Abstract
Variability in pain-related outcomes can hamper assay sensitivity of chronic pain clinical trials. Expectations of outcome in such trials may account for some of this variability, and thereby impede development of novel pain treatments. Measurement of participants’ expectations prior to initiating study treatment (active or placebo) is infrequent, variable, and often unvalidated. Efforts to optimize and standardize measurement, analysis, and management of expectations are needed. In this Focus Article, we provide an overview of research findings on the relationship between baseline expectations and pain-related outcomes in clinical trials of pharmacological and non-pharmacological pain treatments. We highlight the potential benefit of adjusting for participants’ expectations in clinical trial analyses and draw on findings from patient interviews to discuss critical issues related to measurement of expectations. We conclude with suggestions regarding future studies focused on better understanding the utility of incorporating these measures into clinical trial analyses.
Perspective
This focus article provides an overview of the relationship between participants’ baseline expectations and pain-related outcomes in the setting of clinical trials of chronic pain treatments. Systematic research focused on the measurement of expectations and the impact of adjusting for expectations in clinical trial analyses may improve assay sensitivity.
Keywords: outcome expectations, chronic pain, clinical trials, covariate adjustment, assay sensitivity
1. Introduction
Currently available analgesics for chronic pain are only moderately effective and, in practice, provide little to no relief for many patients. Development of novel analgesics has proven challenging, with decreasing treatment effect sizes observed in recent randomized clinical trials (RCTs), even for drugs with known efficacy.15, 36 High variability in pain ratings and substantial placebo group responses (i.e., reduction in pain intensity ratings among control group participants exposed to a placebo/”sham” treatment) can hamper assay sensitivity of these trials.11 One factor that could contribute to high variability of outcomes and to placebo group responses is participants’ outcome expectations (i.e., one’s prediction or belief about the outcome of receiving a treatment).5 While evidence suggests that expectations account for some of the variability of outcomes after analgesic and placebo treatments (e.g.,21, 28), evaluation of and adjustment for participants’ outcome expectations in pain clinical trials is infrequent. Efforts to optimize, standardize, and validate measures of outcome expectations for use (and analysis) in chronic pain clinical trials are needed.6
In this Focus Article, we summarize evidence for the relationship between baseline expectations and outcome after analgesic or placebo treatments, discuss the potential advantages of including baseline outcome expectations for change in pain as a covariate in chronic pain RCTs, discuss some measurement issues revealed through concept elicitation interviews among patients with chronic pain, and outline important next steps.
2. Evidence of association between expectation and pain-related outcomes in clinical trials of pain treatments clinical trials for chronic pain
Several studies have evaluated the relationship between baseline expectations of pain relief or functional improvement and outcomes of chronic pain interventions. Many of these studies focused on acupuncture,2, 3, 28, 34, 41 physical therapy (e.g., dry needling,18 or manual therapy21, 31) for the treatment of musculoskeletal disorders (e.g., back pain, osteoarthritis). These trials included a variety of assessments of expectations of outcomes, most often a single item that asked participants about how much improvement they expected in their condition in general (regardless of treatment group assignment) or with regard to specific treatment(s) under investigation. Several studies revealed that positive expectations were associated with significantly better patient-reported outcomes, including greater reduction in pain,19, 21, 28, 38, 41, 45 greater improvement in function,21 greater probability of recovery,31 and a more favorable global perceived effect of treatment,3, 19, 21 compared with neutral or negative expectations. Studies that evaluated the interaction between treatment assignment and expectations revealed either that the expectation-outcome association occurred with active, but not placebo treatment38, 41 or that the interaction was not significant.21, 45 In contrast, experimental modifications of expectations (e.g., neutral vs. positive drug presentation) have been shown to have greater effects on outcomes in placebo than active treatment groups.24, 44 Other studies have demonstrated associations between expectations and some but not all outcomes,17, 18, 20, 23 or no significant association30 between treatment expectations and outcomes. Taken together, the variability in both measurement of expectations and in the outcomes evaluated preclude any clear conclusions about the impact of expectations on outcomes in currently available chronic pain trials investigating these relationships. Of note, while the relationship between expectations and outcome has been explored, the inclusion of expectations as a pre-specified covariate in analyses of RCT data is very infrequent.
3. Benefits of covariate adjustment in analyses of clinical trial data
The FDA and EMA both suggest pre-specified adjustment for baseline covariates that are likely associated with trial outcomes to increase the precision of treatment effect estimates and thus increase trial assay sensitivity (or ability to detect a true treatment response).14, 40 Therefore, given the evidence summarized above, it is reasonable to hypothesize that adjustment for baseline expectations may improve assay sensitivity. Inclusion of a baseline assessment of expectations in clinical trials would also make it possible to examine whether baseline expectations moderate analgesic treatment effect sizes (e.g., examine whether the magnitude of the difference between treatment groups varies as a function of participants’ baseline expectations). Measurement of expectations across multiple clinical trials could provide data to investigate whether adjustment for baseline expectations does in fact increase precision (and therefore assay sensitivity) in clinical trials and whether baseline expectations do, in fact, moderate clinical trial outcomes. Consistently-identified moderation effects would support the utility of strategies to modify participant expectations in clinical trials (e.g.,24, 44), justifying randomized studies to evaluate the utility of specific strategies.
To this end, a valid assessment of baseline expectations and systematic investigation of the relationships between expectations and outcomes are needed. A brief, valid and reliable measure of outcome expectations in the context of chronic pain clinical trials could promote uptake in clinical trials, and thus provide the data necessary to evaluate the benefits of adjusting for expectations in the analyses of chronic pain clinical trials.
4. Measurement of expectations
How expectations should be assessed is not clear, as considerable heterogeneity remains in their definition and measurement. Multiple patient-reported measures exist to assess outcome expectations (e.g., see 1 for systematic review); however, many measures are either quite lengthy, thereby prohibiting their use in clinical trials where expectations are not the primary outcome (e.g., 35-item Treatment Expectation Questionnaire1), not worded appropriately for chronic pain that is unlikely to “completely” resolve (e.g., Stanford Expectations of Treatment Scale46), and/or do not incorporate the possibility of receiving placebo treatment (e.g., “this treatment” may refer to active or placebo treatment9, 46). Of note, a prior qualitative study identified modifications to the generic Credibility/Expectancy Questionnaire (CEQ) that were necessary to ensure content validity among patients with chronic pain in the setting of rehabilitative therapy.29
With some exceptions (e.g., CEQ), clinical trials of pain treatments have predominantly included unvalidated and variably worded single-item questions (e.g., “How helpful do you believe [treatment X] would be for your current back problems?”23). Measures also vary in terms of response options (e.g., 0 – 10 numeric rating scales for expected improvement,17, 19, 23 expected pain intensity,41 likelihood of recovery,31 0% - 100% for expected pain relief,38 “much worse / worse / a little worse/ the same / better / much better”18). Given that we lack evidence for how these questions might be interpreted, and what factors or experiences might influence expectations, it is critical that we include patient perspectives.8, 26 A more defined patient-centered conceptualization of expectations, particularly as they pertain to clinical trial outcomes in chronic pain, is essential to inform valid assessment.
4.1. A qualitative exploration of expectation measurement
Given that (1) the literature suggests that adjusting for baseline expectations may improve assay sensitivity, (2) little is known about patients’ interpretation of questions about expectations, (3) there is inconsistency in the literature on measures of expectations, and (4) evaluating the patient perspective is recommended as an initial step in the development of new measurement tools (e.g., by regulatory agencies, such as FDA39), we conducted an exploratory qualitative inquiry into how patients with chronic pain rate outcome expectations in the context of a hypothetical clinical trial. We conducted semi-structured qualitative interviews among 22 individuals with a wide range of chronic pain conditions over a 3-month period. The study was approved by the University of Rochester RSRB. All interviews were done by a single trained interviewer (R.L.). English-speaking adults who had experienced chronic pain for at least 3 months prior, which was verified through medical records, were eligible to participate in the study. All participants were compensated monetarily ($50) upon interview completion. Participants self-reported age, gender, race, and level of education at the outset of the interview. Participants ranged in age from 25 to 76 years old (M = 51.8; SD =16.9). The sample was 68% female; 5% Asian, 14% Black or African American, 73% White, and 9% mixed race (i.e., endorsed two or more racial groups) or unknown; 5% had less than a high school degree, 32% were high school graduates, and 50% and 14% obtained a college or graduate degree, respectively.
During the interviews, participants were presented with a hypothetical scenario that asked them to imagine that they were starting a clinical trial for a new treatment for their chronic pain condition, with equal chance of receiving a placebo or active treatment. Interview questions evaluated participant feedback on single-item questions designed to rate “study treatment” outcome expectations, as well as what factors participants perceived as contributing to their expectation ratings. Participants were introduced to the concept of a randomized clinical trial with 50% chance of receiving active treatment or placebo and then asked to rate their expectations for a change in pain after receiving “study treatment” (i.e., active or placebo). Participants were intentionally not asked to rate expectations of group assignment and outcome of active treatment separately because the construct that is important to assess for the purposes of predicting outcomes in a clinical trial is participant expectations of outcome in the context of the possibility of receiving a placebo. Consensus on which specific question(s) best captured study treatment expectations was not achieved; however, interviews, which included a “think-aloud” technique (used to gauge insight into an individual’s cognitive processing10, 42, 43), revealed several themes regarding those factors that contributed to participants’ expectations for outcome. To enact the think-aloud portion of the interviews, the single interviewer (R.L.) instructed participants to verbalize their thought processes while answering each interview question. To provide clarity on this technique, participants were presented with an example scenario/question. The example scenario and question were as follows: “Imagine you are going to eat at a brand-new Italian restaurant that just opened downtown and someone then asks you the following question: ”After eating at this, I expect to feel [response options]: ‘Very satisfied and will want to eat here again as soon as possible’, ‘Satisfied’, ‘Neutral’, ‘Okay, but I probably won’t eat here again’, or ‘I want my money back’. The interviewer then demonstrated the following example think-aloud process for what they might be thinking while answering the example question: “I expect that I will feel satisfied because this restaurant is brand new, which is often a promising sign, and I like to try new things. I also love Italian food, so I expect to at least enjoy the meal somewhat, but trying a completely new place can also be risky and I might not like it.” This think-aloud technique was used to more accurately capture all the factors that contribute to and shape an individual’s outcome expectations, whereas having participants answer multiple scripted questions about expectations or participating in focus group discussions may not have provided this rich and more personal information.
A content analysis based on participants’ responses was conducted using audio-recordings of all interviews. Direct quotes from participants in response to each question were extracted by the single reviewer (R.L.) and preliminary concepts identified. The number and types of conceptual categories were finalized through discussion of direct quotes among three authors (R.L., J.S.G., and D.J.L). The number of participants who endorsed a conceptual category (i.e., made relevant direct quote) was then tallied by R.L. For the think-aloud portion of interviews, three common concepts were identified: (1) balance between hope and realistic expectations for treatment efficacy (n=17; 77%; e.g., “I’m optimistic, but don’t expect full relief”), hope for treatment efficacy (n=13; 59%, e.g., “I’m hoping that it gives some relief”); and evidence of experimental efficacy (n=6, 27%, e.g., “You said that the research has shown that the new drug has been shown to be effective at reducing chronic pain”). Interestingly, either using think-aloud or a probing follow-up question, the majority of participants (64%) did not factor in the possibility of receiving the placebo treatment when considering how to rate their expectations (e.g., “my mind didn’t go there [placebo], no”; “I always just assume I am not getting the placebo”; “I’m hoping that I get the real thing”). If this finding generalizes to real clinical trial settings, it suggests that participants’ expectations are commonly based on the assumption (or hope) that they will receive the active treatment, disregarding the possibility of assignment to placebo. Mitigating this assumption of treatment assignment may serve to decrease expectations, which could reduce improvements in subjective outcomes in the placebo group of clinical trials (and thereby improve assay sensitivity) (e.g., 24, 44). However, given findings that expectations are uniquely associated with active treatment group outcomes,20, 38, 41 attenuating baseline expectations could potentially have a neutral or even harmful effect on assay sensitivity.
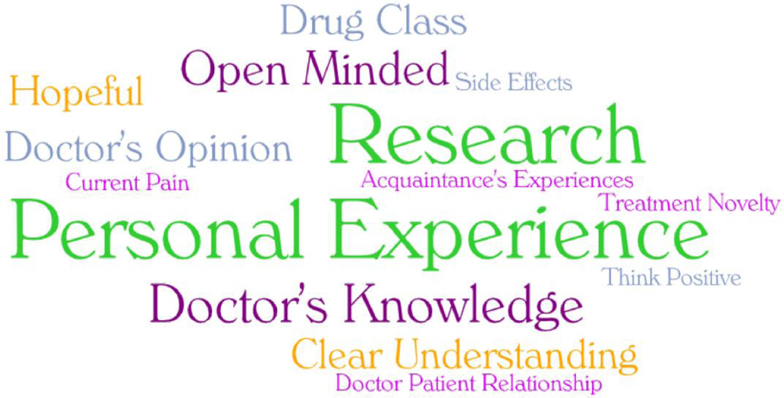
Participants noted a number of factors when asked what contributed to their expectations for pain treatment (Figure 1). Personal experience with previous pain treatments and existing research on the specific pain treatment were most commonly reported (each by 12 participants; 55%). Participants also considered their doctor’s knowledge (n=5; 23%), noted a willingness to be open-minded about treatment (n=4; 18%), and highlighted the importance of a clear understanding of the treatment, the type of drug, the doctor’s opinion or belief in the treatment, and hopefulness (all 14%). That participants were less likely to verbalize “hopefulness” as a contributing factor for expectations than when they described their thinking while rating their expectations (14% vs 59%) reinforces the added value of incorporating a “think-aloud” approach. Other less prevalent factors included acquaintances’ treatment experience, current pain state, relationship with their doctor, side effects, positive thinking, and treatment novelty (all 5%).
Figure 1.
Themes of contributions to expectations described participants
5. Conclusions, considerations, and future directions
Taken together, these findings highlight the heterogeneous factors surrounding the construct of outcome expectations in the context of chronic pain clinical trials, as well as the impact of the individual’s unique perspectives and considerations, some of which may be unconsciously formulated,22 and therefore outside the realm of patient-reported measurement. This observation is aligned with evidence from studies of outcome expectations in the context of psychotherapy,7 in which outcome expectations may be delineated as overt or “cognitive” expectations (e.g., influenced by doctor’s opinion or research findings as noted in our study) or conditioned or “non-cognitive” (e.g., influenced by patient’s personal experience).
While evidence suggests that adjusting for treatment expectations may improve assay sensitivity, further work is necessary to determine the best approach to assess it in a reliable and valid way. For example, whether a single question is sufficient or whether more questions explicitly capturing cognitive and non-cognitive domains are necessary to adequately capture the concept of expectation (without inadvertently amplifying expectation with in-depth questioning) in the context of chronic pain trials warrants evaluation. Evaluation of potential measures of expectations that could be used as covariates in primary analyses to maximize assay sensitivity could be achieved through inclusion of different measurement tools using a SWAT (“studies within a trial”)-like approach,37 wherein participants are randomized within each arm of the study to complete one of two (or three) candidate expectation measures and their relative impact on assay sensitivity is evaluated.
In addition, delineating between treatment assignment expectations and outcome expectations and comparing which construct best predicts study outcomes may be worthwhile, considering our study suggests that the expectations for assignment to treatment or placebo groups may be overlooked when rating expectations. In fact, an interesting line of inquiry might focus on measuring expectations of study outcomes in general and separately measuring expectations supposing assignment to active treatment. This approach would: (1) provide a clearer understanding of what drives ratings of overall expectations of study outcome and (2) allow for comparison of whether overall expectations or expectations specific to active treatment are most predictive of outcomes in a clinical trial. Such an investigation could be conducted systematically, again employing a SWAT-like approach, with randomization to rating overall expectations only or rating both overall expectations and expectations supposing active treatment.
It should also be acknowledged that outcome expectations are dynamic and may change over the course of a trial. If participants experience pain relief or adverse effects soon after initiating treatment, they may guess their assignment to active treatment (i.e., unblinding) and therefore recalibrate their outcome expectations accordingly. It should be noted, however, that participants’ guesses are not always correct, as improvement and side-effects can occur independent of the treatment.27, 32 In this dynamic context, outcome expectations might be viewed as a potential mediator of the effect of the intervention requiring more complex methods for analysis.
Outcome expectations may also change across the lifespan as a result of unique contextual and developmental factors. While there is a paucity of research devoted to this topic, it is of relevance given that different approaches to measurement may be necessary for pediatric and geriatric populations. For example, recent reviews suggest that children’s expectations may be more easily modulated/impacted by suggestion compared to adults,4, 35 and psychological determinants, such as magical thinking (which likely declines with age), is associated with larger placebo effects in children.25 Further, while evidence of differential placebo effects by age is inconsistent,33 given that developmental and/or degenerative processes can affect the endogenous pain modulatory system, the relationship between expectations and outcome may change across the lifespan. Perhaps most importantly, children and older adults are often part of a child-parent-clinician or patient-caregiver-clinician interaction. Given this complex psychosocial context, expectations may be influenced by a multitude of cognitive and non-cognitive factors. In fact, for clinical trials of chronic pain treatments among pediatric and geriatric populations, it may be useful to include measures of parents’ or caregivers’ expectations of outcome, respectively, in addition to the participants’ expectations.
Importantly, aggregation of findings across multiple clinical trials that include valid baseline measures of expectation will permit an evidence-based conclusion about the potential moderating effect of expectations. These findings could then inform optimal study designs and statistical approaches for minimizing the impact of expectations on assay sensitivity in order to increase the ability of trials to identify true therapeutic effects of novel pain treatments. Worthwhile future directions may include: (1) identification and/or development of a measure(s) that is content-valid, reliably interpreted, and easily administered; (2) systematic evaluation and comparison of candidate measures embedded in clinical trials to select a measure that accounts for more variability in the primary outcome; (3) pre-specification of outcome expectations as a covariate in analyses of chronic pain RCT data, and; (4) aggregation of findings across studies to determine the impact of covariate adjustment on assay sensitivity. Given the notable challenges with analgesic drug development, including the discouraging observation of reduced effectiveness among established pain therapies,12, 13, 16 efforts aimed at improving assay sensitivity in clinical trials are critical in order to accelerate the identification of safe and effective therapies that might otherwise be overlooked. Assessing and adjusting for outcome expectations could be one effective strategy toward this important goal.
Highlights.
Participants’ outcome expectations may contribute to clinical trial outcome variability
Outcome expectations are influenced by a number of factors
A brief, content-valid measure of outcome expectations is needed
Adjusting for expectations in clinical trial analyses may improve assay sensitivity
Declaration of Competing Interest
Financial support for this article was provided by a NIH K award (K24NS126861; JSG) and the ACTTION public-private partnership with the FDA (U01FD007474; RHD), which has received research contracts, grants, or other revenue from the FDA, multiple pharmaceutical and device companies, philanthropy, and other sources. No official endorsement by the FDA or the pharmaceutical and device companies that have provided unrestricted grants to support the activities of ACTTION should be inferred. JTF reports over the past 3 years funding from NIH-NCATS – UL1 Grant (Co-I), NIH-NIDDK - U01 Grant (CoI), from NIH-NINDS - U24 Grant (PI), and two FDA-BAA Contracts; and compensation for serving on two NIH DSMBs and advisory boards or consulting on clinical trial methods from Vertex and Lilly. During than the past 3 years, DCT has received research grants and contracts from the US Food and Drug Administration and US National Institutes of Health and has received compensation for consulting on clinical trial and patient preferences from Eli Lilly & Company, Flexion, Novartis/GlaxoSmithKline, and Pfizer. RHD has received in the past 5 years research grants and contracts from the US Food and Drug Administration and the US National Institutes of Health, and compensation for serving on advisory boards or consulting on clinical trial methods from Abide, Acadia, Adynxx, Analgesic Solutions, Aptinyx, Aquinox, Asahi Kasei, Astellas, Beckley, Biogen, Biohaven, Biosplice, Boston Scientific, Braeburn, Cardialen, Celgene, Centrexion, Chiesi, Chromocell, Clexio, Collegium, Concert, Confo, Decibel, Editas, Eli Lilly, Endo, Ethismos (equity), Eupraxia, Exicure, Glenmark, Gloriana, Grace, Hope, Lotus, Mainstay, Merck, Mind Medicine (also equity), Neumentum, Neurana, NeuroBo, Novaremed, Novartis, OCT, OliPass, Pfizer, Q-State, Reckitt Benckiser, Regenacy (also equity), Sangamo, Sanifit, Scilex, Semnur, SIMR Biotech, Sinfonia, SK Biopharmaceuticals, Sollis, SPRIM, Teva, Theranexus, Toray, Vertex, Vizuri, and WCG. The remaining authors report no conflicts of interest related to this work.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Alberts J, Lowe B, Glahn MA, Petrie K, Laferton J, Nestoriuc Y, Shedden-Mora M. Development of the generic, multidimensional Treatment Expectation Questionnaire (TEX-Q) through systematic literature review, expert surveys and qualitative interviews. BMJ Open. 10:e036169, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bauml J, Xie SX, Farrar JT, Bowman MA, Li SQ, Bruner D, DeMichele A, Mao JJ. Expectancy in real and sham electroacupuncture: does believing make it so? J Natl Cancer Inst Monogr. 2014:302–307, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen LX, Mao JJ, Fernandes S, Galantino ML, Guo W, Lariccia P, Teal VL, Bowman MA, Schumacher HR, Farrar JT. Integrating acupuncture with exercise-based physical therapy for knee osteoarthritis: a randomized controlled trial. J Clin Rheumatol. 19:308–316, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colloca L. Treatment of Pediatric Migraine. N Engl J Med. 376:1387–1388, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colloca L. The Placebo Effect in Pain Therapies. Annu Rev Pharmacol Toxicol. 59:191–211, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colloca L, Barsky AJ. Placebo and Nocebo Effects. N Engl J Med. 382:554–561, 2020 [DOI] [PubMed] [Google Scholar]
- 7.Constantino MJ, Arnkoff DB, Glass CR, Ametrano RM, Smith JZ. Expectations. J Clin Psychol. 67:184–192, 2011 [DOI] [PubMed] [Google Scholar]
- 8.de Williams AC, Davies HTO, Chadury Y. Simple pain rating scales hide complex idiosyncratic meanings. Pain. 85:457–463, 2000 [DOI] [PubMed] [Google Scholar]
- 9.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 31:73–86, 2000 [DOI] [PubMed] [Google Scholar]
- 10.Drennan J. Cognitive interviewing: verbal data in the design and pretesting of questionnaires. J Adv Nurs. 42:57–63, 2003 [DOI] [PubMed] [Google Scholar]
- 11.Dworkin RH, Turk DC, Peirce-Sandner S, Burke LB, Farrar JT, Gilron I, Jensen MP, Katz NP, Raja SN, Rappaport BA, Rowbotham MC, Backonja MM, Baron R, Bellamy N, Bhagwagar Z, Costello A, Cowan P, Fang WC, Hertz S, Jay GW, Junor R, Kerns RD, Kerwin R, Kopecky EA, Lissin D, Malamut R, Markman JD, McDermott MP, Munera C, Porter L, Rauschkolb C, Rice AS, Sampaio C, Skljarevski V, Sommerville K, Stacey BR, Steigerwald I, Tobias J, Trentacosti AM, Wasan AD, Wells GA, Williams J, Witter J, Ziegler D. Considerations for improving assay sensitivity in chronic pain clinical trials: IMMPACT recommendations. Pain. 153:1148–1158, 2012 [DOI] [PubMed] [Google Scholar]
- 12.Dworkin RH, Turk DC, Peirce-Sandner S, He H, McDermott MP, Farrar JT, Katz NP, Lin AH, Rappaport BA, Rowbotham MC. Assay sensitivity and study features in neuropathic pain trials: an ACTTION meta-analysis. Neurology. 81:67–75, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dworkin RH, Turk DC, Peirce-Sandner S, He H, McDermott MP, Hochberg MC, Jordan JM, Katz NP, Lin AH, Neogi T, Rappaport BA, Simon LS, Strand V. Meta-analysis of assay sensitivity and study features in clinical trials of pharmacologic treatments for osteoarthritis pain. Arthritis Rheumatol. 66:3327–3336, 2014 [DOI] [PubMed] [Google Scholar]
- 14.European Medicines Agency: Guideline on adjustment for baseline covariates in clinical trials.(Use, C.f.M.P.f.H., Ed.), London, UK, 2015. [Google Scholar]
- 15.Finnerup NB, Haroutounian S, Baron R, Dworkin RH, Gilron I, Haanpaa M, Jensen TS, Kamerman PR, McNicol E, Moore A, Raja SN, Andersen NT, Sena ES, Smith BH, Rice ASC, Attal N. Neuropathic pain clinical trials: factors associated with decreases in estimated drug efficacy. Pain. 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finnerup NB, Haroutounian S, Baron R, Dworkin RH, Gilron I, Haanpaa M, Jensen TS, Kamerman PR, McNicol E, Moore A, Raja SN, Andersen NT, Sena ES, Smith BH, Rice ASC, Attal N. Neuropathic pain clinical trials: factors associated with decreases in estimated drug efficacy. Pain. 159:2339–2346, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foster NE, Thomas E, Hill JC, Hay EM. The relationship between patient and practitioner expectations and preferences and clinical outcomes in a trial of exercise and acupuncture for knee osteoarthritis. Eur J Pain. 14:402–409, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gallego-Sendarrubias GM, Voogt L, Arias-Buria JL, Bialosky J, Fernandez-de-Las-Penas C. Can Patient Expectations Modulate the Short-Term Effects of Dry Needling on Sensitivity Outcomes in Patients with Mechanical Neck Pain? A Randomised Clinical Trial. Pain Med. 2021 [DOI] [PubMed] [Google Scholar]
- 19.Garcia AN, Costa LOP, Costa L, Hancock M, Cook C. Do prognostic variables predict a set of outcomes for patients with chronic low back pain: a long-term follow-up secondary analysis of a randomized control trial. J Man Manip Ther. 27:197–207, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldstein MS, Morgenstern H, Hurwitz EL, Yu F. The impact of treatment confidence on pain and related disability among patients with low-back pain: results from the University of California, Los Angeles, low-back pain study. Spine J. 2:391–399; discussion 399–401, 2002 [DOI] [PubMed] [Google Scholar]
- 21.Groeneweg R, Haanstra T, Bolman CAW, Oostendorp RAB, van Tulder MW, Ostelo R. Treatment success in neck pain: The added predictive value of psychosocial variables in addition to clinical variables. Scand J Pain. 14:44–52, 2017 [DOI] [PubMed] [Google Scholar]
- 22.Jensen KB, Kaptchuk TJ, Kirsch I, Raicek J, Lindstrom KM, Berna C, Gollub RL, Ingvar M, Kong J. Nonconscious activation of placebo and nocebo pain responses. Proc Natl Acad Sci U S A. 109:15959–15964, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine (Phila Pa 1976). 26:1418–1424, 2001 [DOI] [PubMed] [Google Scholar]
- 24.Kam-Hansen S, Jakubowski M, Kelley JM, Kirsch I, Hoaglin DC, Kaptchuk TJ, Burstein R. Altered placebo and drug labeling changes the outcome of episodic migraine attacks. Sci Transl Med. 6:218ra215, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krummenacher P, Kossowsky J, Schwarz C, Brugger P, Kelley JM, Meyer A, Gaab J. Expectancy-induced placebo analgesia in children and the role of magical thinking. J Pain. 15:1282–1293, 2014 [DOI] [PubMed] [Google Scholar]
- 26.Langford DJ, Gewandter JS, Amtmann D, Reeve BB, Corneli A, McKenna K, Swezey T, McFatrich M, Jensen MP, Turk DC, Dworkin RH. Initial Content Validation and Roadmap for a New Patient-Reported Outcome Measure of Pain Intensity. J Pain. 23:1945–1957, 2022 [DOI] [PubMed] [Google Scholar]
- 27.Lee JY, Moore P, Kusek J, Barry M, Group CS. Treatment assignment guesses by study participants in a double-blind dose escalation clinical trial of saw palmetto. J Altern Complement Med. 20:48–52, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Linde K, Witt CM, Streng A, Weidenhammer W, Wagenpfeil S, Brinkhaus B, Willich SN, Melchart D. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 128:264–271, 2007 [DOI] [PubMed] [Google Scholar]
- 29.Mertens VC, Moser A, Verbunt J, Smeets R, Goossens M. Content Validity of the Credibility and Expectancy Questionnaire in a Pain Rehabilitation Setting. Pain Pract. 17:902–913, 2017 [DOI] [PubMed] [Google Scholar]
- 30.Myers SS, Phillips RS, Davis RB, Cherkin DC, Legedza A, Kaptchuk TJ, Hrbek A, Buring JE, Post D, Connelly MT, Eisenberg DM. Patient expectations as predictors of outcome in patients with acute low back pain. J Gen Intern Med. 23:148–153, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palmlof L, Holm LW, Alfredsson L, Skillgate E. Expectations of recovery: A prognostic factor in patients with neck pain undergoing manual therapy treatment. Eur J Pain. 20:1384–1391, 2016 [DOI] [PubMed] [Google Scholar]
- 32.Popovic M, Cesana-Nigro N, Winzeler B, Thomann R, Schutz P, Muller B, Christ-Crain M, Blum CA. Estimation of treatment allocation in a randomised, double-blinded, placebo-controlled trial. Swiss Med Wkly. 149:w20114, 2019 [DOI] [PubMed] [Google Scholar]
- 33.Savvas SM, Zelencich LM, Gibson SJ. Should placebo be used routinely for chronic pain in older people? Maturitas. 79:389–400, 2014 [DOI] [PubMed] [Google Scholar]
- 34.Sherman KJ, Cherkin DC, Ichikawa L, Avins AL, Delaney K, Barlow WE, Khalsa PS, Deyo RA. Treatment expectations and preferences as predictors of outcome of acupuncture for chronic back pain. Spine (Phila Pa 1976). 35:1471–1477, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Simmons K, Ortiz R, Kossowsky J, Krummenacher P, Grillon C, Pine D, Colloca L. Pain and placebo in pediatrics: a comprehensive review of laboratory and clinical findings. Pain. 155:2229–2235, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith SM, Fava M, Jensen MP, Mbowe OB, McDermott MP, Turk DC, Dworkin RH. John D. Loeser Award Lecture: Size does matter, but it isn’t everything: the challenge of modest treatment effects in chronic pain clinical trials. Pain. 161 Suppl 1:S3–s13, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Treweek S, Bevan S, Bower P, Campbell M, Christie J, Clarke M, Collett C, Cotton S, Devane D, El Feky A, Flemyng E, Galvin S, Gardner H, Gillies K, Jansen J, Littleford R, Parker A, Ramsay C, Restrup L, Sullivan F, Torgerson D, Tremain L, Westmore M, Williamson PR. Trial Forge Guidance 1: what is a Study Within A Trial (SWAT)? Trials. 19:139, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Turner JA, Jensen MP, Warms CA, Cardenas DD. Blinding effectiveness and association of pretreatment expectations with pain improvement in a double-blind randomized controlled trial. Pain. 99:91–99, 2002 [DOI] [PubMed] [Google Scholar]
- 39.U.S. Food and Drug Administration: Patient-focused drug development: colecting comprehensive and representative input. Guidance for industry, FDA staff, and other stakeholders.(Research, C.f.D.E.a.R.C.f.B.E.a., Ed.), U.S. Food and Drug Administration, Silver Spring, MD, 2020. [Google Scholar]
- 40.Food US and Drug Administration: Adjusting for covariates in randomized clinical trials for drugs and biological products: guidance for industry.(Research, C.f.D.E.a., Ed.), Silver Spring, MD, 2021. [Google Scholar]
- 41.Wasan AD, Kong J, Pham LD, Kaptchuk TJ, Edwards R, Gollub RL. The impact of placebo, psychopathology, and expectations on the response to acupuncture needling in patients with chronic low back pain. J Pain. 11:555–563, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Willis GB: Cognitive interviewing: A tool for improving questionnaire design, SAGE Publications, Inc, Thousand Oaks, CA, 2004. [Google Scholar]
- 43.Willis GB: Analysis of the cognitive interview in questionnaire design, Oxford University Press, 2015. [Google Scholar]
- 44.Wise RA, Bartlett SJ, Brown ED, Castro M, Cohen R, Holbrook JT, Irvin CG, Rand CS, Sockrider MM, Sugar EA, American Lung Association Asthma Clinical Research C. Randomized trial of the effect of drug presentation on asthma outcomes: the American Lung Association Asthma Clinical Research Centers. J Allergy Clin Immunol. 124:436–444, 444e431–438, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang CP, Chang MH, Li TC, Hsieh CL, Hwang KL, Chang HH. Predicting prognostic factors in a randomized controlled trial of acupuncture versus topiramate treatment in patients with chronic migraine. Clin J Pain. 29:982–987, 2013 [DOI] [PubMed] [Google Scholar]
- 46.Younger J, Gandhi V, Hubbard E, Mackey S. Development of the Stanford Expectations of Treatment Scale (SETS): a tool for measuring patient outcome expectancy in clinical trials. Clin Trials. 9:767–776, 2012 [DOI] [PubMed] [Google Scholar]