Abstract
Undernutrition (stunting, wasting and underweight) among children remains a public health concern in North Africa, especially following recent conflicts in the region. Therefore, this paper systematically reviews and meta-analyses the prevalence of undernutrition among children under five in North Africa to determine whether efforts to reduce undernutrition are on track to achieving the Sustainable Development Goals (SDGs) by 2030. Eligible studies published between 1st January 2006 and 10th April 2022 were searched for, using five electronic bibliographic databases (Ovid MEDLINE, Web of Science, Embase (Ovid), ProQuest and CINAHL). The JBI critical appraisal tool was used, and a meta-analysis was conducted using the ‘metaprop’ command in STATA, to estimate the prevalence of each undernutrition indicator in the seven North African countries (Egypt, Sudan, Libya, Algeria, Tunisia, Morocco, and Western Sahara). Due to the significant heterogeneity among studies (I2 >50%), a random effect model and sensitivity analysis were conducted to examine the effect of outliers. Out of 1592 initially identified, 27 met the selection criteria. The prevalence of stunting, wasting and being underweight were 23.5%, 7.9% and 12.9%, respectively. Significant variations between the countries with the highest rates of stunting and wasting were reported in Sudan (36%, 14.1%), Egypt (23.7%, 7.5%), Libya (23.1%, 5.9%), and Morocco (19.9%, 5.1%). Sudan also had the highest prevalence of underweight (24.6%), followed by Egypt (7%), Morocco (6.1%), and Libya (4.3%) with more than one in ten children in Algeria and Tunisia having stunted growth. In conclusion, undernutrition is widespread in the North African region, particularly in Sudan, Egypt, Libya, and Morocco, making it challenging to meet the SDGs by 2030. Nutrition monitoring and evaluation in these countries is highly recommended.
Introduction
Malnutrition, whether under- or over-nutrition, affects hundreds of millions of children worldwide. Approximately, one hundred and forty nine (149.2) million, 45.4 million, 38.9 million and 12.6% of children under-five suffer from stunting, wasting, overweight and underweight, respectively [1]. Globally, undernutrition is responsible for approximately 45% of deaths among children under five [2]. To measure undernutrition, the three anthropometric indices, namely, stunting (low height-for-age), wasting (low weight-for-height), and underweight (low weight-for-age) are used. These three undernutrition indices also represent one of 100 indicators used to measure a community’s progress toward achieving the 17 Sustainable Development Goals (SDGs) [3]. In this study, we focus on the three anthropometric indices of undernutrition (stunting, wasting, and underweight) in North African countries (Egypt, Sudan, Libya, Algeria, Tunisia, Morocco, and Western Sahara).
Nutrition during the first 2000 days (the first five years) of life is critical for the physical, cognitive, social, and emotional development of a child. Irreversible effects on a child’s physical and mental health will occur if nutritional needs are not met during this period [2, 4, 5]. Yet, the burden of undernutrition remains high among children in North African countries. For instance, stunting affects more than 35% of under-five children in Libya and Sudan. At the same time, 22.3% of children suffer from stunting in Egypt, while 6.6% of children in the entire region suffer from wasting [1]. Undernutrition has profound direct and indirect effects on individuals and families due to a child’s increased susceptibility to illnesses resulting in a heightened risk of morbidity and mortality [2]. Furthermore, undernutrition affects the economy and productivity of the entire community. Besides impairing physical growth, it also decreases academic performance, cognitive abilities, work efficiency, and earnings of individuals. Undernutrition may also result in increased costs of health care services, thereby causing the economy to grow slower, leading to less investment in human capital [6]. In Egypt and Sudan, the health costs of undernutrition among children amounts to approximately 1.10 billion Egyptian Pounds (EGP) and 11.66 billion Sudanese Pounds (SDG), respectively. In Egypt, 11% of child deaths are attributable to undernutrition and this is expected to increase by 32% by 2025, resulting in a cost of 26.8 billion EGP [7, 8].
To eliminate all forms of undernutrition, it is imperative to invest in interventions, monitor the progress of essential government initiatives and collect and analyse quality data [9]. In North African countries, there is a lack of current and specific information regarding undernutrition among children [10]. Previous studies on child undernutrition, carried out in various individual North African countries, namely Tunisia [11]; Egypt [12]; Sudan [13]; Algeria [14]; Morocco [15] and Western Sahara [16], highlighted the prevalence of undernutrition among children under five. Joulaei et al. [17]. conducted a review to examine the prevalence of stunting among children and adolescences aged 2–18 in 24 countries in the Middle Eastern and North African regions [17]. Apart from including a wide range of children ages with different growth requirements and health needs which affects the validity and generalizability of the results to all age groups, there was no information on Libya, Algeria, or Tunisia. A recent study in the Eastern Mediterranean region (including Afghanistan, Bahrain, Djibouti, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Pakistan, Oman, Palestine, Qatar, Saudi, Somalia, Sudan, Syrian, Tunisia, Emirates and Yemen) found a prevalence of malnutrition [18]. These findings did not specifically target North African countries as the results combined the area with other regions or countries; this may result in an over- or under-estimation of the problem due to a separation from local contexts. More concerningly, this may result in the misrepresentation of data used to inform local policies, strategies and decisions [19]. The limitations of the study included an over-reliance on grey literature, no peer-reviewed journal articles, and the limited timeframe of the search (2019–2020). Two years is too short a period of time to gather and analyse trends in the wider literature, or to reach comprehensive representative results as nutrition guidelines are typically updated every 5 years [18, 20, 21]. Finally, Algeria was not included in the review which could affect the generalizability of the findings to all Eastern Mediterranean countries including North African countries.
As discussed above, childhood undernutrition plays an increasingly significant role in childhood morbidity and mortality. Despite this, there are currently no ongoing nutrition monitoring and evaluation programs in North Africa to target the reduction of childhood undernutrition. Investigating how the prevalence of stunting, wasting, and underweight varies across North African countries would offer insights into how well these countries are progressing towards SDGs 1, 2, and 3 by the year 2030.
This systematic review and meta-analysis study addresses this gap. It was conducted to determine the prevalence of undernutrition (stunting, wasting, and underweight) among children under five in the North African region. The findings of this systematic review aim to help strengthen existing child nutrition policies and practices and enable policymakers to determine whether countries in the North African region are on track to meet SDGs 1, 2, and 3 by 2030. Results of the study are specific to the region and may lead to more efficient and practical applications of detailed nutrition interventions aimed at improving child health and nutrition in North Africa.
Methods
Anthropometric indicators
The current systematic review utilised three anthropometric indicators for analysis:
Stunting (chronic malnutrition): an indicator of retardation of linear growth and cumulative growth deficits in children; height-for-age <-2 standard deviation (SD) of the World Health Organisation (WHO) child growth standards median.
Wasting (acute malnutrition): measuring of body mass concerning the height and describing the current nutritional status; weight-for-height <-2 SD of the WHO child growth standards median.
Underweight: is a composite index of height-for-age and weight-for-height. It takes into account both acute malnutrition (wasting) and chronic malnutrition (stunting), but it does not distinguish between the two; weight-for-age <-2 standard deviations (SD) of the WHO child growth standards median [22].
Search strategy
To review the existing literature, the study used the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) 2020 guidelines [23]. The PRISMA 2020 checklists for the manuscript and abstract are attached as additional S1 and S2 Tables. The protocol was submitted and registered with the Prospective Registry of Systematic Reviews (PROSPERO number CRD42022311922). Five databases were scanned for relevant peer-reviewed articles: Ovid MEDLINE, Web of Science, Embase (Ovid), ProQuest, and CINAHL. In addition, MeSH headings with related subheadings were combined with key terms for the included countries, region, and age-specific search terms were added to ensure all relevant studies were identified. In addition, the reference lists of retrieved articles and Google Scholar were screened for further relevant publications. Articles retrieved were imported from each database into an EndNote library. The following combination of keywords was used in the search: (Child* or under-five* or paediatr* or infant* or bab*) AND (Malnutr* or malnourish* or undernourish* or undernutr* or stunt* or wast* or underweight*) AND (Egypt* or Sudan* or Libya* or Algeria* or Tunisia* or Morocco* or Western Sahara* or North Africa*) AND (prevalence* or rate*).
Eligibility criteria
To be included in the review studies needed to meet the following criteria: 1) participants aged between 0 and 59 months of age; 2) conducted in any or all of the North African countries (Egypt, Sudan, Libya, Algeria, Tunisia, Morocco and Western Sahara); (3) investigated one or more anthropometric indicators of undernutrition (stunting, wasting, and underweight); 4) observational studies only (no qualitative, intervention, review, or experimental studies were considered); (5) published in peer-reviewed journals (no abstracts, policy briefs, or conference proceedings were reviewed); (6) written only in English and (7) published between 1 January 2006 and 10 April 2022. The year 2006 was used as a baseline in this review to capture the period when WHO Child Growth Standards were introduced by the WHO.
Data extraction
All retrieved articles were imported from each database into EndNote X20 (Clarivate Analytics, USA) and sorted and ordering in a scientific and organised manner [24]. After removing duplicates, the first author, NFE, reviewed the study titles and screened all the publications. Following this initial screening, the second phase involved reading the abstracts and to identify the eligible studies. The third and final screening involved reading the full texts and ensuring each study met the eligibility criteria.
The identified studies are listed in Table 1, with the following information: The author, year of publication, geographic region, year of data collection, number of children and age, sample strategy, study design, population characteristics, and quality assessment score. In S4 Table, the included literature was classified according to the country of study and the prevalence of the three indices of undernutrition.
Table 1. Characteristics of included publications in the literature.
| Author; year | Geographical Region | Year of Data Collection | Children (No); Age | Sample Strategy | Study Design | Population Characteristics | Quality Assessment Score |
|---|---|---|---|---|---|---|---|
| Abdalla et al. 2009 | El Fau (Rural area) in Sudan | 2003 | N = 150 6–60 months |
Random sampling | Cross sectional study | Children under five in the three target villages | Medium |
| Abu-Manga et al. 2021 | Sudan | 2019 | N = 145,002 0–5 years |
Multi-stage stratified sampling design | Cross sectional study | Children under five from households in the Sudanese community | High |
| Aitsi-Selmi 2014 | Egypt | 1992–95 | N = 9,201 0–5 years |
Multi-stage stratified sampling design | Cross sectional study | Children under five in the community | High |
| 2005–8 | N = 13,376 0–5 years |
||||||
| Almasi et al. 2019 | Egypt | 2014 | N = 14898.9 0–5 years |
Multi-stage stratified sampling design | Cross sectional study | Children under five in the Eastern Mediterranean countries | Medium |
| Libya | 2007 | N = 10723 0–5 years |
|||||
| Morocco | 2011 | N = 6872.6 0–5 years |
|||||
| Sudan | 2014 | N = 11712.3 0–5 years |
|||||
| Tunisia | 2012 | N = 2677.3 0–5 yrs. |
|||||
| Barouaca 2012 | Morocco | 2004 | N = 5311 0–5 yrs. |
Multistage sampling surveys | Cross sectional study | Children under five in the community | Medium |
| 1997 | N = 5240 0–5 years |
||||||
| 1992 | N = 4502 0–5 years |
||||||
| Dahab et al 2020 | Sudan | 2014 | N = 14,081 0–5 years |
Stratified multistage cluster sampling design | Cross sectional study | Children under five from households in armed conflicts in Darfur in Eastern state, Blue Nile and South Kordofan | High |
| Elsary 2017 | Egypt (Tamiya district in Fayoum) | 2014 | N = 400 0–5 years |
Multi-stage stratified sampling design | Cross sectional study | Children under five who attend the health care facilities | High |
| El-Taguri et al. 2009 | Libya | 2003 | N = 7232 0–5 years |
Multistage sampling designs | Cross sectional study | Children under five in five Arab countries (Libya, Djibouti, Syria, Morocco and Yemen | High |
| Morocco | 2003 | N = 5380 0–5 years |
|||||
| El Taguri et al. 2008 | Libya | 1995 | N = 5348 0–5 years |
Multi-stage stratified sampling design | Cross sectional study | Children under five from households across Libya | High |
| Fagbamigbe et al. 2020 | Egypt | 2014 | N = 13,682 0–5 years |
Multi-stage stratified sampling design | Cross sectional study | Children under five in the community | High |
| Figueroa and Kurdi 2019 | Egypt | 2014 | N = 13601 6–59 months |
Multi-stage stratified sampling design | Cross sectional study | Children under five in the community | Medium |
| 2008 | N = 9103 6–59 months |
||||||
| 2005 | 12131 6-59m |
||||||
| Ghattas et al. 2020 | Egypt | 2014 | N = 13,857 6–59 months |
Stratified cluster sampling | Cross sectional study | Children under five in Middle East and North African (MENA) region | High |
| Algeria | 2013 | N = 13,077 6–59 months |
|||||
| Sudan | 2014 | N = 12,538 6–59 months |
|||||
| Morocco | 2003 | N = 5309 6–59 months |
|||||
| Tunisia | 2012 | N = 2593 6–59 months |
|||||
| Kavle et al. 2015 | (Egypt) | 2008 | N = 6091 6–59 months |
Multi-stage stratified sampling design | Cross sectional study | Children under five from households across Egypt | High |
| 2005 | N = 7794 6–59 months |
||||||
| Kerac et al 2019 | Egypt | 2014 | N = 1,210 0–6 months |
Multi-stage stratified sampling design | Cross sectional study | Children less than six months of age in developing countries | High |
| Kiarie et al. 2021 | Sudan Yambio country | 2018 | N = 630 6–59 months |
Cluster multistage sampling method | Cross Sectional study | Children aged 6–59 months living in Yambio County, Sudan | High |
| Mberu et al. 2016 | Egypt (Slum communities) | 2003 | N = 5761 0–5 years |
Multi-stage stratified sampling design | Cross sectional study | Children under five in the community | Medium |
| Musa et al. 2014 | Sudan (Khartoum State) | 2014 | N = 411 0–5 years |
Simple random sampling | Cross sectional study | Children under five in Khartoum state, Sudan | Medium |
| Nikooyeh et al. 2022 | Egypt | 2020 | N = 163 0–5 years |
Online surveys | Cross sectional study | Children under five in Eastern Mediterranean countries | Medium |
| 2015 | N = 258 0–5 years |
||||||
| 2010 | N = 409 0–5 years |
||||||
| 2005 | N = 713 0–5 years |
||||||
| 2000 | N = 1142 0–5 years |
||||||
| Sudan | 2020 | N = 29 0–5 years |
|||||
| 2015 | N = 99 0–5 years |
||||||
| 2010 | N = 266 0–5 years |
||||||
| 2005 | N = 80 0–5 years |
||||||
| 2000 | N = 28 0–5 years |
||||||
| Libya | 2020 | N = 74 0–5 years |
|||||
| 2015 | N = 111 0–5 years |
||||||
| 2010 | N = 225 0–5 years |
||||||
| 2005 | N = 320 0–5 years |
||||||
| 2000 | N = 241 0–5 years |
||||||
| Morocco | 2020 | N = 286 0–5 years |
|||||
| 2015 | N = 347 0–5 years |
||||||
| 2010 | N = 640 0–5 years |
||||||
| 2005 | N = 652 0–5 years |
||||||
| 2000 | N = 679 0–5 years |
||||||
| Tunisia | 2020 | N = 507 0–5 years |
|||||
| 2015 | N = 960 0–5 years |
||||||
| 2010 | N = 1064 0–5 years |
||||||
| 2005 | N = 1212 0–5 years |
||||||
| 2000 | N = 985 0–5 years |
||||||
| Özaltin et al. 2010 | Egypt | 2005–2008 | N = 33440 0–59 months |
Multi-stage stratified sampling design | Cross sectional study | Children under five in Egypt and Morocco | High |
| Morocco | 2003–04 | N = 5544 0–59 months |
|||||
| Rico et al. 2010 | Egypt | 2005 | N = 3242 6–59 months |
Multi-stage stratified sampling design | Cross sectional study | Children under five in the community | High |
| Seedhom et al. 2014 | Egypt (El-Minia) | 2014 | N = 700 6–24 months |
Non-random sampling | Cross sectional study | Children 6–24 months in Minia region, Egypt | Medium |
| Shaker-Berbari et al 2021 | Egypt | 2014 | N = 5100 6–23 months |
Multi-stage stratified sampling design | Cross sectional study | Children under five in the Middle East | High |
| Sudan | 2014 | N = 4009 6–23 months |
|||||
| Sharaf and Rashad 2016 | Egypt | 2014 | N = 12,997 0–5 years |
Multi-stage stratified sampling design | Cross sectional study | Children under five in the community | Medium |
| Sulaiman et al. 2018 | North Sudan (Rural area) | 2014 | N = 1635 0–5 years |
Cluster multistage sampling method | Cross Sectional study | Children under five who live in the Four Nile River rural area of Sudan | High |
| Tzioumis et al. 2016 | Egypt | 2008 | N = 9275 0–5 years |
Multi-stage stratified sampling design | Cross sectional study | Children under five in the community | High |
| 2005 | N = 12038 0–5 years |
||||||
| 2003 | N = 5911 0–5 years |
||||||
| 2000 | N = 10078 0–5 years |
||||||
| 1995 | N = 10165 0–5 years |
||||||
| 1992 | N = 7241 0–5 years |
||||||
| Winskill et al. 2021 | Egypt | 2014 | N = 11,706 0–5 years |
Multi-stage stratified sampling design | Cross sectional study | Children under five in 39 low to middle-income countries | High |
| Zotarelli et al. 2007 | Egypt | 2000 | N = 10194 0–5 years |
Multi-stage stratified sampling design | Cross sectional study | Children under five in the community | High |
High = 7–9; medium = 4–6, and poor = 0–3
Reliability
A second reviewer (MVD) who was blinded to the primary reviewer (NFE), checked the article’s relevance and the recorded details. In each stage, the articles’ appropriateness was checked, with any differences of opinion discussed. A third reviewer (KEA) was available to clarify differences regarding the final publications for inclusion.
Quality assessment
The JBI critical appraisal tool was used to evaluate the degree of reliability, validity, and usefulness of the identified studies and to assess the quality of the reviewed studies. The tool is a set of 9 questions (a checklist) used to evaluate the external validity (bias in selection) and internal validity (information biases and bias of cofounders) [25]. The accuracy, suitability, and confidentiality of the JBI tool for critical appraisal of systematic reviews were confirmed [26]. For each reviewed study, a score ranging from zero to nine was allocated (zero if none of the criteria was met, and nine if all the criteria were met). This sum of points determined the overall quality of the study. Studies were rated as being high quality (7–9), medium (4–6) or poor quality (0–3), as shown in S3 Table.
Statistical methods
The results were imported into STATA version 17 (Stata Corp LLC, Texas, USA) [27]. For each country, the prevalence of undernutrition indicators (stunting, wasting and underweight) was assessed through the forest plot. Each indicator was displayed in the forest plots with its corresponding weight, 95% confidence interval, and overall prevalence in the region.
A heterogeneity test of the different studies showed a high level of inconsistency (I2 > 50%), thereby indicating the use of a random effect model in all the meta-analyses conducted. Sensitivity analysis was also conducted by examining the effect of outliers. We employed a similar method to Patsopoulos et al. [28] which compared the pooled prevalence before and after eliminating one study at a time. The funnel plot was used to report potential bias and small/large study effects, and Begg’s tests were used to assess asymmetry. Their respective funnel plots are shown as S1-S4 Figs.
Results
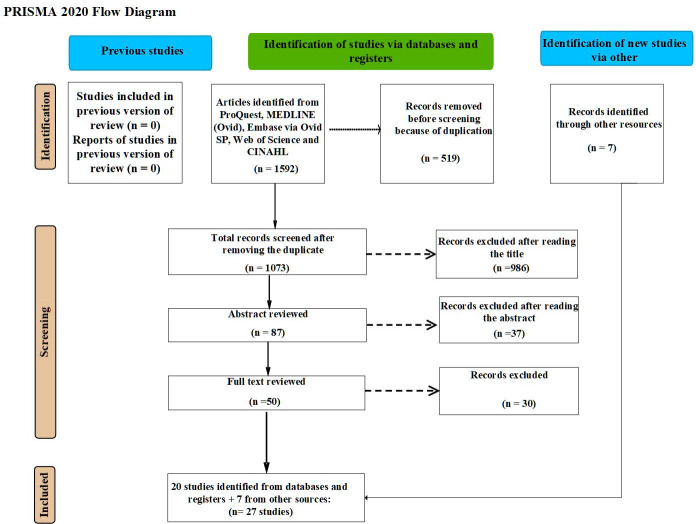
As displayed in Fig 1, a total of 1592 peer-reviewed articles were initially identified from the five databases. After removing 519 duplicates, 1073 articles remained. The screening of the titles in the first screening phase excluded 986 articles. Further screening of the remaining 87 abstracts excluded another 37 articles. In the final phase, the full texts of the remaining 50 articles were screened and a further 30 articles were excluded. During the screening processes seven more papers were identified from Google scholar and other papers [29, 30]. Accordingly, 27 peer-reviewed papers were eligible for critical appraisal.
Fig 1. Flow chart of the study selection process based on PRISMA 2020.
Characteristics of included studies
As shown in Table 1, all 27 studies included in this review were cross-sectional surveys. Eighteen of these studies were investigated in Egypt [30–47], and 10 studies explored the problem in Sudan [32, 35, 38, 42, 48–53]. In addition, 6 studies assessed prevalence of undernutrition in Morocco [32, 35, 38, 39, 54, 55]; 4 studies assessed prevalence of undernutrition in Libya [32, 38, 55, 56], 3 studies demonstrated prevalence of undernutrition in Tunisia [32, 35, 38], and 1 study investigated in Algeria [35]. Six studies were conducted on children aged 6 to 60 months [30, 35, 40, 47, 48, 51], 2 studies investigated children aged 6–24 months [41, 42] and only 1 study investigated children from 0–6 months [36] and the remaining studies focused on children aged 0–60 months [31–34, 37–39, 43–47, 49, 50, 52–56]. Twenty two papers used secondary source data (nationally-representative data) [30–32, 34–40, 42–47, 49, 50, 53–56], and only 5 studies used a primary source data [33, 41, 48, 51, 52). The prevalence of stunting was found in 22 studies [30–33, 35, 37–44, 46, 47, 49, 51–56], prevalence of wasting was found in 18 studies [32–34, 36–39, 41, 42, 45, 46, 48, 49, 51–53, 55, 56] and that of underweight in 12 studies [33, 37, 39, 41, 46, 49–54, 56].
Among the nine JBI criteria used to assess the quality of the studies, 18 (66.7%) articles scored seven points or higher [30, 31, 33–36, 39, 40, 42, 44–46, 49, 50, 51, 53, 55, 56], while 9 (33.3%) papers scored medium between 4 and 6 [32, 37, 38, 41, 43, 47, 48, 52, 54] as seen in S3 Table.
Meta-analysis of the prevalence of undernutrition
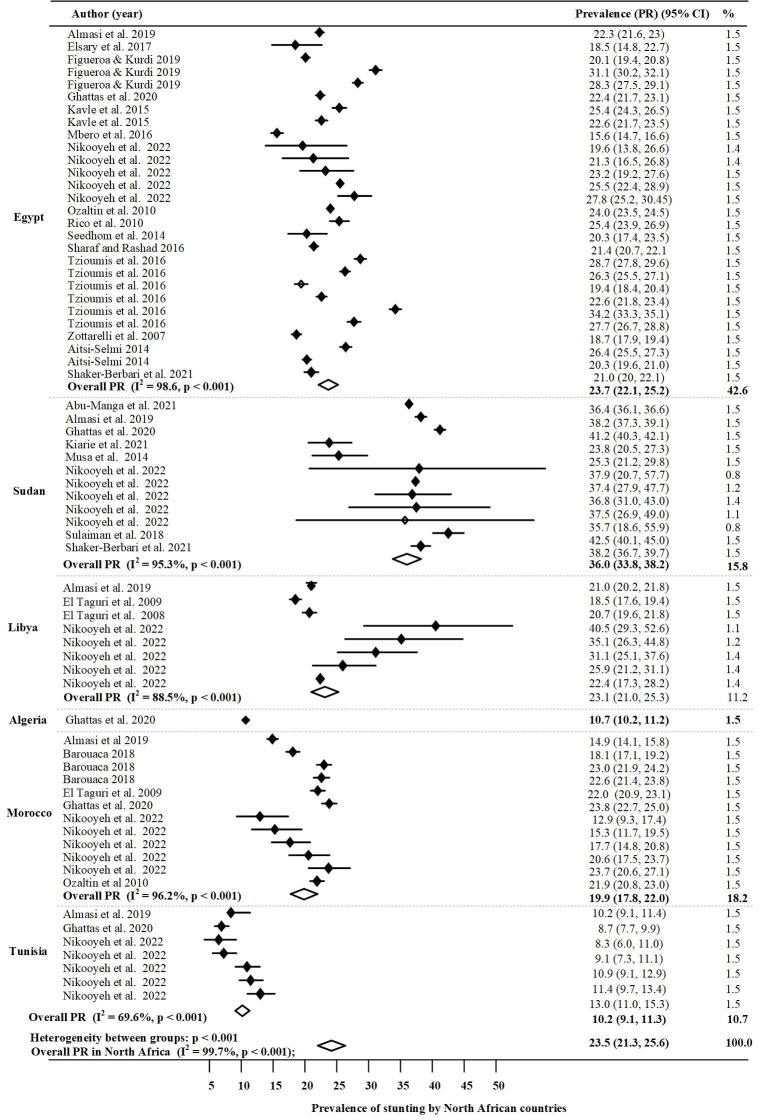
Stunting
A forest plot of the prevalence of stunting among children under five in study is shown in Fig 2. The overall random effect pooled prevalence of stunting was approximately one in five, 23.5% with high heterogeneity (I2 = 99.7%). Funnel plots and the use of Begg’s test for stunting in North Africa indicated homogeneity (S1 Fig), and meta-regression analysis of undernutrition by year of publication indicated that the year of publication increased as the proportion of undernutrition decreased as shown in S4 Fig. However, this relationship did not differ statistically (p = 0.0083). Countries with the highest significant prevalence of stunting in the North Africa region were Sudan 36% (95% CI: 33.8, 38.2; P < 0.001), Egypt 23.7% (95% CI: 22.1, 25.2; P < 0.001), Libya 23.1% (95% CI: 21.0, 25.3; P < 0.001) and Morocco 19.9% (95% CI: 17.8, 22.0; P < 0.001). However, the overall pooled prevalence of stunting was not significant in Algeria 10.7% (95% CI: 10.17, 11.2; P < 0.001) and Tunisia 10.2% (95% CI: 9.1, 11.3; P < 0.001).
Fig 2. Prevalence of stunting in North Africa by country.
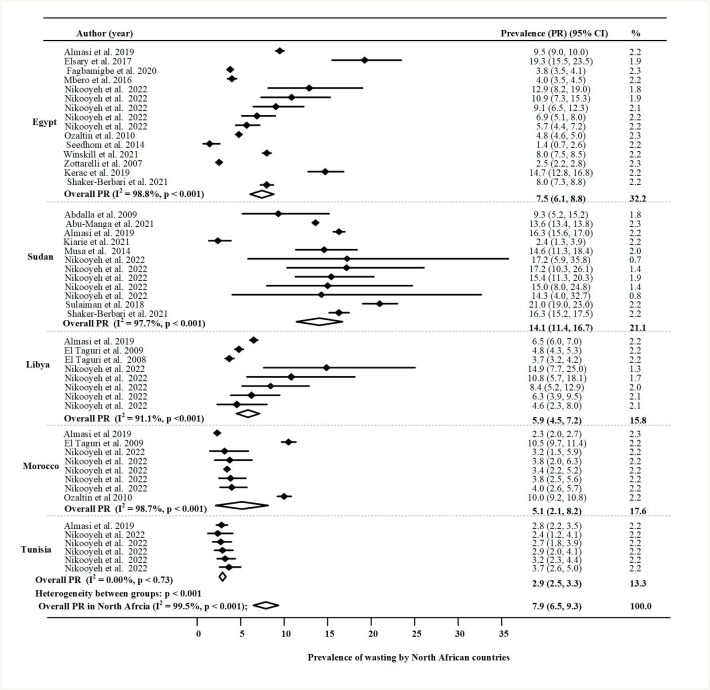
Wasting
Fig 3 presents a forest plot of the prevalence of wasting among children under five in the North African region. The overall random effect pooled prevalence of wasting was 7.9% (95% CI: 6.5, 9.3); p <0.001), with high heterogeneity (I2 = 99.5%). The Funnel plots and use of Begg’s test for wasting shown in S2 Fig reported the absence of publication biases. The highest significant rate of wasting in the region was reported in Sudan 14.1% (95% CI: 11.4,16.7; P < 0.001); and medium rates were found in Egypt 7.5% (95% CI: 6.1, 8.8; P < 0.001), Libya 5.9% (95% CI: 4.5, 7.2; P < 0.001) and Morocco 5.1% (95% CI: 2.1, 8.2; P < 0.001). However, the weighted prevalence in Tunisia was minor at 2.9% (95% CI: 2.5, 3.3; P < 0.001).
Fig 3. Prevalence of wasting in North Africa by country.
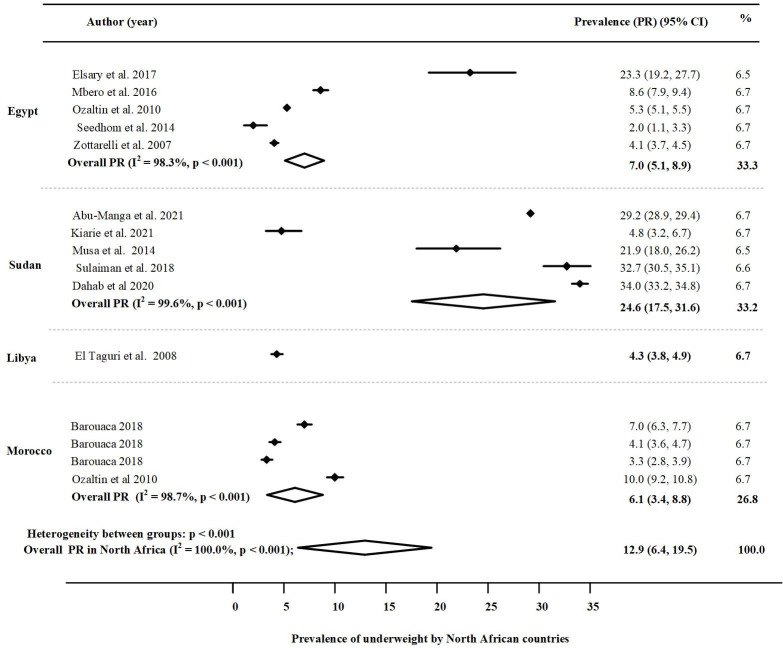
Underweight
The prevalence of underweight among children under five across the North African region, and in the individual countries under study is presented in Fig 4. Accordingly, the overall random effect pooled prevalence of underweight was 12.9% (95% CI:6.4, 19.5); p <0.001), with high heterogeneity (I2 = 100.0%). The highest pooled prevalence of underweight was reported in Sudan 24. 6% (95% CI: 17.5, 31.6; P < 0.001) and the medium weighted rates of underweight were reported in Egypt 7% (95% CI: 5.1, 9.0; P < 0.001), Morocco 6.1% (95% CI: 3.4, 8.8: P < 0.001) and in Libya 4.3% (95% CI: 3.8, 4.9; P < 0.001). However, there was a little evidence of an effect on the prevalence, which implied homogeneity due to limited data. Funnel plots and the use of Begg’s test for underweight, indicated an absence of publication biases, S3 Fig).
Fig 4. Prevalence of underweight in North Africa by country.
Discussion
In the current study, 27 studies within the last 15 years met the eligibility criteria to determine the prevalence of stunting, wasting and underweight in North African children under five years of age. The critical appraisal of the 27 studies ranged from medium (9) to high (18). No studies were appraised as low. The overall prevalence of stunting, wasting and underweight in the current study were 23.5%, 7.9% and 12.9%, respectively.
Accordingly, the overall pooled prevalence of stunting among children under five in North Africa was approximately one in four. This is higher than that the global average of one in five. It is however lower than that of West Africa one in three children have stunting [57]. The review also found that the overall pooled prevalence of wasting among children under five in North Africa was approximately 7.9% which is higher than the global average of 6.7% and higher than the West Africa value of 6.9% [57]. Furthermore, the overall pooled prevalence of underweight among the children under five in North Africa was approximately one in eight. This is higher than the 2020 global average of 12.6% [58], and lower than the WHO 2018 estimate for the Africa region of 17.1% [59].
As described above, the study revealed stunting (chronic undernutrition) and underweight rates in children under five in North African countries were higher than the global average, while wasting was moderate (acute undernutrition). The results are consistent with a study by by Akombi et al [60]. Our results are also consistent with the study of Joulaei et al. [17] that focused on children 2–18 years in Middle East and North African countries, and found high stunting rates among children [17]. Finally, our results agree with the 2021 WHO report which observed that stunting was prevalent and increasing in the North African region [1].
North African countries, similar to other low- and middle-income countries, is experiencing increased malnutrition as a result of conflicts and civil wars, increased food insecurity, displacement, communicable diseases, and a changing climate [61–63]. For example, due to conflicts in Libya, children and families are experiencing inadequate dietary diversity and reduced access to food due to rapid declines in public services, particularly education and health services, as well as higher food and fuel prices, loss of shelter and livelihoods, loss of jobs and income [64]. Similarly, the ongoing crisis in Sudan has been exacerbated by a worsening economic situation, recurring violence throughout many states, a poor harvest, and global price shocks in grains and other food commodities. Children who live in conflict areas are often malnourished due to conflict displacement, infectious diseases, poverty, a decrease in food production, and a lack of essential resources such as food, water, and shelter. Most children aged 6 to 23 months did not consume the Minimum Acceptable Diet daily in Libya [64]. Additionally, families are unable to buy food at the market due to economic deterioration, political instability, and low salaries [65–68]. The effects of climate change are also possible contributors; Sudan and Libya, for example, are among the world’s most water-scarce countries. Water, sanitation, and hygiene (WASH) services and facilities have been severely impacted by conflict, non-renewable water supply, and climate change in these countries [69]. Poverty might also play a role; 29.7% of Egyptians live below the official poverty line in 2019, despite Egypt having the third highest GDP in Africa [70, 71].
In the current study, we also found a significant variation between the prevalence rates of stunting and wasting among the countries with the highest rates, Sudan, and the lowest, Morocco. Sudan had the highest prevalence of underweight, followed by Egypt, Morocco, and Libya. More than one in ten children under five in Algeria and Tunisia had stunted growth. These conclusions align with several other studies. For instance, a study by Akombi et al. [60] on Sub-Saharan African countries found a substantial prevalence of undernutrition in the region, higher within East and West African countries than in South or Central countries in the same region [60].
The previously mentioned observations could be attributed to the concluded variation in the region, which also shows the high prevalence of undernutrition in countries like Sudan and Libya. That are still experiencing violent conflicts or countries like Egypt and Morocco, where conflicts have recently ended, compared with countries that have never experienced conflict or war.
The variation in undernutrition is likely due to high levels of disadvantage, inequality, and food insecurity in the North African region. This is exacerbated by conflict, displacement, and a changing climate. The United Nations Children’s Fund (UNICEF) recently conducted a study of 11 countries in the Middle East and North Africa and found that poverty continues to affect at least 29 million children, or one in four children in this region [72]. Poverty and unemployment rates, which are already high in Algeria, Tunisia, and Libya, are unevenly distributed across age, gender, and geography. Economic inequality is identified as a major obstacle to the global goal of ending global poverty by 2030 [73]. Africa represented the third unequal region after Latin America and Middle East [74]. The inequality may be attributed to economic, governmental, and social structures that limit the equal distribution of medical care, access to food, the impact on dietary intake, and other factors that affect child health directly or indirectly [75]. Poverty, food insecurity and inequality are the roots of undernutrition; these are exacerbated when regional conflicts and other environmental factors increase. For instance, studies from Bangladesh and South Asia found a strong direct, immediate association between higher income inequality and child health. The most vulnerable children suffer the most significant burden of stunting [76, 77]. Furthermore, in 2010, before recent conflicts begun, North African countries were already identified as food security-challenged countries, which faced challenges that prompted them to reconsider their approaches to development [78]. To achieve food security and development, it was suggested that these North African countries need to grow economically, increase employment, manage to sustain water resources, adapt to climate change in a timely manner [78].
Policy implications of the study
Findings from our study may inform governments, policymakers, public health researchers and other stakeholders to identify countries in North Africa whose children are most vulnerable to undernutrition. The current study also serves as a needs assessment indicator for specific countries that report a high prevalence of child undernutrition. Our findings suggest specific policies are needed to address undernutrition within each North African country as an important public health issue. The current review contributes to the evidence for aid organizations and programming to continue allocating resources within North African countries to address undernutrition. This study also provides the latest update on national and international levels of undernutrition which can help determine whether North African countries are making progress towards achieving SDG goals 1, 2 and 3 by 2030.
Strengths and limitations
The main strength of this review is its unique focus of undernutrition in the North African region, specifically in its seven countries of Egypt, Sudan, Libya, Algeria, Tunisia, Morocco, and Western Sahara. Other strengths include the use of uniform standards of measurement from the 2006 WHO standards for child health and the exclusion of studies in clinical settings (e.g., hospitalized children) thereby enhancing the generalizability of results to the general population. The study’s eligibility criteria that evaluated the robustness of the study designs employed in each study was another strength. Nonetheless, this review has a certain number of limitations. Firstly, it was unable to investigate trends in the prevalence of undernutrition indices in the region due to inconsistent data collection and the limited number of studies from some included countries. Secondly, the selection of English-only studies likely biased the results towards studies in countries where the findings are reported in English. Nor did the current review examine the various factors that influence the epidemiology of undernutrition within this region.
Conclusions
Undernutrition is a concern for children under five years of age in North Africa. Considerable variations by country were determined in undernutrition for stunting, wasting and underweight. The North Africa region is at risk of an escalating burden of child undernutrition (particularly in Sudan, Libya, Egypt, and Morocco) due to ongoing conflicts, increased disadvantages and impacts of a changing climate. Public health attention must be paid to this region due to the wide range of inequalities experienced by families and young children living there. This review indicates that ongoing nutrition monitoring and evaluation programs are needed in North African countries to determine and measure progress made by these countries in achieving Sustainable Development Goals (SDGs) 1, 2 and 3 by 2030.
Supporting information
(TIF)
(TIF)
(TIF)
The vertical axis is the log proportion of undernutrition, and the horizontal axis represents the year of publication. Each dark dot represented one selected study, and the size of each dark dot corresponds to the weight assigned to each study. Given the slope of the regression line has descended slightly in this figure, this could be interpreted as the publication of year increased as the proportion of undernutrition decreased but this relationship differs statistically (p = 0.0083).
(TIF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
This paper is a part of the first author’s doctoral dissertation at Western Sydney University’s School of Health Sciences.
Availability of data and other materials
Sample size was not always explicitly stated in studies. The authors; however, direct readers to the name of the national data report or a link for more information. Demographic Health Survey (DHS) reports and databases for each country are available @ dhsprogram.com; information about Multiple Indicator Cluster Surveys (MIC) are available @ mics.unicef.org; and child malnutrition estimates data for 2021 can be found @ UNICEF/WHO/World Bank joint websites.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.United Nations Children’s Fund (UNICEF), World Health Organization, International Bank for Reconstruction and Development/The World Bank. Levels and trends in child malnutrition: key findings of the 2021 edition of the joint child malnutrition estimates. Geneva: World Health Organization; 2021.
- 2.WHO. Fact sheets: malnutrition. In fact sheets: malnutrition [Internet]. 2021 [cited 4 Jan 2023]. https://www.who.int/news-room/fact-sheets/detail/malnutrition.
- 3.WHO Nutrition Landscape Information System (NLiS). Stunting, wasting, overweight and underweight [Internet]. World Health Organization; [cited 4 Jan 2023]. Available from: https://apps.who.int/nutrition/landscape/help.aspx?menu=0&helpid=391&lang=.
- 4.Caulfield LE, de Onis M, Blössner M, Black RE. Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. The American journal of clinical nutrition. 2004;80(1):193–8. doi: 10.1093/ajcn/80.1.193 [DOI] [PubMed] [Google Scholar]
- 5.NSW Ministry of Health. First 2000 days implementation strategy 2020–2025 [Internet]. NSW Goverment. 2021.
- 6.Akseer N, Tasic H, Onah MN, Wigle J, Rajakumar R, Sanchez-Hernandez D, et al. Economic costs of childhood stunting to the private sector in low-and middle-income countries. EClinicalMedicine. 2022;45:101320. doi: 10.1016/j.eclinm.2022.101320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abu-Fatima O, Abbas AA, Racalbuto V, Smith L, Pizzol D. Child undernutrition in Sudan: the social and economic impact and future perspectives. The American Journal of Tropical Medicine and Hygiene. 2021;104(3):1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Union A. The cost of hunger in Africa: Social and economic impact of child undernutrition in Egypt, Ethiopia, Swaziland and Uganda background paper. Abuja, Nigeria. 2014 Mar.
- 9.United Nations. The Sustainable development goals report 2022. United Nations.
- 10.Kim W, Sandler T. Middle East and North Africa: terrorism and conflicts. Global Policy. 2020;11(4):424–38. [Google Scholar]
- 11.Rabeh RB, Missaoui N, Mazigh S, Atiattalah S, Yahyaoui S, Boukthir S. 268 Assessment of nutritional status in hospitalized children in Tunisian tertiary referral pediatric hospital. BMJ Publishing Group Ltd; 2021. [Google Scholar]
- 12.Abdelaziz SB, Youssef MRL, Sedrak AS, Labib JR. Nutritional status and dietary habits of school children in Beni-Suef Governorate, Egypt. Food and Nutrition Sciences. 2015;6(01):54. [Google Scholar]
- 13.Kanan SO, Abd Elmoneim OE. Prevalence and causes of undernutrition among underfive Sudanese Cchildren: A mini-review. Journal of Advances in Medicine and Medical Research. 2020;32(15):12–20. [Google Scholar]
- 14.Bouziane Nedjadi K, Hamous A, Hadjkadi A, Dida N, Benadouda S, Boureghda I, et al. Frequency of Malnutrition (Undernutrition, Overweight/Obesity) and Prevalence of Iron Deficiency in Western Algeria Infants. 2018. [Google Scholar]
- 15.Ahami A, Fadel H, Azzaoui F-Z. Anthropometric measurements of school children in North-Eastern Morocco. International Research Journal of Public and Environmental Health. 2020;7(4):100–4. [Google Scholar]
- 16.Grijalva-Eternod CS, Wells JC, Cortina-Borja M, Salse-Ubach N, Tondeur MC, Dolan C, et al. The double burden of obesity and malnutrition in a protracted emergency setting: a cross-sectional study of Western Sahara refugees. PLoS Med. 2012;9(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joulaei H, Keshani P, Ashourpour M, Bemani P, Amiri S, Rahimi J, et al. The prevalence of stunting among children and adolescents living in the Middle East and North Africa region (MENA): A systematic review and meta-analysis. Journal of global health. 2021;11. doi: 10.7189/jogh.11.04070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Shameri EA, Al-Shahethi AH, Wafa SW. Nutritional status and its determinants in the Eastern Mediterranean region. A review. Saudi Med J. 2022;43(4):423–7. doi: 10.15537/smj.2022.43.4.20210676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scott N, Delport D, Hainsworth S, Pearson R, Morgan C, Huang S, et al. Ending malnutrition in all its forms requires scaling up proven nutrition interventions and much more: a 129-country analysis. BMC medicine. 2020;18(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fanzo J. Food policies’ roles on nutrition goals and outcomes: connecting of food and public health systems. In international food law and policy; Springer: Berlin/Heidelberg, Germany, 2016; pp. 213–251. [Google Scholar]
- 21.World Health Organization. Developing nutrition guidelines [Internet]. World Health Organization; [cited 4 Jan 2023]. Available from: https://www.who.int/activities/developing-nutrition-guidelines.
- 22.De Onis M. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: WHO; 2006.
- 23.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. Journal of clinical epidemiology. 2021;134:103–12. doi: 10.1016/j.jclinepi.2021.02.003 [DOI] [PubMed] [Google Scholar]
- 24.EndNote. The best reference management tool [Internet]. EndNote. 2022 [cited4 Jan 2023]. Available from: https://endnote.com/
- 25.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. International journal of evidence-based healthcare. 2015;13(3):147–53. doi: 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 26.Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI evidence synthesis. 2020;18(10):2127–33. doi: 10.11124/JBISRIR-D-19-00099 [DOI] [PubMed] [Google Scholar]
- 27.StataCorp. Stata statistical software: Release 17. College Station. TX: StataCorp LLC. 2021.
- 28.Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. International journal of epidemiology. 2008;37(5):1148–57. doi: 10.1093/ije/dyn065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Onis M, Blössner M, Borghi E. Prevalence and trends of stunting among pre-school children, 1990–2020. Public health nutrition. 2012;15:142–8. doi: 10.1017/S1368980011001315 [DOI] [PubMed] [Google Scholar]
- 30.Kavle JA, El-Zanaty F, Landry M, Galloway R. The rise in stunting in relation to avian influenza and food consumption patterns in Lower Egypt in comparison to Upper Egypt: results from 2005 and 2008 Demographic and Health Surveys. BMC public health. 2015;15(1):1–18. doi: 10.1186/s12889-015-1627-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aitsi-Selmi A. Households with a Stunted Child and Obese Mother: Trends and Child Feeding Practices in a Middle-Income Country, 1992–2008. Matern Child Health. 2014; 19:1284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Almasi A, Saeidi S, Zanganeh A, Ziapour A, Choobtashan M, Saeidi F, et al. Investigation of some factors affecting stunting and wasting among the under-five children in eastern Mediterranean region. International Journal of Pediatrics. 2019;7(7):9759–72. [Google Scholar]
- 33.Elsary AY, Abd El-moktader AM, Alkassem Elgameel W, Mohammed S, Masoud M, Abd El-Haleem NG. Nutritional survey among under five children at Tamyia district in Fayoum, Egypt. International Journal of Community Medicine and Public Health. 2017;4(6):1813. [Google Scholar]
- 34.Fagbamigbe AF, Kandala N-B, Uthman OA. Correction: Mind the gap: What explains the poor-non-poor inequalities in severe wasting among under-five children in low-and middle-income countries? Compositional and structural characteristics. Plos one. 2021;16(6):e0253831. doi: 10.1371/journal.pone.0253831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ghattas H, Acharya Y, Jamaluddine Z, Assi M, El Asmar K, Jones AD. Child‐level double burden of malnutrition in the MENA and LAC regions: Prevalence and social determinants. Maternal & child nutrition. 2020;16(2):e12923. doi: 10.1111/mcn.12923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kerac M, Frison S, Connell N, Page B, McGrath M. Informing the management of acute malnutrition in infants aged under 6 months (MAMI): risk factor analysis using nationally-representative demographic & health survey secondary data. PeerJ. 2019;6:e5848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mberu BU, Haregu TN, Kyobutungi C, Ezeh AC. Health and health-related indicators in slum, rural, and urban communities: a comparative analysis. Global health action. 2016;9(1):33163. doi: 10.3402/gha.v9.33163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nikooyeh B, Ghodsi D, Amini M, Rasekhi H, Rabiei S, Doustmohammadian A, et al. The Analysis of Trends of Preschool Child Stunting, Wasting and Overweight in the Eastern Mediterranean Region: Still More Effort Needed to Reach Global Targets 2025. Journal of Tropical Pediatrics. 2022;68(3):fmac028. doi: 10.1093/tropej/fmac028 [DOI] [PubMed] [Google Scholar]
- 39.Özaltin E, Hill K, Subramanian S. Association of maternal stature with offspring mortality, underweight, and stunting in low-to middle-income countries. Jama. 2010;303(15):1507–16. doi: 10.1001/jama.2010.450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rico E, Fenn B, Abramsky T, Watts C. Associations between maternal experiences of intimate partner violence and child nutrition and mortality: findings from Demographic and Health Surveys in Egypt, Honduras, Kenya, Malawi and Rwanda. Journal of epidemiology & community health. 2011;65(4):360–7. doi: 10.1136/jech.2008.081810 [DOI] [PubMed] [Google Scholar]
- 41.Seedhom AE, Mohamed ES, Mahfouz EM. Determinants of stunting among preschool children, Minia, Egypt. International Public Health Forum [Internet]. 2014; 1(2):[6–9 pp.]. [Google Scholar]
- 42.Shaker-Berbari L, Qahoush Tyler V, Akik C, Jamaluddine Z, Ghattas H. Predictors of complementary feeding practices among children aged 6–23 months in five countries in the Middle East and North Africa region. Maternal & child nutrition. 2021;17(4):e13223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sharaf MF, Rashad AS. Regional inequalities in child malnutrition in Egypt, Jordan, and Yemen: a Blinder-Oaxaca decomposition analysis. Health economics review. 2016;6(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tzioumis E, Kay MC, Bentley ME, Adair LS. Prevalence and trends in the childhood dual burden of malnutrition in low-and middle-income countries, 1990–2012. Public health nutrition. 2016;19(8):1375–88. doi: 10.1017/S1368980016000276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Winskill P, Hogan AB, Thwing J, Mwandigha L, Walker PG, Lambert B. Health inequities and clustering of fever, acute respiratory infection, diarrhoea and wasting in children under five in low-and middle-income countries: a Demographic and Health Surveys analysis. BMC medicine. 2021;19(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zottarelli LK, Sunil TS, Rajaram S. Influence of parental and socioeconomic factors on stunting in children under 5 years in Egypt. Eastern Mediterranean Health Journal. 2007;13(6):1330–42. doi: 10.26719/2007.13.6.1330 [DOI] [PubMed] [Google Scholar]
- 47.Figueroa JL, Kurdi S. Ex post adjustment for measurement error in stunting calculations: an illustration from Egypt. Public health nutrition. 2020;23(5):776–81. doi: 10.1017/S1368980019003100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Abdalla MA, Sulieman SA, El Tinay AH, Khattab AGH. Socio-economic aspects influencing food consumption patterns among children under age of five in rural area of Sudan. Pakistan Journal of Nutrition. 2009;8(5):653–9. [Google Scholar]
- 49.Abu-Manga M, Al-Jawaldeh A, Qureshi AB, Ali AME, Pizzol D, Dureab F. Nutrition assessment of under-five children in sudan: Tracking the achievement of the global nutrition targets. Children. 2021;8(5):363. doi: 10.3390/children8050363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dahab R, Bécares L, Brown M. Armed conflict as a determinant of children malnourishment: a cross-sectional study in The Sudan. BMC public health. 2020;20(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kiarie J, Karanja S, Busiri J, Mukami D, Kiilu C. The prevalence and associated factors of undernutrition among under-five children in South Sudan using the standardized monitoring and assessment of relief and transitions (SMART) methodology. BMC NUTRITION. 2021;7(1). doi: 10.1186/s40795-021-00425-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Musa TH, Musa HH, Ali EA, Musa NE. Prevalence of malnutrition among children under five years old in Khartoum State, Sudan. Polish Annals of Medicine. 2014;21(1):1–7. [Google Scholar]
- 53.Sulaiman AA, Bushara SO, Elmadhoun WM, Noor SK, Abdelkarim M, Aldeen IN, et al. Prevalence and determinants of undernutrition among children under 5-year-old in rural areas: A cross-sectional survey in North Sudan. Journal of family medicine and primary care. 2018;7(1):104–10. doi: 10.4103/jfmpc.jfmpc_73_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Barouaca H. Situation of malnutrition in Morocco: Results after 40 years of struggle. Nutr Clin Diet Hosp. 2012;32:76–81. [Google Scholar]
- 55.El Taguri A, Besmar F, Abdel Monem A, Betilmal I, Ricour C, Rolland Cachera M. Stunting is a major risk factor for overweight: results from national surveys in 5 Arab countries. Eastern Mediterranean Health Journal. 2009;15(3):549–62. [PubMed] [Google Scholar]
- 56.El Taguri A, Rolland-Cachera MF, Mahmud SM, Elmrzougi N, Abdel Monem A, Betilmal I, et al. Nutritional Status Of Under-Five Children In Libya; A National Population-Based Survey. LIBYAN JOURNAL OF MEDICINE. 2008;3(1):13–9. doi: 10.4176/071006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Global Nutrition Report. Country Nutrition Profiles. West Africa. The burden of malnutrition at a glance. [Available from: https://globalnutritionreport.org/resources/nutrition-profiles/africa/western-africa/.
- 58.The World Bank. Prevalence of underweight, weight for age (% of children under 5) [Available from: https://data.worldbank.org/indicator/SH.STA.MALN.ZS.
- 59.Development Education.ie. Factsheet: Child under-nutrition in Africa [Available from: https://developmenteducation.ie/feature/factsheet-child-under-nutrition-in-africa/.
- 60.Akombi BJ, Agho KE, Merom D, Renzaho AM, Hall JJ. Child malnutrition in sub-Saharan Africa: A meta-analysis of demographic and health surveys (2006–2016). PloS one. 2017;12(5):e0177338. doi: 10.1371/journal.pone.0177338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Malley R. 10 conflicts to watch in 2021 [Internet]. International Crisis Group. 2022 [cited 4 Jan 2023]. Available from: https://www.crisisgroup.org/global/10-conflicts-watch-2021
- 62.Cho R, How climate change impacts the economy [Internet]. State of the Planet. 2019. [cited 4 Jan 2023]. Available from: https://news.climate.columbia.edu/2019/06/20/climate-change-economy-impacts/ [Google Scholar]
- 63.UNICEF for every child. Childhood diseases [Internet]. UNICEF. 2022 [cited 4 Jan 2023]. Available from: https://www.unicef.org/health/childhood-diseases
- 64.Where we work: Libya [Internet]. World Food Programme: Saving lives changing lives. 2022 [cited 4 Jan 2023]. Available from: https://docs.wfp.org/api/documents/wfp-0000114546/download/
- 65.Fore H. Libya: Tens of thousands of children at risk amidst violence and chaos of unrelenting conflict [Internet]. UNICEF for every child. 2020. Jan [cited 1 Dec 2022]. Available from: https://www.unicef.org/press-releases/libya-tens-thousands-children-risk-amidst-violence-and-chaos-unrelenting-conflict. [Google Scholar]
- 66.Amusan L. Libya’s Implosion and its Impacts on Children. Journal of international Women’s studies. 2013;14(5):66–79. [Google Scholar]
- 67.O’hare BA, Southall DP. First do no harm: the impact of recent armed conflict on maternal and child health in Sub-Saharan Africa. Journal of the Royal Society of Medicine. 2007;100(12):564–70. doi: 10.1177/0141076807100012015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dureab F, Al-Falahi E, Ismail O, Al-Marhali L, Al Jawaldeh A, Nuri NN, et al. An overview on acute malnutrition and food insecurity among children during the conflict in Yemen. Children. 2019;6(6):77. doi: 10.3390/children6060077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.UNICEF. Water, sanitation and hygiene (WASH) [Internet]. UNICEF. 2023 [cited 4 Jan 2023]. Available from: https://www.unicef.org/wash
- 70.Kamer L. Africa: GDP by country 2021 [Internet]. Statista. 2022 [cited 4 Jan 2023]. Available from: https://www.statista.com/statistics/1120999/gdp-of-african-countries-by-country/
- 71.Genoni ME. Poverty & Equity Brief Arab Republic of Egypt Middle East & North Africa. 2022.
- 72.UNICEF for every child. At least one in four children live in poverty in the Middle East and North Africa [Internet]. UNICEF for every child; 2017 May [cited 1 Jan 2022]. Available from: https://www.unicef.org/press-releases/least-one-four-children-live-poverty-middle-east-and-north-africa#:~:text=Press%20release.
- 73.World Bank Group. Poverty has fallen in the Maghreb, but inequality persists [Internet]. World Bank. World Bank Group; 2016 [cited 4 Jan 2023]. Available from: https://www.worldbank.org/en/news/feature/2016/10/17/poverty-has-fallen-in-the-maghreb-but-inequality-persists
- 74.WID World. Global inequality data 2020 update. World inequality database [Internet]. WID. 2020 [cited 4 Jan 2023]. Available from: https://wid.world/news-article/2020-regional-updates/#:~:text=The%20World%20Inequality%20Lab%20releases,over%20time%2C%20countries%20and%20regions. .
- 75.Perez-Escamilla R, Bermudez O, Buccini GS, Kumanyika S, Lutter CK, Monsivais P, et al. Nutrition disparities and the global burden of malnutrition. Bmj. 2018;361. doi: 10.1136/bmj.k2252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Krishna A, Mejía‐Guevara I, McGovern M, Aguayo VM, Subramanian S. Trends in inequalities in child stunting in South Asia. Maternal & child nutrition. 2018;14:e12517. doi: 10.1111/mcn.12517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hong R, Banta JE, Betancourt JA. Relationship between household wealth inequality and chronic childhood under-nutrition in Bangladesh. International journal for equity in health. 2006;5(1):1–10. doi: 10.1186/1475-9276-5-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Breisinger C, Van Rheenen T, Ringler C, Pratt AN, Minot N, Aragon C, et al. Food security and economic development in the Middle East and North Africa. Current State and Future Perspective IFPRI Discussion Paper. 2010;985. [Google Scholar]