Abstract
Purpose:
In this study, we investigated the relationship between the results of thoracic curve correction using minimally invasive surgeries in 35 patients and open surgical correction in 47 patients with adolescent idiopathic scoliosis.
Methods:
The correlations between the Cobb’s angle of the primary and postoperative curves, angle of thoracic kyphosis and lumbar lordosis, correction percentage, derotation values, estimated blood loss, duration of surgery, and period of hospitalization after surgery were assessed by calculating the mean and standard deviation. Calculation and comparison were performed using Pearson correlation.
Results:
The Cobb’s angle correction ranged from 53.4° ± 11.8° to 6.7° ± 5.2° (p < 0.001) in the open surgical correction group and from 51.2° ± 11.4° to 11.7° ± 5.8° (p < 0.001) in the minimally invasive surgery group before and after surgery, respectively. The percentage of curvature correction was 88.2% ± 8.0% and 77.7% ± 10.7% (p < 0.001) in the open surgical correction and minimally invasive surgery groups, respectively. The estimated blood loss was higher in the open surgical correction group than in the minimally invasive surgery group (208.7 ± 113.4 vs 564.3 ± 242.7 mL). Axial rotation was changed from 29.1°± 7.5 to 17.1°± 6.8 (p < 0.001) in the open surgical correction group and from 28.9°± 7.8 to 19.4°± 6.4 (p < 0.001) in the minimally invasive surgery group. The duration of surgery was shorter in the open surgical correction group than in the minimally invasive surgery group (266.6 ± 64.3 vs 346.2 ± 70.5 min). A positive correlation between time of operation and Cobb’s angle correction (in °) in open surgical correction (r = 0.37) and minimally invasive surgery (r = 0.43) was found.
Conclusion:
The open surgical correction procedures were more effective than minimally invasive surgery in correcting the spinal curve. The increase in the duration of open surgical correction increases the estimated blood loss, but it also more significantly improves the correction of Cobb’s angle.
Level of evidence:
III.
Keywords: Adolescent idiopathic scoliosis, minimally invasive surgeries, open surgical correction, estimated blood loss, duration of surgery, Cobb’s angle
Introduction
Adolescent idiopathic scoliosis (AIS) is a form of idiopathic scoliosis that causes physical and emotional pain, as well as surgery. When Cobb’s curve is more than 45°, 1 surgery is often utilized to treat AIS. 1 The amount of blood loss and the length of the procedure have a direct relationship with the short-term result of surgery. As the number of vertebral levels included in the fusion increases, the amount of blood lost also increases. 2 Since spinal surgery is linked to a high rate of blood transfusions, numerous options for minimizing the bleeding have been proposed, including endoscopic spine surgery, minimally invasive, micro-invasive, and/or laser spine surgery.3,4 Minimally invasive surgery (MIS) with a minimal operative approach results in less tissue trauma, less hospitalization time, and less blood volume loss. There are conflicting data outcomes regarding the effects of MIS for curve correction versus open surgery; so more research is required before conclusive clinical recommendations can be made. 5
Selective thoracic fusion prevents Cobb’s angle aggravation and even causes spontaneous axial derotation of the lumbar curves. 6 The duration of the operation and the surgeon’s experience with the MIS technique may be related to divisive treatment outcomes. Despite a large number of studies on the influence of various factors in reconstructive spine surgery, little is known about the advantages of long-term correction in the MIS technique. This enables less traumatic access as compared to short-term surgical operation by open surgical correction (OSC) with a large incision to postoperative patient outcomes.
As a result, the goal of this study was to determine the optimal duration of surgical management of AIS by OSC and MIS, as well as whether there was a link between additional different factors and postoperative clinical outcomes.
Materials and methods
The retrospective study included 82 patients who had undergone surgical treatment for AIS at The Federal State Budgetary Institution “Federal Center for Traumatology, Orthopedics, and Arthroplasty” in Cheboksary, Russia, between 2014 and 2020. The following are the patient selection criteria: AIS Lenke type 1 dextral curves and Cobb’s angle 30° to 77°, lumbar spine modifier A, B, or C. According to the type of surgical intervention, all patients were divided into two groups.
The first group consisted of 35 patients (31 females and 4 males) with an average age of 15.7 ± 1.5 years (range, 13–18 years) who had undergone OSC of AIS. The second group of 47 patients (44 females and 3 males) underwent MIS for AIS, with an average age during the treatment was 16.1 ± 2.2 years (range, 10–22 years). All the patients had preoperative antero-posterior and lateral scoliosis radiographs. Standard radiographic parameters were assessed, including the pre- and postoperative coronal curve, sagittal vertical axis, and lumbar lordosis (LL). All patients underwent pre- and postoperative computed tomography of the vertebra to assess vertebral rotation of the apex of the deformity by the Aaro-Dalborn method. Bending X-rays with assessment of the lateral bending angle were performed on the preoperative side to assess the flexibility of curves and determine the level of fixation (Table 1).
Table 1.
Demographic, clinical, and treatment data of patients with AIS.
| OSC | MIS | p-value | |
|---|---|---|---|
| Mean age | 15.7 ± 1.5 | 16.1 ± 2.2 | ns |
| Female/male | 31/4 | 44/3 | – |
| Cobb’s angle correction (°) | 46.7 ± 9.2 | 40.5 ± 10.2 | 0.005 |
| Cobb’s angle correction (%) | 88.2 ± 8.0 | 77.7 ± 10.7 | <0.001 |
| Axial rotation correction (°) | 12.0 ± 5.0 | 9.0 ± 5.4 | 0.003 |
| Axial rotation correction (%) | 42.0 ± 14.5 | 30.8 ± 15.3 | 0.002 |
| Lateral bending (°) | 29.17 ± 14.06 | 22.45 ± 10.74 | 0.029 |
| EBL (mL) | 564.3 ± 242.7 | 208.7 ± 113.4 | <0.001 |
| Duration of operation (min) | 266.6 ± 64.3 | 346.2 ± 70.5 | <0.001 |
| Number of levels fused | 10.7 ± 1.7 | 10.4 ± 0.8 | ns |
| Mean length of inpatient stay (days) | 11.2 ± 1.4 | 8.1 ± 1.6 | <0.001 |
AIS: adolescent idiopathic scoliosis; EBL: estimated blood loss; MIS: minimally invasive surgery; OSC: open surgical correction; SD: standard deviation; ns: not significant.
Data are expressed as the mean ± SD and were compared by Student’s t-test.
OSC was carried out using the single posterior approach, as previously described.6,7 In OSC, the following corrective maneuvers were used: the axial translation technique in the concave side, blocking apical vertebral derotation using a Vertebral Column Manipulator device. MIS included a procedure with three posterior skin incisions, muscle-splitting alternately to the convex and concave sides of the spine. In the case of OSC, the screws were inserted first and the bone graft was set up after all corrections only. Whereas in MIS, screw channels were performed first and then markers were set up and only after that were a bone graft placed. This procedure was repeated in all three approaches, following pedicle screw (PS) installation for spinal fusion and correction with MIS devices. 8 First, the correction is performed on the convex side and then on the concave side. For MIS, the following maneuvers were used: inserting the rod on the convex side and the derotation maneuver using the vertical alignment technique. The angle of the primary curve, thoracic kyphosis (TK) and LL parameters before and after surgery, correction and derotation values, blood loss, manipulation duration, and hospitalization period after surgery were all assessed. The mean follow-up period was 101.3 ± 5.9 months in OSC and 47.2 ± 13.3 months in MIS group. All surgical procedures in this study were performed by the same surgeon with more than 4 years of experience in MIS.
The mean and standard deviation (SD) were calculated to assess the difference between the two groups, OSC and MIS. Student’s t-test was used to compare data between the groups, and a p-value below 0.05 was considered statistically significant. The Pearson correlation test was used to assess the relationship between different sets of variables in OSC or MIS, separately for each group. The indicators included Cobb’s angle correction in degrees and percent, rotation correction in degrees and percent, estimated blood loss (EBL), duration of surgery, duration of patient stay, number of vertebrae fused, and age at the time of operation. The r coefficient value between 0.90 and 1.00 (−0.90 to −1.00) was considered a very strong positive (negative) correlation, respectively, 0.70 and 0.90 (−0.70 to −0.90) as strong positive (negative) correlation with a marked relationship, 0.40 and 0.70 (−0.40 to −0.70) as moderate positive (negative) with substantial relationship, 0.20 and 0.40 (−0.20 to −0.40) as weak correlation, and 0 and 0.20 (0 to −0.20) as a very weak correlation. 9 For the Pearson correlation test, the p-value was calculated. The assessment was additionally performed for OSC, by calculating the ratio of the number of vertebrae fused to the correction of Cobb’s angle in % with following linear regression analysis to obtain the best predictive equation model.
Results
All surgical procedures in this study were carried out by the same surgeons. In the coronal plane, the preoperative Cobb’s angle in the first group was 53.4° ± 6.7° (range, 36°–75°); and in the second, it was 52.2° ± 11.3° (range, 30°–77°). After surgery, the Cobb’s angle decreased in the first group to 6.7° ± 5.2° and 11.7° ± 5.8° (p = 0.0002) in the second group. The estimated correction angle and percentage after surgery were significantly higher in the OSC group (46.7° ± 9.2° and 88.2% ± 8.0%, respectively) than in the MIS group (40.5° ± 10.2° and 77.6% ± 10.7%, p = 0.005 and p < 0.001, respectively). The first group’s TK ranged from 14.3° ± 10.2° to 18.4° ± 4.8° (p = 0.014) and the second group’s TK ranged from 17.7° ± 10.0° to 13.8° ± 6.2°. LL changed correspondingly from 53.4° ± 11.4° to 49.3° ± 8.0° in the ORS group and from 55.0° ± 9.4° to 44.3° ± 8.4° (<0.0001) in MIS group. The first group had more apical vertebral derotation 12.0° ± 5.0° (42.0% ± 14.5%, p = 0.003) versus 9.0° ± 5.4° (30.2% ± 15.3%, 0.002) (Table 2).
Table 2.
Preoperational and postoperative curve parameters for patients with AIS treated by MIS or OSC.
| OSC | MIS | OSC/MIS | ||||||
|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative |
p Pre-op/post-op |
Preoperative | Postoperative |
p Pre-op/post-op |
p Preoperative |
p Postoperative |
|
| Cobb’s angle (°) | 53.4 ± 11.7 | 6.7 ± 5.2 | <0.001 | 52.2 ± 11.3 | 11.7 ± 5.8 | <0.001 | ns | <0.001 |
| Compensatory curve (°) | 17.0 ± 21.1 | 2.8 ± 5.4 | 0.04 | 37.8 ± 7.5 | 11.8 ± 7.6 | <0.001 | <0.001 | <0.001 |
| Thoracic kyphosis (TK) (°) | 14.3 ± 10.2 | 18.4 ± 4.8 | 0.01 | 17.7 ± 10.0 | 13.8 ± 6.2 | 0.07 | 0.13 | <0.001 |
| Lumbar lordosis (LL) (°) | 53.4 ± 11.4 | 49.3 ± 8.0 | ns | 55.0 ± 9.4 | 44.3 ± 8.4 | <0.001 | ns | 0.02 |
| Axial rotation (AR) (°) | 29.1 ± 7.5 | 17.1 ± 6.8 | <0.001 | 28.9 ± 7.8 | 19.9 ± 6.4 | <0.001 | ns | 0.04 |
AIS: adolescent idiopathic scoliosis; MIS: minimally invasive surgeries; OSC: open surgical correction; SD: standard deviation; ns: not significant.
Data are expressed as the mean ± SD and were compared by Student’s t-test.
The EBL decreased when the MIS technique was used (208.7 ± 113.4 mL vs 564.3 ± 242.7 mL in the OSC group, p < 0.001). The OSC group had a shorter surgery time (266.6 ± 64.3 min) than that of the MIS group (346.2 ± 70.5 min) (p < 0.001). There was no significant difference in the number of levels fused between OSC and MIS groups. The number of days after surgery in hospitals with the first group was 11.2 ± 1.4 days, while in the second group it was 8.1 ± 1.6 days (p < 0.001) (Tables 1 and 2).
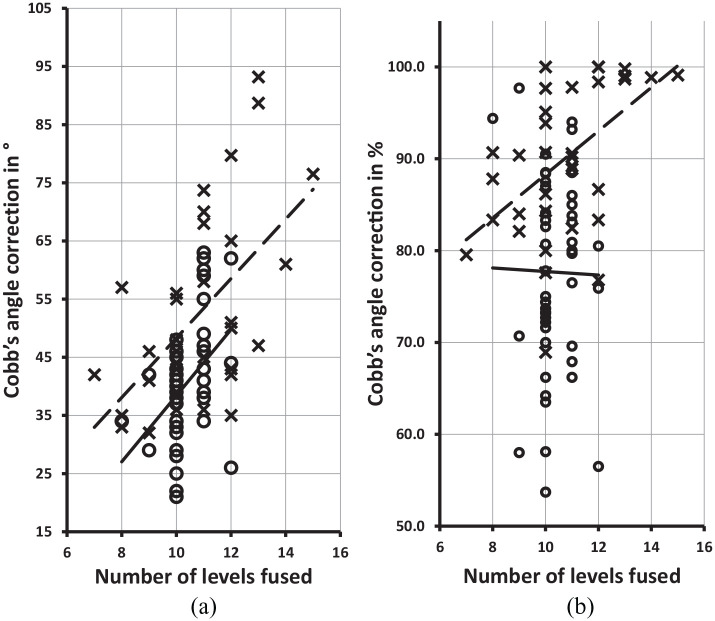
The correlation analysis discovered a moderately positive correlation between: (1) positive correction of rotation in degree and Cobb’s angle correction in degree after OSC (r = 0.33, p = 0.06, respectively) or MIS (r = 0.34, p = 0.02); (2) between the duration of surgery and the results of correction of primary Cobb’s angle in degrees in both groups (OSC: r = 0.37, p = 0.03 and MIS: r = 0.43, p = 0.002); (3) EBL and operation time in both groups (OSC: r = 0.35, p = 0.04 and MIS: r = 0.58, p < 0.001) (Table 3; Figure 1); (4) EBL and Cobb’s angle correction in degree in MIS group (r = 0.33, p = 0.02); (5) EBL and inpatient stay in OSC group (r = 0.3, p = 0.08); (6) EBL and the number of vertebrae fused in OSC group (r = 0.41, p = 0.02); (7) EBL and number of vertebrae fused in OSC group (r = 0.41, p = 0.02); (8) number of vertebrae fused and Cobb’s angle correction in degree in MIS group (r = 0.44, p = 0.002); (9) number of vertebrae fused and operation time in OSC group (r = 0.65, p < 0.001); (10) number of vertebrae fused and mean length of inpatient stay in OSC group (r = 0.44, p = 0.008); and (11) negative correlation between age and Cobb’s angle correction in degree in MIS group (r = 0.3, p = 0.05, r = 0.33, p = 0.02) (Table 3; Figure 2). Simple linear regression analysis indicated that the independent predictive variable number of vertebrae fused in OSC was strongly related to Cobb’s angle correction in degree or percent per vertebra. In the case of MIS, Cobb’s angle correction is less increased, and the number of vertebrae fused did not change the percent of correction (Figure 2).
Table 3.
Calculation of the correlation (r) between different factors in MIS and OSC compared by the Pearson correlation test.
| Correction of Cobb’s angle (°) | Correction of Cobb’s angle (%) | Rotation correction (°) | Rotation correction (%) | EBL (mL) | Duration of surgery (min) | Inpatient stay | Number of vertebrae fused | ||
|---|---|---|---|---|---|---|---|---|---|
| Correction of Cobb’s angle (%) | MIS |
0.48 p < 0.001 |
1 | ||||||
| OSC | –0.04p = 0.84 | 1 | |||||||
| Rotation correction (°) | MIS |
0.34 p = 0.02 |
–0.08p = 0.57 | 1 | |||||
| OSC |
0.33 p = 0.06 |
0.05p = 0.79 | 1 | ||||||
| Rotation correction (%) | MIS | 0.05p = 0.74 | 0.02p = 0.17 |
0.83 p < 0.001 |
1 | ||||
| OSC | 0.05p = 0.77 | 0.26p = 0.13 |
0.76 p < 0.001 |
1 | |||||
| EBL (mL) | MIS |
0.33 p = 0.02 |
0.14p = 0.34 | 0.15p = 0.30 | 0.06p = 0.69 | 1 | |||
| OSC | 0.11p = 0.54 | –0.04p = 0.84 | 0.25p = 0.14 | 0.14p = 0.41 | 1 | ||||
| Duration of surgery (min) | MIS |
0.43 p = 0.002 |
0.25p = 0.09 | 0.09p = 0.56 | –0.06p = 0.65 |
0.58 p < 0.001 |
1 | ||
| OSC |
0.37 p = 0.03 |
–0.36 p = 0.04 |
0.06p = 0.71 | –0.16p = 0.37 |
0.35 p = 0.05 |
1 | |||
| Inpatient stay | MIS | –0.01p = 0.93 | 0.12p = 0.43 | –0.15p = 0.31 | 0.12p = 0.43 | 0.01p = 0.98 | 0.04p = 0.78 | 1 | |
| OSC | 0.02p = 0.89 | 0.23p = 0.19 | –0.07p = 0.69 | 0.11p = 0.51 |
0.30 p = 0.08 |
0.21p = 0.23 | 1 | ||
| Number of vertebrae fused | MIS |
0.44 p = 0.002 |
–0.01p = 0.92 | 0.23p = 0.11 | –0.03p = 0.82 | 0.14p = 0.36 | 0.25p = 0.09 | –0.27p = 0.06 | 1 |
| OSC | 0.20p = 0.25 | –0.08p = 0.65 | –0.06p = 0.74 | –0.26p = 0.13 |
0.41 p = 0.02 |
0.65 p < 0.001 |
0.44 p = 0.008 |
1 | |
| Age | MIS | –0.28 p = 0.05 |
0.33 p = 0.02 |
–0.22p = 0.13 | –0.14p = 0.33 | –0.07p = 0.66 | –0.08p = 0.56 | –0.17p = 0.24 | –0.12p = 0.44 |
| OSC | –0.23p = 0.17 | –0.17p = 0.33 | –0.03p = 0.83 | –0.16p = 0.36 | –0.08p = 0.65 | 0.07p = 0.70 | –0.05p = 0.79 | 0.01p = 0.94 |
EBL: estimated blood loss; MIS: minimally invasive surgery; OSC: open surgical correction.
Figure 1.

Linear regression analysis between the EBL (in mL) and duration of operation (in min) by using MIS (bottom solid line, circles) or OSC (upper discontinuous line).
Figure 2.
Linear regression analysis between the number of vertebrae fused and Cobb’s angle correction in degree (a) or percent (b) by using OSC (upper discontinuous line, crosses in both graphs) and MIS (bottom solid line, circles in both graphs).
Discussion
In this study, the correction gained with ORS was better than with MIS which can be explained by improved access to the vertebra for joint and ligament release. These findings are supported by other studies that found better deformity correction with OSC than with MIS. 10 Uribe et al. found opposite results in angle change after surgery: −22° in MIS surgery and −14° in OSC surgery, but in this study the MIS and groups had more fused interbody levels, that is, 4.5 than in the OSC group, that is, 1.6. However, this study did not take into account that correction angle per vertebra was still better in OSC group. 11 Despite a positive relationship between the number of vertebrae fused and the correction of Cobb’s angle in degrees, a negative relationship was found for the correction of Cobb’s angle in percent in MIS. As shown by additional regression analysis, this finding can be explained by the fact that each subsequent fusion of the vertebrae contributes less to the correction of the angle. Navigation based on intraoperative 3D imaging can help to achieve more precise instrumented fusion. 8
Our findings support this approach, as in OSC age has a negative effect on the correction of Cobb’s angle in percent. 12 This could be one of the motivations to decide the use of MIS surgery instead of ORS with increasing age. 13 The possible reason may be that due to elderly patients requiring less correction according to the minimally invasive spinal deformity surgery (MISDEF2) algorithm, 14 less coronal curve correction is a significant factor to choose in favor of ORS that also decreases with an age. 13 Given the better mobilization in open surgery and more fixation points, the results of angle correction are better than those with MIS, but with MIS, we obtained less blood loss and faster recovery, and a better cosmetic effect.
The decreases in the angle of TK in the MIS group may be due to the corrective maneuvers used. The implant rod’s angle of curvature at the convex sides of the deformity and the use of the vertebral coplanar alignment (VCA) procedure for derotation leads to a spontaneous increase in TK and simultaneous LL. The increase in angle is similar than in other studies where the rod’s angle of curvature was used at the convex sides of the deformity. 15 Meanwhile according to the Lenke classification, the angle of pre- and postoperative TK in our study with an OSC and MIS surgery was still in the normal range (TK 0.75 from LL). When MIS is associated with hypokyphosis, it has less axial plane correction than when hyperkyphosis is corrected by OSC. These findings cannot be compared with other studies that found that direct vertebral derotation by PS causes thoracic spine hypokyphosis, as our study compared groups using different surgical techniques. 16 In the literature, we found only a comparison of the angle of TK to the study with an operation on Lenke 5C AIS using OSC or MIS, in our study, on Lenke 1 AIS, we found an opposite result on correction when the OSC angle increased and MIS decreased. 8 Additional research is required to assess long-term outcomes. In some cases, the loss of correction requires revision surgery. 17 The reduced correction with MIS is a more relevant long-term outcome and can warrant additional emphasis.
Blood loss in this study was reduced by more than half in the group that had undergone MIS as compared to OSC. Moreover, the results indicate that the volume of blood loss correlated with the duration of operation, both after OSC and MIS treatment or number of vertebrae fused after MIS, which roughly corresponds to the values of other studies.18,19 Compared to previous data from other scientists with a similar initial group, MIS in our study showed higher operative blood loss, but better coronal curve correction results. As in our study, the operative blood loss was 218.3 ± 17.1 mL with a corrected angle of 76.1 ± 11.1 as compared to that published by other authors who had an operative blood loss of 138.75 ± 50.04 mL with corrected angle of 68.25% ± 6.1 %. 8 In reduction of the volume of bleeding, different additional methods can also play a role, including the use of hemostatic agent tranexamic acid or special techniques. 20 These modifications of surgical techniques applied to reduce tissue injuries and blood loss were offered, including endoscope-assisted spinal surgery. 21 Perhaps, when more traumatic MIS manipulations for AIS are applied, there is improvement in correction results but an increase in blood loss and duration also.
Our study is closely linked to increase in the duration of operation which simultaneously improved the success of deformity correction in both MIS and ORS. Prolonged operation duration can trigger the development of one or more complications, including bleeding. 22 In contrast, reducing the duration of operation procedure diminished bleeding. 23 Differences in the volume of blood loss between the patients can also be explained by demographics, perioperative characteristics, and patient-specific risk factors, including physical status and comorbidities.24,25 A longer median operative time for MIS was also shown by other signs as well, and more precise movements, which take time, are required for a more accurate MIS technique. Nevertheless, to complete MIS, the surgeons usually spend more time as compared to standard scoliosis surgery.26,27
A higher volume of bleeding, which leads to a significant increase in the median length of hospital stay, was shorter in MIS than in OSC, and a positive correlation in duration of operation time was also discovered in the MIS group. Before this study, only a few studies with a small sample sizes reported about hospital stay. These studies found no significant tendency to reduce the time of hospital stay. 5 It is difficult to compare the average absolute length of stay for curative care in different countries because traditional and economic factors can lead to different duration of surgery. 28
Conclusion
The number of connected vertebrae correlates with better correction of the curve in AIS, leading to increased operation duration and bleeding volume. As a result, surgeons in AIS must constantly strike a balance between better curve correction and minimizing bleeding during surgery.
Footnotes
Author contributions: Ayrat R Syundyukov: conceptualization, data curation, investigation, methodology, supervision, writing—review & editing; Nikolai S Nikolaev: project administration, supervision, resources, supervision, writing—review & editing; Sergei V Vissarionov—review & editing; Pavel N Kornyаkov: data curation, investigation, methodology; Kalind S Bhandarkar: writing—validation, review & editing; Vladimir U Emelianov: writing—original draft, visualization, writing—review & editing.
Compliance with ethical standards: The study was conducted according to the Helsinki Declaration, after University Ethics Committee approval and written informed consent from all patients.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Vladimir U Emelianov  https://orcid.org/0000-0003-1720-1741
https://orcid.org/0000-0003-1720-1741
References
- 1. Fusco C, Donzelli S, Lusini M, et al. Low rate of surgery in juvenile idiopathic scoliosis treated with a complete and tailored conservative approach: end-growth results from a retrospective cohort. Scoliosis 2014; 9: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shapiro F, Sethna N. Blood loss in pediatric spine surgery. Eur Spine J 2004; 13(Suppl. 1): S6–S17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. White SJW, Cheung ZB, Ye I, et al. Risk factors for perioperative blood transfusions in adult spinal deformity surgery. World Neurosurg 2018; 115: e731–e737. [DOI] [PubMed] [Google Scholar]
- 4. Kim M, Kim HS, Oh SW, et al. Evolution of spinal endoscopic surgery. Neurospine 2019; 16(1): 6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tarpada SP, Morris MT. Minimally invasive surgery in the treatment of adolescent idiopathic scoliosis: a literature review and meta-analysis. J Orthop 2017; 14(1): 19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ha AS, Cerpa M, Lenke LG. State of the art review: vertebral osteotomies for the management of spinal deformity. Spine Deform 2020; 8(5): 829–843. [DOI] [PubMed] [Google Scholar]
- 7. Vissarionov S, Syundyukov A, Kokushin D, et al. A comparative analysis of the surgical treatment of preschool children with congenital spinal deformation and isolated hemivertebra from the combined and dorsal approaches. Pediatric Traumatol Orthop Reconstr Surg 2020; 7: 5–14. [Google Scholar]
- 8. Urbanski W, Zaluski R, Kokaveshi A, et al. Minimal invasive posterior correction of Lenke 5C idiopathic scoliosis: comparative analysis of minimal invasive vs. open surgery. Arch Orthop Trauma Surg 2019; 139(9): 1203–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Overholser BR, Sowinski KM. Biostatistics primer: part 2. Nutr Clin Pract 2008; 23(1): 76–84. [DOI] [PubMed] [Google Scholar]
- 10. Lak AM, Lamba N, Pompilus F, et al. Minimally invasive versus open surgery for the correction of adult degenerative scoliosis: a systematic review. Neurosurg Rev 2021; 44(2): 659–668. [DOI] [PubMed] [Google Scholar]
- 11. Uribe JS, Deukmedjian AR, Mummaneni PV, et al. Complications in adult spinal deformity surgery: an analysis of minimally invasive, hybrid, and open surgical techniques. Neurosurg Focus 2014; 36(5): E15. [DOI] [PubMed] [Google Scholar]
- 12. Yahara Y, Seki S, Makino H, et al. Three-dimensional computed tomography analysis of spinal canal length increase after surgery for adolescent idiopathic scoliosis: a multicenter study. J Bone Joint Surg Am 2019; 101(1): 48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Park P, Than KD, Mummaneni PV, et al. Factors affecting approach selection for minimally invasive versus open surgery in the treatment of adult spinal deformity: analysis of a prospective, nonrandomized multicenter study. J Neurosurg Spine. Epub ahead of print 19 June 2020. DOI: 10.3171/2020.4.SPINE20169. [DOI] [PubMed] [Google Scholar]
- 14. Mummaneni PV, Park P, Shaffrey CI, et al. The MISDEF2 algorithm: an updated algorithm for patient selection in minimally invasive deformity surgery. J Neurosurg Spine 2019; 32(2): 221–228. [DOI] [PubMed] [Google Scholar]
- 15. Kokabu T, Sudo H, Abe Y, et al. Effects of multilevel facetectomy and screw density on postoperative changes in spinal rod contour in thoracic adolescent idiopathic scoliosis surgery. PLoS ONE 2016; 11(8): e0161906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Watanabe K, Nakamura T, Iwanami A, et al. Vertebral derotation in adolescent idiopathic scoliosis causes hypokyphosis of the thoracic spine. BMC Musculoskelet Disord 2012; 13: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang LN, Hu BW, Yang X, et al. Loss of correction after removal of spinal implants in congenital scoliosis. World Neurosurg 2020; 144: e916–e925. [DOI] [PubMed] [Google Scholar]
- 18. Guay J, Haig M, Lortie L, et al. Predicting blood loss in surgery for idiopathic scoliosis. Can J Anaesth 1994; 41(9): 775–781. [DOI] [PubMed] [Google Scholar]
- 19. Ahmad AA. Minimal invasive surgery techniques for patients with adolescent idiopathic and early onset scoliosis. J Clin Orthop Trauma 2020; 11(5): 830–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jones KE, Butler EK, Barrack T, et al. Tranexamic acid reduced the percent of total blood volume lost during adolescent idiopathic scoliosis surgery. Int J Spine Surg 2017; 11(4): 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Park J, Ham DW, Kwon BT, et al. Minimally invasive spine surgery: techniques, technologies, and indications. Asian Spine J 2020; 14(5): 694–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schoenfeld AJ, Ochoa LM, Bader JO, et al. Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg Am 2011; 93(17): 1577–1582. [DOI] [PubMed] [Google Scholar]
- 23. de Bodman C, Miyanji F, Borner B, et al. Minimally invasive surgery for adolescent idiopathic scoliosis: correction of deformity and peri-operative morbidity in 70 consecutive patients. Bone Joint J 2017; 99-B(12): 1651–1657. [DOI] [PubMed] [Google Scholar]
- 24. Somani S, Capua JD, Kim JS, et al. ASA classification as a risk stratification tool in adult spinal deformity surgery: a study of 5805 patients. Global Spine J 2017; 7(8): 719–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Parrish JM, Jenkins NW, Hrynewycz NM, et al. The influence of gender on postoperative PROMIS physical function outcomes following minimally invasive transforaminal lumbar interbody fusion. J Clin Orthop Trauma 2020; 11(5): 910–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sarwahi V, Horn JJ, Kulkarni PM, et al. Minimally invasive surgery in patients with adolescent idiopathic scoliosis: is it better than the standard approach? A 2-year follow-up study. Clin Spine Surg 2016; 29(8): 331–340. [DOI] [PubMed] [Google Scholar]
- 27. Anand N, Rosemann R, Khalsa B, et al. Mid-term to long-term clinical and functional outcomes of minimally invasive correction and fusion for adults with scoliosis. Neurosurg Focus 2010; 28(3): E6. [DOI] [PubMed] [Google Scholar]
- 28. OECD. Average length of stay in hospitals. Paris: OECD, 2017. [Google Scholar]