Abstract
Many attempts have been made to discover and characterize the mechanisms of change in psychotherapies for depression, yet no clear, evidence-based account of the relationship between therapeutic procedures, psychological mechanisms, and symptom improvement has emerged. Negatively-biased thinking plays an important role in the phenomenology of depression, and most theorists acknowledge that cognitive changes occur during successful treatments. However, the causal role of cognitive change procedures in promoting cognitive change and alleviating depressive symptoms has been questioned. We describe the methodological and inferential limitations of the relevant empirical investigations and provide recommendations for addressing them. We then develop a framework within which the possible links between cognitive procedures, cognitive change, and symptom change can be considered. We conclude that cognitive procedures are effective in alleviating symptoms of depression and that cognitive change, regardless of how it is achieved, contributes to symptom change, a pattern of findings that lends support to the cognitive theory of depression.
Keywords: Psychotherapy processes, Mechanisms of change, Cognitive change, Cognitive therapy, Mediation
It is widely accepted that psychological interventions can be effective in the treatment of Major Depressive Disorder (MDD). Despite a long history of attempts to understand the processes and mechanisms by which psychotherapies achieve their effects, consensus has not emerged regarding the associations between therapeutic procedures, psychological mechanisms, and the symptom improvement they lead to. Although basic psychological research supports the notion that maladaptive cognitions play an important role in the etiology and maintenance of depression (Ingram, Atchley, & Segal, 2011), some have questioned the role of cognitive change procedures in psychotherapies, as well as the status of cognitive change as a mechanism of symptom reduction. Interpreting the literature regarding cognitive change as a mediator of symptom change in cognitive therapy (CT), Kazdin (2007) concluded: “[W]e can state more confidently now than before that whatever may be the basis of changes with CT, it does not seem to be the cognitions as originally proposed.” (p. 08; see also Longmore & Worrell, 2007).
Proponents of a common factor view of psychotherapy (see Messer & Wampold, 2002), as well as advocates of the “third-wave” cognitive-behavioral therapies (e.g., Hayes, 2004), have also questioned the basic premises that underlie the cognitive therapies. A common factor account of the effectiveness of CT places little if any weight on the importance of specific techniques, cognitive or otherwise, and third-wave therapies were developed in part as a reaction against a mechanistic understanding of the relation of cognitive change to symptom change. In the context of these critiques, a clarification of the propositions implied by a cognitive theory of change in CT, as well as a review of the relevant evidence, is warranted. As has been recognized in other areas of health, an understanding of the mechanisms of therapeutic change can lead to better treatments.
Consistent with Kazdin (2009), we distinguish two terms, mechanism and mediator, that are used in descriptions and tests of models of therapeutic change. A mechanism is a phenomenon that, when changed by a treatment, causes change in symptoms. Two treatments could mobilize different mechanisms and yet lead to similar effects on symptoms (DeRubeis, Brotman, & Gibbons, 2005). In such cases, each of the treatments would be expected to produce greater change in its theory-relevant mechanism, relative to the other. However, because mechanisms are causal agents, when changes in a mechanism occur, they are followed by changes in symptoms, irrespective of the treatment in which the change occurred.
Investigations that address mechanistic theories often include tests of mediation. In studies of psychotherapeutic change, a mediator is a variable that accounts, statistically, for a treatment effect, either partially or fully. A study in which the statistical criteria for mediation are met can provide some support for a causal theory. However, because mediators are observed rather than manipulated, no test of mediation can rule out all competing causal accounts.
The theory behind CT can be stated thus: Engaging in procedures aimed at altering negatively biased beliefs and thinking styles leads to cognitive change, which is the mechanism by which depressive symptoms are reduced (Beck, Rush, Shaw, & Emery, 1979; Beck & Haigh, 2014). Evidence in support of cognitive change as a therapeutic mechanism would be that changes in cognitive processes or contents predict symptom change, irrespective of the cause of the cognitive change (Gelfand & DeRubeis, 2014). However, it is possible that cognitive changes cause symptom change only, or especially, in the context of a treatment that focuses on changing cognitions. In this case, cognitive change would not be a general mechanism, but rather would act as a mediator that is specific to contexts in which cognitive procedures lead to the cognitive change.
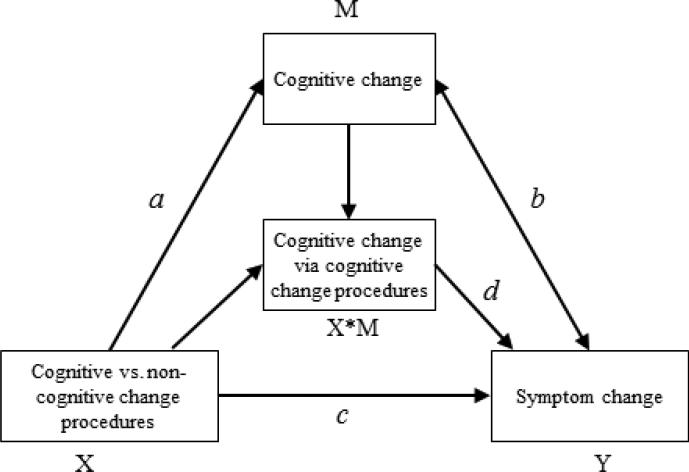
Based on existing evidence (Barth et al., 2013; Cuijpers et al., 2008), it is safe to assert that cognitive change procedures, the defining features of CT, produce more symptom change, on average, than would occur simply with the passage of time. As tempting as it may be to infer that this provides strong support for a cognitive model of therapeutic change, such findings do not address the following questions (see Figure 1):
Do cognitive change procedures (X), which are the focus of CT, lead to greater reduction in depressive symptoms (Y) than do procedures that emphasize change in other domains, such as behaviors? (path c.)
Do cognitive change procedures (X) produce greater cognitive change (M) than do non-cognitive change procedures (path a)?
Do changes in cognition (M) lead to changes in depressive symptoms (Y), irrespective of the procedures that brought them about (path b)?
Is cognitive change a specific mediator, such that changes in cognition resulting from cognitive change procedures (X*M) lead to greater symptom change (Y) than does cognitive change that is brought about by non-cognitive therapy procedures (path d)?
Figure 1.
Links between cognitive change procedures, cognitive change, and symptom change in depression.
A study that would address all four of these questions would need to include: (a) a test of the relative effects on symptoms of treatment procedures that differ either in kind (e.g., cognitive vs. non-cognitive) or strength (e.g., high vs. low adherence to cognitive procedures) (differential efficacy of procedures on symptoms); (b) a test of the relative effects of different treatment procedures on cognitive change (differential effects of procedures on cognition); (c) a test of the effects of changes in cognition on symptom change (effects of cognitive change on symptom change); (d) a test of whether the relation of cognitions to symptoms differs as a function of the conditions under which cognitive change occurs (cognitive specificity). The validity of the inferences derived from this set of tests is limited, however, insofar as the research methods employed do not address reverse causality and third variable confounds.
In investigations of the effects of cognitive procedures on cognitive change and symptom change in depression, very few studies have included tests of all four of the relationships described above while also attempting to rule out reverse causality and third variable confounds (e. g., DeRubeis et al., 1990; Evans et al., 2013; Kuyken et al., 2010) and only one of these included a test of mediation (Kuyken et al.). Other investigations have included tests of all four relationships without including using methods that address these confounds (see Kazdin, 2007). Still other studies have been designed with a focus on a subset of the four relationships. In this paper we attempt to provide conceptual clarity and to address disagreements among commentators who have written about the cognitive mediation of psychotherapeutic change. We briefly discuss the ways in which negatively biased cognition has been implicated in depression and the different ways in which psychotherapies are purported to foster cognitive change. We then refer to recent reviews of the literature, relevant empirical studies that include tests of one or more of the four questions. We will distinguish between a variety of positions that have been proposed either implicitly or explicitly to account for relationships between cognitive change procedures, cognitive changes, and improvement in depression. We will assume that cognitive change can result from therapeutic interventions initiated by a therapist as well from other sources, such as positive life events. When we use the term cognitive change procedures we are referring to actions taken by the therapist with the aim of promoting cognitive change. In neither case do we assume that therapeutic techniques or psychological changes are uniquely cognitive or non-cognitive in nature. Rather, we adhere to conventional use of language to refer to cognitive change procedures as those that are primarily aimed at changing cognitions and cognitive change as change that is well-characterized as cognitive but may be associated with changes, such as behavioral change, that do not fit the “cognitive” rubric.
Cognition and depression
There is abundant evidence that negative thinking plays an important role in the phenomenology and ontology of depression. Measures of negative thinking have been shown to predict prospectively the onset, relapse, and recurrence of symptoms of depression (e.g., Mathews & MacLeod, 2005; Scher et al., 2005; Wenze, Gunthert, & Forand, 2010). These and other findings suggest that negatively biased cognition is not merely characteristic of depression, but it also is a mechanism whereby depression arises and is maintained. A corollary is that changes in negative cognition can also be a mechanism by which symptoms of depression remit. A defining feature of the cognitive-behavioral therapies (CBTs), which includes CT, is the assumption that changes in thinking mediate the effects of therapeutic interventions on psychiatric symptoms (Dobson & Dozois, 2009). However, among different CBT approaches, as well as among clinical theorists who write about CBTs, there are differences regarding which aspects of cognition are presumed to be the most important targets of therapeutic intervention. Similarly, there is no broad consensus as to what are the most effective cognitive procedures for promoting cognitive change or symptom change.
A common set of distinctions within the general term cognition is between processes, contents, and compensatory skills. Information processing that is biased, for example, in directing attention to negative stimuli has been implicated in the pathology of depression (Ingram, Atchley, & Segal, 2011). Such biased information processing tendencies have been related to the concepts of schemas or modes (Beck, 1996). Although the use of refocusing and distancing is recommended in CT as a way of altering these processes (Beck J.S., 2011), a major emphasis in treatment is in accumulating evidence that can be used to compare the validity of negative schemata with more accurate and adaptive alternatives. Proponents of third-wave CBTs have gone further and stress the value of shifting the focus of therapy away from the contents of cognitions and towards an exclusive focus on processes. As exemplified by the names of the most popular third-wave CBTs, mindfulness and acceptance techniques are emphasized in these treatments (Brown, Gaudiano, & Miller, 2011). In traditional CBTs, with their emphasis on the modification of beliefs and assumptions, an important distinction is between more immediate cognitive content and contents that remain latent until they are activated (e.g., schemas; Kwon & Oei, 1994). One further target of traditional CBTs is the development of skills that can be used to respond to depressogenic thoughts and negative affect (Barber & DeRubeis, 1989).
More than 25 years ago, Barber and DeRubeis (1989) noted the presence of “conceptual ambiguities regarding cognitive processes and contents as they have been applied in the cognitive therapy literature,” (p. 441). These ambiguities remain. For example, whereas a distinction has been drawn between cognitive processes and content (e.g., Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008), there is considerable overlap in the referents and operationalizations of the constructs that are categorized as processes versus contents. For example, although a distinction between process and content is raised in discussions of the targets of third-wave CBTs, the study of maladaptive cognitive processes has focused on those processes that involve negative contents.
Although CBTs differ in the extent to which they target processes, content, and skills, a unifying assumption is that cognitive change mediates the effects of treatment on reduction or prevention of psychopathological symptoms. Thus, we will include investigations of changes in any of these three kinds of cognitive phenomena in our consideration of the links between cognitive change procedures, cognitive change, and symptom change.
Distinguishing therapeutic modalities, change procedures, and mechanisms of change
Questions about the validity of a theory of psychotherapeutic change are best addressed by investigations of specific therapeutic procedures – such as the examination of evidence for and against a belief – instead of investigations of a therapeutic modality. This is because a treatment (say, CT) may contain multiple procedures, some of which may overlap with those that also define other psychotherapeutic modalities (Haaga, 2007). For example, descriptions of psychodynamic therapies often include techniques that could also be categorized as cognitive-behavioral (Barth, Michlig, & Munder, 2014). Moreover, practitioners of a therapy modality can, and in fact often do, use techniques from other modalities (McCarthy & Barber, 2009).
The effectiveness of cognitive change procedures as a means of bringing about symptom change has been questioned on the basis of findings from studies in which components of CBTs have been compared (e.g., Jacobson et al., 1996). Longmore and Worrell (2007, p. 174) ask whether “the direct, explicit modification of maladaptive cognitions [is] a necessary or sufficient intervention in CBT.” These authors then discussed studies that have failed to find a statistically significant difference between cognitive and behavioral interventions on short-term outcomes. They conclude from these data that cognitive change procedures do not contribute to symptom change beyond what is achieved via the non-cognitive procedures that are a part of CBT.
Longmore and Worrell (2007) infer from the lack of statistically significant differences in symptom change between cognitive and non-cognitive interventions that cognitive change is not a mechanism of symptom change. This interpretation of the kinds of findings reviewed by Longmore and Worrell, which is echoed in the writings of Hayes (2004; see also Jacobson et al., 1996), does not employ a distinction between therapeutic packages, therapeutic procedures, and mechanisms of therapeutic change. As observed by McCarthy and Barber (2009), a non-cognitive therapy session can include “cognitive” procedures such as comparing the evidence for and against a belief. More importantly, as Hofmann (2008) has argued, even when so-called non-cognitive procedures lead to symptom change, the mechanism of that change may nonetheless be cognitive. For example, assigning an activity, insofar as engagement in the activity contributes to mood change, could do so through the mechanism of a decrease in hopelessness. Thus, comparisons of treatment packages cannot provide the most informative tests of the relative efficacy of therapeutic procedures or of the mechanisms of symptom change. Instead, investigations of therapeutic modalities should include attempts to isolate the specific behaviors of the therapists – procedures or techniques – that lead to symptom change. To uncover the mechanism by which these procedures lead to outcome, such investigations should include measurements of a purported change variable.
Testing links between cognitive procedures, cognitive change and symptom change
Investigations of the processes of psychotherapeutic change are often focused on one of the three potential links between therapeutic procedures, psychological mechanisms, and outcomes. Mediation analyses can be used to characterize the network of relations among these variables (Baron & Kenny, 1986; McKinnon, 2008). Tests of empirical data that meet the statistical criteria for mediation can contribute to our understanding of the causal links among measured constructs. Although other approaches, such as structural equation modeling (SEM), have also been recommended (Gelfand, Mensinger, & Tenhave, 2003), mediational analyses are the most widely used statistical tests of causal hypotheses. However, statistical tests alone, no matter how robust, cannot fully substantiate a set of causal claims. The validity of such claims rests on two assumptions that are difficult or impossible to meet.
The first assumption is that no causal variable has been omitted from the analysis (Gelfand et al., 2003). Even in the most thorough and rigorous test of mediation, it cannot be known if all causal variables have been included. Therefore, as there may be an unmeasured third variable that could represent the causal mechanism, the most that can be said when a positive finding is obtained in a mediation analysis is that the pattern in the data is consistent with a causal model. The second assumption is that the temporal order of the phenomena is consistent with the order implied by the tests (Gelfand, Mensinger, & Tenhave, 2003). As has been noted by others (Haaga, 2007; Kazdin, 2007), it can be difficult to establish that changes in a putative mediator precede changes in the outcomes they are meant to explain. In fact, the temporal order assumption has rarely been met in tests of the mediation of the effects of treatments for MDD. Thus, an investigation in which temporal order is accounted for, even if it only provides a test of one link in the mediational chain, may provide stronger evidence in support of a causal hypothesis than one in which mediation testing is conducted but in which the temporal order assumption has not been met. Negative findings, on the other hand, can help to disconfirm causal hypotheses.
We describe empirical tests of each of the bivariate associations between measures of procedures, potential mediators, and outcomes, as well as investigations that have included mediation analyses. We will focus on the inferences supported by the findings, as well as on the ways in which common features of research designs place limits on these inferences.
Differential effects of procedures on symptoms (X → Y)
Findings from randomized comparisons (i.e., outcome research) of treatment packages that focus on cognitive change (such as CT) versus treatment packages that do not (e.g., BA) provide evidence regarding the effects of cognitive procedures on symptom change. Another type of evidence that bears on the relation between procedures and outcomes comes from observational studies of courses of treatment that vary in the degree to which cognitive change procedures are employed (i.e., process-outcome research).
Outcome research
Tolin (2010), in his meta-analysis of outcome findings in anxiety or depressive disorders, found CBT to be superior to other treatments. Similarly, in the Vittengl, Clark, Dunn, and Jarrett (2007) meta-analysis, there was evidence that continuation CBT was superior in reducing relapse-recurrence rates after discontinuation, relative to other continuation therapies. When Barth et al. (2013) limited their meta-analytic review to trials that were adequately powered, their findings suggested that CBT, problem-solving (PST) and interpersonal therapies (IPT) for depression produce greater symptom reduction than do control conditions. By contrast, there was insufficient evidence for the efficacy of BA and social skills training, and the existing evidence did not suggest that psychodynamic and supportive therapies are more efficacious than control conditions. In a meta-analytic review of comparative outcome studies for patients with mild to moderate MDD, Cuijpers et al. (2008) concluded that the effects of CBTs do not differ from the effects observed in each of six other psychological treatments. This pattern of findings is consistent with the Dodo Bird verdict (Luborsky, et al., 2002), a widely held belief that all psychotherapies are equally effective. Thus, the findings regarding the superiority of CBTs compared to other treatment modalities are equivocal or, at least, debatable, and likely hinge not only on the methods used to conduct the meta-analyses, but also on the focus (e.g., mild or moderate depression versus more severe depression) or the timeframe (acute vs. longer-term).
Process research
Within CBT for depression, variation in therapist adherence and competence has been found to account for variation in outcomes (Kuyken & Tsivriko, 2008; Shaw et al., 1999). DeRubeis and Feeley (1990) found that, early in therapy, variation in therapists’ use of concrete cognitive therapy techniques, such as examining evidence concerning belief, was related to subsequent symptom change. This finding has been replicated by Feeley, DeRubeis, and Gelfand (1999). Strunk, Brotman, and DeRubeis (2010) also replicated these findings, showing that the use of specific cognitive change methods but not behavioral methods, was related to subsequent change in depression.
Ilardi and Craighead (1994) argued that the specific cognitive procedures of CBTs cannot account for symptom change, on the assumption that most symptom change occurs before cognitive strategies are implemented. The findings referenced by Ilardi and Craighead were from trials in which CBT sessions were conducted biweekly for the first three to four weeks. Therefore, the change they were referring to had occurred by what in most cases was the sixth to eighth session. Since it has been shown that cognitive procedures are used extensively by cognitive therapists as early as the second session of therapy (e.g., DeRubeis & Feeley, 1990; Feeley, DeRubeis, & Gelfand, 1999; Strunk, Brotman, & DeRubeis, 2010), there is nothing in the outcome literature that rules out the causal effects of cognitive procedures on symptom change. However, there are few investigations that have been designed to test the hypothesis that cognitive change procedures produce more symptom change than do non-cognitive change procedures.
Even if it were known that cognitive change procedures do not yield greater symptom improvement than other therapeutic interventions, this would not inform our understanding of the mechanisms through which CBTs, or other interventions, achieve their effects. In the approach to mediation analysis described by Baron and Kenny (1986), a significant effect of X (procedures) on Y (outcome) is required in order to proceed with the remaining tests. However, several authors have advocated approaches to mediation testing that do not require a between-treatment difference in outcomes (Kraemer, 2002; MacKinnon & Fairchild, 2009).
One of the intuitions that motivates these alternative approaches is that although equivalent outcomes between two treatments can be brought about by the same mechanism, alternatively, equivalently effective treatments may achieve their effects via different mechanisms (DeRubeis, Brotman, & Gibbons, 2005). For example, cognitive change procedures and procedures aimed at changing behavior may both ultimately work via the mechanism of cognitive change. However, it may instead be that they work via different mechanisms: cognitive change procedures via cognitive means and behavior change procedures via alternate means. In neither one of these cases would one proceed to conduct the tests recommended by Baron and Kenny (1986), although tests of mediation for each treatment would still be of interest. The presence in the research design of a condition that is less effective than either of the treatments, as well as the inclusion of variables that represent the different treatments’ presumed mechanisms, would help to distinguish whether the comparable efficacy of the two treatments is driven by change in the same mechanism or by differential change in two or more different mechanisms.
Differential effects of procedures on cognitions (X → M)
The effect of cognitive change procedures on cognitive change can be examined by investigating changes in cognitive variables that occur during treatments that include cognitive change procedures. Hundt et al. (2013) reviewed 13 studies in which the frequency of patients’ use of CBT skills was assessed at the end of CBT treatments for depression, as well as 11 studies that focused on the quality of patients’ CBT skills. In the majority of the investigations, increases in the frequency and quality of patients’ use of cognitive restructuring and other CBT skills (e.g., thought records) were observed. Other reviews confirm significant cognitive changes following CBTs (Oei & Free, 1995). Process-outcome research provides another way of exploring the relation between cognitive procedures and cognitive change. In an observational study of CT processes, Webb, DeRubeis, Dimidjian, Hollon, Amsterdam, and Shelton (2012) found that variation in therapists’ use of concrete cognitive therapy techniques accounted for variability in patients’ later use of cognitive strategies. Taken together, these findings suggest that cognitive change procedures lead to cognitive change.
Comparisons of antidepressant medication therapy versus CBTs have yielded evidence suggesting that cognitive procedures can result in greater change in depressive cognitions and cognitive processes, relative to medications (e.g., Dozois et al., 2009; Fresco, Segal, & Kennedy, 2007; Ma & Teasdale, 2004; Segal, Gemar, & Williams, 1999; Segal et al., 2006). However, this pattern has not been consistently reported (DeRubeis et al., 1990; Fournier et al., 2013). Garratt et al. (2007) argue that, in general, cognitive changes following medication treatments are more superficial whereas CBTs are able to facilitate deeper cognitive change, altering processes such as cognitive reactivity. In contrast to the comparisons of CBTs versus antidepressants, comparisons between CBTs and other psychotherapies have tended not to reveal differences in the magnitude of cognitive change (see Garratt et al.; Oei & Free, 1995).
Null findings regarding the magnitude of cognitive change following different treatment procedures may reflect the fact that equivalent cognitive change can follow from different therapeutic procedures. However, such findings could also reflect a misspecification of the cognitive change variable. The literature on the differential effects of CT and medications illustrates this point. Patients treated with antidepressants or CT typically show no difference in responses to the Dysfunctional Attitudes Scale (DAS; Weissman & Beck, 1978) when a standard administration of it is used. However, when the DAS has been given following a negative mood induction, patients who have gone through CT tend to endorse fewer negative cognitions than those who received medications (Segal et al., 1999; 2006). This kind of comparison, however, has not yet been reported between CBT and others psychotherapies.
Effects of cognitive change on symptom change (M → Y)
Contemporaneous associations between cognitive change and symptom change during treatments for depression have been observed in numerous investigations (Garratt et al., 2007; Oei & Free, 1995). Within CBT, Christopher, Jacob, Neuhaus, Neary, and Fiola (2009) found that symptom improvement covaried with cognitive change, but not with behavioral change. Jacob, Christopher, and Neuhaus (2011), by contrast, found that both behavioral and cognitive changes were correlated with symptom improvement. In their review, Hundt et al. (2013) reported that in most of the studies of changes in cognitive and behavioral compensatory skills, significant positive relations between increases in these skills and symptom improvement were observed.
Findings of associations between cognitive change and symptom change might reflect a causal link from cognition to symptoms, but without a control for temporal confounds one cannot rule out the possibility that cognitions and symptoms change simultaneously, or that changes in symptoms lead to changes in cognition. However, in studies of cognitive change in CBT that have addressed the issue of temporal order, cognitive changes have been found to predict subsequent symptom change (e.g., Neimeyer & Feixas, 1990; Powers, Thompson, & Gallagher-Thompson, 2008; Shirk, Crisostomo, Jungbluth, & Gudmundsen, 2013). In CT, within-session cognitive changes predict “sudden gains” (Tang & DeRubeis, 1999a; Tang, DeRubeis, Beberman, & Pham, 2005), which are associated with positive long-term outcomes (Aderka, Nickerson, Bøe, & Hofmann, 2012). Strunk, DeRubeis, Chiu, and Alvarez (2007) found that changes in patients’ CT skills, as well their use of the skills, predicted resistance to relapse in the year following a course of CT for depression. Similarly, changes from pre- to post-treatment in extreme responding (Forand & DeRubeis, 2014), as well as a measure of cognitive reactivity at post-treatment (Segal et al., 1999; Teasdale et al., 2002), have been found to predict relapse.
Statistical tests of the mediation of symptom change
Few studies have included tests of the mediation of the effects of cognitive procedures on symptom change. In Hundt et al.'s (2013) review of 22 studies that examined the relation between depression outcomes and a cognitive variable – the use of CBT skills – only 2 studies included statistical tests of mediation. In one of those (Gallagher-Thompson, Gray, Dupart, Jimenez, & Thompson, 2008), the superiority of a group CBT intervention relative to a control condition was statistically mediated by changes in CBT skills. However, cognitive change and symptom change were measured concurrently. Kuyken et al. (2010) randomized patients who had responded to medications to either continuation medication treatment or a mindfulness-based CT intervention (MBCT). Increases in self-compassion and in the use of mindfulness skills met criteria for mediation of the superior prevention effects of MBCT. Thus, both studies found evidence of the cognitive mediation of positive treatment effects. However, only Kuyken et al. employed a research design that could reasonably rule out reverse causality.
In a study that compared CBT, PST, and a waiting list condition, Warmerdam, van Straten, Jongsma, Twisk, and Cuijpers (2010) found that changes in dysfunctional attitudes, worry, and a negative problem orientation met the statistical criteria for the mediation of symptom change for both CBT and PST. Forman et al. (2012) found that changes in dysfunctional thinking and cognitive defusion mediated decreases in depressive symptoms following ACT and CT. However, like the Gallagher-Thompson et al. (2008) study, cognitive change and symptom change were measured concurrently in these studies.
Structural equation models (SEM) have also been employed to investigate the causal role of cognitive change in therapy. Burns and Spangler (2001) compared fit statistics across models that differed in the hypothesized direction of the relation between cognitive change and symptom change. The model that represented co-occurring cognitive change and symptom change fit the data better than one in which cognitive change preceded and predicted symptom change. Similar findings were obtained by Oei, Bullbeck, and Campbell (2006) in their SEM of data obtained during group CBT for depression. Although SEM has been recommended as an alternative to traditional tests for mediation (see Garratt et al., 2007; Haaga, 2007), if the temporal order in the model is not correctly specified, causal inferences are subject to the same limitation as are claims that follow from standard mediation models.
Virtually every published finding regarding the link between cognitive change and symptom change has been consistent with a cognitive model of change. Moreover, findings from tests of mediation suggest that cognitive changes can account for the effects produced by cognitive, as well as non-cognitive, change procedures. However few of the studies have included a control for temporal confounds, and the issue of temporality is a non-trivial one. This is exemplified in Smits, Rosenfield, McDonald, and Telch's (2006) study of CBT for social anxiety. Changes in one cognitive variable – the predicted probability of negative events – preceded and predicted change in symptoms, whereas changes in another cognitive variable – the predicted cost of a negative event – appeared to follow from symptom improvement. Thus, temporal confounds in the existing literature limit the confidence with which causal claims can be asserted. However, it does not follow that cognitive change does not cause symptom change, as Kazdin (2007, 2009) has suggested. An assertion that cognitive change is not a mechanism of symptom change would gain support from null or negative findings obtained in studies with the necessary design features. To our knowledge, such evidence does not exist, and yet evidence of positive associations between cognitive change and symptom change are abundant. Moreover, positive evidence for alternative mechanisms of change is lacking. Thus, there is support for the hypothesis that cognitive change is a mechanism of symptom change. Although evidence consistent with this hypothesis comes largely from studies in which reverse causality has not been ruled out, there is little if any support for alternative causal accounts.
Cognitive specificity
Tests of cognitive change as a mediator of symptom change specifically in the context of cognitive change procedures have been conducted by comparing associations between cognitive change and symptom change across different treatment conditions, especially CBTs vs. somatic therapies. DeRubeis et al. (1990) found that cognitive changes predicted subsequent symptom improvement for patients treated with CT, but not for those treated with antidepressant medications. They concluded that whereas in CT cognitive change may have driven further symptom change, the cognitive change observed in medication-treated patients may have been a result rather than a cause of symptom change. Quilty, McBride, and Bagby (2008) reached a similar conclusion from an investigation in which they used structural equation modeling to characterize pre- to post-treatment changes in cognitions and symptoms, although cognitive change and symptom change was measured concurrently. In a study of seasonal affective depression, Evans et al. (2013) reported that in CBT, but not in light therapy, cognitive changes during 6 weeks of treatment predicted depressive symptoms at 1-year winter follow-up. In contrast to the three studies just cited, each of which found specificity in the relation between cognitive change and symptom change, Segal and colleagues reported that cognitive reactivity predicted depressive relapse irrespective of whether it followed from treatment with CT or antidepressant medications (Segal et al.,1999; Segal et al., 2006).
The specificity of cognitive change has also been explored across psychotherapies. In a meta-analytic review of cognitive change and symptom change, Oei and Free (1995) reported a positive correlation between cognitive change and symptom change in studies that focused on non-CT psychotherapies, as well as in those that focused on CT. By contrast, the association of cognitive change and symptom change was small and non-significant in studies of antidepressant medication treatments. Similarly, Quilty et al. (2008) found that cognitive change co-varied with symptom change in both IPT and CBT. Warmerdam et al. (2010) also reported cognitive change as a mediator of the treatment effects of both PST and CBT relative to a waitlist condition. These findings suggest that cognitive change might be a non-specific mediator of change across PST, CBT, and IPT. However, none of these studies included controls for temporal confounds.
Forman, Herbert, Moitra, Yeomans, and Geller (2007) reported that theory-relevant variables were differentially associated with outcomes in CT versus Acceptance and Commitment Therapy (ACT). In CT, but not in ACT, observing one's internal experience was associated with reduced levels of depression. By contrast, in ACT but not in CT, acceptance of internal experiences was associated with outcome. The authors replicated and extended these findings by showing that patients’ use of cognitive and affective change strategies, as opposed to acceptance strategies, were related to positive outcomes in CT, whereas in ACT acceptance was positively related to outcome and changes in cognitive variables were negatively related to symptom change (Forman et al., 2012).
When a mediator is non-specific, it suggests that the phenomenon represented by the mediator may be a mechanism of therapeutic change (Gelfand & DeRubeis, 2014). Findings of specific cognitive mediation raise the issue of why cognitive changes are related to outcomes in some treatment contexts but not in others. It is possible that the observed cognitive change variables in a given study do not reflect mechanisms in and of themselves. Rather, the variables may reflect phenomena that play a causal role if and only if other – unmeasured – phenomena are present. In the treatment in which cognitive mediation is observed, the assumption would be that the cognitive change variable and the variable that was not included combine to represent a single mechanism. Consistent with this idea, DeRubeis et al. (1990) hypothesized that in their CT condition, change in measured beliefs (e.g., DAS), combined with the acquisition and use of compensatory skills, which were not measured, accounted for symptom change in CT. Whereas medications did induce cognitive change, in that treatment the acquisition and use of compensatory skills was unlikely to have occurred to a similar degree, and therefore medications would not engage this mechanism. It is implied in any account of specific mediation that alternative causal paths are engaged by the different treatments.
Another hypothesis that is consistent with a finding of specific cognitive mediation is that changes in cognition are a proxy for a third variable only in the context of cognitive change procedures. For example, some have argued that a sufficient mechanism in treatment-induced change is the provision of a rationale specific to the treatment that allows patients to understand their symptoms (Frank & Frank, 1993). Under this view, it is not cognitive change per se that leads to symptom change. Instead, cognitive change in a cognitive treatment is a proxy for patients’ belief in the treatment rationale, which is itself the mechanism of change. What follows from this kind of analysis is that cognitive change in the context of a cognitive treatment will lead to symptom improvement, as will bringing about behavior change in the context of a behavioral treatment, changing role conflicts in IPT, and so forth.
The ways in which cognitive change procedures, changes in cognitions and symptom change could relate to each other
In Table 1 we outline a framework for representing competing views of the links between cognitive change procedures, cognitive change, and symptom change. Regarding the differential effects of procedures on symptoms (path c in Figure 1), a cognitive change procedure may be: more efficacious than (+1), equally efficacious as (0), or less efficacious than (−1) a non-cognitive change procedure in the treatment of depression. Considering the differential effects of procedures on cognition (path a), a cognitive change procedure may alter cognitions: more than (+1), equal to (0), or less than (−1) a non-cognitive change procedure. Regarding the effect of cognitive change on symptom change (path b), there may either be a causal effect (+1) or no causal effect (0). Finally, regarding cognitive specificity (path d), cognitive change might act as a non-specific mediator (0), irrespective of how the change occurred, or the magnitude of the effects of cognitive change on symptom change may depend upon whether cognitive change procedures brought about the cognitive change (+1).
Table 1.
Framework for understanding the links between cognitive change procedures, cognitive change, and symptom change in treatments for depression.
| Path c | Path a | Path b | Path d | |
|---|---|---|---|---|
| Links | Effects of procedures on symptoms | Effects of procedures on cognition | Role of cognitive change | Cognitive specificity |
|
| ||||
| +1 | Cognitive change procedures are more efficacious than non-cognitive procedures | Cognitive change procedures alter cognitions more than non-cognitive procedures | Cognitive change leads to symptom change | Cognitive change is a non-specific mediator of symptom change |
|
| ||||
| 0 | Cognitive change procedures are equally efficacious as non-cognitive procedures | Cognitive change procedures and non-cognitive procedures alter cognitions equally | Cognitive change does not lead to symptom change | Cognitive change is a specific mediator of symptom change |
|
| ||||
| −1 | Cognitive change procedures are less efficacious than non-cognitive procedures | Cognitive change procedures alter cognitions less than non-cognitive procedures | -- | -- |
A comprehensive theory of therapeutic change implies a set of claims or hypotheses that integrates the four links. Our framework, using the notation just described, yields 36 possible models (see Appendix A) that can be distinguished primarily by whether they consider that cognitive changes are: (1) mechanisms of change, (2) not mechanisms of change, or (3) specific mediators of therapeutic effects. The relative efficacy of cognitive and non-cognitive procedures in producing symptom change further distinguishes the positions. However, a relatively small subset of the models generated by this framework warrant detailed consideration. For example, models in which cognitive change does not mediate symptom change in any way can be discussed as representing one position; in these models the magnitude of cognitive change following different therapeutic procedures becomes relatively unimportant (X, X, 0, 0). Other models are illogical or internally inconsistent (e.g., a model of cognitive change as a general mechanism that posits that cognitive change procedures produce superior symptom change but inferior cognitive change, +1,−1, +1, 0). Finally, we do not discuss models in which cognitive change is both a specific and a non-specific mediator of symptom change, although we recognize that one or more of the models with this feature might be worthy of consideration.
We are left with five kinds of models that are consistent with theoretical positions outlined or suggested by experts in the literature on psychotherapy (see table 2). In the following, we focus on the relevant empirical evidence that speaks to the links, and the connections among them, implied by each of these five positions. As in the reviews of evidence regarding the links, we consider issues of omitted variables and temporal confounds. We also describe research that would fill gaps in the empirical literature. We begin with three positions that, although different from one another in an important respect, each assume that change in cognitions plays a causal role in symptom change (i.e., cognitive change is a mechanism). A fourth position assumes that there is no causal link between cognition change and symptom change (i.e., no cognitive mediation). The last position we consider is one that ascribes a mediational role to cognitive change, but only in the context of cognitive change procedures (i.e., specific cognitive mediation).
Table 2.
Positions that refer to links between cognitive change procedures, cognitive change, and symptom change in depression treatments
| Path c | Path a | Path b | Path d | ||||
|---|---|---|---|---|---|---|---|
| Position | Effects of procedures on symptoms | Effects of procedures on cognition | Role of cognitive change | Cognitive specificity | Mechanistic account | Potency of cognitive procedures | Relevant papers |
| 1A | 1 | 1 | 1 | 0 | Cognitions as mechanisms of change | Cognitive change procedures produce more cognitive change and symptom change | Beck (1976) |
| 1B | 0 | 0 | 1 | 0 | Cognitions as mechanisms of change | Cognitive change procedures produce equal amounts of cognitive change and symptom change | Hofmann (2008) |
| 1C | −1 | −1 | 1 | 0 | Cognitions as mechanisms of change | Cognitive change procedures produce less cognitive change and symptom change | Linehan (1993) |
| 2 | -- | -- | 0 | 0 | Cognitions are not mechanisms | -- | Kazdin (2007) Longmore & Worrell (2007) |
| 3 | -- | -- | 0 | 1 | Cognitions are specific mediators | -- | DeRubeis et al. (1990) Messer & Wampold (2002) |
Note. For path c, a cognitive change procedure may be more efficacious than (+1); equally efficacious as (0); or less efficacious than (−1) a non-cognitive change procedure. For path a, a cognitive change procedure may alter cognitions more than (+1), equal to (0), or less than (−1) a non-cognitive change procedure. For path b, there may either be a causal effect (+1) or no causal effect (0). For path d, cognitive change might act as a non-specific mediator (0), or a specific mediator (+1).
Position 1: Cognitive change is a mechanism of symptom change in psychotherapy (X, X, +1, 0)
The three positions outlined below share the view that cognitive change is a therapeutic mechanism, but they differ in regard to whether cognitive procedures are more, or less, effective than other procedures in bringing about cognitive change and, as a consequence, symptom change.
1A. Cognitive procedures produce superior cognitive change and symptom change (+1, +1, +1, 0)
A strong proposition regarding the efficacy of cognitive change procedures is that: (a) such procedures are more efficacious than alternative change procedures because (b) they are the most powerful means of producing cognitive change and (c) changing cognitions results in symptom change (or resistance to relapse). Evidence for this position is that CBTs, which emphasize cognitive change procedures, yield better outcomes than medications over the long term (Cuijpers et al., 2013), and that changes in cognitive reactivity are greater in CT relative to medications (Segal et al., 1999; Segal et al., 2006). Whereas the relative efficacy and the mediation of the long-term effects of CBTs in relation to antidepressants are clear, less is known about the relative long-term effects of CBTs compared to other psychotherapies.
1B. Cognitive procedures and non-cognitive procedures produce indistinguishable effects on cognitive change and symptom change (0, 0, +1, 0)
A moderate proposition regarding the efficacy of cognitive change procedures is that: (a) they are equally as effective as alternative change procedures because (b) they are among the procedures that lead to cognitive change and (c) cognitive change causes symptom change. Hofmann (2008) suggests that non-cognitive change procedures, such as exposure and behavioral activation, as well as cognitive change procedures, may work through cognitive change to produce symptom change. Similarly, Warmerdam et al. (2010) suggest that changes in cognitive measures are a proxy for common cognitive processes that account for change across psychotherapies for depression. Evidence for this position is that CBT has been found to yield short-term outcomes (Cuijpers et al., 2008) and changes in cognitive measures (Oei & Free, 1995) that are similar to those observed in other psychotherapies, and that changes in cognitions co-vary with changes in symptoms across treatments.
1C. Cognitive change procedures are inferior to non-cognitive change procedures (−1, −1, +1, 0)
A third proposition regarding the efficacy of cognitive change procedures is that: (a) they are less effective than alternative change procedures because (b) cognitive change procedures are a relatively ineffective means of producing the cognitive changes that (c) result in symptom change. Some suggest that the cognitive change procedures in CBTs detract from therapeutic activities that would lead more efficiently to symptom change, such as behavioral activation (Jacobson et al., 1996). Others go further and argue that cognitive change procedures can produce harm in that they encourage a maladaptive focus on cognitive processes, through the process of examining beliefs, or they invalidate the patient (Linehan, 1993). As Linehan stated, “[s]tandard behavior therapy (including standard cognitive-behavioral therapy) by itself, at least as I practiced it, invalidated my patients” (p. 77). To our knowledge there is no evidence that cognitive procedures are less effective than alternatives in producing cognitive change.
Position 2: Cognitive change is not a mechanism of symptom change in psychotherapy (X, X, 0, 0)
It is possible, as Kazdin (2007) has asserted, that cognitive mechanisms do not account for the efficacy of CBT for depression. His conclusion is based on the fact that although numerous studies have revealed links between cognitive change and symptom change during treatment, only a handful of studies have used designs that could address reverse causality or third variable explanations. Given that Kazdin's claim rests on the acceptance of a null hypothesis, evidence is required that a non-cognitive mechanism, such as behavioral change, is responsible for symptom change in CBT, whereas cognitive change is not. We are aware of no such evidence.
Aside from CBT, the most extensively-researched psychotherapies for depression are IPT and PST (Barth et al., 2013), making the mechanisms implied by their respective theories of change likely candidates as non-cognitive mechanisms of psychotherapeutic change. However, there has been little research on the mechanisms of change in IPT (Markowitz & Weissman, 2004) and PST (Mynors-Wallis, 2002), and the roles of changes in interpersonal processes or problem-solving skills have received little attention in research on CT for depression. Thus, to bolster the claim that cognitive change is not a mechanism of symptom change in CT, findings would need to emerge that reveal that non-cognitive constructs account for symptom change over and above the effects of cognitive change.
Position 3: The role of cognitive change as a mediator of symptom change is specific to cognitive procedures (X, X, 0, +1)
Finally, it is possible that cognitive change functions as a mediator of symptom change only when it occurs in the context of a treatment that emphasizes cognitive change procedures. Although there is evidence that cognitive change is associated with symptom change in CBT, IPT, and PST, there is also some evidence that this association is not found in somatic therapies (i.e., light therapy and antidepressants; DeRubeis et al., 1990; Evans et al., 2013; Quilty et al., 2008) or in ACT (Forman et al., 2007; Forman et al., 2012). Thus, the position that cognitive change is a specific mediator has some support. As a way of integrating these seemingly disparate findings, it may be that the measurement of self-reported cognitive change in CBTs captures change in cognitive vulnerabilities whereas in treatment with somatic therapies, measurements of cognitive change capture the deactivation of state-dependent negative cognitions. (For a similar argument, see Evans et al., 2013). This hypothesis is endorsed by Garratt et al. (2007), who conclude that “evidence suggests that cognitive changes associated with pharmacotherapy are more superficial than those associated with cognitive therapy” (p. 224). Alternatively, cognitive change in a CBT may be a proxy for a third variable, such as adopting the treatment rationale.
In the context of evidence that cognitive change is a mediator of change in IPT and PST as well as in CBT, it is tempting to propose that most or all psychotherapies work via cognitive change whereas somatic therapies work via other mechanisms. However, the findings of Forman et al. (2007, 2012), in their comparisons of CT and ACT, suggest the possibility that at least these two psychotherapies work via different mechanisms. Insofar as PST and IPT may engage the same mechanisms as CBT, they too might differ from ACT, but thus far there are no data that speak to this possibility. Interestingly, although MBCT has also been classified as a third wave CBT, in studies of MBCT cognitive change also correlates with symptom change. For example, Manicavasagar, Perich, and Parker (2012) reported that decreases in rumination correlated with change both in MBCT and CBT.
State of the Evidence Regarding the Five Positions
Our review suggests that the evidence available to address questions concerning cognitive mediation is limited in a variety of ways. The position with the most consistent empirical support is that cognitive change is a mechanism of change in therapies for depression and that cognitive as well as non-cognitive change procedures can produce similar levels of cognitive change and therefore similar levels of symptom improvement (position 1B).
CBT is the most extensively researched form of psychotherapy for depression. Findings from dismantling and component studies, which are often cited as evidence against a cognitive model of change, can only address claims that cognitive procedures are not necessary for the induction of cognitive change, or not superior to the non-cognitive procedures in a therapy package. Across courses of CT or CBT, the contents and processes of patients’ thinking undergo change. They evidence increases in meta-cognitive awareness and compensatory skills, allowing them to respond to their biased or maladaptive negative thoughts. Insofar as these changes are also brought about by therapeutic procedures that do not expressly address cognitive contents or processes, this is often taken as evidence against the cognitive theory of depression, yet in fact it follows logically from a cognitive theory. If cognitive changes are a mechanism by which depressive symptoms are reduced (or relapses are prevented), cognitive change should predict symptom change (or relapse prevention) irrespective of how cognitive change is brought about. There are suggestions in the literature that somatic therapies as well as some psychotherapies that focus on internal experiences (e.g., ACT) may work through mechanisms that are not well-characterized as cognitive. Any cognitive change that occurs in these therapies may thus be a byproduct of the activation of other mechanisms. This would be consistent with the idea that the relation between cognition and affect is reciprocal (Mayberg et al., 1999).
Research Strategies That Will Further the Understanding of Mechanisms
Attention to temporal features
It is understood that the best evidence regarding the mediational status of a phenomenon, vis a vis the effects of procedures on subsequent symptom status, is obtained in studies in which the temporal order (procedures → mediator → outcome) can be established unambiguously. We have highlighted how, in empirical tests, the failure to attend to the temporal features of a mediation model severely limits the causal inferences that can be supported by the data. Investigators have called for the early assessment of potential mediators, with the idea that changes in a mediator variable must precede the symptom change they are hypothesized to account for (Stice, Presnell, Gau, & Shaw, 2007). In studies of psychotherapies for depression, in which a substantial proportion of symptom change tends to occur by the fourth week (or eighth session) of therapy (Ilardi & Craighead, 1994; Tang & DeRubeis, 1999b), it behooves investigators to assess potential mediators early enough to capture the causal processes that occur during this period. Kraemer et al. (2007) have made this point, highlighting that the measurement of mediators must occur before most therapeutic change is evident. However, not only must these assessments take place early in treatment, but the symptom change predicted by the mediator must include only change that occurs after the assessment of the mediator. It is therefore not enough to assess change in a mediator, for example, over the first few weeks or sessions of therapy and use this variable to “predict” change in symptoms pre-treatment to post- treatment, as has often been done in studies that are ostensibly designed to rule out reverse causality (see, for example, Kraemer et al.; Wilson, Fairburn, Agras, Walsh, & Kraemer, 2002). In these analyses, the “symptom change” variable conflates change that occurred before an early assessment of the mediator with symptom change that occurred after that assessment. Only the prediction of change that occurs subsequent to the mediator addresses fully the possibility of a temporal order confound. Thus, along with Kazdin (2007), we recommend the frequent measurement of symptoms as well as proposed mediators, especially early in treatment, so that the mediator variables can be tested for their ability to predict change subsequent to the time when the mediator is assessed.
In the interest of attending to temporal confounds, it may be tempting to limit investigations of mechanisms of change to the earlier sessions of therapy. However, even studies that focus only on the early phases of therapy might be insufficient for detecting relationships between cognitive change procedures, cognitive change, and symptom change. Trajectories of symptom change in psychotherapy are known to vary between patients (Hayes, Laurenceau, Feldman, Strauss, & Cardaciotto, 2007). These variations may be related to differences in the timing of the delivery of different therapeutic procedures or to between-patient differences in the onset of changes in relevant mechanisms. Insofar as change in therapy occurs at different times in a manner that is patient-specific, any exploration that does not account for this fact will, at best, provide limited evidence for what accounts for change in therapy. Rice and Greenberg (1984) suggest that attending to “critical moments” in therapy sessions, and exploring variables that could account for these changes, is one way to address this potential limitation. Research on sudden gains is a variation on this idea, with its focus on individual patients’ between-session shifts in symptoms, whenever they occur (Aderka, Nickerson, Bøe, & Hofmann, 2012). However, even analyses that examine session-to-session or week-to-week changes in cognitions and symptoms may fail to find evidence in support of causal links, even if the causal theory that informs the tests is correct. Insofar as change in a cognitive phenomenon produces effects on a time scale of days, hours, or briefer intervals, even week-to-week assessments may be inadequate to detect these effects. Ecological momentary assessment (EMA) methodologies represent one alternative to regular, periodic (e.g., weekly) assessments. EMAs have shown promise in their ability to disambiguate reciprocal effects between processes that affect each other over brief intervals (see Stone & Shiffman, 1994).
This is not to say that findings from studies in which temporal confounds are not controlled are uninformative. At the very least, negative findings can help to rule out causal hypotheses regarding a purported mediator of outcome. However, positive findings of the association between cognitive change and symptom change during psychotherapy are by now abundant, such that further positive findings are unlikely to increase confidence in the view that cognitive change may lead to symptom change.
Long-term outcomes
There is evidence to indicate that acute treatment with CBTs yields superior longer-term outcomes than does equally brief treatment with antidepressant medications (Cuijpers et al., 2013), yet the data on the acute effects of these two treatments would suggest that they are approximately equally efficacious (Cuijpers et al., 2013; Cuijpers, van Straten, van Oppen, & Andersson, 2008). However, there are relatively few comparative outcome studies that provide data on the long term outcomes of depressed patients who are treated with different psychotherapeutic modalities (see Cuijpers et al., 2008; Hollon, Stewart, & Strunk, 2006). Thus, little is known about whether and to what extent different therapeutic procedures, even those that are observed to produce similar short-term outcomes, might evidence differential efficacy over the longer term. In a recent meta-analysis, Bell, Marcus, and Goodland (2013) reported that treatment packages with more than one component led to better outcomes than treatment packages that focus on a single component. This effect, which was small (d = 0.14) but significant at the end of treatment, became larger at follow-up (d = 0.28). If the differential effects of psychotherapy procedures are more readily detected in the long term, a focus on the prediction of longer-term outcomes could yield more informative tests of mediation.
Focus on populations that can reveal true differences in procedures
DeRubeis, Gelfand, German, Fournier, and Forand (2014) illustrate how the magnitude of process-outcome correlations, such as the relation between cognitive change procedures and symptom change, can vary substantially as a function of the extent to which variability in the therapeutic procedure is represented in a study. In addition, they illustrate how the magnitude of process-outcome estimates can vary as a function of the makeup of the patient population under study. Specifically, a study is unlikely to reveal evidence of a link between procedures and outcomes insofar as the sample contains a high proportion of patients who are either likely to improve even if given a weak treatment (i.e., placebo responders or spontaneous remitters) or unlikely to improve even if given a strong treatment (i.e., treatment non-responsive or intractable patients). Similarly, links between procedures and mechanisms will be difficult to detect if the proportion of spontaneous remitters and intractable patients is high. Thus, research that aims to advance an understanding of the links between cognitive change procedures, cognitive change, and change in depression should sample from patient populations with low proportions of such patients, in the context of variability in the therapeutic procedures of interest.
Distinguishing measures of symptoms from measures of potential mechanisms
Measures of cognitive change, insofar as they derive from self-reports or clinical interviews, tend to conflate, at least to some extent, cognitive change with symptom change. Haaga (2007) recommends that researchers focus greater attention on the development of more nuanced assessments of cognitive change by using measures that are not contaminated with depressive symptoms. Illustrating this point, findings from independent research teams suggest that the predictive validity of the DAS is contingent on whether it is used as a measure of cognitive content or, instead, response style or cognitive reactivity (see Forand & DeRubeis, 2014; Segal, et al., 1999; Segal et al., 2006). Attention should also be paid to the external validity of cognitive measures. For example, the Ways of Responding questionnaire (WOR; Barber & DeRubeis, 1992), designed to assess patients’ acquisition of the kinds of cognitive skills thought to be useful after therapy has ended, has been found to predict relapse (Strunk et al., 2007).
Expand the focus of the analysis of cognitive processes
Importantly, a focus on self-report or cognitive measures of processes relevant to depression does not preclude consideration of other types of variables that may be markers of cognitive processes. Findings from neuroimaging and genetic studies, for example, indicate that these kinds of approaches can be used to reveal biological indicators of processes that reflect cognitive vulnerability to depression (Firk, Siep, & Markus, 2013) as well as changes that occur during a course of psychotherapy (Fournier & Price, 2014). An inclusion of these variables in studies of change in therapy should expand our understanding of the mechanisms involved in changes in depression.
Exploration of patient-level moderators
Our discussion of cognitive procedures and cognitive change as predictors of symptom improvement has not addressed the possibility that patient variables moderate one or more of these relationships. For some patients, successful cognitive change might best be achieved with direct cognitive change procedures, such as Socratic questioning, whereas for others non-cognitive techniques, such as behavioral assignments, may be a more effective means of producing cognitive change. Similarly, cognitive change may result in greater symptom reduction in some patients relative to others. For example, Sasso, Strunk, Braun, DeRubeis, and Brotman (2014) found that for patients with more recurrent forms of depression a relatively greater emphasis on cognitive as opposed to behavioral methods predicted greater change in depression.
Summary and Conclusions
Our review of the many methodological and inferential issues that arise when studying cognitive mediation of cognitive procedures highlights how the study of mechanisms of change in treatment is a difficult enterprise. The evidence for bivariate associations between cognitive procedures and symptom change, cognitive procedures and cognitive change, and cognitive change and symptom change is clear. Findings from experimental research suggests that strategies that involve cognitive reappraisal, similar to those encouraged in CT, lead to changes in negative affect (see Gross, 2002). These findings can be taken as support for the cognitive model of depression, which posits that cognitive change causes changes in depressive symptoms. By contrast, in the literature on psychotherapeutic change, the direction of causality between cognitive change and symptom change has not been well established. However, it does not follow from the evidence that cognitive change is not a mechanism of symptom change. Even if the positive evidence is discounted completely, it would only follow that that there is an absence of evidence, not evidence of absence, of a causal role for cognitive change in symptom change. The few studies that have tested a cognitive mediation model while ruling out the temporal confound have yielded findings that are consistent with such a model (e.g., DeRubeis et al., 1990; Kuyken et al., 2010; Shirk et al., 2013), particularly as it relates to change in depression that is likely to be sustained over time (e.g., Strunk et al., 2007; Tang et al., 2005). However, more studies that address the methodological issues we have discussed are needed.
Our review of the literature and of commentaries on mechanisms of change in psychotherapy highlights differences in the interpretation of research findings. For example, the observation that cognitive change occurs across various psychotherapies for depression has been cited as evidence against the theory behind CBTs for depression (e.g., Longmore & Worrell, 2007). We have argued, to the contrary, that it follows from a cognitive theory of therapeutic change that cognitive change will be related to symptom change irrespective of the nature of the intervention that has brought about the cognitive change (see also Hofmann, 2008), an argument that has even been extended to medications (Harmer, Goodwin, & Cowen, 2009). Similarly, some have assumed that results from randomized comparative studies, including those with additive or dismantling designs, are able to answer questions about mediators or mechanisms of therapeutic change (e.g., Jacobson et al., 1996; Longmore & Worrell, 2007). As we and others have argued (Hofmann, 2008), different procedures may work through the same mechanisms or, alternatively, different procedures may engage and work through different mechanisms (DeRubeis et al., 2005). As a separate issue, some have argued that the ability to infer causality from a given finding is determined, in part, by the kind of statistical analysis employed by the investigators (see, for example, Hundt et al., 2013). Test statistics that are estimated in mediational models, SEMs, or mixed models are not more or less able to rule out temporal confounds than are any other kind of statistic. The crucial matter is whether the study was designed to rule out reverse causality.
In our review, we have employed a pragmatic distinction between cognitive and non-cognitive change. Given that the role of cognitive change in psychotherapies has been questioned, an exploration of alternative, non-cognitive, psychological variables that explain change in treatment is warranted. Moreover, within the rubric of change that we have considered cognitive, a demarcation of the specific variables that drive change will be needed in order to advance cognitive theories of depression. It is possible, as Smit et al. (2006) found in social anxiety, that certain types of cognitive changes drive change in therapy, whereas others are the product of symptom change. These distinctions are also highlighted by proponents of third-wave CBTs who additionally underscore the need to focus on different types of therapy procedures that we have discussed under the umbrella of cognitive change procedures. However, there are very few direct comparisons of the relative efficacy of different kinds of cognitive change procedures. Thus studies that compare the relative efficacy of different cognitive change procedures, as well as different non-cognitive change procedures, and that also measure different potential cognitive mediators, as well as non-cognitive ones, are needed.
Correlational studies have provided information about the relations between therapeutic procedures, psychological mechanisms and symptom change. The existing literature supports a claim that various therapeutic procedures produce cognitive change that can in turn lead to symptom change which in turn leads to even more cognitive change. However, the literature is replete with disagreement among researchers as to the best measures to include in a study, how to test for causality, and even how to interpret the findings from such tests. We have attempted to provide some clarity, along with a framework to aid in the characterization of research on cognitive mediation, but a consensus regarding the mechanisms of change in therapy may not soon be reached. This is in part because there are multiple types of interventions that therapists engage in, and the interventions are sometimes difficult to tell apart from each other. Moreover, any given intervention might affect more than one potential mechanism of change. Investigators who wish to elucidate change mechanisms will need to consider including measurements of all these variables. Moreover, such measurements probably need to be taken early and often, and the data will need to be modeled in a manner consistent with causal inference the investigator wishes to draw. Even if one has conducted the most thorough and valid possible test of a causal hypothesis, it still might be that an unmeasured variable would reflect better the actual causal mechanism. Thus are the limitations of investigations of mechanisms that employ observational methods. It is not too surprising, then, that consensus is a difficult-to-achieve goal. It is, after all, complicated.
Supplementary Material
Highlights.
Various therapeutic procedures produce both cognitive and symptom change
Cognitive change appears to be a general mechanism of change
Cognitive mediation studies often violate temporality assumptions
A framework for research on cognitive mediation is proposed
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aderka IM, Nickerson A, Bøe HJ, Hofmann SG. Sudden gains during psychological treatments of anxiety and depression: A meta-analysis. Journal of Consulting and Clinical Psychology. 2012;80(1):93–101. doi: 10.1037/a0026455. doi: 10.1037/a0026455. [DOI] [PubMed] [Google Scholar]
- Barber JP, DeRubeis RJ. On second thought: Where the action is in cognitive therapy for depression. Cognitive Therapy and Research. 1989;13(5):441–457. doi: 10.1007/BF01173905. [Google Scholar]
- Barber JP, DeRubeis RJ. The Ways of Responding: A scale to assess compensatory skills taught in cognitive therapy. Behavioral Assessment. 1992;14(1):93–115. [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barth J, Michlig N, Munder T. Unique and shared techniques in cognitive-behavioural and short-term psychodynamic psychotherapy: a content analysis of randomised trials on depression. Health Psychology and Behavioral Medicine: an Open Access Journal. 2014;2(1):929–950. doi: 10.1080/21642850.2014.931231. doi: 10.1080/21642850.2014.931231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barth J, Munder T, Gerger H, Nüesch E, Trelle S, Znoj H, Cuijpers P. Comparative efficacy of seven psychotherapeutic interventions for patients with depression: a network meta-analysis. PLOS Medicine. 2013;10(5):e1001454. doi: 10.1371/journal.pmed.1001454. doi: 10.1371/journal.pmed.1001454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT. Beyond belief: A theory of modes, personality, and psychopathology. In: Salkovskis PM, editor. Frontiers of cognitive therapy. Guilford; New York, NY: 1996. pp. 1–25. [Google Scholar]
- Beck AT, Haigh EA. Advances in Cognitive Theory and Therapy: The Generic Cognitive Model. Annual Review of Clinical Psychology. 2014;10:1–24. doi: 10.1146/annurev-clinpsy-032813-153734. doi: 10.1146/annurevclinpsy-032813-153734. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. Guilford Press; New York, NY: 1979. [Google Scholar]
- Bell EC, Marcus DK, Goodland JK. Are the parts as good as the whole? A meta-analysis of component treatment studies. Journal of Consulting and Clinical Psychology. 2013;81(4):722–736. doi: 10.1037/a0033004. doi: 10.1037/a0033004. [DOI] [PubMed] [Google Scholar]
- Brown LA, Gaudiano BA, Miller IW. Investigating the similarities and differences between practitioners of second-and third-wave cognitive-behavioral therapies. Behavior Modification. 2011;35(2):187–200. doi: 10.1177/0145445510393730. doi: 10.1177/0145445510393730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns DD, Spangler DL. Do changes in dysfunctional attitudes mediate changes in depression and anxiety in cognitive behavioral therapy? Behavior Therapy. 2001;32(2):337–369. doi: 10.1016/S0005-7894(01)80008-3. [Google Scholar]
- Christopher MS, Jacob KL, Neuhaus EC, Neary TJ, Fiola LA. Cognitive and behavioral changes related to symptom improvement among patients with a mood disorder receiving intensive cognitive-behavioral therapy. Journal of Psychiatric Practice. 2009;15(2):95–102. doi: 10.1097/01.pra.0000348362.11548.5f. doi: 10.1097/01.pra.0000348362.11548.5f. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Hollon SD, van Straten A, Bockting C, Berking M, Andersson G. Does cognitive behaviour therapy have an enduring effect that is superior to keeping patients on continuation pharmacotherapy? A meta-analysis. BMJ Open. 2013;3(4):1–8. doi: 10.1136/bmjopen-2012-002542. doi:10.1136/bmjopen-2012-002542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds CF. The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta-analysis of direct comparisons. World Psychiatry. 2013;12(2):137–148. doi: 10.1002/wps.20038. doi: 10.1002/wps.20038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, Andersson G, van Oppen P. Psychotherapy for depression in adults: a meta-analysis of comparative outcome studies. Journal of Consulting and Clinical Psychology. 2008;76(6):909–922. doi: 10.1037/a0013075. doi: 10.1037/a0013075. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, van Oppen P, Andersson G. Are psychological and pharmacologic interventions equally effective in the treatment of adult depressive disorders? A meta-analysis of comparative studies. Journal of Clinical Psychiatry. 2008;69(11):1675–1685. doi: 10.4088/jcp.v69n1102. doi: 10.4088/JCP.v69n1102. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Brotman MA, Gibbons CJ. A conceptual and methodological analysis of the nonspecifics argument. Clinical Psychology: Science and Practice. 2005;12(2):174–183. doi: 10.1093/clipsy.bpi022. [Google Scholar]
- DeRubeis RJ, Evans MD, Hollon SD, Garvey MJ, Grove WM, Tuason VB. How does cognitive therapy work? Cognitive change and symptom change in cognitive therapy and pharmacotherapy for depression. Journal of Consulting and Clinical Psychology. 1990;58(6):862–869. doi: 10.1037//0022-006x.58.6.862. doi: 10.1037/0022-006X.58.6.862. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Feeley M. Determinants of change in cognitive therapy for depression. Cognitive Therapy and Research. 1990;14(5):469–482. doi: 10.1007/BF01172968. [Google Scholar]
- DeRubeis RJ, Gelfand LA, German RE, Fournier JC, Forand NR. Understanding processes of change: How some patients reveal more than others—and some groups of therapists less—about what matters in psychotherapy. Psychotherapy Research. 2014;24(3):419–428. doi: 10.1080/10503307.2013.838654. doi: 10.1080/10503307.2013.838654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, Gallop R. Cognitive therapy vs medications in the treatment of moderate to severe depression. Archives of General Psychiatry. 2005;62(4):409–416. doi: 10.1001/archpsyc.62.4.409. doi: 10.1001/archpsyc.62.4.409. [DOI] [PubMed] [Google Scholar]
- Dozois DJ, Bieling PJ, Patelis-Siotis I, Hoar L, Chudzik S, McCabe K, Westra HA. Changes in self-schema structure in cognitive therapy for major depressive disorder: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2009;77(6):1078–1088. doi: 10.1037/a0016886. doi: 10.1037/a0016886. [DOI] [PubMed] [Google Scholar]
- Evans M, Rohan KJ, Sitnikov L, Mahon JN, Nillni YI, Lindsey KT, Vacek PM. Cognitive change across cognitive-behavioral and light therapy treatments for seasonal affective disorder: What accounts for clinical status the next winter? Cognitive Therapy and Research. 2013;37(6):1201–1213. doi: 10.1007/s10608-013-9561-0. doi: 10.1007/s10608-013-9561-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeley M, DeRubeis RJ, Gelfand LA. The temporal relation of adherence and alliance to symptom change in cognitive therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67(4):578–582. doi: 10.1037//0022-006x.67.4.578. doi: 10.1037/0022-006X.67.4.578. [DOI] [PubMed] [Google Scholar]
- Fournier JC, Price RB. Psychotherapy and Neuroimaging. FOCUS: The Journal of Lifelong Learning in Psychiatry. 2014;12(3):290–298. doi: 10.1176/appi.focus.12.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forand NR, DeRubeis RJ. Extreme response style and symptom return after depression treatment: The role of positive extreme responding. Journal of Consulting and Clinical Psychology. 2014;82(3):500–509. doi: 10.1037/a0035755. doi: 10.1037/a0035755. [DOI] [PubMed] [Google Scholar]
- Forman EM, Chapman JE, Herbert JD, Goetter EM, Yuen EK, Moitra E. Using session-by-session measurement to compare mechanisms of action for acceptance and commitment therapy and cognitive therapy. Behavior Therapy. 2012;43(2):341–354. doi: 10.1016/j.beth.2011.07.004. doi: 10.1016/j.beth.2011.07.004. [DOI] [PubMed] [Google Scholar]
- Forman EM, Herbert JD, Moitra E, Yeomans PD, Geller PA. A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behavior Modification. 2007;31(6):772–799. doi: 10.1177/0145445507302202. doi: 10.1177/0145445507302202. [DOI] [PubMed] [Google Scholar]
- Fournier JC, DeRubeis RJ, Hollon SD, Gallop R, Shelton RC, Amsterdam JD. Differential change in specific depressive symptoms during antidepressant medication or cognitive therapy. Behaviour Research and Therapy. 2013;51(7):392–398. doi: 10.1016/j.brat.2013.03.010. doi: 10.1016/j.brat.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank JD, Frank JB. Persuasion and healing: A comparative study of psychotherapy. Johns Hopkins University Press; Baltimore, MD: 1993. [Google Scholar]
- Fresco DM, Segal ZV, Buis T, Kennedy S. Relationship of posttreatment decentering and cognitive reactivity to relapse in major depression. Journal of Consulting and Clinical Psychology. 2007;75(3):447–455. doi: 10.1037/0022-006X.75.3.447. doi: 10.1037/0022-006X.75.3.447. [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Gray HL, Dupart T, Jimenez D, Thompson LW. Effectiveness of cognitive/behavioral small group intervention for reduction of depression and stress in non-Hispanic white and Hispanic/Latino women dementia family caregivers: Outcomes and mediators of change. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2008;26(4):286–303. doi: 10.1007/s10942-008-0087-4. doi: 10.1007/s10942-008-0087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garratt G, Ingram RE, Rand KL, Sawalani G. Cognitive processes in cognitive therapy: Evaluation of the mechanisms of change in the treatment of depression. Clinical Psychology: Science and Practice. 2007;14:224–239. doi: 10.1111/j.1468-2850.2007.00081.x. [Google Scholar]
- Gelfand LA, DeRubeis RJ. Models of specific and nonspecific change mechanisms in mental health treatments. In: Cautin R, Lilienfeld S, editors. Encyclopedia of Clinical Psychology. Wiley-Blackwell; New York: 2014. in press. [Google Scholar]
- Gelfand LA, Mensinger JL, Tenhave T. Mediation analysis: A retrospective snapshot of practice and more recent directions. The Journal of General Psychology. 2009;136(2):153–178. doi: 10.3200/GENP.136.2.153-178. doi: 10.3200/GENP.136.2.153-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ. Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology. 2002;39(3):281–291. doi: 10.1017/s0048577201393198. doi: 10.1017/S0048577201393198. [DOI] [PubMed] [Google Scholar]
- Haaga DA. Could we speed this up? Accelerating progress in research on mechanisms of change in cognitive therapy of depression. Clinical Psychology: Science and Practice. 2007;14(3):240–243. doi: 10.1111/j.1468-2850.2007.00082.x. [Google Scholar]
- Harmer CJ, Goodwin GM, Cowen PJ. Why do antidepressants take so long to work? A cognitive neuropsychological model of antidepressant drug action. The British Journal of Psychiatry. 2009;195(2):102–108. doi: 10.1192/bjp.bp.108.051193. doi: 10.1192/bjp.bp.108.051193. [DOI] [PubMed] [Google Scholar]
- Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy. 2004;35(4):639–665. doi: 10.1016/j.beth.2016.11.006. doi:10.1016/S0005-7894(04)80013-3. [DOI] [PubMed] [Google Scholar]
- Hayes AM, Laurenceau JP, Feldman G, Strauss JL, Cardaciotto L. Change is not always linear: The study of nonlinear and discontinuous patterns of change in psychotherapy. Clinical Psychology Review. 2007;27(6):715–723. doi: 10.1016/j.cpr.2007.01.008. doi: 10.1016/j.cpr.2007.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG. Common misconceptions about cognitive mediation of treatment change: A commentary to Longmore and Worrell (2007). Clinical Psychology Review. 2008;28(1):67–70. doi: 10.1016/j.cpr.2007.03.003. doi: 10.1016/j.cpr.2007.03.003. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Stewart MO, Strunk D. Enduring effects for cognitive behavior therapy in the treatment of depression and anxiety. Annual Review of Psychology. 2006;57:285–315. doi: 10.1146/annurev.psych.57.102904.190044. doi: 10.1146/annurev.psych.57.102904.190044. [DOI] [PubMed] [Google Scholar]
- Hundt NE, Mignogna J, Underhill C, Cully JA. The relationship between use of CBT skills and depression treatment outcome: A theoretical and methodological review of the literature. Behavior Therapy. 2013;44(1):12–26. doi: 10.1016/j.beth.2012.10.001. doi: 10.1016/j.beth.2012.10.001. [DOI] [PubMed] [Google Scholar]
- Ilardi SS, Craighead WE. The role of nonspecific factors in cognitive-behavior therapy for depression. Clinical Psychology: Science and Practice. 1994;1(2):138–155. doi: 10.1111/j.1468-2850.1994.tb00016.x. [Google Scholar]
- Ingram RE, Atchley RA, Segal ZV. Vulnerability to depression: From cognitive neuroscience to prevention and treatment. Guilford Press; New York: 2011. [Google Scholar]
- Jacob KL, Christopher MS, Neuhaus EC. Development and validation of the Cognitive-Behavioral Therapy Skills Questionnaire. Behavior Modification. 2011;35(6):595–618. doi: 10.1177/0145445511419254. doi: 10.1177/0145445511419254. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, Prince SE. A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology. 1996;64(2):295–304. doi: 10.1037//0022-006x.64.2.295. doi: 10.1037/0022-006X.64.2.295. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Understanding how and why psychotherapy leads to change. Psychotherapy Research. 2009;19:418–428. doi: 10.1080/10503300802448899. doi: 10.1080/10503300802448899. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. doi:10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Tsivrikos D. Therapist competence, comorbidity and cognitive-behavioral therapy for depression. Psychotherapy and Psychosomatics. 2008;78(1):42–48. doi: 10.1159/000172619. doi:10.1159/000172619. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Watkins E, Holden E, White K, Taylor RS, Byford S, Dalgleish T. How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy. 2010;48(11):1105–1112. doi: 10.1016/j.brat.2010.08.003. doi.org/10.1016/j.brat.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Kwon SM, Oei TP. The roles of two levels of cognitions in the development, maintenance, and treatment of depression. Clinical Psychology Review. 1994;14(5):331–358. doi:10.1016/0272-7358(94)90032-9. [Google Scholar]
- Linehan M. Cognitive-behavioral treatment of borderline personality disorder. Guilford Press; New York: 1993. [Google Scholar]
- Longmore RJ, Worrell M. Do we need to challenge thoughts in cognitive behavior therapy? Clinical Psychology Review. 2007;27(2):173–187. doi: 10.1016/j.cpr.2006.08.001. doi:10.1016/j.cpr.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Luborsky L, Rosenthal R, Diguer L, Andrusyna TP, Berman JS, Levitt JT, Krause ED. The dodo bird verdict is alive and well—mostly. Clinical Psychology: Science and Practice. 2002;9(1):2–12. doi: 10.1093/clipsy.9.1.2. [Google Scholar]
- Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology. 2004;72(1):31–40. doi: 10.1037/0022-006X.72.1.31. doi: 10.1037/0022-006X.72.1.31. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ. Current directions in mediation analysis. Current Directions in Psychological Science. 2009;18(1):16–20. doi: 10.1111/j.1467-8721.2009.01598.x. doi: 10.1111/j.1467-8721.2009.01598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manicavasagar V, Perich T, Parker G. Cognitive predictors of change in cognitive behaviour therapy and mindfulness-based cognitive therapy for depression. Behavioural and Cognitive Psychotherapy. 2012;40(02):227–232. doi: 10.1017/S1352465811000634. doi: 10.1017/S1352465811000634. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Weissman MM. Interpersonal psychotherapy: Principles and applications. World Psychiatry. 2004;3(3):136–139. [PMC free article] [PubMed] [Google Scholar]
- Mathews A, MacLeod C. Cognitive vulnerability to emotional disorders. Annual Review of Clinical Psychology. 2005;1(1):167–195. doi: 10.1146/annurev.clinpsy.1.102803.143916. doi: 10.1146/annurev.clinpsy.1.102803.143916. [DOI] [PubMed] [Google Scholar]
- Mayberg HS, Liotti M, Brannan SK, McGinnis S, Mahurin RK, Jerabek PA, Fox PT. Reciprocal limbic-cortical function and negative mood: Converging PET findings in depression and normal sadness. American Journal of Psychiatry. 1999;156(5):675–682. doi: 10.1176/ajp.156.5.675. [DOI] [PubMed] [Google Scholar]
- Messer SB, Wampold BE. Let's face facts: Common factors are more potent than specific therapy ingredients. Clinical Psychology: Science and Practice. 2002;9(1):21–25. doi: 10.1093/clipsy.9.1.21. [Google Scholar]
- McCarthy KS, Barber JP. The multitheoretical list of therapeutic interventions (MULTI): Initial report. Psychotherapy Research. 2009;19(1):96–113. doi: 10.1080/10503300802524343. doi: 10.1080/10503300802524343. [DOI] [PubMed] [Google Scholar]
- Mynors-Wallis L. Does problem-solving treatment work through resolving problems? Psychological Medicine. 2002;32(7):1315–1319. doi: 10.1017/s0033291702006025. doi: 10.1017/s0033291702006025. [DOI] [PubMed] [Google Scholar]
- Neimeyer RA, Feixas G. The role of homework and skill acquisition in the outcome of group cognitive therapy for depression. Behavior Therapy. 1990;21(3):281–292. doi: 10.1016/j.beth.2016.08.013. doi: 10.1016/s0005-7894(05)80331-4. [DOI] [PubMed] [Google Scholar]
- Oei TPS, Bullbeck K, Campbell JM. Cognitive change process during group cognitive behaviour therapy for depression. Journal of Affective Disorders. 2006;92(2-3):231–241. doi: 10.1016/j.jad.2006.02.004. doi: [DOI] [PubMed] [Google Scholar]
- Oei TPS, Free ML. Do cognitive behaviour therapies validate cognitive models of mood disorders? A review of the empirical evidence. International Journal of Psychology. 1995;30(2):145–180. doi: 10.1080/00207599508246564. [Google Scholar]
- Powers DV, Thompson LW, Gallagher-Thompson D. The benefits of using psychotherapy skills following treatment for depression: An examination of “afterwork” and a test of the skills hypothesis in older adults. Cognitive and Behavioral Practice. 2008;15(2):194–202. doi: 10.1016/j.cbpra.2007.01.002. [Google Scholar]
- Quilty LC, McBride C, Bagby RM. Evidence for the cognitive mediational model of cognitive behavioural therapy for depression. Psychological Medicine. 2008;38:1531–1541. doi: 10.1017/S0033291708003772. doi: 10.1017/s0033291708003772. [DOI] [PubMed] [Google Scholar]
- Rice L, Greenberg L, editors. Patterns of change: An intensive analysis of psychotherapeutic process. Guilford Press; New York: 1984. [Google Scholar]
- Sasso KE, Strunk DR, Braun JD, DeRubeis RJ, Brotman MA. Identifying moderators of the adherence-outcome relation in cognitive therapy for depression. 2014 doi: 10.1037/ccp0000045. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scher CD, Ingram RE, Segal ZV. Cognitive reactivity and vulnerability: Empirical evaluation of construct activation and cognitive diatheses in unipolar depression. Clinical Psychology Review. 2005;25(4):487–510. doi: 10.1016/j.cpr.2005.01.005. doi:10.1016/j.cpr.2005.01.005. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Gemar M, Williams S. Differential cognitive response to a mood challenge following successful cognitive therapy or pharmacotherapy for unipolar depression. Journal of Abnormal Psychology. 1999;108(1):3–10. doi: 10.1037//0021-843x.108.1.3. doi:10.1037/0021-843x.108.1.3. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Kennedy S, Gemar M, Hood K, Pedersen R, Buis T. Cognitive reactivity to sad mood provocation and the prediction of depressive relapse. Archives of General Psychiatry. 2006;63(7):749–755. doi: 10.1001/archpsyc.63.7.749. doi:10.1001/archpsyc.63.7.749. [DOI] [PubMed] [Google Scholar]
- Shaw BF, Elkin I, Yamaguchi J, Olmsted M, Vallis TM, Dobson KS, Imber SD. Therapist competence ratings in relation to clinical outcome in cognitive therapy of depression. Journal of Consulting and Clinical Psychology. 1999;67(6):837–846. doi: 10.1037//0022-006x.67.6.837. doi: 10.1037/0022-006X.67.6.837. [DOI] [PubMed] [Google Scholar]
- Shirk SR, Crisostomo PS, Jungbluth N, Gudmundsen GR. Cognitive Mechanisms of Change in CBT for Adolescent Depression: Associations among Client Involvement, Cognitive Distortions, and Treatment Outcome. International Journal of Cognitive Therapy. 2013;6(4):311–324. doi: 10.1521/ijct.2013.6.4.311. [Google Scholar]
- Smits JA, Rosenfield D, McDonald R, Telch MJ. Cognitive mechanisms of social anxiety reduction: An examination of specificity and temporality. Journal of Consulting and Clinical Psychology. 2006;74(6):1203–1212. doi: 10.1037/0022-006X.74.6.1203. doi: 10.1037/0022-006x.74.6.1203. [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, Gau J, Shaw H. Testing mediators of intervention effects in randomized controlled trials: An evaluation of two eating disorder prevention programs. Journal of Consulting and Clinical Psychology. 2007;75(1):20–32. doi: 10.1037/0022-006X.75.1.20. doi: 10.1037/0022-006X.75.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavorial medicine. Annals of Behavioral Medicine. 1994;16(3):199–202. [Google Scholar]
- Strunk DR, Brotman MA, DeRubeis RJ. The process of change in cognitive therapy for depression: Predictors of early inter-session symptom gains. Behaviour Research and Therapy. 2010;48(7):599–606. doi: 10.1016/j.brat.2010.03.011. doi: 10.1016/j.brat.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strunk DR, DeRubeis RJ, Chiu AW, Alvarez J. Patients' competence in and performance of cognitive therapy skills: relation to the reduction of relapse risk following treatment for depression. Journal of Consulting and Clinical Psychology. 2007;75(4):523–530. doi: 10.1037/0022-006X.75.4.523. doi: 10.1037/0022-006x.75.4.523. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ. Sudden gains and critical sessions in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 1999a;67(6):894–904. doi: 10.1037//0022-006x.67.6.894. doi: 10.1037/0022-006X.67.6.894. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ. Reconsidering rapid early response in cognitive behavioral therapy for depression. Clinical Psychology: Science and Practice. 1999b;6(3):283–288. doi: 10.1093/clipsy.6.3.283. [Google Scholar]
- Tang TZ, DeRubeis RJ, Beberman R, Pham T. Cognitive changes, critical sessions, and sudden gains in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 2005;73(1):168–172. doi: 10.1037/0022-006X.73.1.168. doi: 10.1037/0022-006X.73.1.168. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: Empirical evidence. Journal of Consulting and Clinical Psychology. 2002;70(2):275–287. doi: 10.1037//0022-006x.70.2.275. doi: 10.1037/0022-006X.70.2.275. [DOI] [PubMed] [Google Scholar]
- Tolin DF. Is cognitive-behavioral therapy more effective than other therapies?: A meta-analytic review. Clinical Psychology Review. 2010;30(6):710–720. doi: 10.1016/j.cpr.2010.05.003. doi: 10.1016/j.cpr.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Dunn TW, Jarrett RB. Reducing relapse and recurrence in unipolar depression: A comparative meta-analysis of cognitive-behavioral therapy's effects. Journal of Consulting and Clinical Psychology. 2007;75(3):475–488. doi: 10.1037/0022-006X.75.3.475. doi: 10.1037/0022-006X.75.3.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warmerdam L, van Straten A, Jongsma J, Twisk J, Cuijpers P. Online cognitive behavioral therapy and problem-solving therapy for depressive symptoms: Exploring mechanisms of change. Journal of Behavior Therapy and Experimental Psychiatry. 2010;41(1):64–70. doi: 10.1016/j.jbtep.2009.10.003. doi: 10.1016/j.jbtep.2009.10.003. [DOI] [PubMed] [Google Scholar]
- Webb CA, DeRubeis RJ, Dimidjian S, Hollon SD, Amsterdam JD, Shelton RC. Predictors of patient cognitive therapy skills and symptom change in two randomized clinical trials: The role of therapist adherence and the therapeutic alliance. Journal of Consulting and Clinical Psychology. 2012;80(3):373–381. doi: 10.1037/a0027663. doi: 10.1037/a0027663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman AN, Beck AT. Development and validation of the Dysfunctional Attitude Scale: A preliminary investigation.. Paper presented at the annual meeting of the Association for the Advancement of Behavior Therapy; Chicago, IL.. Nov, 1978. [Google Scholar]
- Wenze SJ, Gunthert KC, Forand NR. Cognitive reactivity in everyday life as a prospective predictor of depressive symptoms. Cognitive Therapy and Research. 2010;34(6):554–562. doi 10.1007/s10608-010-9299-x. [Google Scholar]
- Wilson GT, Fairburn CC, Agras WS, Walsh BT, Kraemer H. Cognitive-behavioral therapy for bulimia nervosa: Time course and mechanisms of change. Journal of Consulting and Clinical Psychology. 2002;70(2):267–274. doi: 10.1037/0022-006X.70.2.267. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.