Abstract
Background.
Health care executives and policymakers have raised concerns for the adequacy of the United States nursing workforce to meet service demands. Workforce concerns have risen given the SARS-CoV-2 pandemic and chronically poor working conditions. There are few recent studies that directly survey nurses on their work plans to inform possible remedies.
Methods.
In March, 2022 9,150 nurses with a Michigan license completed a survey on their plans to leave their current nursing position, reduce their hours, or pursue travel nursing. Another 1,224 nurses who left their nursing position within the past two years also reported their reasons for departure. Logistic regression models with backward selection procedures estimated effects of age, workplace concerns, and workplace factors on intent to leave, hour reduction, pursuit of travel nursing (all within the next year), or departure from practice within the past two years
Results.
Among practicing nurses surveyed, 39% intend to leave their position in the next year, 28% plan to reduce their clinical hours, and 18% plan to pursue travel nursing. Top-ranked workplace concerns among nurses were adequate staffing, patient safety, and staff safety. The majority of practicing nurses (84%) met the threshold for emotional exhaustion. Consistent factors associated with adverse job outcomes include inadequate staffing and resource adequacy, exhaustion, unfavorable practice environments, and workplace violence events. Frequent use of mandatory overtime was associated with a higher likelihood of departure from practice in the past two years (Odds Ratio 1.72, 95% CI 1.40–2.11).
Conclusions.
The factors associated with adverse job outcomes among nurses – intent to leave, reduced clinical hours, travel nursing, or recent departure – consistently align with issues that predated the pandemic. Few nurses cite COVID as the primary cause for their planned or actual departure. To maintain an adequate nursing workforce in the United States, health systems should enact urgent efforts to reduce overtime use, strengthen work environments, implement anti-violence protocols, and assure adequate staffing to meet patient care needs.
INTRODUCTION
The United States registered nurse population has experienced substantial strain over the past two years, which places patients at risk for harm. Nurses have delivered extraordinary care to individuals infected with the SARS-CoV-2 virus (COVID), individuals whose underlying disease course has been complicated by the pandemic, and to important communities. Nurses have delivered both acute and community-based care in rapidly changing and potentially dangerous contexts.
Media reports, policymakers, and health system leaders have cited growing concerns for the adequacy of the nursing workforce, yet few studies have quantified these concerns and examined contributing factors to nursing workforce departures. It is unclear from currently available data, for example, whether nurses are leaving their positions due to the clinical burdens of caring for COVID patients or whether already strained workplaces became intolerable. Nurses cite an adequate nursing workforce as a key determinant to high-quality care.1 Further, as a large proportion of the US nursing workforce reaches retirement age (the median age of US nurses is 52 years), it is important to examine nurses’ workforce decisions by age to understand how these decisions vary by years potentially available to remain in the workforce. Such an analysis provides the opportunity for health system leaders and policymakers to target recruitment and retention strategies. The National Academy of Medicine draft plan for health workforce well-being cited a dearth of recent, multi-site data to inform interventions and policy strategies.2
Given the absence of recent available data, we launched the Michigan Nurses Survey on February 22, 2022, with the goal of generating timely and actionable data to inform nursing workforce strategies. At the time of publication, Michigan ranked ninth among US states in both COVID cumulative cases and deaths.3 Through a statewide survey of current and recently employed registered nurses in one of the hardest-hit states in the nation, the survey results provide timely insights into the challenges that nurses have faced in their workplaces and identify opportunities to stem the losses of nurses from the US health care workforce.
Our four research questions were as follows:
Among practicing nurses, what proportion plan to make the following changes over the next year: leave their position, reduce their clinical hours, and/or pursue travel nursing?
What are the workplace conditions of practicing nurses, in terms of burnout, staffing adequacy, overtime use, and abusive events?
Among nurses who left clinical practice in the past two years, what factors were associated with their departures?
What workplace features were associated with intent to change clinical positions or leave the field entirely?
STUDY DATA AND METHODS
Study Population.
Individuals who held a valid, unrestricted license as a registered nurse in the State of Michigan as of February 2022 and provided email addresses were eligible to participate. Nurses with restricted licenses or those who were identified in the database as in a disciplinary process were excluded. 99 percent of registered nurses in the state provide email addresses upon licensure application or renewal.
Up to three email message invitations were sent to the sampling frame, eight days apart, following established procedures.4 No monetary incentives were offered, but individuals could request to receive a copy of the study results at the conclusion of the analysis.
To protect participant identities, the anonymous feature in Qualtrics™ (Provo, UT) was used to blind the study team from the email addresses of respondents; our team delivered reminders to those who had not yet responded, but identifiers were not linked to individual study data.
Nurses with multiple roles or positions were asked to report on their primary nursing position. Given the diversity of roles and employment arrangements, nurses were asked to answer survey questions that were pertinent to their role and skip any questions that were not. Hence, some outcomes analyzed have different sample sizes. The study protocol was reviewed by the University of Michigan and determined to be exempt from review. The survey included a larger set of research questions; this manuscript focuses on nurses’ job outcomes and potential factors associated with those outcomes, as guided by the four aforementioned research questions. The measures included in the survey and included in these analyses were chosen given their hypothesized relationships in extant models of clinician job outcomes.5–7
Job Outcomes.
Among currently practicing registered nurses, we examined three unique outcomes of intentions in the next year: to leave their current job, reduce their clinical hours from their current baseline, and/or pursue travel nursing.
Among all surveyed nurses, we asked whether they were currently practicing in nursing or not. For those who stated they were not currently practicing, we asked whether they had stopped working within the past two years (i.e., recently resigned). These questions allowed us to identify a cohort of nurses who had left their clinical position during the pandemic (i.e., between March 2020 to March 2022).
Top Workplace Concerns.
Among practicing and recently-resigned nurses, we asked them to rank their top three concerns in their current or most recent workplace (staffing, training, patient safety, staff safety, being recognized, promotion, getting breaks, and a write-in option).
Workplace Factors.
Our team hypothesized that several workplace factors would be associated with adverse nurse job outcomes. Among them, clinician burnout was measured using the 16-item Oldenburg Burnout Inventory,8 which reports a total score on a 5-point scale. Given prior work, we focused on the instrument’s emotional exhaustion subscale. Higher scores reflect greater levels of burnout, with emotional exhaustion scores above 2.25 considered clinically meaningful.9 We asked whether nurses had experienced workplace bullying, or physical, emotional, or sexual abuse in the past year.10 Using measures from prior surveys,11 we asked nurses to rate the overall quality of care delivered in their workplace (excellent, good, fair, or poor), whether their practice environments are favorable, mixed, or unfavorable to deliver high-quality care, and staffing and resource adequacy12 (5-point Likert scale). We also asked respondents if their workplace never used, rarely used, or frequently used mandatory overtime policies.
Demographic variables included age category and whether the nurse held an advanced practice role (midwife, anesthetist, nurse practitioner, or clinical nurse specialist).
Analyses.
Analyses were performed with SAS 9.4 (Cary, NC). After descriptive statistics were calculated for outcomes and independent variables, we used logistic regression models to examine the association of variables with the population odds of each outcome. In order to identify variables that were independently associated with each outcome and to eliminate the effect of collinearity when interpreting the coefficients, we employed model reduction techniques that included backward, stepwise, and best subset selection with inclusion criteria of alpha of 5%. When different reduction techniques yielded different models, we compared nested models using the likelihood ratio test, and un-nested models using the Bayesian Information criterion (BIC). Model diagnostics included examination of variance inflation factors (VIF) and a Hosmer-Lemeshow test for goodness of fit.
Stratification and Sensitivity Analyses.
In the accompanying appendix, we show full models with all variables examined, including those removed during selection procedures. We also show results separately for registered nurses with and without advanced practice degrees. We also show bivariate models unadjusted for important covariates like age and role (RN vs APRN.) (Appendix Table 4).
STUDY RESULTS
We received 167,534 email addresses of nurses with a Michigan license directly from the state’s Board of Nursing. We excluded 246 individuals whose licenses were under suspension or disciplinary review. We identified 2,103 email addresses in the database as invalid prior to survey deployment. Of 165,185 emails sent, 4,366 email messages were undeliverable and 2,565 opted out of the survey without explanation. 17,936 recipients (11% of the entire sample) opened the email survey invitation and among these, 13,687(76%) completed the survey. For the analyses reported herein, 9,150 reported that they currently practiced as a nurse and 1,224 reported that they had stopped practicing within the past two years. Table 1 shows participant characteristics.
Table 1.
Nurse Participant Characteristics, 2022
| Participants1 | |||
|---|---|---|---|
| Characteristics | Full Sample N= 13,687 | Currently practicing in nursing (n=9,150) | Left nursing practice in the past two years (n= 1,224) |
| n(%) | |||
| Age | |||
| - Under 25 | 216 (1.6) | 213 (2.3) | < 1 |
| - 25–34 | 1,295 (9.5) | 1172 (12.8) | 79 (6.5) |
| - 35–44 | 1,785 (13.0) | 1611 (17.6) | 86 (7.0) |
| - 45–54 | 2,036 (14.9) | 1838 (20.1) | 92 (7.5) |
| - 55–64 | 2,584 (18.9) | 1914 (20.9) | 348 (28.4) |
| - 65 and older | 1,787 (13.1) | 568 (6.2) | 462 (37.8) |
| Self-Described Gender | |||
| - Female | 8,687 (63.5) | 6,495 (71.0) | 969 (79.2) |
| - Male | 894 (6.5) | 736 (8.0) | 85 (6.9) |
| - Transgender | < 1 | < 1 | < 1 |
| - Nonbinary | < 1 | < 1 | < 1 |
| - Gender non-conforming | < 1 | < 1 | < 1 |
| - Another choice | < 1 | < 1 | < 1 |
| Race and Ethnicity2 | |||
| - Asian | 204 (1.5) | 173 (1.9) | < 1 |
| - Black or African American | 398 (2.9) | 313 (3.4) | 42 (3.4) |
| - Hispanic/Latino | 201 (1.5) | 176 (1.9) | 13 (1.1) |
| - Native American or Alaska Native | < 1 | < 1 | 15 (1.2) |
| - Native Hawaiian or Pacific Islander | < 1 | < 1 | < 1 |
| - White | 8587 (62.7) | 6454 (70.5) | 955 (78.0) |
| - Another answer | 279 (2.0) | 203 (2.2) | 32 (2.6) |
| - Unknown | < 1 | < 1 | < 1 |
| Nursing Role | |||
| -Registered Nurse | 8361 (61.1) | 6289 (68.7) | 918 (75.0) |
| -Advanced Practice | 1328 (9.7) | 1021 (11.2) | 149 (12.2) |
| Primary Nursing Setting | |||
| -Inpatient/Acute Care | 3887 (28.4) | 3887 (42.5) | 424 (34.6) |
| -Long-term care | 331 (2.4) | 331 (3.6) | 80 (6.5) |
| -Community/public health | 746 (5.5) | 746 (8.2) | 169 (13.8) |
| -School nursing | < 1 | 112 (1.2) | 21 (1.7) |
| -Nursing education | 184 (1.3) | 184 (2.0) | 38 (3.1) |
| -Other setting | 2074 (15.2) | 2074 (22.7) | 338 (27.6) |
Notes:
Data are expressed as No. (%) of participants. Cells with < 1% had too few observations to report precise numbers within each cell to protect privacy.
Participants could choose multiple categories.
Two variables – age and advanced practice status – were available on all registered nurses in the state. Age was categorized to enable comparable results with available state data on all nurses. When comparing our sample with the Michigan registered nurse census, the survey sample is similar to the distribution of advanced practice nurses. The age distribution differs slightly from the statewide data and 3,985 surveyed nurses did not answer the question. Details are provided in the Appendix, Table 1.
Top Workplace Concerns.
The most frequently-cited workplace concerns were shared between currently practicing nurses and nurses who had recently left practice: adequate staffing (83 and 70 percent, respectively), patient safety (60 and 57 percent), and staff safety (50 and 51 percent) (Appendix, Table 2). Promotion and compensation were the least frequently reported concerns of surveyed nurses (range of 3–6 percent).
In the analyses summarized below, we focus on registered nurses without advanced practice degrees given the pressing concerns for the registered nurse workforce across multiple settings. Findings for nurses with advanced practice roles are in the Appendix.
Burnout, Staffing Adequacy, Overtime, and Abusive Events
Selected nurse reports of explanatory variables are in Table 2. Among practicing nurses, the number with clinically-meaningful emotional exhaustion, reflected by a score of 2.25 or above, was 7,719(84%). Among currently practicing nurses who answered the question, 1,709(19%) reported their employer used mandatory overtime frequently, 1,978(22%) reported mandatory overtime occurred occasionally, and 3,439(38%) reported that their employer did not use mandatory overtime. The nurse survey offered nurses the opportunity to report four distinct workplace abusive events in the past year. Among respondents to this question, 3,921(43%) reported emotional abuse, 2,397 (26%) reported workplace bullying, 2,031(22%) reported physical abuse, and 903(10%) reported sexual abuse in the past twelve months. Only 3,692(40%) of nurses reported that staffing and resources were adequate to deliver patient care (at or above the theoretical midpoint of the scale).
Table 2.
Nurse-Reported Burnout, Overtime, Abuse Events in the Workplace, and Staffing and Resource Adequacy, 2022 (N=9,150)
| Variable | n | % |
|---|---|---|
| Emotional Exhaustion above threshold | 7,719 | 84.4 |
| Mandatory Overtime | ||
| -Never Used | 3,439 | 37.5 |
| -Used Occasionally | 1,978 | 21.6 |
| -Used Frequently | 1,709 | 18.7 |
| Workplace Abusive Events in Past 12 months | ||
| -Physical | 2,031 | 22.2 |
| -Emotional | 3,921 | 42.8 |
| -Workplace bullying | 2,397 | 26.2 |
| -Sexual | 903 | 9.9 |
| Staffing and Resource Adequacy | ||
| -Adequate (at or above scale midpoint) | 3,692 | 40.3 |
| -Inadequate (below scale midpoint) | 3,893 | 42.6 |
Note. Numbers and percentages might not add up to 100% due to missing data.
Practicing Nurses’ Intentions to Leave their Current Position.
Among the 9,150 practicing nurses in the sample, 3,576 (39%) planned to leave their current position within the next year: 1,554 within the next six months and 2,022 between 6 months and one year. The remaining 344 (58%) reported no plans to leave their position and 230 (2.51%) did not answer the question. Intention to leave was highest in the youngest age categories (59% among nurses under 25 years old and 53% among nurses 25–34 years), followed by nurses at or above the age of 65 (45%)(Figure 1).
Figure 1.
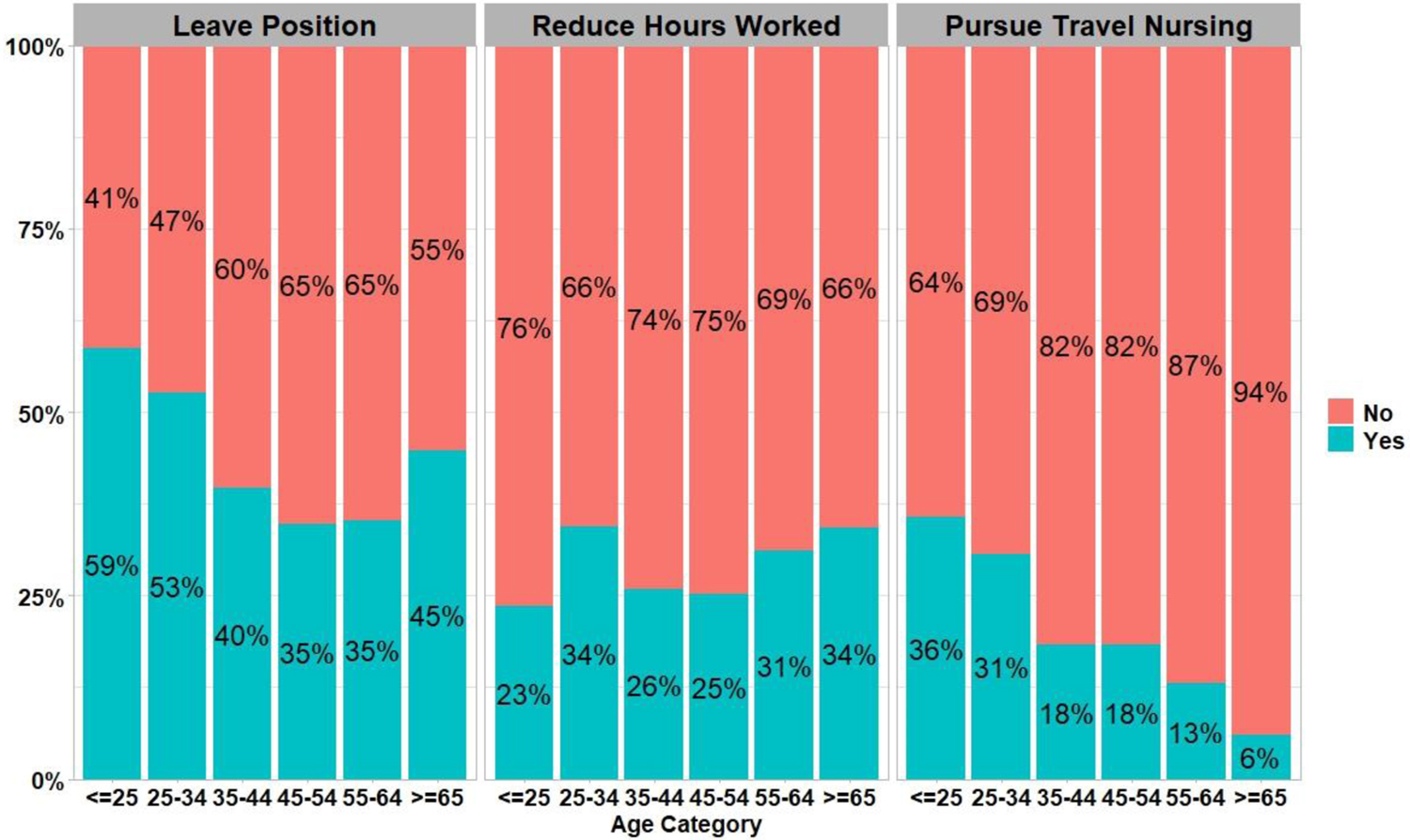
Currently Practicing Nurse Job Plans Within Next 12 Months by Age
Note: N of each age category. 1) <=25 years old=213, 2) 25–34 years old=1,172, 3) 35–44 years old=1,611, 4) 45–54 years old=1,838, 5) 55–64 years old=1,914, 6) >=65 years old=568
In multivariable logistic regression models, restricted to registered nurses without advanced practice degrees (Table 3), the following factors were associated with an increased likelihood of leaving in the next year: reported any type of abuse (physical, emotional, bullying, or sexual) event in the past year (Odds Ratio 1.27, 95% Confidence Interval 1.11–1.44), and higher subscale exhaustion scores on the Oldenburg Burnout Inventory (OR 1.72, 95% CI 1.48–2.01). Nurses were less likely to plan to leave their position when they rated their practice environment as favorable (OR 0.27, 95% CI 0.21–0.35) (versus unfavorable), reported higher staffing and resource adequacy (OR 0.87, 95% CI 0.82–0.92), and good (OR 0.34, 0.24–0.48) or excellent (OR 0.26, 95% CI 0.18–0.39) (versus poor) quality of care. Similar factors associated with employment plans were observed in the subset of nurses with advanced practice roles (Appendix, Table 3).
Table 3.
Associations between job outcomes and age and workplace factors among registered nurses, 2022
| Leave within one year N=5,9071,2 |
Reduce clinical hours N=5,9231,3 |
Pursue travel nursing N=5,9231,4 |
Left practice in past two years N=6,8211,5 |
|||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Age(ref. 65 and older) | ||||||||
| - Under 25 | 0.74 (0.51, 1.09) |
0.13 | 0.33 (0.22, 0.50) |
<0.001 | 5.83 (3.43, 9.90) |
<0.001 | 0.009 (0.002, 0.04) |
<0.001 |
| - 25–34 | 0.66 (0.51, 0.86) |
0.002 | 0.66 (0.51, 0.86) |
0.002 | 4.87 (3.08, 7.71) |
<0.001 | 0.06 (0.05, 0.09) |
<0.001 |
| - 35–44 | 0.41 (0.32, 0.53) |
<0.001 | 0.47 (0.37, 0.61) |
<0.001 | 2.58 (1.63, 4.09) |
<0.001 | 0.06 (0.04, 0.07) |
<0.001 |
| - 45–54 | 0.36 (0.28, 0.47) |
<0.001 | 0.48 (0.37, 0.62) |
<0.001 | 2.98 (1.85, 4.62) |
<0.001 | 0.05 (0.04, 0.07) |
<0.001 |
| - 55–64 | 0.41 (0.32, 0.53) |
<0.001 | 0.72 (0.56, 0.92) |
0.01 | 2.13 (1.34, 3.37) |
0.001 | 0.19 (0.16, 0.24) |
<0.001 |
| Reported any abusive event (ref. No) | 1.27 (1.11, 1.44) |
<0.001 | 1.26 (1.70, 1.44) |
<0.001 | 1.62 (1.38, 1.90) |
<0.001 | N/A6 | N/A6 |
| Emotional Exhaustion | 1.72 (1.48, 2.01) |
<0.001 | 1.36 (1.46, 1.97) |
<0.001 | N/A | N/A | N/A6 | N/A6 |
| Practice Environment (ref. Unfavorable) | ||||||||
| -Mixed | 0.53 (0.44, 0.63) |
<0.001 | 0.88 (.74, 1.03) |
0.11 | 0.83 (0.69, 1.00) |
0.05 | 0.62 (0.51, 0.77) |
<0.001 |
| -Favorable | 0.27 (0.21, 0.35) |
<0.001 | 0.62 (0.49, 0.78) |
<0.001 | 0.55 (0.41, 0.73) |
<0.001 | 0.45 (0.34, 0.60) |
<0.001 |
| Staffing and Resource Adequacy | 0.87 (0.82, 0.92) |
<0.001 | N/A | N/A | 0.89 (0.83, 0.95) |
<0.001 | 0.87 (0.80, 0.94) |
<0.001 |
| Quality of Care (ref. Poor) | ||||||||
| -Fair | 0.53 (0.38, 0.74) |
<0.001 | 0.83 (0.63, 1.09) |
0.19 | 0.67 (0.51, 0.89) |
0.006 | N/A | N/A |
| -Good | 0.34 (0.24, 0.48) |
<0.001 | 0.64 (0.48, 0.85) |
0.002 | 0.48 (0.35, 0.65) |
<0.001 | N/A | N/A |
| -Excellent | 0.26 (0.18, 0.39) |
<0.001 | 0.63 (0.45, 0.88) |
0.006 | 0.46 (0.31, 0.66) |
<0.001 | N/A | N/A |
| Overtime (ref. Not used) | ||||||||
| -Used frequently | N/A | N/A | 1.23 (1.07, 1.42) |
0.005 | N/A | N/A | 1.72 (1.40, 2.11) |
<0.001 |
| -Used occasionally | N/A | N/A | 1.03 (0.90, 1.18) |
0.66 | N/A | N/A | 1.31 (1.07, 1.59) |
0.008 |
| Staff Safety is a top concern | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Patient Safety is a top concern | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Adequate Staffing is a top concern | N/A | N/A | N/A | N/A | N/A | N/A | 0.55 (0.45, 0.69) |
<0.001 |
N reflects the denominator for each model. Observations dropped if missing data for any model covariates. 2Abusive events and burnout were only collected on currently working nurses.
N/A: Variable excluded from the reduced model.
N of nurses who plan to leave within one year=2,449, N of nurses who do not have plans to leave within one year=3,458.
N of nurses who plan to reduce clinical hours=1757, N of nurses who do not plan to reduce clinical hours=4,166.
N of nurses who plan to pursue travel nursing=1192, N of nurses who do not plan to pursue travel nursing=2,331.
N of nurses in model who left practice in past two years=810, N of nurses in model who did not leave practice in past two years=6011.
”Reported any abusive event” and “Exhaustion” not included in model for nurses who left practice in past two years.
Practicing Nurses’ Intentions to Reduce their Clinical Hours.
Of nurses currently practicing, both those with and without advanced practice roles, 2,549 (28%) reported plans to reduce their clinical hours within the next 12 months and 6,601 (72%) did not plan to do so. Higher exhaustion subscale scores from the Burnout Inventory were associated with increased likelihood of reducing clinical hours (OR 1.36, 95% CI 1.16–1.60) among registered nurses without advanced practice roles (Table 3).
Practicing Nurses’ Intentions to Pursue Travel Nursing.
Among practicing nurses, 1,652 (18%) planned to pursue travel nursing within the next 12 months and 7,498 (82%) did not plan to do so. Nurses below the age of 25 (OR 5.83, 95% CI 3.43–9.90) and 25–34 (OR 4.87, 95% CI 3.08–7.71) were more likely to report travel nursing plans (Table 3), as were nurses who experienced workplace abuse (OR 1.62, 95% CI 1.38–1.90). Nurses were less likely to pursue travel nursing with higher reported staffing and resource adequacy (OR 0.89, 95% CI 0.83–0.95), good (OR 0.48, 95% CI 0.35–0.65), or excellent (OR 0.46, 95% CI 0.31–0.66) quality of care, and a favorable practice environment (OR 0.55, 95% CI 0.41–0.73).
Factors associated with recent departure from the clinical nursing workforce.
For this analysis, we excluded survey respondents who left nursing more than two years ago. 1,224 (12%) nurses reported leaving the clinical nursing workforce in the past two years. The most frequent reasons cited for departure in the past two years were retirement (56%), stress of the position (38%), and inadequate staffing (32%). In multivariable analyses, factors associated with increased likelihood for recent workforce departure included frequent use of mandatory overtime (OR 1.72, 95% CI 1.40–2.11) (Table 3). Factors associated with lower likelihood for recent departure included higher staffing and resource adequacy (OR 0.87, 95% CI 0.80–0.94), younger age, and favorable practice environment (OR 0.45, 95% CI 0.34–0.60). Associations with job outcomes were similar for advanced practice nurses.
DISCUSSION
This study examined the views of practicing registered nurses and those who had recently left the nursing workforce to quantify factors associated with intent to leave, reduce their clinical hours, pursue travel nursing, and recent departure from the RN workforce thereby providing leaders and policymakers with actionable targets for interventions. This study found an alarmingly high rate of planned (39%) and recent departures (9%), as well as a high proportion of nurses who plan to make other changes, including reducing clinical hours (28%) and pursuing travel nursing (18%). Collectively, these actions are likely to disrupt the stability of the nursing workforce in the US health care system. Survey respondents reported high rates of emotional exhaustion and abusive events – physical, emotional, bullying, and sexual – in their workplace. Nurses also reported that staffing and resources were inadequate to deliver high-quality patient care. Importantly, these concerns correlated highly and significantly with adverse job outcomes.
Nurses who reported notable exhaustion were less likely to pursue travel nursing, perhaps reflecting that their personal and working conditions did not align with the potential stressors of relocation and orientation to new and challenging clinical assignments.
Our findings align with the recent literature. Namely, nurses’ concerns for adequate staffing and concerns for patient safety predate the pandemic.13 Nurses reported worsening rates of physical and mental health during the pandemic, which correlated with suboptimal working environments.14 Importantly, nurses reported helplessness and traumatic feelings with these increasingly challenging situations and sought institutional leadership for assistance;15,16 their calls for help went largely unanswered.17
The findings underscore the urgent need to correct factors leading to poor job outcomes such as the identification and correction of factors associated with burnout, coupled with policy strategies and facility-level changes to prevent workplace violence. While a relatively small group in the survey and in the overall profession, special attention should be paid to younger nurses, who report plans to workplace departures in relatively high proportions. Currently, it is unclear whether these plans reflect a broader societal trend of hastened job departures – termed the “Great Resignation” - among younger individuals, or whether this phenomenon is unique to nursing. Nurses of younger age were more likely to report anxiety and depression during the pandemic.18 Focused studies to identify their specific concerns and test targeted interventions for this age cohort are urgently needed to stem the potentially preventable losses of nursing personnel.
Study Limitations
Our sampling frame excluded very small numbers of nurses who declined to provide valid email addresses for the public use file (less than one percent). Nurses self-submitted email addresses, many of which were personal accounts and may be outdated, not routinely checked, or protected by anti-spam software. Due to the size of the sample, cash incentives were not possible to distribute equitably across the sample, which may have affected the overall response rate across the state’s registered nurse population. Potential participants may not have perceived the survey as relevant to them and opted to not engage. It is also possible that non-respondents have different perceptions of their workplaces and planned changes to their employment that are not captured in our analysis. To protect nurses’ identities we did not ask for residence or employer details, which would have enabled us to compare geographic differences. We also do not know whether nurse respondents or their dependents had been diagnosed with COVID, which may have influenced their reports. Our sampling frame excludes other health care professionals at risk for poor job outcomes, including physicians, pharmacists, respiratory therapists, medical/nursing assistants, and other essential members of the health care workforce.
The limitations above are presented among important strengths, including a large, statewide sample, which included those who had recently departed the workforce, reliance on previously used and validated measures, and timely data collection and analyses that are pertinent to pressing workforce policy questions. The completion rate of 76% of those who opened the survey compares favorably with other recently-published literature.19,20 Moreover, the distribution of age and advanced practice degrees correlates highly with the complete census of Michigan nurses,21 suggesting that our sample is representative of the population.
CONCLUSIONS
The findings from the large, rapid-scale survey of registered nurses has immediate implications for health care executives and policymakers. Solutions are available for many of the items cited by survey respondents.22 These include implementation of safer staffing models to support higher-quality nursing care; evidence for safer staffing models and potential legislation has existed for decades.23 Nurses who recently departed the workplace were more likely to report high use of mandatory overtime policies, suggesting that elimination of this management practice would promote retention efforts. Hospital executives do not need to wait for legislation, they can make these changes within their own institutions. Leaders can also restore trust with nurses through active listening, advocacy, and commitment to change work environments in ways that improve staff and patient outcomes.24
Policymakers can acknowledge the potential for substantial disruptions to the health care workforce and advance legislation that promotes safer, more supportive workplaces for nurses. Options include safer staffing legislation, policies to curtail mandatory overtime, and strengthened penalties, reporting, and corrective plans to reduce violence against health care workers. Legislators can advance appropriations for research funding opportunities that develop new models of nursing care delivery that urgently address patient and nurse outcomes.
The findings also suggest there is no time to waste. Without concerted efforts, it is likely that disruptions to the health care workforce will worsen, which will induce a spiral of additional resignations and threaten the delivery of essential care. Leaders need the moral courage to enact evidence-based strategies to stanch the hemorrhage of registered nurses and enable the US health care system to deliver the care that patients expect and deserve.
Supplementary Material
Acknowledgements:
We acknowledge the technical assistance of Drs. Robert Ploutz-Snyder and Marjorie McCullagh in the design of this study.
Funding:
This work was principally supported by the Elizabeth Tone Hosmer Endowed Professorship funds awarded to Dr. Friese. Dr. Friese also received research support from T32-CA-236621 and P30-CA-046592. Drs. Ridge and Titler received research support from T32-NR-016914. The views expressed in this manuscript are solely of the authors and do not represent the views of their employer, the National Cancer Institute, the National Institute of Nursing Research, or the United States Department of Health and Human Services.
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
REFERENCES CITED
- 1.Joo JY, Liu MF. Nurses’ barriers to caring for patients with COVID-19: a qualitative systematic review. Int Nurs Rev [Internet]. 2021. Jun;68(2):202–13. Available from: 10.1111/inr.12648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Plan for health workforce well-being [Internet]. National Academy of Medicine. 2022. [cited 2022 Jun 9]. Available from: https://nam.edu/initiatives/clinician-resilience-and-well-being/national-plan-for-health-workforce-well-being/ [Google Scholar]
- 3.US COVID-19 cases and deaths by state [Internet]. USAFacts. 2022. [cited 2022 Jun 9]. Available from: https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/ [Google Scholar]
- 4.Dillman DA, Smyth JD, Christian LM. Internet, phone, mail, and mixed-mode surveys: the tailored design method. John Wiley & Sons; 2014. [Google Scholar]
- 5.Linzer M, Poplau S. Eliminating burnout and moral injury: Bolder steps required. EClinicalMedicine [Internet]. 2021. Sep;39(101090):101090. Available from: 10.1016/j.eclinm.2021.101090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm [Internet]. 2009. Jul;39(7/8):S45–51. Available from: 10.1097/nna.0b013e3181aeb4cf [DOI] [PubMed] [Google Scholar]
- 7.Action Collaborative on Clinician Well-Being and Resilience, National Academy of Medicine. National plan for health workforce well-being [Internet]. Dzau VJ, Kirch D, Murthy V, Nasca T, editors. Washington, D.C.: National Academies Press; 2022. Available from: 10.17226/26744 [DOI] [Google Scholar]
- 8.Demerouti E, Demerouti E, Bakker AB, Vardakou I, Kantas A. The convergent validity of two burnout instruments. Eur J Psychol Assess [Internet]. 2003. Mar;19(1):12–23. Available from: 10.1027//1015-5759.19.1.12 [DOI] [Google Scholar]
- 9.Westwood S, Morison L, Allt J, Holmes N. Predictors of emotional exhaustion, disengagement and burnout among improving access to psychological therapies (IAPT) practitioners. J Ment Health [Internet]. 2017. Apr;26(2):172–9. Available from: 10.1080/09638237.2016.1276540 [DOI] [PubMed] [Google Scholar]
- 10.Vento S, Cainelli F, Vallone A. Violence against healthcare workers: A worldwide phenomenon with serious consequences. Front Public Health [Internet]. 2020. Sep 18;8:570459. Available from: 10.3389/fpubh.2020.570459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friese CR, Mendelsohn-Victor K, Medvec BR, Ghosh B, Bedard L, Griggs JJ, et al. Factors associated with job satisfaction in medical oncology practices: Results from a multisite survey. J Nurs Adm [Internet]. 2021. Apr 1;51(4):200–5. Available from: 10.1097/NNA.0000000000000998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lake ET. Development of the practice environment scale of the nursing work index. Res Nurs Health [Internet]. 2002. Jun;25(3):176–88. Available from: 10.1002/nur.10032 [DOI] [PubMed] [Google Scholar]
- 13.Lasater KB, Aiken LH, Sloane DM, French R, Martin B, Reneau K, et al. Chronic hospital nurse understaffing meets COVID-19: an observational study. BMJ Qual Saf [Internet]. 2021. Aug;30(8):639–47. Available from: 10.1136/bmjqs-2020-011512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Melnyk BM, Hsieh AP, Tan A, Teall AM, Weberg D, Jun J, et al. Associations among nurses’ mental/physical health, lifestyle behaviors, shift length, and workplace wellness support during COVID-19: Important implications for health care systems. Nurs Adm Q [Internet]. 2022;46(1):5–18. Available from: 10.1097/NAQ.0000000000000499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arnetz JE, Goetz CM, Arnetz BB, Arble E. Nurse reports of stressful situations during the COVID-19 pandemic: Qualitative analysis of survey responses. Int J Environ Res Public Health [Internet]. 2020. Nov 3;17(21):8126. Available from: 10.3390/ijerph17218126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hendrickson RC, Slevin RA, Hoerster KD. The Impact of the COVID-19 Pandemic on Mental Health, Occupational Functioning, and Professional Retention Among Health Care Workers and First Responders. J Gen Intern Med [Internet]. 2022;37(2):397–408. Available from: 10.1007/s11606-021-07252-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stone W. Nurses have had an up-close view of the pandemic deaths in the U.S. NPR; [Internet]. 2022. May 19 [cited 2022 Jun 9]; Available from: https://www.npr.org/2022/05/19/1099997232/nurses-have-had-an-up-close-view-of-the-pandemic-deaths-in-the-u-s [Google Scholar]
- 18.Kovner C, Raveis VH, Van Devanter N, Yu G, Glassman K, Ridge LJ. The psychosocial impact on frontline nurses of caring for patients with COVID-19 during the first wave of the pandemic in New York City. Nurs Outlook [Internet]. 2021. Sep;69(5):744–54. Available from: 10.1016/j.outlook.2021.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trinkoff AM, Selby VL, Han K, Baek H, Steele J, Edwin HS, et al. The prevalence of substance use and substance use problems in registered nurses: Estimates from the nurse worklife and wellness study. J Nurs Regul [Internet]. 2022. Jan;12(4):35–46. Available from: 10.1016/s2155-8256(22)00014-x [DOI] [Google Scholar]
- 20.Smiley RA, Ruttinger C, Oliveira CM, Hudson LR, Allgeyer R, Reneau KA, et al. The 2020 national nursing workforce survey. J Nurs Regul [Internet]. 2021. Apr;12(1):S1–96. Available from: 10.1016/s2155-8256(21)00027-2 [DOI] [Google Scholar]
- 21.Comparison between nurse population & survey respondents from 2021 annual nurse survey [Internet]. [cited 2022 Jun 9]. Available from: https://www.minurse.org/survey/2021/2021-nurse-pop-to-survey-respondent-comparison.html
- 22.Costa DK, Friese CR. Policy strategies for addressing current threats to the U.s. nursing workforce. N Engl J Med [Internet]. 2022. Apr 20; Available from: 10.1056/NEJMp2202662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med [Internet]. 2002. May 30;346(22):1715–22. Available from: 10.1056/NEJMsa012247 [DOI] [PubMed] [Google Scholar]
- 24.Jenkins D, Burton C, Holmes D. Re)defining nursing leadership: On the importance of parrhèsia and subversion. J Nurs Manag [Internet]. 2021; Available from: 10.1111/jonm.13520 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


