Abstract
Aim:
The purpose of this study was to examine the trajectories of condition and independent living self-management in youth with spina bifida.
Methods:
A diverse sample of adolescents and young adults (AYA) with spina bifida (SB) completed the Adolescent/Young Adult Self-Management and Independence Scale (AMIS-II) across four time points. Parents reported on demographic characteristics including age, sex, race/ethnicity, and family income. Growth in self-management and its subscales (condition and independent living) were estimated using linear mixed effects models as a function of respondents’ demographics.
Results:
This study included 99 respondents age 18 to 27 years old. About half were female (52.5%) and White (52.5%); 15.2% were Black, and about a third were Hispanic/Latino (32.3%). Eighty-seven AYAs (87.9%) had myelomeningocele. The lesion level was 31.3% sacral, 48.5% lumbar, and 18.2% thoracic. A third of the families earned less than 50K. Overall, self-management growth was dependent on age, sex, and race/ethnicity, but not income. Growth in condition self-management depended on sex; only males demonstrated increasing growth (, p < .001). Black participants endorsed higher increasing total and condition self-management when compared to White ( and 0.17, respectively, both p < .05) and Hispanic/Latino ( and 0.21, respectively, both p = .02) respondents.
Conclusion:
This study provides evidence of differences in growth of self-management by demographic/social determinants of health. Possible reasons for differences are discussed. Predictors of changes in self-management behaviors over time in young adults with SB can identify subgroups in need of further study.
Keywords: adolescents, independence, self-management, spina bifida, trajectory, young adults
Spina bifida (SB) is a complex congenital condition involving the central nervous system, which results in secondary conditions and complications (Copp et al., 2015; National Institute of Neurological Disorders and Stroke [NINDS], 2013). Youth experience physical disabilities, orthopedic conditions, shunt surgeries, and alterations in bowel and bladder patterns, which require complex care regimens. Parents share responsibility for care with youth and may do so in varying amounts over adolescence and young adulthood; the long-term goal for most youth with SB is independent self-management.
Disparities exist among race/ethnicity in the prevalence of SB worldwide (Atta et al., 2016). Hispanics/Latinos living in the United States have a higher prevalence of SB (3.80 per 10,000 live births) than non-Hispanic Whites (3.09) and non-Hispanic Blacks (2.73) (Canfield et al., 2014). Unfortunately, with a few exceptions (e.g., Betz et al., 2010; Castillo et al., 2017), diverse samples in the study of self-management in SB are atypical. Indeed, Whites make up the majority of samples in the study of self-management and SB (i.e., 85% or more; Sawin et al., 2021). Therefore, little is known about self-management among non-White participants or possible differences in self-management behaviors across demographic groups.
Self-management is “an active daily and flexible process in which youth and their parents share responsibility and decision making for managing their condition, health, and well-being through a wide range of knowledge, attitudes, activities, and skills. The goal of this increasing responsibility is to develop skills needed for transition to adulthood and independent living” (Logan et al., 2020, p. 583; Sawin et al., 2009; Schilling et al., 2002). The process by which self-management develops includes knowledge and beliefs, self-regulation skills and abilities, and social facilitation as relevant correlates (Ryan & Sawin, 2009). Condition self-management includes activities and skills that prevent or manage complications (e.g., pressure injuries, bladder infections, renal disease) and reduce the effects of condition severity. Behaviors that fall within the condition self-management domain require knowledge of medical regimen and action to complete care tasks (i.e., intermittent catheterization, bowel management, use of assistive devices, and keeping appointments). Independent living self-management includes lifestyle activities such as household (e.g., laundry, preparing meals) and community living tasks (e.g., planning meals, deciding to do groceries), managing finances, and arranging transportation. Identifying the rate of independence across these domains over time provides an assessment of the acquisition of self-management behaviors (i.e., trajectory of condition self-management and independent living self-management). Trajectories provide a way to monitor the successful development of self-management as well as identify targets for intervention.
Grounded in the Individual and Family Self-Management Theory (Ryan & Sawin, 2009), individual (demographic and condition) characteristics are often proposed to be correlates of the process of self-management and the behavioral outcomes (Sawin et al., 2021). Although youth with SB gradually acquire increasing responsibility for their own care, emerging adults with SB (22–23 years of age) lag behind peers without SB in reaching developmental milestones including decision-making responsibility, educational and vocational achievement, financial independence, and independent living (< 30% live independently; Holmbeck & Kritikos, 2022). It is important to study both self-management and independence over time to better understand factors that foster healthy adolescent and young adult self-management in SB.
A useful instrument for the assessment of self-management behaviors is the Adolescent/Young Adult Self-Management and Independence Scale (AMIS-II), a validated measure for use in people with SB (Sawin et al., 2018). This measure captures the actual achievement of self-management behaviors, not an individual’s capacity to perform the skills. The measure provides a total (i.e., overall) score and subscale scores for condition and independent living self-management.
Few studies have evaluated demographic factors associated with self-management. Past evidence suggests that older age is associated with higher levels of self-management (Sawin et al., 2021). Less is known about the relationship between race/ethnicity and self-management in SB, since a third of the literature omits reporting race and only 16% report ethnicity (Sawin et al., 2021). Only three studies with small samples (< 100 participants) examined associations between race/ethnicity and self-management; none have found significant associations (Chowanadisai et al., 2013; Fremion et al., 2021; Ridosh et al., 2021). Although self-management did not differ by race/ethnicity, Chowanadisai et al. (2013) reported that the Hispanic participants had higher rates of bladder and bowel management complications (i.e., urinary incontinence rates, bladder accidents, and less satisfaction with bladder and bowel management). Another study found non-Hispanic Black males experience more incontinence, but did not evaluate self-management behaviors (Schechter et al., 2015). Further assessment of self-management behaviors by race/ethnicity may determine if Hispanics and non-Hispanic Black males are at greater risk with respect to the nature of their self-management trajectory when compared to other race/ethnicities.
Knowledge of sex differences across self-management behaviors within SB is also limited. In a study identifying correlates of independent use of intermittent self-catheterization, male gender was associated with a higher rate of self-management behaviors (Castillo et al., 2017). Males may eventually engage in more self-management, given that they experience more challenges with continence than females (Schechter et al., 2015). However, adolescent females (i.e., < 18 years old) have demonstrated more growth than males in condition self-management by taking on more responsibility for care (e.g., catheterization, medications; Kayle et al., 2020). Another study found that sex predicted independent living status (i.e., females were less likely to live with parents or in a supervised living environment) in youth 18 to 25 years old, but this study did not examine the independent living self-management behaviors assessed by the AMIS-II (Bellin et al., 2011).
Only three studies have used a longitudinal growth analysis approach in the study of self-management in SB. Two of these studies were from the same study cohort as the current study but in youth under 18 years of age and found two distinct groups using measures of responsibility for care, namely, a low (flat) trajectory and a high increasing (steep) trajectory; the latter was found for roughly 2/3 of the sample. Higher skill mastery and lower self-management behaviors reported by parents, not gender, predicted group membership in a high increasing trajectory for self-catheterization (Chu et al., 2022). Kayle et al. (2020) reported that females were 2.65 times more likely to be in the high increasing medical responsibility group compared to males. Race/ethnicity and socioeconomic status assessed by the Hollingshead Index were not predictors of growth in medical responsibility (Kayle et al., 2020). In another study, and using a self-report, parallel version of the AMIS-II (Sawin et al., 2013), the total self-management score did increase over time in the study sample, which included 14- to 20-year-olds (Fremion et al., 2021). Demographic characteristics (e.g., sex, race/ethnicity, insurance) were not associated with baseline self-management scores (Fremion et al., 2021); relations with trajectories were not assessed.
The current study will be the first to examine growth of self-management with the interview version of the AMIS-II and evaluate components of self-management. Generating one trajectory for each outcome (i.e., total, condition, independent living), this study will examine growth of self-management and predictors of such growth. Building on past work, we will determine if young adult females (i.e., > 18 years old) continue to demonstrate more growth of independence in self-management behaviors than males or if they do not differ at later ages. It will also establish whether race/ethnicity and income are important predictors of growth in self-management after youth are 18 years old.
This study aims to: (a) determine if there is growth in self-management over time, and (b) examine age, gender, race, ethnicity, and income in association with trajectories of self-management. Specifically, we hypothesize that self-management will increase over time and that growth in AMIS total, condition, and independent living scores will depend on respondent characteristics. That is, we believe that such trajectories will be higher (steeper) for respondents identifying as female (rather than male) and for those identifying as non-Hispanic White (relative to those identifying as Black or Hispanic/Latino).
Method
Families were recruited to participate in a longitudinal study examining family, psychosocial, and neurocognitive functioning in youth with SB from four hospitals near Chicago and through a Midwest-based Spina Bifida Association (e.g., Devine, Holmbeck, et al., 2012). Inclusion criteria were as follows: (a) an SB diagnosis; (b) 8–15 years old; (c) can understand English or Spanish; (d) involvement of at least one main caregiver; and (e) lives within 300 miles of the study lab for home visit data collection. A total of 246 families were recruited and 163 families agreed to participate. After initial consent, 21 families either declined to participate or could not be contacted and two families did not meet the inclusion criteria. Thus, at Time 1, the beginning of the longitudinal data collection, 140 families with children with SB participated, including Hispanics (n = 42). Participants who enrolled in the larger study did not differ from those who declined on type of SB, shunt status, or the number of shunt infections (Driscoll et al., 2018). In the sample of 140, youth were 52.9% White, 13.6% Black, 27.9% Hispanic, 1.4% Asian, and 4.3% multiracial. Of those who identified as multiracial, three were White and Black; two were White and Hispanic; and one was White, Hispanic, and Asian. Slightly more females (n=75, 53.6%) versus males (n=65, 46.4%) participated. Over half of parents reported a family income of 50K or above (59.3%; 12 or 8.6% were missing data on income). The type of SB was 87.9% myelomeningocele, 77.9% had a shunt, and half had a lumbar lesion level (49.3%). Demographic details for the subsample examined in the current study are presented in the Results section below.
Sample Description
Longitudinal data collections occurred every 2 years in the family home or in the youth’s home, if living independently at later time points. The first time point (Time 1) included children 8 to 15 years of age and their parents, Time 2 included 10- to 17-year-olds, and so on. About 25% of the sample youth reached 18 years of age at Time 3, 50% at Time 4, 75% at Time 5, and 100% at Time 6. Self-management was assessed with the AMIS-II for youth over 18 years of age; therefore, Times 3 – 6 were used for youth who completed the interview to examine the trajectory of self-management. Overall, the level of missing data on the AMIS-II at each time point corresponds roughly to the number of individuals who were ineligible to complete the assessments at a given time point (due to being < 18 years old). Specifically, rates of missing data were 76.5% at Time 3, 52% at Time 4, 33.7% at Time 5, and 20.4% at Time 6. During the latter portion of Time 6, the data collection method for the interview changed from in-home to virtual sessions due to the COVID-19 pandemic. This study includes only those participants who completed the AMIS-II interview in-person during the home visit data collection before the pandemic began in March 2020. All participants with a minimum of one observation over the four data collection points were included. Thus, the sample included 99 unique participants and 214 total observations. The mean age of the first recorded observation was 19.98 (SD 1.80). Although age rather than time point was used to examine predictors over time, mean ages for those who were > 18 at each time point were as follows: Time 3 = 19.2, Time 4 = 20, Time 5 = 21.4, and Time 6 = 23.3.
Procedures for Data Collection
Youth were interviewed during home visits conducted by trained undergraduate- and graduate-level research assistants. Demographic information was reported by parents (mothers and fathers) at the beginning of the study (Time 1). Informed consent from parents and assent from youth were obtained at Time 1 and adolescents and young adults (AYA) >18 years old were consented as adults when eligible beginning at Time 3. The longitudinal study was approved by university and hospital-based IRBs. The AMIS-II interviews were audio-recorded by a research assistant. Participants were provided with a description of each item prior to the interview question. Follow up questions were also used for clarification as described in the administration instructions.
Measures
Parent Demographic Questionnaire
The Parent Demographic Questionnaire was completed by both mothers and fathers. Questions about the child included the child’s date of birth, sex, race, ethnicity, and family income. Exact age was used for the analysis (i.e., age was not rounded or truncated). The item for the child’s race and ethnicity was combined (i.e., “Your child’s ethnicity/race”); possible responses were White, African-American, Hispanic, Asian, and other. If participants selected “other,” they were provided with space to write in a response. The race and ethnicity data were recoded to identify those participants who selected ‘other’ or were multiracial. If participants identified as multiracial including Hispanic (i.e., if participant reported White and Hispanic) they were included in the study as a Hispanic. Mother and father report of annual family income at Time 1 were significantly correlated (r = .920); therefore, scores were averaged and recoded as dichotomous based on earning less than or greater than 50K.
Adolescent/Young Adult Self-Management and Independence Scale (AMIS-II)
The AMIS-II interview was completed by AYA > 18 years old. The structured interview assesses the level of assistance required by the AYA to perform independent living skills and condition-related self-management. The interview includes 17 items (e.g., condition: knowledge; condition: complication prevention; self-management: ordering medication/supplies, making health care appointment; transportation; household skills; community living skills) scored on a 7-point Likert scale from 1 to 7 (1 = total assistance: AYA does little or none of the activity less than 25% of the time; 2 = maximal assistance/prompting: AYA does the activity 25 – 49% of the time; 3 = moderate assistance: AYA does the activity 50–74% of the time; 4 = minimal assistance/prompting: AYA does activity 75 to 90% of the time; 5 = supervision: AYA does activity independently but needs supervision [90% or more independent]; 6 = modified independence: AYA does activity independently but has safety or time issues, or independent with use of assistive device; 7 = complete independence: AYA does activity independently 100% of the time. A score of 8 is assigned when item is “not applicable”). If a score of 8 was recorded, the item was omitted from the subscale score. The AMIS-II total and subscales (condition self-management and independent living self-management; see Table 1 for items per subscale) were calculated only if no more than two items were missing from the scales. An individual’s subscale or total scores were based on the mean of all items that were not scored as “not applicable” (Sawin et al., 2018). Sawin et al. (2018) provide psychometric evidence for the AMIS-II including stability over time (i.e., AYA report in a 2-week interval intraclass correlation coefficient [ICC] = 0.84, 95% CI 0.71 to 0.92). This measure was also validated in a subsample (n = 64) from the larger longitudinal study and further described in Ridosh et al. (2021).
Table 1.
AMIS-II Subscale Items
| Condition Self-management (7 items) | Independent Living Self-management (10 items) |
|---|---|
| 1. Personal Safety | 4. Self-Management: Making Health Care Appointment |
| 2. Condition: Knowledge | 5. Self-Management: Ordering Medication/Supplies |
| 3. Self-Management: Medication | 7. Manages Insurance |
| 6. Condition: Complication Prevention | 8. Money/Finances: Income |
| 11. Accessibility | 9. Money/Finances: Managing Money |
| 16. Advocacy | 10. Transportation |
| 17a. Family involvement in Self-Management | 12. Household Tasks |
| 13. Community Living | |
| 14. Social Communication | |
| 15. Problem solving |
The responses to interview items were scored by two coders in this study to assess for scoring reliability; two research assistants independently scored the audio-recorded interviews. Reliability between coders using Pearson correlations at the item level were high. The lowest correlations were: rtime 3 = .764 for item 3 (self-management of medications); rtime 4 = .670 for item 6 (condition: complication prevention); and rtime 4 = .657 for item 16 (advocacy). ICCs (e.g., inter-rater reliability between coders of the AMIS-II interviews) for total and subscales were also computed. Guidelines for interpreting ICCs were 0.90 = excellent; 0.80 = very good; and 0.70 = adequate (Kline, 2016, p. 92). ICCs were excellent (≥ .946). Therefore, data for the AMIS-II were averaged across the 2 coders.
Analyses
Preliminary analyses included screening all variables for outliers and skewness. An attrition analysis was conducted to assess differences between the 99 participants and the 41 who did not participate (see below for details on non-participants). Internal consistency reliability for AMIS-II total and subscales was assessed at each occasion.
Participant characteristics are provided as counts with proportions for nominal and ordinal variables and as a mean and standard deviation (or median with range) for quantitative variables. To describe the sample, SB type, lesion level, presence of a shunt, and intelligence quotient (IQ) were reported. Age, sex, race, and income were included in the trajectory analyses. Linear mixed effect models were used to measure AMIS-II scores (total, condition, and independent living) over time. In these models, the explanatory variable of interest was elapsed time (age), which was centered at age 18. Interaction terms were included to assess when change in AMIS-II over time depended on participant demographics (i.e., sex, race, and income) and used a Sidak correction to control the Type 1 error rate. Further, because this study was longitudinal, participants could contribute multiple AMIS-II responses to the model. For this reason, random intercepts were allowed for each participant to account for their longitudinal (correlated) responses using a completely general (unstructured) covariance matrix. Random slopes were also allowed for each participant if inclusion improved model fit and parsimony as measured using Akaike’s information criterion (AIC).1 For all models, the denominator degrees of freedom were estimated using the method of Kenward and Roger (Kenward & Roger, 2009). All analyses were completed using R 4.1.0 (R Core Team, 2021) and the lmerTest package (v.1.1–28; Kunzetsova et al., 2017) as well as the ggplot2 package (v.3.3.3; Wickham, 2016).
Results
The current study sample (n = 99) ranged in age from 18.2 to 27.0 years old (depending on the time point assessed). Roughly half were female (52.5%) and White (52.5%); 15.2% were Black, and about a third were Hispanic/Latino (32.3%). Eighty-seven AYAs (87.9%) had myelomeningocele. The lesion level was 31.3% sacral, 48.5% lumbar, and 18.2% thoracic (level of lesion was mother-reported at Time 1 and verified by medical chart review; two reports were missing). A third of the sample earned less than 50K (32.3%; 8 cases were missing report of family income). See Table 2 for sample characteristics. Table 3 includes descriptive statistics for AMIS-II scale and subscales by time point in the study.
Table 2.
Sample Characteristics and Study Variables
| Variables | Overall (N = 99) |
|---|---|
| Spina bifida type | |
| Myelomeningocele | 87 (87.9%) |
| Not myelomeningocele | 12 (12.1%) |
| Lesion level | |
| Sacral | 31 (31.3%) |
| Lumbar | 48 (48.5%) |
| Thoracic | 18 (18.2%) |
| Missing | 2 (2.0%) |
| Shunt present | |
| Yes | 81 (81.8%) |
| No | 17 (17.2%) |
| Missing | 1 (1.0%) |
| Intelligence Quotient | |
| Mean (SD) | 84.7 (19.9) |
| Median [Min, Max] | 84.0 [55.0, 137] |
| Missing | 2 (2.0%) |
| Age at time 1 | |
| Mean (SD) | 12.0 (2.29) |
| Median [Min, Max] | 12.0 [8.00, 16.0] |
| Age at time 3 | |
| Mean (SD) | 19.2 (0.719) |
| Median [Min, Max] | 19.4 [18.2, 20.5] |
| Missing | 76 (76.8%) |
| Age at time 4 | |
| Mean (SD) | 20.0 (1.24) |
| Median [Min, Max] | 19.8 [18.0, 22.1] |
| Missing | 52 (52.5%) |
| Age at time 5 | |
| Mean (SD) | 21.4 (1.87) |
| Median [Min, Max] | 21.6 [18.0, 25.3] |
| Missing | 34 (34.3%) |
| Age at time 6 | |
| Mean (SD) | 23.3 (2.42) |
| Median [Min, Max] | 23.5 [19.1, 27.0] |
| Missing | 20 (20.2%) |
| Sex | |
| Male | 47 (47.5%) |
| Female | 52 (52.5%) |
| Race/Ethnicity | |
| White | 52 (52.5%) |
| Black | 15 (15.2%) |
| Hispanic/Latino | 32 (32.3%) |
| Income | |
| <50K | 32 (32.3%) |
| >=50K | 59 (59.6%) |
| Missing | 8 (8.1%) |
Table 3.
Descriptive Statistics AMIS-II by Time Point
| Variables | Time 3 (obs = 23) |
Time 4 (obs = 47) |
Time 5 (obs = 65) |
Time 6 (obs = 79) |
|---|---|---|---|---|
| AMIS-II Total scale | 3.19 (1.45) | 3.49 (1.41) | 3.72 (1.32) | 3.97 (1.43) |
| AMIS-II Condition | 3.88 (1.76) | 4.10 (1.64) | 4.12 (1.44) | 4.36 (1.55) |
| AMIS-II Independent Living | 2.72 (1.27) | 3.07 (1.34) | 3.44 (1.34) | 3.70 (1.44) |
Note. Means and standard deviations are reported by number of observations (obs) for each time point.
Preliminary Analyses
All variables were examined for outliers. Only two participants identified as Asian; these cases were removed from the analysis because this would have produced a subsample that was too small for the race/ethnicity analyses. Subsequently, the AMIS-II items by coder were evaluated for skewness, which was determined by values greater than ± 2 (West et al., 1995). The highest skewness values were 2.7 and 2.8 for items 12 and 13, respectively. These items correspond to household skills and community living only at time 3; most participants endorsed total assistance (i.e., participants at their first observation did little to none of the activity). All other items were not skewed (i.e., < 2). No other skewness was detected at the item level for time points 4 – 6. No skewness was detected at the scale level for any time point. Thus, data transformations were not conducted.
Of the 41 enrolled who were not included in this study, 29 participants stopped participating in the study before they turned 18 years of age at their study visit(s) (i.e., did not complete the AMIS-II interview), five participated by only completing questionnaires and were not interviewed, five were interviewed only in an online format due to Covid-19 restrictions after March 1st, 2020, and as noted earlier two were of Asian background. For the attrition analyses, as expected, the included cohort was 2 years (95% CI −2.67 to −0.96; p < .001) older than the participants without the outcomes of interest for this study but remained comparable on key demographic characteristics (sex, race, income, lesion level; all p > .05). Regarding the internal consistency reliability of the AMIS-II, the alphas were very high for both the total and subscale constructs (range: α = .896 - .956), which are somewhat higher than the published results in the original psychometric paper (Sawin et al., 2018).
For all analyses, age was centered at 18 years old. The average intercepts and slopes for total, condition, and independent living self-management were significantly different from zero (all p < .05). Although the variances for the random slopes within the total and independent living models were small (σ2 = .01 and σ2 =.02, respectively), adding them improved model fit. For the condition self-management score, all models fit best when using only a random intercept (rather than both a random intercept and slope) term. At age 18, most youth required at least moderate assistance for self-management overall. Based on a possible range of scores from 1 to 7, the average AMIS-II score was roughly 3 points (intercept = 3.26; SE = 0.13; 95% CI 3.01 to 3.52) for the total scale, almost 4 points for the condition self-management subscale (intercept = 3.93; SE = 0.16; 95% CI 3.61 to 4.25), and below 3 points for the independent living self-management subscale (intercept = 2.80; SE = 0.12; 95% CI 2.55 to 3.05). An independent living score less than 3 points indicates that the individual requires maximal assistance/prompting in domains of independent living self-management. In our study, the AMIS-II total score increased by almost 1 point over 8 years (.96 points; 0.12 points per year; i.e., slope = 0.12, SE = 0.02; p < .001). The condition self-management subscale increased about a half point (0.4 points; slope = 0.05, SE = 0.02; p = .01) and the independent living scale increased by slightly over one point (1.28) during the study (slope = 0.16, SE = 0.03; p < .001).
Predictors of Growth Trajectories
Findings from linear mixed effect models are reported by total and subscales. See Table 4. When considering participant characteristics, race and income (but not sex) were associated with the AMIS-II total score (all p < .05). The association between age and the AMIS-II total score depended on race (p = .02). That is, for every year increase in age, the AMIS-II total score increased by 0.10 (95% CI: 0.05 to 0.15) points for White participants and increased by 0.08 (95% CI: 0.02 to 0.15) for Hispanics/Latinos. However, for respondents who identified as Black, the AMIS-II total score increased by 0.27 for every year increase in age (95% CI: 0.15 to 0.39), or an increase of about 2 points over 8 years. This increase was sharper than the increase for Whites (p = .03) as well as for those who identified as Hispanic/Latino (p = .02). See Figure 1 for differences in growth of total self-management by race/ethnicity.
Table 4.
AMIS-II Assessment
| N | AMIS-II | ||||||
|---|---|---|---|---|---|---|---|
| Total | Condition | Independent Living | |||||
| (95% CI) | p | (95% CI) | p | (95% CI) | p | ||
| Age (per year increase) | 99 | 0.12 (0.07 to 0.16) | <.001 | 0.05 (0.01 to 0.09) | .01 | 0.16 (0.11 to 0.23) | <.001 |
| Sexa: Females vs Males | 99 | 0.30 (−0.19 to 0.79) | .23 | 0.16 (−0.42 to 0.74) | .58 | 0.25 (−0.21 to 0.78) | .28 |
| Race/Ethnicity a | 99 | .02b | .02b | .01b | |||
| Black vs Whitec | 0.27 (−0.59 to 1.13) | .83 | 0.11 (−0.90 to 1.11) | .99 | 0.48 (−0.33 to 1.29) | .39 | |
| Hispanic/Latino vs Whitec | −0.64 (−1.29 to 0.02) | .06 | −0.86 (−1.63 to −0.09) | .02 | −0.52 (−1.14 to 0.09) | .12 | |
| Black vs Hispanic/Latinoc | 0.91 (0.01 to 1.83) | .053 | 0.96 (−0.11 to 2.04) | .09 | 1.01 (0.14 to 1.87) | .02 | |
| Incomea: >=50K vs <50K | 91 | 0.77 (0.24 to 1.28) | .004 | 0.91 (0.31 to 1.51) | .003 | 0.64 (0.14 to 1.14) | .01 |
| Age*Sex Interaction | 99 | .18b | .01b | .84b | |||
| Age | Male | 0.15 (0.09 to 0.21) | <.001 | 0.11 (0.05 to 0.17) | <.001 | 0.17 (0.09 to 0.24) | <.001 | |
| Age | Female | 0.09 (0.03 to 0.15) | .005 | 0.001 (−0.06 to 0.06) | .96 | 0.16 (0.08 to 0.23) | <.001 | |
| Age*Race Interaction | 99 | .02b | .03b | .23b | |||
| Age | White | 0.10 (0.05 to 0.15) | <.001 | 0.05 (−0.01 to 0.10) | .08 | 0.16 (0.09 to 0.22) | <.001 | |
| Age | Black | 0.27 (0.15 to 0.39) | <.001 | 0.21 (0.08 to 0.34) | .001 | 0.28 (0.13 to 0.44) | <.001 | |
| Age | Hispanic/Latino | 0.08 (0.02 to 0.15) | .01 | 0.01 (−0.07 to 0.08) | .84 | 0.13 (0.04 to 0.22) | .007 | |
| Age*Income Interaction | 91 | .94b | .54b | .85b | |||
| Age | <50K | 0.12 (0.04 to 0.20) | .005 | 0.08 (−0.001 to 0.16) | .053 | 0.15 (0.05 to 0.25) | .003 | |
| Age | >=50K | 0.12 (0.06 to 0.17) | <.001 | 0.05 (−0.005 to 0.10) | .08 | 0.16 (0.10 to 0.23) | <.001 | |
Note. N = Number of participants used to compute the univariate estimates. Estimates for age are per year increase.
Model conclusions are adjusted for elapsed time (age).
Type-III test of the fixed-effect.
Estimate is corrected for multiple pairwise comparisons using a Sidak correction.
Figure 1.
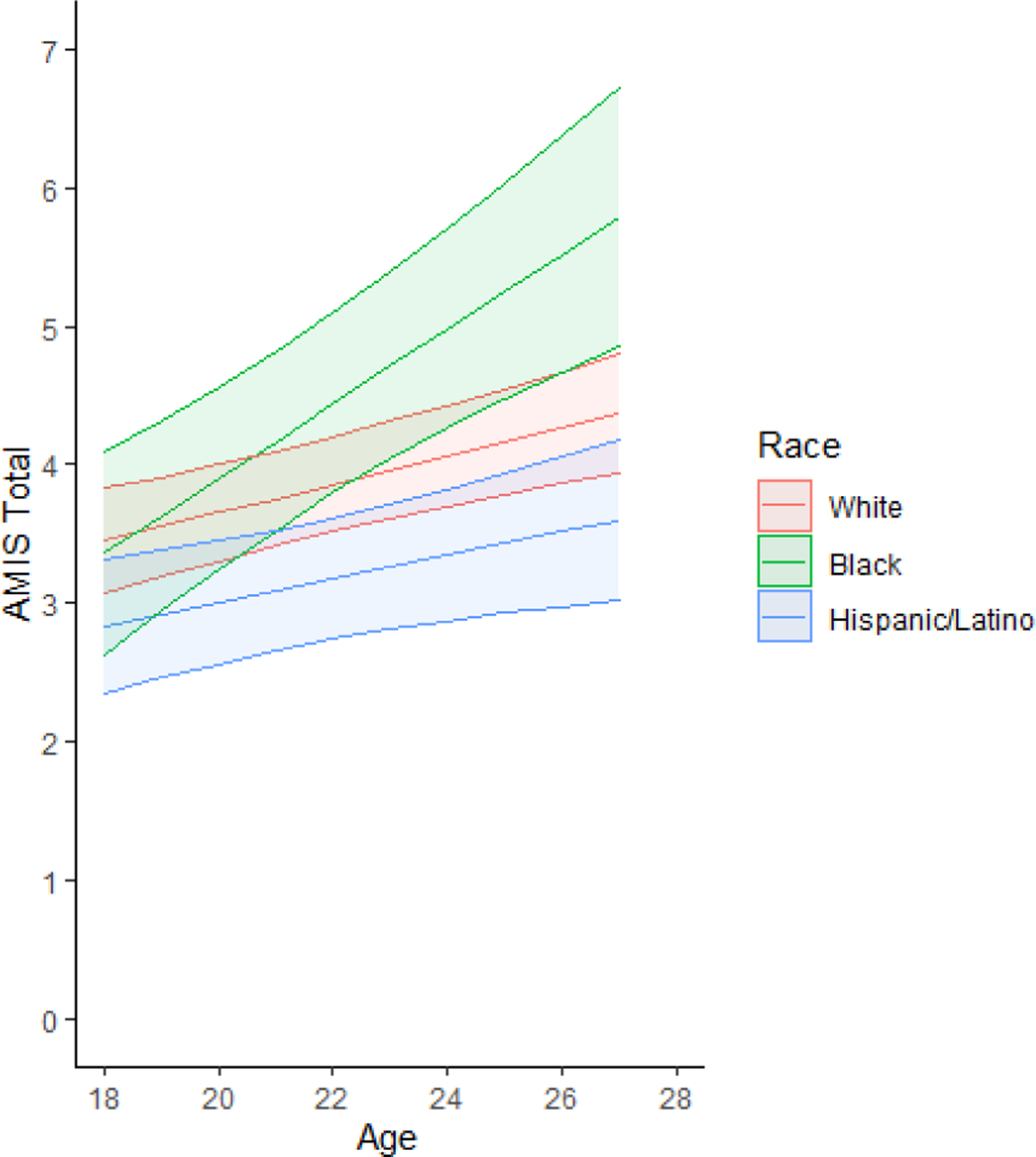
AMIS-II Total: Race by age trajectories
The association between age and AMIS-II condition also depended on the race of the participant (interaction p = .03). Those identifying as Black saw an increase of 0.21 in their condition score (95% CI: 0.08 to 0.34, p = .001) for every 1-year increase in age. Conversely, the slope was flatter for those identifying as White (, 95% CI: −0.01 to 0.10) as well as for those identifying as Hispanic/Latino (, 95% CI: −0.07 to 0.08). Figure 2 displays AMIS-II condition by race/ethnicity. While growth in AMIS condition over time was comparable between those with high and low income (interaction p = .54), participants with high income were on average about 0.91 (95% CI: 0.31 to 1.51) points higher than those with low income regardless of age (p = .003). Finally, the association between age and AMIS-II condition depended on sex (interaction p = .01). For males, the trajectory was steeper (, 95% CI: 0.05 to 0.17; p <.001) than for females (, 95% CI: −0.06 to 0.06; p = .96). See Figure 3 for sex differences in trajectories for AMIS-II condition.
Figure 2.
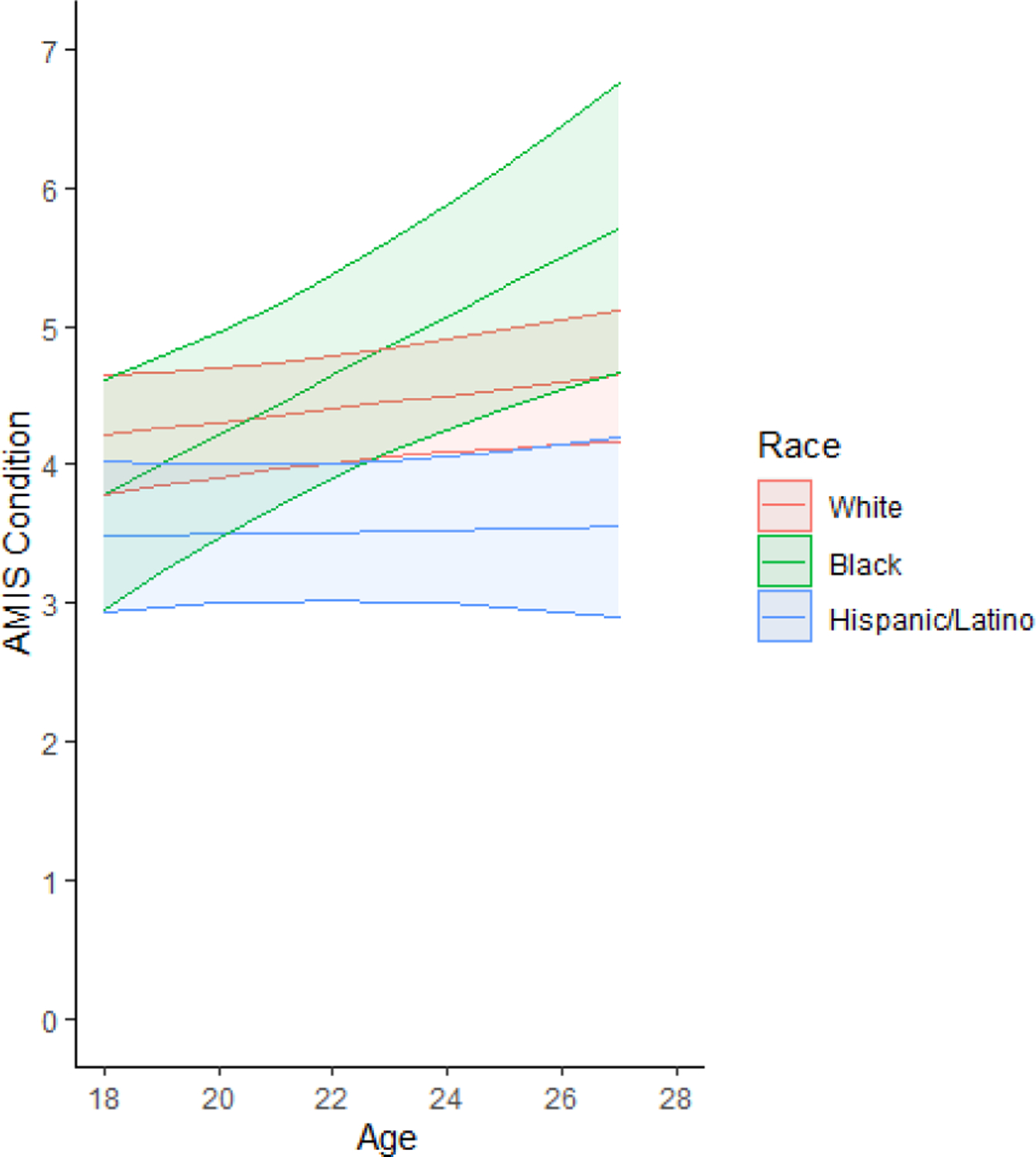
AMIS-II Condition: Race by age trajectories
Figure 3.
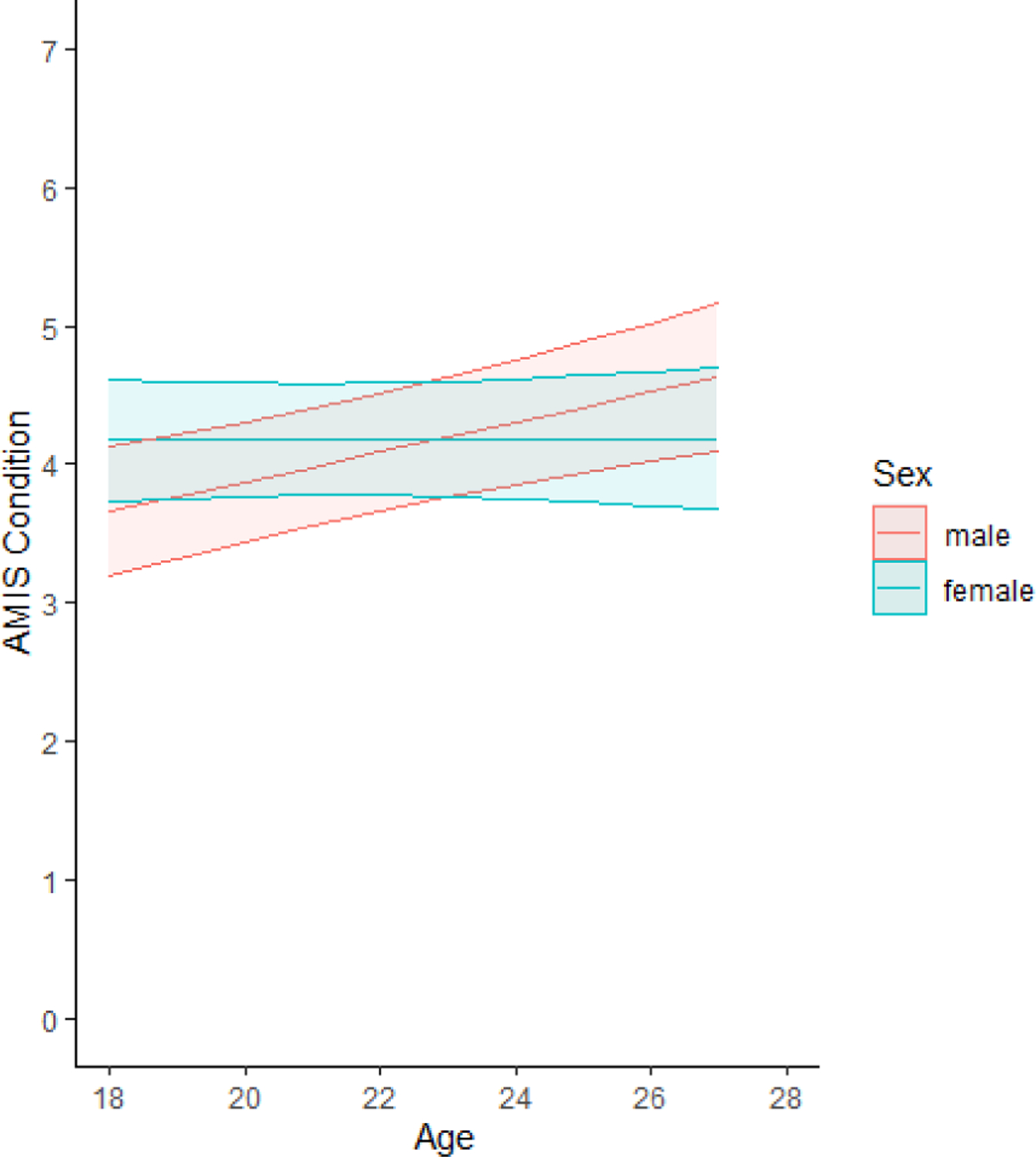
AMIS-II Condition: Sex by age trajectories
Regarding the independent living subscale, growth over time did not depend on sex (interaction p = .84), and both sexes had comparable scores regardless of age (Mdiff = 0.25, 95% CI: −0.21 – 0.78; p = .28). However, findings for age and race were different from those reported for the AMIS-II condition and total self-management conclusions. For this outcome, individuals identifying as Black had comparable growth over time relative to those identifying as White or Hispanic (interaction p = .23). Still, regardless of age, participants identifying as Black reported higher independent living scores relative to those identifying as Hispanic (Mdiff = 1.01, 95% CI: 0.14 – 1.87; p = .02) but not relative to those identifying as White (Mdiff = 0.48, 95% CI: −0.33 – 1.29; p = .39). Finally, growth in AMIS independent living over time was also comparable between those with high and low income (interaction p = .85), but participants with high income reported an average independent living score that was about 0.64 (95% CI: 0.14 – 1.14) points higher than those with low income, regardless of age (p = .01).
Discussion
The current study provides evidence of growth in self-management for youth over 18 years of age and this growth also varied by demographic characteristics. Consistent with our hypothesis, self-management increases over time in early adulthood. The achievement of total self-management depends on race/ethnicity while condition self-management depends on both sex and race/ethnicity. Further, contrary to our hypothesis, some groups that we expected to have less growth exhibited more growth (e.g., males, Blacks).
Regarding condition self-management, though no sex differences were demonstrated at age 18 (males 3.85 vs. females 4.01), males unexpectedly demonstrated change over time; females’ scores remained relatively unchanged across this age range. Using a different self-management measure of shared responsibility for care in the same study cohort at earlier time points (a measure highly correlated with the AMIS-II; Ridosh et al., 2021), females under 18 demonstrated more growth in self-management than males (Kayle et al., 2020). These findings over time demonstrate that females’ growth may occur earlier than is the case for males, while males show later growth and appear to ‘catch up’. Also, once females reach 18, their level of independence appears to plateau. Both sexes perform at a level of independence that continues to require minimal assistance/prompting to supervision (scores averaging between 4 to 5 on the AMIS-II). These scores and other assessments demonstrating increased independence skills and responsibility for care when youth were younger (8 – 17 years) suggest that continued parent involvement/caregiver assistance is needed to optimize outcomes, especially given evidence of decreased adherence to their medical regimen in many youth during this developmental period (Psihogios et al., 2015).
Contrary to our hypothesis, Black respondents demonstrated the most growth in self-management. While this conclusion was not statistically significant for the independent living construct (interaction p = .23), it was significant for the total self-management (interaction p = .02) and condition self-management constructs (interaction p = .03). For the total self-management score, Black respondents reported sharper growth relative to White respondents (p = .03) as well as Hispanic/Latino respondents (p = .02). Hispanics/Latinos fared worse than expected with little to no growth in total and condition self-management. Given findings from the National Spina Bifida Patient Registry (NSBPR) regarding poorer health outcomes for Blacks (i.e., less likely to exhibit bowel and urinary continence), the current results are concerning. Although it is desirable for most youth to reach higher levels of independence, the combination of these 2 sets of findings indicate that youth in this subgroup may have been granted a higher level of independence than is developmentally appropriate.
For Hispanics/Latinos, lack of growth in condition self-management is also concerning and may be attributed to a parents’ higher perceptions of vulnerability in their children (Devine, Holbein, et al., 2012) resulting in more continued parent involvement in care (i.e., less AYA responsibility for care). From our analysis, we know when and the rate by which youth experience growth in self-management, not how Black or Hispanic/Latino families facilitate the transfer of self-management. Perhaps parents in families of these youth promote condition management, in preparation for independent living status in different ways than in other families. Further study of contextual and process factors, such as other sociodemographic factors or the family environment, may help explain these differences across ethnic/racial subgroups.
Higher income was related to better self-management in our study. Regardless of participants’ age, the AMIS total score was about 0.77 units higher for high income respondents than low-income respondents, but rate of growth in self-management did not depend on income. Importantly, income was collected at the beginning of the study when youth were 8 – 15 years old and reflects the family’s income as reported by parents. Participants who earned lower income (<50K) started out at lower rating of total self-management and remained lower. Put another way, the rate of change (slope Mdiff = 0.01) was the same for both groups so those in the low-income group did not ‘catch up’. In a study of sociodemographic risk conducted with the same sample when they were younger, a higher family income-to-needs ratio was associated with fewer lifetime number of urinary tract infections (Papadakis & Holmbeck, 2021). It is possible that the families with higher income have more resources for consistent access to supplies and are able to provide more support while youth remain at home. Continued attention to predictors of healthy self-management trajectories including social determinants of health must be considered to promote better health outcomes for individuals with SB.
Limitations and Future Research
The present study has a number of strengths as well as limitations. First, this was a longitudinal study which included a larger number of Hispanics/Latinos than is typical. Also, the inclusion of multiple observations in this longitudinal study allowed us to examine the trajectories of self-management. However, while our study observed differences by race/ethnicity including steeper slopes of self-management for the Black participants, the Black participants made up the smallest proportion of the sample (15%). Also, although this study demonstrated differences across low versus high income on self-management, it will be important to select other sociodemographic factors in future studies to identify which may promote change in self-management over time. Our study collected race/ethnicity data as a combined category; therefore, when someone identified as Hispanic/Latino, their race was not considered since the majority of respondents did not select multiple categories (e.g., 4.3% multiracial in original sample). Finally, not all possible predictor variables were incorporated into the analyses and should be included in future studies (e.g., condition severity, neuropsychological functioning).
Conclusions and Clinical Implications
The present study contributes to our understanding of the trajectories of self-management as well as differences in growth by demographic variables (age, sex, race/ethnicity). Overall self-management in this community sample 18 – 27 years of age improves every year, but youth continue to need supervision; they have not yet achieved full self-management independence. These findings are important to consider with respect to clinical care, particularly as youth transition to adult-oriented care. Strategies for supervision or assistance in self-management remain important for emerging adults, since slow growth seems to occur in condition self-management in later years. Monitoring and reminder systems, whether through the use of technology or paper record/binders and checklists can be used to facilitate independence to ensure completion of medical care regimens (e.g., bowel/bladder care, medication/supply ordering, appointment making). Assessments of self-management in the clinic setting can prompt clinicians to make concrete recommendations for assistive devices and to follow up on concerns, when responsibility for care is compromised. Future research must take into account differences in self-management across demographic groups, such as when identifying other predictors of self-management and related health outcomes.
Acknowledgements
This research was supported in part by grants from the National Institute of Nursing Research and the Office of Behavioral and Social Sciences Research (R01 NR016235; K01NR018907), Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD048629), and the March of Dimes Birth Defects Foundation (12- FY13-271). This study is part of an ongoing longitudinal study. The authors thank the Illinois Spina Bifida Association as well as staff of the spina bifida clinics at Ann & Robert H. Lurie Children’s Hospital of Chicago, Shriners Hospital for Children-Chicago, and Loyola University Medical Center. We also thank the numerous undergraduate and graduate research assistants who helped with data collection and data entry. Finally, we would like to thank the families who generously participated in this study.
Footnotes
This occurred for all models of the AMIS-II total self-management score except for the association between AMIS-II total and elapsed time stratified by race. For that model, the inclusion of a random slope produced unstable estimates and standard errors (poor convergence).
References
- Atta CA, Fiest KM, Frolkis AD, Jette N, Pringsheim T, St Germaine-Smith C, Rajapakse T, Kaplan GG, & Metcalfe A (2016). Global birth prevalence of spina bifida by folic acid fortification status: A systematic review and meta-analysis. Am J Public Health, 106(1), e24–34. 10.2105/ajph.2015.302902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellin MH, Dicianno BE, Levey E, Dosa N, Roux G, Marben K, & Zabel TA (2011). Interrelationships of sex, level of lesion, and transition outcomes among young adults with myelomeningocele. Dev Med Child Neurol, 53(7), 647–652. 10.1111/j.1469-8749.2011.03938.x [DOI] [PubMed] [Google Scholar]
- Betz CL, Smith K, & Macias K (2010). Testing the transition preparation training program: A randomized controlled trial. Int J Child Adolesc health, 3(4), 595–607. https://www.ncbi.nlm.nih.gov/pubmed/22229060 [PMC free article] [PubMed] [Google Scholar]
- Canfield MA, Mai CT, Wang Y, O’Halloran A, Marengo LK, Olney RS, Borger CL, Rutkowski R, Fornoff J, Irwin N, Copeland G, Flood TJ, Meyer RE, Rickard R, Alverson CJ, Sweatlock J, Kirby RS, & National Birth Defects Prevention, N. (2014). The association between race/ethnicity and major birth defects in the United States, 1999–2007. Am J Public Health, 104(9), e14–e23. 10.2105/AJPH.2014.302098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castillo J, Ostermaier KK, Fremion E, Collier T, Zhu H, Huang GO, Tu D, & Castillo H (2017). Urologic self-management through intermittent self-catheterization among individuals with spina bifida: A journey to self-efficacy and autonomy. J Pediatr Rehabil Med, 10(3–4), 219–226. 10.3233/prm-170447 [DOI] [PubMed] [Google Scholar]
- Chowanadisai M, de la Rosa Perez DL, Weitzenkamp DA, Wilcox DT, Clayton GH, & Wilson PE (2013). The role of ethnicity and culture on functional status in children with spina bifida. J Pediatr Rehabil Med, 6(4), 205–213. 10.3233/prm-140259 [DOI] [PubMed] [Google Scholar]
- Chu DI, Kayle M, Stern A, Bowen DK, Yerkes EB, & Holmbeck GN (2022). Longitudinal trajectories of clean intermittent catheterization responsibility in youths with spina bifida. J Urol, 207(1), 192–200. 10.1097/JU.0000000000002204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN, & Shaw GM (2015). Spina bifida. Nat Rev Dis Primers, 1, 15007. 10.1038/nrdp.2015.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine KA, Holbein CE, Psihogios AM, Amaro CM, & Holmbeck GN (2012). Individual adjustment, parental functioning, and perceived social support in Hispanic and non-Hispanic White mothers and fathers of children with spina bifida. J Pediatr Psychol, 37(7), 769–778. 10.1093/jpepsy/jsr083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine KA, Holmbeck GN, Gayes L, & Purnell JQ (2012). Friendships of children and adolescents with spina bifida: Social adjustment, social performance, and social skills. J Pediatr Psychol, 37(2), 220–231. 10.1093/jpepsy/jsr075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driscoll CFB, Buscemi J, & Holmbeck GN (2018). Parental distress and stress in association with health-related quality of life in youth with spina bifida: A longitudinal study. J Dev Behav Pediatr, 39(9), 744–753. 10.1097/dbp.0000000000000603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fremion E, Madey R, Staggers KA, Morrison-Jacobus M, Laufman L, Castillo H, & Castillo J (2021). Factors associated with self-management independence and quality of life for adolescents and young adults with spina bifida engaged in a guideline-based transition clinic. J Pediatr Rehabil Med, 14(4), 631–641. 10.3233/PRM-200758 [DOI] [PubMed] [Google Scholar]
- Holmbeck GN, & Kritikos TK (2022). Psychosocial adjustment in emerging adults with and without spina bifida: A 14-year follow-up study. J Dev Behav Pediatr, 43(1), e20–e28. 10.1097/DBP.0000000000000956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayle M, Chu DI, Stern A, Pan W, & Holmbeck GN (2020). Predictors of distinct trajectories of medical responsibility in youth with spina bifida. J Pediatr Psychol, 45(10), 1153–1165. 10.1093/jpepsy/jsaa065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenward MG, & Roger JH (2009). An improved approximation to the precision of fixed effects from restricted maximum likelihood. Comput Stat Data Anal, 53(7), 2583–2595. 10.1016/j.csda.2008.12.013 [DOI] [Google Scholar]
- Kline RB (2016). Principles and practice of structural equation modeling. Guilford publications. [Google Scholar]
- Kunzetsova A, Brockhoff P, & Christensen R (2017). lmerTest package: Tests in linear mixed effect models. J Stat Softw, 82, 1–26. [Google Scholar]
- Logan LR, Sawin KJ, Bellin MH, Brei T, & Woodward J (2020). Self-management and independence guidelines for the care of people with spina bifida. J Pediatr Rehabil Med, 13(4), 583–600. 10.3233/prm-200734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NINDS. (2013). Spina Bifida Fact Sheet (NIH Publication No. 13–309). Bethesda, MD [Google Scholar]
- Papadakis JL, & Holmbeck GN (2021). Sociodemographic factors and health-related, neuropsychological, and psychosocial functioning in youth with spina bifida. Rehabil Psychol, 66(3), 286–299. 10.1037/rep0000381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psihogios AM, Kolbuck V, & Holmbeck GN (2015). Condition self-management in pediatric spina bifida: A longitudinal investigation of medical adherence, responsibility-sharing, and independence skills. J Pediatr Psychol, 40(8), 790–803. 10.1093/jpepsy/jsv044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/ [Google Scholar]
- Ridosh MM, Stiles-Shields C, Stern A, Winning AM, Anderson L, Sawin KJ, & Holmbeck GN (2021). The Adolescent/Young Adult Self-Management and Independence Scale (AMIS-II): Expanding evidence for validity and reliability. J Pediatr Rehabil Med, 14(4), 583–596. 10.3233/PRM-200679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan P, & Sawin KJ (2009). The Individual and Family Self-Management Theory: Background and perspectives on context, process, and outcomes. Nurs Outlook, 57(4), 217–225.e6. 10.1016/j.outlook.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawin KJ, Bellin MH, Roux G, Buran CF, & Brei TJ (2009). The experience of self-management in adolescent women with spina bifida. Rehabil Nurs, 34(1), 26–38. https://www.ncbi.nlm.nih.gov/pubmed/19160922 [DOI] [PubMed] [Google Scholar]
- Sawin KJ, Brei TJ, Holmbeck GN, & Pasulka J (2013). Adolescent and Young Adult Self-Management and Independence Scale II Self-Report Questionnaire [Instrument].
- Sawin KJ, Heffelfinger A, Cashin SE, & Brei TJ (2018). The development of the Adolescent/Young Adult Self-Management and Independence Scale II: Psychometric data. J Pediatr Rehabil Med, 11(4), 311–322. 10.3233/prm-170479 [DOI] [PubMed] [Google Scholar]
- Sawin KJ, Margolis RHF, Ridosh MM, Bellin MH, Woodward J, Brei TJ, & Logan LR (2021). Self-management and spina bifida: A systematic review of the literature. Disabil Health J, 14(1), 100940. 10.1016/j.dhjo.2020.100940 [DOI] [PubMed] [Google Scholar]
- Schechter MS, Liu T, Soe M, Swanson M, Ward E, & Thibadeau J (2015). Sociodemographic attributes and spina bifida outcomes. Pediatrics, 135(4), e957–964. 10.1542/peds.2014-2576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling LS, Grey M, & Knafl KA (2002). The concept of self-management of type 1 diabetes in children and adolescents: An evolutionary concept analysis. J Adv Nurs, 37(1), 87–99. 10.1046/j.1365-2648.2002.02061.x [DOI] [PubMed] [Google Scholar]
- West SG, Finch JF, & Curran PJ (1995). Structural equation models with nonnormal variables: Problems and remedies. In Hoyle RH (Ed.), Structural equation modeling: Concepts, issues, and applications (pp. 56–75). Sage Publications. [Google Scholar]
- Wickham H (2016). ggplot2: Elegant graphics for data analysis. Springer-Verlag; New York. https://ggplot2.tidyverse.org [Google Scholar]


