Abstract
Purpose:
The purpose of the study was to compare the post-reduction magnetic resonance imaging morphology for hips that developed residual acetabular dysplasia, hips without residual dysplasia, and uninvolved contralateral hips in patients with unilateral developmental dysplasia of the hip undergoing closed or open reduction and had a minimum 10-year follow-up.
Methods:
Retrospective study of patients with unilateral dysplasia of the hip who underwent open/closed hip reduction followed by post-reduction magnetic resonance imaging. Twenty-eight patients with a mean follow-up of 13 ± 3 years were included. In the treated hips, residual dysplasia was defined as subsequent surgery for residual acetabular dysplasia or for Severin grade > 2 at latest follow-up. On post-reduction, magnetic resonance imaging measurements were performed by two readers and compared between the hips with/without residual dysplasia and the contralateral uninvolved side. Magnetic resonance imaging measurements included acetabular version, coronal/ axial femoroacetabular distance, acetabular depth–width ratio, osseous/cartilaginous acetabular indices, and medial/lateral (limbus) cartilage thickness.
Results:
Fifteen (54%) and 13 (46%) hips were allocated to the “no residual dysplasia” group and to the “residual dysplasia” group, respectively. All eight magnetic resonance imaging parameters differed between hips with residual dysplasia and contralateral uninvolved hips (all p < 0.05). Six of eight parameters differed (all p < 0.05) between hips with and without residual dysplasia. Among these, increased limbus thickness had the largest effect (odds ratio = 12.5; p < 0.001) for increased likelihood of residual dysplasia.
Conclusions:
We identified acetabular morphology and reduction quality parameters that can be reliably measured on the post-reduction magnetic resonance imaging to facilitate the differentiation between hips that develop with/without residual acetabular dysplasia at 10 years postoperatively.
Level of evidence:
level III, prognostic case-control study.
Keywords: Post-reduction MRI, developmental dysplasia of the hip, hip, surgical hip reduction, hip MRI
Introduction
Closed or open reduction of the hip is the mainstay of treatment for children aged 6–18 months with a dislocated hip due to developmental dysplasia of the hip (DDH). 1 Following reduction, patients often undergo advanced imaging with computed tomography (CT) or magnetic resonance imaging (MRI) to confirm a proper reduction in the spica cast. Although cost remains a concern, MRI permits a detailed assessment of the femur and acetabulum, making it a better option for morphological analysis compared with a CT scan or hip arthrogram. 2 Most previous studies using MRI are limited to a qualitative description of the reduction, and objective descriptive data about the actual morphology of the acetabulum and femur remain scarce.3–11 Furthermore, prior studies have been unable to identify an association between specific anatomic parameters on the post-reduction MRI and acetabular development.8,12
The goal of this study is to compare the post-reduction MRI morphology for hips that developed residual acetabular dysplasia, hips without residual dysplasia, and uninvolved contralateral hips in patients with unilateral DDH who underwent closed or open reduction and had a minimum 10-year follow-up.
Material and methods
Patients and study design
After institutional review board approval was obtained, we performed a retrospective study on a surgical database of patients who underwent open or closed hip reduction between 2000 and 2018 at a tertiary pediatric hospital. A search to the hospital database yielded 510 patients. Patients were excluded for the following reasons: comorbidities/neuromuscular syndromes (125 patients), previous surgery at an external institution (109 patients), traumatic hip dislocation (15 patients), no post-reduction MRI (64 patients), and not yet eligible for a minimum 10-year postoperative follow-up (103 patients). Of the resulting 94 patients, 66 were excluded for the following reasons: lost to follow-up (35 patients), radiographic signs of avascular necrosis based on Kalamchi and MacEwen 13 grade > 1 at latest follow-up (9 patients), concomitant femoral/acetabular osteotomy (8 patients), and treatment for bilateral DDH (14 patients) (Figure 1). The final cohort comprised 28 patients who had undergone closed reduction (18/28 hips, 64%) or open reduction (10/28 hips, 36%) for unilateral DDH at a mean age of 8 ± 6 months (Table 1). The mean time of follow-up was 13 ± 3 years (Table 1). Patients undergoing hip reduction were allocated to a “residual dysplasia” group based on whether they met one of the following endpoints: subsequent surgery for residual acetabular dysplasia during the follow-up period or grade > 2 according to the Severin 14 classification. Patients who did not undergo additional surgical treatment and had a Severin 14 classification ≤ 2 were allocated to the “no residual dysplasia” group. The contralateral uninvolved hip for the 28 patients were selected as a control group. However, 4 contralateral initially uninvolved hips were excluded because of a Severin 14 grade > 2 at the latest follow-up, yielding 24 contralateral hips which served as the control group (Figure 1).
Figure 1.
Flowchart of the study population is shown.
Table 1.
Demographic characteristics of hips undergoing closed or open reduction for DDH.
| Characteristic | Overall (n = 28 hips) |
Residual dysplasia (n = 13 hips) |
No residual
dysplasia (n = 15 hips) |
p | |||
|---|---|---|---|---|---|---|---|
| Freq. | (%) | Freq. | (%) | Freq. | (%) | ||
| Age at surgery (months; mean ± SD) | 8 | ±6 | 10 | ±6 | 7 | ±5 | 0.16 |
| Sex (% female) | 23 | (82%) | 11 | (85%) | 12 | (80%) | >0.99 |
| Time of follow-up (years; mean ± SD) | 13 | ±3 | 14 | ±3 | 13 | ± 3 | 0.17 |
| Previous bracing | 13 | (46%) | 4 | (31%) | 9 | (60%) | 0.24 |
| Closed reduction | 18 | (64%) | 11 | (85%) | 7 | (47%) | 0.05 |
| Open reduction | 10 | (36%) | 2 | (15%) | 8 | (53%) | 0.05 |
| Medial | 3 | (10%) | 0 | (0%) | 3 | (38%) | – |
| Anterior | 7 | (70%) | 2 | (100%) | 5 | (63%) | – |
| Subsequent surgery | 8 | (29%) | 8 | (62%) | – | – | |
| Femoral osteotomy | 1 | (13%) | 1 | (13%) | – | – | |
| Acetabular osteotomy | 4 | (50%) | 4 | (50%) | – | – | |
| Femoral and acetabular osteotomy | 2 | (25%) | 2 | (25%) | – | – | |
| PAO | 1 | (13%) | 1 | (13%) | – | – | |
DDH: developmental dysplasia of the hip; SD: standard deviation; PAO: periacetabular osteotomy.
Magnetic resonance imaging and 10-year follow-up radiographs
Post-reduction magnetic resonance imaging (MRI) was performed without sedation on most patients on two different 1.5-T scanners (Siemens Medical Solutions, Erlangen, Germany, and General Electric, Milwaukee, WI, USA) using a posterior surface coil. Although the MRI protocols were subject to changes over time, the minimum requirement of the imaging protocol was consistently maintained throughout the study period. 15 The protocol included at least one axial and one coronal T1-weighted spin-echo sequence with fat suppression, each with an acquisition time of 1 minute. Repetition time and echo time for the T1-weighted sequence were 800–1000 ms and 11 ms, respectively. Slice thickness was 4 mm with 1 mm spacing in between images, and the field of view was 22–24 cm with a minimum matrix of 256 × 256. Sequences were repeated to obtain at least 2 images of the epiphysis and physis. In addition, at least two images of the epiphysis and the physis were obtained on which the position of the femoral head relative to the acetabulum was visible.
As part of the routine follow-up, patients were seen at 4- to 6-week intervals for a spica cast change. After the cast was changed under general anesthesia, the cast was kept on for 12 weeks postoperatively. Clinical visits, including an anteroposterior radiograph of the pelvis, were scheduled at 1 year, 2 years, 5 years, and 10 years after the closed or open reduction.
Image analysis
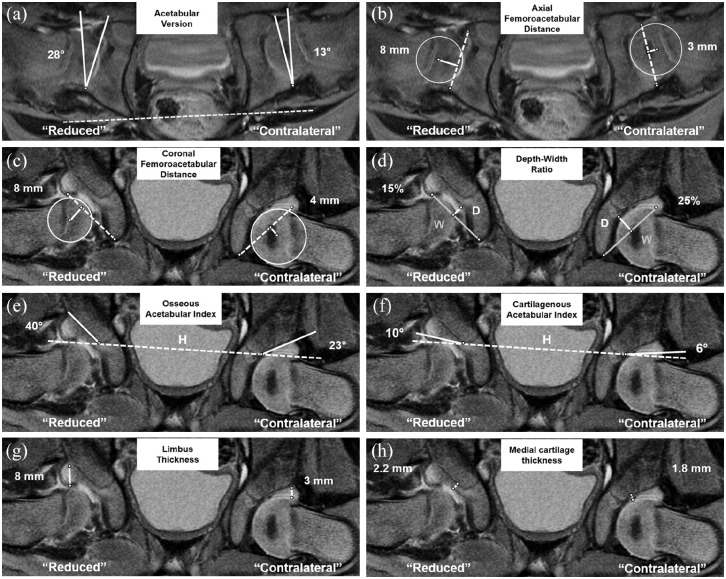
A radiology resident (FS, 6 years of imaging experience) and a research student (JRK, 1 year of imaging experience) assessed the post-reduction MRIs. Both assessors were blinded to each other and underwent formal training with a senior pediatric musculoskeletal radiologist (SDB) using 20 post-reduction MRIs that were not included in the study. Two parameters (acetabular version and axial femoroacetabular distance) were measured on the axial MRI (Table 2). For the axial images, the MRI slice at the level of the femoral head center was used, as previously suggested 5 (Table 2, Figure 2). Acetabular version describes the opening of the cartilaginous acetabulum relative to an anatomical vertical axis, while axial femoroacetabular distance describes the lateralization of the femoral rotation center to a line connecting the anterior and posterior cartilaginous acetabulum. This measurement was adapted from a study assessing acetabular coverage applied in adult patients undergoing MRI for acetabular dysplasia or pincer-type femoroacetabular impingement (FAI). 16 Six parameters (coronal femoroacetabular distance, acetabular depth–width ratio, osseous and cartilaginous acetabular indices, lateral cartilage (limbus) thickness, and medial cartilage thickness) were measured on the coronal MRI view (Table 2, Figure 2). For coronal images, one slice anterior to the mid-coronal position was selected. This slice reflects the middle of the acetabulum and identifies the superior limbus formation/osseous acetabular rim as well as the inferior and superior margins of the triradiate cartilage, which serve as landmarks. 17 In brief, coronal femoroacetabular distance describes the lateralization of the femoral rotation center relative to a line connecting the superior and inferior cartilaginous acetabulum. The acetabular depth–width ratio was adapted from measurements performed on radiographs. 18 The osseous/cartilaginous acetabular indices were respectively defined as the angle between the lateral aspect of the osseous acetabulum/the joint space and Hilgenreiner’s line.5,17 Lateral cartilage (limbus) thickness was measured with a vertical line drawn along the lateral joint space at the transition between labrum and cartilage. Medial cartilage thickness was measured just above the level of the triradiate cartilage with a line drawn perpendicular to the osseous acetabulum along the medial cartilage space.
Table 2.
Measurements of hip morphology on post-reduction MRI.
| Parameter | Orientation | Description of measurement |
|---|---|---|
| Acetabular version (°) | Axial | The lateral aspect of the anterior and posterior cartilage is connected with a line perpendicular to a line connecting the posterior columns of the acetabulum which serves as an anatomic horizontal. |
| Femoroacetabular distance (mm) | Axial | The lateral aspect of the anterior and posterior cartilage is connected with a line and serves as a reference. A circle is drawn to determine the femoral head center. Distance between the rotation center and the reference line is measured with a perpendicular line |
| Femoroacetabular distance (mm) | Coronal | A line is drawn connecting the inferior aspect of the acetabular teardrop with the lateral aspect of the cartilage space and serves as reference. A circle is drawn to determine the femoral head center. Distance between the rotation center and the reference line is measured with a perpendicular line. |
| Acetabular depth–width ratio (depth/width in mm, %) | Coronal | ‘Width’ corresponds to a line connecting the inferior aspect of the acetabular teardrop with the lateral aspect of the cartilage space. ‘Depth’ corresponds to the perpendicular distance between the halfway point of the acetabular width and the triradiate cartilage. |
| Osseous acetabular index (°) | Coronal | A line connecting the inferior margin of the triradiate cartilage with the lateral aspect of the osseous acetabulum is drawn, the Hilgenreiner line (horizontal connection between the inferior margins of the triradiate cartilage) serves as horizontal reference |
| Cartilaginous acetabular index (°) | Coronal | A line connecting the inferior margin of the triradiate cartilage with the lateral aspect of the cartilage space is drawn, the Hilgenreiner line (horizontal connection between the inferior margins of the triradiate cartilage) serves as horizontal reference |
| Limbus thickness (mm) | Coronal | A vertical line is drawn along the lateral joint space at the transition between labrum and cartilage |
| Medial cartilage thickness (mm) | Coronal | Just above the level of the triradiate cartilage a line perpendicular to the osseous acetabulum is drawn along the medial cartilage space |
MRI: magnetic resonance imaging.
Figure 2.
Bilateral MRI measurements are shown in a hip undergoing closed reduction and in the untreated contralateral side. Differences in quantitative parameters are demonstrated with the treated hip showing a greater degree of morphologic instability. (a and b) Axial measurements: (a) Acetabular version is measured as a line connecting anterior and posterior acetabular cartilage perpendicular to a line connecting the posterior acetabular columns (dashed line). (b) Axial femoroacetabular distance corresponds to the perpendicular line between the rotation center and a line connecting anterior and posterior acetabular cartilage (dashed line). (c-g) Coronal measurements are shown. (c) Coronal femoroacetabular distance corresponds to the perpendicular line between the rotation center and a reference line (dashed line) connecting the teardrop with the lateral cartilage space. (d) Depth–width ratio. “Width” (gray line) corresponds to the distance between teardrop and the lateral cartilage space. “Depth” (white line) corresponds to the perpendicular distance between the halfway point of the acetabular width and the triradiate cartilage. (e) Osseous/(f) cartilaginous acetabular index corresponds to the angle between the lateral aspect of the osseus/cartilaginous acetabular edge relative to the Hilgenreiner line (dashed line). (g) Limbus thickness corresponds to a vertical line drawn along the lateral joint space at the transition between labrum and cartilage. (h) Medial cartilage thickness corresponds to a line drawn perpendicular to the osseous acetabulum along the medial cartilage space just above the level of the triradiate cartilage.
Radiographs obtained at the most recent follow-up (minimum 10 years from reduction) were assessed by a radiology resident (FS) with 6 years of experience. The Kalamchi and MacEwen 13 system was used to exclude hips with avascular necrosis. Anteroposterior radiographs of the pelvis were used for the measurement of the lateral-center edge angle (LCEA), 19 the acetabular index of Tönnis, 20 and the assessment of the integrity of Shenton’s line. For patients > 6 years at the time of radiographic imaging, hips were graded into the two radiographic outcome groups according to the Severin 14 classification: For patients < 6 years at the time of radiographic imaging, dysplasia was defined as having acetabular indices exceeding two standard deviations of the age- and sex-specific population-based mean value. 18
Statistical analysis
Continuous characteristics were summarized by mean and standard deviation (SD) or median and interquartile range (IQR), as determined by the data distribution. Categorical and binary characteristics were summarized by frequency and percentage. Demographic and treatment characteristics were summarized by outcome group and compared using Student’s t test, chi-square tests, or Fisher’s exact test, as appropriate. For the outcome analysis, dedicated statistical tests which take the relationship between different parameters into account were used. Post-reduction MRI characteristics and characteristics at final follow-up were summarized and compared across residual dysplasia groups and contralateral hips using binary logistic regression. Post-reduction MRI characteristics were assessed for their association with an increased likelihood of residual dysplasia at follow-up using binary logistic regression with a penalized maximum likelihood estimation methodology. Generalized estimation equation analysis was used to assess factors associated with an increased likelihood of failure on either the treated or the contralateral side taking into account the dependent nature of hips belonging to the same patient. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated.
MRI analysis was performed by two independent raters (FS, JRK) and repeated by one of the raters (FS) for inter- and intra-rater reliability analysis. This was based on a power analysis (46 hips for intraclass correlation coefficient (ICC) > 0.80, alpha 0.05, 80% power). Interpretations of the ICC estimates were based on the scale from Cicchetti and Sparrow: 21 <0.40, poor; 0.40–0.59, fair; 0.60–0.74, good; and >0.74, excellent.
Statistical analysis was performed by a biostatistician (Blinded) using software (SAS, version 9.4; SAS Institute, Cary, NC, USA).
Results
Fifteen (15/28 hips, 54%) hips with Severin ≤ 2 were allocated to the “no residual dysplasia” group. Thirteen (13/28 hips, 46%) hips were allocated to the “residual dysplasia” group (Figure 1). Of these, 5 (5/13 hips, 38%) hips had Severin classification 14 > 2 at the latest follow-up, with a median LCEA of 18° (interquartile range (IQR) 13°–18°) (Table 3). Eight (8/13 hips, 62%) hips underwent subsequent surgery at a median follow-up of 3 (IQR, 2–5) years after reduction. At the time of the subsequent surgery, the median acetabular index was 34° (IQR, 30°–37°), reflecting a median percentile of 99.9 (IQR, 97–100) (Table 3). Typically, residual acetabular dysplasia was treated with an acetabular osteotomy (4/8 hips, 50%) (Tables 1 and 3).
Table 3.
Demographic and radiographic characteristic in the residual dysplasia group.
| Characteristic | Radiographic endpoint (n = 5) | Surgical endpoint (n = 8) | ||||
|---|---|---|---|---|---|---|
| Latest follow-up |
Before subsequent surgery | Latest follow-up |
||||
| Median | IQR | Median | IQR | Median | (IQR) | |
| Age at initial surgery (months) | 10 | 7–13 | 7 | 6–10 | - | |
| Age (years) | 18 | 16–19 | 3 | 2–5 | 13 | 12–13 |
| Follow-up (years) | 16 | 15–17 | 3 | 1–4 | 12 | 11–13 |
| Lateral center edge angle (°) | 18 | 13–18 | 7 | 7–9 | 31 | 24–36 |
| Acetabular index (°) | 20 | 17–20 | 34 | 30–37 | 6 | 4–16 |
| Breach in Shenton’s line (hips, %) | 1 | 20% | 6 | 75% | 2 | 25% |
| Age ≤ 6 years at evaluation (hips, %) | – | 7 | 88% | - | ||
| Percentile acetabular index | – | 99.9 | 97–100 | - | ||
| Percentile acetabular index > 95% (hips, %) | – | 7 | 100% | - | ||
| Age > 6 years at evaluation (hips, %) | 5 | 100% | 1 | 12% | 8 | 100% |
| Severin grade > 2 (hips, %) | 5 | 100% | 1 | 100% | 2 | 25% |
IQR: interquartile range.
Six of the eight parameters differed between hips with and without residual dysplasia, namely, acetabular version (25° ± 6° (95% CI, 22°–29°) vs 20° ± 5° (17°–22°), p = 0.03), axial femoroacetabular distance (6 ± 1 mm (5–7 mm) vs 4 ± 2 mm (3–5 mm), p = 0.01), coronal femoroacetabular distance (7 ± 1 mm (6–7 mm) vs 5 ± 1 mm (4–5 mm), p = 0.006), osseous acetabular index (39° ± 7° (35°–43°) vs 31° ± 7° (27°–35°), p = 0.02), limbus thickness (6 ± 1 mm (5–7 mm) vs 4 ± 1 mm (3°–4 mm), p = 0.02) and medial cartilage thickness (3 ± 1 mm (2–3 mm) vs 2 ± 1 mm (1–2 mm), p = 0.01) (Table 4). All eight MRI parameters differed between hips with residual dysplasia and contralateral uninvolved hips (Table 5). Comparing the hips without residual dysplasia against the contralateral controls, differences were found for five of the eight parameters, namely, acetabular version, coronal femoroacetabular distance, acetabular depth–width ratio, and the osseous and cartilaginous acetabular indices (Table 5). By contrast, no differences were found for axial femoroacetabular distance (4 ± 2 mm vs 3 ± 1 mm (mean difference 1 mm, 95% CI, 0–2 mm, p = 0.05)), limbus thickness (4 ± 1 mm vs 3 ± 1 mm (1 mm, 0–1 mm, p = 0.15)), and medial cartilage thickness (2 ± 1 mm vs 2 ± 1 mm, (1 mm, 0–1 mm, p = 0.26)) (Table 5).
Table 4.
Comparison of MRI parameters between the hips with and without residual dysplasia.
| Groups | Residual dysplasia (n = 13 hips) |
No residual dysplasia (n = 15 hips) |
p | ||
|---|---|---|---|---|---|
| Post-reduction MRI | Mean | ±SD (95% CI) | Mean | ±SD (95% CI) | |
| Acetabular version (°) | 25 | ±6 (22 to 29) | 20 | ±5 (17 to 22) | 0.03 |
| Femoroacetabular distance axial (mm) | 6 | ±1 (5 to 7) | 4 | ±2 (3 to 5) | 0.01 |
| Femoroacetabular distance coronal (mm) | 7 | ±1 (6 to 7) | 5 | ±1 (4 to 5) | 0.006 |
| Acetabular depth–width ratio (%) | 19 | ±6 (15 to 23) | 20 | ±4 (18 to 22) | 0.38 |
| Osseous acetabular index (°) | 39 | ±7 (35 to 43) | 31 | ±7 (27 to 35) | 0.02 |
| Cartilaginous acetabular index (°) | 17 | ±6 (13 to 21) | 14 | ±5 (11 to 17) | 0.17 |
| Limbus thickness (mm) | 6 | ±1 (5 to 7) | 4 | ±1 (3 to 4) | 0.02 |
| Medial cartilage thickness (mm) | 3 | ±1 (2 to 3) | 2 | ±1 (1 to 2) | 0.01 |
| Last radiographic follow-up | Mean | ±SD | Mean | ±SD (95% CI) | p |
| Duration of follow-up (years) | 14 | ±3 (12 to 16) | 13 | ±3 (11 to 14) | 0.16 |
| Lateral center edge angle (°) | 23 | ±11 (17 to 29) | 30 | ±6 (26 to 33) | 0.06 |
| Acetabular index (°) | 13 | ±10 (7 to 19) | 10 | ±6 (6 to 13) | 0.26 |
| Breach in Shenton’s line (hips, %) | 3 | 23% (0% to 46%) | 1 | 7% (–6% to 20%) | 0.24 |
| Severin grade > 2 (hips, %) | 7 | 54% (27% to 81%) | 0 | 0% | <0.001 |
MRI: magnetic resonance imaging; SD: standard deviation; CI: confidence interval.
Table 5.
Paired comparison of MRI parameters between the hips with and without residual dysplasia and uninvolved contralateral hips.
| Groups | Residual dysplasia (n = 13 hips) |
Contralateral hip (n = 10 hips) |
Difference | No residual dysplasia (n = 15 hips) |
Contralateral hip (n = 14 hips) |
Difference | p | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Post-reduction MRI | Mean | ±SD | Mean | ±SD | Mean (95% CI) | p | Mean | ±SD | Mean | ±SD | Mean (95% CI) | |
| Acetabular version (°) | 25 | ±6 | 16 | ±3 | 9 (6 to 12) | 0.003 | 20 | ±5 | 17 | ±4 | 3 (–1 to 7) | 0.047 |
| Femoroacetabular distance axial (mm) | 6 | ±1 | 3 | ±1 | 3 (2 to 5) | 0.01 | 4 | ±2 | 3 | ±1 | 1 (0 to 2) | 0.05 |
| Femoroacetabular distance coronal (mm) | 7 | ±1 | 4 | ±1 | 3 (2 to 4) | <0.001 | 5 | ±1 | 4 | ±1 | 1 (0 to 1) | 0.02 |
| Acetabular depth–width ratio (%) | 19 | ±6 | 27 | ±4 | 8 (4 to 12) | 0.003 | 20 | ±4 | 26 | ±4 | 6 (2 to 10) | 0.002 |
| Osseous acetabular index (°) | 39 | ±7 | 25 | ±5 | 13 (7 to 19) | 0.002 | 31 | ±7 | 26 | ±7 | 5 (0 to 10) | 0.01 |
| Cartilaginous acetabular index (°) | 17 | ±6 | 10 | ±4 | 6 (2 to 10) | 0.008 | 14 | ±5 | 9 | ±4 | 5 (1 to 9) | 0.01 |
| Limbus thickness (mm) | 6 | ±1 | 3 | ±1 | 3 (1 to 4) | 0.003 | 4 | ±1 | 3 | ±1 | 1 (0 to 1) | 0.15 |
| Medial cartilage thickness (mm) | 3 | ±1 | 2 | ±1 | 1 (0 to 1) | 0.004 | 2 | ±1 | 2 | ±1 | 1 (0 to 1) | 0.26 |
| Last radiographic follow-up | Mean | ±SD | Mean | ±SD | Mean (95% CI) | p | Mean | ±SD | Mean | ±SD | Mean (95% CI) | p |
| Lateral center edge angle (°) | 23 | ±11 | 27 | ±5 | 1 (–6 to 8) | 0.06 | 30 | ±6 | 29 | ±8 | 2 (–2 to 5) | 0.42 |
| Acetabular index (°) | 13 | ±10 | 9 | ±4 | 1 (–5 to 7) | 0.09 | 10 | ±6 | 8 | ±6 | 2 (2 to 6) | 0.44 |
| Breach in Shenton’s line (hips, %) | 3 | 23% | 0 | 0% | 23% (0% to 46%) | 0.24 | 1 | 7% | 0 | 0% | 7% (–7% to 21%) | 1 |
| Severin grade > 2 (hips, %) | 7 | 54% | 0 | 0% | 54% (27% to 81%) | <0.001 | 0 | 0% | 0 | 0% | 0% | 1 |
MRI: magnetic resonance imaging; SD: standard deviation; CI: confidence interval.
Logistic regression analysis revealed that limbus thickness had the largest effect (OR = 12.5; p < 0.001), followed by coronal (OR = 7.68; p < 0.001) and axial (OR = 2.7; p = 0.001) femoroacetabular distance for increased likelihood of residual dysplasia at a minimum 10-year follow-up (Table 6).
Table 6.
Association of MRI measurements with an increased likelihood of residual dysplasia at 10-year follow-up.
| Post-reduction MRI | OR | 95% CI | p |
|---|---|---|---|
| Acetabular cartilage version | 1.17 | 1.03-1.39 | 0.02 |
| Femoroacetabular distance axial | 2.70 | 1.39-7.93 | 0.001 |
| Femoroacetabular distance coronal | 7.68 | 2.38-54.68 | <0.001 |
| Acetabular depth–width ratio | 0.94 | 0.80-1.08 | 0.41 |
| Osseous acetabular index | 1.20 | 1.05-1.47 | 0.004 |
| Cartilaginous acetabular index | 1.09 | 0.96-1.29 | 0.18 |
| Limbus thickness | 12.49 | 2.78-283.10 | <0.001 |
| Medial cartilage thickness | 9.12 | 1.91-91.16 | 0.002 |
MRI: magnetic resonance imaging; OR: odds ratio; CI: confidence interval.
The intra-rater and inter-rater reliabilities were poor and fair for the measurement of the medial cartilage thickness (ICC of 0.30 and 0.06) and acetabular depth–width ratio (ICC of 0.57 and 0.56). By contrast, the intra-and inter-rater reliabilities ranged from good to excellent for the remaining six parameters (Table 7).
Table 7.
Inter- and intra-rater reliability for post-reduction MRI measurements.
| Intra-rater reliability | Inter-rater reliability | |||
|---|---|---|---|---|
| Post-reduction MRI | ICC | 95% CI | ICC | 95% CI |
| Acetabular version | 0.79 | 0.65 to 0.88 | 0.76 | 0.56 to 0.87 |
| Femoroacetabular distance axial | 0.84 | 0.72 to 0.91 | 0.86 | 0.75 to 0.92 |
| Femoroacetabular distance coronal | 0.84 | 0.73 to 0.91 | 0.84 | 0.71 to 0.91 |
| Acetabular depth–width ratio | 0.57 | 0.34 to 0.74 | 0.56 | 0.21 to 0.76 |
| Osseous acetabular index | 0.73 | 0.57 to 0.84 | 0.70 | 0.45 to 0.83 |
| Cartilaginous acetabular index | 0.76 | 0.61 to 0.86 | 0.75 | 0.54 to 0.86 |
| Limbus thickness | 0.77 | 0.62 to 0.87 | 0.77 | 0.58 to 0.87 |
| Medial cartilage thickness | 0.30 | 0.01 to 0.54 | 0.06 | −0.71 to 0.48 |
MRI: magnetic resonance imaging; ICC: intraclass correlation coefficient; CI: confidence interval.
Discussion
To optimize the remodeling of the acetabulum, it is important to confirm that the femoral head has been concentrically reduced following the closed or open reduction of the dislocated hip. MRI has gained popularity over post-reduction CT scans due to its increasing availability and minimization of patients’ exposure to ionizing radiation.2,22,23 Post-reduction MRI has the additional benefit of improved soft tissue and cartilage analysis. Potentially, the role of post-reduction MRI could be expanded beyond the dichotomous assessment of acceptable versus non-acceptable reduction, incorporating measurements of the femoral head position and acetabular morphology, which may have long-term implications for joint development. However, there is a paucity of information on how specific MRI measurements associate with acetabular development after closed or open reduction. Notably, previous studies found no anatomic factors could predict the need for future hip surgery.8,12 To address this gap, the current study investigated 28 children with unilateral DDH who underwent an MRI after closed or open hip reduction and were followed up for a minimum of 10 years. Based on a set of parameters quantifying the quality of the reduction and the acetabular morphology on the post-reduction MRI, we demonstrated that they presented differences between hips that developed residual acetabular dysplasia in the long term and uninvolved contralateral hips. Furthermore, we identified specific post-reduction MRI parameters that differed between hips with and without residual acetabular dysplasia at minimum of 10-year follow-up.
All measurements assessing acetabular morphology were different between hips with residual acetabular dysplasia and contralateral uninvolved normal hips. Although this finding was expected, it was important to compare hips that developed residual acetabular dysplasia with normal contralateral hips as a proof of concept that these measurements indeed depict the abnormal morphology of a dysplastic acetabulum in infant hips with DDH. Notably, the coronal and axial femoroacetabular distance, medial and lateral cartilage (limbus) thickness, acetabular version, and osseous acetabular index were different between hips with and without residual dysplasia at a minimum 10-year follow-up. In contrast, previous studies have failed to link morphological parameters with residual acetabular dysplasia.5,8 Duffy et al., 5 investigating 59 patients with DDH (73 dislocated hips) treated with open or closed reduction and undergoing post-reduction MRI, found significant differences in the cartilaginous morphology of dysplastic acetabular compared with uninvolved contralateral hips. However, they could not find a correlation between the bony or cartilaginous parameters measured on the post-reduction MRI and the need for surgery for residual dysplasia. In another study, Mitchell et al. 8 compared post-reduction MRI for 13 hips in which acetabular dysplasia had resolved by age 4 and five hips that developed residual dysplasia and underwent pelvic osteotomy. Although the post-reduction MRI identified several morphological changes to the acetabulum, none of the measured variables was associated with the long-term outcomes, and the authors were unable to identify which anatomical features could predict whether the acetabulum would or would not remain dysplastic.
Our study further determined that limbus thickness is an independent factor associated with the risk of developing residual acetabular dysplasia in the long term following open or closed reduction. Notwithstanding the controversy surrounding the definition of the limbus in the literature, it has been described as proliferative tissue composed of cellular hyaline cartilage at the superior and posterior aspects of the acetabulum that develops in DDH. 24 It should be noted that hips with a thicker limbus laterally potentially have a more severe degree of dysplasia and, hence, less capacity for acetabular remodeling following closed or open reduction. However, further longitudinal studies with a larger patient population are warranted to confirm whether the limbus thickness is predictive of acetabular remodeling after reduction.
In a clinical setting, it may be over-laborious and unrealistic to measure all the parameters described here. Based on the inter- and intra-rater agreement, we found good or excellent agreement for most of our parameters, except medial cartilage thickness and the acetabular depth–width ratio, which had fair and poor reliability, respectively, suggesting their unsuitability for use in clinical settings. Our findings are in line with a previous study investigating the reliability of indices measured on infant hip spica MRI, which found good and excellent agreement for coronal acetabular index and acetabular version, respectively, yet poor agreement for acetabular depth. 7 Meanwhile, a study in the early 2000s reported poor repeatability, particularly for transverse plane measurements and cartilaginous measurements. 5 We found excellent reliability when measuring the quality of the reduction and the position of the femoral head in relation to the acetabulum (femoroacetabular distance) in the axial and coronal planes. Furthermore, the femoroacetabular distance was significantly greater in hips with residual acetabular dysplasia compared with those without dysplasia. Therefore, we believe that femoroacetabular distance should be implemented in clinical settings to quantify the position of the femoral head as it provides more information than the simplistic qualitative discrimination of the hip being reduced versus not being concentrically reduced. In addition to the femoroacetabular distance, we propose lateral limbus thickness as an important parameter to measure in clinical settings to assess the morphology of the acetabulum post-reduction. With the given sample size and the multiple parameters assessed, it was not possible to perform a more comprehensive analysis such as to define a combination of the prognostic parameters. Further prospective investigation is needed to determine the threshold values of these parameters before any recommendations can be made regarding the acceptable degree of reduction and limbus thickness.
Our study has several limitations. First, we assessed only patients who had post-reduction MRI as well as radiographs taken at a minimum 10-year follow-up, which limited the number of hips available for our study and introduces risk of a selection bias since we could not analyze the entire patient cohort. We deliberately chose a longer follow-up due to the controversy surrounding how long the acetabulum continues to remodel following reduction. Since the goal of this study was not to explicitly assess the outcome of open or closed reduction, this limitation may be considered acceptable, as the primary objective was to compare MRI hip morphology in patients with and without residual DDH. Second, we did not have follow-up radiographs for 35 (37%) of our patients which had to be excluded, raising concerns about bias. Our institution is a tertiary referral center and several of the patients come from out of state, limiting our ability to follow all patients in the long term. Third, only one post-reduction MRI was available per patient; if additional prospective MRI scans had been available, we might have identified different factors associated with acetabular development. However, the costs of performing multiple subsequent MRIs are prohibitive and this practice has not been the standard of care at our institution. Fourth, it is possible that the assessors measuring the post-reduction MRI and follow-up radiographs introduced bias. To reduce the risk of assessor bias, the reading of the radiographs was independent and blinded to MRI readings. Finally, we used two criteria to define patients with residual acetabular dysplasia, that is, the Severin classification 14 at a minimum of 10 years after the reduction and patients undergoing a procedure to treat dysplasia during childhood. Surgical treatment as a criterion of residual dysplasia poses a risk of selection bias as it depends on the surgeon’s indication. However, we carefully reviewed the radiographs of all patients who had undergone surgical treatment and found that all patients receiving surgical treatment had an acetabular index value above two standard deviations from the mean, which is classically considered a diagnostic for residual dysplasia. 18
In conclusion, we identified a series of acetabular morphology and reduction quality parameters that can be reliably measured on the post-reduction MRI to facilitate the differentiation between hips that develop with and without residual acetabular dysplasia at minimum of 10 years postoperative. We also found that increased limbus thickness is an independent factor predictive of residual acetabular dysplasia. This work provides a framework for future longitudinal studies investigating the role of post-reduction MRI in identifying hips at risk of residual acetabular dysplasia, presenting limbus thickness as a promising parameter to predict residual dysplasia.
Footnotes
Authors’ note: This study was performed at the Department of Orthopaedic Surgery, Boston Children’s Hospital, Harvard Medical School.
Author contributions: Florian Schmaranzer: study design, data acquisition, data analysis and interpretation, drafting and critical revision of the manuscript, approved final version of the manuscript
Pedro Justo: study design, data acquisition, data analysis and interpretation, drafting and critical revision of the manuscript, approved final version of the manuscript
Jennifer R Kallini: study design, data acquisition, data analysis and interpretation, drafting and critical revision of the manuscript, approved final version of the manuscript
Marianna G Ferrer: study design, data acquisition, data analysis and interpretation, drafting and critical revision of the manuscript, approved final version of the manuscript
Patricia E Miller: study design, data analysis and interpretation, drafting and critical revision of the manuscript, approved final version of the manuscript
Travis Matheney: study design, data analysis and interpretation, drafting and critical revision of the manuscript, approved final version of the manuscript
Sarah D Bixby: study design, data acquisition, drafting and critical revision of the manuscript, approved final version of the manuscript
Eduardo N Novais: study design, data acquisition, data analysis and interpretation, drafting and critical revision of the manuscript, approved final version of the manuscript
Compliance with ethical standards: The authors confirm that this retrospective study involving human participants was performed in compliance with the Helsinki declaration following IRB approval issued from of Boston Children’s Hospital, Harvard Medical school with a waiver for written informed consent.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: One of the authors (FS) states that he received financial support of the Swiss National Science Foundation (Grant No. P1BEP3_181643) during the conduction of this study. Each author certifies that he or she, or a member of their immediate family, has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
References
- 1. Weinstein SL, Mubarak SJ, Wenger DR. Developmental hip dysplasia and dislocation: part II. Instr Course Lect 2004; 53: 531–542. [PubMed] [Google Scholar]
- 2. Chin MS, Betz BW, Halanski MA. Comparison of hip reduction using magnetic resonance imaging or computed tomography in hip dysplasia. J Pediatr Orthop 2011; 31(5): 525–529. [DOI] [PubMed] [Google Scholar]
- 3. Chin MS, Shoemaker A, Reinhart DM, et al. Use of 1.5 Tesla and 3 Tesla MRI to evaluate femoral head reduction in hip dysplasia. J Pediatr Orthop 2011; 31(6): 633–637. [DOI] [PubMed] [Google Scholar]
- 4. Dibello D, Odoni L, Pederiva F, et al. MRI in postreduction evaluation of developmental dysplasia of the hip. J Pediatr Orthop 2019; 39(9): 449–452. [DOI] [PubMed] [Google Scholar]
- 5. Duffy CM, Taylor FN, Coleman L, et al. Magnetic resonance imaging evaluation of surgical management in developmental dysplasia of the hip in childhood. J Pediatr Orthop 2002; 22(1): 92–100. [PubMed] [Google Scholar]
- 6. Gould SW, Grissom LE, Niedzielski A, et al. Protocol for MRI of the hips after spica cast placement. J Pediatr Orthop 2012; 32(5): 504–509. [DOI] [PubMed] [Google Scholar]
- 7. Jaremko JL, Wang CC, Dulai S. Reliability of indices measured on infant hip MRI at time of spica cast application for dysplasia. Hip Int 2014; 24(4): 405–416. [DOI] [PubMed] [Google Scholar]
- 8. Mitchell PD, Chew NS, Goutos I, et al. The value of MRI undertaken immediately after reduction of the hip as a predictor of long-term acetabular dysplasia. J Bone Joint Surg Br 2007; 89(7): 948–952. [DOI] [PubMed] [Google Scholar]
- 9. Ranawat V, Rosendahl K, Jones D. MRI after operative reduction with femoral osteotomy in developmental dysplasia of the hip. Pediatr Radiol 2009; 39(2): 161–163. [DOI] [PubMed] [Google Scholar]
- 10. Rosenbaum DG, Servaes S, Bogner EA, et al. MR imaging in postreduction assessment of developmental dysplasia of the hip: goals and obstacles. Radiographics 2016; 36(3): 840–854. [DOI] [PubMed] [Google Scholar]
- 11. Westhoff B, Wild A, Seller K, et al. Magnetic resonance imaging after reduction for congenital dislocation of the hip. Arch Orthop Trauma Surg 2003; 123(6): 289–292. [DOI] [PubMed] [Google Scholar]
- 12. Shirai Y, Wakabayashi K, Wada I, et al. Magnetic resonance imaging evaluation of the labrum to predict acetabular development in developmental dysplasia of the hip: a STROBE compliant study. Medicine 2017; 96(21): e7013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kalamchi A, MacEwen GD. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am 1980; 62(6): 876–888. [PubMed] [Google Scholar]
- 14. Severin E. Congenital dislocation of the hip; development of the joint after closed reduction. J Bone Joint Surg Am 1950; 32-A(3): 507–518. [PubMed] [Google Scholar]
- 15. Tiderius C, Jaramillo D, Connolly S, et al. Post-closed reduction perfusion magnetic resonance imaging as a predictor of avascular necrosis in developmental hip dysplasia: a preliminary report. J Pediatr Orthop 2009; 29(1): 14–20. [DOI] [PubMed] [Google Scholar]
- 16. Pfirrmann CW, Mengiardi B, Dora C, et al. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology 2006; 240(3): 778–785. [DOI] [PubMed] [Google Scholar]
- 17. Huber H, Mainard-Simard L, Lascombes P, et al. Normal values of bony, cartilaginous, and labral coverage of the infant hip in MR imaging. J Pediatr Orthop 2014; 34(7): 674–678. [DOI] [PubMed] [Google Scholar]
- 18. Novais EN, Pan Z, Autruong PT, et al. Normal percentile reference curves and correlation of acetabular index and acetabular depth ratio in children. J Pediatr Orthop 2018; 38(3): 163–169. [DOI] [PubMed] [Google Scholar]
- 19. Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand 1939; 83: 58. [Google Scholar]
- 20. Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. Berlin: Springer, 1987. [Google Scholar]
- 21. Cicchetti DV, Sparrow SA. Developing criteria for establishing interrater reliability of specific items: applications to assessment of adaptive behavior. Am J Ment Defic 1981; 86(2): 127–137. [PubMed] [Google Scholar]
- 22. Bachy M, Thevenin-Lemoine C, Rogier A, et al. Utility of magnetic resonance imaging (MRI) after closed reduction of developmental dysplasia of the hip. J Child Orthop 2012; 6(1): 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Barkatali BM, Imalingat H, Childs J, et al. MRI versus computed tomography as an imaging modality for postreduction assessment of irreducible hips in developmental dysplasia of the hip: an interobserver and intraobserver reliability study. J Pediatr Orthop B 2016; 25(6): 489–492. [DOI] [PubMed] [Google Scholar]
- 24. Ponseti IV. Morphology of the acetabulum in congenital dislocation of the hip. Gross, histological and roentgenographic studies. J Bone Joint Surg Am 1978; 60(5): 586–599. [PubMed] [Google Scholar]