Abstract
Cutaneous metastasis (CM) is a rare clinical entity with an incidence of less than 10% among oncology patients. Dissemination to the skin can be via bloodstream, lymphatics, direct expansion or by seeding after surgical procedures. Skin metastases usually develop months to years after the diagnosis of the primary tumor, while it may be the opposite in some rare cases. CM has various clinical presentations; diagnoses can be easily overseen as CM can mimic other dermatologic diseases. Herein, we present five different cutaneous metastasis cases, each with distinct dermatological presentation. Our main aim here is to allow dermatologists to consider skin metastases in the differential diagnoses of dermatological diseases, in their clinical practice.
Key words: Cutaneous metastasis, dermatooncology, internal malignancies
Case Report #1
A 86-year-old male patient came to our clinic with the complaint of pruritic skin lesions on his scrotum. The lesions were present for 7 months and were unresponsive to antifungal treatment. His personal history of illness and family history were both unremarkable. Dermatological examination revealed multiple, erythematous, pruritic nodules in the scrotal region. (Figure 1A).
A 4 mm punch biopsy was performed with the initial diagnoses of cutaneous metastasis, calcinosis cutis, prurigo nodularis and lymphocytoma cutis. In the biopsy specimen, tumoral infiltration was noted, starting from the superficial dermis, deep into subcutis. Tumoral infiltration was composed of atypical cells with pleomorphic, hyperchromatic nuclei. These atypical cells were in the form of solid islands and cribriform structures with necrotic debris. Immunohistochemical study was patchypositive for CK20; diffuse and strong positive for PanCK and EMA; nuclear-positive for CDX2 and positive for SALL4. According to the histopathological and immunohistochemical findings, the patient was diagnosed with cutaneous metastasis of either colorectal adenocarcinoma or scrotal germ cell tumor. Our patient was referred to the oncology department for systemic evaluation; his scrotal ultrasonography was completely normal. Therefore, the diagnosis of scrotal germ cell tumor was excluded. Colonoscopy was planned for definitive diagnosis of colorectal adenocarcinoma. Our patient died as a result of serious intestinal bleeding, hours after taking laxatives for pre-op preparation. Therefore, treatment and follow-up of the patient could not be performed.
Case Report #2
A 54-year-old female patient presented for evaluation of pruritic skin lesions on her posterior trunk. The lesions were present for several months. Her personal and family history of illness was unremarkable. Dermatologic examination revealed multiple, erythematous and skin colored, pruritic nodules on the posterior trunk (Figure 1B). A 4 mm punch biopsy was performed with preliminary diagnoses of cutaneous lymphoma, romatoid nodule, cutaneous leukemia and cutaneous metastasis. Histopathological examination revealed intact epidermis, atypical epithelial cells with hyperchromatic and vesicular nuclei, invading dermis and subcutaneous tissue. Immunohistochemical study was negative for E-Cadherin and positive for estrogen receptor (ER). According to the biopsy report and immunohistochemical results, our patient was diagnosed with cutaneous metastasis of invasive lobular breast carcinoma. She was referred to general surgery for further evaluation. Unfortunately, the patient was lost to follow-up.
Case Report #3
A 58-year-old female patient came to our clinic with complaints of redness and nodular lesions on her left breast. The lesions had been present for 1.5 months. She had been diagnosed with invasive ductal breast cancer a year before and she had undergone mastectomy and received 3 cures of radiotherapy. Skin lesions occurred 5 months after this treatment. In the dermatological examination, there were red, firm nodules on an erythematous background on her left breast. Some of the nodules had hemorrhagic crusts on them (Figure 2A). Two 4 mm punch biopsies were performed from the erythematous plaque and from the nodule. In the biopsy specimens taken from both regions, tumor islands consisting of atypical cells with pleomorphic nuclei, prominent nucleoli, and faint cytoplasm were observed in the dermis. Immunohistochemically, negative staining with GATA3, mammaglobin, GCDFP-15, ER and Cerb-B2, and diffuse membranous positive staining with E-Cadherin were observed.
As a result of these findings, our patient was diagnosed with cutaneous metastasis of invasive ductal carcinoma of the breast. The patient was consulted to the oncology department for chemotherapy treatment.
Case Report #4
A 67-year-old male patient was consulted to our clinic with an erythematous rash on the tip of his nose. His past medical history included squamous cell carcinoma (SCC) of the lung and he was taking tyrosine kinase inhibitor for his condition. The patient had a red-violet plaque on his nose tip, with desquamation and hemorrhagic crusts (Figure 2B). An incisional biopsy was performed considering acneiform eruption secondary to tyrosine kinase inhibitor, as the initial diagnosis. His biopsy result was consistent with cutaneous metastasis of SCC of the lung. The patient was referred to the oncology department for treatment; unfortunately, he was lost to follow-up.
Case Report #5
A 72-year-old male patient presented to our clinic for evaluation of a livid, painful nodule on his right submandibular region (Figure 3). The nodule was present for 3 months and showed no response to topical antibiotic treatment. Her personal history of illness included chronic obstructive pulmonary disease. A 3 mm punch biopsy was obtained; initial diagnoses were cutaneous metastatic tuberculosis, sweet syndrome and cutaneous lymphoma. Histopathology result was consistent with cutaneous metastasis of large cell carcinoid tumor of the lung. Immunohistochemical staining was positive for TTF-1, CD56 and synaptophysin. Unfortunately, our patient passed away 6 months after his diagnosis.
Figure 1.
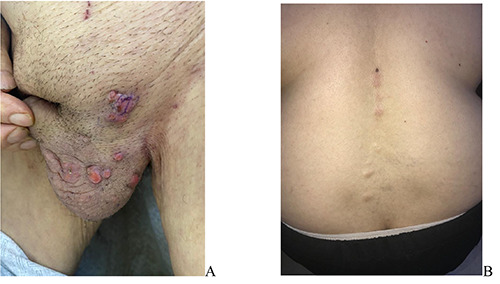
A) Multiple, erythematous, pruritic nodules in the scrotal region of the patient; B) Multiple, erythematous and skin coloured, pruritic nodules on the posterior trunk of the patient.
Figure 2.

A) Red, firm nodules with hemorrhagic crusts on an erythematous background on left breast of the patient; B) Red-violet plaque on the nose tip, with desquamation and hemorrhagic crusts.
Figure 3.

Livid, painful nodule on right submandibular region of the patient.
Discussion
Skin metastases from internal malignancies are very rare with an incidence between 0.7-10%.1 Cutaneous metastases are usually seen in an advanced stage of internal malignancies; dissemination can be via hematologic or lymphatic route, direct extension or surgical implantation.2 The most common primary sites of cutaneous metastases are lung cancer, colon cancer, melanoma and squamous cell carcinoma (oral cavity) respectively, in males; breast cancer, colon cancer, melanoma and ovarian cancer respectively, in females.3
Cutaneous metastasis of colorectal cancer is very rare, with an incidence between 2.3-6%.4 The most frequent sites of skin metastases include abdomen, extremities, perineum, head, neck, and penis.
Scrotum is an exceedingly unusual site for colorectal cancer metastasis.5 These metastases generally occur within the first 2 years following surgery and often present simultaneously with metastases to the liver, peritoneum, and lung.6
Scrotal metastatic lesions of colorectal carcinoma are various, ranging from papules, nodules, ulcers, plaques and erythematous, sclerodermoid areas.7 Patients can be asymptomatic or can present pain or pruritus. Our patient presented painless, pruritic nodules.
There are only few cases of colorectal metastasis to the scrotum, in the literature. The majority of the reported cases had colorectal adenocarcinoma, as in our case, while the rest of them had colorectal squamous cell carcinoma.7 In most cases, scrotal metastases appeared months after the diagnosis of primary malignancy. However, our patient was unaware of his colorectal cancer, at the time of presentation to our clinic.
Histopathologically, scrotal metastases share similar findings with the primary cancer. These findings include atypical tumoral cells with pleomorphic, hyperchromatic nuclei and increased mitotic activity, as in our patient.
Breast cancer is the most common malignancy that metastasizes to the skin, in females. Five to ten percent of women with breast cancer present cutaneous metastasis.8 The most common histologic subtype of breast cancer is invasive ductal carcinoma; breast adenocarcinomas - lobular and ductal breast carcinomas - are the most common histologic subtypes to manifest cutaneous metastasis. Invasive lobular carcinomas are more likely to be positive for estrogen and progesterone receptors compared to invasive ductal carcinomas, which was consistent with our cases.9
Furthermore, lung cancer is the leading cause of cancer-related deaths in both sexes. About 85% of lung cancers are non-small cell lung cancers and squamous cell carcinoma is the most common subtype. The incidence of lung cancer with cutaneous metastases is between 1–12%, with the highest incidence in males. The common sites of skin metastases from lung cancer are head and neck, chest and abdomen. Cutaneous metastases usually present with firm, painless nodules, with or without ulceration.
In addition, skin metastases are associated with poor prognosis, with an average survival between 3 and 5 months.10
Skin lesions arising from lung cancer may develop before diagnosis of the primary tumor and can be spread by the venous, arterial or lymphatic system. A retrospective analysis by Schoenlaub et al. demonstrated that large cell lung cancer is the most common lung cancer type presenting with skin metastases, whereas SCC is the least likely. 11 Carcinoid tumors are derived from enterochromaffin cells in the gastrointestinal tract (65%) and bronchopulmonary tract (25%). Skin metastasis is very uncommon; they mostly present as multiple, erythematous- violaceous nodules. The histopathological and immunohistochemical studies are used for definitive diagnosis of carcinoid cutaneous metastases. There is dermal and sometimes subcutaneous infiltration by uniform tumor nests and sheets of cells, with hyperchromatic oval nuclei and scarce cytoplasm, showing immunoreactivity for neuroendocrine markers, including chromogranin, synaptophysin and low molecular weight cytokeratin. The immunoexpression of TTF-1 and CDX2 is helpful in determining the primary site. TTF-1 has high sensitivity and specificity for carcinoid tumors originating in the lung, whereas CDX2 expression is highly specific for tumors of gastrointestinal origin. Although rare, cutaneous metastasis of carcinoid tumors may represent the first sign of an unknown primary neuroendocrine tumor.12
Conclusions
Cutaneous metastases from internal malignancies represent wide spectrum of clinical appearances and can act as the great mimicker in our practice. Therefore, dermatologists should consider skin metastases in their differential diagnosis of dermatologic diseases.
Acknowledgement
Special thanks to Icim Komurcugil’s father, Hasan Komurcugil.
Funding Statement
Funding: None.
References
- 1.Sariya D, Ruth K, Adams-McDonnell R, et al. Clinicopathologic correlation of cutaneous metastases: experience from a cancer center. Arch Dermatol 2007;143:613-20. [DOI] [PubMed] [Google Scholar]
- 2.Lehman JS, Benacci JC. Cutaneous metastasis of invasive ductal carcinoma of the breast to an infusaport site. Cutis 2008;81:223-6. [PubMed] [Google Scholar]
- 3.Johnston RB. Weedon's skin pathology essentials. 2nd ed. Amsterdam, Netherlands: Elsevier; 2016. [Google Scholar]
- 4.Wang DY, Ye F, Lin JJ, Xu X. Cutaneous metastasis: a rare phenomenon of colorectal cancer. Ann Surg Treat Res 2017;93:277-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lookingbill DP, Spangler N, Helm KF. Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patients. J Am Acad Dermatol 1993;29:228-36. [DOI] [PubMed] [Google Scholar]
- 6.Liao L, Cheng Q, Zhu G, et al. Cutaneous metastasis of ascending colon cancer harboring a BRAF V600E mutation: a rare case report. Medicine (Baltimore) 2020;99:e20026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Udkoff J, Cohen PR. Adenocarcinoma of the colon presenting with scrotal metastasis: case report and review of the literature. Dermatol Online J 2016;22:13030. [PubMed] [Google Scholar]
- 8.Tan AR. Cutaneous manifestations of breast cancer. Semin Oncol 2016;43:331-4. [DOI] [PubMed] [Google Scholar]
- 9.Nahhas AF, Scales AT, Pfeifle J, Stephenson SR. An unusual presentation of cutaneous metastatic lobular breast carcinoma. Cutis 2021;107:E23-E26. [DOI] [PubMed] [Google Scholar]
- 10.Khaja M, Mundt D, Dudekula RA, et al. Lung cancer presenting as skin metastasis of the back and hand: a case series and literature review. Case Rep Oncol 2019;12:480-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schoenlaub P, Sarraux A, Grosshans E, et al. Survie après métastases cutanées: étude de 200 cas [Survival after cutaneous metastasis: a study of 200 cases]. Ann Dermatol Venereol 2001;128: 1310–5. [PubMed] [Google Scholar]
- 12.Fiorio LM, Diniz LM, Lucas EA. Cutaneous metastasis on the nasal tip: first clinical sign of pulmonary carcinoid tumor. An Bras Dermatol 2021;96:578-80. [DOI] [PMC free article] [PubMed] [Google Scholar]


