Abstract
Objective
To determine whether nurse practitioners can provide care at first point of contact equivalent to doctors in a primary care setting.
Design
Systematic review of randomised controlled trials and prospective observational studies.
Data sources
Cochrane controlled trials register, specialist register of trials maintained by Cochrane Effective Practice and Organisation of Care Group, Medline, Embase, CINAHL, science citation index, database of abstracts of reviews of effectiveness, national research register, hand searches, and published bibliographies.
Included studies
Randomised controlled trials and prospective observational studies comparing nurse practitioners and doctors providing care at first point of contact for patients with undifferentiated health problems in a primary care setting and providing data on one or more of the following outcomes: patient satisfaction, health status, costs, and process of care.
Results
11 trials and 23 observational studies met all the inclusion criteria. Patients were more satisfied with care by a nurse practitioner (standardised mean difference 0.27, 95% confidence interval 0.07 to 0.47). No differences in health status were found. Nurse practitioners had longer consultations (weighted mean difference 3.67 minutes, 2.05 to 5.29) and made more investigations (odds ratio 1.22, 1.02 to 1.46) than did doctors. No differences were found in prescriptions, return consultations, or referrals. Quality of care was in some ways better for nurse practitioner consultations.
Conclusion
Increasing availability of nurse practitioners in primary care is likely to lead to high levels of patient satisfaction and high quality care.
What is already known on this topic
Nurse practitioners have existed in North America for many years
An increasing number of such nurses are being employed in the United Kingdom in general practice, emergency departments, and other primary care settings
Reviews suggest that nurse practitioners are equivalent to doctors on most variables studied, but the relevance of this in the context of the NHS is unclear
What this study adds
Patients are more satisfied with care from a nurse practitioner than from a doctor, with no difference in health outcomes
Nurse practitioners provide longer consultations and carry out more investigations than doctors
Most recent research has related to patients requesting same day appointments for minor illness, which is only a limited part of a doctor's role
Introduction
Recent policy developments in the National Health Service, including NHS walk-in centres, NHS Direct, and nurse led personal medical services schemes, have been based on nurses rather than doctors acting as first point of contact with the health service.1,2 Several factors have led to this expansion in the role of nurses, including issues of cost, the need to increase provision of care to improve access, the availability of doctors, and the skills and expertise of nurses.
Particular interest has been shown in the concept of nurse practitioners providing front line care in general practice and in emergency departments. In this way they may potentially substitute for doctors, particularly in the management of patients with acute illness. Nurse practitioners have undergone further training, often at graduate level, to work autonomously, making independent diagnoses and treatment decisions.3 It is important to consider whether the evidence supports the notion that nurse practitioners can substitute for doctors by providing safe, effective, and economical front line management of patients.
Nurse practitioners have been established in North America for several decades, and studies of their role have been reviewed previously.4,5 But these reviews are dated and of limited applicability to the United Kingdom. After the expansion of nurse practitioners in the NHS during the 1990s, several relevant randomised controlled trials have been published that directly compare nurse practitioners and doctors. We aimed to systematically review research that assesses the process, costs, or outcomes of care provided by nurse practitioners compared with doctors, working in primary care as a first point of contact for any patient with undifferentiated health problems.
Methods
Selection of studies for review
We included randomised controlled trials and observational studies with a prospective experimental design comparing nurse practitioners and doctors working in a similar way as concurrent controls. Because of inconsistency in the use of the term “nurse practitioner,” we developed criteria to determine whether papers should be included. We included studies where nurses provided first point of contact, made an initial assessment, and managed patients autonomously, whether or not they were described as nurse practitioners. We used sensitivity analysis to examine the effect on our results of including or excluding “ambiguous” studies where inclusion was debatable.
We also included studies if the nurse provided care at first point of contact for unselected patients in primary care including general practice, out of hours centres, walk-in centres, and emergency departments. The main focus of our review was previously undiagnosed patients with undifferentiated health problems. We limited our review to studies from developed countries (Europe, North America, Australasia, Israel, South Africa, and Japan) to increase its relevance for the UK system. Some studies concerned care provided at a single consultation, others concerned care over a period of time. We included both types of study, but we used sensitivity analysis to compare the results from these different types. Finally, we only included studies if they provided data about one or more of the following outcomes: patient satisfaction, health status, health service costs, or process of care measures (consultation length, number of prescriptions, investigations, referrals, admissions, return consultations, patient adherence, or measures of quality of care).
Identification of studies
We identified studies from searches of electronic databases and hand searches of recent editions of relevant journals, bibliographies, and reference lists of other reviews and papers.6,7 We scrutinised the following databases with no language restrictions: Medline (1966-2001), Embase (1980-2001), CINAHL (1982-2001), science citation index, database of abstracts of reviews of effectiveness, national research register, Cochrane controlled trials register and the specialist register of trials maintained by the Cochrane Effective Practice and Organisation of Care Group. We used the Cochrane optimal search strategy for randomised controlled trials, with advice from university librarians. All educational centres offering training for nurse practitioners in the United Kingdom and nurse practitioner organisations in the United States, South Africa, and Australia were approached for any unpublished studies. We contacted authors of included studies for additional research and for missing data. Data were extracted by one reviewer (SH) and one of two other reviewers (EA or CS) working independently. Disagreements were resolved by discussion with the third reviewer.
Assessment of study quality
We assessed methodological quality on the basis of the criteria of the review group of the Cochrane Effective Practice and Organisation of Care Group. We did not calculate a composite score for study quality in view of the current debate about the validity of such scores.8,9
Data analysis
We conducted our analyses with Meta-View Rev-Man software version 4.1. We calculated odds ratios for dichotomous outcomes and standardised mean differences for continuous outcomes. We used random effects methods in the analysis because of the degree of heterogeneity of the studies. If standard deviations were not available we used the average standard deviation reported by other studies for that outcome. We used meta-analytic techniques to combine data from the randomised controlled trials where at least two studies provided data on a particular outcome. For the observational studies we compared the findings qualitatively. These studies were carried out in a variety of settings; many were small and had other methodological shortcomings, making quantitative synthesis inappropriate. We analysed studies set in emergency departments or minor injury units together and separately from those based in general practice owing to the degree of heterogeneity between these different settings.
We investigated heterogeneity by examining the results from studies conducted in differing settings, studies of individual consultations or care over time, and studies of nurse practitioners with different levels of qualification. We carried out sensitivity analysis to explore the impact of including or excluding studies where there was ambiguity regarding inclusion.
Results
Searches identified 119 potentially relevant papers, of which 35 reporting 34 studies fulfilled the inclusion and exclusion criteria. These papers comprised 11 randomised controlled trials (table A on bmj.com) and 23 observational studies (table B on bmj.com). Tables C and D on bmj.com show the quality assessment of the included studies.
The results for the observational studies may be obtained from the authors. The findings of the observational studies replicated those of the randomised controlled trials for all outcomes except costs and investigations, despite shortcomings in their design.
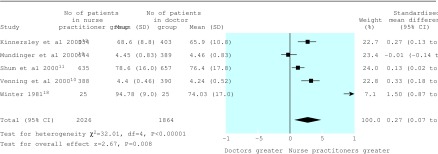
Patient satisfaction
Nine randomised trials reported patient satisfaction (one of these was unpublished).10–18 One paper could not be included in a meta-analysis owing to a lack of detail in the reporting of results.13 Five trials reported continuous data on patient satisfaction (figure). These were all in general practice settings, three in the United Kingdom and two in the United States.10–12,14,18
The figure presents the summary statistics for studies using continuous data. These suggest that patients were more satisfied with consultations with nurse practitioners than those with doctors. The results showed considerable heterogeneity, which was explored by comparing studies of individual consultations with care over time and by comparing studies based on nurse practitioners with different levels of training. Although there remained considerable heterogeneity between the studies, all analyses suggested that patients were more satisfied with consultations with nurse practitioners. Three randomised controlled trials reported results with dichotomous data.15–17 Two of them were set in emergency units.16,17 No significant difference was found in patient satisfaction for patients attending either provider with these studies (all studies (n=3), odds ratio 1.56, 0.56 to 4.34; overall effect z=0.85, P=0.4; and all studies of emergency units (n=2), 3.27, 0.41 to 25.98; z=1.12, P=0.3).
Health status
Any measure used by the authors to determine either health status or quality of life and its validity for this purpose were recorded. Seven randomised controlled trials reported on these outcomes.10–12,14,16,19,20 These results were not analysed with meta-analysis because of the heterogeneity between measures and episode of care length, but a comparison of the results showed no significant differences in patient health outcomes (table E on bmj.com).
Process measures
The results for process outcomes for which there were sufficient data for meta-analysis showed that nurse practitioners undertook significantly more investigations and had longer consultations than doctors (table).
Quality of care
Quality of care measures may include communication skills, accurate diagnosis, investigations appropriately carried out, and appropriate advice on self management or medication.21 Six randomised controlled trials reported quality of care outcomes (see table F on bmj.com).11–13,15–17 Heterogeneity of measures used meant that analysis was restricted to qualitative review only. Nurse practitioners seemed to identify physical abnormalities more often.13 In one study nurse practitioners gave more information to patients.11 Interestingly this study also reported no apparent difference in patients' intention to self treat next time. Nurse practitioners made more complete records and scored better on communication than did doctors.16,17 They also offered more advice on self care and management.11,12 Two studies set in emergency departments tested the appropriateness of investigations and ability to interpret x ray films.16,17 The results suggested that nurse practitioners were as accurate as doctors at ordering and interpreting x ray films, with small in-study variations depending on the relative experience of both providers.
Discussion
Nurse practitioners can provide care that leads to increased patient satisfaction and similar health outcomes when compared with care from a doctor. Nurse practitioners seemed to provide a quality of care that is at least as good, and in some ways better, than doctors.
Although all of the randomised trials found no significant differences between doctors and nurse practitioners in health outcomes, the research has important limitations. The studies used many different outcome measures, reflecting the difficulty in measuring changes in health outcomes after single consultations predominantly about minor illnesses. None of the studies in our review was adequately powered to detect rare but serious adverse outcomes. Since one important function of primary care is to detect potentially serious illness at an early stage, a large study with adequate length of follow up is now justified.
Limitations of the review
Ambiguity exists over the use of the term “nurse practitioner,” with much debate about this role.22,23 The overlap between nursing roles in the United Kingdom and the introduction of another advanced practice nursing title, nurse consultant, adds to the difficulty in understanding the role definitions in nursing.1,2,24 Although specific training for nurse practitioners is available, the content of this varies.25 Because of this ambiguity, the definition used in our review was purposefully inclusive.
Our review was limited by the quality of the available studies. There were few recent randomised trials, and the larger number of observational studies were generally of poor quality. Because of these problems we based our conclusions primarily on the randomised trials, the more recent of which were of generally high quality, although only one study used patients new to both providers.14
Noticeable heterogeneity was observed between the studies on almost all outcomes. Although differences between studies in terms of setting, level of nurse training, and the period of time studied were anticipated and explored in our review, much heterogeneity remained after allowing for these factors. This probably reflects the diverse ways in which nurse practitioners currently work. Despite these differences, the direction of the effect for the main findings was consistent between different studies and also between the randomised controlled trials and the observational studies.
It was not possible to conduct a robust economic analysis of the costs of care from nurse practitioners compared with doctors. Only five studies provided data about costs.10,12,15,16,26 These used different approaches to the valuing of resources and were inadequately powered for economic analysis. The lack of good evidence about the economic impact of substituting nurse practitioners for doctors needs to be addressed in future research, otherwise changes may be introduced that are thought to be efficient when they may not be so.27
Policy implications
Our review lends support to an increased involvement of nurse practitioners in primary care. However, most recent research has been based on nurse practitioners providing care for patients requesting same day appointments predominantly for acute minor illness and working in a team supported by doctors. It cannot be assumed that similar results would be obtained by nurse practitioners working in different settings or with different groups of patients, nor that they could substitute entirely for general practitioners.
Unresolved issues
Future research should address several unresolved issues. Firstly, if patients are more satisfied with care provided by nurse practitioners then the factors that lead to this effect should be elucidated. Satisfaction with care could be related to differences in the training and consultation skills of nurses, patients' expectations, or the extra length of time that nurse practitioners spend in consultations.
Secondly, nurse practitioners and doctors did not necessarily work under similar circumstances or with similar pressures on their time, even in the controlled trials. It is necessary to determine whether the differences between nurse practitioners and doctors in patient satisfaction and quality of care remain if they work under identical circumstances, particularly with the same rates of booked consultations.
Thirdly, research on nurse practitioners needs to be broadened to encompass a wider range of patient groups, including those with complex psychosocial problems or chronic diseases. Research is also necessary that extends beyond the scope of comparing individual nurses with doctors and evaluates different models of organisation, such as several nurse practitioners providing care at first point of contact supported by a smaller number of general practitioners providing second line advice.
Finally, the role of a nurse practitioner is not clearly defined in the United Kingdom and includes nurses from a wide range of educational backgrounds. In addition, nurses are increasingly involved in assessing and advising patients with minor illness in settings such as NHS Direct and NHS walk-in centres without a recognised qualification for this role. It is important to study the training, skills, and experience that nurses need in order to offer the benefits to patients shown by our review.
Conclusion
Patients are at least as satisfied with care at the point of first contact with nurse practitioners as they are with that from doctors. Although assessments of the quality of care and short term health outcomes seem to be equivalent to that of doctors, further research is needed to confirm that nurse practitioner care is safe in terms of detecting rare but important health problems.
Supplementary Material
Figure.
Studies reporting continuous data on patient satisfaction
Table.
Process measures
| No of studies | No in intervention group | No in control group | Odds ratio or weighted mean difference (95% CI) |
Heterogeneity
|
Overall
effect
|
||||
|---|---|---|---|---|---|---|---|---|---|
| χ2 | P value | Z value | P value | ||||||
| Consultation length | 5 | 2277; mean 14.89 min | 2286; mean 11.14 min | 3.67 (2.05 to 5.29)* | 81.67 df=4 | <0.00001 | 4.44 | 0.00001 | |
| Prescriptions | 4 | 1685/2503 | 1944/2861 | 1.02 (0.90 to 1.15) | 3.26 df=3 | 0.35 | 0.32 | 0.8 | |
| Investigations | 5 | 932/2573 | 1015/2896 | 1.22 (1.02 to 1.46) | 6.31 df=4 | 0.18 | 2.18 | 0.03 | |
| Return consultations | 6 | 835/2919 | 913/3247 | 1.05 (0.87 to 1.28) | 12.06 df=5 | 0.034 | 0.54 | 0.6 | |
| Referrals | 2 | 44/1293 | 59/1367 | 0.71 (0.30 to 1.70) | 4.07 df=1 | 0.044 | 0.76 | 0.4 | |
Weighted mean difference. Only one study reported admissions and none reported patient adherence.
Acknowledgments
We thank Kate Baxter, Knut Schroeder, Alan Montgomery, and Tom Fahey (Division of Primary Health Care); Karen Rees and Margaret Burke (Department of Social Medicine); Cherry Cullen; and those authors who responded to our call for further research in this field.
Footnotes
Funding: South and West Research and Development Directorate. The views expressed are those of the authors and not necessarily those of the NHS Executive South West.
Competing interests: None declared.
Additional tables and references appear on bmj.com
References
- 1.Department of Health. The NHS plan. London: DoH; 2000. [Google Scholar]
- 2.Department of Health. Making a difference: strengthening the nursing, midwifery and health visitor contribution to health and health care. London: DoH; 1999. [Google Scholar]
- 3.Royal College of Nursing. Nurse practitioners: your questions answered. London: RCN; 1996. [Google Scholar]
- 4.Sox HC., Jr Quality of patient care by nurse practitioners and physician's assistants: a ten-year perspective. Ann Intern Med. 1979;91:459–468. doi: 10.7326/0003-4819-91-3-459. [DOI] [PubMed] [Google Scholar]
- 5.Brown SA, Grimes DE. A meta-analysis of nurse practitioners and nurse midwives in primary care. Nurs Res. 1995;44:332–339. [PubMed] [Google Scholar]
- 6.Sergison M, Sibbald B, Rose S. Skill mix in primary care: a bibliography. Manchester: National Primary Care Research and Development Centre, University of Manchester; 1998. [Google Scholar]
- 7.Halliwell S, Sibbald B, Rose S. A bibliography of skill mix in primary care. Manchester: National Primary Care Research and Development Centre, University of Manchester; 1999. [Google Scholar]
- 8.Juni P, Altman DG, Egger M. Assessing the quality of controlled clinical trials. BMJ. 2001;323:42–46. doi: 10.1136/bmj.323.7303.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Egger M, Davey Smith G, Altman DG. Systematic reviews in health care: meta-analysis in context. London: BMJ Publishing Group; 2001. [Google Scholar]
- 10.Venning P, Durie A, Roland M, Roberts C, Leese B. Randomised controlled trial comparing cost effectiveness of general practitioners and nurse practitioners in primary care. BMJ. 2000;320:1048–1053. doi: 10.1136/bmj.320.7241.1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shum C, Humphreys A, Wheeler D, Cochrane MA, Skoda S, Clement S. Nurse management of patients with minor illnesses in general practice: multicentre, randomised controlled trial. BMJ. 2000;320:1038–1043. doi: 10.1136/bmj.320.7241.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kinnersley P, Anderson E, Parry K, Clement J, Archard L, Turton P. Randomised controlled trial of nurse practitioner versus general practitioner care for patients requesting “same day” consultations in primary care. BMJ. 2000;320:1043–1048. doi: 10.1136/bmj.320.7241.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoekelman RA. What constitutes adequate well-baby care? Pediatrics. 1975;55:313–326. [PubMed] [Google Scholar]
- 14.Mundinger MO, Kane RL, Lenz ER, Totten A, Tsai W-Y, Cleary PD. Primary care outcomes in patients treated by nurse practitioners or physicians: a randomized trial. JAMA. 2000;283:59–68. doi: 10.1001/jama.283.1.59. [DOI] [PubMed] [Google Scholar]
- 15.Spitzer WO, Sackett DL, Sibley JC, Roberts RS, Gent M, Kergin DJ. The Burlington randomized trial of the nurse practitioner. N Engl J Med. 1974;290:251–256. doi: 10.1056/NEJM197401312900506. [DOI] [PubMed] [Google Scholar]
- 16.Sakr M, Angus J, Perrin J, Nixon C, Nicholl J, Wardrope J. Care of minor injuries by emergency nurse practitioners or junior doctors: a randomised controlled trial. Lancet. 1999;354:1321–1326. doi: 10.1016/s0140-6736(99)02447-2. [DOI] [PubMed] [Google Scholar]
- 17.Cooper M. Glasgow: Accident and Emergency, Glasgow Royal Infirmary; 2001. An evaluation of the safety and effectiveness of the emergency nurse practitioner in the treatment of patients with minor injuries: a pilot study. . (Typescript.) [Google Scholar]
- 18.Winter C. MSc thesis. Long Beach, CA: California State University; 1981. Quality health care: patient assessment. [Google Scholar]
- 19.Sackett DL, Spitzer WO, Gent M, Roberts RS. The Burlington randomized trial of the nurse practitioner: health outcomes of patients. Ann Intern Med. 1974;80:137–142. doi: 10.7326/0003-4819-80-2-137. [DOI] [PubMed] [Google Scholar]
- 20.Chambers LW, West AE. The St John's randomized trial of the family practice nurse: health outcomes of patients. Int J Epidemiol. 1978;7:153–161. doi: 10.1093/ije/7.2.153. [DOI] [PubMed] [Google Scholar]
- 21.Campbell JD, Mauksch HO, Neikirk HJ, Hosokawa MC. Collaborative practice and provider styles of delivering health care. Soc Sci Med. 1990;30:1359–1365. doi: 10.1016/0277-9536(90)90316-k. [DOI] [PubMed] [Google Scholar]
- 22.Offredy M, Townsend J. Nurse practitioners in primary care. Fam Pract. 2000;17:564–569. doi: 10.1093/fampra/17.6.564. [DOI] [PubMed] [Google Scholar]
- 23.Holcomb LO. A Delphi survey to identify activities of nurse practitioners in primary care. Clin Excel Nurse Pract. 2000;4:172. [PubMed] [Google Scholar]
- 24.Roberts-Davis M, Read S. Clinical role clarification: using the Delphi method to establish similarities and differences between nurse practitioners and clinical nurse specialists. J Clin Nurs. 2001;10:33–43. doi: 10.1046/j.1365-2702.2001.00437.x. [DOI] [PubMed] [Google Scholar]
- 25.Ashburner L, Birch K, Latimer J, Scrivens E. Nurse practitioners in primary care. Keele: Centre for Health Planning and Management, Keele University; 1997. [Google Scholar]
- 26.Burnip R, Erickson R, Barr GD, Shinefield H, Schoen EJ. Well-child care by pediatric nurse practitioners in a large group practice. Am J Dis Child. 1976;130:51–55. doi: 10.1001/archpedi.1976.02120020053008. [DOI] [PubMed] [Google Scholar]
- 27.Kernick D, Scott A. Economic approaches to doctor/nurse skill mix: problems, pitfalls and partial solutions. Br J Gen Pract. 2001;17:42–47. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.