Abstract
From January 2020 to December 2022, there was a total of 8,872,955 confirmed COVID-19 cases in Taiwan. In addition, a total of 15,253 COVID-19 related deaths were reported. During these three years, the government and health authority did many efforts to response this pandemic. In the early pandemic, Taiwan Central Epidemic Command Center was established in the early 2020 to organize associated resource, develop effective policy and implement strict intervention. In response to COVID-19 pandemic, many infection control policy and interventions, including universal mask wearing with increasing production of face mask, hand hygiene, border control, introduce of digital technology incorporating big data, quarantine of COVID-19 cases, travel and gathering restriction, were implemented. In the meanwhile, two COVID-19 vaccines, namely MVC-COV1901 and UB-612, have been developed under the support of government. Furthermore, MVC-COV1901 was taken into clinical practice after received emergency use approval. In addition, two traditional Chinese medicines, including NRICM101 and NRICM102 showed their promising effect against SARS-CoV-2 infection and were recommended as potential therapeutic options for COVID-19. During the pandemic, the nonpharmacologic intervention help reduce many infectious diseases, especially for airborne/droplet-transmitted diseases. However, COVID-19 exhibited some adverse impacts on the healthcare systems, such as emergency medical service on out of hospital cardiac arrest, cancer screening, HIV screening and prevention services, and public health, namely the psychosocial status of healthcare workers. Although the outbreak of SARS-CoV-2 infections may gradually subsided, we should keep monitoring its associated impact and appropriately response to this pandemic.
Keywords: COVID-19, Taiwan, SARS-CoV-2, Omicron, Vaccines
Introduction
In December 2019, a cluster of patients with pneumonia caused by a novel coronavirus - severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) occurred in Wuhan, China.1 Thereafter, this infectious disease rapidly spread to the whole world and has been declared as coronavirus disease 2019 (COVID-19) pandemic by World Health Organization (WHO) on 11 March 2020.2 , 3 To date, there have been more than 757 million confirmed cases of COVID-19, including more than six million deaths, reported to WHO.4 To fight COVID-19 pandemic, the world brought together governments, scientists, and global health organizations to develop and implement strategies and tools for COVID-19 mitigation. There is no exception for Taiwan. In this article, we present how Taiwan responded to COVID-19 and how COVID-19 affected Taiwan during these three years.
Epidemiology
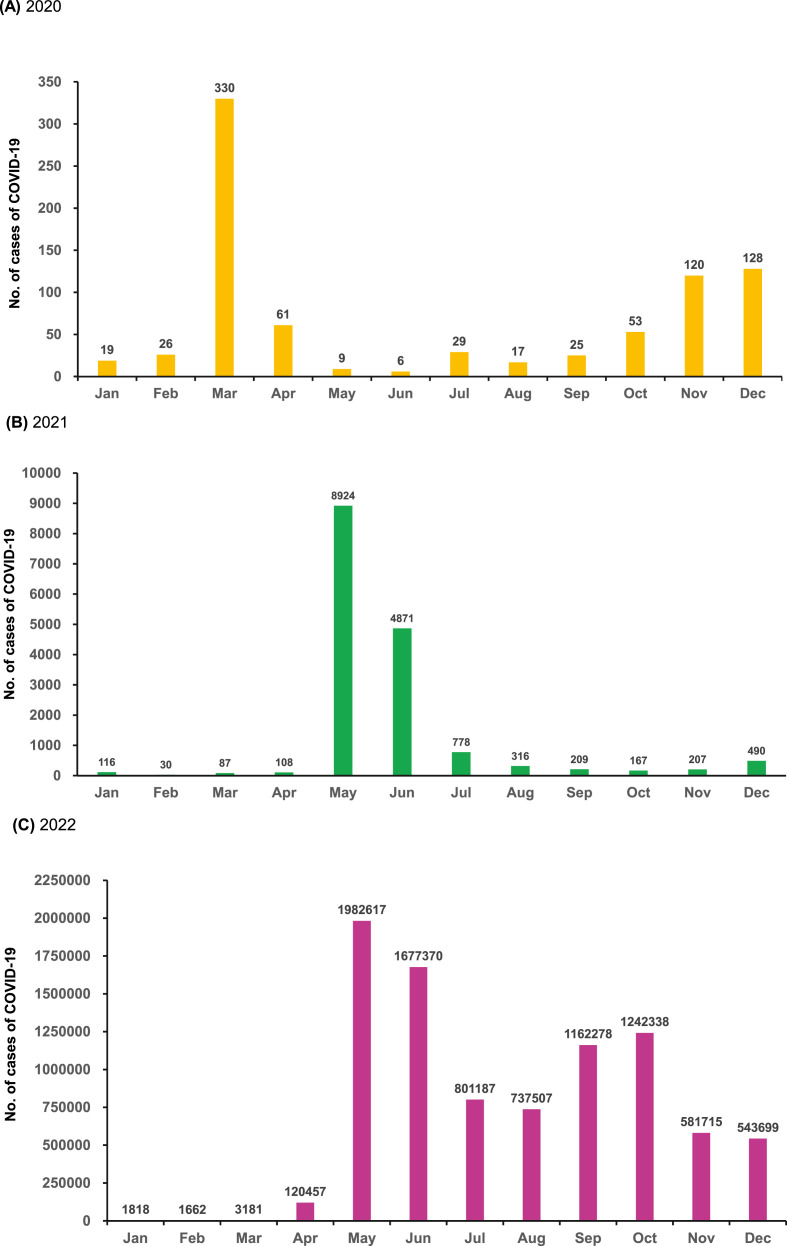
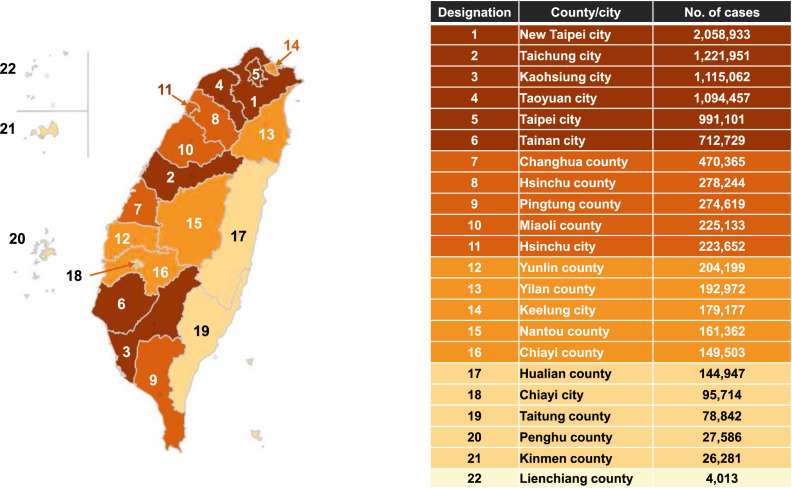
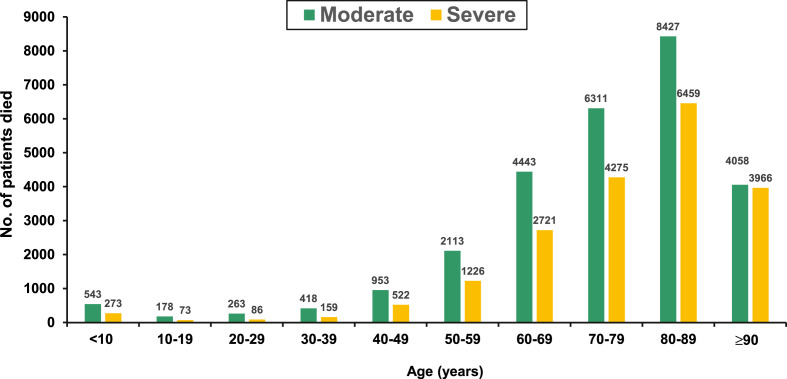
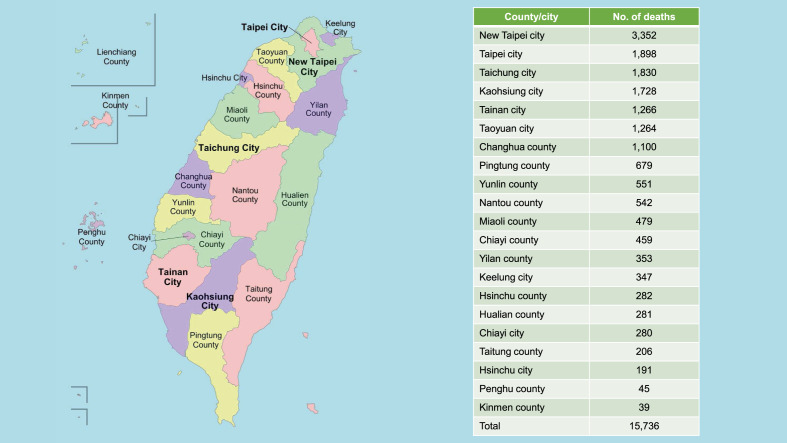
SARS-CoV-2 was confirmed to have spread to Taiwan on 21 January 2020, with the first case being a 50-year-old woman who had been teaching in Wuhan, China and one week later, the first locally-transmitted COVID-19 case was identified in a 50-year-old husband, who got infection from his wife.5 In 2020, the number of active cases in this first wave peaked on 6 April 2020 at 307 cases. Overall, 823 confirmed COVID-19 cases, including a total of nine deaths were reported to Taiwan CDC in 2020 (Fig. 1 A).6 , 7 However, an outbreak among Taiwanese crew members of the state-owned China Airlines in late April 2021 led to a sharp surge in cases, mainly in the Greater Taipei area.6 This surge caused a total of 8,924 and 4,871 COVID-19 cases in May and June, respectively. Until June 21, 2021, the daily new case numbers dropped below 100 for the first time since this outbreak. On 17 July, the number of new domestic cases dropped to single digits, with eight new domestic cases, for the first time since mid-May. Finally, there was a total of 16,303 confirmed cases, including 842 deaths in 2021 (Fig. 1B).6 Although no domestic case was found in the end of 2021, a new surge causing by omicron variant developed since January 2022. In the meanwhile, the distribution system of at-home COVID-19 rapid test kits were implemented on April 28, 2022. Thereafter, the monthly case number increased and peaked at May (n = 1,982,617). Overall, there was a total of 9,167,811 cases, including 15,755 deaths in 2022 (Fig. 1C). As of February 23, 2023, a total of 9,985,320 cases, including 9,930,554 domestic case (Fig. 2 ) and 80,737 imported cases have been reported to Taiwan CDC.6 Among them, 99.52% were reported as mild disease or asymptomatic cases and moderate and severe cases only comprised 0.28% and 0.20%, respectively. In addition, there were a total of 17,709 deaths, and most of them developed in patients with moderate-to-severe COVID-19 (Fig. 3 ). Among 17,172 domestic cases related deaths, new Taipei city had the most deaths (n = 3,352), followed by Taipei city (n = 1,898), Taichung city (n = 1,830) and Kaohsiung city (n = 1,728) (Fig. 4 ).6
Figure 1.
The monthly case number of new COVID-19 in 2020 (A), 2021 (B) and 2022 (C).
Figure 2.
Distribution of domestic case from 2020 to January 13, 2022. Data obtained from Taiwan Centers for Diseases Control (https://www.cdc.gov.tw) as of February 23, 2023.
Figure 3.
Number of deaths among patients with moderate and severe COVID-19 according to different age groups.
Figure 4.
Distribution of deaths of domestic cases of COVID-19 from January 1st 2020 to February 14th, 2023.
How Taiwan responses to COVID-19
Nonpharmacologic interventions
To prevent and control the SARS-CoV-2 outbreak, Taiwan Central Epidemic Command Center (CECC) was soon established in the early 2020 to organize associated resource, develop effective policy and implement strict intervention.7, 8, 9 CECC promptly initiated stepwise border control for major cities and provinces in China, European and American countries, and eventually expanded it to the whole world in March 2020. This early response combining with stringent quarantine measures successfully blocked the first wave of imported cases, and slowed down subsequent large local outbreaks.8 In addition, the introduce of digital technologies including comprehensive contact tracing for confirmed cases, digital fencing, and government database linkage were adopted to facilitate the application of public health interventions and data collection.10, 11, 12 In the meanwhile, several measures including quarantine of suspicious cases, holiday extension, travel restriction were implemented.9 Even more, the government decided to prohibit the export of surgical masks to make sure masks were not too short and started to manufacture masks. Through this policy and intervention with dispensing services of surgical masks within community pharmacies, the healthcare authority can provide adequate N95 respirators and face masks for the health care professionals and the general public in Taiwan and for other countries in need.11
To interrupt the community-hospital-community transmission cycle, enhanced Traffic Control Bundling (eTCB) was proposed to include expanding the TCB transition zone - the quarantine ward, which housed patients exhibiting atypical manifestations or awaiting definitive diagnosis.13 A second adaptation involves enhancing the checkpoint hand disinfection and gowning up with Personal Protective Equipment deployed in traditional TCB. Under eTCB, checkpoint hand disinfection and donning of face masks are now required of all visitors who seek to enter hospitals.13
Within healthcare system, each hospital developed many infection control policy and implemented preventive measures to mitigate the in-hospital outbreak of COVID-19 according to the recommendation of CECC and its own setting.14, 15, 16, 17, 18, 19, 20, 21 Because the residents in long-term care facility were vulnerable to SARS-CoV-2 infection,22 eTCB was adopted, particularly by incorporating compartmentalization within zones plus active surveillance and implemented as a means of protecting LTCF residents and staff.23
Vaccine development
Vaccine is an important tool to prevent the spread and progress of COVID-19, however, the initial supply of vaccine cannot meet the large demand in Taiwan.24 Therefore, two kinds of COVID-19 vaccines - MVC-COV1901 and UB-612 have been developed under the support of Taiwan's government. MVC-COV1901 is a subunit SARS-CoV-2 vaccine based on stabilized spike protein adjuvanted with CpG 1018 and aluminum hydroxide that has received emergency use approval (EUA) for adults in Taiwan.25 Phase 2 randomized controlled trials had confirmed the safety and immunogenicity of two doses of MVC-COV1901 in adolescents, adults and older adults in Taiwan.25, 26, 27 The interim analysis of a phase 3, randomized, double-blind, active-controlled trial in Paraguay also showed that when compared against AZD1222, MVC-COV1901 exhibited superiority in terms of neutralizing antibody titers and non-inferiority in terms of seroconversion rates.28
UB-612 is a novel subunit protein-peptide COVID-19 vaccine, which composed of: (i) receptor binding domain of SARS-CoV-2 spike protein fused to a modified single-chain human IgG1 Fc; (ii) five synthetic peptides incorporating conserved helper and cytotoxic T lymphocyte epitopes derived from SARS-CoV-2 structural proteins; and (iii) aluminum phosphate as adjuvant.29 RCTs showed that a favorable safety profile, potent booster effect against variant of concerns (VOCs) including Delta and Omicron, and long-lasting B and broad T cell immunity.30 , 31
Traditional Chinese medicine (TCM)
Traditional medicine is practiced in many societies and offers a rich reservoir of safe-to-use drug candidates and experiences in dealing with endemics over a long period of time.32 In Taiwan, the “Traditional Chinese Medicine Clinical Guideline for COVID-19” suggested integrated treatment of mild-to-moderate and severe-to-critical cases with TCM formulae NRICM101 and NRICM102, respectively.33 Taiwan Chingguan Yihau (NRICM101), a TCM designed based on a medicinal formula with a long history of almost 500 years and obtained an Emergency Use Authorization in Taiwan. A bedside-to-bench study using pharmacological assays demonstrated that NRICM101 was effective in inhibiting the spike protein/ACE2 interaction, 3CL protease activity, viral plaque formation, and production of cytokines interleukin (IL)-6 and tumor necrosis factor (TNF)-α.34 In addition, NRICM101 has multiple functions that may affect cytokine regulation to prevent human lung cell injury.35 Similarly, NRICM102 was found to disrupt spike protein/ACE2 interaction, 3CL protease activity, reduce activation of neutrophils, monocytes and expression of cytokines (TNF-α, IL-1β, IL-6, IL-8), chemokines (MCP-1, MIP-1, RANTES) and proinflammatory receptor (TLR4).36 NRICM102 also inhibited the spread of virus and progression to embolic and fibrotic pulmonary injury through reducing prothrombotic (vWF, PAI-1, NET) and fibrotic (c-Kit, SCF) factors, and reducing alveolar type I (AT1) and type II (AT2) cell apoptosis.36 Further multicenter retrospective study demonstrated that both NRICM101 and NRICM102 were significantly associated with a lower risk of intubation/ICU admission or death among patients with mild-to-severe COVID-19.33
How COVID-19 affects Taiwan
Collateral effect on other infectious diseases
Since the outbreak of COVID-19, many non-pharmacologic interventions (NPIs) have been developed for the prevention of SARS-CoV-2 spread. The implementation of NPIs not only help mitigate COVID-19, but also control other infectious diseases in Taiwan.37 , 38 During early pandemic, Kuo et al. found that nationwide surveillance data revealed drastic decreases in influenza diagnoses in outpatient departments, positivity rates of clinical specimens, and confirmed severe cases during the first 12 weeks of 2020 compared with the same period of 2019.39 Furthermore, using the open database from Taiwan CDC, Lai et al. showed that the number of notifiable infectious diseases (NIDs) cases was 21,895 between January and September 2020, which was lower than the number of cases during the same period in 2019 (n = 24,469), with a decline in incidence from 102.9 to 91.7 per 100,000 people in 2019 and 2020.37 Regarding airborne/droplet-transmitted NIDs, the number of cases of 14 diseases including measles, rubella, pertussis, influenza with severe complications, invasive pneumococcal disease, Q fever, mumps, meningococcal meningitis, varicella, legionellosis, invasive Haemophilus influenzae type b infection, hantavirus syndrome, tuberculosis (TB), and multidrug-resistant TB (MDRTB) decreased from 10,631 in 2019–7636 in 2020, with a reduction of 28.2%.38 Even more, 11 fecal-oral, seven vector-borne, and four direct-contact transmitted NID also had an overall reduction of 156 (−23.0%), 557 (−54.8%), and 73 (−45.9%) cases, respectively, from 2019 to 2020 and the changes in incidence 6.7 (−23.4%), 2.4 (−55.0%), and 0.3 (−46.2%) per 100,000 people for fecal-oral, vector-borne, and direct-contact transmitted NID, respectively.37 These collateral benefit of NPIs on NIDs persisted till 2021.40 In contrast to most NIDs with decreasing trend during pandemic, the case of gonorrhea had significantly increased.37 , 41 All these findings suggest the importance of the continue surveillance of these NIDs during the COVID-19 pandemic, especially while the NPIs are gradually relaxed.
Healthcare utility
Healthcare was the most affected system during the pandemic, and the utilization of related services for many diseases fell dramatically due to voluntary behaviors or enforced measures since the COVID-19 outbreak. In Taiwan, Tsai et al. used a county-by-week-level dataset from Taiwan's National Health Insurance to measure healthcare utilization during the COVID-19 pandemic.42 They found that people voluntarily reduced their demand for healthcare, due to fears of contagion, or COVID-related precautionary behaviors, even if there were no human mobility restrictions or supply-side constraints.42 Overall, the number of outpatient visits and inpatient hospitalization decreased by 19% and 10%, respectively, during the pandemic period (February to May 2020). In addition, the demand response of healthcare for Influenza-like illness (ILI) was much greater and more persistent than for non-ILI. Even more, the demand for healthcare services did not return to the pre-pandemic period, even when there were no local coronavirus cases for more than 250 consecutive days (mid-April to December 2020).42
Similarly, Tan et al. found that the overall emergency department (ED) visits were 122,542 during this period in 2021, which was much lower than those in the lunar new year in Taiwan from 2017 to 2020 (the average was 174,653)43 Additionally, the ED visits for ILI were 9816 during this period in 2021, which was much lower than those in the same period from 2017 to 2020 (the average was 34,347). Even more, the ED visits for acute diarrhea illness was 10,447 during this period in 2021, which was also lower than those in the same period in the prior four years (the average was 13,785).43 Lin et al. reported the same findings using a multicenter retrospective study collected data from three regional hospitals between March 2019 and December 2020.44 Overall, there was a 16%–23% reduction in ED patient volume, especially in non-trauma adult visits and pediatric visits, and ED visits in both high and low severity levels decreased in these regional hospitals.44
Moreover, emergency medical service on out of hospital cardiac arrest (OHCA) in Taiwan was affected by COVID-19. A retrospective observational study observed that the EMS response time was longer during the COVID-19 pandemic (445.8 ± 210.2 s in 2020 vs 389.7 ± 201.8 s in 2019, p < 0.001). The rate of prehospital return of spontaneous circulation was lower in 2020 (6.49% vs 2.57%, p = 0.001) and significantly fewer cases had favorable neurological function in 2020 (4.21% vs 2.09%, p = 0.035).45 Another study focusing pediatric patients showed children with OHCA had a significantly lower rate of sustained return of spontaneous circulation (ROSC) and survival to hospital-discharge (STHD) during the pandemic than that in the pre-pandemic period.46
In addition, Liu et al. conducted an online, cross-sectional survey for people living with HIV, individuals at risk of HIV infection, and service prescribers and reported that although HIV services in Taiwan were not severely affected by the initial wave of COVID-19, there were notable disruptions in HIV screening and prevention services.47 For patients with acute ischemic stroke requiring mechanical thrombectomy, Chang et al. demonstrated that there would be no time delay under a prepared protocol for the pandemic.48 Similarly, Li et al. showed that there was no increase in endoscopic retrograde cholangiopancreatography-related complications and mortality during the lockdown period.49 However, the COVID-19 pandemic could negatively affect the utilization of cancer screening in Taiwan.50, 51, 52 Using nationwide cervical, breast, colorectal and oral cancer screening data, Shen et al. demonstrated that the average percentage change declined from 15% to 40% for cervical, breast, and colorectal cancer screening, with a nearly 50% decline in oral cancer screening.50 This effect could result in delay diagnosis of early cancer. Such as breast cancer, Chou et al. reported that total breast biopsy, mammography-guided, and ultrasound-guided biopsies decreased by 17%, 23%, and 14%, respectively, from pre-COVID-19 to COVID-19.53 In addition, the number of total breast cancers and early breast cancers (stages 0 and 1) decreased by 10% and 38%, respectively, during pandemic. Finally, the ratio of early breast cancer among total breast cancer significantly reduced from 71% to 49% (p < 0.001).53
Finally, Liu et al. conducted a retrospective study using the Taiwan Clinical Performance Indicators to assess the impacts of COVID-19 on healthcare quality of medical centers.54 The authors found that unscheduled returns of emergency patients, unscheduled returns of hospitalized patients, and unscheduled returns of surgical patients to the operating room during hospitalization all declined during the COVID-19 outbreak.54 Although these findings indicated that health care quality seemed to improve during pandemic, we did not know whether those who were in need of returning to the emergency room or hospital were reluctant or were prevented from travel by the shelter-in-place policy. In addition, there were significant regional variations in healthcare quality indicators among medical centers in northern and middle/southern, so further investigation is warranted to clarify these issues.54
In summary, most of the healthcare utilities in Taiwan, including ED visits, outpatient visits, inpatients hospitalization, and specific services, such as HIV screening and prevention service, or cancer screening had significantly reduced during COVID-19 pandemic. However, further study is warranted to assess the long-term effect.
Psychosocial and motor effect
The workloads of HCWs significantly increased during the pandemic and medical workers might be particularly vulnerable to mental illness due to long working hours, the risk of infection, the lack of personal protective equipment, physical fatigue, and separation from their family members during critical times.25 , 55 , 56 To date, many studies had reported its negative impact on the incidence of mental health disorders, such as depression, anxiety, and burnout, among healthcare professionals.55, 56, 57, 58, 59 Compared with the non-pandemic period (2019), employees working in Taiwan during the COVID-19 pandemic (2020) have higher burnout scores and percentages of severe burnout.60 Moreover, Yang et al. found that the increases of the personal burnout levels and living apart from families were the main factors associated with the posttraumatic stress disorder symptoms symptom among emergency nurses in Taiwan.61
Furthermore, a comparative and cross-sectional study during two waves of the COVID-19 pandemic in Taiwan showed that the social impact during the second wave was higher for first- and second-line HCWs than during the first wave, and they expressed a higher intention to maintain social distancing and were more aware of the pandemic overseas in the second wave.62 In addition, sleep quality was worse in the first-line HCWs than in the second-line HCWs during both waves.62 In addition to adverse psychomotor impact, Liao et al. using a hospital-based repeated measures study found that the risks of hypertension, diabetes, and dyslipidemia among HCWs increased in Taiwan after the COVID-19 pandemic.63 Such an increase might be further magnified by specific sociodemographic factors, especially female gender, workplace seniority, and higher levels of education. Ke et al. conducted a cross-sectional study to evaluate the impact of the COVID-19 pandemic on physical activity (PA) and dietary habits, and their impact on body weight changes during the Level 3 alert period (between 1 July 2021 and 15 July 2021) in Taiwan.64 They found that all levels of PA, including vigorous and moderate activities and walking decreased, and an daily sitting time increased during the study period.64 Wang et al. explored the changes of cognitive, physical, and nutritional status before and after the interruption and resumption of daycare services during the COVID-19 pandemic in older dementia people in a daycare center and found that their mini-nutritional assessment-short forms (MNA-SF) scores and timed up-and-go (TUG) values deteriorated significantly after a 3-month closure of daycare services (p < 0.05), and after resumption of daycare services the MNA-SF scores and TUG values recovered to near the pre-lockdown levels.65 All these findings indicated that COVID-19 pandemic has had an adverse impact on psychosocial and motor status among Taiwanese and suggested that adequate measures should be adopted as early as possible to support the healthcare system.
Conclusions
Like other countries, the government and healthcare authority paid great efforts, including the implementation of NPIs, and development of novel vaccine and TCMs in response to COVID-19. During the pandemic, the NPIs against COVID-19 helped prevent many NIDs in Taiwan, but COVID-19 also negatively affected the healthcare utility and public health. Although the outbreak of SARS-CoV-2 infections may gradually subsided, we should keep monitoring its associated impact and appropriately response to this pandemic.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in china, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and Coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lai C.C., Wang C.Y., Wang Y.H., Hsueh S.C., Ko W.C., Hsueh P.R. Global epidemiology of coronavirus disease 2019 (COVID-19): disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. Int J Antimicrob Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. https://covid19.who.int/accessed on February 24, 2023.
- 5.Liu Y.C., Liao C.H., Chang C.F., Chou C.C., Lin Y.R. A locally transmitted case of SARS-CoV-2 infection in Taiwan. N Engl J Med. 2020;382:1070–1072. doi: 10.1056/NEJMc2001573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taiwan CDC. https://nidss.cdc.gov.tw/nndss/cdcwnh07?Id=19cov accessed on January 13, 2023.
- 7.Lai C.C., Yen M.Y., Lee P.I., Hsueh P.R. How to keep COVID-19 at bay: a Taiwanese perspective. J Epidemiol Glob Health. 2021;11:1–5. doi: 10.2991/jegh.k.201028.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng H.Y., Liu D.P. Early prompt response to COVID-19 in Taiwan: comprehensive surveillance, decisive border control, and information technology support. J Formos Med Assoc. 2022 doi: 10.1016/j.jfma.2022.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020;323:1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 10.Cheng H.Y., Jian S.W., Liu D.P., Ng T.C., Huang W.T., Lin H.H. Taiwan COVID-19 Outbreak Investigation Team. Contact tracing assessment of COVID-19 transmission dynamics in Taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern Med. 2020;180:1156–1163. doi: 10.1001/jamainternmed.2020.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ou H.T., Yang Y.H.K. Community pharmacists in Taiwan at the frontline against the novel coronavirus pandemic: gatekeepers for the rationing of personal protective equipment. Ann Intern Med. 2020;173:149–150. doi: 10.7326/M20-1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Summers J., Cheng H.Y., Lin H.H., Barnard L.T., Kvalsvig A., Wilson N., et al. Potential lessons from the Taiwan and New Zealand health responses to the COVID-19 pandemic. Lancet Reg Health West Pac. 2020;4 doi: 10.1016/j.lanwpc.2020.100044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yen M.Y., Schwartz J., Chen S.Y., King C.C., Yang G.Y., Hsueh P.R. Interrupting COVID-19 transmission by implementing enhanced traffic control bundling: implications for global prevention and control efforts. J Microbiol Immunol Infect. 2020;53:377–380. doi: 10.1016/j.jmii.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang C.J., Chen T.C., Chen Y.H. The preventive strategies of community hospital in the battle of fighting pandemic COVID-19 in Taiwan. J Microbiol Immunol Infect. 2020;53:381–383. doi: 10.1016/j.jmii.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee I.K., Wang C.C., Lin M.C., Kung C.T., Lan K.C., Lee C.T. Effective strategies to prevent coronavirus disease-2019 (COVID-19) outbreak in hospital. J Hosp Infect. 2020;105:102–103. doi: 10.1016/j.jhin.2020.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hsu F.F., Yang C.J., Tsai M.S., Tsai H.Y., Chen H.A., Liao C.H. Control of an outbreak of COVID-19 at a tertiary hospital in Taiwan. J Microbiol Immunol Infect. 2022;55:1052–1059. doi: 10.1016/j.jmii.2022.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Su W.L., Lin C.P., Huang H.C., Wu Y.K., Yang M.C., Chiu S.K., et al. Clinical application of 222 nm wavelength ultraviolet c irradiation on SARS-CoV-2 contaminated environments. J Microbiol Immunol Infect. 2022;55:166–169. doi: 10.1016/j.jmii.2021.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang P.Y., Wu T.S., Cheng C.W., Chen C.J., Huang C.G., Tsao K.C., et al. A hospital cluster of COVID-19 associated with a SARS-CoV-2 superspreading event. J Microbiol Immunol Infect. 2022;55:436–444. doi: 10.1016/j.jmii.2021.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan W.P., Yao M.S., Lin M.F., Chang H.C., Kosik R.O., Lee W.S. Management and infection control practices in a Taiwanese radiology department during the COVID-19 outbreak. J Microbiol Immunol Infect. 2021;54:349–358. doi: 10.1016/j.jmii.2021.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kung C.T., Wu K.H., Wang C.C., Lin M.C., Lee C.H., Lien M.H. Effective strategies to prevent in-hospital infection in the emergency department during the novel coronavirus disease 2019 pandemic. J Microbiol Immunol Infect. 2021;54:120–122. doi: 10.1016/j.jmii.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang J.H., Chang H.T., Liao C.H., Chiu K.M. Rapid response of a medical center upon the surge of COVID-19 epidemic in Taiwan. J Microbiol Immunol Infect. 2022;55:1–5. doi: 10.1016/j.jmii.2021.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lai C.C., Wang J.H., Ko W.C., Yen M.Y., Lu M.C., Lee C.M., et al. COVID-19 in long-term care facilities: an upcoming threat that cannot be ignored. J Microbiol Immunol Infect. 2020;53:444–446. doi: 10.1016/j.jmii.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yen M.Y., Schwartz J., King C.C., Lee C.M., Hsueh P.R. Recommendations for protecting against and mitigating the COVID-19 pandemic in long-term care facilities. J Microbiol Immunol Infect. 2020;53:447–453. doi: 10.1016/j.jmii.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lai C.C., Chen I.T., Chao C.M., Lee P.I., Ko W.C., Hsueh P.R. COVID-19 vaccines: concerns beyond protective efficacy and safety. Expert Rev Vaccines. 2021;20:1013–1025. doi: 10.1080/14760584.2021.1949293. [DOI] [PubMed] [Google Scholar]
- 25.Hsieh S.M., Liu M.C., Chen Y.H., Lee W.S., Hwang S.J., Cheng S.H., et al. Safety and immunogenicity of CpG 1018 and aluminium hydroxide-adjuvanted SARS-CoV-2 S-2P protein vaccine MVC-COV1901: interim results of a large-scale, double-blind, randomised, placebo-controlled phase 2 trial in Taiwan. Lancet Respir Med. 2021;9:1396–1406. doi: 10.1016/S2213-2600(21)00402-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu L.T., Chiu C.H., Chiu N.C., Tan B.F., Lin C.Y., Cheng H.Y., et al. Safety and immunogenicity of SARS-CoV-2 vaccine MVC-COV1901 in Taiwanese adolescents: a randomized phase 2 trial. NPJ Vaccines. 2022;7:165. doi: 10.1038/s41541-022-00589-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Waits A., Chen J.Y., Cheng W.H., Yeh J.I., Hsieh S.M., Chen C., et al. Safety and immunogenicity of MVC-COV1901 vaccine in older adults: phase 2 randomized dose-comparison trial. Int J Infect Dis. 2022;124:21–26. doi: 10.1016/j.ijid.2022.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Torales J., Cuenca-Torres O., Barrios L., Armoa-Garcia L., Estigarribia G., Sanabria G., et al. An evaluation of the safety and immunogenicity of MVC-COV1901: results of an interim analysis of a phase iii, parallel group, randomized, double-blind, active-controlled immunobridging study in Paraguay. Vaccine. 2023;41:109–118. doi: 10.1016/j.vaccine.2022.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang S., Wang C.Y., Kuo H.K., Peng W.J., Huang J.H., Kuo B.S., et al. A novel RBD-protein/peptide vaccine elicits broadly neutralizing antibodies and protects mice and macaques against SARS-CoV-2. Emerg Microb Infect. 2022;11:2724–2734. doi: 10.1080/22221751.2022.2140608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang C.Y., Hwang K.P., Kuo H.K., Peng W.J., Shen Y.H., Kuo B.S., et al. A multitope SARS-CoV-2 vaccine provides long-lasting B cell and T cell immunity against Delta and Omicron variants. J Clin Invest. 2022;132 doi: 10.1172/JCI157707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guirakhoo F., Wang S., Wang C.Y., Kuo H.K., Peng W.J., Liu H., et al. High neutralizing antibody levels against severe acute respiratory syndrome coronavirus 2 omicron BA.1 and BA.2 after UB-612 vaccine booster. J Infect Dis. 2022;226:1401–1406. doi: 10.1093/infdis/jiac241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paudyal V., Sun S., Hussain R., Abutaleb M.H., Hedima E.W. Complementary and alternative medicines use in COVID-19: a global perspective on practice, policy and research. Res Soc Adm Pharm. 2022;18:2524–2528. doi: 10.1016/j.sapharm.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tseng Y.H., Lin S.J., Hou S.M., Wang C.H., Cheng S.P., Tseng K.Y., et al. Curbing COVID-19 progression and mortality with traditional chinese medicine among hospitalized patients with COVID-19: a propensity score-matched analysis. Pharmacol Res. 2022;184 doi: 10.1016/j.phrs.2022.106412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsai K.C., Huang Y.C., Liaw C.C., Tsai C.I., Chiou C.T., Lin C.J., et al. A traditional chinese medicine formula nricm101 to target COVID-19 through multiple pathways: a bedside-to-bench study. Biomed Pharmacother. 2021;133 doi: 10.1016/j.biopha.2020.111037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheng Y.D., Lu C.C., Hsu Y.M., Tsai F.J., Bau D.T., Tsai S.C., et al. In Silico and in vitro studies of Taiwan Chingguan Yihau (NRICM101) on TNF-α/IL-1β-induced human lung cells. Biomedicine. 2022;12:56–71. doi: 10.37796/2211-8039.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wei W.C., Liaw C.C., Tsai K.C., Chiou C.T., Tseng Y.H., Chiou W.F., et al. Targeting spike protein-induced tlr/net axis by COVID-19 therapeutic NRICM102 ameliorates pulmonary embolism and fibrosis. Pharmacol Res. 2022;184 doi: 10.1016/j.phrs.2022.106424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lai C.C., Chen S.Y., Yen M.Y., Lee P.I., Ko W.C., Hsueh P.R. The impact of the coronavirus disease 2019 epidemic on notifiable infectious diseases in Taiwan: a database analysis. Trav Med Infect Dis. 2021;40 doi: 10.1016/j.tmaid.2021.101997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lai C.C., Chen S.Y., Yen M.Y., Lee P.I., Ko W.C., Hsueh P.R. The impact of COVID-19 preventative measures on airborne/droplet-transmitted infectious diseases in Taiwan. J Infect. 2021;82:e30–e31. doi: 10.1016/j.jinf.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuo S.C., Shih S.M., Chien L.H., Hsiung C.A. Collateral benefit of COVID-19 control measures on influenza activity, Taiwan. Emerg Infect Dis. 2020;26:1928–1930. doi: 10.3201/eid2608.201192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hung S.H., Lin W.T., Wang J.H., Lai C.C. The impact of COVID-19 on the epidemiology of non-airborne/droplet-transmitted notifiable infectious diseases in Taiwan: a descriptive study. J Infect Public Health. 2022:100151–100155. doi: 10.1016/j.jiph.2022.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee K.K., Lai C.C., Chao C.M., Tang H.J. Increase in sexually transmitted infection during the COVID-19 pandemic in Taiwan. J Eur Acad Dermatol Venereol. 2021;35:e171–e172. doi: 10.1111/jdv.17005. [DOI] [PubMed] [Google Scholar]
- 42.Tsai Y.Y., Yang T.T. Measuring voluntary responses in healthcare utilization during the COVID-19 pandemic: evidence from Taiwan. PLoS One. 2022;17 doi: 10.1371/journal.pone.0271810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tan C.K., Lai C.C. The impact of COVID-19 control measures on the utilization of emergency department during lunar new year in Taiwan. Am J Emerg Med. 2021;43:252–254. doi: 10.1016/j.ajem.2021.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lin P.H., Su H.Y., Tsai I.T., Lee K.H., Wang Y.H., Chang C.S., et al. Impact of COVID-19 pandemic on emergency department volume and acuity in low incidence area: Taiwan's experience in three hospitals. J Acute Med. 2022;12:105–112. doi: 10.6705/j.jacme.202209_12(3).0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yu J.H., Liu C.Y., Chen W.K., Yu S.H., Huang F.W., Yang M.T., et al. Impact of the COVID-19 pandemic on emergency medical service response to out-of-hospital cardiac arrests in Taiwan: a retrospective observational study. Emerg Med J. 2021;38:679–684. doi: 10.1136/emermed-2020-210409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen C.Y., Lee E.P., Chang Y.J., Yang W.C., Lin M.J., Wu H.P. Impact of coronavirus disease 2019 pandemic on pediatric out-of-hospital cardiac arrest in the emergency department. Front Pediatr. 2022;10 doi: 10.3389/fped.2022.846410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu W.D., Wang H.Y., Du S.C., Hung C.C. Impact of the initial wave of COVID-19 pandemic in Taiwan on local HIV services: results from a cross-sectional online survey. J Microbiol Immunol Infect. 2022;55:1135–1143. doi: 10.1016/j.jmii.2022.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chang Y.H., Liao N.C., Tsuei Y.S., Chen W.H., Shen C.C., Yang Y.C., et al. Maintaining the quality of mechanical thrombectomy after acute ischemic stroke in COVID19 patients. Brain Sci. 2022;12:1431. doi: 10.3390/brainsci12111431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li C.J., Chang T.E., Hou M.C., Huang Y.H., Lee P.C., Chang N.W., et al. Lockdown period during sars COVID-19 endemic outbreak in Taiwan did not cause an increase of the complications nor mortality of patients received ercp: a single center retrospective study. J Chin Med Assoc. 2022 doi: 10.1097/jcma.0000000000000861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shen C.T., Hsieh H.M., Chang Y.L., Tsai H.Y., Chen F.M. Different impacts of cancer types on cancer screening during COVID-19 pandemic in Taiwan. J Formos Med Assoc. 2022;121:1993–2000. doi: 10.1016/j.jfma.2022.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tsai H.Y., Chang Y.L., Shen C.T., Chung W.S., Tsai H.J., Chen F.M. Effects of the COVID-19 pandemic on breast cancer screening in Taiwan. Breast. 2020;54:52–55. doi: 10.1016/j.breast.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Peng S.M., Yang K.C., Chan W.P., Wang Y.W., Lin L.J., Yen A.M., et al. Impact of the COVID-19 pandemic on a population-based breast cancer screening program. Cancer. 2020;126:5202–5205. doi: 10.1002/cncr.33180. [DOI] [PubMed] [Google Scholar]
- 53.Chou C.P., Lin H.S. Delayed breast cancer detection in an asian country (Taiwan) with low COVID-19 incidence. Cancer Manag Res. 2021;13:5899–5906. doi: 10.2147/CMAR.S314282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu S.A., Wu C.L., Chou I.J., Wang P.C., Hsu C.L., Chen C.P. The impacts of COVID-19 on healthcare quality in tertiary medical centers-a retrospective study on data from Taiwan clinical performance indicators system. Int J Environ Res Publ Health. 2022;19:2278. doi: 10.3390/ijerph19042278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kang L., Li Y., Hu S., Chen M., Yang C., Yang B.X., et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatr. 2020;7:e14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Luceño-Moreno L., Talavera-Velasco B., García-Albuerne Y., Martín-García J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int J Environ Res Publ Health. 2020;17:5514. doi: 10.3390/ijerph17155514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Serrano-Ripoll M.J., Meneses-Echavez J.F., Ricci-Cabello I., Fraile-Navarro D., Fiol-deRoque M.A., Pastor-Moreno G., et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. 2020;277:347–357. doi: 10.1016/j.jad.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Magnavita N., Soave P.M., Antonelli M. Prolonged stress causes depression in frontline workers facing the COVID-19 pandemic-a repeated cross-sectional study in a COVID-19 hub-hospital in central Italy. Int J Environ Res Publ Health. 2021;18:7316. doi: 10.3390/ijerph18147316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Saragih I.D., Tonapa S.I., Saragih I.S., Advani S., Batubara S.O., Suarilah I., et al. Global prevalence of mental health problems among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud. 2021;121 doi: 10.1016/j.ijnurstu.2021.104002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lin Y.Y., Pan Y.A., Hsieh Y.L., Hsieh M.H., Chuang Y.S., Hsu H.Y., et al. COVID-19 pandemic is associated with an adverse impact on burnout and mood disorder in healthcare professionals. Int J Environ Res Publ Health. 2021;18:3654. doi: 10.3390/ijerph18073654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yang B.J., Yen C.W., Lin S.J., Huang C.H., Wu J.L., Cheng Y.R., et al. Emergency nurses' burnout levels as the mediator of the relationship between stress and posttraumatic stress disorder symptoms during COVID-19 pandemic. J Adv Nurs. 2022;78:2861–2871. doi: 10.1111/jan.15214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li D.J., Wu H.C., Chou F.H., Hsu S.T., Huang J.J., Hsieh K.Y., et al. The social and mental impact on healthcare workers: a comparative and cross-sectional study during two waves of the COVID-19 pandemic in Taiwan. Medicine (Baltim) 2022;101 doi: 10.1097/MD.0000000000031316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liao M.H., Lai Y.C., Lin C.M. Cardiovascular risk factors in hospital workers during the COVID-19 pandemic: a hospital-based repeated measures study. Int J Environ Res Publ Health. 2022;19 doi: 10.3390/ijerph192316114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ke H.T., Hsieh C.L., Cheng W.J. Physical activity, dietary behavior, and body weight changes during the COVID-19 nationwide level 3 alert in Taiwan: results of a Taiwanese online survey. Nutrients. 2022;14:4941. doi: 10.3390/nu14224941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang Y.S., Lin C.F., Kuo F.H., Chou Y.C., Lin S.Y. Impact of daycare service interruption during COVID-19 pandemic on physical and mental functions and nutrition in older people with dementia. Healthcare (Basel) 2022;10:1744. doi: 10.3390/healthcare10091744. [DOI] [PMC free article] [PubMed] [Google Scholar]