Abstract
The high morbidity and mortality of hepatocellular carcinoma (HCC) has encouraged the search for new biomarkers to be used alongside alpha-foetoprotein (AFP) and imaging tests. The aim of this study was to evaluate the clinical contribution of protein induced by vitamin K absence or antagonist-II (PIVKA-II) for HCC monitoring after liver transplantation (LT) and compare it with AFP, a routinely used tumour marker. A total of 46 HCC patients (Milan criteria) were enrolled in this study. Serum levels of PIVKA-II and AFP were measured before and after transplantation. Clinical features were determined for all the patients that were included. Significant correlations were found between PIVKA-II expression levels and some clinicopathological features, such as tumour size and number of pre-transplant transarterial chemoembolizations (TACEs). Serum levels of PIVKA-II and AFP decreased significantly after LT and increased in patients with tumour recurrence. Serum PIVKA-II levels may play an important role in predicting disease severity. Furthermore, monitoring PIVKA-II levels in HCC transplant recipients reflects the tumor early recurrence after transplantation and could be used, complementing AFP and imaging tests, as a novel biomarker of this pathology.
Subject terms: Biochemistry, Cancer, Biomarkers, Gastroenterology, Oncology
Introduction
Hepatocellular carcinoma (HCC) accounts for 75–85% of all neoplasms occurring in the liver. Primary liver cancer was the sixth most commonly diagnosed cancer and the third leading cause of cancer death worldwide in 2020, with approximately 906,000 new cases and 830,000 deaths1. Most HCCs occur in patients with underlying liver disease, mostly as a result of hepatitis B or C virus (HBV or HCV) infection or alcohol abuse2. Early diagnosis and effective treatment of this disease remains a challenge. If detected early, HCC could be cured with an excellent long-term prognosis, and the main treatment options would be surgical resection or liver transplantation (LT), when the patient is a suitable candidate for transplantation3.
Serum alpha-fetoprotein (AFP) has been commonly used as a tumour biomarker for the detection of HCC and to monitor the course of the disease. However this tumour marker has shown a low yield as its values in many cases are normal in early tumours4, and 80% of small tumours (under 2 cm) do not express AFP. In addition, patients with liver cirrhosis may have transient elevations of AFP in the absence of HCC5,6. The high morbidity and mortality of this disease has encouraged the search for new biomarkers to be used together with AFP and imaging tests, such as positron emission tomography computed tomography (PET/CT), to monitor the evolution of patients after transplantation and predict relapses and metastases7,8.
Protein induced by vitamin K absence or antagonist-II (PIVKA-II), also known as des gamma-carboxyprothrombin (DCP), is an abnormal prothrombin molecule resulting from an acquired defect in post-translational carboxylation of the prothrombin precursor in malignant cells9 and this marker has been shown to be released in association with vitamin K deficiency and in the presence of HCC10. Previous studies on the relationship between serum PIVKA-II level and various clinicopathological factors in HCC have shown that elevated PIVKA-II may be associated with worse tumour behaviour and prognosis in patients with HCC11. Serum PIVKA-II level may reflect extrahepatic disease progression after LT better than AFP level, because PIVKA-II can induce tumour cell proliferation and promote tumour angiogenesis11,12. Furthermore, PIVKA-II has been recommended as one of the surveillance biomarkers for HCC in at-risk populations and described in the Japanese Society of Hepatology (JSH) guidelines13,14. Despite the many studies that have demonstrated the usefulness of PIVKA-II as a marker of HCC and as an important factor in the selection criteria prior to LT, its clinical utility for early detection of HCC recurrence after transplantation remains unclear12.
Methods
Aim, design and setting of the study
The aim of the present study is to investigate the potential usefulness of PIVKA-II as a biomarker in the follow-up of HCC transplant patients and in the early detection of recurrence in these patients, complementing AFP and imaging tests. This analytical observational prospective dynamic cohort study was conducted at the Virgen de la Arrixaca Hospital (HCUVA, Murcia, Spain) and the Asturias Central Hospital (HUCA). Patients were recruited between September 2014 and May 2021, in two distinct stages: between September 2014 and October 2017 at HCUVA, and between September 2020 and May 2021, at both HCUVA and HUCA.
Characteristics of participants
The inclusion criteria were HCC patients between 18 and 80 years, candidates for LT and in compliance with the Milan criteria. The diagnosis of HCC was made according to clinical, biological and radiological criteria. It was established based on the presence of at least two compatible imaging scans or the existence of a compatible histological diagnosis. The exclusion criteria were patients with HCC outside the Milan criteria, metastatic HCC and taking vitamin K antagonist drugs, such as the anticoagulants acenocoumarol or warfarin, or vitamin K, in the 6 months prior to sample collection. Most patients underwent at least one session of transarterial chemoembolization (TACE) as bridge therapy until transplantation.
Of the 46 patients recruited after being evaluated by the liver transplant programmes of both hospitals, 35 patients were eventually transplanted and followed up for biomarkers at 1, 6, 12 and 24 months after transplantation. Due to losses in the follow-up of some patients, because of death or any other cause, a total of 46 blood samples were collected pre-transplant, 28 samples at 1 month post-transplant, 24 samples at 6 months post-transplant, 24 samples at 1 year post-transplant and 23 samples at 2 years post-transplant.
Materials
PIVKA-II was determined by immunoenzymatic assay using chemiluminescence on the LUMIPULSE® G1200 system analyser (Fujirebio Europe N.V., Gent, Belgium), with an analysis range of 5–75,000 mAU/mL and a cut-off value of 48 mAU/mL. Serum AFP levels were analysed by immunochemistry assay on the Cobas 8000 Modular Analyzer series (Roche Diagnostics, Basel, Switzerland) with a measurement range of 0.605–1210 ng/mL and a cut-off value of 11 ng/mL. The number of tumours was determined by histopathological study of the tissue sample obtained during surgery. The remaining clinical variables (aetiology of cirrhosis, tumour size, number of pre-transplant TACEs, vascular invasion, tumour necrosis, presence/absence of recurrence or post-transplant metastasis) were obtained from the clinical history of each patient, considering for tumour size the diameter in centimetres of the largest lesion at diagnosis by imaging test (computerized tomography or magnetic resonance imaging). The presence of vascular invasion and tumor necrosis was determined by liver biopsy of the explant. For the variable aetiology, we distinguished 10 different groups, according to the cause: alcoholism (ALCH), hepatitis B virus infection (HBV), hepatitis C virus infection (HCV), hepatitis B + C virus infection (HBV + HCV), HCV infection plus alcoholism (HCV + ALCH), HBV infection plus alcoholism (HBV + ALCH,) non-alcoholic steatosis (NASH), haemochromatosis (HEMO) and HCV infection + alcoholism + iron overload (HCV + ALCH + Fe). The aetiology of liver disease was considered cryptogenic (CRIPTO) if no cause was identified. Different aetiologies were then classified into 3 groups: viral aetiology (HBV, HCV, HBV + HCV), non-viral aetiology (ALCH, NASH, HEMO, CRIPTO) and mixed aetiology, which encompasses viral plus non-viral aetiology (HCV + ALCH and HCV + ALCH + ALCH + Fe).
Statistical analysis
The normality of all quantitative variables was tested using the Shapiro–Wilk test. Variables that followed a normal distribution were represented by the mean and standard deviation, while those that did not show a normal distribution were represented by the median and interquartile range (IQR). Qualitative variables were expressed as absolute frequency and relative frequency in percentages. For statistical analysis of the obtained data, Spearman's rho test was used to verify the correlation between biomarkers, as well as between biomarkers and quantitative clinical variables. To study the association between pre-transplant biomarker levels and qualitative clinical variables, the Mann–Whitney U test or the Kruskal–Wallis test was used, depending on whether two groups or more than two groups were compared, respectively. To assess whether there were significant differences in PIVKA-II and AFP levels between the groups before and after transplantation, the Wilcoxon signed-rank test for related samples was performed. Receiver Operating Characteristic (ROC) analysis was performed and the Area Under the Curve (AUC) was estimated to study the predictive efficacy of pre-transplant PIVKA-II and AFP values for post-transplant relapse. The cut-off point for these markers with the best sensitivity and specificity, corresponding to the maximum Youden index, was determined. Multimarker analysis was performed by binary logistic regression by the method of introduction. A pooled ROC analysis was then performed to determine whether additional predictive power could be achieved. IBM® SPSS® Statistics 23.0 software (SPSS, Chicago, Illinois, USA) was used for statistical analysis, considering values of p ≤ 0.05 statistically significant.
Ethics approval and consent to participate
The study was approved by the Clinical Research Ethics Committee of HCUVA and HUCA hospitals and the subjects gave their written informed consent. All procedures were in accordance with the ethical standards of the institutional and national research committees, as well as with the 1964 Helsinki Declaration and its later amendments.
Results
The general characteristics of the study population for all patients are shown in Table 1. The median follow-up was 57 months (IQR 4.5–76.5 months), with a minimum follow-up time of 2 months and a maximum follow-up time of 84 months.
Table 1.
Baseline and pathologic characteristics of 46 patients with HCC on the waiting list for LT. Variables are represented by median and interquartile range or by frequency and percentage, as appropriate.
| No. of patients | 46 |
| Age (years) | 60 (55–63) |
| No. of tumors | 2 (1–3) |
| Tumor size | 2.6 cm (2–4.6) |
| MELD score | 9 (8–12) |
| No. of preoperative TACEs | 1 (0–2) |
| Sex | n = 46 |
| Male | 41 (89.1%) |
| Female | 5 (10.9%) |
| Etiology | n = 46 |
| Viral (%) | 18 (39.13%) |
| Non-viral (%) | 18 (39.13%) |
| Mixed (viral + non-viral) (%) | 10 (21.74%) |
| Child–Pugh score | n = 32 |
| A | 20 (62.5%) |
| B | 9 (28.1%) |
| C | 3 (9.4%) |
| Tumor size | n = 46 |
| ≤ 3 cm | 28 (60.9%) |
| > 3 cm | 18 (39.1%) |
| MELD score | n = 43 |
| ≤ 9 | 24 (55.8%) |
| > 9 | 19 (44.2%) |
| Preoperative TACES | n = 46 |
| Yes | 31 (67.4%) |
| No | 15 (32.6%) |
| Vascular invasion | n = 31 |
| Yes | 4 (12.9%) |
| No | 27 (87.1%) |
| Tumoral necrosis | n = 36 |
| Yes | 22 (61.1%) |
| No | 14 (38.9%) |
| Recurrence | n = 35 |
| Yes | 4 (11.43%) |
| No | 31 (88.57%) |
| Post-transplant death | n = 35 |
| Yes | 7 (20%) |
| No | 28 (80%) |
HCC hepatocellular carcinoma, MELD model for end-stage liver disease.
The correlations between PIVKA-II and AFP with clinicopathological variables are shown in Table 2. We observed statistically significant differences in pre-transplant PIVKA-II and AFP values between the group with a diameter of the largest tumour lesion at diagnosis ≤ 3 cm and the group with lesions > 3 cm, such that patients with a tumour size > 3 cm had significantly higher serum PIVKA-II and AFP levels than those with a tumour size < 3 cm. Furthermore, we found statistically significant differences in AFP levels between the different Child–Pugh groups, with patients in the Child C group having significantly higher AFP levels than patients in the Child A and B groups (p = 0.035). Finally, pre-transplant PIVKA-II and AFP levels were not significantly associated with the aetiology of the underlying liver disease, neither when analyzing individual etiologies [PIVKA-II (X2 = 15.288; p = 0.083); AFP (X2 = 10.441; p = 0.316)] nor when analyzing etiologies in different groups: viral, non-viral or mixed [PIVKA-II (X2 = 2.059; p = 0.357); AFP (X2 = 2.157; p = 0.340)].
Table 2.
Correlation between serum biomarkers levels and clinicopathological characteristics using Spearman test.
| PIVKA-II (mAU/mL) | AFP (ng/mL) | |
|---|---|---|
| Age | 0.100 (p = 0.508) | 0.135 (p = 0.372) |
| No. of tumors | 0.174 (p = 0.248) | 0.206 (p = 0.169) |
| Tumor size | 0.423 (p = 0.003) | 0.189 (p = 0.208) |
| Number of preoperative TACEs | 0.372 (p = 0.011) | 0.130 (p = 0.391) |
| MELD score | − 0.020 (p = 0.900) | 0.075 (p = 0.633) |
| PIVKA-II (mAU/mL) | – | 0.273 (p = 0.067) |
| AFP (ng/mL) | 0.273 (p = 0.067) | – |
Significant values are in [bold].
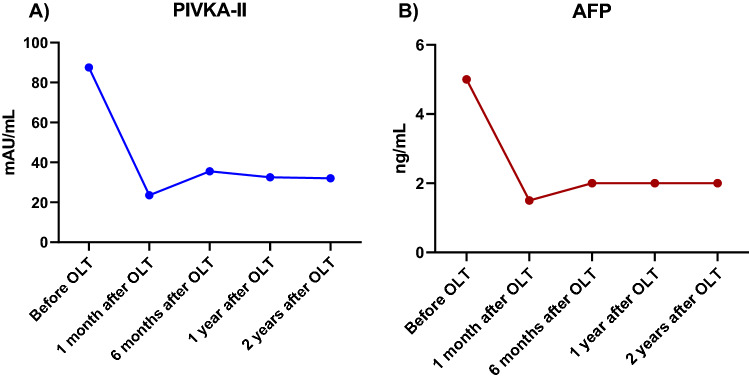
Table 3 shows the median values of PIVKA-II and AFP at the different times studied, before and after transplantation. In the analysis of the evolution of the biomarkers after transplantation (Fig. 1), PIVKA-II levels experienced a statistically significant decrease at 1 month (Z = − 4.042; p < 0.001), 6 months (Z = − 2.814; p = 0.005) and one year post-transplantation (Z = − 2.315; p = 0.021). AFP levels decreased significantly at 1 month (Z = − 4.262, p < 0.001), 1 year (Z = − 3.257, p = 0.001) and 2 years post-transplant (Z = − 3.436, p = 0.001).
Table 3.
Median levels of PIVKA-II and AFP in serum of HCC patients before and after transplantation.
| Tumor marker | Sample | ||||
|---|---|---|---|---|---|
| Before OLT | 1 month after OLT | 6 months after OLT | 1 year after OLT | 2 years after OLT | |
| PIVKA-II (mAU/mL) | |||||
| Median | 62 | 23.50 | 35.50 | 32.50 | 32 |
| IQR | 30.75–227.75 | 14.75–35.75 | 26.50–37.75 | 24–41.25 | 23–53.75 |
| AFP (ng/mL) | |||||
| Median | 5 | 1.50 | 2 | 2 | 2 |
| IQR | 2.75–6.25 | 1–2.50 | 1–2.75 | 1–3.25 | 1–5 |
OLT orthotopic liver transplant, IQR interquartile range.
Figure 1.
Evolution of median levels of PIVKA-II and AFP after OLT in patients with HCC. OLT orthotopic liver transplant.
Four patients had recurrence, ascertained by imaging, after LT (patients 7, 13, 19 and 23), who eventually died of disease progression. A total of 7 patients died after liver transplantation for various causes. Of the 3 patients who did not relapse, one died after several re-interventions related to biliary stenosis with associated liver abscess, one from a liver abscess leading to septic shock and the last from a cardiovascular event. Pre- and post-transplant PIVKA-II and AFP levels in patients with recurrence are shown in Table 4.
Table 4.
PIVKA-II and AFP levels in patients with recurrence after transplantation.
| Biomarker | Sample | Patient 7 | Patient 13 | Patient 19 | Patient 23 |
|---|---|---|---|---|---|
| PIVKA-II (mAU/mL) | Before OLT | 596 | 19 | 725 | 71 |
| 1 month after OLT | 17 | 112 | 52 | 33 | |
| 6 months after OLT | 271 | 45 | 4780 | 36 | |
| 1 year after OLT | – | – | 75,000 | 1915 | |
| 2 years after OLT | – | – | – | 75,000 | |
| AFP (ng/mL) | Before OLT | 3 | 253 | 11 | 4 |
| 1 month after OLT | 4 | 9 | 2 | 1 | |
| 6 months after OLT | 93 | 17 | 108 | 2 | |
| 1 year after OLT | – | – | 163 | 2 | |
| 2 years after OLT | – | – | – | 3 |
OLT orthotopic liver transplant.
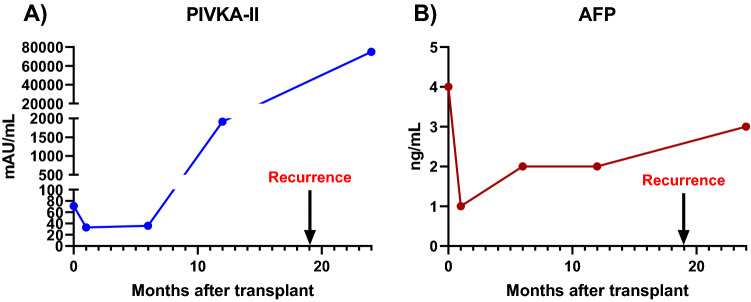
Figure 2 shows an example of variations in tumour marker concentration in a male patient whose age at diagnosis was 47 years and who underwent LT for HCC, the aetiology of which was mixed (HCV and alcoholism). Preoperative PIVKA-II and AFP levels in this patient were 71 mAU/mL and 4 ng/mL, respectively. In this patient, PIVKA-II levels increased sharply at one year post-transplant (1915 mAU/mL) with no elevation of AFP (2.0 ng/mL). AFP levels remained within baseline values at 2 years post-transplant (3 ng/mL) while PIVKA-II increased sharply to 75,000 mAU/mL. This patient was diagnosed with intrahepatic and bone relapse 19 months post-LT.
Figure 2.
Evolution of PIVKA-II and AFP levels after OLT in patient 23. OLT orthotopic liver transplant.
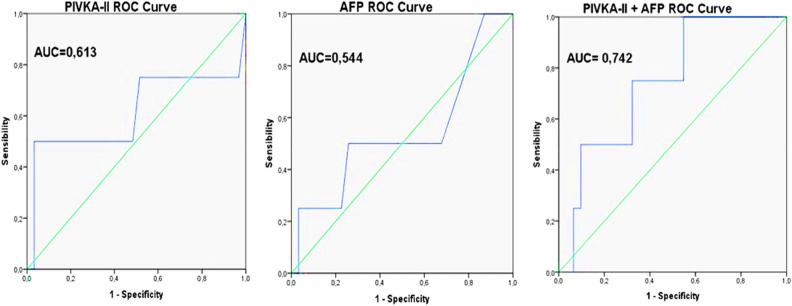
As shown in Fig. 3, the AUC for determining the post-transplant recurrence/metastasis predictive efficacy of pre-transplant levels of the biomarkers studied was 0.613 (95% CI 0.220–1 and p = 0.468) for PIVKA-II and 0.544 (95% CI 0.206–0.883 and p = 0.776) for AFP. The best PIVKA-II cut-off point for predicting post-transplant recurrence/metastasis with best sensitivity and specificity, corresponding to the maximum Youden index, was established at ≥ 592 mAU/mL, with a sensitivity of 50% and a specificity of 96.8%. For AFP, the best cut-off point for predicting post-transplant recurrence/metastasis with the best sensitivity and specificity was ≥ 9.65 ng/mL, with a sensitivity of 50% and a specificity of 74.2%. After constructing a binary logistic regression model to study the prediction of recurrence of the combination formed by PIVKA-II and AFP and analysing the AUC of this combination of markers using a ROC curve, an AUC of 0.742 (95% CI 0.520–0.964) was found, although these results were not statistically significant (p = 0.120).
Figure 3.
ROC curves of PIVKA-II, AFP and PIVKA-II + AFP.
Discussion
HCC is one of the leading causes of cancer-related mortality. Despite strict selection criteria, recurrence occurs in 6–18% transplanted HCC patients15. The main reason for this is the presence of residual micrometastases formed even before transplantation, or the spread of tumour cells from the original tumour into the bloodstream during surgical manipulation16. Sometimes patients experience extrahepatic metastases even when no primary lesion is found after surgical resection or liver transplantation. In addition, extrahepatic metastases may occur after locoregional therapies for early stage HCC17. Serum markers for both early diagnosis of patients at high risk for HCC and early detection of recurrence after transplantation are of great importance as they offer the opportunity to decrease patient mortality and reduce medical costs. Although the role of PIVKA-II has been widely studied in the diagnosis and prognosis of HCC, as well as in the evaluation of surgical treatments such as TACE, there are hardly any studies in the literature that have explored the role of PIVKA-II in the follow-up of patients after LT for HCC.
Regarding the different underlying aetiologies of liver disease in the patients included in our study, HCV is the predominant aetiology, accounting for 34.8% of patients. Overall, taking into account also the combined aetiologies, more than half of the patients had HCV, with this aetiology accounting for 56.5% of the cases. Our results are similar to those of other studies in HCC patients in which HCV is also the predominant aetiology18–20. Unlike hepatitis B infection, there is no vaccine for HCV21; however, the prevalence of both factors is decreasing due to vaccination of newborns against HBV and the existence of effective treatments for carriers of HBV and HCV22. Although some studies have suggested that PIVKA-II and AFP levels are associated with the aetiology of liver disease23,24, we did not find significant differences, indicating that the serum levels of the biomarkers analyzed are independent of the etiology of liver disease, in agreement with the findings of Sharman et al.25.
When studying the association of pre-transplant PIVKA-II levels with Child–Pugh classification, in our study no statistically significant differences between the different groups were found, so that PIVKA-II levels are independent of the Child–Pugh class to which the patient belongs. Our results are in concordance with those of Saito et al. who also found no significant association between serum PIVKA-II level and Child–Pugh score before treatment with TACE26. In contrast, we did find significant differences in serum AFP levels between the different groups of Child–Pugh patients, with Child–Pugh class C patients having significantly higher AFP levels than those in classes A and B, in agreement with previous studies27. This finding confirms the ability of AFP to reflect the severity of liver dysfunction in patients with HCC.
After evaluating the association between PIVKA-II and the different clinicopathological parameters of the patients in our study, it was found that patients with larger tumor size had higher levels of PIVKA-II, which suggests that the serum concentration of this biomarker may play an important role in predicting disease severity, such that a higher PIVKA-II concentration may indicate larger tumour volume and worse clinical stage. This correlation has also been observed in other studies in patients diagnosed with HCC, but not on the OLT waiting list28–31. PIVKA-II would be a better biomarker for predicting tumor size in HCC than AFP, since although patients with a tumor size > 3 cm had higher serum levels of both biomarkers, AFP did not correlate with tumor size, whereas PIVKA-II did have a statistically significant positive correlation with tumor size. Therefore, we believe that the combination of the levels of both markers would be a better predictor of clinical tumor parameters, such as tumor size, than the determination of only one of them. However, in our study, neither serum PIVKA-II nor AFP levels correlated with the number of tumours, in line with other studies such as that of Feng et al. who found no correlation between serum PIVKA-II levels and the number of tumours30, or Lapinski et al. who also found no significant association between serum AFP levels and the number of tumour nodules32.
Most of the patients enrolled in the study underwent at least one TACE before liver transplantation. TACE is an effective treatment in patients with unresectable HCC, however most patients treated with TACE will need repeat therapy due to partial response or tumor recurrence. Treatment outcomes after TACE depend on both the severity of underlying liver dysfunction and tumor burden33. In our study, pre-transplant PIVKA-II levels correlated with the number of TACEs performed prior to pre-transplant sampling. This result suggests that those patients who received multiple treatments with the intention of reducing the tumor to carry out the transplant had more advanced HCC and a worse clinical stage. Today, the benefits of repeating this treatment are unclear, since on the one hand it does reduce the size of the tumour, but at the same time it could favour tumour spread and local inflammation. Li et al. showed that residual liver cancer cells and normal liver tissue undergo changes in gene expression after TACE, so that the possibility of recurrence and metastasis of residual HCC cells increases after TACE34. Furthermore, remnants of normal liver tissue can lead to HCC recurrence, due to cirrhosis and increased compensatory hyperplasia and proliferative activity after TACE. In addition, several previous studies have shown that the establishment of collateral circulation after TACE is an important factor for HCC recurrence and metastasis, which can lead to tumour cell growth with high metastatic potential35. Serum AFP levels, in contrast, did not correlate significantly with the number of pre-transplant TACES.
After studying the association between serum PIVKA-II and AFP levels of the patients included in the study, they did not correlate with each other, in agreement with other studies in which, even dealing with HCC patients, they were not candidates for OLT36–38. The found results reflect that these two biomarkers are independent of each other, which could be explained by the different synthesis pathways of the two markers in hepatoma cells39. Both biomarkers may reflect the tumour burden of HCC patients40, and may be complementary markers in terms of their clinical utility41.
Ideally, tumour marker levels should fall within a reference range after effective treatment, and rise before imaging studies detect tumour relapse36. The exact mechanism by which PIVKA-II is produced by the tumour remains unclear, but the normalisation of PIVKA-II levels after curative treatment of HCC, such as liver resection, clearly indicates that the tumour is the source of its production42. In our study, we observed that both PIVKA-II and AFP decreased significantly between pre-transplant and post-transplant values, in agreement with previous studies, such as that of Feng et al., in which serum levels of PIVKA-II and AFP decreased significantly after liver resection30. Specifically, in the patients in our study, PIVKA-II shows a statistically significant decrease at 1 month, 6 months and 1 year post-transplantation. In contrast, at 2 years and 3 years post-transplant, we did not find a significant decrease in the levels of this marker. It is important to note that PIVKA-II levels may be elevated in certain situations other than HCC, for example in cases of biliary obstruction11. Also the level of PIVKA-II can be strongly influenced by drugs such as rifampicin, vitamin K deficiency (e.g. due to malnutrition in cirrhotic patients) and antivitamin K drugs (e.g. anticoagulants such as acenocoumarol and warfarin)42. However, PIVKA-II elevations in patients in our study who did not have post-transplant tumour recurrence were not associated with any specific cause, as none of these patients were found to be on treatment with the aforementioned drugs or to have vitamin K deficiency or obstructive jaundice. AFP levels were significantly lower at 1 month, 1 year and 2 years post-transplantation. Considering that tumour growth patterns are highly variable among individuals, there is probably no single perfect biomarker for HCC monitoring after transplantation; therefore, the combination of biomarkers might be more informative than any single biomarker alone43.
Patient 13 was found to have recurrence 6 months after transplantation. PIVKA-II levels in this patient increased at 1 month after OLT, with respect to pretransplant levels, and decreased at 6 months post-transplant, coinciding approximately with the time at which the recurrence was detected by imaging. This patient probably developed tumor recurrence around one month after OLT, so that PIVKA-II would be indicating post-transplant recurrence before imaging tests, such as computed tomography (CT) or magnetic resonance imaging (MRI). However, these levels decreased again at 6 months after transplantation, when HCC recurrence and extrahepatic metastases were detected by imaging, so we cannot affirm that the elevation of PIVKA-II at one month post-transplant was caused by tumor recurrence, even though other causes of PIVKA elevation, already mentioned above, were ruled out, such as the use of anticoagulant antivitamin K drugs. In patients 7 and 19 in our study, the evolution of PIVKA II levels after OLT follows an ideal pattern, in which these levels decreased at 1 month post-transplant with respect to pre-transplant values, reflecting that the diseased liver of HCC patients is the source of production of this abnormal prothrombin molecule, and increased considerably at 6 months post-transplant, coinciding approximately with the detection of tumor recurrence by imaging in both patients. In the case of patient 23, PIVKA-II levels increased abruptly, even before the detection of tumour recurrence by imaging, while AFP levels remained within the reference range. This is in line with the study by Nanashima et al., who showed that changes in PIVKA-II levels after treatment, including hepatectomy and ablation therapy, tended to be more reflective of tumour recurrence than changes in AFP level44. Therefore, according to our findings, and despite its limitations, PIVKA-II could be a good marker in the study of progression after liver transplantation, complementing AFP.
After evaluating the predictive ability of pre-transplant AFP and PIVKA-II levels to predict post-transplant recurrence, we found that PIVKA-II was a better predictor of recurrence than AFP, with a PIVKA-II AUC of 0.613 versus AFP AUC of 0.544. Our results are consistent with previous studies18,45–47, in which PIVKA-II was also a better predictor of post-transplant recurrence than AFP. This is biologically feasible because PIVKA-II binds to vascular endothelial growth factor receptor 2 and induces autophosphorylation of the receptor and downstream effectors, including phospholipase C-Y and mitogen-activated protein kinase, promoting endothelial cell proliferation and migration. However, AFP is a product of tumour cells and has no biological effect on promoting tumour growth48. Combining pre-transplant levels of PIVKA-II and AFP for prediction of post-transplant recurrence increased the AUC to 0.742 with increased sensitivity (100%) but decreased specificity (45.2%). Our results are in partial agreement with other authors such as Chon et al. in whose study sensitivity, but also specificity, were simultaneously improved when both AFP and PIVKA-II levels were measured (sensitivity, 66.7%; specificity, 47.9%) compared to those obtained when only AFP levels were measured (sensitivity 60.1% and specificity 45.2%) or PIVKA-II levels alone (sensitivity 62.9% and specificity 47.9%)49. Lee et al. also demonstrated that the combination of AFP and PIVKA-II was a better predictor of recurrence after transplantation in advanced HCC than either marker alone50. Thus, this combination of markers could improve the ability of each marker alone to identify patients most likely to have post-transplant recurrence, although the results were also not statistically significant (p > 0.05). The number of patients was a limitation of these studies due to two factors: on the one hand, patients must meet a series of strict requirements to be on the waiting list and be candidates for transplantation, and in addition, there must be a donor with an organ compatible with the recipient. The other limitation is the moderate post-transplant recurrence rate of 6–18%, both of which contribute to severely limit the cases under study. In this context, the results of this study may be useful for the development of new lines of research that provide new evidence for PIVKA-II to be incorporated as a useful biomarker in the management of HCC in the clinical laboratory, as occurs in countries such as Japan, where together with ultrasound and lens culinaris agglutinin-reactive fraction of AFP (AFP-L3), it is used in the screening of at-risk patients every 6 months51.
Conclusions
Pre-transplant PIVKA-II concentration in peripheral blood in patients with HCC is significantly associated with clinical factors such as larger tumour size and the number of TACEs performed before transplantation, however the levels of this biomarker are independent of the aetiology of the underlying liver disease. According to the results of the present study, high levels of this tumour marker could play an important role in predicting disease severity by indicating larger tumour volume and worse clinical stage.
Monitoring PIVKA-II levels in HCC transplant recipients reflects the tumor early recurrence after transplantation and could be used, complementing AFP and imaging tests, as a novel biomarker of this pathology. Despite not reaching statistical significance, pre-transplant levels of PIVKA-II are better predictors of post-transplant recurrence than AFP, and the use of these biomarkers together may improve the predictive ability of using AFP alone. Althogh PIVKA-II is already included in clinical practice guidelines in some Asian countries52–54, there are practically no published studies on the role of PIVKA-II in the follow-up of HCC after liver transplantation in Western countries. Our findings place PIVKA-II as a promising worldwide marker, serving as a basis for future large-scale studies or meta-analyses that can strengthen its usefulness in clinical practice.
Abbreviations
- AFP
Alpha-fetoprotein
- AFP-L3
lens culinaris Agglutinin-reactive fraction of AFP
- ALCH
Alcoholism
- AUC
Area under the curve
- CRIPTO
Cryptogenic
- CT
Computed tomography
- DCP
Des gamma-carboxyprothrombin
- Fe
Iron overload
- HBV
Hepatitis B virus
- HCC
Hepatocellular carcinoma
- HCUVA
Virgen de la arrixaca hospital
- HCV
Hepatitis C virus infection
- HEMO
Haemochromatosis
- HUCA
Asturias Central Hospital
- IQR
Interquartile range
- JSH
Japanese Society of Hepatology
- LT
Liver transplantation
- MELD
Model for end-stage liver disease
- MRI
Magnetic resonance imaging
- NASH
Non-alcoholic steatosis
- OLT
Orthotopic liver transplant
- PET/CT
Positron emission tomography computed tomography
- PIVKA-II
Protein induced by vitamin K absence or antagonist-II
- ROC
Receiver operating characteristic
- TACE
Transarterial chemoembolization
Author contributions
F.V. and M.I.S. called the patients for the extraction of the samples and collected the analytical and clinical data. F.V. performed the statistical analysis and data analysis. F.V. and L.F.S. drafted the manuscript. A.B. and V.D.L.O. reviewed the article. All authors have read and approved the final manuscript.
Funding
The work was supported by the following funded research projects: 1: Usefulness of CTC, PETTAC and dynamic MRI with gadoxetic acid to predict the efficacy of transarterial chemoembolization in hepatocellular carcinoma awaiting transplantation. Carlos III Institute (PI13/01195). 2: Usefulness of CTCs, PIVKA II and PET-CT levels to predict the efficacy of transarterial chemoembolization in hepatocarcinoma awaiting transplantation. Seneca Foundation, Regional Science and Technology Agency (19447/PI/14). 3: Long-term prognostic assessment of the detection and characterization of CTC by microfluidic liquid biopsy in patients with hepatocarcinoma on the liver transplant waiting list (PI18/01302).
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Francisco Villalba López, Luis Francisco Sáenz Mateos, Alberto Baroja Mazo and Pablo Ramírez Romero.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Villanueva A. Hepatocellular carcinoma. N. Engl. J. Med. 2019;380(15):1450–1462. doi: 10.1056/NEJMra1713263. [DOI] [PubMed] [Google Scholar]
- 3.Ogunwobi OO, Harricharran T, Huaman J, Galuza A, Odumuwagun O, Tan Y, et al. Mechanisms of hepatocellular carcinoma progression. World J. Gastroenterol. 2019;25(19):2279–2293. doi: 10.3748/wjg.v25.i19.2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forner A, Vilana R, Ayuso C, Bianchi L, Solé M, Ayuso JR, et al. Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: Prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology. 2008;47:97–104. doi: 10.1002/hep.21966. [DOI] [PubMed] [Google Scholar]
- 5.Di Bisceglie AM, Sterling RK, Chung RT, Everhart JE, Dienstag JL, Bonkovsky HL, et al. Serum alpha-fetoprotein levels in patients with advanced hepatitis C: Results from the HALT-C Trial. J. Hepatol. 2005;43:434–441. doi: 10.1016/j.jhep.2005.03.019. [DOI] [PubMed] [Google Scholar]
- 6.Lok AS, Lai CL. Alpha-Fetoprotein monitoring in Chinese patients with chronic hepatitis B virus infection: Role in the early detection of hepatocellular carcinoma. Hepatology. 1989;9:110–115. doi: 10.1002/hep.1840090119. [DOI] [PubMed] [Google Scholar]
- 7.Ramirez P, Sáenz L, Cascales-Campos PA, González Sánchez MR, Llàcer-Millán E, Sánchez-Lorencio MI, et al. Oncological evaluation by positron-emission tomography, circulating tumor cells and alpha fetoprotein in patients with hepatocellular carcinoma on the waiting list for liver transplantation. Transpl. Proc. 2016;48:2962e5. doi: 10.1016/j.transproceed.2016.07.035. [DOI] [PubMed] [Google Scholar]
- 8.Sánchez-Lorencio MI, Saenz L, Ramirez P, Villalba-López F, de la Orden V, Mediero-Valeros B, Revilla Nuin B, Gonzalez MR, Cascales-Campos PA, Ferreras-Martínez D, et al. Matrix metal- loproteinase 1 as a novel biomarker for monitoring hepatocellular carcinoma in liver transplant patients. Transpl. Proc. 2018;50:623–627. doi: 10.1016/j.transproceed.2017.11.061. [DOI] [PubMed] [Google Scholar]
- 9.Xing H, Zheng YJ, Han J, Zhang H, Li ZL, Lau WY, Shen F, Yang T. Protein induced by vitamin K absence or antagonist-II versus alpha-fetoprotein in the diagnosis of hepatocellular carcinoma: A systematic review with meta-analysis. Hepatobiliary Pancreat. Dis. Int. 2018;17:487–495. doi: 10.1016/j.hbpd.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Lefrere JJ, Gozin D. Use of des-gamma-carboxyprothrombin in retrospective diagnosis of hidden intoxication of anticoagulants. J. Clin. Pathol. 1987;40(5):589. doi: 10.1136/jcp.40.5.589-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park MS, Lee KW, Kim H, Choi YR, Hong G, Yi NJ, et al. Usefulness of PIVKA-II after living-donor liver transplantation for hepatocellular carcinoma. Transpl. Proc. 2017;49:1109–1113. doi: 10.1016/j.transproceed.2017.03.017. [DOI] [PubMed] [Google Scholar]
- 12.Matsubara M, Shiraha H, Kataoka J, Iwamuro M, Horiguchi S, Nishina S, et al. Des-gamma-carboxyl prothrombin is associated with tumor angiogenesis in hepatocellular carcinoma. J. Gastroenterol. Hepatol. 2012;27:1602e8. doi: 10.1111/j.1440-1746.2012.07173.x. [DOI] [PubMed] [Google Scholar]
- 13.Izumi N. Diagnostic and treatment algorithm of the Japanese society of hepatology: A consensus-based practice guideline. Oncology. 2010;78(Suppl 1):78–86. doi: 10.1159/000315234. [DOI] [PubMed] [Google Scholar]
- 14.Kudo M, Izumi N, Kokudo N, Matsui O, Sakamoto M, Nakashima O, et al. Management of hepatocellular carcinoma in Japan: Consensus-based clinical practice guidelines proposed by the Japan Society of Hepatology (JSH) 2010 updated version. Dig. Dis. 2011;29:339–364. doi: 10.1159/000327577. [DOI] [PubMed] [Google Scholar]
- 15.Au KP, Chok KSH. Multidisciplinary approach for post-liver transplant recurrence of hepatocellular carcinoma: A proposed management algorithm. World J. Gastroenterol. 2018;24(45):5081–5094. doi: 10.3748/wjg.v24.i45.5081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah SA, Greig PD, Gallinger S, Cattral MS, Dixon E, Kim RD, et al. Factors associated with early recurrence after resection for hepatocellular carcinoma and outcomes. J. Am. Coll. Surg. 2006;202(2):275–283. doi: 10.1016/j.jamcollsurg.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 17.Bae HM, Lee JH, Yoon JH, Kim YJ, Heo DS, Lee HS. Protein induced by vitamin K absence or antagonist-II production is a strong predictive marker for extrahepatic metastases in early hepatocellular carcinoma: A prospective evaluation. BMC Cancer. 2011;10(11):435. doi: 10.1186/1471-2407-11-435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shindoh J, Sugawara Y, Nagata R, et al. Evaluation methods for pretransplant oncologic markers and their prognostic impacts in patient undergoing living donor liver transplantation for hepatocellular carcinoma. Transpl. Int. 2014;27(4):391–398. doi: 10.1111/tri.12274. [DOI] [PubMed] [Google Scholar]
- 19.Shirabe K, Aishima S, Taketomi A, Soejima Y, Uchiyama H, Kayashima H, et al. Prognostic importance of the gross classification of hepatocellular carcinoma in living donor-related liver transplantation. Br. J. Surg. 2011;98(2):261–267. doi: 10.1002/bjs.7311. [DOI] [PubMed] [Google Scholar]
- 20.Takada Y, Uemoto S. Liver transplantation for hepatocellular carcinoma: The Kyoto experience. J. Hepatobiliary Pancreat. Sci. 2010;17(5):527–532. doi: 10.1007/s00534-009-0162-y. [DOI] [PubMed] [Google Scholar]
- 21.Caines A, Selim R, Salgia R. The changing global epidemiology of hepatocellular carcinoma. Clin. Liver Dis. 2020;24(4):535–547. doi: 10.1016/j.cld.2020.06.001. [DOI] [PubMed] [Google Scholar]
- 22.McGlynn KA, Petrick JL, El-Serag HB. Epidemiology of hepatocellular carcinoma. Hepatology. 2021;73(Suppl 1):4–13. doi: 10.1002/hep.31288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marrero JA, Su GL, Wei W, Emick D, Conjeevaram HS, Fontana RJ, et al. Des-gamma carboxyprothrombin can differentiate hepatocellular carcinoma from nonmalignant chronic liver disease in American patients. Hepatology. 2003;37(5):1114–1121. doi: 10.1053/jhep.2003.50195. [DOI] [PubMed] [Google Scholar]
- 24.Nakamura S, Nouso K, Sakaguchi K, Ito YM, Ohashi Y, Kobayashi Y, et al. Sensitivity and specificity of des-gamma-carboxy prothrombin for diagnosis of patients with hepatocellular carcinomas varies according to tumor size. Am. J. Gastroenterol. 2006;101(9):2038–2043. doi: 10.1111/j.1572-0241.2006.00681.x. [DOI] [PubMed] [Google Scholar]
- 25.Sharma B, Srinivasan R, Chawla YK, Kapil S, Saini N, Singla B, et al. Clinical utility of prothrombin induced by vitamin K absence in the detection of hepatocellular carcinoma in Indian population. Hepatol. Int. 2010;4(3):569–576. doi: 10.1007/s12072-010-9186-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saito M, Seo Y, Yano Y, Miki A, Yoshida M, Azuma T. A high value of serum des-γ-carboxy prothrombin before hepatocellular carcinoma treatment can be associated with long-term liver dysfunction after treatment. J. Gastroenterol. 2012;47(10):1134–1142. doi: 10.1007/s00535-012-0577-0. [DOI] [PubMed] [Google Scholar]
- 27.Qari YA, Mosli MH. Epidemiology and clinical features of patients with hepatocellular carcinoma at a tertiary hospital in Jeddah. Niger. J. Clin. Pract. 2017;20(1):43–47. doi: 10.4103/1119-3077.180062. [DOI] [PubMed] [Google Scholar]
- 28.Wang Q, Chen Q, Zhang X, Lu XL, Du Q, Zhu T, et al. Diagnostic value of gamma-glutamyltransferase/aspartate aminotransferase ratio, protein induced by vitamin K absence or antagonist II, and alpha-fetoprotein in hepatitis B virus-related hepatocellular carcinoma. World J. Gastroenterol. 2019;25(36):5515–5529. doi: 10.3748/wjg.v25.i36.5515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Durazo FA, Blatt LM, Corey WG, Lin JH, Han S, Saab S, et al. Des-gamma-carboxyprothrombin, alpha-fetoprotein and AFP-L3 in patients with chronic hepatitis, cirrhosis and hepatocellular carcinoma. J. Gastroenterol. Hepatol. 2008;23(10):1541–1548. doi: 10.1111/j.1440-1746.2008.05395.x. [DOI] [PubMed] [Google Scholar]
- 30.Feng H, Li B, Li Z, Wei Q, Ren L. PIVKA-II serves as a potential biomarker that complements AFP for the diagnosis of hepatocellular carcinoma. BMC Cancer. 2021;21(1):401. doi: 10.1186/s12885-021-08138-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gawad IAAE, Mossallam GI, Radwan NH, Elzawahry HM, Elhifnawy NM. Comparing prothrombin induced by vitamin K absence-II (PIVKA-II) with the oncofetal proteins glypican-3, Alpha feto protein and carcinoembryonic antigen in diagnosing hepatocellular carcinoma among Egyptian patients. J. Egypt Natl. Canc. Inst. 2014;26(2):79–85. doi: 10.1016/j.jnci.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 32.Łapiński TW, Tarasik A, Januszkiewicz M, Flisiak R. Clinical aspects and treatment of hepatocellular carcinoma in north-eastern Poland. Clin. Exp. Hepatol. 2021;7(1):79–84. doi: 10.5114/ceh.2021.104631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mishra G, Dev A, Paul E, Cheung W, Koukounaras J, Jhamb A, et al. Prognostic role of alpha-fetoprotein in patients with hepatocellular carcinoma treated with repeat transarterial chemoembolisation. BMC Cancer. 2020;20(1):483. doi: 10.1186/s12885-020-06806-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li HL, Ji WB, Zhao R, Duan WD, Chen YW, Wang XQ, et al. Poor prognosis for hepatocellular carcinoma with transarterial chemoembolization pre-transplantation: Retrospective analysis. World J. Gastroenterol. 2015;21(12):3599–3606. doi: 10.3748/wjg.v21.i12.3599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li Z, Hu DY, Chu Q, Wu JH, Gao C, Zhang YQ, et al. Cell apoptosis and regeneration of hepatocellular carcinoma after transarterial chemoembolization. World J. Gastroenterol. 2004;10(13):1876–1880. doi: 10.3748/wjg.v10.i13.1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yamamoto K, Imamura H, Matsuyama Y, Kume Y, Ikeda H, Norman GL, et al. AFP, AFP-L3, DCP, and GP73 as markers for monitoring treatment re- sponse and recurrence and as surrogate markers of clinicopathological vari- ables of HCC. J. Gastroenterol. 2010;45:1272–1282. doi: 10.1007/s00535-010-0278-5. [DOI] [PubMed] [Google Scholar]
- 37.Choi JY, Jung SW, Kim HY, Kim M, Kim Y, Kim DG, et al. Diagnostic value of AFP-L3 and PIVKA-II in hepatocellular carcinoma according to total-AFP. World J. Gastroenterol. 2013;19(3):339–346. doi: 10.3748/wjg.v19.i3.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gentile I, Buonomo AR, Scotto R, Zappulo E, Carriero C, Piccirillo M, et al. Diagnostic accuracy of PIVKA-II, alpha-fetoprotein and a combination of both in diagnosis of hepatocellular carcinoma in patients affected by chronic HCV infection. In Vivo. 2017;31(4):695–700. doi: 10.21873/invivo.11115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Loglio A, Iavarone M, Facchetti F, Di Paolo D, Perbellini R, Lunghi G, et al. The combination of PIVKA-II and AFP improves the detection accuracy for HCC in HBV caucasian cirrhotics on long-term oral therapy. Liver Int. 2020;40(8):1987–1996. doi: 10.1111/liv.14475. [DOI] [PubMed] [Google Scholar]
- 40.Park H, Park JY. Clinical significance of AFP and PIVKA-II responses for monitoring treatment outcomes and predicting prognosis in patients with hepatocellular carcinoma. Biomed. Res. Int. 2013;2013:310427. doi: 10.1155/2013/310427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Suh SW, Choi YS. Predictors of micrometastases in patients with barcelona clinic liver cancer classification b hepatocellular carcinoma. Yonsei Med. J. 2017;58(4):737–742. doi: 10.3349/ymj.2017.58.4.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lai Q, Iesari S, Levi Sandri GB, Lerut J. Des-gamma-carboxy prothrombin in hepatocellular cancer patients waiting for liver transplant: A systematic review and meta-analysis. Int. J. Biol. Markers. 2017;32(4):e370–e374. doi: 10.5301/ijbm.5000276. [DOI] [PubMed] [Google Scholar]
- 43.Choi J, Lee D, Shim JH, Kim KM, Lim YS, Lee YS, et al. Evaluation of transarterial chemoembolization refractoriness in patients with hepatocellular carcinoma. PLoS ONE. 2020;15(3):e0229696. doi: 10.1371/journal.pone.0229696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nanashima A, Taura N, Abo T, Ichikawa T, Sakamoto I, Nagayasu T, et al. Tumor marker levels before and after curative treatment of hepatocellular carcinoma as predictors of patient survival. Dig. Dis. Sci. 2011;56(10):3086–3100. doi: 10.1007/s10620-011-1796-6. [DOI] [PubMed] [Google Scholar]
- 45.Shirabe K, Itoh S, Yoshizumi T, Soejima Y, Taketomi A, Aishima S, Maehara Y. The predictors of microvascular invasion in candidates for liver transplantation with hepatocellular carcinoma-with special reference to the serum levels of des-gamma-carboxy prothrombin. J. Surg. Oncol. 2007;95:235–240. doi: 10.1002/jso.20655. [DOI] [PubMed] [Google Scholar]
- 46.Taketomi A, Sanefuji K, Soejima Y, Yoshizumi T, Uhciyama H, Ikegami T, Harada N, Yamashita Y, Sugimachi K, Kayashima H, Iguchi T, Maehara Y. Impact of des-gamma-carboxy prothrombin and tumor size on the recurrence of hepatocellular carcinoma after living donor liver transplantation. Transplantation. 2009;87:531–537. doi: 10.1097/TP.0b013e3181943bee. [DOI] [PubMed] [Google Scholar]
- 47.Fujiki M, Takada Y, Ogura Y, Oike F, Kaido T, Teramukai S, et al. Significance of des-gamma-carboxy prothrombin in selection criteria for living donor liver transplantation for hepatocellular carcinoma. Am. J. Transpl. 2009;9(10):2362–2371. doi: 10.1111/j.1600-6143.2009.02783.x. [DOI] [PubMed] [Google Scholar]
- 48.Chaiteerakij R, Zhang X, Addissie BD, Mohamed EA, Harmsen WS, Theobald PJ, Peters BE, Balsanek JG, Ward MM, Giama NH, Moser CD, Oseini AM, Umeda N, Venkatesh S, Harnois DM, Charlton MR, Yamada H, Satomura S, Algeciras-Schimnich A, Snyder MR, Therneau TM, Roberts LR. Combinations of biomarkers and Milan criteria for predicting hepatocellular carcinoma recurrence after liver transplantation. Liver Transpl. 2015;21:599–606. doi: 10.1002/lt.24117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chon YE, Choi GH, Lee MH, Kim SU, Kim DY, Ahn SH, et al. Combined measurement of preoperative α-fetoprotein and des-γ-carboxy prothrombin predicts recurrence after curative resection in patients with hepatitis-B-related hepatocellular carcinoma. Int. J. Cancer. 2012;131(10):2332–2341. doi: 10.1002/ijc.27507. [DOI] [PubMed] [Google Scholar]
- 50.Lee HW, Song GW, Lee SG, Kim JM, Joh JW, Han DH, et al. Patient selection by tumor markers in liver transplantation for advanced hepatocellular carcinoma. Liver Transpl. 2018;24(9):1243–1251. doi: 10.1002/lt.25056. [DOI] [PubMed] [Google Scholar]
- 51.Singh G, Yoshida EM, Rathi S, Marquez V, Kim P, Erb SR, et al. Biomarkers for hepatocellular cancer. World J. Hepatol. 2020;12(9):558–573. doi: 10.4254/wjh.v12.i9.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, et al. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol. Int. 2010;4(2):439–474. doi: 10.1007/s12072-010-9165-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kokudo, N., Hasegawa, K., Akahane, M., Igaki, H., Izumi, N., Ichida, T., et al. Evidence-based clinical practice guidelines for hepatocellular carcinoma: The Japan Society of Hepatology 2013 update (3rd JSH-HCC Guidelines). Hepatol. Res.45(2). 10.1111/hepr.12464 (2015). [DOI] [PubMed]
- 54.Kumar A, Acharya SK, Singh SP, Saraswat VA, Arora A, Duseja A, et al. The Indian National Association for Study of the Liver (INASL) consensus on prevention, diagnosis and management of hepatocellular carcinoma in India: The Puri Recommendations. J. Clin. Exp. Hepatol. 2014;4(Suppl 3):S3–S26. doi: 10.1016/j.jceh.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.