximately 1% also heard and/or spoke another language at home, typically indigenous languages of Central or South America (e.g., Mixteco, Mam, Maya).
Latino/a with English and Spanish home language (i.e., Latino/a Bilingual)
Latino/a with English as the home language (i.e., Latino/a English)
Non-Latino/a with a language other than English and Spanish as the home language (i.e., non-Latino/a Other Language)
Non-Latino/a with English as the home language (i.e., non-Latino/a English). Approximately 90% were identified as White. This group served as the reference category in all analyses unless otherwise stated.
Children (n = 506; 1.2%) who did not match the above categories (e.g., Latino/a with Vietnamese home language) were excluded.
Data were also collected on child sex, Medicaid eligibility (yes or no), age in months at first referral, and urbanicity. Urbanicity was derived from home zip code, using the Oregon Office of Rural Health’s (2020) urban, rural, or frontier designations.
Referral and Evaluation.
We collected information on referral source, child age at referral, and outcome (evaluated or not). Referral sources were grouped as “Physician/clinic,” “Parents/family,” “Childcare/Head Start/preschool,” and “other.” Age at referral was classified as EI (up to 33 months) or ECSE (36 to 50 months). Children 33 to 35 months old or within one year of kindergarten were excluded, as it was unclear which evaluation protocol (EI vs. ECSE) was used.
Eligibility and Placement.
All communication-related eligibility codes in ecWeb were included in this study: Communication Delay (CD), Autism Spectrum Disorder (ASD), and Hearing Impairment (HI). CD represented children found eligible for developmental delay with communication as the primary delay in EI and children found eligible for speech or language impairment in ECSE. Within the CD eligibility, we also analyzed the subcategories of “Language delay” and “Articulation”. Twenty-two children found eligible for “Voice” and/or “Fluency” subcategories, and 152 children missing all eligibility variables (0.9%) were excluded.
Data Analysis
Due to the large sample size and multiple outcomes, we calculated 99% confidence intervals and used a significance threshold of p < 0.01. Analyses were stratified and performed separately for EI and ECSE using Stata/IC for Windows version 15.
Child characteristics.
We examined child demographics, program referred to (EI, ECSE, or both), mean number of referrals per child, and source of first referral for children overall and for the ethnicity/language groups. Differences for categorical variables were tested using chi square tests; for the number of referrals, we used the non-parametric Kruskal-Wallis test.
Evaluation and placement.
We calculated the probability that referral resulted in evaluation overall, by ethnicity/language, and by referral source. Risk ratios were calculated using log-binomial regression, which yields risk ratios—the proportion in the interest group divided by the proportion for the reference group (non-Latino English-speaking children). A risk ratio of 1 indicates that the groups being compared have an equal likelihood of the targeted outcome (i.e., being evaluated, placed, or labeled with a specific disability). A risk ratio higher than 1 for a particular ethnic/linguistic group suggests increased probability of experiencing the service than non-Latino English children, while a risk ratio less than 1 suggests decreased likelihood than non-Latino English children. The magnitude of difference in risk is noted by how far the risk ratio is from 1 (e.g., risk ratios of 1.25 or 0.5 mean 25% greater likelihood or 50% as likely, respectively, for a particular group on the targeted outcome). An adjusted risk ratio adjusts these proportions for other factors that likely contribute to differences in outcomes.
When modeling ECSE placement, we encountered convergence issues and substituted a Poisson model with robust variance estimators (Chen et al., 2018). Because children could contribute multiple referrals, we used variance estimators with clustering by child identification number. For adjusted risk ratios, the model included ethnicity/language groups, referral source, child sex, and Medicaid eligibility - selected based on associations with ethnicity/language and special education outcomes, both in the literature and in this dataset.
To assess associations with general EI/ECSE placement, we limited the analysis to referrals resulting in evaluation. We calculated the likelihood that the referral resulted in placement using the same methods described above for probability of evaluation.
Among children with any communication disorder placement, we tested the association between placement type and ethnicity/language group. Separate models were created for communication disorder placement (CD), ASD placement (regardless of other placement), HI placement (regardless of other placement), and any placement for a disability type related to communication challenges (CD, ASD, and HI combined). For children with CD placement, we assessed for placement based on language and/or articulation disorder subcodes using separate bivariate and multivariable models for EI and ECSE adjusted for referral source, child sex, and Medicaid eligibility.
Results
The initial query identified 38,407 children with primary referrals to EI or ECSE in calendar years 2016 to 2018. Approximately 22.3% of children were Latino/a (n = 7,141): 46.5% reported Spanish as the home language, 38.5% reported English as the home language, and 14.9% reported Spanish and English as the home languages. Children from non-Latino/a Other Language backgrounds represented 4.7% of the sample. Common languages spoken by these children included Vietnamese, Arabic, Russian, Mandarin, Hindi, Cantonese, Telegu, and Somali. About 10% (n = 2,377) of non-Latino/a English-speaking children were identified as Black, Asian, Pacific Islander, and/or Indigenous. Sixty-four percent of all children were male, and 40% were Medicaid-eligible. Most children (65%) lived in urban areas. See Table 1 for an overview of child demographic characteristics.
Table 1.
Child demographic characteristics and referral data
| Overall | Latino/a |
Non-Latino/a |
p-valuec | ||||
|---|---|---|---|---|---|---|---|
| Spanish | Bilingual | English | Other Languagea | Englishb | |||
| N | 31,985 | 3,324 | 1,065 | 2,752 | 1,519 | 23,325 | |
| Male (%) | 64 | 64 | 66 | 63 | 66 | 63 | 0.08 |
| Medicaid (%) | 40 | 43 | 51 | 43 | 37 | 39 | <0.0001 |
| Age (months) at first referral (%) | |||||||
| 0 to 8 months | 13 | 10 | 8 | 12 | 10 | 13 | <0.0001 |
| 9 to 17 | 17 | 18 | 17 | 18 | 17 | 17 | |
| 18 to 23 | 15 | 15 | 19 | 14 | 19 | 14 | |
| 24 to 35 | 23 | 27 | 27 | 24 | 26 | 22 | |
| 36 to 47 | 24 | 22 | 24 | 24 | 22 | 25 | |
| 48 to 69 | 9 | 8 | 6 | 8 | 8 | 9 | |
| Median Age (months) at first referral (25th, 75th percentile) | 24 (15, 38) | 24 (15, 37) | 24 (18, 37) | 24 (15, 38) | 24 (16, 37) | 24 (15, 39) | 0.40 |
| Program referred (ever) (%) | |||||||
| EI | 63 | 66 | 65 | 63 | 67 | 62 | <0.0001 |
| ECSE | 34 | 30 | 30 | 32 | 30 | 34 | |
| Both | 4 | 4 | 5 | 4 | 4 | 3 | |
| Number of referrals per child (M, SD) | |||||||
| EI | 1.17 (0.43) | 1.17 (0.42) | 1.22 (0.49) | 1.17 (0.43) | 1.13 (0.37) | 1.16 (0.44) | <0.001 |
| ECSE | 1.07 (0.29) | 1.07 (0.28) | 1.08 (0.31) | 1.08 (0.29) | 1.04 (0.19) | 1.08 (0.29) | 0.06 |
| Source of first referral (%) | |||||||
| Physician/clinic | 49 | 61 | 51 | 54 | 53 | 46 | <0.0001 |
| Parents/family | 28 | 16 | 23 | 23 | 31 | 30 | |
| Childcare/Head Start/preschool | 10 | 13 | 15 | 11 | 9 | 9 | |
| Other source | 14 | 10 | 11 | 13 | 7 | 15 | |
| Urbanicityd | |||||||
| Urban | 65 | 73 | 72 | 64 | 95 | 62 | <0.0001 |
| Rural | 32 | 24 | 23 | 30 | 4 | 35 | |
| Frontier | 3 | 3 | 5 | 6 | 1 | 2 | |
Note. Excludes children with ‘transition’ referrals only (n = 5422), unknown sex (n = 118), or unknown urbanicity (n = 295).
Common non-English languages include Vietnamese, Arabic, Russian, Mandarin, Hindi, Cantonese, Telegu, and Somali
The vast majority of children in this group were identified as White
p-value for group comparison, using chi-square test (for categorical variables) and Kruksal-Wallis (for number of referrals)
Missing urbanicity ~0.5% to 1%; highest in English-speaking groups (p-value 0.004 for group differences)
Child-level Referral Patterns
Approximately 63% of children were referred to EI, 34% to ECSE, and 4% to both programs. Most children (47%) were referred between 24 and 48 months of age. Most children were initially referred by medical personnel (49%) followed by parents (28%), early education professionals (10%), or another source (14%).
While the median age of first referral was the same for all groups (24 months), English speakers were referred more often at the youngest and oldest ages. Monolingual English speakers (non-Latino/a and Latino/a) were more likely than Latino/a Spanish and non-Latino/a Other Language children to be referred before 9 months and after 36 months (see online Supplementary Material). There were also significant differences in referral source for EI and ECSE combined: only 18% of Latino/a Spanish children's referrals came from parents rather than other sources. The percentage was higher for Latino/a bilingual and English speakers (27% and 26%, respectively), while 33% of non-Latino/a children's referrals were from parents (p value for differences between Latino/a groups and non-Latino/a English speakers <.001). See Figure 1a for percent of referrals that originated from parents by child ethnicity and language. Children could be referred again if not evaluated or placed. Non-Latino/a Other Language children had the lowest average number of referrals to EI and ECSE (1.13 and 1.04 vs. overall means 1.17 [p < .0001] and 1.07 [p = .06], respectively). Group differences were statistically significant in EI but not ECSE. Refer to Table 1 for referral age, source, and number of referrals.
Figure 1a. Percent of Referrals that Originate with Parents/Family by Child Ethnicity and Language(s).
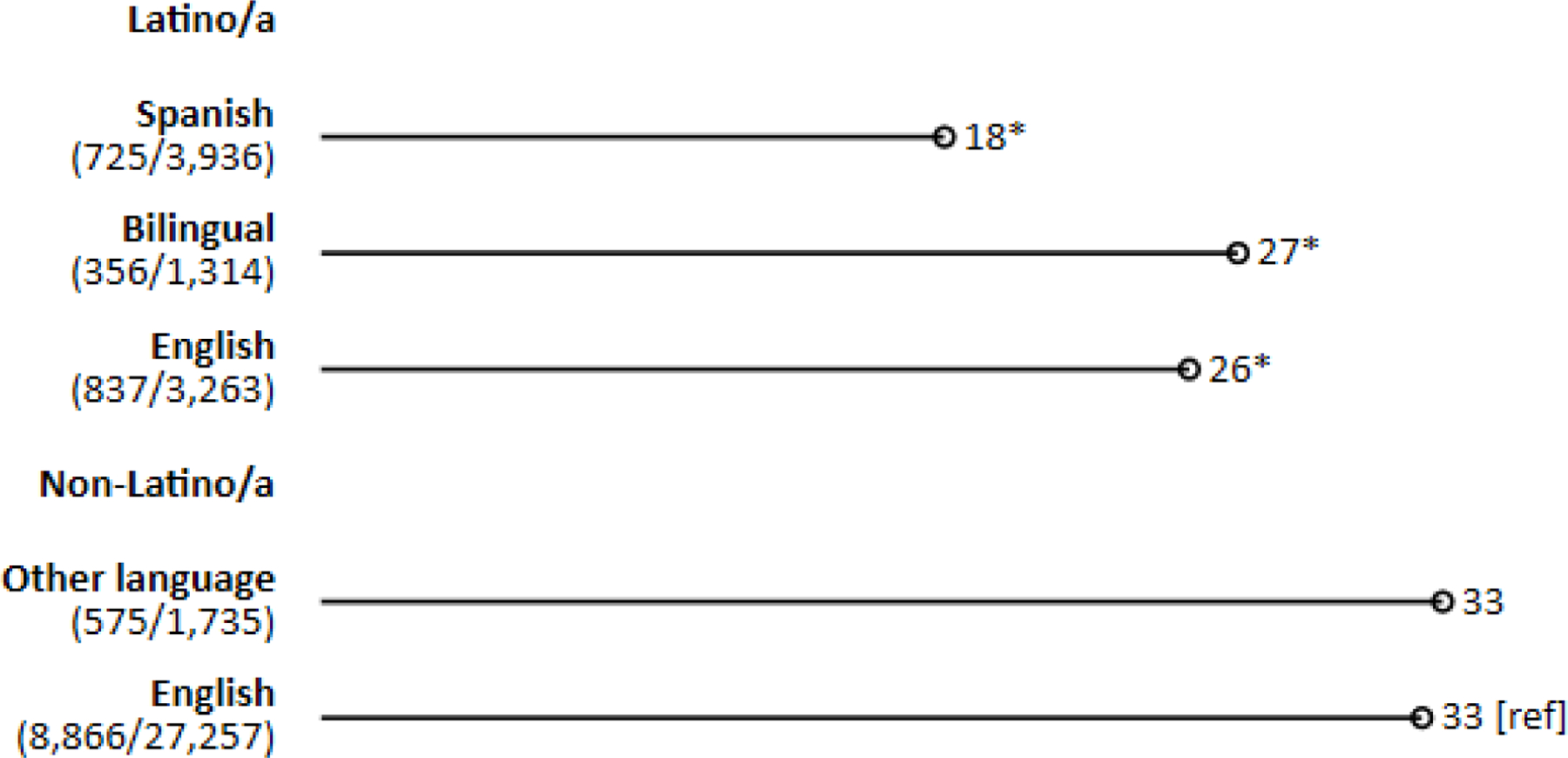
Note. [ref] = reference group (non-Latino/a English-speaking children). Values in parentheses represent (number of referrals by parents)/(total number of referrals) for a given group. Approximately 15% of referrals are repeats for a given child and p values account for clustering.
*Differs from non-Latino/a English-speaking children at p < .001.
Referrals Resulting in Evaluation
Table 2 provides detail on total referrals, those that resulted in evaluations, and the associations with referral source as well as child ethnicity and language. Overall, 63% of EI referrals and 64% of ECSE referrals were evaluated. Results showed few significant differences in EI or ECSE evaluation rates by ethnicity and language(s) after adjustment. As an exception, there was a slight but statistically significant elevation in evaluation rates for Latino/a Spanish children (66%) in EI compared to non-Latino/a English children (62%; risk ratio [RR] 1.07; adjusted risk ratio [aRR] 1.09 [99% CI 1.05–1.13]). Referrals from parents were most likely to be evaluated, and physician referrals were least likely to be evaluated, regardless of ethnicity/language (see Figure 1b for percent of referrals evaluated by source and child characteristics). The difference was most pronounced in EI: only 54% of physician referrals were evaluated versus 78% of parent referrals (aRR 0.69 [0.67–0.71]; Table 2).
Table 2.
Sociodemographic Associations with EI/ECSE Referrals Resulting in Evaluation and Placement
| Evaluated | Placed | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All referrals | Evaluation completed |
Unadjusted RR |
Adjusted RR* |
Placement |
Unadjusted RR |
Adjusted RRa |
||||||||
| N |
% of total |
N |
RR |
99% CI |
RR |
99% CI |
% of evaluated |
N |
RR |
99% CI |
RR |
99% CI |
||
| EI | Overall | 24,788 | 63 | 15,508 | 69 | 10,676 | ||||||||
| Latino/a | Spanish | 2,707 | 66 | 1,794 | 1.07 | (1.02, 1.11) | 1.09 | (1.05, 1.13) | 65 | 1,161 | 0.93 | (0.89, 0.98) | 0.97 | (0.94, 1.01) |
| Bilingual | 906 | 66 | 594 | 1.05 | (0.99, 1.12) | 1.00 | (0.94, 1.07) | 71 | 422 | 1.02 | (0.96, 1.10) | 0.96 | (0.90, 1.02) | |
| English | 2,178 | 58 | 1,255 | 0.93 | (0.88, 0.97) | 0.96 | (0.92, 1.00) | 67 | 843 | 0.97 | (0.92, 1.02) | 0.98 | (0.95, 1.02) | |
| Non-Latino/a | Other Language | 1,210 | 66 | 797 | 1.06 | (1.00, 1.12) | 1.05 | (0.99, 1.11) | 72 | 571 | 1.03 | (0.97, 1.10) | 1.03 | (0.98, 1.09) |
| English | 17,787 | 62 | 11,068 | [ref] | [ref] | 69 | 7,679 | [ref] | [ref] | |||||
| Referral Source | Parents/family | 6,299 | 78 | 4,935 | [ref] | [ref] | 70 | 3,468 | [ref] | [ref] | ||||
| Physician/clinic | 13,861 | 54 | 7,472 | 0.69 | (0.67, 0.71) | 0.72 | (0.70, 0.74) | 67 | 5,015 | 0.96 | (0.93, 0.99) | 0.97 | (0.95, 1.00) | |
| Childcare/Head Start/Preschool | 828 | 67 | 553 | 0.85 | (0.80, 0.91) | 0.85 | (0.80, 0.91) | 66 | 365 | 0.94 | (0.86, 1.02) | 0.91 | (0.85, 0.98) | |
| Other sources | 3,800 | 67 | 2,548 | 0.86 | (0.83, 0.89) | 0.88 | (0.85, 0.91) | 72 | 1,828 | 1.02 | (0.98, 1.06) | 0.98 | (0.95, 1.01) | |
| ECSE | Overall | 12,717 | 64 | 8,153 | 83 | 6,765 | ||||||||
| Latino/a | Spanish | 1,229 | 65 | 803 | 1.02 | (0.97, 1.08) | 1.04 | (0.99, 1.10) | 79 | 632 | 0.95 | (0.90, 1.00) | 0.94 | (0.90, 0.99) |
| Bilingual | 408 | 68 | 276 | 1.06 | (0.97, 1.16) | 1.00 | (0.91, 1.09) | 81 | 224 | 0.98 | (0.90, 1.06) | 0.96 | (0.89, 1.04) | |
| English | 1,085 | 62 | 670 | 0.97 | (0.91, 1.03) | 0.98 | (0.93, 1.04) | 86 | 577 | 1.04 | (0.99, 1.08) | 1.01 | (0.97, 1.05) | |
| Non-Latino/a | Other Language | 525 | 67 | 353 | 1.05 | (0.97, 1.14) | 1.04 | (0.97, 1.12) | 87 | 308 | 1.05 | (1.00, 1.11) | 1.07 | (1.01, 1.13) |
| English | 9,470 | 64 | 6,051 | [ref] | [ref] | 83 | 5,024 | [ref] | [ref] | |||||
| Referral Source | Parents/family | 5,060 | 71 | 3,604 | [ref] | [ref] | 84 | 3,037 | [ref] | [ref] | ||||
| Physician/clinic | 3,474 | 54 | 1,866 | 0.75 | (0.72, 0.79) | 0.78 | (0.74, 0.81) | 81 | 1,520 | 0.97 | (0.93, 1.00) | 0.94 | (0.91, 0.97) | |
| Childcare/Head Start/Preschool | 2,738 | 65 | 1,792 | 0.92 | (0.88, 0.96) | 0.89 | (0.86, 0.93) | 79 | 1,414 | 0.94 | (0.90, 0.97) | 0.90 | (0.87, 0.93) | |
| Other sources | 1,445 | 62 | 891 | 0.87 | (0.82, 0.92) | 0.86 | (0.82, 0.91) | 89 | 794 | 1.06 | (1.02, 1.10) | 1.00 | (0.97, 1.04) | |
Note. [ref], reference group (non-Latino/a, English-speaking children); CI, confidence interval; EI, Early Intervention; ECSE, Early Childhood Special Education; RR, relative risk
Adjusted estimates from model with language/ethnicity, referral source, child sex, and Medicaid eligible.
Figure 1b. Percent of Referrals Evaluated by Source and by Child Ethnicity and Language(s).
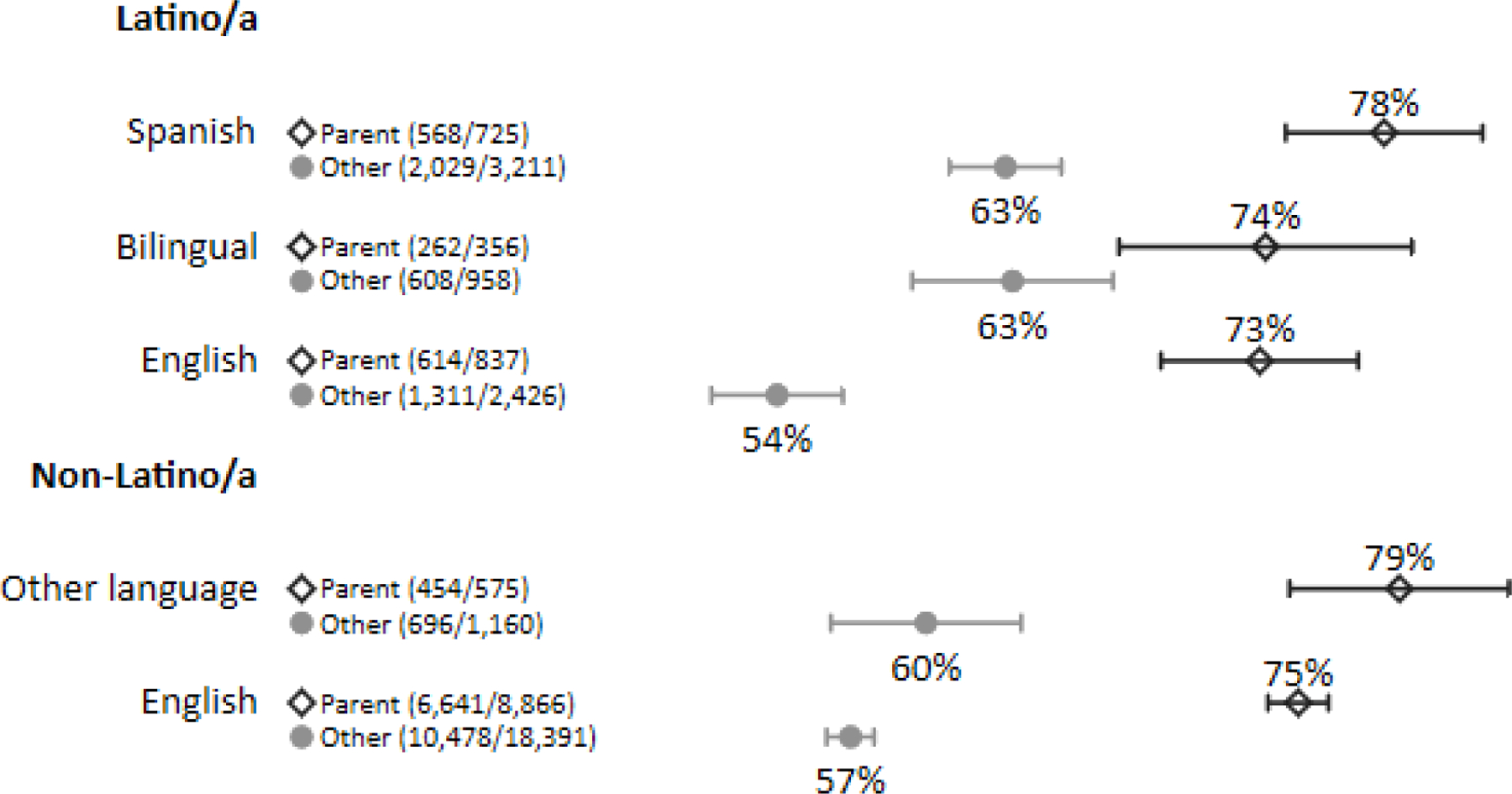
Note. Values in parentheses represent (number of referrals evaluated)/(number of referrals) to both early intervention (EI) and early childhood special education (ECSE), combined, for a given group. Bars represent 99% confidence intervals using variance estimates that take repeated referrals for some children into account. Other sources include medical clinics, childcare providers, and others.
General Placement
See Table 2 for details on evaluations that resulted in placement and the associations with referral source and child ethnicity and language. Overall, 69% of EI evaluations and 83% of ECSE evaluations resulted in placement. Parent referrals, which were the most common type in ECSE, had the highest chance of placement (70% and 84% in EI and ECSE) after adjustment. Physician/clinic referrals, the most common type in EI, were nearly as likely to be placed in EI (67%; aRR 0.97 [0.95–1.00] vs. parent referrals) but less likely to result in placement in ECSE (81%; aRR 0.94 [0.91–0.97]). Percentage placed was lowest for childcare referrals at 66% for EI (aRR 0.91 [0.85–0.98] vs. parents) and 79% for ECSE (aRR 0.90 [0.87–0.93] vs. parents). Differences in EI placement according to ethnicity and language(s) were not significant after adjustment. However, when compared to non-Latino English speakers (83% of children evaluated were placed), statistically significant differences after adjustment were found in ECSE placement for non-Latino/a Other Language speakers (87% were placed; aRR 1.07 [1.01–1.13]) and Latino/a Spanish speakers (79% were placed; aRR 0.94 [0.90–0.99]).
Communication Placement Types
Overall, 2,858 children in EI (27% of placements) and 4,970 children in ECSE (75% of placements) were placed for a communication-related disability. Of all children placed, 19% in EI and 66% in ECSE had CD as a primary placement, 4% and 8% had ASD eligibility, and 4% and 3% had HI eligibility. Refer to Table 3 and Figure 2 for details on communication placements and their associations with child ethnicity and language.
Table 3.
Sociodemographic Associations with Communication Placement Types
| Communication Disorder Primary Eligibility |
Any Autism Eligibility |
Any Hearing Impairment Eligibility |
Any Communication-Related Disability |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N Total Place-ments |
N |
% |
RR |
ARRa |
99% CI |
N |
% |
RR |
ARRa |
99% CI |
N |
% |
RR |
ARRa |
99% CI |
N |
% |
RR |
ARRa |
99% CI |
||
| EI | All | 10,571 | 2,020 | 19 | 468 | 4 | 398 | 4 | 2,858 | 27 | ||||||||||||
| Latino/a | S | 1,150 | 276 | 24 | 1.28 | 1.27 | (1.09, 1.47) | 41 | 4 | 0.83 | 0.83 | (0.54, 1.27) | 44 | 4 | 1.01 | 1.24 | (0.83, 1.83) | 359 | 31 | 1.17 | 1.20 | (1.06, 1.36) |
| B | 418 | 101 | 24 | 1.29 | 1.24 | (0.98, 1.57) | 13 | 3 | 0.72 | 0.70 | (0.34, 1.43) | 15 | 4 | 0.95 | 1.15 | (0.60, 2.19) | 129 | 31 | 1.16 | 1.16 | (0.95, 1.41) | |
| E | 825 | 149 | 18 | 0.96 | 0.98 | (0.80, 1.19) | 32 | 4 | 0.90 | 0.89 | (0.56, 1.42) | 33 | 4 | 1.05 | 1.09 | (0.70, 1.72) | 211 | 26 | 0.96 | 0.98 | (0.83, 1.14) | |
| Non-Latino/a | OL | 563 | 63 | 11 | 0.60 | 0.56 | (0.41, 0.77) | 55 | 10 | 2.27 | 2.23 | (1.55, 3.19) | 17 | 3 | 0.80 | 1.13 | (0.62, 2.04) | 135 | 24 | 0.90 | 0.90 | (0.73, 1.09) |
| E | 7,615 | 1,431 | 19 | [ref] | [ref] | 327 | 4 | [ref] | [ref] | 289 | 4 | [ref] | [ref] | 2,024 | 27 | [ref] | [ref] | |||||
| ECSE | All | 6,596 | 4,342 | 66 | 535 | 8 | 212 | 3 | 4,970 | 75 | ||||||||||||
| Latino/a | S | 628 | 437 | 70 | 1.04 | 1.04 | (0.97, 1.12) | 16 | 3 | 0.30 | 0.31 | (0.16, 0.60) | 7 | 1 | 0.32 | 0.36 | (0.13, 0.96) | 454 | 72 | 0.94 | 0.95 | (0.89, 1.02) |
| B | 220 | 159 | 72 | 1.09 | 1.09 | (0.94, 1.19) | 8 | 4 | 0.43 | 0.46 | (0.19, 1.13) | 13 | 6 | 1.71 | 1.85 | (0.90, 3.78) | 175 | 80 | 1.04 | 1.03 | (0.94, 1.13) | |
| E | 560 | 373 | 67 | 1.00 | 1.02 | (0.94, 1.10) | 40 | 7 | 0.85 | 0.86 | (0.57, 1.29) | 14 | 3 | 0.72 | 0.72 | (0.36, 1.49) | 421 | 75 | 0.98 | 0.99 | (0.93, 1.06) | |
| Non-Latino/a | OL | 294 | 114 | 39 | 0.58 | 0.58 | (0.48, 0.70) | 58 | 20 | 2.34 | 2.34 | (1.69, 3.26) | 9 | 3 | 0.89 | 0.89 | (0.40, 2.29) | 176 | 60 | 0.78 | 0.78 | (0.68, 0.88) |
| E | 4,894 | 3,259 | 67 | [ref] | [ref] | 413 | 8 | [ref] | [ref] | 169 | 3 | [ref] | [ref] | 3,744 | 77 | [ref] | [ref] | |||||
Note. [ref], reference group (non-Latino/a, English-speaking children); EI, Early Intervention; ECSE; Early Childhood Special Education; S, Spanish; B, Bilingual; E, English, OL, Other Language; RR, risk ratio; ARR, adjusted risk ratio; CI, confidence interval.
Adjusted for source of first referral, child sex, and Medicaid eligible
Figure 2. Percent of Evaluated Referrals Resulting in Placement by Source and Child Ethnicity and Language(s).
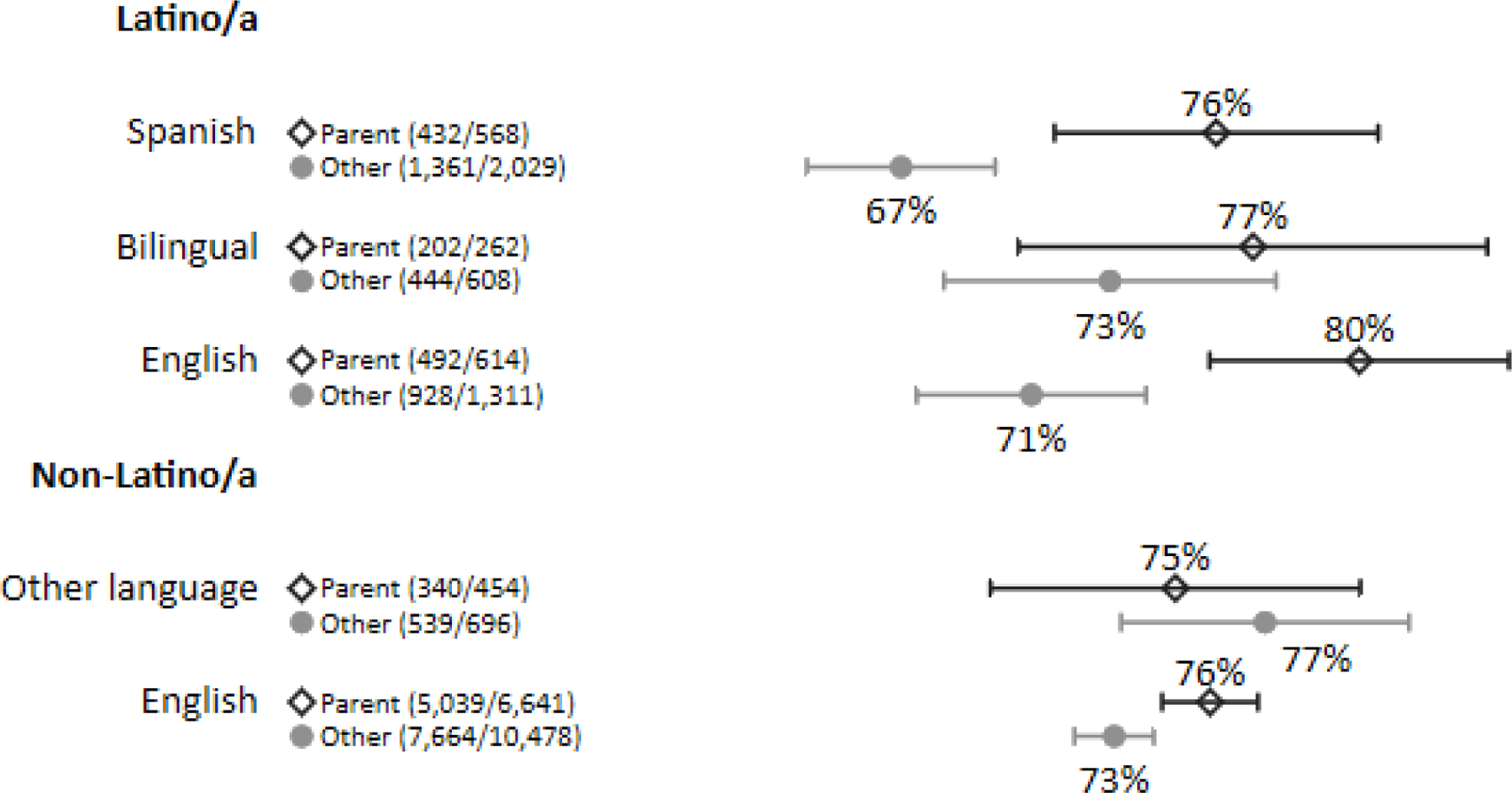
Note. Values in parentheses represent (number resulting in placement)/(total number of referrals evaluated) for a given group. Total counts of referrals are given in Figure 1b. Bars represent 99% confidence intervals.
In EI, Latino/a Spanish children were significantly more likely than non-Latino/a English children to have a CD placement (24% of placements; aRR 1.27 [1.09, 1.47] or any communication-related placement (31%; aRR 1.20 [1.06, 1.36] as compared to 19% and 27% of non-Latino English placements, respectively. In contrast, non-Latino/a Other Language children were least likely (11%) to have a CD placement (aRR 0.56 [0.41, 0.77]); less than half the rate of Latino/a Spanish children above. The same non-Latino/a Other Language children were more than twice as likely as any group to have an ASD placement: 10% of non-Latino/a Other Language children (aRR 2.23 [1.55, 3.19]) vs. 3–4% among all other groups.
In ECSE, a similar pattern was observed: non-Latino/a Other Language children were significantly less likely to have a CD placement than other groups (39% vs. 67–72%; aRR 0.58 [0.48, 0.70] vs. reference group) or a placement for any communication-related disability (60% vs. 72–80%; aRR 0.78 [0.68, 0.88]). Children who were non-Latino/a Other Language were also significantly more likely (20%; aRR 2.34 [1.69, 3.26]) and Latino/a Spanish children were significantly less likely to have an ASD placement (aRR 0.31 [0.16, 0.60]) than non-Latino/a English speakers. Only 16 out of 628 (3%) Latino/a Spanish children placed in Oregon received an ASD placement compared to 8% (413/4894 placed) of non-Latino/a English children. Latino/a Spanish children were also less likely to have an HI placement—only 7 of 628 placements (1%) compared to 169 of 4,894 non-Latino/a English (3%) (aRR 0.36 [0.13, 0.96]).
Table 4 provides information on children’s communication disorder eligibility and its association with child ethnicity and language. In EI, Language Delay was the most common CD placement subcode (75% of children). In ECSE, Articulation was the most common subcode (70% of children). All groups other than non-Latino/a English were more likely to receive the Language Delay subcode, with the highest likelihood among Latino/a Spanish children (aRR 1.27 [1.19, 1.34] vs reference group). For instance, in EI, language delay was assigned to 93% of Latino/a Spanish children but 69% of non-Latino/a English children. A similar pattern was found in ECSE. Differences for non-Latino/a Other Language children were similar to Latino/a Spanish, especially in ECSE. A reverse pattern was seen for the Articulation subcode: non-Latino/a English were most likely to receive this subcode, compared to every other group. The difference was pronounced in EI: only 13% of Latino/a Spanish children were labeled with an articulation disorder compared to 44% of non-Latino/a English children (aRR 0.32 [0.21, 0.48]). In ECSE, 51% of Latino/a Spanish and 75% of non-Latino/a English CD codes were labeled with an articulation disorder (aRR 0.70 [0.62, 0.79]).
Table 4.
Sociodemographic Associations with EI/ECSE Communication Disorder Eligibility Categories
| Total |
Language Delay |
Articulation |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N with CD |
N |
% |
RR |
Adjusted RRa |
99% CI |
N |
% |
RR |
Adjusted RRa |
99% CI |
||
| EI | Overall | 2,020 | 1,518 | 75 | 728 | 36 | ||||||
| Latino/a | Spanish | 276 | 257 | 93 | 1.35 | 1.27 | (1.19, 1.34) | 36 | 13 | 0.30 | 0.32 | (0.21, 0.48) |
| Bilingual | 101 | 89 | 88 | 1.27 | 1.19 | (1.07, 1.33) | 24 | 24 | 0.55 | 0.57 | (0.36, 0.93) | |
| English | 149 | 130 | 87 | 1.26 | 1.20 | (1.10, 1.32) | 29 | 19 | 0.45 | 0.47 | (0.31, 0.73) | |
| Non-Latino/a | Other Language | 63 | 52 | 83 | 1.19 | 1.16 | (0.99, 1.36) | 16 | 25 | 0.58 | 0.58 | (0.33, 1.02) |
| English | 1,431 | 990 | 69 | [ref] | [ref] | 623 | 44 | [ref] | [ref] | |||
| ECSE | Overall | 4,342 | 1,705 | 39 | 3,036 | 70 | ||||||
| Latino/a | Spanish | 437 | 280 | 64 | 1.95 | 1.76 | (1.57, 1.98) | 225 | 51 | 0.68 | 0.70 | (0.62, 0.79) |
| Bilingual | 159 | 94 | 59 | 1.80 | 1.66 | (1.39, 1.99) | 82 | 52 | 0.68 | 0.71 | (0.58, 0.86) | |
| English | 373 | 190 | 51 | 1.55 | 1.45 | (1.25, 1.68) | 221 | 59 | 0.79 | 0.80 | (0.72, 0.90) | |
| Non-Latino/a | Other Language | 114 | 72 | 63 | 1.93 | 1.78 | (1.45, 2.19) | 54 | 47 | 0.63 | 0.63 | (0.49, 0.82) |
| English | 3,259 | 1,069 | 33 | [ref] | [ref] | 2,454 | 75 | [ref] | [ref] | |||
Note. [ref], reference group (non-Latino/a, English-speaking children); CD, communication disorder; CI, confidence interval; EI, Early Intervention; ECSE, Early Childhood Special Education; RR, relative risk
Adjusted for source of first referral (parent/other), child sex, and Medicaid eligibility.
Discussion
This study’s goal was to explore differences in the EI and ECSE pipelines from referral, to evaluation, to placement as related to children’s intersecting ethnic and linguistic identities with a focus on children who are Latino/a. Using state-level data on individual children, the study identified several differences in the distribution of outcomes in EI/ECSE by child background. Findings can be used in tandem with stakeholder-engaged research to understand inequities and to develop targeted implications for research, policy, and practices that improve equity across steps in the EI/ECSE pipeline (Nalani et al., 2021).
Importance of Intersectional Analyses
Scholars have called for disproportionality research in EI/ECSE to move away from analyzing effects of isolated identity markers and toward analytical models that account for the interdependency of children’s multiple marginalizing identities (Love & Beneke, 2021). Our intersectional analyses lend credit to the value of this approach and support the notion that language and ethnicity in particular are intertwined (Rosa & Flores, 2017). In our models, Medicaid status, urbanicity, and child sex were held constant whenever possible to focus on the intersections of ethnicity and language. Children’s language background appeared to play a more important role than their ethnicity in achieving distributional equity at some points in Oregon’s EI and ECSE pipelines while children’s ethnicity, regardless of home language(s), appeared to have a greater effect at other points. For example, we found that Latino/a Spanish-speaking children were slightly over-represented in EI referrals and evaluations when compared to non-Latino/a English-speaking peers. This finding contrasted prior research that showed no differences in referral when analyzing data by Latino/a ethnicity alone (Clements et al., 2008; Jimenez et al., 2014; McManus et al., 2020). Ethnic/language differences were also noted for general ECSE placement for children who were Latino/a Spanish speakers and those who were non-Latino/a Other Language speakers. No differences were noted in referrals, evaluation, or general placement for Latino/a children from homes where English was spoken (Latino/a English and Latino/a Bilingual) compared to non-Latino/a English speakers, suggesting a systemic bias favoring English speakers regardless of ethnicity (Rosa & Flores, 2017). Yet, disproportionality in EI and ECSE placement for a language or an articulation delay was noted for all Latino/a groups regardless of home language, pointing toward a more general effect of ethnicity on equity at this point in the system. With the level of detail available through intersectional analyses, state policies and interventions for outreach and evaluation can be finely tuned to build equity in particular communities.
Points of Focus for Equity Efforts in EI/ECSE: Practice and Policy
In addition to intersectional analyses, equity initiatives further benefit from identifying the precise points in any system where resources are unequally distributed (Nalani et al., 2021). Such precision allows researchers and policymakers to direct the generally scant resources to interventions that may lead to the greatest improvement in equity. Our findings specify where in the EI/ECSE process Latino/a children with CDs may face the least and greatest structural challenges to access to care. Based on these data alone, for Latino/a children in Oregon, the most substantial structural challenges appeared to manifest at the points of referral to and placement in these systems whereas access to evaluations may be less affected by structural biases. Specifically, the likelihood of receiving an ECSE evaluation following referral and being placed in EI following evaluation appeared fairly equitable across children in Oregon. No ethnic/language differences were noted in the rates of evaluation in ECSE, and there was only a slightly greater likelihood of evaluation for Spanish-exposed Latino/a children in EI. This contrasts the findings of Clements et al. (2008) who found a lower likelihood of evaluation for referred children whose mothers were Hispanic and whose preferred language was not English in Massachusetts before adjustment; however, the magnitude of difference from the reference group was similarly slight in both studies. Certainly, any degree of over- and under-evaluation risks inappropriate EI/ECSE enrollment decisions for individual children; nonetheless, these findings taken together may point toward the possibility that the procedures around who is evaluated in EI and ECSE systems may be more equitable than other steps in the process, at least in Oregon. In contrast, careful attention to referral and placement practices with Latino/a children with CDs is needed to disrupt structural racism and enhance equity in Oregon’s EI/ECSE programs.
Referral source.
As previously mentioned, children’s ethnicity regardless of home language was a driving factor of differences in how children were referred to EI and ECSE systems. While non-Latino/a Other Language children were referred by their parents as often as non-Latino/a English children, Latino/a children from all language backgrounds were less likely to have a parental referral. This difference is notable because our findings show that referral source is a strong mediator of evaluation completion and ultimate placement – parent referrals are more likely to be evaluated than other referral types in EI and ECSE, and parent referrals are more likely to result in placement in ECSE. Parents who have concerns and make referrals directly may be intrinsically motivated to pursue services. This may not be the case when other sources make the referral. It is not clear why Latino/a families are less likely to self-refer to EI/ECSE. Some possibilities include limited familiarity with EI/ECSE, differing trust and empowerment in educational or medical systems, lack of information sharing by providers about the reason for referral or how to follow up on the referral with EI/ECSE (including in families’ home languages), and/or varied information about and/or cultural perspectives on development and disability in early childhood (Jimenez et al., 2012; 2013; Magnusson et al., 2017).
Irrespective of the reason, ethnic differences in referral source should be considered in efforts to enhance access to EI and ECSE. Certainly, referring agencies and medical providers could enhance their communication with parents about child development and how to access EI/ECSE services. However, we caution that these results do not translate into a call for health care and educational providers to rely on parents alone to make referrals - active primary care management of referrals in early childhood is associated with higher rates of evaluation (Conroy et al., 2018). Nonetheless, states must have a program that aims to raise parent awareness of EI services per federal law (IDEA, 2004), and these findings suggest that such efforts (at least in Oregon) may be more effective at reaching some parents than others. Thus, updating policies to specify an intentional focus on developing outreach approaches that are culturally- and linguistically-responsive to the diverse communities served in each state may be beneficial. For example, emerging research shows that Promotoras de Salud (similar to Community Health Workers) are effective for mitigating health disparities (Koskan et al., 2013; WestRasmus et al., 2012), including in delivering health education in Latino/a families of children with disabilities who may not speak English (Magaña et al., 2014). This model could be replicated in EI/ECSE to increase parental referrals among Latino/a populations to EI and ECSE, perhaps through supporting families to monitor their child’s progress toward developmental milestones and to learn how to connect with EI/ECSE services. While Part B of IDEA legislation requires that states “ensure that all children with disabilities…are identified, located, and evaluated” (§300.111; 2004), this guidance is quite general. Increasing the specificity of the policy to include community-specific parental outreach about referrals may be useful, especially for children who do not attend preschool where Part B child find efforts often take place.
In addition, increasing parental referrals may be supported by policy that requires that each state’s “central directory that includes information on early intervention services, resources, and experts available in the State” (§1435; IDEA, 2004) be available in the languages commonly spoken by state residents. Oregon has parent referral instructions available to download in Spanish; however, the website where these documents are found is only available in English, which may limit access for some parents. Adding a similar statute that requires states to house information about Part B and the referral process in multiple languages may also be needed.
Placement practices.
The steps in the EI/ECSE pipelines at which children with CDs are diagnosed and found eligible for services may be the primary source of inequities. We start by discussing unequal distribution in general placement, which was noted in ECSE only. Irrespective of socioeconomic or geographic backgrounds, children whose families reportedly did not speak English were less likely to be placed (in the case of Latino/a Spanish children) or more likely to be placed (in the case of non-Latino/a Other Language children) in ECSE as compared to non-Latino English-speaking peers. Parents of varied ethnicities who are not proficient English speakers have consistently described language-related barriers to navigating eligibility in ECSE (Cho & Gannotti, 2005; Lo, 2008; Wolfe & Durán, 2013), and practitioners regularly report lacking knowledge and skills in determining eligibility for linguistically-diverse children in particular (e.g., Banerjee & Luckner, 2014; Guiberson & Atkins, 2012). These challenges to accurate placement decisions must be addressed as both enrollment patterns enact costs – children who do not receive the supports they need early in life are at risk for persistent communication concerns and, relatedly, challenges to future academic success (e.g., Young et al., 2002), which may warrant more intensive and expensive special education services at school age. Children who receive supports they do not need may face undue burden (e.g., Bianco, 2005; Green, 2003; Huang & Diamond, 2009) while adding unnecessary costs to ECSE budgets. Ensuring that families have access to interpreters and understand their rights and role in eligibility decisions coupled with provider training in collaborating with diverse families is necessary to address such inequities (Rossetti et al., 2017).
Ultimately, the starkest group differences were found in type of communication disorder placement for both general CDs and specific CD types. Patterns of over- and under-representation were noted in EI and ECSE as related to ethnicity and home language(s). Children from Latino/a Spanish backgrounds were more likely to receive an EI eligibility associated with communication concerns (of any type) than children from any other background, apparently driven by high use of communication delay as a primary disability category. In ECSE, Latino/a Spanish children were very unlikely to be found eligible under the categories of ASD or HI. In comparison to non-Latino/a English peers, Latino/a children (regardless of home language) and children from other language backgrounds were more likely to qualify for EI and ECSE for a language delay than for concerns about speech production (i.e., articulation).
Reasons for this lack of diagnostic specificity (i.e., getting a “general” communication disorder diagnosis versus an ASD or HI diagnosis) could not be examined in this dataset. However, these results reflect similar national patterns regarding Latino/a disparities in ASD diagnosis in particular (Maenner et al., 2020), likely related to biased evaluation practices, bias in diagnostic tools, and/or differences in parental knowledge, social capital, empowerment, and/or involvement in the EI/ECSE eligibility process (Azim et al., 2020; Huerta et al., 2021; Parish et al., 2012; Stahmer et al., 2019; Vanegas et al., 2016; Zuckerman et al., 2013; Zuckerman et al., 2014). It is also unclear why some children are more likely to receive a diagnosis of language versus speech delay, particularly given the lack of evidence that prevalence of CD types should inherently vary by child ethnicity or home language(s). EI/ECSE providers may not know how or have the resources to properly assess speech production in multilingual or multicultural contexts (Huerta et al., 2021; Guiberson & Atkins, 2012), may misattribute articulation difficulties to language delay when children are from multilingual backgrounds, may fail to notice differences in articulation in a language that they do not speak proficiently, or may overattribute errors in articulation to dialectal differences in a failed attempt to be sensitive to children’s linguistic varieties. Regardless of the cause, differences in ASD and HI identification rates and misdiagnosis of CDs are of serious concern. Condition-specific therapy is associated with improving long-term outcomes for ASD (e.g., Weitlauf et al., 2014) and is available in Oregon. Early diagnosis of HI similarly supports favorable child outcomes (Pimperton & Kennedy, 2012). Wrong-condition focused speech and language treatment plans is also likely to limit communication growth. Therefore, EI/ECSE providers may need specific training in identifying early signs of ASD and HI in diverse contexts in addition to administration and interpretation of least-biased approaches that support differential diagnosis of CDs from the natural influences of children’s language(s) and culture(s) on communication development (e.g., dynamic assessment; Castilla-Earls et al., 2020) as required by law (IDEA, 2004). Unfortunately, research demonstrates that Oregon’s EI/ECSE providers are not currently using such practices when evaluating Latino/a children (Huerta et al., 2021), potentially leading to non-condition-focused, or wrong-condition-focused treatment plans for children from diverse backgrounds.
Adding specificity to federal policy around what should be required of states to promote preparation of “fully and appropriately qualified” EI providers (§1435; IDEA, 2004) could be an avenue for addressing this issue. Currently, IDEA statutes include language suggesting that training addresses “rural and inner city areas” and “the emotional and social development of young children”, which could be expanded to include training on diagnostic approaches in multilingual contexts. Similar policies could be enacted in Part B to support ECSE personnel involved in assessment, who are required to be “trained and knowledgeable” and to not make a determination of eligibility for special education services based on “limited English proficiency” (§1414; IDEA, 2004); however, in contrast to Part C, Part B of IDEA does not require states to provide training. Thus, a general provision added to Part B that promotes the role of states in ensuring ongoing professional development of ECSE providers could be beneficial. Relatedly, allocation of federal funding to support implementation of such policy is needed.
Limitations and Future Directions
This study has limitations. The sample size was large, and we examined multiple outcomes. There is a possibility of Type 1 error with large datasets (Kaplan et al., 2014), and significant differences may not always represent clinically meaningful effects. We adjusted for this challenge by using a higher-than-conventional level for statistical significance and focusing our discussion on outcomes with the most notable differences between groups. In addition, the data were from Oregon, which differs from other states in its EI/ECSE structure, developmental screening practices, and population characteristics (Hirai et al., 2018; McManus et al., 2009). Thus, future research is needed to replicate and generalize these findings. It is further recommended that states analyze their data on children’s experiences in EI and ECSE in similar ways to identify state-specific policy and practice recommendations for enhancing equity.
Moreover, there are several limitations to the use of administrative data only. First, analyses of these data only provide information on outcome distribution by child ethnicity and language, which are only proxy variables for underlying constructs such as cultural views on disability, acculturation to the US special education system, and health literacy; further research is needed to examine the interpersonal factors or relational inequities that ultimately lead to the distributional inequities identified in this study. Together, this information will provide a complete picture of interventions needed to improve equity in EI/ECSE (Nalani et al., 2021). Second, although missing data were low, data entry may have been subject to error. For instance, we were unable to verify children’s ethnicity and language or the accuracy of their EI/ECSE eligibilities and whether this differed across groups. Third, the data source did not capture all relevant variables. For example, we had no measure of parental English proficiency, which has been shown to be a strong predictor of child health and educational differences (Flores et al., 2005). We were also unable to assess in this study whether the EI/ECSE assessment services were culturally and linguistically responsive or compliant with state and federal regulations specific to children from multilingual and multicultural homes; yet, previous reports on this issue suggest they are not (Huerta et al., 2021). Last, the dataset only had information on children who had engaged with EI/ECSE; disparities in who accesses this system in the first place may be of critical importance.
Conclusions
This study has broad implications. First, our analyses make clear that understanding state-level disparities benefits from specifying discrete steps along the EI/ECSE pipeline as well as child ethnic and language groups. Ultimately, this level of precision supports development of targeted policy and practice solutions with particular communities in light of the generally scant resources available in special education. For example, our evidence suggests that, in Oregon, access to EI/ECSE evaluations following referral is fairly equitable. However, differences by ethnicity and language were noted in placement for communication disorders, suggesting patterns of over- and under-identification for children from specific communities. This is the primary leak in Oregon’s EI/ECSE pipeline, which may be addressed through a focus on systemic change, including (but not limited to) improved diagnostic procedures, professional development, and state guidelines. Second, this study underlines the importance of moving beyond examining only children’s race or ethnicity to also assess their language(s) when answering questions about disparities. Our results suggest that both Latino/a ethnicity and home language are important; however, home language often enacted a greater influence on EI/ECSE inequities.
Supplementary Material
Acknowledgements.
This study was funded by a University of Oregon – Oregon Health & Science University Collaborative Seed Grant, awarded to the first and last authors. The authors thank Dan Smellow, Steve Nordby, and Cortney McIntyre-Trent for their technical support.
References
- Annamma SA, Connor D, & Ferri B (2013). Dis/ability critical race studies (DisCrit): Theorizing at the intersections of race and dis/ability. Race Ethnicity and Education, 16(1), 1–31. [Google Scholar]
- American Speech-Language-Hearing Association [ASHA] (n.d.). Early Intervention. (Practice Portal) Retrieved November 17, 2021, from www.asha.org/Practice-Portal/Professional-Issues/Early-Intervention/.
- American Speech-Language-Hearing Association [ASHA]. (1993). Definitions of communication disorders and variations [Relevant Paper] Available from www.asha.org/policy. [PubMed]
- Atkins KL, Dolata JK, Blasco PM, Saxton SN, & Duvall SW (2020). Early Intervention Referral Outcomes for Children at Increased Risk of Experiencing Developmental Delays. Maternal and Child Health Journal, 24(2), 204–212. 10.1007/s10995-019-02830-4 [DOI] [PubMed] [Google Scholar]
- Azim A, Rdesinski RE, Phelps R, & Zuckerman KE (2020). Nonclinical factors in autism diagnosis: Results from a national health care provider survey. Journal of Developmental & Behavioral Pediatrics, 41(6), 428–435. [DOI] [PubMed] [Google Scholar]
- Banerjee R, & Luckner J (2014). Training needs of early childhood professionals who work with children and families who are culturally and linguistically diverse. Infants & Young Children, 27(1), 43–59. [Google Scholar]
- Bianco M (2005). The effects of disability labels on special education and general education teachers’ referrals for gifted programs. Learning Disability Quarterly, 28(4), 285–293. [Google Scholar]
- Blanchard SB, Ryan Newton J, Didericksen KW, Daniels M, & Glosson K (2021). Confronting Racism and Bias Within Early Intervention: The Responsibility of Systems and Individuals to Influence Change and Advance Equity. Topics in Early Childhood Special Education, 41(1), 6–17. [Google Scholar]
- Castilla-Earls A, Bedore L, Rojas R, Fabiano-Smith L, Pruitt-Lord S, Restrepo MA, & Peña E (2020). Beyond scores: Using converging evidence to determine speech and language services eligibility for dual language learners. American Journal of Speech-Language Pathology, 29(3), 1116–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W, Qian L, Shi J, & Franklin M (2018). Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Medical Research Methodology, 18(1), 63. 10.1186/s12874-018-0519-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho SJ, & Gannotti ME (2005). Korean‐American mothers’ perception of professional support in early intervention and special education programs. Journal of Policy and Practice in Intellectual Disabilities, 2(1), 1–9. [Google Scholar]
- Clements KM, Barfield WD, Kotelchuck M, & Wilber N (2008). Maternal socio-economic and race/ethnic characteristics associated with early intervention participation. Maternal and Child Health Journal, 12(6), 708–717. DOI: 10.1007/s10995-007-0291-3 [DOI] [PubMed] [Google Scholar]
- Collins PH (2015). Intersectionality's definitional dilemmas. Annual review of sociology, 41, 1–20. [Google Scholar]
- Conroy K, Rea C, Kovacikova GI, Sprecher E, Reisinger E, Durant H, ... & Toomey SL (2018). Ensuring timely connection to early intervention for young children with developmental delays. Pediatrics, 142(1). 10.1542/peds.2017-4017 [DOI] [PubMed] [Google Scholar]
- Delgado CE, & Scott KG (2006). Comparison of referral rates for preschool children at risk for disabilities using information obtained from birth certificate records. The Journal of Special Education, 40(1), 28–35. 10.1177/00224669060400010301 [DOI] [Google Scholar]
- Dunn L (1968). Special education for the mildly retarded: Is much of it justifiable? Exceptional Children, 7, 5–24. 10.1177/001440296803500101 [DOI] [PubMed] [Google Scholar]
- Duranti A, Ochs E, & Schieffelin BB (Eds.). (2014). The handbook of language socialization West Sussex, UK: John Wiley & Sons. [Google Scholar]
- Flores G, Abreu M, & Tomany-Korman SC (2005). Limited English proficiency, primary language at home, and disparities in children's health care: how language barriers are measured matters. Public Health Reports, 120(4), 418–430. 10.1177/003335490512000409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guiberson M, & Atkins J (2012). Speech-language pathologists’ preparation, practices, and perspectives on serving culturally and linguistically diverse children. Communication Disorders Quarterly, 33(3), 169–180. 10.1177/1525740110384132 [DOI] [Google Scholar]
- Green SE “What do you mean ‘what’s wrong with her?’”: Stigma and the lives of families of children with disabilities. Social Science & Medicine, 57(8), 1361–1374. [DOI] [PubMed] [Google Scholar]
- Hardin BJ, Mereoiu M, Hung HF, & Roach-Scott M (2009). Investigating parent and professional perspectives concerning special education services for preschool Latino children. Early Childhood Education Journal, 37(2), 93–102 [Google Scholar]
- Hebbeler K, Spiker D, Bailey D, Scarborough A, Mallik S, Simeonsson R, & Nelson L (2007). Early intervention for infants and toddlers with disabilities and their families: Participants, services, and outcomes Menlo Park, CA: SRI International. https://www.sri.com/wp-content/uploads/pdf/neils_finalreport_200702.pdf [Google Scholar]
- Hirai AH, Kogan MD, Kandasamy V, Reuland C, & Bethell C (2018). Prevalence and variation of developmental screening and surveillance in early childhood. JAMA Pediatrics, 172(9), 857–866. 10.1001/jamapediatrics.2018.1524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang HH, & Diamond KE (2009). Early childhood teachers’ ideas about including children with disabilities in programmes designed for typically developing children. International Journal of Disability, Development and Education, 56(2), 169–182. [Google Scholar]
- Huerta L, Cycyk LM, Sanford-Keller H, Busch A, Dolata J, Moore H, ... & Zuckerman K (2021). A Retrospective Review of Communication Evaluation Practices of Young Latinx Children. Journal of Early Intervention [advanced online publication]
- Individuals with Disabilities Education Improvement Act [IDEA] of 2004 (2004).
- Jimenez ME, Barg FK, Guevara JP, Gerdes M, & Fiks AG (2012). Barriers to evaluation for early intervention services: parent and early intervention employee perspectives. Academic Pediatrics, 12(6), 551–557. 10.1016/j.acap.2012.08.006 [DOI] [PubMed] [Google Scholar]
- Jimenez ME, Fiks AG, Shah LR, Gerdes M, Ni AY, Pati S, & Guevara JP (2014). Factors associated with early intervention referral and evaluation: a mixed methods analysis. Academic Pediatrics, 14(3), 315–323. 10.1016/j.acap.2014.01.007 [DOI] [PubMed] [Google Scholar]
- Kaplan RM, Chambers DA, & Glasgow RE (2014). Big data and large sample size: a cautionary note on the potential for bias. Clinical and Translational Science, 7(4), 342–346. 10.1111/cts.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koskan A, Friedman D, Hilfinger Messias D, Brandt H, & Walsemann K (2013). Sustainability of promotora initiatives: Program planners’ perspectives. Journal of Public Health Management and Practice, 19, E1–E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law J, Boyle J, Harris F, Harkness A, & Nye C (2000). Prevalence and natural history of primary speech and language delay: findings from a systematic review of the literature. International Journal of Language and Communication Disorders, 35, 165–188. [DOI] [PubMed] [Google Scholar]
- Lo L (2008). Chinese families' level of participation and experiences in IEP meetings. Preventing School Failure: Alternative Education for Children and Youth, 53(1), 21–27. [Google Scholar]
- Love HR, & Beneke MR (2021). Pursuing justice-driven inclusive education research: Disability critical race theory (DisCrit) in early childhood. Topics in Early Childhood Special Education, 41(1), 31–44. 10.1177/0271121421990833 [DOI] [Google Scholar]
- Maenner MJ, Shaw KA, & Baio J (2020). Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveillance Summaries, 69(4), 1–12. 10.15585/mmwr.ss6904a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaña S, Lopez K, Paradiso De Sayu R, & Miranda E (2014). Use of promotoras de salud in interventions with Latino families of children with IDD. In Hodapp R (Ed.) International Review of Research in Developmental Disabilities (Vol. 47, pp. 39–75). IRRDD, UK: Academic Press. [Google Scholar]
- Magnusson DM, Minkovitz CS, Kuhlthau KA, Caballero TM, & Mistry KB (2017). Beliefs regarding development and early intervention among low-income African American and Hispanic mothers. Pediatrics, 140(5), e20172059. 10.1542/peds.2017-2059 [DOI] [PubMed] [Google Scholar]
- Meek S, Smith L, Allen R, Catherine E, Edyburn K, Williams C, . . .Pontier R (2020). Start with equity: From the early years to the early grades Children’s Equity Project and Bipartisan Policy Center. https://childandfamilysuccess.asu.edu/sites/default/files/2020-07/CEP-report-071520-FINAL.pdf [Google Scholar]
- McManus B, McCormick MC, Acevedo-Garcia D, Ganz M, & Hauser-Cram P (2009). The effect of state early intervention eligibility policy on participation among a cohort of young CSHCN. Pediatrics, 124(Supplement_4), S368–S374. 10.1542/peds.2009-1255G [DOI] [PubMed] [Google Scholar]
- McManus BM, Richardson Z, Schenkman M, Murphy NJ, Everhart RM, Hambidge S, & Morrato E (2020). Child characteristics and early intervention referral and receipt of services: a retrospective cohort study. BMC pediatrics, 20(1), 84. 10.1186/s12887-020-1965-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan PL, Farkas G, Hillemeier MM, & Maczuga S (2012). Are minority children disproportionately represented in early intervention and early childhood special education?. Educational Researcher, 41(9), 339–351. 10.3102/0013189X12459678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrier MJ, & Gallagher PA (2011). Disproportionate representation in placements of preschoolers with disabilities in five southern states. Topics in Early Childhood Special Education, 31(1), 48–57. 10.1177/0271121410363830 [DOI] [Google Scholar]
- Nalani A, Yoshikawa H, & Carter PL (2021). Social Science–Based Pathways to Reduce Social Inequality in Youth Outcomes and Opportunities at Scale. Socius, 7, 1–17. [Google Scholar]
- National Kids Count. Child population by race in Oregon. (n.d.) https://datacenter.kidscount.org/data/tables/103-child-population-by-race#detailed/2/39/false/37,871,870/68,69,67,12,70,66,71,72/423,424.
- Oregon Administrative Rules [OAR] Oregon administrative rules database. (n.d.). https://secure.sos.state.or.us/oard/processLogin.action.
- Oregon Office of Rural Health (2020). Oregon Service Areas and Their ORH Urban/Rural/Frontier Designation Retrieved from www.ohsu.edu/oregon-office-of-rural-health/orh-service-areas.
- Parish S, Magaña S, Rose R, Timberlake M, & Swaine JG (2012). Health care of Latino children with autism and other developmental disabilities: Quality of provider interaction mediates utilization. American Journal on Intellectual and Developmental Disabilities, 117(4), 304–315. [DOI] [PubMed] [Google Scholar]
- Pimperton H, & Kennedy CR (2012). The impact of early identification of permanent childhood hearing impairment on speech and language outcomes. Archives of Disease in Childhood, 97(7), 648–653. 10.1136/archdischild-2011-301501 [DOI] [PubMed] [Google Scholar]
- Romo HD, Thomas KJ, & García EE (2018). Changing demographics of dual language learners and English learners: implications for school success. Social Policy Report, 31(2), 1–35. Retrieved from 10.1002/j.2379-3988.2018.tb00028.x [DOI] [Google Scholar]
- Rosa J, & Flores N (2017). Unsettling race and language: Toward a raciolinguistic perspective. Language in Society, 46(5), 621–647. [Google Scholar]
- Rossetti Z, Sauer JS, Bui O, & Ou S (2017). Developing collaborative partnerships with culturally and linguistically diverse families during the IEP process. Teaching Exceptional Children, 49(5), 328–338. [Google Scholar]
- Sapiets SJ, Totsika V, & Hastings RP (2021). Factors influencing access to early intervention for families of children with developmental disabilities: A narrative review. Journal of Applied Research in Intellectual Disabilities, 34(3), 695–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schieffelin BB, & Ochs E (1986). Language socialization. Annual Review of Anthropology, 15(1), 163–191. [Google Scholar]
- Shapiro BJ, & Derrington TM (2004). Equity and disparity in access to services: An outcomes-based evaluation of early intervention child find in Hawaii. Topics in Early Childhood Special Education, 24(4), 199–212. 10.1177/02711214040240040201 [DOI] [Google Scholar]
- Stahmer AC, Dababnah S, & Rieth SR (2019). Considerations in implementing evidence-based early autism spectrum disorder interventions in community settings. Pediatric medicine (Hong Kong, China), 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States [US] Census. Quick facts: Oregon. (n.d.) https://www.census.gov/quickfacts/OR.
- United States Department of Education [US DOE], Office of Special Education and Rehabilitative Services, Office of Special Education Programs (2022). 43rd Annual Report to Congress on the Implementation of the Individuals with Disabilities Education Act, 2021, Washington, D.C. [Google Scholar]
- Vanegas SB, Magaña S, Morales M, & McNamara E (2016). Clinical validity of the ADI-R in a US-based Latino population. Journal of Autism and Developmental Disorders, 46(5), 1623–1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitlauf AS, McPheeters ML, Peteres B, Sathe N, Travis R, Aiello R, Williamson E, Veenstra-VanderWeele J, Krishnaswami S, Jerome R, & Warrren Z (2014). Therapies for children with autism spectrum disorder: behavioral interventions update. Comparative Effectiveness Review No. 137 Agency for Healthcare Research and Quality, Rockville: MD. [PubMed] [Google Scholar]
- WestRasmus EK, Pineda-Reyes F, Tamez M, & Westfall JM (2012). Promotora de salud and community health workers: An annotated bibliography. Family Community Health, 35(2), 172–182. [DOI] [PubMed] [Google Scholar]
- Wolfe K, & Durán LK (2013). Culturally and linguistically diverse parents’ perceptions of the IEP process: A review of current research. Multiple Voices for Ethnically Diverse Exceptional Learners, 13(2), 4–18. [Google Scholar]
- Young AR, Beitchman JH, Johnson C, Douglas L, Atkinson L, Escobar M, & Wilson B (2002). Young adult academic outcomes in a longitudinal sample of early identified language impaired and control children. Journal of Child Psychology and Psychiatry, 43(5), 635–645. [DOI] [PubMed] [Google Scholar]
- Zuckerman et al., 2013 Zuckerman KE, Mattox K, Donelan K, Batbayar O, Baghaee A, & Bethell C (2013). Pediatrician identification of Latino children at risk for autism spectrum disorder. Pediatrics, 132(3), 445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Mattox KM, Sinche BK, Blaschke GS, & Bethell C (2014). Racial, ethnic, and language disparities in early childhood developmental/behavioral evaluations: A narrative review. Clinical Pediatrics, 53(7), 619–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


