Abstract
Resulting from chronic exposure to parenting stress, parental burnout is a syndrome located on a continuum between stress and depression. Research interest is growing, and several risk factors have already been identified, but more studies are needed. We assessed the relationship between early maladaptive schemas (as potential risk factors), coping strategies, and the three dimensions of parental burnout (emotional and physical exhaustion, emotional distancing, and loss of parental accomplishment). A total of 115 French-speaking parents answered an online questionnaire. Results (correlations and acyclic graph driven by emotion-focused coping) confirmed the influence of EMSs on the expression of parental burnout. More specifically, schemas in the following three EMS domains were identified as major risk factors: disconnection and rejection (especially abandonment/instability, emotional deprivation, and defectiveness/shame), impaired autonomy and performance (especially dependence/incompetence and failure), and over-vigilance and inhibition (especially negativity/pessimism and punitiveness). Interestingly, our results suggest that emotional coping is not a risk factor for parental burnout, but a consequence of emotional and physical exhaustion and loss of parental accomplishment. Thus, the more parents reported overactivation of these EMSs, the more they are exhausted, and the more they use emotion-focused coping. These results are discussed in terms of possible therapies.
Keywords: Exhaustion, Parenthood, Early maladaptive schemas, Adjustment, Directed acyclic graph
Introduction
Parental Burnout
Parental burnout is a unique and context-specific syndrome that lies on a continuum between stress and depression (Mikolajczak et al., 2020; Roskam et al., 2017). This syndrome can be defined along three dimensions: emotional and physical exhaustion, emotional distancing from children, and sense of inefficacy or loss of parental accomplishment (Roskam et al., 2017). Emotional and physical exhaustion result in inappropriate behaviors, including an inability to respond appropriately to the children’s needs, and major mood swings. Emotional distancing from children is typically reflected in fewer parent–child exchanges, although behaviors that meet the children’s physiological and instrumental needs are maintained. Loss of parental accomplishment translates as feelings of no longer being as good a parent as before, no longer being up to the job, and no longer deriving fulfillment from the role of father or mother. In France and Belgium and before the COVID-19 pandemic, 2–12% of parents experience parental burnout syndrome (Roskam et al., 2017; Sánchez-Rodríguez et al., 2019). The prevalence of parental burnout is estimated between 6.2 and 6.7% for France and between 7.5 and 9.8% for Belgium (Roskam et al., 2021; van Bakel et al., 2022).
Several studies (Kawamoto et al., 2018; Le Vigouroux & Scola, 2018; Mikolajczak et al., 2017; Sánchez-Rodríguez et al., 2019) have shown that dispositional risk factors are more important in parental burnout than either demographic (e.g., age of parent or child: Le Vigouroux et al., 2022). The most salient dispositional factors are parental personality (Le Vigouroux & Scola, 2018; Le Vigouroux et al., 2017) and perfectionism (Kawamoto et al., 2018; Sorkkila & Aunola, 2020). Behavioral risk factors have already been the subject of various studies. However, risk factors related to mental beliefs or representations have seldom been studied, if at all, with scant attention being paid to the influence of early maladaptive schemas (EMSs), even though these have been shown to play a major role in pathologies similar to parental burnout, such as depression, anxiety (e.g., Nicol et al., 2020), and occupational burnout (e.g., Abeltina & Rascevska, 2021).
Early Maladaptive Schemas and Mood Disorders
EMSs can be defined as mental beliefs that serve as filters through which individuals interpret the events they experience (Young et al., 2017). These salient representations are made up of thoughts (particularly memories), emotions, and bodily sensations concerning the individuals and their relations with others. They are described as early because they are constructed during childhood and adolescence and maladaptive because they continue to be systematically activated in adulthood. Young et al.’s (2017) model identifies 18 early maladaptive schemas, divided into five major domains of unmet emotional needs. The first domain is entitled disconnection and rejection and consists of the schemas of abandonment/instability, mistrust/abuse, emotional deprivation, defectiveness/shame, and social isolation/alienation. The second domain is entitled impaired autonomy and performance and corresponds to dependence/incompetence, vulnerability to harm or illness, enmeshment/undeveloped self, and failure. The third domain is called impaired limits and includes two schemas: entitlement/grandiosity and insufficient self-control/self-discipline. The fourth domain is other-directedness and corresponds to subjugation, self-sacrifice, and approval-seeking/recognition-seeking. The fifth domain is over-vigilance and inhibition and refers to negativity/pessimism, emotional inhibition, unrelenting standards/hypercriticalness, and punitiveness. This categorization of EMS is presented in Table 1.
Table 1.
Structuration and description of EMS
| Domains | EMS | Description |
|---|---|---|
| Disconnection and rejection | Abandonment/instability | Belief that affective relationships will not last |
| Mistrust/abuse | Belief that others will mistreat the individual | |
| Emotional deprivation | Belief that emotional needs will not be met | |
| Defectiveness/shame | Belief that one is inferior to others | |
| Social isolation/alienation | Belief that one is apart from others | |
| Impaired autonomy and performance | Dependence/incompetence | Belief that one is incapable of shouldering one's daily responsibilities |
| Vulnerability to harm or illness | Belief that an uncontrollable catastrophe is about to happen | |
| Enmeshment/undeveloped self | Belief that one of the two linked individuals cannot survive without the other | |
| Failure | Belief that one is incompetent in performance domains | |
| Impaired limits | Entitlement/grandiosity | Belief of being superior to others |
| Insufficient self-control/self-discipline | Inability or refusal to exercise sufficient self-control and frustration | |
| Other-directedness | Subjugation | Belief that in order to avoid the anger or abandonment of others, one must submit to it excessively |
| Self-sacrifice | Belief of having to comply with the demands and expectations of others to avoid feeling guilty or egoistic | |
| Approval-seeking/recognition-seeking | Excessive need for attention and approval from others | |
| Over-vigilance and inhibition | Negativity/pessimism | Focus on the negative aspects of life at the expense of the positive |
| Emotional inhibition | Excessive control of spontaneous reactions | |
| Unrelenting standards/hypercriticalness | Belief that perfection must be achieved | |
| Punitiveness | Tendency to be intolerant of others and of oneself in the face of imperfection |
In order to adjust to EMS, individuals and parents develop patterns at an early age. There are three patterns of adaptation to EMS: submission (or surrender, i.e., the parent submits to the EMS), avoidance (or escape, i.e., the parent psychologically withdraws from the distress caused by the EMS, adopting various forms of avoidance) and compensation (or battle, i.e., the parent fights against his or her pattern as if to prove the opposite, either by mistreating others or by behaving in an extreme way, but in a way that ultimately turns out to be very inappropriate). Thus, these patterns are dysfunctional because they maintain EMS in adult life (Young et al., 2017).
To the best of our knowledge, no study has so far explored the relationship between EMSs and parental burnout, even though EMSs are strongly activated in individuals with depressive symptoms (Chen et al., 2019; Cormier et al., 2011; Hawke & Provencher, 2011; Nicol et al., 2020), anxiety (Hawke & Provencher, 2011; Nicol et al., 2020; Tariq et al., 2021), or occupational burnout (Abeltina & Rascevska, 2021; Grebot et al., 2011; Simpson et al., 2019). More specifically, schemas in the disconnection and rejection, impaired autonomy and performance, and over-vigilance and inhibition domains seem to be risk factors for depression (Chen et al., 2019; Cormier et al., 2011; Walburg et al., 2008; Young et al., 2001, 2017), anxiety (Billoux et al., 2012; Pinto-Gouveia et al., 2006), and occupational burnout (Grebot et al., 2011; Simpson et al., 2019). Given the major role of schema overactivation in these psychopathological disorders, it is important to explore the importance of EMSs in relation to parental burnout syndrome, particularly their influence on individuals’ psychological adjustment.
Coping, Early Maladaptive Schemas, and Mood Disorders
Coping was defined by Lazarus and Folkman (1984) as the set of cognitive and behavioral efforts made by individuals to manage stress. This stress results from the interaction between the situation experienced by the individual and his perceived resources. More precisely, an individual, or in this case a parent, feels stress when he/she evaluates the situation as threatening (i.e., as having an important stake), according to the activation of certain EMS, and his/her resources as insufficient to respond to it. Coping is a dynamic, changing process, with considerable intra-individual variability and no stable general characteristics (Bruchon-Schweitzer & Boujut, 2014). Three types of coping are classically identified: problem-focused, emotion-focused, and social support-seeking. Problem-focused coping involves solving the problem by seeking information, developing a plan of action, and confronting the situation (Folkman & Lazarus, 1980; Lazarus & Folkman, 1984). Emotion-focused coping refers to efforts made to change the emotional state engendered by a stressful situation (Lazarus & Folkman, 1984), such as such as avoidance, rumination, or denial. Social support-seeking coping corresponds to the actions of individuals to obtain help, encouragement, and/or sympathy from others (Cousson et al., 1996). This strategy differs from reliance on an established social network, in that it does not concern existing resources (Bruchon-Schweitzer & Boujut, 2014).
The relation between coping strategies and psychopathological disorders, especially emotion-focused ones, has been highlighted (Aldao et al., 2010; Groth et al., 2019; Heffer & Willoughby, 2017). The more individuals use emotional coping, the more they experience anxiety and stress (Koleck et al., 2003), depression (Horwitz et al., 2011; Thompson et al., 2010), and occupational burnout (Friganovic et al., 2019; Pronost, 2001). In the field of parenthood, coping strategies are related with parental stress (Razurel et al., 2013), especially in the context of child disability (Dabrowska & Pisula, 2010; Hastings et al., 2005; Najmi et al., 2018). For example, the more parents use emotion-focused coping, the more vulnerable they are to parental stress (Dabrowska & Pisula, 2010), and the more mothers uses problem-focused coping, the less they are in maternal burnout (Lebert-Charron et al., 2018).
Thus, both EMSs and coping strategies are related to emotional distress. Furthermore, EMSs are related to coping strategies (Ke & Barlas, 2020; Zadahmad & Torkan, 2016). Gallagher and Gardner (2007) highlighted a significant negative correlation between avoidance-focused coping (i.e., cognitive avoidance, resignation, seeking alternative rewards, and emotional discharge) and EMSs, and more specifically between avoidance-focused coping and the disconnection and rejection, impaired autonomy and performance, and other-directedness domains. Furthermore, the association between EMSs and psychopathology is mediated by the use of maladaptive compensatory coping and deficits in adaptive coping. For example, coping strategies mediate the relationships between schema domains and internalizing or externalizing behaviors (van Wijk-Herbrink et al., 2018) and occupational burnout (Simpson et al., 2019).
Objectives and Hypotheses
The present study had two main objectives. The first was to pursue the identification of dispositional variables associated with parental burnout (Le Vigouroux & Scola, 2018; Mikolajczak et al., 2017), focusing on EMSs. The second was to examine further how parents cope with burnout, by studying the relationships between parental burnout and coping strategies. We also sought to highlight the relationships between parental burnout, coping strategies, and EMSs, in order to understand this syndrome better.
Our first hypothesis concerned the relationship between parental burnout and EMSs. Parental burnout lies on a continuum between stress and depression (Mikolajczak et al., 2020; Roskam et al., 2017), and EMS overactivation has been observed in both these psychological disorders, as well as in occupational burnout (Chen et al., 2019; Gallagher & Gardner, 2007; Simpson et al., 2019; Tariq et al., 2021). We therefore expected EMSs are related to parental burnout syndrome too. More specifically, we assumed that parents with overactivated schemas in the domains of disconnection and rejection (e.g., emotional deprivation and defectiveness/shame), impaired autonomy and performance (e.g., dependence/incompetence and failure), and over-vigilance and inhibition (e.g., negativity/pessimism, emotional inhibition, punitiveness, and unrelenting standards/hypercriticalness) would experience more parental burnout.
Our second hypothesis concerned the relations between coping strategies and parental burnout. Given that emotion-focused strategies are used more in the context of parenting stress (Razurel et al., 2013), occupational burnout (Friganovic et al., 2019), and anxiety and depression (Aldao et al., 2010), whereas problem-focused coping is a protective factor in parental burnout (Lebert-Charron et al., 2018), we hypothesized that the more parents use problem-focused coping, the lower they feel parental burnout. Conversely, the more parents use emotion-focused coping, the higher their risk of experiencing parental burnout.
Our third hypothesis concerned the possible mediation by emotion-focused coping of the relationship between EMSs (those identified in first hypothesis) and parental burnout, which has already been observed other pathologies (Simpson et al., 2019; van Wijk-Herbrink et al., 2018). We hypothesized that the more these EMSs are activated, the more parents use emotion-focused coping, putting them at greater risk of parental burnout.
Method
Participants
The sample was composed of 115 participants (including 107 mothers) aged 25–61 years (M = 35, SD = 6.2). The inclusion criterion was having at least one child living at home. For the remainder of the study, parental burnout was treated as a continuous variable. Given the correlations presented in the literature between MSE, coping and experience dimensions such as anxiety and depressive symptomatology, and professional burnout (r < 0.30), the power analysis indicates that a sample of 84 participants is sufficient.
Measure
Parental burnout was measured using the Parental Burnout Inventory (PBI: Roskam et al., 2017). This inventory has been validated in French and consists of 22 items assessing the three dimensions of parental burnout: emotional and physical exhaustion (e.g., “I feel my parental role is breaking me down”), emotional distancing from children (e.g., “I sometimes feel as though I am taking care of my children on autopilot”), and parental accomplishment (e.g., “I am easily able to create a relaxed atmosphere with my children”). For the total parental burnout score, the parental accomplishment scores are reversed. Participants rate these items on a scale ranging from 1 (never) to 7 (every day). In the validation study, this inventory has good internal consistency (respectively, 0.88, 0.95, and 0.87, for the three dimensions, and 0.91 for global score).
EMSs were assessed using the French version of the Young Schema Questionnaire–Short Form 3 (YSQ—S3: Bouvard et al., 2018). This 90-item questionnaire probes 18 EMSs (each EMS is measured by 5 items) in five domains: (I) disconnection and rejection: abandonment/instability (e.g., “I hold on to the people I am close to for fear they will leave me”), mistrust/abuse (e.g., “I feel like others will take advantage of me”), emotional deprivation (e.g., “I have had no one to help me grow, to share their inner world with me, or who cares deeply about anything that happens to me”), defectiveness/shame (e.g., “No one I desire could stay close to me if they knew who I really am”), and social isolation/alienation (e.g., “I feel alienated from others, or cut off from others”); (II) impaired autonomy and performance: dependence/incompetence (e.g., “I don't feel like I can take care of myself in everyday life”), vulnerability to harm or illness (e.g., “I am afraid of being physically attacked by people”), enmeshment/undeveloped self (e.g., “In my relationships, I let the other have the upper hand”), and failure (e.g., “I am incompetent when it comes to success”); (III) impaired limits: entitlement/grandiosity (e.g., “When I expect something from others, I find it very difficult to accept a refusal”) and insufficient self-control/self-discipline (e.g., “I can't seem to discipline myself to complete routine or boring tasks”); (IV) other-directedness: subjugation (e.g., “I couldn't separate myself from my mother or father as people my age seem to do”), self-sacrifice (e.g., “I am the one who usually ends up taking care of the people I am close to”), and approval-seeking/recognition-seeking (e.g., Having money and knowing important people are things that give me value”); and (V) over-vigilance and inhibition: negativity/pessimism (e.g., “Even when everything is going well, I have the impression that it will only be temporary”), emotional inhibition (e.g., “I am too embarrassed to express positive feelings to others (e.g., affection, interest)”), unrelenting standards/hypercriticalness (e.g., “I have to be the best at almost everything I do, I can't accept being second best”), and punitiveness (e.g., “If I make a mistake, I deserve to be punished”). Participants rate each item on a scale ranging from 1 (“This is completely wrong for me”) to 6 (“Describes me perfectly”). In the validation study, the reliability was satisfactory for fourteen schemas (> 0.70). In this study, the reliability was satisfactory too (> 0.63).
Coping strategies were assessed using the French version of the Ways of Coping Checklist (WCC: Cousson et al., 1996). This version contains 27 items and has good internal consistency, test–retest reliability, and construct and criterion validities (Cousson et al., 1996). The WCC is composed of three subscales: emotion-focused coping (e.g., “I wished the situation would go away or end”), problem-focused coping (e.g., “I established an action plan and followed it”), and social support-seeking (e.g., “I asked for advice from someone worthy of respect and I took it”). Participants rate items on a scale ranging from 1 (“No”) to 4 (“Yes”). In the validation study, the reliability of each subscale was satisfactory (respectively, 0.72, 0.79, and 0.73).
Procedure
We used online survey platforms (first LimeSurvey and then Qualtrics) to distribute the questionnaire via social media (Facebook) in two data collection (first in 2018, and the second to expand sample in 2019). All participants freely agreed (free and informed consent) to take part in the study and were guaranteed anonymity. The order of the questionnaires was identical for all participants. Participants did not receive financial compensation for their participation. At the time of data collection, the University of Nîmes did not yet have an ethics committee. Each respondent was given an opportunity to contact a psychologist specializing in behavioral, cognitive, and emotional therapy following completion of the questionnaires.
Statistical Analyses
We ran descriptive and correlation analyses for EMSs, coping strategies, and parental burnout with JASP software. In order to explore the relationships and their directions between our variables of interest, we estimated a directed acyclic graph (DAG). This model allows to estimate the directed structure of a system of variables, or more precisely directional probabilities of relation between several variables (e.g., McNally et al., 2017). The data and r script are available on OSF (https://doi.org/10.17605/OSF.IO/8GEWU). After examination of correlations results, we selected the most strongly and positively related variables in it. Then, we estimate the structure of the system between our variable of interest at first time with “bnlearn” package on R (Scutari, 2010). In this package, the bootstraph function computes the structural aspects of the network model by adding edges, removing them, and reversing their direction in order to propose an optimal and parsimonious network of directed relations between the variables that constitute the nodes of the system. In a first step, we have estimated a network according to an iterative procedure of randomly restarting this process with different possible edges linking different node pairs, perturbing the system, and using 50 different random restarts to avoid local maxima. We estimated 100 perturbations (i.e., attempts to insert, delete, or reverse an edge) for each restart. As this iterative procedure unfolds, the function returns the best fitting network based on this random restart/perturbation process. In a second step, we tested the stability of the DAG obtained with a bootstrapping method (on 10,000 samples with replacement) based to Scutary and Nagarajan’s (2013) recommendations.
Results
Descriptive data for the variables of interest are set out in Table 2. Regarding parental burnout, our sample had a higher total mean score (M = 40.19, SD = 23.07) than that reported in previous studies (M = 31.05, SD = 19.38: Mikolajczak et al., 2017, M = 32.52, SD = 21.23: 2018, M = [27.17;33.58], SD = [19.80;22.26]: 2019). However, as noted in the “Participants” subsection, only 11% of our sample were considered to be in burnout, consistent with the prevalence reported in the literature. Regarding coping strategies, our sample’s mean levels of coping strategy use were similar to those observed by Lebert-Charron and colleagues (2018), and their mean levels of EMS activation were similar to those observed by Simpson and colleagues (2019).
Table 2.
Descriptive data on parental burnout, EMSs, and coping
| Min | Max | M | SD | Skewness | Kurtosis | |
|---|---|---|---|---|---|---|
| Parental burnout | 0 | 121 | 40.19 | 23.07 | 0.78 | 1.17 |
| Emotional and physical exhaustion | 0 | 47 | 23.17 | 12.53 | − 0.01 | − 0.93 |
| Emotional distancing | 0 | 46 | 10.09 | 8.85 | 1.68 | 3.72 |
| Loss of parental accomplishment | 0 | 28 | 6.93 | 6.78 | 1.53 | 1.93 |
| Early maladaptive schemas | ||||||
| Disconnection and rejection | ||||||
| Abandonment/instability | 1 | 5 | 2.66 | 1.05 | 0.38 | − 0.85 |
| Mistrust/abuse | 1 | 5.20 | 2.53 | 1.03 | 0.85 | 0.48 |
| Emotional deprivation | 1 | 6 | 2.44 | 1.29 | 0.93 | 0.05 |
| Defectiveness/shame | 1 | 6 | 1.82 | 1.05 | 1.91 | 3.74 |
| Social isolation/alienation | 1 | 6 | 2.63 | 1.16 | 1.03 | 0.77 |
| Impaired autonomy and performance | ||||||
| Dependence/incompetence | 1 | 3.80 | 1.82 | 0.76 | 0.79 | − 0.26 |
| Vulnerability to harm or illness | 1 | 6 | 2.30 | 1.08 | 1.12 | 1.16 |
| Enmeshment/undeveloped self | 1 | 5 | 1.87 | 0.93 | 1.42 | 1.74 |
| Failure | 1 | 6 | 2.14 | 1.17 | 1.38 | 1.57 |
| Impaired limits | ||||||
| Entitlement/grandiosity | 1 | 5.20 | 2.84 | 0.87 | 0.52 | 0.09 |
| Insufficient self-control/self-discipline | 1 | 5 | 2.44 | 0.83 | 0.66 | − 0.06 |
| Other-directedness | ||||||
| Subjugation | 1 | 6 | 2.20 | 1.02 | 1.26 | 1.73 |
| Self-sacrifice | 1 | 6 | 3.84 | 1.13 | − 0.19 | − 0.59 |
| Approval-seeking/recognition-seeking | 1 | 5.80 | 2.81 | 1 | 0.58 | 0.04 |
| Over-vigilance and inhibition | ||||||
| Negativity/pessimism | 1 | 6 | 2.65 | 1.22 | 0.60 | − 0.47 |
| Emotional inhibition | 1 | 5.60 | 2.41 | 1.05 | 0.75 | 0.14 |
| Unrelenting standards/hypercriticalness | 1 | 5.80 | 3.34 | 1.04 | 0.15 | − 0.34 |
| Punitiveness | 1.20 | 5.40 | 2.61 | 0.93 | 0.93 | 0.79 |
| Coping | ||||||
| Problem-focused coping | 17 | 39 | 29.46 | 4.52 | − 0.24 | − 0.20 |
| Emotion-focused coping | 13 | 35 | 24.32 | 5.76 | − 0.18 | − 0.70 |
| Social support-seeking | 9 | 32 | 23.23 | 4.87 | − 0.40 | − 0.06 |
Concerning the relationship between EMSs and parental burnout, and in accordance with our first hypothesis, results (Table 3) highlighted moderate positive relationships between EMSs and parental burnout. Only four of the 18 EMS failed to vary with the parental burnout score: enmeshment/undeveloped self, entitlement/grandiosity, approval-seeking/recognition-seeking, and self-sacrifice, although the latter was positively and moderately related to the emotional and physical exhaustion dimension. More specifically, and in accordance with our first hypothesis, parents who reported strong activation of schemas in the disconnection and rejection (specifically defectiveness/shame, followed by emotional deprivation), impaired autonomy and performance (specifically dependence/incompetence and failure), and over-vigilance and inhibition (specifically negativity/pessimism) domains also reported high levels of parental burnout (results were similar for each of the three burnout dimensions).
Table 3.
Correlation matrix between parental burnout and its three dimensions, early maladaptive schemas, and coping strategies
| PB | EPE | ED | LPA | CopP | CopE | CopS | |
|---|---|---|---|---|---|---|---|
| Early maladaptive schemas | |||||||
| Disconnection and rejection | |||||||
| Abandonment/instability | .34*** | .31*** | .20* | .31** | − .19 | .42*** | − .07 |
| Mistrust/abuse | .40*** | .26** | .30** | .50*** | − .23* | .38*** | − .14 |
| Emotional deprivation | .48*** | .38*** | .37*** | .43*** | − .23* | .35*** | − .25* |
| Defectiveness/shame | .55*** | .39*** | .46*** | .55*** | − .37*** | .40*** | − .33** |
| Social isolation/alienation | .38*** | .26** | .35*** | .34*** | − .18 | .25* | − .23* |
| Impaired autonomy and performance | |||||||
| Dependence/incompetence | .53*** | .39*** | .48*** | .45*** | − .33** | .42*** | − .16 |
| Vulnerability to harm or illness | .42*** | .43*** | .23* | .30** | − .33** | .38*** | − .12 |
| Enmeshment/undeveloped self | .14 | .09 | .10 | .18 | − .16 | .19 | − .05 |
| Failure | .50*** | .36** | .42*** | .50*** | − .25* | .35*** | − .26* |
| Impaired limits | |||||||
| Entitlement/grandiosity | .17 | .17 | .16 | .07 | − .04 | .25* | 0 |
| Insufficient self-control/self-discipline | .39*** | .31* | .30*** | .36*** | − .29** | .38*** | − .23* |
| Other-directedness | |||||||
| Subjugation | .37*** | .34*** | .22 | .32** | − .17 | .38*** | − .08 |
| Self-sacrifice | .20* | .32** | .01 | .06 | .12 | .10 | .02 |
| Approval-seeking/recognition-seeking | .12 | .15 | .07 | .02 | − .01 | .32** | .12 |
| Over-vigilance and inhibition | |||||||
| Negativity/pessimism | .50*** | .49*** | .31** | .38*** | − .32** | .48*** | − .10 |
| Emotional inhibition | .33*** | .26** | .30*** | .25** | − .16 | .17 | − .31** |
| Unrelenting standards/hypercriticalness | .30** | .30** | .23* | .13 | − .13 | .36*** | .05 |
| Punitiveness | .44*** | .38*** | .37*** | .31** | − .29** | .50*** | − .18 |
| Coping | |||||||
| Problem-focused coping | − .48*** | − .34** | − .39*** | − .51*** | |||
| Emotion-focused coping | .58*** | .50*** | .44*** | .47*** | − .20 | ||
| Social support-seeking | − .16 | .01 | − .25** | − .24** | .45*** | .18 | |
PB, parental burnout; EPE, emotional and physical exhaustion; ED, emotional distancing; LPA, loss of parental accomplishment; CopP, problem-focused coping; CopE, emotion-focused coping; CopS, social support-seeking coping
* p < .05, ** p < .01, ***p < .001
Concerning the relationship between coping strategies and parental burnout, and in accordance with our second hypothesis, correlation analyses (Table 3) showed that the more parents used problem-based coping strategies, the less they reported high levels of parental burnout (especially loss of parental accomplishment). Conversely, the more parents used emotion-focused coping, the more they reported high levels of parental burnout (especially emotional and physical exhaustion). The use of strategies centered on social support-seeking was not correlated with emotional and physical exhaustion. However, our results revealed negative, moderate, and significant correlations between these strategies and both emotional distancing and loss of parental accomplishment. The more parents used social support-seeking, the less they reported emotional distancing with their child and loss of parental accomplishment. Moreover, the more parents used problem-focused coping, the more they also reported using social support-seeking coping. By contrast, the use of emotion-focused coping was not correlated with either of the other two forms of coping.
Concerning the relationship between coping and EMSs, our results (Table 3) revealed that emotion-focused coping was more closely related to EMSs (particularly those in the disconnection and rejection, impaired autonomy and performance, and over-vigilance and inhibition domains), than problem-focused coping, and even more so than social support-seeking coping. More specifically, the more parents reported strong activation of schemas in the disconnection and rejection (specifically abandonment/instability), impaired autonomy and performance (specifically dependence/incompetence), and over-vigilance and inhibition (specifically punitiveness and negativity/pessimism) domains, the more they used emotion-focused coping. By contrast, the more they reported strong activation of EMSs in the disconnection and rejection (specifically defectiveness/shame), impaired autonomy and performance (specifically dependence/incompetence and vulnerability to harm or illness), and over-vigilance and inhibition (specifically negativity/pessimism) domains, the less they used problem-focused coping.
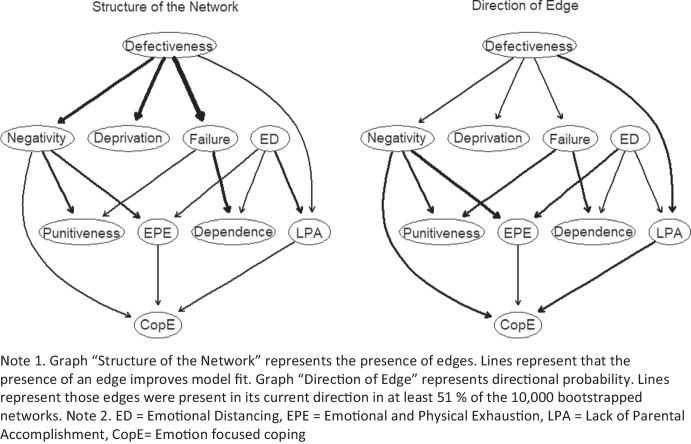
Concerning the relationship between EMS, emotion-focused coping and parental burnout dimensions, and based on the correlation results presented above, we retained the schemas and coping strategies most closely and positively related to parental burnout dimensions scores. Accordingly, we selected the schemas of emotional deprivation and defectiveness/shame in the disconnection and rejection domain, dependence/incompetence and failure in the impaired autonomy and performance domain, and negativity/pessimism and punitiveness in the over-vigilance and inhibition domain. We then estimated the DAG. Figure 1 shows DAGs resulting from 10, 000 bootstrapped samples. For both graph (Fig. 1), edges were retained when their strength was greater than the optimal cut resulting from the method of Scutari and Nagarajan (2013). The first graph (Fig. 1, structure of the network) illustrates the importance of each edge to the overall network structure. Edge thickness indicates the importance of that edge to the overall network structure, with greater thickness signifying that an edge is more crucial to model fit. The second graph (Fig. 1, direction of edge) illustrates the probability of prediction is in the direction depicted. Thick arrows indicate high directional probabilities, and thin arrows indicate low directional probabilities.
Fig. 1.
Directed acyclic graphs (DAGs) representing the structure of the network and the direction of the relationships between the variables of interest
Specifically in the first graph (Fig. 1), edge thickness reflects the network. Greater thickness thus signifies that an edge is more crucial to model fit (McNally, 2016). The edges most important to the network structure connect defectiveness schema to failure and deprivation schemas (with a change in BIC of − 55.92 and − 34.12, respectively). The edges least important to the network structure, meanwhile, connect schema of negativity and emotional and psychical exhaustion to emotion-focused coping (with a change in BIC of − 1.11 and − 2.70, respectively). In the second graph, edges signify directional probabilities: an edge is thicker if it points from one node to another in a greater proportion of the bootstrapped networks. The thickest edges connect negativity schema to emotional and physical exhaustion (0.80, i.e., this edge was pointing in that direction in 8, 000 of the 10, 000 bootstrapped networks and in the other direction in 2000 of the 10, 000 bootstrapped networks) and schemas of failure to punitiveness (0.74). The thinnest edges connect emotional distancing to loss of parental accomplishment (0.50) and dependance schema (0.54). Then, structurally, schema of defectiveness arises at the top of the DAG, directly influencing schemas of negativity, deprivation, and failure, which then directly influence schema of punitiveness and dependance and emotional and physical exhaustion, while emotional distancing influences dependence schema and emotional and physical exhaustion. Finally, parental burnout dimension of emotional and physical exhaustion and loss of parental accomplishment influence emotion-focused coping.
Discussion
This study had two main objectives. The first was to continue the search for dispositional variable related to parental burnout (e.g., Le Vigouroux & Scola, 2018; Le Vigouroux et al., 2017; Mikolajczak et al., 2017), by focusing on EMSs. The second was to examine further how parents cope with parental burnout, by studying the relationships between EMSs, parental burnout dimensions, and coping strategies. To our knowledge, ours was the first study to probe the relationships between these variables.
Our results highlighted the relation between EMS activation and the expression of parental burnout and were in line with those yielded by studies of depressive disorder, anxiety, and occupational burnout (Billoux et al., 2012; Cormier et al., 2011; Hawke & Provencher, 2011; Walburg et al., 2008; Young et al., 2001, 2017). They suggested that some EMSs can be regarded as potential risk factors for parental burnout. More specifically, our results revealed the strong relation between parental burnout dimensions and EMS belonging to the disconnection and rejection (especially abandonment/instability, emotional deprivation, and defectiveness/shame), impaired autonomy and performance (especially dependence/incompetence and failure), and over-vigilance and inhibition (especially negativity/pessimism and punitiveness) domains. For example, parents who consider themselves to be imperfect (defectiveness/shame schema) may strive to reach an unattainable parenting ideal, may not feel fulfilled in their roles as parents, and may exhaust themselves trying to achieve their impossible goal. Parents who perceive their emotional needs to be unmet by their coparent and/or children (emotional deprivation schema) may feel that they are not good parents and distance themselves emotionally from their children. Parents who overly and negatively anticipate future events (negativity/pessimism schema) may rapidly become emotionally and physically exhausted, as they focus on all the possible risks and are unsuccessful in their attempts to attain their goals. Thus, EMSs, and more particularly idealized representations of parenthood (in terms of what defines the ideal parent and parental expectations), and discrepancies with self-beliefs, are potential risk factors for parental burnout.
Moreover, our results indicated that coping strategies are also associated with the expression of parental burnout. Parents who primarily resorted to emotion-focused coping also reported high levels of parental burnout. Moreover, Lebert-Charron et al.’s (2018) study of maternal burnout found that the lower the parents’ sense of efficacy (i.e., loss of parental accomplishment), the less they used problem-focused coping, and the more physically and emotionally exhausted they were, the more they resorted to emotion-focused coping. These are interesting results, as they highlight the importance of considering the different dimensions of parental burnout. Mikolajzcak and Roskam (2017) pointed out that it is not necessary to have high scores on all three dimensions to be classified as having parental burnout. It is therefore important to consider scores on the individual dimensions when adapting psychotherapy.
However and contrary to what was expected, the results of the DAG suggest that it is not because parents have activated EMSs that they use emotion coping and that they are then at potential risk of parental burnout, but that it would be because parents have activated EMSs that they are at potential risk of emotional and physical exhaustion, which in connection with a loss of personal accomplishment leads them to use emotion coping. Thus, it would be the EMS and parental burnout that would explain the use of coping, and particularly emotion-focused coping. In other words, contrary to regulation models, especially in health psychology, it is not the adjustment to a specific context (here parenthood), through the choice of emotional regulation strategies used, that would explain the differences in psychosocial consequences, but the opposite. The more burnt out the parents are, the more they try to cope with this experience by using emotion-centered regulation strategies (i.e., rumination, avoidance, denial). However, it is possible that the pattern of adjustment to EMS also plays a role in the choice of coping strategies used in the face of parental burnout. Indeed, it is possible to consider that a parent who adopts a submission style would actually use emotion-focused coping, because they feel they cannot change, whereas a parent who has adopted a compensatory adjustment pattern would possibly seek to use other coping strategies such as social support or problem-focused coping to counteract burnout and schema activation because he thinks he has control over these EMS.
Implications and Applications
The important relation between EMS activation and the expression of parental burnout allowed us to identify interesting therapeutic approaches. First, in a prevention approach, it could be interesting to communicate more about the risk of parental burnout in relation to the activation of certain beliefs. It could be proposed to parents presenting these patterns but not yet in parental burnout, a preventive accompaniment aiming at deconstructing these thoughts or giving them the resources to face them in accordance with the balance between risks and resources model (Mikolajczak & Roskam, 2018). Second, and after assessment of patterns in burnout parents, in order to verify their activation in patients, Cognitive interventions should target negative beliefs related to the self as a person and as a parent and hypersensitivity to criticism, rejection, and reprimands (related to defectiveness/shame schema). Therapists need to focus on deconstructing the unattainable parental ideal (related to the overactivation of dependence/incompetence, failure, and punitiveness schemas), in order to develop representations that are congruent with the parents’ values. This cognitive focus would improve parents’ adjustment to stressful situations and thus prevent the persistence and worsening of parental burnout. Schema therapy, which combines emotional, behavioral, cognitive, and interpersonal techniques, seems to be the best approach to associate with the above-mentioned interventions. By engaging in therapeutic work focused on schema modes and the use of flashcards, as well as structured conversations in which they argue both for and against a schema, patients learn to develop and strengthen the healthy part of their self.
Limitations and Perspectives
The present results, albeit promising, need to be interpreted with caution. Our sample size is small (especially for DAGs) with a predominantly female composition, and our results cannot be generalized. We did not take into account all the situational factors that can influence parental burnout, such as the presence of a psychiatric or physical disorder in the children or the presence of support for the parents. In addition, the measure of parental burnout is not the most current (PBI, not PBA). This lag is due to the timing of the collection of this data in 2018 and 2019. Replication studies need to be conducted with larger samples and with a longitudinal approach to confirm the direction of the relationships presented here. In addition, it would be interesting to consider more coping strategies than the three studied here. Adjustment to stress can take a variety of forms. For example, our study did not explore strategies such as positive reinterpretation, perspective-taking, and acceptance (Garnefski et al., 2002). It would be relevant to study the role of such strategies (targeting cognitive aspects) in the relationship between beliefs (schemas) and parental burnout. Finally, it would be relevant to question the pattern of adjustment to EMS that could explain inter-individual differences in the selection of strategies related to EMS activation.
Conclusion
The present study highlighted additional potential risk factors for parental burnout, in terms EMSs, and these consequences on coping. To our knowledge, it was the first to explore these relationships. Results showed that schemas in the disconnection and rejection, impaired autonomy and performance, and over-vigilance and inhibition domains play a major role in the expression of parental burnout, especially on the emotional distancing and loss of parental accomplishment dimensions. In addition, emotion-focused coping strategies are more closely related to EMSs and parental burnout than other coping strategies. Indeed, an interesting result of this study is that DAG results suggest that emotion-focused coping would be the consequence of parental burnout, more than the other way around. These results open up interesting new perspectives for future psychotherapeutic interventions.
Data Availability
The data that support the findings of this study are openly available in OSF at http://doi.org/10.17605/OSF.IO/8GEWU.
Declarations
Ethical Approval
All procedures performed in the present study complied with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from each of the participants included in the study.
Conflict of Interest
The authors declare no competing interests.
References
- Abeltina, M., & Rascevska, M. (2021). A network analysis of burnout subtypes, early maladaptive schemas and schema modes. Activitas Nervosa Superior Rediviva,63(2), 84–94. [Google Scholar]
- Aldao, A., Nolen-Hoeksema, S., & Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review,30(2), 217–237. 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- Billoux, S., Chapelle, F., Giocanti-Belmonte, C., & Callahan, S. (2012). Étude des relations entre les schémas précoces inadaptés, les stratégies de coping et la flexibilité psychologique chez des sujets présentant des troubles anxieux. Journal De Therapie Comportementale Et Cognitive,22(2), 46–52. 10.1016/j.jtcc.2012.02.001 [Google Scholar]
- Bouvard, M., Denis, A., & Roulin, J.-L. (2018). Psychometric properties of the French version of the Young schema questionnaire - short form 3 (YSQ-S3). The Spannish Journal of Psychology,27(21), E57. [DOI] [PubMed] [Google Scholar]
- Bruchon-Schweitzer, M., & Boujut, É. (2014). Psychologie de la santé (2ème édition). Dunod. [Google Scholar]
- Chen, K., Tam, W., & Chang, K. (2019). Early maladaptive schemas, depression severity, and risk factors for persistent depressive disorder: A cross-sectional study. East Asian archives of psychiatry,29(4), 112–117. 10.12809/eaapl821 [DOI] [PubMed] [Google Scholar]
- Cormier, A., Jourda, B., Laros, C., Walburg, V., & Callahan, S. (2011). L’influence entre les schémas précoces inadaptés et la dépression. Encephale,37(4), 293–298. 10.1016/j.encep.2011.01.001 [DOI] [PubMed] [Google Scholar]
- Cousson, F., Bruchon-Schweitzer, M., Quintard, B., Nuissier, J., & Rascle, N. (1996). Analyse multidimensionnelle d’une échelle de coping Validation française de la W.C.C. (Way of Coping Checklist). Psychologie française,41(2), 155–164. [Google Scholar]
- Dabrowska, A., & Pisula, E. (2010). Parenting stress and coping styles in mothers and fathers of pre-school children with autism and Down syndrome. Journal of Intellectual Disability Research,54(3), 266–280. 10.1111/j.1365-2788.2010.01258.x [DOI] [PubMed] [Google Scholar]
- Folkman, S., & Lazarus, R. S. (1980). An analysis of coping in a middle-aged community sample. Journal of Health and Social Behavior,21(3), 219–239. [PubMed] [Google Scholar]
- Friganovic, A., Selic, P., Ilic, B., & Sedic, B. (2019). Stress and burnout syndrome and their associations with coping and job satisfaction in critical care nurses: A literature review. Psychiatria Danubina,31(1), 21–31. [PubMed] [Google Scholar]
- Gallagher, B. V., & Gardner, F. L. (2007). An examination of the relationship between early maladaptive schemas, coping, and emotional response to athletic injury. Journal of Clinical Sport Psychology,1(1), 47–67. 10.1123/jcsp.1.1.47 [Google Scholar]
- Garnefski, N., Van Den Kommer, T., Kraaij, V., Teerds, J., Legerstee, J., & Onstein, E. (2002). The relationship between cognitive emotion regulation strategies and emotional problems: Comparison between a clinical and a non-clinical sample. European Journal of Personality,16(5), 403–420. 10.1002/per.458 [Google Scholar]
- Grebot, E., Berjot, S., Lesage, F. X., & Dovero, M. (2011). Schémas précoces inadaptés, activisme professionnel et épuisement professionnel chez des internes en médecine. Journal De Therapie Comportementale Et Cognitive,21(2), 43–52. 10.1016/j.jtcc.2011.04.004 [Google Scholar]
- Groth, N., Schnyder, N., Kaess, M., Markovic, A., Rietschel, L., Moser, S., Michel, C., Schultze-Lutter, F., & Schmidt, S. J. (2019). Coping as a mediator between locus of control, competence beliefs, and mental health: A systematic review and structural equation modelling meta-analysis. Behaviour Research and Therapy,121, 103442. 10.1016/j.brat.2019.103442 [DOI] [PubMed] [Google Scholar]
- Hastings, R. P., Kovshoff, H., Brown, T., Ward, N. J., Espinosa, F. D., & Remington, B. (2005). Coping strategies in mothers and fathers of preschool and school-age children with autism. Autism,9(4), 377–391. 10.1177/1362361305056078 [DOI] [PubMed] [Google Scholar]
- Hawke, L. D., & Provencher, M. D. (2011). Schema theory and schema therapy in mood and anxiety disorders: A review. Journal of Cognitive Psychotherapy,25(4), 257–276. 10.1891/0889-8391.25.4.257 [DOI] [PubMed] [Google Scholar]
- Heffer, T., & Willoughby, T. (2017). A count of coping strategies: A longitudinal study investigating an alternative method to understanding coping and adjustment. Plos One,12(10), 1–16. 10.1371/journal.pone.0186057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz, A. G., Hill, R. M., & King, C. A. (2011). Specific coping behaviors in relation to adolescent depression and suicidal ideation. Journal of Adolescence,34(5), 1077–1085. 10.1016/j.adolescence.2010.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawamoto, T., Furutani, K., & Alimardani, M. (2018). Preliminary validation of Japanese version of the parental burnout inventory and its relationship with perfectionism. Frontiers in Psychology,9, 970. 10.3389/fpsyg.2018.00970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ke, T., & Barlas, J. (2020). Thinking about feeling: Using trait emotional intelligence in understanding the associations between early maladaptive schemas and coping styles. Psychology and Psychotherapy: Theory, rResearch and Practice,93(1), 1–20. 10.1111/papt.12202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koleck, M., Bruchon-Schweitzer, M., & Bourgeois, M. L. (2003). Stress et coping: Un modèle intégratif en psychologie de la santé. Annales Medico-Psychologiques,161(10), 809–815. 10.1016/j.amp.2003.10.005 [Google Scholar]
- Lazarus, R. S., & Folkman, S. (1984). Coping and adaptation. In W. D. Gentry (Ed.), The handbook of behavioral medicine (pp. 282–325). Guilford. [Google Scholar]
- Le Vigouroux, S., & Scola, C. (2018). Differences in parental burnout : Influence of demographic factors and personality of parents and children. Frontier,9, 887. 10.3389/fpsyg.2018.00887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Vigouroux, S., Scola, C., Raes, M.-E., Mikolajczak, M., & Roskam, I. (2017). The big five personality traits and parental burnout: Protective and risk factors. Personality and Individual Differences,119, 216–219. 10.1016/j.paid.2017.07.023 [Google Scholar]
- Le Vigouroux, S., Charbonnier, E., & Scola, C. (2022). Profiles and age-related differences in the expression of the three parental burnout dimensions. European Journal of Developmental Psychology,19(6), 885–904. 10.1080/17405629.2021.1990749 [Google Scholar]
- Lebert-Charron, A., Dorard, G., Boujut, É., & Wendland, J. (2018). Maternal burnout syndrome: Contextual and psychological associated factors. Frontiers in Psychology,9, 885. 10.3389/fpsyg.2018.00885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally, R. J., Heeren, A., & Robinaugh, D. J. (2017). A Bayesian network analysis of posttraumatic stress disorder symptoms in adults reporting childhood sexual abuse. European Journal of Psychotraumatology,8, 1341276. 10.1080/20008198.2017.1341276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikolajczak, M., & Roskam, I. (2018). A theoretical and clinical framework for parental burnout: The balance between risks and resources (BR 2). Frontiers in Psychology,9, 886. 10.3389/fpsyg.2018.00886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikolajczak, M., Raes, M.-E., Avalosse, H., & Roskam, I. (2017). Exhausted parents: Sociodemographic, child-related, parent-related, parenting and family-functioning correlates of parental burnout. Journal of Child and Family Studies,26(10), 57–69. 10.1007/s10826-017-0892-4 [Google Scholar]
- Mikolajczak, M., Brianda, M.-E., Avalosse, H., & Roskam, I. (2018). Consequences of parental burnout: Its specific effect on child neglect and violence. Child Abuse and Neglect,80, 134–145. 10.1016/j.chiabu.2018.03.025 [DOI] [PubMed] [Google Scholar]
- Mikolajczak, M., Gross, J. J., & Roskam, I. (2019). Parental burnout: What is it, and why does it matter? Clinical Psychological Science,7(6), 1319–1329. 10.1177/2167702619858430 [Google Scholar]
- Mikolajczak, M., Gross, J. J., Stinglhamber, F., LindahlNorberg, A., & Roskam, I. (2020). Is Parental burnout distinct from job burnout and depressive symptoms? Clinical Psychological Science,8(4), 673–689. 10.1177/2167702620917447 [Google Scholar]
- Najmi, B., Heidari, Z., Feizi, A., Hovsepian, S., Momeni, F., & Azhar, S. M. M. (2018). Do psychological characteristics of mothers predict parenting stress? A cross-sectional study among mothers of children with different disabilities. Archives of Psychiatric Nursing,32(3), 396–402. [DOI] [PubMed] [Google Scholar]
- Nicol, A., Mak, A. S., Murray, K., Walker, I., & Buckmaster, D. (2020). The relationships between early maladaptive schemas and youth mental health: A systematic review. Cognitive Therapy and Research,44(4), 715–751. 10.1007/s10608-020-10092-6 [Google Scholar]
- Pinto-Gouveia, J., Castilho, P., Galhardo, A., & Cunha, M. (2006). Early maladaptive schemas and social phobia. Cognitive Therapy and Research,30(5), 571–584. 10.1007/s10608-006-9027-8 [Google Scholar]
- Pronost, A.-M. (2001). La prévention du burn-out et ses incidences sur les stratégies de coping. Recherche En Soins Infirmiers,67(12), 121–131. [PubMed] [Google Scholar]
- Razurel, C., Kaiser, B., Sellenet, C., & Epiney, M. (2013). Relation between perceived stress, social support, and coping strategies and maternal well-being: A review of the literature. Women & Health,53, 74–99. 10.1080/03630242.2012.732681 [DOI] [PubMed] [Google Scholar]
- Roskam, I., Raes, M.-E., & Mikolajczak, M. (2017). Exhausted parents : Development and validation of the parental burnout inventory. Frontiers in Psychology,8, 163. 10.3389/fpsyg.2017.00163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roskam, I., Aguiar, J., Akgun, E., Arikan, G., Artavia, M., & Avalosse, H. (2021). Parental burnout around the globe : A 42-country study. Affective Science,2, 58–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez-Rodríguez, R., Perier, S., Callahan, S., & Séjourné, N. (2019). Revue de la littérature relative au burnout parental. Canadian Psychology,60(2), 77–89. 10.1037/cap0000168 [Google Scholar]
- Scutari, M. (2010). Learning Bayesian networks with the bnlearn R Package. Journal of Statistical Software,35(3), 1–22.21603108 [Google Scholar]
- Scutari, M., & Nagarajan, R. (2013). Identifying significant edges in graphical models of molecular networks. Artificial Intelligence in Medicine,57(3), 207–217. 10.1016/j.artmed.2012.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson, S., Simionato, G., Smout, M., van Vreeswijk, M. F., Hayes, C., Sougleris, C., & Reid, C. (2019). Burnout amongst clinical and counselling psychologist: The role of early maladaptive schemas and coping modes as vulnerability factors. Clinical Psychology and Psychotherapy,26(1), 35–46. 10.1002/cpp.2328 [DOI] [PubMed] [Google Scholar]
- Sorkkila, M., & Aunola, K. (2020). Risk factors for parental burnout among Finnish parents: The role of socially prescribed perfectionism. Journal of Child and Family Studies,29(3), 648–659. 10.1007/s10826-019-01607-1 [Google Scholar]
- Tariq, A., Quayle, E., Lawrie, S. M., Reid, C., & Chan, S. W. Y. (2021). Relationship between early maladaptive schemas and anxiety in adolescence and young adulthood: A systematic review and meta-analysis. Journal of Affective Disorders,295, 1462–1473. 10.1016/j.jad.2021.09.031 [DOI] [PubMed] [Google Scholar]
- Thompson, R. J., Mata, J., Jaeggi, S. M., & Buschkuehl, M. (2010). Maladaptive coping, adaptive coping, and depressive symptoms. Behaviour Research and Therapy,48(6), 459–466. 10.1016/j.brat.2010.01.007.Maladaptive [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Bakel, H., Bastiaansen, C., Hall, R., Schwabe, I., Verspeek, E., Gross, J. J., Brandt, J. A., Aguiar, J., Akgun, E., Arikan, G., Beyers, W., Zuzana, B., Andres, R., & Lasso, B. (2022). Parental burnout across the globe during the COVID-19 pandemic. International Perspectives in Psychology,11(3), 141–152. [Google Scholar]
- van Wijk-Herbrink, M. F., Bernstein, D. P., Broers, N. J., Roelofs, J., Rijkeboer, M. M., & Arntz, A. (2018). Internalizing and externalizing behaviors share a common predictor: The effects of early maladaptive schemas are mediated by coping responses and schema modes. Journal of Abnormal Child Psychology,46, 907–920. 10.1007/s10802-017-0386-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walburg, V., Paez, J., Henini, N., & Leroux, D. (2008). Comparison of early maladaptive schemas among students between the beginning and the end of university studies. Journal De Thérapie Comportementale Et Cognitive,18, 53–56. [Google Scholar]
- Zadahmad, M., & Torkan, H. (2016). Investigation of the multiple relationships between early maladaptive schemas and coping styles with anxiety. International Journal of Educational and Psychological Researches,2(1), 49. 10.4103/2395-2296.174791 [Google Scholar]
- Young, J. E., Weinberger, A. D., & Beck, A. T. (2001). Cognitive therapy for depression. In D. H. Barlow (Ed.), Clinical handbook of psychological disorders. Guilford Press.
- Young, J. E., Klosko, J. S., & Weishaar, M. E. (2017). La thérapie des schémas : Approche cognitive des troubles de la personnalité (2ème éditi). De Boeck Supérieur.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are openly available in OSF at http://doi.org/10.17605/OSF.IO/8GEWU.