Abstract
In many parts of the world nursing home residents have experienced a disproportionate risk of exposure to COVID-19 and have died at much higher rates than other groups. There is a critical need to identify the factors driving COVID-19 risk in nursing homes to better understand and address the conditions contributing to their vulnerability during public health crises. This study investigates the characteristics associated with COVID-19 cases and deaths among residents in U.S. nursing homes from 2020 to 2021, with a focus on geospatial and racial inequalities. Using data from the Centers for Medicare and Medicaid Services and LTCFocus, this paper uses zero-inflated negative binomial regression models, Kruskal-Wallis tests, and Local Moran's I to generate statistical and geospatial results. Our analysis reveals that majority Hispanic facilities have alarmingly high COVID-19 cases and deaths, suggesting that these facilities have the greatest need for policy improvements in staffing and financing to reduce racial inequalities in nursing home care. At the same time we also detect COVID-19 hot spots in rural areas with predominately White residents, indicating a need to rethink public messaging strategies in these areas. The top states with COVID-19 hot spots are Kentucky, Pennsylvania, Illinois, and Oklahoma. This research provides new insights into the socio-spatial contexts and inequities that contribute to the vulnerability of nursing home residents during a pandemic.
Keywords: Nursing Homes, Long-term care, LTC, COVID-19, Racial inequality, Racial disparities, Spatial analysis
1. Introduction
Throughout the COVID-19 pandemic, residents and staff in nursing homes across the world have faced a disproportionate risk of exposure to the disease, revealing major shortcomings in facility conditions that left the people in them susceptible to contracting COVID-19 and dying from it (Mathews et al., 2020). In the U.S. nursing home system, which has been chronically under-resourced and increasingly marketized, residents and staff did not have adequate safeguards to protect themselves against COVID-19 (Ouslander and Grabowski, 2020). Nursing home residents and staff are especially vulnerable because they tend to be older – and if infected, are more likely to experience serious medical complications, require hospitalization, and die (Ouslander and Grabowski, 2020). The results have been devastating. As of June 2021, nearly one-third of COVID-19 deaths have been linked to nursing homes despite representing only 4% of all cases in the U.S. (The New York Times, 2020). This trend is mirrored internationally, where more than one-third of COVID-19 deaths in over two dozen countries are in long-term care facilities (Mathews et al., 2020).
Globally, there is a critical need to identify the factors driving COVID-19 risk in long-term care homes to better understand and address the conditions contributing to their vulnerability during public health crises. In the U.S., higher cases and deaths are associated with larger facility/bed count (Abrams et al., 2020), higher occupancy rate, for-profit status (Wang et al., 2021), lower ratings on staffing levels (Harrington et al., 2020), and lower overall quality ratings (Khairat et al., 2021). This indicates that more crowded facilities have worse working and care conditions, referred to as relational care (Rockwell, 2012; Armstrong and Braedley, 2013), and are vulnerable to COVID-19 outbreaks. Higher COVID-19 risk is also associated with resident characteristics, including a higher proportion of racial/ethnic minority residents (Abrams et al., 2020; Li et al., 2020), greater health deficiencies (Harrington et al., 2020), and more residents whose primary support is Medicaid (Wang et al., 2021). However, results are not uniform across studies. Literature reviews reveal that many of the aforementioned factors have inconsistent correlations with COVID-19 risk in nursing homes (Konetzka et al., 2021; Kruse et al., 2021). Of the factors under study, the most consistent finding is that larger bed count is associated with higher COVID-19 risk (Konetzka et al., 2021).
Racial disparities in the U.S. COVID-19 rates are widely publicized, with racialized minorities experiencing higher infections as they are more likely to be frontline workers and have greater exposure risk (Lee et al., 2022; Skinner-Dorkenoo et al., 2022). While these disparities are well-known among the general population, much less is known about rates among residents of color in nursing homes. Black and Hispanic residents are more likely to be in nursing homes that are understaffed and under-resourced, and to receive fewer services and experience lower quality of life (Fennell et al., 2010; Estrada et al., 2022). Given these conditions, we expect residents of color to receive substandard care during COVID-19 outbreaks and for racial disparities to worsen.
While geography is acknowledged as an important factor in COVID-19 cases and deaths in nursing homes (Gorges and Konetzka, 2020; Konetzka et al., 2021), considerations of geography in most nursing home research is often limited to the use of regression models that include a covariate representing urbanity or rurality, county-level fixed effects, or a random intercept for states (Abrams et al., 2020; Khairat et al., 2021; Yang et al., 2021). While spatial analysis has been utilized to examine COVID-19 outbreaks in general populations across the world (Franch-Pardo et al., 2020), there has been limited spatial analysis focusing on nursing homes. To our knowledge, Sugg et al. (2021) are among the first and only to use spatial analytic techniques to investigate COVID-19 outcomes in nursing homes. They applied a hot spot analysis of cumulative COVID-19 cases and deaths, and in doing so identified significant hot spots in specific regions of the U.S. as of June 2020 (Sugg et al., 2021).
Our study builds on the extant research by generating updated population-level patterns and conducting a more detailed analysis of geospatial clusters to better understand the spatial and racial inequalities of COVID-19 risk across nursing homes. Additionally, our work contributes to aging research on vulnerability, where vulnerability is understood as comprising multiple and intersecting material, social, physiological, and psychological challenges that influence older adults’ well-being (Shin et al., 2021; Levasseur et al., 2022). However, geography is often overlooked. In a scoping review of vulnerability definitions and measurements in older adults, space was only considered in one article and it referred to the home environment (Levasseur et al., 2022). In our study, we consider geography at multiple scales (neighborhood, county, state) and its relationship to COVID-19 risk and vulnerability among nursing home residents. By drawing attention to social and geographic inequalities, we expand on predominant understandings of vulnerability that emphasize individual factors.
Our overarching research question is: What geospatial and racial characteristics are correlated with COVID-19 cases and deaths in nursing homes, and where are clusters of COVID-19 risk? This research provides new insights into the socio-spatial contexts contributing to COVID-19 risk (i.e., cases and deaths) among residents. In particular, we consider how the racial/ethnic distribution of residents (specifically, majority White, Black, and Hispanic nursing homes) influences COVID-19 trends, as racial segregation in nursing homes stems from structural racism, reflects residential segregation patterns in local communities, and results in disparities in care and inequitable health outcomes (Smith et al., 2007; Sloane et al., 2021). We follow Bailey et al. (2017) in understanding structural racism as, “the totality of ways in which societies foster racial discrimination through mutually reinforcing systems of housing, education, employment, earnings, benefits, credit, media, health care, and criminal justice, and that this is likely a ‘fundamental cause’ of health disparities” (Tan, deSouza and Raifman, 2022; citing Phelan and Link, 2015). While the focus of this paper is to identify COVID-19 disparities by race/ethnicity, we also recognize that these inequities derive from the multi-faceted presence of structural racism in these aforementioned areas.
2. Materials and methods
2.1. Study setting
The continental U.S. has 15,000 nursing homes with over one million residents (National Center for Health Statistics, 2022). Regulated by both federal and state laws, most nursing homes are privately owned and operated, whether via faith-based, philanthropic, non-profit, for-profit organizations, or a mix. As of 2016, almost 70% of nursing homes reported for-profit ownership structures (ibid), however, most of the sector's revenues stem from public sources (Giacalone, 2015), creating a scenario in which federal and state governments depend upon a largely for-profit industry to for care of older adults and provide transparency in reporting funding needs and working and caring conditions. Recently, the sector has experienced deepening processes of marketization, including changes in corporate ownership structure, costs priorities (e.g., a deprioritization of labor remuneration), and quality of services provided (Harrington et al., 2017; Ponder et al., 2021). The increasing ownership of nursing home facilities by private equity in particular, has raised alarm bells in terms of public transparency, cost controls, and quality of care (Harrington et al., 2017; Horton, 2021, 2022).
2.2. Data
Nursing home data were obtained from the Centers for Medicare and Medicaid Services (CMS) and from LTCFocus, a data repository sponsored by the National Institute on Aging (1P01AG027296) through a cooperative agreement with the Brown University School of Public Health. We obtained CMS data last updated in January 2022 on total COVID-19 cases and deaths among residents and staff since the start of the pandemic, vaccination rates among residents and staff, facility ownership type, bed count, occupancy rate, staffing hours per resident day, overall rating (from a scale of 1–5, with 1 being low and 5 being high), reported incidents and complaints, fines, and citations from infection control inspections. From LTCFocus, we included facility data on acute care hospital admissions, Activities of Daily Living (ADL) score, hospitalizations per resident year; and resident data on sex, race/ethnicity (Black, Hispanic, and White), age, and patient days that were private pay. LTCFocus data were dated in the year 2020, except for patient days that were private pay which was in 2015. These were the most recent data available at the time of analysis.
From the Department of Agriculture, we downloaded the 2010 Rural-Urban Commuting Area (RUCA) codes that categorize census tracts as metropolitan, micropolitan, or rural. As proxies for neighborhoods, census tracts are commonly used to represent residential contexts and characteristics. This was the most recent data available categorizing census tracts across the urban to rural continuum.
3. Methods
3.1. Data processing
With CMS data, we included facilities that passed the Quality Assurance process (n = 14,946). We merged the CMS and LTCFocus datasets by CMS provider number, dropping facilities that did not match. Finally, we spatially joined the datasets with tract and county shapefiles using the facilities’ latitude and longitude. We excluded facilities outside the continental U.S. as our cluster analysis relies on polygon contiguity.
3.2. Statistical analysis
Using RStudio (R Core Team, 2021) and the pscl package, we produced two zero-inflated negative binomial (ZINB) regression models (Jackman et al., 2020). For each model, the dependent variable was total nursing home resident deaths and cases, respectively. We applied the Variance Inflation Factor (VIF) to test for multicollinearity between independent variables (Faraway, 2016) and excluded variables with a VIF>5. Our final models included the following numeric covariates: staff cases, staff deaths, bed size, vaccination rates among residents and staff, average number of residents per day, acute care hospital admissions, average age of residents, hospitalizations per resident year, average ADL score, % female, % private pay patient days, adjusted total nurse staffing hours per resident per day, and number of fines, incidents, complaints, and citations. The models also included the following categorical variables: overall rating, ownership type, race/ethnicity, RUCA, and the state that the facility is located in. We removed facilities with missing and/or NA values, leaving 11,690 facilities in the final models.
We utilized ZINB regression models due to numerous zeroes and overdispersion (i.e., the variance is greater than the mean) in the data (Karim and Chen, 2021). The data were highly right skewed with approximately 9% (1088 out of 11,690) of facilities having 0 deaths and 0.9% (n = 108) with 0 cases. Not accounting for excess zeroes in count data can result in inaccurately calculated regression coefficients and bias results. Additionally, ZINB allows us to consider two processes that may be occurring in nursing homes: attributes associated with the presence of cases and deaths via negative binomial regression, and factors associated with zero cases and deaths via logistic regression. Zero cases and deaths may suggest early, successful interventions (Khedhiri, 2021) such as effective infection-control procedures and safe working conditions. To test this, we included total staff cases and deaths in the logistic model, as fewer infections and deaths among staff are likely to lead to lower exposure and cross-infection rates between residents and staff. For the ZINB model with total resident deaths as the outcome variable, we also included total resident cases in both the negative binomial and logistic models (Karim and Chen, 2021), as COVID-19 infections influence death rates.
3.21. Comparative analysis by race/ethnicity
We categorized facilities as majority (≥51%) White, Black, or Hispanic. If facilities did not meet the 51% threshold, they were categorized as “Other” race/ethnicity as no other racial/ethnic data were collected. We are interested in how structural racism is linked to care conditions and COVID-19 outcomes in nursing homes, and seek to gain insight into the patterns and outcomes related to this process by examining the racial characteristics of residents alongside facility qualities. As majority Black and Hispanic resident facilities comprise a small proportion of the data (4.7% and 0.4%, respectively), we opted for a more descriptive analysis and used Kruskal-Wallis tests to test the equality of distribution between groups.
3.3. Cluster analysis
To detect statistically significant clusters of cases and deaths per 1000 residents, we used GeoDa to generate univariate Local Moran's I (Anselin, 2010). Spatial relationships were defined by Queen contiguity. We identified hot and cold spots of median case and death rates within counties (n = 2801). We considered examining clusters at the tract level, but most tracts had no facilities, resulting in insufficient spatial contiguity for cluster analysis. Thus, we aggregated and summarized facility data by county. Then, we used Kruskal-Wallis tests to compare the distribution of our variables between different cluster types.
4. Results
4.1. Population-level trends of COVID-19 risk
The mean total resident cases is 56 and mean total deaths is 10. The minimum number of cases and deaths is 0, and the maximum cases is 428 while the maximum deaths is 138. Table 1 presents the descriptive statistics for all the resident, staff, and facility variables. On average, 89% of residents and 84% of staff are vaccinated. Most facilities are for-profit (72%) and majority White (89%). Table 2 describes the descriptive statistics of the geographic variables: facilities located in metropolitan, micropolitan, and rural tracts, as well as state locations. Most facilities are in metropolitan tracts (68%). The states with the most facilities are Texas (7%), California (6.9%), and Ohio (6.5%).
Table 1.
Summary statistics for resident, staff, and facility variables (n = 11,690).
| Variable | Mean | Median | SD |
|---|---|---|---|
| Total Resident Cases | 55.6 | 49 | 38.9 |
| Total Resident Deaths | 10.4 | 8 | 11.2 |
| Total Staff Cases | 53.2 | 47 | 32.6 |
| Total Staff Deaths | 0.15 | 0 | 0.65 |
| Total Beds | 112 | 104 | 57 |
| % Residents Vaccinated | 89.1 | 91.1 | 9.1 |
| % Staff Vaccinated | 84.2 | 87.8 | 14.8 |
| Average Residents Per Day | 80.6 | 72.9 | 45.6 |
| % Admissions from Acute Care Hospital | 84.7 | 87.9 | 12.4 |
| Average Age of Residents | 78.9 | 79.4 | 6.1 |
| % Hospitalizations Per Resident Year | 1.33 | 1.22 | 0.66 |
| ADL Score | 17.2 | 17.3 | 1.9 |
| % Female Residents | 57.9 | 58.7 | 10.0 |
| % Patient Days Private Pay | 17.2 | 12.4 | 15.1 |
| Adjusted Nurse Staffing Hours PRPR | 3.67 | 3.58 | 0.85 |
| Number of Fines | 1.5 | 1 | 2.2 |
| Number of Incidents | 1.5 | 0 | 3.5 |
| Number of Complaints | 4.7 | 2 | 8.7 |
| Number of Citations | 1.3 | 1 | 2.3 |
|
% |
n |
||
| Ownership Type | |||
| For-profit | 72.5 | 8473 | |
| Non-profit | 22.6 | 2645 | |
| Government | 4.9 | 572 | |
| Race/Ethnicity | |||
| Majority White | 89.0 | 10,402 | |
| Majority Black | 4.8 | 561 | |
| Majority Hispanic | 0.5 | 58 | |
| Other Race/Ethnicity | 5.7 | 669 | |
| Overall Rating | |||
| 1-Star | 16.5 | 1926 | |
| 2-Stars | 20.7 | 2425 | |
| 3-Stars | 19.4 | 2263 | |
| 4-Stars | 22.1 | 2587 | |
| 5-Stars | 21.3 | 2489 | |
ADL = Activities of Daily Living; PRPR = Per Resident Per Day.
Table 2.
Summary statistics for geographic variables (n = 11,690).
| Variable Type | Variable | % | n |
|---|---|---|---|
| RUCA | Metropolitan | 68.30 | 7984 |
| (Rural-Urban | Micropolitan | 14.71 | 1720 |
|
Commuting Area) |
Rural |
16.99 |
1986 |
| State | TX | 7.01 | 820 |
| CA | 6.92 | 809 | |
| OH | 6.54 | 764 | |
| FL | 5.12 | 598 | |
| PA | 5.04 | 589 | |
| IL | 4.97 | 581 | |
| NY | 4.47 | 522 | |
| IN | 3.54 | 414 | |
| MO | 3.35 | 392 | |
| NC | 2.94 | 344 | |
| MI | 2.80 | 327 | |
| MA | 2.79 | 326 | |
| IA | 2.75 | 322 | |
| GA | 2.54 | 297 | |
| WI | 2.50 | 292 | |
| NJ | 2.44 | 285 | |
| TN | 2.30 | 269 | |
| MN | 2.20 | 257 | |
| KY | 2.04 | 239 | |
| LA | 1.93 | 226 | |
| OK | 1.82 | 213 | |
| VA | 1.82 | 213 | |
| KS | 1.80 | 211 | |
| MD | 1.59 | 186 | |
| CT | 1.53 | 179 | |
| AR | 1.51 | 177 | |
| WA | 1.46 | 171 | |
| AL | 1.45 | 170 | |
| SC | 1.32 | 154 | |
| MS | 1.29 | 151 | |
| CO | 1.19 | 139 | |
| NE | 1.11 | 130 | |
| AZ | 0.92 | 107 | |
| WV | 0.88 | 103 | |
| OR | 0.78 | 91 | |
| ME | 0.58 | 68 | |
| RI | 0.56 | 66 | |
| NH | 0.55 | 64 | |
| SD | 0.54 | 63 | |
| UT | 0.54 | 63 | |
| ND | 0.47 | 55 | |
| ID | 0.40 | 47 | |
| MT | 0.33 | 39 | |
| NM | 0.33 | 39 | |
| NV | 0.33 | 39 | |
| DE | 0.30 | 35 | |
| VT | 0.21 | 25 | |
| WY | 0.16 | 19 |
Table 3, Table 4 report the beta coefficients and p-values for the ZINB models for cases and deaths, respectively. Incidence rate ratios (IRR) are included for the negative binomial results, and odds ratios (OR) are included for the logistic regression results. The results demonstrate the impact of COVID-19 risk factor on resident cases and deaths when controlling for the other factors included in the analysis. These are factors associated with residents’ COVID-19 vulnerability. To complement the material, social, and physiological factors that are commonly investigated in vulnerability research on older adults (Shin et al., 2021; Levasseur et al., 2022), the models also include geographic attributes (i.e., tracts and states).
Table 3.
ZINB regression model results with total resident cases as the outcome variable.
| Variable | Estimate | 95% CI | IRR/OR | P-Value |
|---|---|---|---|---|
| Negative binomial model: | ||||
| (Intercept) | 3.813 | (3.583, 4.0423) | 45.286 | <0.001 |
| Total Staff Cases | 0.012 | (0.011, 0.012) | 1.012 | <0.001 |
| Total Staff Deaths | 0.011 | (-0.004, 0.026) | 1.011 | 0.152 |
| Total Beds | 0.0003 | (-0.00009, 0.0007) | 1.000 | 0.122 |
| % Residents Vaccinated | −0.003 | (-0.004, −0.002) | 0.997 | <0.001 |
| % Staff Vaccinated | 0.0003 | (-0.0005, 0.001) | 1.000 | 0.455 |
| Average Residents Per Day | 0.001 | (-0.004, −0.002) | 1.001 | <0.001 |
| % Admissions from Acute Care Hospital | 0.0001 | (0.001, 0.002) | 1.000 | 0.699 |
| Average Age of Residents | 0.005 | (-0.0007, 0.001) | 1.005 | <0.001 |
| % Hospitalizations Per Resident Year | 0.021 | (0.001, 0.04) | 1.021 | 0.031 |
| ADL Score | −0.002 | (-0.009, 0.003) | 0.998 | 0.444 |
| % Female Residents | −0.002 | (-0.003, −0.0007) | 0.998 | 0.002 |
| % Patient Days Private Pay | −0.005 | (-0.006, −0.004) | 0.995 | <0.001 |
| Adjusted Nurse Staffing Hours PRPR | −0.144 | (-0.16, −0.128) | 0.866 | <0.001 |
| Number of Fines | −0.001 | (-0.006, 0.003) | 0.999 | 0.603 |
| Number of Incidents | 0.002 | (-0.0009, 0.005) | 1.002 | 0.157 |
| Number of Complaints | 0.001 | (-0.0002, 0.002) | 1.001 | 0.096 |
| Number of Citations | 0.015 | (0.01, 0.02) | 1.015 | <0.001 |
| Overall Rating: 1-Star | Reference | |||
| Overall Rating: 2-Stars | 0.015 | (-0.017, 0.048) | 1.015 | 0.36 |
| Overall Rating: 3-Stars | −0.01 | (-0.046, 0.024) | 0.990 | 0.53 |
| Overall Rating: 4-Stars | −0.013 | (-0.049, 0.022) | 0.987 | 0.46 |
| Overall Rating: 5-Stars | −0.068 | (-0.107, −0.028) | 0.934 | <0.001 |
| Ownership Type: For Profit | Reference | |||
| Ownership Type: Government | −0.114 | (-0.163, −0.065) | 0.892 | <0.001 |
| Ownership Type: Non-Profit | −0.15 | (-0.178, −0.123) | 0.861 | <0.001 |
| Majority White Residents | Reference | |||
| Majority Black Residents | −0.14 | (-0.189, −0.091) | 0.869 | <0.001 |
| Majority Hispanic Residents | −0.105 | (-0.244, 0.033) | 0.900 | 0.138 |
| Other Race/Ethnicity Residents | −0.126 | (-0.172, −0.080) | 0.882 | <0.001 |
| Metropolitan Census Tract | Reference | |||
| Micropolitan Census Tract | 0.001 | (-0.028, 0.031) | 1.001 | 0.909 |
| Rural Census Tract | −0.049 | (-0.079, −0.018) | 0.952 | 0.001 |
| State: PA | Reference | |||
| State: AL | 0.036 | (-0.054, 0.128) | 1.037 | 0.429 |
| State: AR | 0.081 | (-0.01, 0.173) | 1.084 | 0.082 |
| State: AZ | −0.051 | (-0.163, 0.060) | 0.950 | 0.367 |
| State: CA | −0.019 | (-0.083, 0.043) | 0.981 | 0.536 |
| State: CO | −0.21 | (-0.311, −0.109) | 0.811 | <0.001 |
| State: CT | 0.024 | (-0.065, 0.115) | 1.024 | 0.59 |
| State: DE | −0.029 | (-0.210, 0.150) | 0.971 | 0.744 |
| State: FL | −0.21 | (-0.273, −0.146) | 0.811 | <0.001 |
| State: GA | 0.032 | (-0.042, 0.108) | 1.033 | 0.391 |
| State: IA | −0.024 | (-0.103, 0.054) | 0.976 | 0.542 |
| State: ID | −0.298 | (-0.46, −0.137) | 0.742 | <0.001 |
| State: IL | −0.068 | (-0.132, −0.005) | 0.934 | 0.033 |
| State: IN | −0.004 | (-0.111, 0.027) | 0.996 | 0.233 |
| State: KS | −0.085 | (-0.173, 0.003) | 0.919 | 0.058 |
| State: KY | −0.004 | (-0.085, 0.076) | 0.996 | 0.915 |
| State: LA | −0.149 | (-0.232, −0.065) | 0.862 | <0.001 |
| State: MA | −0.072 | (-0.147, 0.001) | 0.931 | 0.054 |
| State: MD | −0.163 | (-0.253, −0.074) | 0.850 | <0.001 |
| State: ME | −0.126 | (-0.267, 0.013) | 0.882 | 0.077 |
| State: MI | −0.363 | (-0.442, −0.285) | 0.696 | <0.001 |
| State: MN | −0.353 | (-0.436, −0.27) | 0.703 | <0.001 |
| State: MO | 0.038 | (-0.033, 0.11) | 1.039 | 0.289 |
| State: MS | 0.016 | (-0.081, 0.113) | 1.016 | 0.747 |
| State: MT | −0.153 | (-0.33, 0.024) | 0.858 | 0.091 |
| State: NC | −0.018 | (-0.089, 0.052) | 0.982 | 0.612 |
| State: ND | −0.249 | (-0.401, −0.097) | 0.780 | 0.001 |
| State: NE | −0.174 | (-0.279, −0.069) | 0.840 | 0.001 |
| State: NH | −0.012 | (-0.15, 0.126) | 0.988 | 0.864 |
| State: NJ | 0.003 | (-0.072, 0.08) | 1.003 | 0.92 |
| State: NM | −0.144 | (-0.317, 0.028) | 0.866 | 0.101 |
| State: NV | −0.078 | (-0.251, 0.095) | 0.925 | 0.376 |
| State: NY | −0.446 | (-0.511, −0.380) | 0.640 | <0.001 |
| State: OH | −0.148 | (-0.207, −0.089) | 0.862 | <0.001 |
| State: OK | 0.045 | (-0.043, 0.133) | 1.046 | 0.314 |
| State: OR | −0.403 | (-0.529, −0.277) | 0.668 | <0.001 |
| State: RI | −0.09 | (-0.226, 0.045) | 0.914 | 0.193 |
| State: SC | 0.005 | (-0.09, 0.101) | 1.005 | 0.909 |
| State: SD | −0.08 | (-0.223, 0.062) | 0.923 | 0.269 |
| State: TN | −0.103 | (-0.18, −0.025) | 0.902 | 0.009 |
| State: TX | −0.006 | (-0.068, 0.054) | 0.994 | 0.827 |
| State: UT | −0.216 | (-0.36, −0.073) | 0.806 | 0.003 |
| State: VA | 0.073 | (-0.01, 0.156) | 1.076 | 0.087 |
| State: VT | −0.575 | (-0.806, −0.345) | 0.563 | <0.001 |
| State: WA | −0.233 | (-0.33, −0.136) | 0.792 | <0.001 |
| State: WI | −0.467 | (-0.544, −0.39) | 0.627 | <0.001 |
| State: WV | −0.04 | (-0.153, 0.072) | 0.961 | 0.486 |
| State: WY | −0.206 | (-0.45, 0.037) | 0.814 | 0.096 |
| Logistic model: | ||||
| Total Staff Cases | −0.193 | (-0.222, −0.164) | 0.824 | <0.001 |
| Total Staff Deaths | 0.114 | (-0.279, 0.509) | 1.121 | 0.568 |
IRR=Incidence Rate Ratio; OR=Odds Ratio; ADL = Activities of Daily Living, PRPR=Per Resident Per Day.
Table 4.
ZINB regression model results with total resident deaths as the outcome variable.
| Variable | Estimate | 95% CI | IRR/OR | P-Value |
|---|---|---|---|---|
| Negative binomial model: | ||||
| (Intercept) | 0.184 | (-0.137, 0.506) | 1.202 | 0.26 |
| Total Resident Cases | 0.011 | (0.010, 0.011) | 1.011 | <0.001 |
| Total Staff Cases | 0.003 | (0.002, 0.004) | 1.003 | <0.001 |
| Total Staff Deaths | 0.071 | (0.050, 0.092) | 1.074 | <0.001 |
| Total Beds | 0.002 | (0.001, 0.003) | 1.002 | <0.001 |
| % Residents Vaccinated | −0.002 | (-0.004, −0.001) | 0.998 | <0.001 |
| % Staff Vaccinated | 0.0004 | (-0.0006, 0.001) | 1.000 | 0.433 |
| Average Residents Per Day | −0.003 | (-0.004, −0.002) | 0.997 | <0.001 |
| % Admissions from Acute Care Hospital | −0.006 | (-0.008, −0.005) | 0.994 | <0.001 |
| Average Age of Residents | 0.0253 | (0.021, 0.029) | 1.026 | <0.001 |
| % Hospitalizations Per Resident Year | 0.066 | (0.038, 0.093) | 1.068 | <0.001 |
| ADL Score | 0.029 | (0.020, 0.038) | 1.029 | <0.001 |
| % Female Residents | −0.003 | (-0.005, −0.001) | 0.997 | <0.001 |
| % Patient Days Private Pay | −0.001 | (-0.003, −0.0003) | 0.999 | 0.012 |
| Adjusted Nurse Staffing Hours PRPR | −0.065 | (-0.087, −0.042) | 0.937 | <0.001 |
| Number of Fines | 0.015 | (0.007, 0.023) | 1.015 | <0.001 |
| Number of Incidents | 0.001 | (-0.002, 0.006) | 1.001 | 0.403 |
| Number of Complaints | 0.003 | (0.001, 0.005) | 1.003 | <0.001 |
| Number of Citations | −0.0001 | (-0.0067, 0.0064) | 1.000 | 0.964 |
| Overall Rating: 1-Star | Reference | |||
| Overall Rating: 2-Stars | 0.042 | (-0.003, 0.087) | 1.043 | 0.069 |
| Overall Rating: 3-Stars | 0.047 | (-0.001, 0.096) | 1.048 | 0.057 |
| Overall Rating: 4-Stars | 0.016 | (-0.033, 0.067) | 1.016 | 0.519 |
| Overall Rating: 5-Stars | −0.005 | (-0.061, 0.049) | 0.995 | 0.837 |
| Ownership Type: For Profit | Reference | |||
| Ownership Type: Government | −0.022 | (-0.091, 0.046) | 0.978 | 0.516 |
| Ownership Type: Non-Profit | −0.009 | (-0.048, 0.030) | 0.991 | 0.65 |
| Majority White Residents | Reference | |||
| Majority Black Residents | −0.054 | (-0.122, 0.014) | 0.947 | 0.12 |
| Majority Hispanic Residents | 0.315 | (0.131, 0.498) | 1.370 | <0.001 |
| Other Race/Ethnicity Residents | 0.063 | (-0.0003, 0.128) | 1.065 | 0.051 |
| Metropolitan Census Tract | Reference | |||
| Micropolitan Census Tract | 0.015 | (-0.026, 0.057) | 1.015 | 0.474 |
| Rural Census Tract | −0.06 | (-0.1039, −0.016) | 0.942 | <0.001 |
| State: PA | Reference | |||
| State: AL | −0.194 | (-0.319, −0.069) | 0.824 | 0.002 |
| State: AR | −0.137 | (-0.264, −0.01) | 0.872 | 0.034 |
| State: AZ | −0.164 | (-0.318, −0.01) | 0.849 | 0.036 |
| State: CA | −0.382 | (-0.470, −0.294) | 0.682 | <0.001 |
| State: CO | 0.039 | (-0.099, 0.177) | 1.040 | 0.579 |
| State: CT | 0.134 | (0.012, 0.256) | 1.143 | 0.03 |
| State: DE | −0.083 | (-0.329, 0.161) | 0.920 | 0.502 |
| State: FL | −0.509 | (-0.598, −0.42) | 0.601 | <0.001 |
| State: GA | −0.202 | (-0.305, −0.098) | 0.817 | <0.001 |
| State: IA | −0.148 | (-0.258, −0.038) | 0.862 | 0.008 |
| State: ID | −0.479 | (-0.721, −0.236) | 0.619 | <0.001 |
| State: IL | −0.187 | (-0.273, −0.101) | 0.829 | <0.001 |
| State: IN | −0.055 | (-0.149, 0.038) | 0.946 | 0.248 |
| State: KS | −0.162 | (-0.286, −0.038) | 0.850 | 0.01 |
| State: KY | −0.243 | (-0.354, −0.131) | 0.784 | <0.001 |
| State: LA | −0.014 | (-0.128, 0.098) | 0.986 | 0.795 |
| State: MA | 0.177 | (0.077, 0.277) | 1.194 | <0.001 |
| State: MD | −0.17 | (-0.293, −0.048) | 0.844 | 0.006 |
| State: ME | −0.231 | (-0.448, −0.014) | 0.794 | 0.036 |
| State: MI | −0.042 | (-0.15, 0.066) | 0.959 | 0.443 |
| State: MN | −0.083 | (-0.2, 0.033) | 0.920 | 0.164 |
| State: MO | −0.285 | (-0.385, −0.184) | 0.752 | <0.001 |
| State: MS | −0.133 | (-0.266, −0.0007) | 0.875 | 0.048 |
| State: MT | −0.011 | (-0.257, 0.234) | 0.989 | 0.92 |
| State: NC | −0.186 | (-0.283, −0.088) | 0.830 | <0.001 |
| State: ND | −0.103 | (-0.314, 0.108) | 0.902 | 0.34 |
| State: NE | −0.307 | (-0.461, −0.153) | 0.736 | <0.001 |
| State: NH | −0.112 | (-0.316, 0.092) | 0.894 | 0.282 |
| State: NJ | 0.06 | (-0.041, 0.162) | 1.062 | 0.248 |
| State: NM | −0.536 | (-0.795, −0.277) | 0.585 | <0.001 |
| State: NV | −0.314 | (-0.553, −0.076) | 0.731 | 0.009 |
| State: NY | −0.133 | (-0.224, −0.042) | 0.875 | 0.003 |
| State: OH | −0.19 | (-0.271, −0.110) | 0.827 | <0.001 |
| State: OK | −0.139 | (-0.262, −0.016) | 0.870 | 0.026 |
| State: OR | 0.058 | (-0.138, 0.254) | 1.060 | 0.56 |
| State: RI | −0.083 | (-0.27, 0.103) | 0.920 | 0.381 |
| State: SC | −0.253 | (-0.386, −0.12) | 0.776 | <0.001 |
| State: SD | 0.024 | (-0.168, 0.216) | 1.024 | 0.805 |
| State: TN | −0.22 | (-0.326, −0.114) | 0.803 | <0.001 |
| State: TX | −0.388 | (-0.474, −0.303) | 0.678 | <0.001 |
| State: UT | −0.14 | (-0.356, 0.075) | 0.869 | 0.02 |
| State: VA | −0.219 | (-0.335, −0.103) | 0.803 | <0.001 |
| State: VT | −0.25 | (-0.662, 0.161) | 0.779 | 0.233 |
| State: WA | −0.141 | (-0.282, −0.001) | 0.868 | 0.048 |
| State: WI | −0.327 | (-0.437, −0.217) | 0.721 | <0.001 |
| State: WV | −0.275 | (-0.433, −0.118) | 0.760 | <0.001 |
| State: WY | −0.213 | (-0.55, 0.123) | 0.808 | 0.213 |
| Logistic model: | ||||
| Total Resident Cases | −0.176 | (-0.201, −0.151) | 0.839 | <0.001 |
| Total Staff Cases | −0.013 | (-0.021, −0.005) | 0.987 | 0.001 |
| Total Staff Deaths | 0.123 | (-0.121, 0.368) | 1.131 | 0.322 |
IRR=Incidence Rate Ratio; OR=Odds Ratio; ADL = Activities of Daily Living, PRPR=Per Resident Per Day.
There are similar results between the models with cases (Table 3) and deaths (Table 4) as the outcome. For both models, multiple resident, staff, and facility characteristics are statistically significant (p ≤ 0.05). Total staff cases, average age of residents, and % hospitalizations per resident year have a positive association with total resident cases and deaths; while % residents vaccinated, % female residents, % patient days that were private pay, and adjusted nurse staffing hours per resident per day have a negative association. In other words, facilities with wealthier and younger residents, and greater financial resources to pay for more staff hours have fewer cases and deaths. As for the logistic regression model, with every one unit increase in total staff cases, the odds of 0 resident cases decrease by 0.82 and the odds of 0 resident deaths decrease by 0.99. In other words, the odds of 0 resident cases and deaths decrease with an increase in staff cases. These findings contribute additional evidence to previous research, which have found inconsistent correlations with COVID-19 risk in nursing homes (Konetzka et al., 2021; Kruse et al., 2021).
There are a few notable differences in results between the models by bed count, ownership type, and residents' racial/ethnic demographics. With cases as the outcome, total bed count is not statistically significant (Table 3). In contrast, with deaths (Table 4), total bed count is positively and statistically significant (p < 0.001). These findings are both consistent and inconsistent with previous research that have found larger bed count to be associated with greater COVID-19 risk (Konetzka et al., 2021; Kruse et al., 2021). Previous studies measured COVID-19 risk as the probability of at least one case or death, or cumulative case counts or rates, and most studies focused on a single or multiple states (Konetzka et al., 2021; Kruse et al., 2021) whereas our study is at the national scale. Government and non-profit facilities have significantly lower cases (p < 0.001) than for-profit facilities (Table 3). While government and non-profit facilities also have fewer deaths than for-profit facilities, the differences are not statistically significant (Table 4). There are mixed findings on the association between ownership and COVID-19 outcomes; underlying factors such as facility size, staffing hours, and contextual factors may mediate this relationship (Kruse et al., 2021). As for residents’ race/ethnicity, compared to majority White facilities, majority Black and Other race/ethnicity have lower cases (p < 0.001) (Table 3). The cases are not significantly different for majority Hispanic facilities (Table 3). As for deaths, majority Hispanic and Other race/ethnicity facilities have higher deaths compared to majority White facilities (p ≤ 0.05) (Table 4), while deaths in majority Black facilities are not significantly different (Table 4).
The ZINB model with deaths as the outcome included total resident cases as a predictor variable in both the negative binomial and logistic models (Table 4). For every one unit increase in resident cases, resident deaths increase by 1.1% (p < 0.001). The logistic regression model also shows that an increase in resident cases results in a 16.1% decrease in zero counts (p < 0.001). In other words, the more resident cases, the more likely a facility will experience resident deaths.
In both logistic models (Table 3, Table 4), increases in staff cases result in a 17.6% decrease in zero resident cases and a 1.3% decrease in zero resident deaths (p ≤ 0.001) (i.e., more staff cases are associated with a higher likelihood of resident cases and deaths). Staff deaths are not statistically significant. These findings suggest that a reduction in staff COVID-19 infections via mitigation measures and safe working and caring conditions are needed to reduce residents’ vulnerability to COVID-19.
Geographically, rural nursing homes have lower cases and deaths (p ≤ 0.001) than those in metropolitan areas while those in micropolitan areas are not significantly different. This aligns with previous research that found rural regions to have lower COVID-19 risk than urban areas (Yang et al., 2021), while also revealing that areas in the middle of the rural-urban continuum may not have considerably different experiences from urban sites. In our models, all states are compared to Pennsylvania, which has the highest cumulative cases and deaths. Eighteen states have significantly lower cases (p < 0.05): Colorado, Florida, Idaho, Illinois, Louisiana, Maryland, Michigan, Minnesota, North Dakota, Nebraska, New York, Ohio, Oregon, Tennessee, Utah, Vermont, Washington, and Wisconsin. Thirty states have lower deaths (p < 0.05): Alabama, Arkansas, Arizona, California, Florida, Georgia, Iowa, Idaho, Illinois, Kansas, Maryland, Maine, Missouri, Mississippi, North Carolina, Nebraska, New Mexico, Nevada, New York, Ohio, Oklahoma, South Carolina, Tennessee, Texas, Utah, Virginia, Washington, Wisconsin, and West Virginia. Of these states, New Mexico has the lowest deaths – 41.5% lower than Pennsylvania. Connecticut and Massachusetts have significantly (p < 0.05) higher deaths: 14.3% and 19.4%, respectively. These findings indicate that urban location and state-level policies are important contextual factors contributing to the residents’ vulnerability during the pandemic. These include state directives related to COVID-19 testing and vaccination, visitation restrictions, and the provision of personal protective equipment (PPE) (Chen et al., 2020).
4.2. Racial disparities between facilities
Table 5 summarizes the median resident, staff, and facility characteristics for majority White, Black, Hispanic, and Other race/ethnicity facilities; as well as their geographic contexts. For all attributes, the Kruskal-Wallis tests indicate that the population median of one group is significantly different from at least one other group.
Table 5.
Facility characteristics by residents’ race/ethnicity.
| Variable | Majority White (n = 11,586) | Majority Black (n = 616) | Majority Hispanic (n = 58) | Other (n = 709) | P-Valuea |
|---|---|---|---|---|---|
| Total Resident Cases (median) | 46 | 55 | 58 | 55 | <0.001 |
| Total Resident Deaths (median) | 7 | 7 | 11.5 | 7 | <0.001 |
| Total Staff Cases (median) | 45 | 50 | 51 | 49 | <0.001 |
| Total Staff Deaths (median) | 0 | 0 | 0 | 0 | <0.001 |
| % Residents Vaccinated (median) | 92 | 87 | 91 | 89 | <0.001 |
| % Staff Vaccinated (median) | 87 | 91 | 94 | 96 | <0.001 |
| Total Beds (median) | 99 | 120 | 120 | 120 | <0.001 |
| Average Residents Per Day (median) | 68 | 91 | 86 | 91 | <0.001 |
| % Admissions from Acute Care Hospital (median) | 87 | 92 | 89 | 93 | <0.001 |
| Average Age of Residents (median) | 80 | 73 | 79 | 75 | <0.001 |
| % Hospitalizations Per Resident Year (median) | 1.16 | 1.61 | 1.53 | 1.68 | <0.001 |
| Average Activities of Daily Living (ADL) Score (median) | 17.1 | 18.2 | 19.6 | 18.5 | <0.001 |
| % Female Residents (median) | 60 | 50 | 53 | 50 | <0.001 |
| % Patient Days Private Pay (median) | 14 | 6 | 9 | 6 | <0.001 |
| Adjusted Nurse Staffing Hours Per Resident Per Day (median) | 3.64 | 3.29 | 3.26 | 3.61 | <0.001 |
| Number of Fines (median) | 1 | 1 | 1 | 1 | <0.001 |
| Number of Incidents (median) | 0 | 0 | 0 | 1 | <0.001 |
| Number of Complaints (median) | 1 | 4 | 1.5 | 4 | <0.001 |
| Number of Citations (median) | 1 | 1 | 1 | 1 | <0.001 |
| Overall Rating, 1–5 (mode) | 5 | 1 | 2 | 2 | |
| Ownership Type (mode) | For Profit | For Profit | For Profit | For Profit | |
| RUCA (mode) | Metropolitan | Metropolitan | Metropolitan | Metropolitan | |
| States (n) | 48 | 27 | 7 | 41 |
P-Value for Kruskal-Wallis Test.
Cases and deaths are lowest among majority White facilities, which are located in every state and in mainly metropolitan areas. Total resident cases and deaths are 46 and 7, respectively; and total staff cases is 45 (Table 5). These facilities have the fewest total beds, average residents per day (calculated using resident census data and averaging by day), percent hospitalizations per resident year, and number of complaints; and the highest vaccination rate among residents, percent patient days that were private pay, adjusted nurse staffing hours per resident day, and highest overall rating.
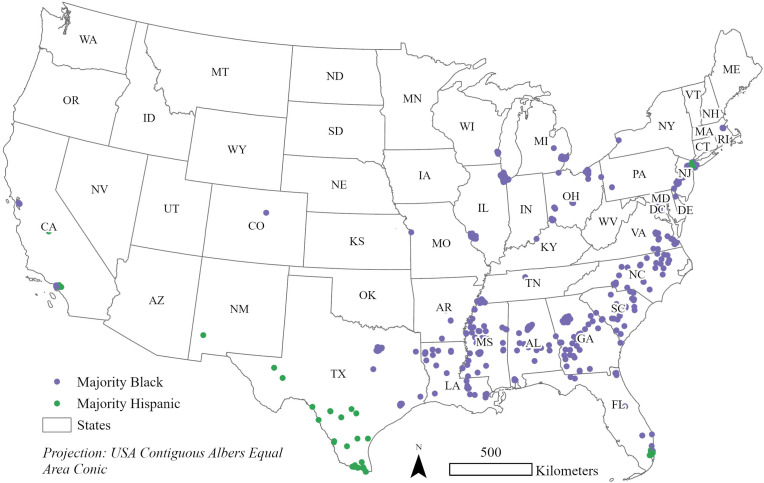
Cases and deaths are highest among majority Hispanic facilities (Table 5), which are predominantly located in metropolitan areas in seven states: California, Florida, Illinois, New Jersey, New Mexico, New York, and Texas (Fig. 1 ). Many facilities are in major cities including Fresno and Los Angeles (California); Miami (Florida); New York City (New York); and Brownsville, Corpus Christi, Laredo, McAllen, and San Antonio (Texas). Total resident cases and deaths are 58 and 12, respectively, and total staff cases is 51. Compared to majority White facilities, majority Hispanic facilities have more total beds (120 versus 99), average residents per day (86 versus 68), admissions from acute care hospitals (89% versus 87%), hospitalizations per resident year (1.5% versus 1.2%), and complaints (1.5 versus 1); and fewer patient days that were private pay (9% versus 14%), adjusted nurse staffing hours per resident per day (3.3 versus 3.6), and lower overall rating (2 versus 5). Hispanic older adults are more likely to reside in nursing homes that are understaffed, financially vulnerable, have performance deficiencies, and provide fewer palliative services (Fennell et al., 2010; Estrada et al., 2022). At the same time, vaccination rates are among the highest for residents (91%) and staff (94%) in majority Hispanic facilities. These findings indicate the importance of contextual factors for assessing the spread of COVID-19 infections and deaths in nursing homes. In other words, while vaccinations are still important, relational care factors (e.g., the environment one lives and works in) also have considerable influence on whether one contracts and/or dies from COVID-19.
Fig. 1.
Locations of majority Black and Hispanic facilities.
In majority Black facilities, which are in 27 states with a notable concentration in the Black Belt (Fig. 1), the trends are more complicated. Resident and staff cases are comparatively high (55 and 50, respectively), but resident deaths are the lowest (7) (Table 5). Resident vaccinations are the lowest (87%), yet staff vaccinations are high (91%). Majority Black facilities also have high total beds (120), average residents per day (91), admissions from acute care hospitals (92%), hospitalizations per resident year (1.6%), and the highest number of complaints (4); in addition to lower patient days that were private pay (6%), adjusted nurse staffing hours per resident per day (3.3), and the lowest overall rating (1). Many of these trends are a result of systemic racism, which has led to racially segregated residential and care settings, lower quality care and working conditions in nursing homes, and poorer health outcomes among Black residents (Smith et al., 2007; Sloane et al., 2021).
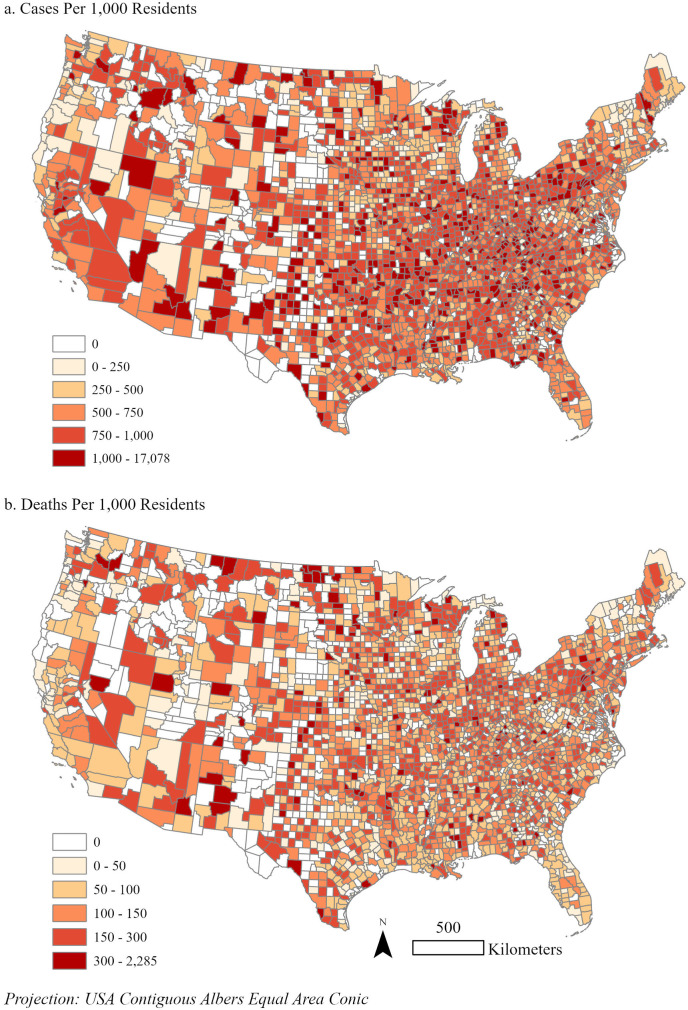
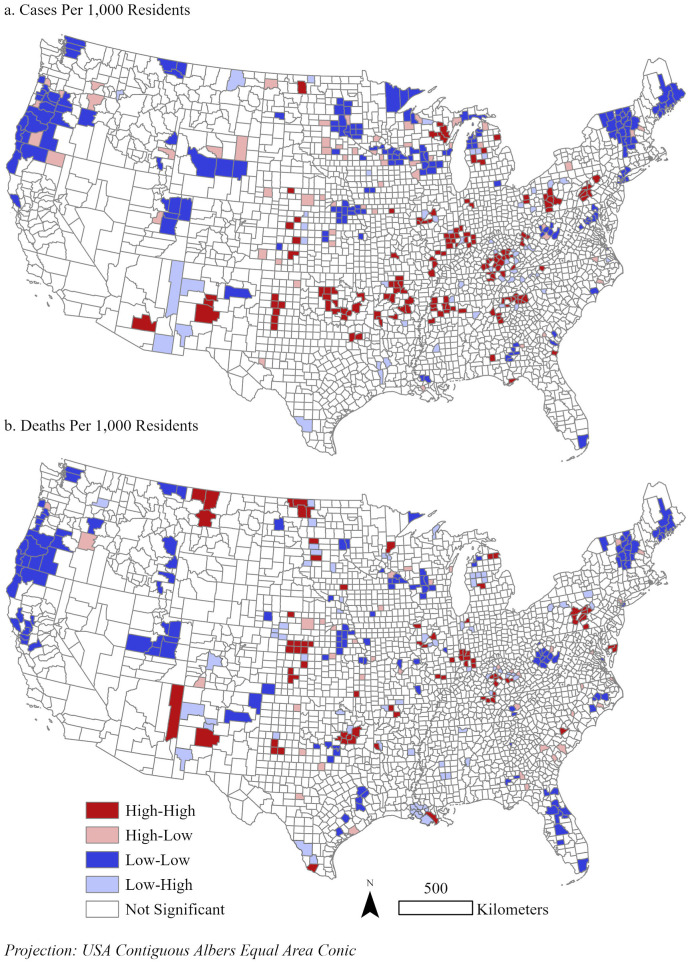
4.3. Local clusters of COVID-19 risk
Since the start of the pandemic, COVID-19 spread to nearly all nursing home facilities in the continental U.S. Fig. 2 maps the total cases and deaths per 1000 residents. The patterns are spatially dispersed. Counties that have facilities with high cases (≥1000) and deaths (≥300) are in most U.S. states (41 and 35 states, respectively).
Fig. 2.
Total cases and deaths per 1,000 residents, by county (n=2,812).
Univariate cluster analysis identified statistically significant (pseudo p-value≤0.05) hot and cold spots of total cases and deaths per 1000 residents (Fig. 3 ). For cases (Fig. 3a), nearly 5.4% of counties are high-high, meaning that they and their neighboring counties have significantly high values. While these hot spots are in 26 states, 56% of them are concentrated in Kentucky, Illinois, Arkansas, Georgia, Pennsylvania, and Oklahoma. Low-low clusters are in 6.3% of counties, meaning that they and their neighbors have significantly low values. Half of these cold spots are in Minnesota, Oregon, Wisconsin, New York, Vermont, and Michigan. Approximately 2% of counties are high-low, indicating that they have a significantly high value while their neighboring counties have low values. Wisconsin (13%) and Minnesota (11%) have the most high-low clusters. Low-high clusters (i.e., significantly low values neighboring counties with high values) comprise 1.9% of counties and are most concentrated in Kentucky (15%) and Tennessee (13%). High-low and low-high clusters reveal outliers among what otherwise should be entirely hot or cold spots. A closer investigation into these unusual clusters is needed to understand why they exist and may uncover a need for county-level intervention.
Fig. 3.
Univariate clusters of median total cases and deaths per 1,000 residents, by county.
The patterns for death clusters (Fig. 3b) share some similarities with cases. Approximately 3% of counties are high-high, 1.4% are high-low, 5.3% are low-low, and 2.3% are low-high clusters. Of the high-high clusters, 54% are concentrated in Indiana, Kentucky, Pennsylvania, Illinois, Kansas, and Oklahoma. Most high-low clusters are in Texas (13%), Georgia (10%), Nebraska (10%), and North Carolina (10%). Of the low-low clusters, 45% are concentrated in Oregon, California, West Virginia, Florida, Vermont, and Texas. Kentucky (12%) and Louisiana (11%) have the most low-high clusters.
Most facilities across all cluster types are rural and comprise of predominantly White residents (Table 6, Table 7 ). Notably, most hot spots contain majority White facilities, revealing that many White, rural residents are not immune to COVID-19 risk. Rural residents are particularly susceptible to contracting COVID-19 and experiencing complications, as they have fewer economic resources and less health care access (Henning-Smith, 2020).
Table 6.
Summary of univariate clusters of median total cases per 1000 residents, by county.
| Variable | High-High (n = 152) | High-Low (n = 56) | Low-Low (n = 177) | Low-High (n = 53) | P-Valuea |
|---|---|---|---|---|---|
| Total Cases Per 1000 Residents (median) | 912 | 864 | 331 | 569 | <0.001 |
| Total Deaths Per 1000 Residents (median) | 151 | 170 | 43 | 85 | <0.001 |
| Total Staff Cases (median) | 49 | 39 | 29 | 43 | <0.001 |
| Total Staff Deaths (median) | 0 | 0 | 0 | 0 | 0.35 |
| % Residents Vaccinated (median) | 89 | 94 | 94 | 91 | <0.001 |
| % Staff Vaccinated (median) | 79 | 81 | 90 | 82 | <0.001 |
| Total Beds (median) | 98 | 64 | 75 | 95 | <0.001 |
| Average Residents Per Day (median) | 65 | 44 | 54 | 62 | <0.001 |
| % Admissions from Acute Care Hospital (median) | 83 | 83 | 89 | 86 | 0.001 |
| Average Age of Residents (median) | 79 | 82 | 81 | 79 | <0.001 |
| % Hospitalizations Per Resident Year (median) | 1.08 | 0.73 | 0.96 | 1.04 | <0.001 |
| Average Activities of Daily Living (ADL) Score (median) | 17.4 | 16.3 | 16.5 | 17.0 | 0.001 |
| % Female Residents (median) | 60 | 58 | 58 | 61 | <0.001 |
| % Patient Days Private Pay (median) | 14 | 18 | 14 | 11 | 0.003 |
| Adjusted Nurse Staffing Hours Per Resident Per Day (median) | 3.44 | 3.99 | 4.01 | 3.51 | <0.001 |
| Number of Fines (median) | 1 | 1 | 1 | 1 | 0.91 |
| Number of Incidents (median) | 0 | 0.25 | 0.5 | 0 | <0.001 |
| Number of Complaints (median) | 1.5 | 1 | 1.5 | 1 | 0.17 |
| Number of Citations (median) | 1 | 0.5 | 0 | 0 | 0.06 |
| Overall Rating, 1–5 (mode) | 2 | 2 | 5 | 2 | |
| Ownership Type (mode) | For Profit | For Profit | For Profit | For Profit | |
| Race/Ethnicity (mode) | Majority White | Majority White | Majority White | Majority White | |
| RUCA (mode) | Rural | Rural | Rural | Rural | |
| States (n) | 26 | 22 | 30 | 25 |
P-Value for Kruskal-Wallis Test.
Table 7.
Summary of univariate clusters of median total deaths per 1000 residents, by county.
| Variable | High-High (n = 84) | High-Low (n = 39) | Low-Low (n = 148) | Low-High (n = 66) | P-Valuea |
|---|---|---|---|---|---|
| Total Cases Per 1000 Residents (median) | 900 | 842 | 492 | 622 | <0.001 |
| Total Deaths Per 1000 Residents (median) | 184 | 182 | 45 | 73 | <0.001 |
| Total Staff Cases (median) | 43 | 40 | 29 | 46 | <0.001 |
| Total Staff Deaths (median) | 0 | 0 | 0 | 0 | 0.16 |
| % Residents Vaccinated (median) | 90 | 91 | 93 | 91 | 0.01 |
| % Staff Vaccinated (median) | 81 | 86 | 87 | 83 | <0.001 |
| Total Beds (median) | 77 | 84 | 81 | 98 | 0.12 |
| Average Residents Per Day (median) | 48 | 58 | 55 | 62 | 0.09 |
| % Admissions from Acute Care Hospital (median) | 81 | 85 | 88 | 82 | <0.001 |
| Average Age of Residents (median) | 81 | 81 | 79 | 80 | 0.06 |
| % Hospitalizations Per Resident Year (median) | 1.00 | 0.99 | 1.04 | 0.99 | 0.94 |
| Average Activities of Daily Living (ADL) Score (median) | 17.1 | 16.8 | 16.6 | 16.9 | 0.65 |
| % Female Residents (median) | 61 | 62 | 58 | 61 | 0.04 |
| % Patient Days Private Pay (median) | 16 | 20 | 14 | 13 | 0.01 |
| Adjusted Nurse Staffing Hours Per Resident Per Day (median) | 3.60 | 3.74 | 4.01 | 3.73 | 0.05 |
| Number of Fines (median) | 1 | 1 | 1 | 1 | 0.53 |
| Number of Incidents (median) | 0 | 0 | 0.5 | 0.5 | 0.30 |
| Number of Complaints (median) | 1.75 | 1 | 1 | 1 | 0.18 |
| Number of Citations (median) | 1 | 0.5 | 0 | 0.5 | 0.15 |
| Overall Rating, 1–5 (mode) | 2 | 4 | 5 | 3 | |
| Ownership Type (mode) | For Profit | For Profit | For Profit | For Profit | |
| Race/Ethnicity (mode) | Majority White | Majority White | Majority White | Majority White | |
| RUCA (mode) | Rural | Rural | Rural | Rural | |
| States (n) | 21 | 19 | 30 | 30 |
P-Value for Kruskal-Wallis Test.
In comparing the distribution of facility attributes across different cluster types, most have values as expected – that is, clusters with high resident cases and deaths tend to have high staff cases, lower vaccination rates, more beds, higher occupancy, and worse facility and working characteristics compared to clusters with low cases and deaths. There are a few unusual values that are unexpected. Among cases (Table 6), low-high clusters have the second highest total staff cases and total beds (high-high clusters have the most). High-low clusters have the highest proportion of vaccinated residents. Low-low clusters have the highest proportion of admissions from acute care hospitals. Similarly, among deaths (Table 7), low-high and low-low clusters have unusual trends. Low-high clusters have the highest total staff cases coupled with the second lowest staff vaccinations. Low-low clusters have the highest acute care hospital admissions.
5. Conclusions
Our study investigated multiple, multi-scalar vulnerability factors associated with COVID-19 risk in nursing homes, including individual and facility characteristics alongside neighborhood and state factors. Of note are racial/ethnic disparities. At first glance, majority White facilities, which comprise most nursing homes (89%), generally have lower cases and deaths and better facility and working conditions than majority Black and Hispanic facilities. These trends align with expectations and findings that racially segregated facilities and communities have fewer economic resources to implement protective measures during a pandemic (Smith et al., 2007; Cai et al., 2021; Sloane et al., 2021). However, the ZINB results reveal more complicated patterns. Compared to majority White facilities, majority Black facilities experience significantly lower cases while their death rates are not significantly different, when controlling for other factors. This may result from taking early mitigation measures, as was the case with a Black-owned nursing home (PBS, 2020). It is with majority Hispanic facilities where our analyses find significant, alarmingly high COVID-19 deaths; suggesting that these facilities have the greatest need for policy improvements in staffing and financing to reduce racial inequalities in nursing home conditions.
At the same time, our cluster analysis detected COVID-19 hot spots in rural areas with majority White facilities, where there is a need to rethink public messaging strategies. The prevailing narrative that racialized minorities are disproportionately infected has reduced fear of COVID-19 and support for safety precautions among White individuals (Skinner-Dorkenoo et al. 2022). Furthermore, rural areas have fewer economic resources and less health care access (Henning-Smith, 2020), and thus have less capacity to manage COVID-19 outbreaks.
We consider different geographic contexts that may affect residents’ vulnerability, expanding on predominant conceptualizations of vulnerability that emphasize individual factors among older adults. Compared to metropolitan facilities, facilities in micropolitan areas have significantly more deaths while those in rural areas have significantly fewer cases and deaths. On the one hand, metropolitan areas have higher population densities than rural areas, which may make social distancing and isolation more difficult, increasing the vulnerability of residents to COVID-19. On the other hand, from the cluster analyses, we find hot spots of cases and deaths in rural areas, indicating that many rural facilities are not immune to COVID-19. Scaling up from neighborhoods to states, the univariate cluster analyses detected most hot spots for cases and deaths in Kentucky, Pennsylvania, Illinois, and Oklahoma.
When assessing facility characteristics between different cluster types, we find stark disparities. Compared to cold spots, hot spots generally have more qualities that make them vulnerable to COVID-19 risk, including lower vaccination rates, fewer adjusted nurse staffing hours per resident per day, and lower overall rating. These findings indicate a need for improving mitigation measures, working conditions, and caring standards in these areas.
The ZINB results indicate that resident vaccinations have a statistically significant negative correlation with COVID-19 risk, while staff vaccinations are not statistically significant. Moreover, the IRR is approximately 1 for resident and staff vaccinations. These findings suggest that vaccinations do not have compelling correlations with COVID-19 risk. However, vaccinations remain important for reducing vulnerability to illness, hospitalization, and death from COVID-19 exposure among older adults.
Our study has implications for practice and policy. First, racial disparities are present. Majority Hispanic facilities have high COVID-19 deaths and some majority White, rural facilities are COVID-19 hot spots. These nursing homes need immediate attention and resources to improve the well-being of residents and staff. Second, the spatial analytic techniques we used can be utilized globally to identify localities where further investigation is needed to examine the vulnerabilities and strengths of facilities and the places where they are located. In our study, we detected multiple hot and cold spots that are worth closer examination. Third, caring, working, and facility conditions are important considerations. ZINB results show that lower staff cases predict zero resident cases and deaths, thus minimizing residents' vulnerability. To lower staff cases, working conditions must have preventative measures. Fourth, location matters. We identify specific states (Connecticut, Massachusetts, Pennsylvania, Kentucky, Illinois, and Oklahoma) whose policies may be exacerbating residents’ vulnerability, including regulations related to PPE provision and use, COVID-19 testing and vaccination, visitation restrictions, workforce expansion, and COVID-19 reporting (Chen et al., 2020).
Future research directions include case studies and comparative analyses of the hot and cold spots identified in our study. A deeper investigation into majority Hispanic, Black, and White facilities can generate valuable insights into how residents and staff navigate multi-scalar processes that affect their COVID-19 vulnerability. Studying racially segregated facilities can provide a better understanding of racial disparities in health and quality of care, and how these inequities stem from structural racism.
Our study has a few limitations. Race/ethnicity data were only available for White, Black, and Hispanic categories, and many facilities had missing data. There needs to be more data collected about other racialized minorities to assess their experiences and better analyze racial disparities. We conceptualize vulnerability as having a negative, unidirectional impact on residents’ well-being residents, partly because of the statistical methods we use and the data available to us. To broaden our understandings of vulnerability in the context of nursing home experiences during a pandemic, more qualitative and mixed method research is needed to assess more nuanced, relational aspects of vulnerability (see for example Jacobs, 2021). As for our statistical methods, we were unable to include multiple tract-level variables as their inclusion caused the ZINB models to fail to achieve convergence. Future research should consider ecological studies using tract-level data to assess neighborhood factors associated with COVID-19 risk or explore multilevel ZINB models. Finally, there are other data issues that are difficult to account for. Case counts are dependent on the availability of testing and death counts are dependent on reporting procedures, which vary across facilities. It is likely that our data underestimates the true numbers of COVID-19, particularly in places where testing is limited (Ouslander and Grabowski, 2020).
As nursing homes across the world navigate ongoing COVID-19 outbreaks, it becomes increasingly important to identify the multiple, intersecting factors that influence the vulnerability of residents and staff to COVID-19 risk. Our study illustrates that the inclusion of geographic factors and spatial analytic techniques provide additional insights into these trends and processes. These considerations allow us to better understand the multi-scalar influences on the vulnerabilities of and racial inequities among older adults living in nursing homes.
CRediT authorship
Sandy Wong: Conceptualization, Methodology, Software, Validation, Formal analysis, Data Curation, Writing–Original Draft, Visualization, Project administration, Funding acquisition. CS Ponder: Conceptualization, Writing–Original Draft, Funding acquisition. Bertram Melix: Methodology, Software, Validation, Formal analysis, Writing–Original Draft, Visualization.
Acknowledgements
This work was supported by the Claude Pepper Center (CPC) at Florida State University. CPC had no involvement in the study design, data collection, analysis, and writing of the paper.
Handling Editor: Susan J. Elliott
Data availability
Data will be made available on request.
References
- Abrams H.R., et al. Characteristics of U.S. Nursing homes with COVID-19 cases. J. Am. Geriatr. Soc. 2020;68(8):1653–1656. doi: 10.1111/jgs.16661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anselin L. Local indicators of spatial association-LISA. Geogr. Anal. 2010;27(2):93–115. [Google Scholar]
- Armstrong P., Braedley S. Canadian Scholars’ Press; 2013. Troubling Care: Critical Perspectives on Research and Practices. [Google Scholar]
- Bailey Z.D., Krieger N., Agénor M., Graves J., Linos N., Bassett M. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- Cai S., Yan D., Intrator O. COVID-19 cases and death in nursing homes: the role of racial and ethnic composition of facilities and their communities. J. Am. Med. Dir. Assoc. 2021;22(7):1345–1351. doi: 10.1016/j.jamda.2021.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen A.T., Ryskina K.L., Jung H.-Y. Long-term care, residential facilities, and COVID-19: an overview of federal and state policy responses. J. Am. Med. Dir. Assoc. 2020;21(9):1186–1190. doi: 10.1016/j.jamda.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrada L.V., et al. Examining regional differences in nursing home palliative care for Black and hispanic residents. J. Palliat. Med. 2022 doi: 10.1089/jpm.2021.0416. [Preprint] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraway J. Faraway: functions and datasets for books by julian faraway. 2016. https://cran.r-project.org/web/packages/faraway/index.html Available at: Accessed:
- Fennell M.L., et al. Elderly hispanics more likely to reside in poor-quality nursing homes. Health Aff. 2010;29(1):65–73. doi: 10.1377/hlthaff.2009.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franch-Pardo I., et al. Spatial analysis and GIS in the study of COVID-19. A review. Sci. Total Environ. 2020;739 doi: 10.1016/j.scitotenv.2020.140033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacalone R.A. US Nurs. Home Indus. 2015 doi: 10.4324/9781315698830. [DOI] [Google Scholar]
- Gorges R.J., Konetzka R.T. Staffing levels and COVID-19 cases and outbreaks in U.S. Nursing homes. J. Am. Geriatr. Soc. 2020;68(11):2462–2466. doi: 10.1111/jgs.16787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington C., et al. Marketization in long-term care: a cross-country comparison of large for-profit nursing home chains. Health Serv. Insights. 2017;10 doi: 10.1177/1178632917710533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington C., et al. Nurse staffing and coronavirus infections in California nursing homes. Pol. Polit. Nurs. Pract. 2020;21(3):174–186. doi: 10.1177/1527154420938707. [DOI] [PubMed] [Google Scholar]
- Henning-Smith C. The unique impact of COVID-19 on older adults in rural areas. J. Aging Soc. Pol. 2020;32:396–402. doi: 10.1080/08959420.2020.1770036. [DOI] [PubMed] [Google Scholar]
- Horton A. Transactions of the Institute of British Geographers; 2021. ‘Liquid Home? Financialisation of the Built Environment in the UK's “Hotel‐style” Care Homes'; pp. 179–192. [Google Scholar]
- Horton A. Financialization and non-disposable women: real estate, debt and labour in UK care homes. Environ. Plann.: Econ. Space. 2022:144–159. [Google Scholar]
- Jackman S., et al. Pscl: political science computational laboratory. 2020. https://cran.r-project.org/web/packages/pscl/index.html Available at: Accessed:
- Jacobs F. Beyond social vulnerability: COVID-19 as a disaster of racial capitalism. Sociologica. 2021;15(1):55–65. [Google Scholar]
- Karim S.A., Chen H. Deaths from COVID‐19 in rural, micropolitan, and metropolitan areas: a county‐level comparison. J. Rural Health. 2021:124–132. doi: 10.1111/jrh.12533. [DOI] [PubMed] [Google Scholar]
- Khairat S., et al. U.S. Nursing home quality ratings associated with COVID-19 cases and deaths. J. Am. Med. Dir. Assoc. 2021;22(10):2021–2025. doi: 10.1016/j.jamda.2021.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khedhiri S. Epidemiol. Methods; 2021. Statistical modeling of COVID-19 deaths with excess zero counts. 10(s1) [Google Scholar]
- Konetzka R.T., et al. A systematic review of long-term care facility characteristics associated with COVID-19 outcomes. J. Am. Geriatr. Soc. 2021;69(10):2766–2777. doi: 10.1111/jgs.17434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruse F.M., et al. Relationship between the ownership status of nursing homes and their outcomes during the COVID-19 pandemic: a rapid literature review. J. Long Term Care. 2021:207–220. [Google Scholar]
- Lee H., et al. Do social determinants of health explain racial/ethnic disparities in COVID-19 infection? Soc. Sci. Med. 2022;306 doi: 10.1016/j.socscimed.2022.115098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levasseur M., et al. Scoping study of definitions and instruments measuring vulnerability in older adults. J. Am. Geriatr. Soc. 2022;70(1):269–280. doi: 10.1111/jgs.17451. [DOI] [PubMed] [Google Scholar]
- Li Y., et al. Racial and ethnic disparities in COVID-19 infections and deaths across U.S. Nursing homes. J. Am. Geriatr. Soc. 2020;68(11):2454–2461. doi: 10.1111/jgs.16847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews A.W., et al. 2020. ‘Covid-19 Stalked Nursing Homes Around the World’, the Wall Street Journal, 31 December. Available at: [Google Scholar]
- National Center for Health Statistics Nursing home care. 2022. https://www.cdc.gov/nchs/fastats/nursing-home-care.htm Available at: Accessed.
- Ouslander J.G., Grabowski D.C. COVID-19 in nursing homes: calming the perfect storm. J. Am. Geriatr. Soc. 2020;68(10):2153–2162. doi: 10.1111/jgs.16784. [DOI] [PubMed] [Google Scholar]
- PBS . 2020. This Maryland Nursing Home Has Had No Coronavirus Cases. How did they do it?’ Available at: [Google Scholar]
- Phelan J.C., Link B. Is racism a fundamental cause of inequalities in health? Annu. Rev. Sociol. 2015;41:311–330. [Google Scholar]
- Ponder C.S., Longhurst A., McGregor M. Contracting-out care: the socio-spatial politics of nursing home care at the intersection of British Columbia's labor, land, and capital markets. Environ. Plan. C Politics Space. 2021;39(4):800–817. [Google Scholar]
- R Core Team . 2021. The R Project for Statistical Computing. Available at: [Google Scholar]
- Rockwell J. From person-centered to relational care: expanding the focus in residential care facilities. J. Gerontol. Soc. Work. 2012:233–248. doi: 10.1080/01634372.2011.639438. [DOI] [PubMed] [Google Scholar]
- Shin O., et al. Types of multidimensional vulnerability and well-being among the retired in the U.S. Aging Ment. Health. 2021;25(7):1361–1372. doi: 10.1080/13607863.2020.1768212. [DOI] [PubMed] [Google Scholar]
- Skinner-Dorkenoo A.L., et al. Highlighting COVID-19 racial disparities can reduce support for safety precautions among White U.S. residents. Soc. Sci. Med. 2022;301 doi: 10.1016/j.socscimed.2022.114951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloane P.D., et al. Addressing systemic racism in nursing homes: a time for action. J. Am. Med. Dir. Assoc. 2021;22(4):886–892. doi: 10.1016/j.jamda.2021.02.023. [DOI] [PubMed] [Google Scholar]
- Smith D.B., et al. Separate and unequal: racial segregation and disparities in quality across U.S. nursing homes. Health Aff. 2007;26(5):1448–1458. doi: 10.1377/hlthaff.26.5.1448. [DOI] [PubMed] [Google Scholar]
- Sugg M.M., et al. Mapping community-level determinants of COVID-19 transmission in nursing homes: a multi-scale approach. Sci. Total Environ. 2021;752 doi: 10.1016/j.scitotenv.2020.141946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan S.B., deSouza P., Raifman M. Structural racism and covid -19 in the USA: a county-level empirical analysis. J. Rac. Ethnic Health Dispar. 2022;9:236–246. doi: 10.1007/s40615-020-00948-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The New York Times . The New York Times; 2020. Nearly One-Third of U.S. Coronavirus Deaths Are Linked to Nursing Homes. 27 June. Available at: [Google Scholar]
- Wang X., Wilson C., Holmes K. Role of nursing home quality on COVID-19 cases and deaths: evidence from Florida nursing homes. J. Gerontol. Soc. Work. 2021;64(8):885–901. doi: 10.1080/01634372.2021.1950255. [DOI] [PubMed] [Google Scholar]
- Yang B.K., Carter M.W., Wayne Nelson H. Trends in COVID-19 cases, deaths, and staffing shortages in US nursing homes by rural and urban status. Geriatr. Nurs. 2021:1356–1361. doi: 10.1016/j.gerinurse.2021.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.