Abstract
Background
Evaluating upper limb (UL) interventions after stroke calls for outcome measures that describe impact on daily life in the community. UL use ratio has been used to quantify the performance domain of UL function, but generally focuses on arm use only. A hand use ratio could provide additional information about UL function after stroke. Additionally, a ratio based on the role of the more-affected hand in bilateral activities (stabilizer or manipulator) may also reflect hand function recovery. Egocentric video is a novel modality that can record both dynamic and static hand use and hand roles at home after stroke.
Objective
To validate hand use and hand role ratios from egocentric video against standardized clinical UL assessments.
Methods
Twenty-four stroke survivors recorded daily tasks in a home simulation laboratory and their daily routines at home using egocentric cameras. Spearman’s correlation was used to compare the ratios with the Fugl-Meyer Assessment-Upper Extremity (FMA-UE), Action Research Arm Test (ARAT), and Motor Activity Log-30 (MAL, Amount of Use (AoU), and Quality of Movement (QoM)).
Results
Hand use ratio significantly correlated with the FMA-UE (0.60, 95% CI: 0.26, 0.81), ARAT (0.44, CI: 0.04, 0.72), MAL-AoU (0.80, CI: 0.59, 0.91), and MAL-QoM (0.79, CI: 0.57, 0.91). Hand role ratio had no significant correlations with the assessments.
Conclusion
Hand use ratio automatically extracted from egocentric video, but not hand role ratio, was found to be a valid measure of hand function performance in our sample. Further investigation is necessary to interpret hand role information.
Keywords: wearable technology, egocentric video, stroke, upper limb, hand function, home-based assessment, outcome measures
Introduction
Upper limb (UL) function is one of the determinants of independence in activities of daily living (ADLs) after stroke. To evaluate the ultimate impact of novel treatments for UL function in daily life, an outcome measure that captures UL function outside of clinical settings is required. The International Classification of Functioning, Disability and Health (ICF) describes the activity domain of function as containing the sub-domains of performance and capacity; the former measures the function demonstrated in an individual’s living environment and the latter measures their highest function in a standardized environment. 1 Measuring UL function in the community belongs to the performance domain and corresponds to only 2 standardized clinical assessments: Motor Activity Log (MAL) 2 and Stroke Impact Scale. 3 However, both assessments are self-reported questionnaires and may be limited by response bias and cognitive issues. Objective assessments of UL performance are required to evaluate UL function for community-dwelling stroke survivors.
To address this need, UL use ratio has been proposed as a sensor-based measurement that quantifies UL performance and has been applied in various environments. The concept is based on describing the amount of more-affected limb use as a fraction of the amount of less-affect limb use. The UL use ratio is very stable and close to one among healthy individuals, 4 however, the ratios reported for stroke survivors vary between studies.5,6 Most studies that reported UL use ratios used wrist-worn devices, such that the ratios described the arm use of stroke survivors rather than hand use.7-9 In contrast, in clinical UL assessments, arm function, and hand function are measured in different subtests to separately evaluate reaching and grasping, such as in the Fugl-Meyer Assessment for Upper Extremity (FMA-UE). 10 How a hand manipulates an object highly depends on the level of hand function impairment. Investigating hand use in addition to arm use is valuable and provides different information about UL function. In addition to hand use, the role of the more-affected hand is another distinct piece of information about hand function during bilateral activities. The role of a hand, as defined in the Chedoke Arm and Hand Activity Inventory (CAHAI), 11 can consist of stabilization or manipulation. All aspects of UL use may depend on impairment level,6,12 the environment in which it is observed,12-14 and whether the dominant hand is affected. 15 These factors call for ecologically valid assessment of hand use and hand role in real-world conditions.
Wearable technologies that have previously been applied to capture UL use include accelerometers,16-19 magnetometers,20,21 force myography,22,23 and wearable cameras.7,24 Finger-worn accelerometers and magnetometers capture hand movements, but may interfere with a stroke survivor’s naturalistic movements during activities, and the functional interpretation of finger movements is not trivial. 21 In addition, wrist-worn accelerometers cannot distinguish functional movements using a threshold due to the heterogeneity of the more-affected limb movements after stroke.19,25 Wrist-worn force myography has been applied to detect reach-to-grasp movements in the community and the reported hand use ratios were approximately 0.3 for stroke survivors and 0.7 for healthy individuals. 23 Hand use ratio from finger-worn accelerometers in a laboratory setting has been reported to have significant correlations with the MAL, the Functional Ability Scale, and the FMA-UE. 8 Despite the high correlation between hand use ratio and clinical UL assessments, additional details are limited due to the lack of studies describing the hand use ratios of community-dwelling stroke survivors. As for hand role, stroke survivors with severe hand function impairment reported in a survey that they were more likely to use their more-affected hand in tasks where it served as a stabilizer; in contrast, respondents with mild impairment reported a greater likelihood to use their more-affected hands in tasks where it would act as a manipulator. 11 No data about measured hand role ratios have been reported, yet this information may be beneficial to quantify performance differences between the 2 hands. Wearable cameras (egocentric video) can record hand movements in context without interfering with the naturalistic movements during activities, and hand use can be identified from the recorded videos using computer vision.26,27 Video data contains information about hand grasp type, compensatory movements, environment facilitators or barriers, and objects involved in a task, which are relevant to interpreting the functional intent of the movement. The rich content of egocentric video is foreseen to provide additional information compared to motion-based sensors, and the potential benefits of this sensor modality for measuring hand use and hand roles warrant investigation. Therefore, egocentric video was chosen to capture hand function performance in this study. To date, the hand use and hand role ratios extracted from egocentric videos of community-dwelling stroke survivors have not been reported and validated against standardized clinical UL assessments. The aim of this study was to validate the hand use ratio and the hand role ratio of stroke survivors in the community.
Methods
Participants
The study was approved by the Research Ethics Board of the University Health Network. Individuals who experienced a stroke were invited to participate in the study. A required sample size of 22 was determined a priori using an estimated correlation coefficient of at least .5, a desired power of .8, and α set to .05, and increased to 25 to account for drop-outs. 28 Written informed consent from participants and their caregivers (if involved) was obtained before enrollment. The inclusion criteria for participants were the following: (1) at least 6 months post-stroke; (2) self-reported difficulty in daily life due to an impairment of the more-affected hand; (3) impaired but not absent hand function, defined as a total Action Research Arm Test (ARAT) score above 10 29 ; (4) Montreal Cognitive Assessment (MoCA) score above 21, to avoid potential cognitive difficulties 30 ; (5) no subluxation or significant pain when using their UL s; and (6) no other neuromusculoskeletal disease affecting UL movements other than stroke.
Study Protocol
Two study visits in a home simulation laboratory at the KITE Research Institute were scheduled for each participant. In the first visit, the researcher obtained consent from participants and their caregivers. The researcher then administered the MoCA and the clinical UL assessments, including the FMA-UE, the ARAT, and the MAL-30. In the second visit, the researcher demonstrated how to use a head-mounted egocentric camera (GoPro Hero 5, GoPro Inc., CA, USA) and participants familiarized themselves with the procedure. The detailed protocol can be found in Tsai et al. 31 After participants learned how to use the camera, 38 daily tasks were carried out in a naturalistic manner in the laboratory while recording egocentric videos. Subsequently, the researcher discussed the participants’ daily routines with them and together agreed on some representative portions of their schedule to record at home. The recording times were selected to capture tasks that they typically carried out during a week and were distributed across different days or times in order to capture a variety of representative tasks. Participants were asked to record a total of 3 sessions, each 1.5 hours long, and to perform the recorded activities as they normally would. The researcher reminded participants about potential privacy issues when recording at home and about the chance to review videos before returning them. The egocentric videos were recorded at 1280 × 720 resolution with 30 frames per second. Participants could return videos in an additional onsite visit or by mailing a prepaid parcel.
Hand Use
Hand use was quantified based on hand-object interactions. The definition of a hand-object interaction was the manipulation of an object by the hand(s) for a functional purpose. The occurrence of hand use in the videos was captured using the Hand Object Detector 32 deep neural network. In our previous work, this algorithm was found to have the best performance for detecting hand-object interactions in egocentric videos recorded by stroke survivors in their home environments, with an average Matthews correlation coefficient of 0.54 ± 0.19 for more- and less-affected hands combined. 33 Each image was fed into the Hand Object Detector to generate hand and object locations and hand contact status as outputs (Figure 1). Portable object contact predictions were categorized as hand uses. The hand use ratio of each participant was calculated as the total number of hand use instances of the more-affected hand over the less-affected hand in their videos recorded at home (equation (1)).
Figure 1.
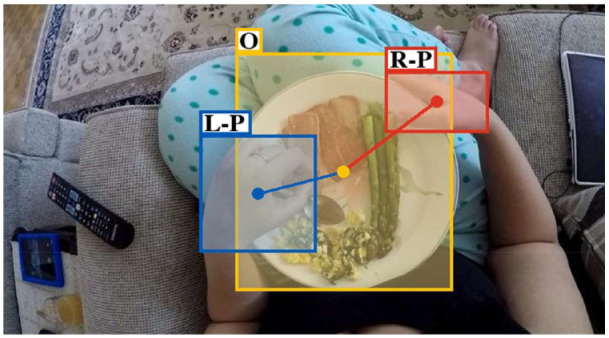
An example of the generated output of an image from home recordings using the Hand Object Detector. Red, blue, and yellow rectangles are right hand (R), left hand (L), and manipulated object (O) locations, respectively. Detected hand contact status in this example was portable object (P) for both hands, as indicated after the hand side label.
| (1) |
M is the total number of self-recorded videos at home, and m is each numbered video from 1 to M. A hand use instance refers to one hand being used in a given video frame. One frame may have 2 hand instances, depending on the number of hands visible in the frame.
Hand Role
Hand roles include stabilizer and manipulator. A stabilizer is defined as a hand that is in static contact with an object without changing the contact area between them (a static interaction) and a manipulator is defined as a hand that is moving an object with the contact area changing over time (a dynamic interaction). An example of the 2 hand roles is provided in Figure 2. The hand role ratio was the total number of manipulation instances over the total number of stabilization instances for the more-affected hands (equation (2)). A manipulation involves more finger movements and shows more fine motor skills than a stabilization, so a higher hand role ratio is hypothesized to correspond to better hand function on the more-affected side. A 2 or 3 bilateral activities in the videos recorded at home and 3 to 8 bilateral tasks in the videos recorded in the home simulation laboratory were manually annotated in order to calculate the hand role ratio for each participant. In the bilateral tasks, hand role was annotated from the instances labeled as interactions (Figure 2). A hand that is not in contact (no interaction) with an object has no hand role. The inter-rater reliabilities of hand role and hand-object interaction annotations were reported in Tsai et al. 33 and showed substantial agreement. No constraints were imposed on how participants carried out the tasks. The number of bilateral tasks depended on the participant’s routine and whether they used their more-affected hands, hence, the number of tasks used in the analysis varied among participants. The bilateral tasks in the laboratory were included to increase the number of analyzed tasks and ensure that each participant at least had some data for analysis. It was possible for the tasks recorded at home not to include bimanual object interactions, because each individual carried out their routines in their usual manner.
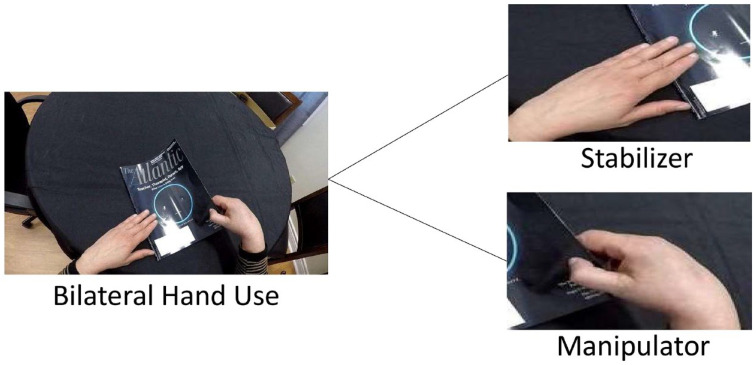
Figure 2.
A task with bilateral hand use was manually annotated for hand roles in each image, including stabilizer and manipulator. Using reading a book as an instance here, a stabilizer (left hand) has a static contact with the book and a manipulator (right hand) is moving the book to flip pages.
| (2) |
N is the total number of bilateral tasks used in both datasets, and n is each numbered task from 1 to N.
Statistical Analysis
To validate the hand use and hand role ratios from egocentric videos, Spearman’s correlation coefficients were calculated between the 2 ratios and the clinical UL assessment scores for the FMA-UE, ARAT, and MAL-30. The 95% confidence interval (CI) of the correlation coefficient in each assessment was also reported. Significance was set as a P-value less than .05. A correlation coefficient ranging from .2 to .6 was fair, .6 to .8 was moderate, and above .8 was strong correlation.34,35 Significant correlations with the FMA-UE, ARAT, and MAL was the criterion for accepting the hand use ratio or hand role ratio as a valid measure of the performance domain of the ICF for hand function after stroke.
Results
Twenty-four participants (7 females and 17 males) were enrolled in this study. No significant difference was found in the total scores of the FMA-UE and ARAT between participants whose dominant side was the more-affected (n = 12) and less-affected side (n = 12) using a two-sample t-test. The average age of participants was 60.9 ± 12.8 years old and they returned an average of 4.0 ± 1.3 hours of home recordings. The home recordings after removing frames that had privacy concerns participants were unaware of reached an average of 3.9 ± 1.2 hours per participant and these recordings were used for the hand use ratio analysis. For the hand role ratio analysis, an average of 2580.4 ± 1957.1 frames from the bimanual tasks recorded at home and the laboratory were manually annotated with inter-rater reliability above 0.85 33 and investigated.
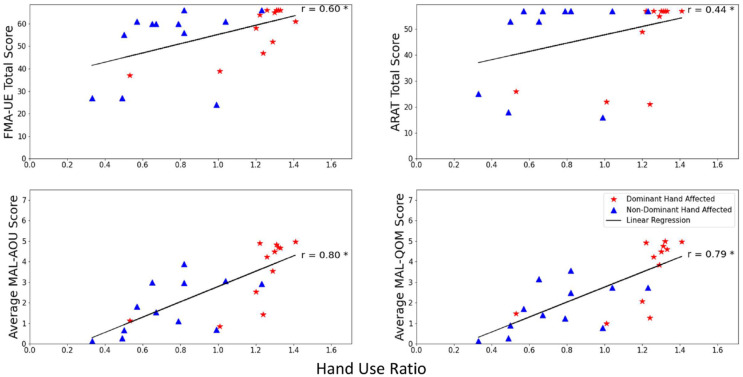
The average hand use ratios of all participants (n = 24), those who had the more-affected hands on the dominant side (n = 12), and those who did not (n = 12), were 0.97 ± 0.34, 1.20 ± 0.23, and 0.74 ± 0.26, respectively. Participants whose more-affected hands were on the dominant side had higher hand use ratios than the others. Spearman’s correlation coefficients of the hand use ratios and the total scores of the FMA-UE, the total scores of the ARAT, and the average rating of the MAL-AoU and QoM were .60 (moderate, P < .05, CI: 0.26, 0.81), .44 (fair, P < .05, CI: 0.04, 0.72), .80 (strong, P < .001, CI: 0.59, 0.91), and .79 (moderate, P < .001, CI: 0.57, 0.91), respectively. Fair to moderate correlation coefficients were found between the ratios and hand-related subscores of the assessments (Supplemental Material), which were .51 (P < .05) for the FMA-UE hand subscore and .45 (P < .05) for the ARAT pinch subscore. The scatter plots and the Spearman’s correlation coefficients between the ratios and the assessment scores are provided in Figure 3.
Figure 3.
Scatterplot of the hand use ratios and the total scores of the Fugl-Meyer Assessment for Upper Extremity (FMA-UE, r = .60), the Action Research Arm Test (ARAT, r = .44), the Amount of Use (AoU, r = .80), and the Quality of Movement (QoM, r = .79) of the Motor Activity Log-30 (MAL). Linear regression lines are shown since significant Spearman’s correlations were found with the assessments.
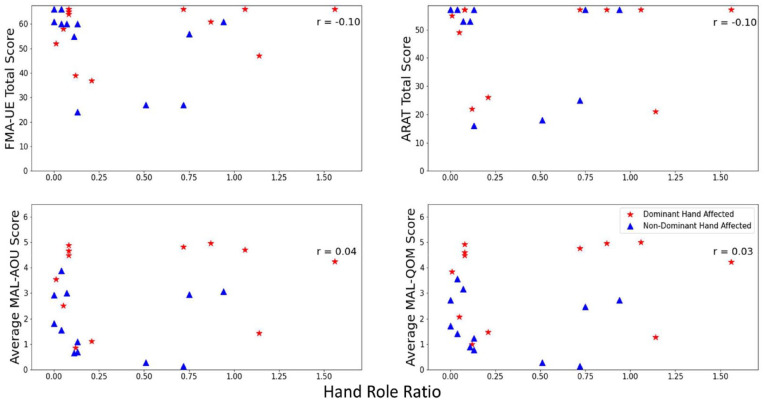
The average hand role ratios were 0.39 ± 0.46 for all participants, 0.50 ± 0.54 for those with their more-affected hands on the dominant side, and 0.29 ± 0.34 for those with the hands on the non-dominant side. No significant Spearman’s correlation coefficient was found between the hand role ratios and any UL function assessment score. The Spearman’s correlation coefficients were −.10 (CI: −0.48, 0.32) with the total score of the FMA-UE, −.10 (CI: −0.48, 0.32) with the total score of the ARAT, .04 (CI: −0.37, 0.44) with the average rating of the MAL-AoU, and .03 (CI: −0.38, 0.43) with the MAL-QoM. As for the hand-related subscores of the FMA-UE and the ARAT (Supplemental Material), the non-significant Spearman’s correlation coefficients were −.25 and −.20, respectively. The scatter plots of the hand role ratios and the clinical UL assessment scores are shown in Figure 4.
Figure 4.
Scatterplot of the hand role ratios and the total score of the Fugl-Meyer Assessment for Upper Extremity (FMA-UE, r = −.10), the Action Research Arm Test (ARAT, r = −.10), the Amount of Use (AoU, r = .04), and the Quality of Movement (QoM, r = .03) of the Motor Activity Log-30 (MAL). No significant Spearman’s correlations were found.
Discussion
This is the first study to demonstrate that hand use ratios measured from egocentric video can assess the performance domain of the ICF for hand function after stroke. The hand use ratios had significant and moderate to strong correlation with the MAL, which was the only clinical UL assessment in our study that targeted the performance domain, albeit through self-report. The correlation with the MAL was stronger than the ones with the FMA-UE and the ARAT, which also supported that hand use measured in this study captured the performance domain of hand function after stroke. The FMA-UE captures the body functions and structures as well as capacity domains of the ICF, whereas the ARAT captures capacity, and therefore it is expected that an assessment of performance would have weaker correlation with these measures than with the MAL. In addition, the ratios also had fair to moderate correlations with the total score and the subscores related to hand function in the FMA-UE and the ARAT, which supported the conclusion that using egocentric video to record ADLs at home can capture the performance of hand function after stroke. Although significant correlation coefficients were found with the FMA-UE hand subscores and the ARAT total scores and pinch subscores, these scores might have been impacted by ceiling effects, as participants in the study mostly had mild UL function impairments that led to a large portion of high subscores.
The hand use in the study included static hand use, which is not captured by accelerometers, magnetometers, or force myography. Our average hand use ratio was close to 1 and higher than the reported hand use ratios using force myography (TENZR device), which were 0.3 for stroke survivors and 0.7 for healthy individuals. 23 The large difference between our average hand use ratio and the one from the TENZR might be caused by additional instances of static hand use being captured in the study. Furthermore, the hand use ratio was also higher than the reported arm use ratios in accelerometry studies, with non-overlapping 95% CIs5,15,36,37 (Table 1). When hand use occurs, the corresponding arm use varies as a function of the task being carried out. 21 In addition, the correlation coefficients between the hand use ratio and the MAL (r = .80 for the MAL-AoU and .79 for the MAL-QoM) were higher compared to the ones between arm use ratios and the MAL.36-38 These results may indicate that the hand use ratio provides complementary information to the arm use ratio. Furthermore, the hand use ratios of the stroke survivors with their more-affected hands on the dominant side were higher than the others. The same phenomenon was also shown in a study regarding arm use ratios. 15 The fact that most of the participants had mild UL impairments in this study may have contributed to the group using their more-affected (dominant) hands more often.
Table 1.
Mean, Standard Deviation, and 95% Confidence Interval (CI) of Upper Limb (UL) Use Ratios and Their Correlation Coefficients With the Motor Activity Log (MAL).
| Study | Participants | Time after stroke | Device placement and duration worn | Environment | Ratio of UL usage* (95% CI) | Correlation between the ratio and MAL (95% CI) |
|---|---|---|---|---|---|---|
| This study | Chronic stroke (N = 24) | 4.1 ± 7.3 years | Head-worn camera for 4.5 hours | Home | 0.97 ± 0.34 (0.83, 1.11) | AoU: 0.8 (0.59, 0.91) QoM: 0.79 (0.57, 0.91) |
| Bailey and Lang 4 | Healthy individuals (N = 74) | N/A | 1 accelerometer on each wrist for 25 hours | Community | 0.95 ± 0.06 (0.94, 0.96) | N/A |
| Michielsen et al. 5 | Chronic stroke (N = 38) | 4.5 ± 3.2 years | 1 accelerometer on each wrist for 24 hours | Community | 0.45 | N/A |
| Bailey et al. 15 | Chronic stroke (N = 46) | Median: 0.9 years (IQR: 1.4 years) | 1 accelerometer on each wrist for 24 hours | Community | 0.64 ± 0.19 (0.59, 0.70) | N/A |
| Uswatte et al. 36 | Subacute and chronic stroke (N = 169) | 3-9 months | 1 accelerometer on each wrist for 3 days | Community | 0.56 ± 0.16 (0.54, 0.58) | QoM: 0.52 (0.40, 0.62) |
| Van der Pas et al. 37 | Chronic stroke (N = 45) | 2.0 ± 1.6 years | 1 accelerometer on each wrist for 3 days | Community | 0.69 ± 0.10 (0.66, 0.72) | AoU: 0.60 (0.37, 0.76) QoM: 0.66 (0.45, 0.80) |
| Uswatte et al. 38 | Subacute and chronic stroke (N = 222) | 3-12 months | 1 accelerometer on each wrist for 3 days | Community | 0.56 ± 0.16 (0.54, 0.58) | AoU: 0.52 (0.42, 0.61) QoM: 0.47 (0.36, 0.57) |
MAL, motor activity log; AoU, amount of use; QoM, quality of movement.
UL use ratio was calculated as more-affected/less-affected side for stroke survivors and non-dominant/dominant side for healthy individuals.
This study has demonstrated that egocentric video combined with artificial intelligence-based video processing can automatically detect hand function performance. In particular, the hand use ratio was highly correlated to the standardized community-based clinical outcome measure, the MAL. In the future, this technology can serve as an objective outcome measure for hand function performance after stroke at home. In addition, real-world impact and progress tracking after novel UL interventions could be quantified outside of clinical settings using this technology.
As for the hand role ratios, they were not found to be a valid measure for the performance domain of hand function after stroke. Currently, there is a lack of studies reporting the hand role ratios for stroke survivors and healthy individuals. Stone et al. 39 reported that healthy individuals mostly used the right hand for grasping and left hand for stabilization, however, no ratio was reported. A few left-handed individuals used their left hand for manipulation, however, a majority of them used the right hand for manipulations in the study. There may be a broader range of hand role ratios among left-handed individuals than right-handed ones. In our study, no significant correlation was found between the hand role ratios and any of the clinical UL assessments. The hand role ratio did not exhibit a change corresponding to the FMA-UE or the ARAT scores, which means that stroke survivors with milder hand function impairments might not be using their more-affected hands for manipulation more than individuals with more severe impairments. The difference may be due to 2 factors. One is that hand dominance would affect fine motor skills in addition to the severity of hand impairment. A healthy individual may use their dominant hand as a manipulator and the other one as a stabilizer since a dominant hand has better fine motor skills. Stroke survivors with their more-affected hands on the non-dominant side might use those hands mainly as stabilizers even if they recovered well. Therefore, the hand role ratio of the more-affected hands might not directly relate to the capacity domain of the UL function assessments. The average hand role ratios of the participants with their more-affected hands on the non-dominant side were all below 1 despite a wide range of FMA-UE scores, which meant that they used the hands mostly as stabilizers regardless of the severity of UL impairment (Figure 4). As for the performance domain, the MAL reports how often the more-affected hand is used rather than hand role, which quantifies how much fine motor skill is demonstrated when the hand is used.
The other factor was that the bilateral tasks may not contain manipulations. The tasks each participant recorded at home were varied due to different routines. Some bilateral tasks may contain only stabilizations, such as carrying an object with both hands, and led to the ratio being zero. A flaw of investigating the hand role ratio is that bilateral tasks might not happen if a stroke survivor with severe hand impairment only uses their less-affected hand in daily life. The hand role ratio may be more practical and helpful for those stroke survivors who use their more-affected hand often. In the future, a bilateral task that requires manipulation, such as the items in the CAHAI, can be used as a mutual task for participants and the measured ratios may be more comparable to the results in the CAHAI. The fact that the recorded tasks were not constrained to require bilateral hand use or to involve a manipulator hand may have contributed to the weak correlations between hand role ratios and clinical scores.
A potential drawback of using egocentric video to capture information in the home environment is that it engenders privacy considerations. Several steps were taken to avoid participant sharing videos with private information: the participants had full control over what to record, were reminded of situations to avoid (eg, computer screens with sensitive information), could stop the recordings at any time through a provided tablet, and had the opportunity to review all videos before returning them to the research team. 31 We previously reported the perspectives of stroke survivors on the use of egocentric video for rehabilitation applications. 40 Although privacy was our initial concern, the participants mostly reported that they did not have such a concern when recording at home. On the other hand, privacy was raised as an issue when recording in public, and most participants were unwilling to do so due to self-consciousness and the concerns for the privacy of others. Nonetheless, capturing information in the home environment is already representative of a large proportion of ADLs. Furthermore, despite the privacy considerations, egocentric video constitutes a novel platform that can be used in future studies to go beyond the quantity of hand use, and capture more detailed information about quality of hand use (eg, grasping ability) and the types of activities that users are prioritizing or struggling to perform.
Five limitations for measuring the hand use and hand role ratios in the study were identified. First, the number of frames for hand role ratios was limited and may not be representative of a broader range of tasks. Second, most participants in the study had mild UL impairments. Hand use and hand role ratios of stroke survivors with moderate and severe impairments need to be further investigated in order to better understand the generalizability of the findings reported here. Third, the methods for capturing hand use and hand role were different. Hand use ratios were automatically calculated from all the home recordings, which was more representative than hand role ratios from manual annotations on a subset of the data. This difference was necessary because we have previously found automated hand-object interaction detection to be much more reliable than hand role classification. 33 In the future, reporting the hand role ratio from the entire video dataset will be more informative, and would be facilitated by novel computer vision approaches for automated hand role classification. Fourth, although care was taken to ensure that participants understood the importance of recording representative examples of their typical routines, it is possible that observation bias may have altered the amount of hand use. Last, the cross-sectional validity of the hand use and hand role ratios was established, however, long-term investigation is still required. Measuring these 2 ratios is a relatively new topic. Therefore, tracking of the ratios over time is necessary to construct a better understanding of how much and what beneficial information regarding UL function can be derived from analyzing hand use and hand role. For example, do the 2 ratios demonstrate test-retest reliability, are they responsive to changes in hand function after an intervention, and does the performance of hand function among community-dwelling stroke survivors evolve over time?
Conclusion
Using egocentric video to capture hand use may provide additional information about UL function compared to arm use measures. Hand use ratio automatically extracted from egocentric video was found to be a valid measure of hand function performance in this sample. The hand use ratios significantly correlated with the UL assessment measures for the performance domain, which was the MAL (r = .80 for the AoU and .79 for the QoM), and the capacity and body structures and function domains, including the ARAT (r = .44) and the FMA-UE (r = .60), respectively. A longitudinal study of the hand use ratio will be beneficial to reveal what additional information about hand function performance this metric can provide. In addition, involving more stroke survivors with moderate or severe UL impairment is required to report the validity of hand use ratio for a broader range of UL impairment levels in the future. Hand role ratio had non-significant correlations with the clinical assessments in this study and therefore was not validated. Additional investigation with an emphasis on bilateral tasks that require manipulation should be carried out to provide a better understanding of hand role ratios.
Supplemental Material
Supplemental material, sj-docx-1-nnr-10.1177_15459683231159663 for Validity of Novel Outcome Measures for Hand Function Performance After Stroke Using Egocentric Video by Meng-Fen Tsai, Rosalie H. Wang and José Zariffa in Neurorehabilitation and Neural Repair
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Heart and Stroke Foundation of Canada [G-18-0020952].
ORCID iD: Meng-Fen Tsai  https://orcid.org/0000-0002-4594-7463
https://orcid.org/0000-0002-4594-7463
Supplementary material for this article is available on the Neurorehabilitation & Neural Repair website along with the online version of this article.
References
- 1.World Health Organization. Towards a Common Language for Functioning, Disability, and Health: ICF. The International Classification of Functioning, Disability Health. WHO; 2002. [Google Scholar]
- 2.Van der Lee J, Beckerman H, Knol D, De Vet H, Bouter L. Clinimetric properties of the motor activity log for the assessment of arm use in hemiparetic patients. Stroke. 2004;35(6):1410-1414. [DOI] [PubMed] [Google Scholar]
- 3.Duncan PW, Wallace D, Lai SM, Johnson D, Embretson S, Laster LJ. The stroke impact scale version 2.0: evaluation of reliability, validity, and sensitivity to change. Stroke. 1999;30(10):2131-2140. [DOI] [PubMed] [Google Scholar]
- 4.Bailey RR, Lang CE. Upper extremity activity in adults: referent values using accelerometry. J Rehabil Res Dev. 2014;50(9):1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Michielsen ME, Selles RW, Stam HJ, Ribbers GM, Bussmann JB. Quantifying nonuse in chronic stroke patients: a study into paretic, nonparetic, and bimanual upper-limb use in daily life. Arch Phys Med Rehabil. 2012;93(11):1975-1981. [DOI] [PubMed] [Google Scholar]
- 6.de Niet M, Bussmann JB, Ribbers GM, Stam HJ. The stroke upper-limb activity monitor: its sensitivity to measure hemiplegic upper-limb activity during daily life. Arch Phys Med Rehabil. 2007;88(9):1121-1126. [DOI] [PubMed] [Google Scholar]
- 7.Lang CE, Waddell KJ, Klaesner JW, Bland MD. A method for quantifying upper limb performance in daily life using accelerometers. J Vis Exp. 2017;122:e55673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim Y, Jung H-T, Park J, et al. Towards the design of a ring sensor-based mHealth system to achieve optimal motor function in stroke survivors. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2019;3(4):1-26.34164595 [Google Scholar]
- 9.Lang CE, Waddell KJ, Barth J, Holleran CL, Strube MJ, Bland MD. Upper limb performance in daily life approaches plateau around three to six weeks post-stroke. Neurorehabil Neural Repair. 2021;35(10):903-914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gladstone DJ, Danells CJ, Black SE. The Fugl-Meyer assessment of motor recovery after stroke: a critical review of its measurement properties. Neurorehabil Neural Repair. 2002;16(3):232-240. [DOI] [PubMed] [Google Scholar]
- 11.Barreca S, Gowland C, Stratford P, et al. Development of the Chedoke Arm and Hand Activity Inventory: theoretical constructs, item generation, and selection. Topics stroke Rehabil. 2004;11(4):31-42. [DOI] [PubMed] [Google Scholar]
- 12.Shim S, Kim H, Jung J. Comparison of upper extremity motor recovery of stroke patients with actual physical activity in their daily lives measured with accelerometers. J Phys Ther Sci. 2014;26(7):1009-1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rand D, Eng JJ. Disparity between functional recovery and daily use of the upper and lower extremities during subacute stroke rehabilitation. Neurorehabil Neural Repair. 2012;26(1):76-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Urbin M, Waddell KJ, Lang CE. Acceleration metrics are responsive to change in upper extremity function of stroke survivors. Arch Phys Med Rehabil. 2015;96(5):854-861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bailey RR, Birkenmeier RL, Lang CE. Real-world affected upper limb activity in chronic stroke: an examination of potential modifying factors. Topics Stroke Rehabil. 2015;22(1):26-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee SI, Liu X, Rajan S, Ramasarma N, Choe EK, Bonato P. A novel upper-limb function measure derived from finger-worn sensor data collected in a free-living setting. PLoS One. 2019;14(3):e0212484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu X, Rajan S, Ramasarma N, Bonato P, Lee SI. The use of a finger-worn accelerometer for monitoring of hand use in ambulatory settings. IEEE J Biomed Health Inform. 2018;23(2):599-606. [DOI] [PubMed] [Google Scholar]
- 18.Rand D, Eng JJ. Arm-hand use in healthy older adults. Am J Occup Ther. 2010;64(6):877-885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tang L, Halloran S, Shi JQ, Guan Y, Cao C, Eyre J. Evaluating upper limb function after stroke using the free-living accelerometer data. Stat Methods Med Res. 2020;29(11):3249-3264. [DOI] [PubMed] [Google Scholar]
- 20.Schwerz de Lucena D, Rowe J, Chan V, Reinkensmeyer D. Magnetically counting hand movements: validation of a calibration-free algorithm and application to testing the threshold hypothesis of real-world hand use after stroke. Sensors. 2021;21(4):1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rowe JB, Friedman N, Chan V, Cramer SC, Bachman M, Reinkensmeyer DJ. The variable relationship between arm and hand use: a rationale for using finger magnetometry to complement wrist accelerometry when measuring daily use of the upper extremity. Annu Int Conf IEEE Eng Med Biol Soc. 2014;2014:4087-4090. [DOI] [PubMed] [Google Scholar]
- 22.Simpson LA, Mow A, Menon C, Eng JJ. Preliminary examination of the ability of a new wearable device to capture functional hand activity after stroke. Stroke. 2019;50(12):3643-3646. [DOI] [PubMed] [Google Scholar]
- 23.Yang C-l, Liu J, Simpson LA, Menon C, Eng JJ. Real-world functional grasping activity in individuals with stroke and healthy controls using a novel wearable wrist sensor. Neurorehabil Neural Repair. 2021;35(10):929-937. [DOI] [PubMed] [Google Scholar]
- 24.Likitlersuang J, Visée RJ, Kalsi-Ryan S, Zariffa J. Capturing hand use of individuals with spinal cord injury at home using egocentric video: a feasibility study. Spinal Cord Ser Cases. 2021;7(1):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lum PS, Shu L, Bochniewicz EM, et al. Improving accelerometry-based measurement of functional use of the upper extremity after stroke: machine learning versus counts threshold method. Neurorehabil Neural Repair. 2020;34(12):1078-1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Likitlersuang J, Sumitro ER, Cao T, Visée RJ, Kalsi-Ryan S, Zariffa J. Egocentric video: a new tool for capturing hand use of individuals with spinal cord injury at home. J Neuroeng Rehabil. 2019;16(1):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsai M-F, Wang RH, Zariffa J. Identifying hand use and hand roles after stroke using egocentric video. IEEE J Transl Eng Health Med. 2021;9:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed.Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 29.Hoonhorst MH, Nijland RH, Van Den Berg JS, Emmelot CH, Kollen BJ, Kwakkel G. How do Fugl-Meyer arm motor scores relate to dexterity according to the action research arm test at 6 months poststroke? Arch Phys Med Rehabil. 2015;96(10):1845-1849. [DOI] [PubMed] [Google Scholar]
- 30.Borland E, Nägga K, Nilsson PM, Minthon L, Nilsson ED, Palmqvist S. The Montreal cognitive assessment: normative data from a large Swedish population-based cohort. J Alzheimer’s Dis. 2017;59(3):893-901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tsai M-F, Bandini A, Wang RH, Zariffa J. Capturing representative hand use at home using egocentric video in individuals with upper limb impairment. J Vis Exp. 2020;166:e61898. [DOI] [PubMed] [Google Scholar]
- 32.Shan D, Geng J, Shu M, Fouhey DF. Understanding human hands in contact at internet scale. Paper presented at: Proceedings of the IEEE/CVF Conference on Computer Vision and Pattern Recognition, Seattle, WA, USA, 14–19 June, 2020. [Google Scholar]
- 33.Tsai M-F, Wang RH, Zariffa J. Recognizing hand use and hand role at home after stroke from egocentric video. arXiv preprint arXiv:220708920. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Akoglu H. User’s guide to correlation coefficients. Turk J Emerg Med. 2018;18(3):91-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chan Y. Biostatistics 104: correlational analysis. Singapore Med J. 2003;44(12):614-619. [PubMed] [Google Scholar]
- 36.Uswatte G, Giuliani C, Winstein C, Zeringue A, Hobbs L, Wolf SL. Validity of accelerometry for monitoring real-world arm activity in patients with subacute stroke: evidence from the extremity constraint-induced therapy evaluation trial. Arch Phys Med Rehabil. 2006;87(10):1340-1345. [DOI] [PubMed] [Google Scholar]
- 37.van der Pas SC, Verbunt JA, Breukelaar DE, van Woerden R, Seelen HA. Assessment of arm activity using triaxial accelerometry in patients with a stroke. Arch Phys Med Rehabil. 2011;92(9):1437-1442. [DOI] [PubMed] [Google Scholar]
- 38.Uswatte G, Taub E, Morris D, Light K, Thompson P. The Motor Activity Log-28: assessing daily use of the hemiparetic arm after stroke. Neurology. 2006;67(7):1189-1194. [DOI] [PubMed] [Google Scholar]
- 39.Stone KD, Bryant DC, Gonzalez CL. Hand use for grasping in a bimanual task: evidence for different roles? Exp Brain Res. 2013;224(3):455-467. [DOI] [PubMed] [Google Scholar]
- 40.Tsai M-F, Atputharaj S, Zariffa J, Wang RH. Perspectives and expectations of stroke survivors using egocentric cameras for monitoring hand function at home: a mixed methods study. Disabil Rehabil Assist Technol. Published online October 7, 2022. doi: 10.1080/17483107.2022.2129851 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-nnr-10.1177_15459683231159663 for Validity of Novel Outcome Measures for Hand Function Performance After Stroke Using Egocentric Video by Meng-Fen Tsai, Rosalie H. Wang and José Zariffa in Neurorehabilitation and Neural Repair