Background:
Patients with COVID-19 will experience high levels of anxiety and depression and poor levels of sleep and quality of life (QoL) due to isolation treatment and uncertain outcomes. Progressive muscle relaxation (PMR) exercises show promising treatment effects on mental health and sleep problems and overall QoL in COVID-19 patients. This study aimed to evaluate the efficacy and safety of PMR exercises in patients with COVID-19.
Methods:
Both experimental and non-experimental studies related to PMR and COVID-19 were systematically searched in the PubMed, Cochrane Library, PEDro and HINARI databases for studies published from the occurrence of the pandemic to December 2022. Study selection, methodological quality assessment and data extraction were carried out by 2 independent authors. Efficacy outcomes were evaluated for sleep quality, anxiety, depression, and QoL. The safety outcomes were evaluated based on adverse events reported. Review manager (RevMan 5.4, Cochrane collaboration) was used for the data analysis.
Results:
Four studies with 227 subjects were included in this systematic review. The pooled results indicated that PMR interventions improved the sleep quality score standardized mean difference (SMD): −0.23; 95% confidence interval (CI): −0.54, 0.07; P = .13, level of anxiety SMD: −1.35; 95% CI −2.38, −0.32; P = .01 compared to the usual care. Depression level, disease severity and QoL were also improved following PMR interventions. Only 1 study reported worsening of 1 patient clinical status while all other studies did not report any adverse events during the interventions.
Conclusions:
PMR interventions can improve the sleep quality, anxiety, depression, disease severity and QoL in patients with mild to moderate COVID-19 in a short-term period compared to the usual care. However, there was indecision about the safety and long-term effects of PMR.
Keywords: COVID-19, meta-analysis, progressive muscle relaxation, systematic review
1. Introduction
Individuals who have infected and/or recovered from COVID-19 frequently experienced mental health problems. During COVID-19 pandemic the prevalence of depression, anxiety, distress, and insomnia was 31.4%, 31.9%, 41.1%, and 37.9%, respectively, with higher risk of depression and anxiety among COVID-19 patients.[1] Interventions focused on alleviation of anxiety, depression, sleep problems and post-traumatic stress disorder symptoms directly or indirectly are recommended to advance the mental well-being of this population.[2,3] Progressive muscle relaxation (PMR) is a relaxation technique which is based on the sequential contraction and relaxation of different group of muscles along with deep breathing, until the whole body is further relaxed. It is a mind-body relaxation approach. PMR was first developed by Edmund Jacobson in 1938.[4] The original Jacobson method includes many sessions intended for relaxing 30 different muscle groups in the patient body and various brief versions have been developed so far.[4,5] Relaxation exercises includes the maximal contraction of the muscle groups of the face, neck, shoulder, arm, forearm, back, abdomen, hip, femur, leg, and foot.[6] PMR has been shown to decrease anxiety and stress and improve sleep quality by reducing the activity of the sympathetic nervous system, which in turn increases the physical and mental relaxation.[7]
The existing literatures have demonstrated emotional and physical benefits of PMR interventions in a variety of ill and healthy populations. Compared to control group, PMR has been more effective in improving anxiety, vomiting, nausea and pain in patients with cancer.[5,8,9] Progressive relaxation exercises were found to be effective in improving dyspnea, fatigue, sleep problems and quality of life (QoL) in patients with moderate and advanced chronic obstructive pulmonary disease.[6,10,11] There is evidence that muscular relaxation improves lung function in patients with asthma, anxiety, fatigue and sleep quality in patients undergoing hemodialysis and sleep quality and QoL in patients who underwent pulmonary resection.[6,12–14] It was also possible to identify PMR intervention studies during COVID-19 pandemic that focused on women during pregnancy, healthcare workers and nurses and presented satisfactory results in minimizing stress levels, anxiety and sleep quality.[15–17]
Many experimental, quasi-experimental and observational studies have evaluated the effect of PMR exercises in patients with COVID-19.[18–24] However, no systematic reviews have summarized the characteristics, efficacy, and safety of PMR exercises in COVID-19 patients. Therefore, this study aimed to comprehensively evaluate the efficacy and safety of PMR exercises in patients with COVID-19. In this study, we included articles addressing PMR exercises in patients with mild to moderate COVID-19 disease to provide concrete evidence on their use in the recovery of patients with COVID-19.
2. Methods and materials
This study was carried out according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses and was registered in the International Prospective Register of Systematic Reviews (PROSPERO) CRD42022372366.
2.1. Search strategy
The PubMed, Cochrane Library, PEDro and HINARI electronic databases were searched from the occurrence of the pandemic to December, 2022. Multiple combinations of the following search terms were used: “progressive muscle relaxation,” “progressive relaxation,” “autogenic training,” “relaxation,” “COVID-19,” “coronavirus disease 2019,” “SARS-CoV-2 infection,” “severe acute respiratory syndrome coronavirus 2 infection” and “COVID-19 pandemic.” The detailed search strategy of PubMed database was described in Table 1. Furthermore, we manually searched the reference lists of eligible studies to identify additional relevant studies.
Table 1.
PubMed search strategy.
| Search number | Search detail |
|---|---|
| #1 | “COVID 19”[MeSH Terms] |
| #2 | “muscle relaxation”[MeSH Terms] |
| #3 | “COVID-19”[Title/Abstract] OR “2019 novel coronavirus disease”[Title/Abstract] OR “2019 novel coronavirus infection”[Title/Abstract] OR “2019 ncov disease”[Title/Abstract] OR “2019 ncov infection”[Title/Abstract] OR “covid 19 pandemic”[Title/Abstract] OR “covid 19 pandemics”[Title/Abstract] OR “covid 19 virus disease”[Title/Abstract] OR “covid 19 virus infection”[Title/Abstract] OR “COVID19”[Title/Abstract] OR “coronavirus disease 2019”[Title/Abstract] OR “coronavirus disease 19”[Title/Abstract] |
| #4 | “progressive muscle relaxation”[Title/Abstract] OR “progressive relaxation”[Title/Abstract] OR “autogenic training”[Title/Abstract] OR “relaxation”[Title/Abstract] OR “muscle relaxation”[Title/Abstract] |
| #5 | #1 AND #2 |
| #6 | #3 AND #4 |
| #7 | #5 OR #6 |
2.2. Study selection criteria
Two independent authors selected studies based on the pre-defined set of criteria. Any disagreement during the screening process was resolved through discussion between the 2 authors. If there was still no agreement, a third independent author decided after group discussion. All potentially eligible studies were screened following the pre-established criteria. All experimental, quasi experimental and observational studies focusing on PMR exercise interventions in mild to moderate COVID-19 patients were considered eligible. The exclusion criteria were case report, conference abstract, or review article, not published in English, and absence of adequate information to be extracted.
2.3. Data extraction
Two authors completed the data extraction independently on a standardized data extraction sheet. The extracted data included the first author name, publication year, sample size, study design, characteristics of the participants (age), interventions, and outcome measures. We tried to contact the corresponding author when relevant data were missed. If there was a disagreement between the review authors, it was resolved by consultation with a third independent author.
2.4. Methodological quality assessment
The methodological quality of the included studies was assessed using Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument (JBI SUMARI) tool based on the nature of the studies. The tool contains different checklists for Randomized Controlled Trials (RCTs), cohort (observational) studies. We used the appropriate type of tool for each eligible study.
2.5. Outcome measures
Efficacy outcomes were evaluated for sleep quality, level of anxiety, depression, and QoL scores. Safety outcomes were evaluated based on adverse events reported in the studies.
2.6. Statistical analysis
Review manager (RevMan 5.4, Cochrane collaboration) software was used to conduct the meta-analysis. Standardized mean difference (SMD) with 95% confidence interval (CI) and the corresponding P value were used to determine the treatment effect between groups. Heterogeneity was assessed using the I2 test. When I2 > 0.5 or P < .1, it is considered that there is significant heterogeneity among studies, and a random-effect model was used. Where statistical pooling is not possible, the findings were presented in narrative form including tables to aid in data presentation where appropriate.
Patient and public involvement: No patient or public were involved in this study.
3. Results
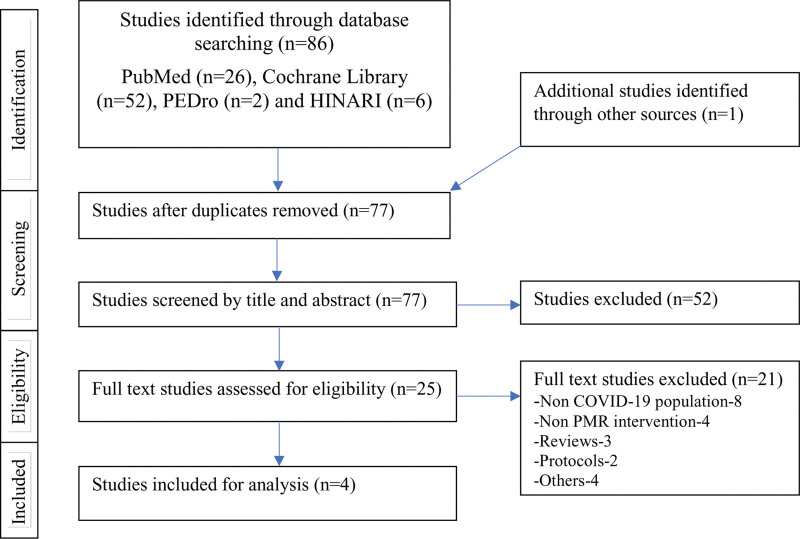
In total, 86 records were identified from the 4 databases. After removing duplicates 77 records were screened by title and abstract and 52 studies were excluded. Studies have been excluded if the title and/or abstract is unrelated to our study or if the study does not meet the inclusion criteria. The remaining 25 full text articles were eligible for detailed assessment. From these 21 articles were excluded and only 4 studies were considered eligible for the final systematic review[18,19,21,23] (Fig. 1).
Figure 1.
PRISMA flow chart. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
3.1. Study characteristics
Table 2 summarizes the main clinical characteristics and outcomes of the included studies. Three RCTs and 1 clinical observational study with 227 participants diagnosed with COVID-19 were included. The mean age of the participants ranged from 33.45 to 59.33 years. The duration of the PMR interventions ranged from 5 days to 2 weeks. The control group of the included studies received the usual care. Three studies reported anxiety and sleep related outcomes.[19,21,23] One study reported blood immune markers, salivary immunoglobulin A & QoL.[18] Only 1 study reported depression related outcome.[23] One study reported follow up data after 1 week of treatment completion.[18] From the 4 studies individual report PMRs were effective in reducing anxiety, depression, sleep problems, disease severity and improving QoL.
Table 2.
Characteristics and outcomes of the included studies.
| Author (yr) | N | Age (mean ± SD) | Design | Intervention | Outcome measures | Control (pre/post) | Intervention (pre/post) | Result | |
|---|---|---|---|---|---|---|---|---|---|
| Alawna A (2022) | IG = 15 CG = 15 |
IG = 37.56 ± 3.25 CG = 33.45 ± 3.96 |
RCT | IG = CBSM and PMR for 2 wk. CG = No relaxation techniques |
Blood immune markers, Salivary immunoglobulin A & Quality of life | Wisconsin Scale | 110.3 ± 5.64 104.27 ± 5.85 |
106.73 ± 5.42 91.27 ± 4.73 | PMR significantly increased immune biomarkers mainly Leucocytes, Lymphocytes, Interleukin-10, & Interleukin-6 along with S-IgA and enhanced quality of life. |
| Leucocytes | 5.26 ± 1.37 5.84 ± 1.43 |
5.46 ± 1.30 7.38 ± 1.43 |
|||||||
| Lymphocytes | 0.93 ± 0.31 1.29 ± 0.23 |
0.93 ± 0.30 2.09 ± 0.21 |
|||||||
| Inter-6 | 22.73 ± 11.53 23.01 ± 11.45 | 23.01 ± 11.60 26.90 ± 11.83 |
|||||||
| Inter-10 | 6.16 ± 1.15 6.31 ± 1.169 |
6.17 ± 1.11 7.05 ± 1.055 |
|||||||
| IgA | 2.20 ± 0.37 2.39 ± 0.51 |
2.32 ± 0.39 3.42 ± 0.34 |
|||||||
| TNF-α | 10.23 ± 0.79 10.23 ± 0.79 |
10.57 ± 0.56 10.57 ± 0.56 |
|||||||
| Özlü I (2021) | IG = 33 CG = 34 |
IG = 36.48 ± 11.63 CG = 33.15 ± 11.90 |
RCT | IG = PMR exercises performed twice a day for 5 d. CG = Routine care. |
Anxiety and Sleep | State Anxiety Scale | 60.68 ± 9.17 61.29 ± 7.95 |
62.33 ± 8.33 44.67 ± 5.41 |
PMR exercises effectively reduced the anxiety & improved the sleep quality of patients with COVID-19. |
| Trait Anxiety Scale | 45.35 ± 8.09 *** |
48.12 ± 5.22 *** |
|||||||
| RCSQ | *** 46.71 ± 19.71 |
*** 68.33 ± 14.53 |
|||||||
| Liu K (2020) | IG = 25 CG = 26 |
50.41 ± 13.04 (overall) | RCT | IG = PMR for 30 min per d for 5 d. CG = Routine care |
Anxiety and Sleep | STAI | 56.92 ± 7.92 57.15 ± 9.24 |
57.88 ± 11.51 44.96 ± 12.68 |
PMR improve sleep quality & reduce anxiety in COVID-19 patients. |
| SRSS | 23.85 ± 2.82 23.23 ± 2.70 |
24.04 ± 3.87 16.76 ± 4.10 |
|||||||
| Xiao CX (2020) | IG = 39 CG = 40 |
IG = 58.45 ± 11.08 CG = 59.33 ± 12.19 |
Clinical observational study | IG = PMR for 30 minutes twice a day for 1 wk duration. CG = Routine care |
Anxiety, Depression and Sleep | GAD-7 | 5.72 ± 3.71 5.77 ± 3.72 |
5.38 ± 5.25 3.69 ± 2.99 |
PMR training can significantly reduce anxiety and depression and improve sleep quality in COVID-19 patients. |
| PHQ-9 | 5.20 ± 2.88 6.02 ± 3.74 |
5.05 ± 4.86 3.69 ± 3.93 |
|||||||
| PSQI | 10.08 ± 5.43 9.72 ± 5.08 |
10.25 ± 2.75 7.41 ± 2.42 |
CBSM = cognitive-behavioral stress management, CG = control group, GAD = generalized anxiety disorder, IG = intervention group, PHQ = patient health questionnaire, PMR = progressive muscle relaxation, PSQI = Pittsburgh Sleep Quality Index Scale, RCSQ = Richards–Campbell sleep questionnaire, RCT = randomized controlled trial, SRSS = Sleep State Self-Rating Scale, STAI = state-trait anxiety scale.
3.2. Results from quality assessments
The quality assessment result of the included studies using the JBI Critical Appraisal tools for the RCTs and cohort study were summarized in Table 3. The Critical Appraisal Tool for RCTs consists of 13 checklists developed by the JBI and collaborators.[25] The JBI Cohort Studies Critical Appraisal Tool also contains 11 checklists for the assessment of cohort studies.[26]
Table 3.
Quality analysis using Joanna Briggs Institute critical appraisal tools.
| JBI critical appraisal checklist for RCTs | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Total |
| Alawna A (2022) | Y | U | Y | Y | U | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Özlü I (2021) | U | N | Y | U | N | N | Y | Y | U | Y | Y | Y | Y | 7 |
| Liu K (2020) | U | N | Y | U | N | N | Y | Y | U | Y | Y | Y | Y | 7 |
| JBI critical appraisal checklist for cohort studies | ||||||||||||||
| Xiao CX (2020) | Y | U | Y | U | U | Y | Y | Y | Y | Y | Y | -- | -- | 8 |
N = no, N/A = not applicable, U = unclear, Y = yes.
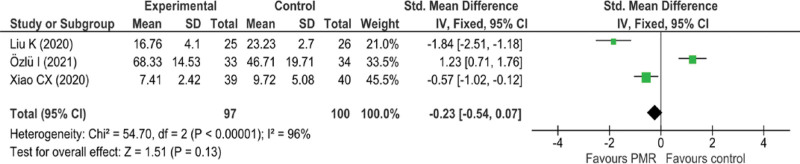
3.3. Effect of PMR on sleep quality
Three studies with 197 subjects[19,21,23] reported sleep quality using different tools. A meta-analysis of post intervention results showed that PMR had improved sleep quality compared to the control group (SMD: −0.23; 95% CI: −0.54, 0.07; P = .13) (Fig. 2).
Figure 2.
The effect of PMR on sleep quality. PMR = progressive muscle relaxation.
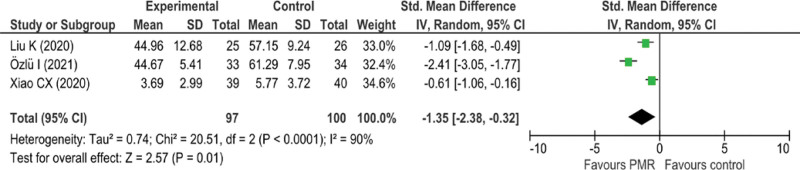
3.4. Effect of PMR on level of anxiety
Three studies of 197 subjects reported level of anxiety. Two studies used State-Trait Anxiety Scale[19,21] and 1 study used Generalized Anxiety Disorder (7) scale.[23] Due to the high heterogeneity (I² = 90%, P < .001), a random effects model was used in the meta-analysis (Fig. 3). The pooled results indicated that PMR had significantly reduced anxiety compared to control group (SMD: −1.35; 95% CI −2.38, −0.32; P = .01).
Figure 3.
The effect of PMR on level of anxiety. PMR = progressive muscle relaxation.
3.5. Effect of PMR on level of depression
Only 1 observational study with 79 participants reported about the effect of PMR on level of depression.[23] Accordingly, no meaningful meta-analysis was performed. But the result highlighted that after PMR a 1.36 ± 4.43 points reduction was observed, which suggests that PMR can improve depression in COVID-19 patients.
3.6. Effect of PMR on QoL
Only 1 RCT study with 30 participants reported about QoL following PMR interventions.[18] The Wisconsin Upper Respiratory Symptom Survey which is used evaluate the negative effect of acute upper respiratory infection on the QoL was reported. The result showed a 15.46 ± 7.19 points reduction following PMR intervention in the experimental group.
3.7. Adverse events
Only 1 study reported worsening of 1 patients clinical status from the control group,[19] while all other studies did not report any information about adverse events during the study period.
4. Discussion
The aim of this systematic review and meta-analysis was to summarize the current evidence about the efficacy and safety of PMR for patients with mild to moderate COVID-19 disease. The results of this study indicated that PMR can improve the sleep quality, anxiety, depression, and QoL in patients with COVID-19 compared to usual care interventions. Importantly, the study also considered another important factor applied to patients with COVID-19: the safety of PMR. Only 1 study from the included studies reported worsening of 1 patient clinical status during intervention. Therefore, the evidence is not yet sufficient to draw firm conclusions about the safety of PMR for patients with COVID-19. More research is required in the future to investigate the safety of PMR for patients with COVID-19.
A systematic review and a meta-analysis of 25 RCTs aimed to evaluate the effectiveness of relaxation techniques on pulmonary function, anxiety, depression, and QoL for people with chronic obstructive pulmonary disease reported that relaxation techniques have little positive effects on pulmonary function, anxiety and depression. On the other hand, relaxation techniques have higher effect on QoL. This might be due to the presence of high heterogeneity between studies and limited number of studies.[27] Another literature review focused on the effect of PMR on sleep quality among chronic disease patients reported that PMR significantly improves the sleep quality among patients with chronic diseases.[28]
A rapid review on home-based activities that have potential beneficial effects on mental health have reported that exercise, yoga, PMR, and listening to relaxing music have beneficial effects on mental health.[7] A scoping review on mental health interventions implemented on COVID-19 patients revealed that telemonitoring, virtual games and strategies focused on social support and muscle relaxation techniques were shown as effective interventions.[29] Another scoping review of 11 studies with 828 patients aimed to examine the current state and findings of mental health treatment research for depression and/or suicidality in COVID-19 patients reported that Cognitive Behavioral Therapy, yoga, muscle relaxation, and mindfulness were the most common used techniques.[2] The findings were promising regarding the immediate effectiveness of mental health treatments and the use of tele-health as a treatment modality for COVID-19 patients.
Public health measures imposed to reduce the pandemic transmission such as isolation, quarantine, and social distancing leads to mental health problems like anxiety and depression.
It is obvious that healthcare professionals were also susceptible to mental health problems like anxiety, depression and insomnia. Rehabilitation programs for COVID-19 patients should be designed to address pulmonary functions, physical functions and psychological health such as anxiety, depression, sleep problems.[30] PMR is a noninvasive, affordable, effective, and easy technique to implement during the hospitalization period starting from the intensive care phase. Therefore, it is worthy to incorporate PMR techniques in the rehabilitation of COVID-19 patients to relieve physical and psychological symptoms.
This study had several limitations. First, the studies included in this systematic review were few in number, heterogeneous with respect to the design and programs of PMR intervention. Second, all studies except 1 reported only short-term follow-up period, <2 weeks duration, so this systematic review only examined the short-term effects of the PMR in mild to moderate severity COVID-19 patients. Therefore, the long-term effects are still unclear. Third, all eligible studies were published in English, and it is obvious that relevant studies published in other languages have been omitted, resulting in a language bias.
5. Conclusion
PMR interventions can improve the sleep quality, anxiety, depression, disease severity and QoL in patients with mild to moderate COVID-19 in a short-term period compared to the usual care. Advancing and integrating the development of PMR in clinical practice is an initiative that might benefit more patients with COVID-19. However, there was uncertainty about the safety of PMR, so rigorously designed high quality trials are needed in the future to verify the safety of PMR in COVID-19 patients including long term effectiveness.
Author contributions
Conceptualization: Abubeker Alebachew Seid.
Data curation: Abubeker Alebachew Seid, Aragaw Asfaw Hasen.
Formal analysis: Abubeker Alebachew Seid, Ahmed Adem Mohammed, Aragaw Asfaw Hasen.
Methodology: Abubeker Alebachew Seid, Ahmed Adem Mohammed, Aragaw Asfaw Hasen.
Software: Abubeker Alebachew Seid, Aragaw Asfaw Hasen.
Writing – original draft: Abubeker Alebachew Seid, Ahmed Adem Mohammed, Aragaw Asfaw Hasen.
Writing – review & editing: Abubeker Alebachew Seid, Ahmed Adem Mohammed, Aragaw Asfaw Hasen.
Abbreviations:
- CI
- confidence interval
- JBI
- Joanna Briggs Institute
- PMR
- progressive muscle relaxation
- QoL
- quality of life
- RCT
- randomized controlled trial
- SMD
- standardized mean difference
The authors have no funding and conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
How to cite this article: Seid AA, Mohammed AA, Hasen AA. Progressive muscle relaxation exercises in patients with COVID-19: Systematic review and meta-analysis. Medicine 2023;102:14(e33464).
Contributor Information
Ahmed Adem Mohammed, Email: ahmedhuda02@gmail.com.
Aragaw Asfaw Hasen, Email: aragawasfaw5@gmail.com.
References
- [1].Wu T, Jia X, Shi H, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021;281:91–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Chennapragada L, Sullivan SR, Hamerling-Potts KK, et al. International PRISMA scoping review to understand mental health interventions for depression in COVID-19 patients. Psychiatry Res. 2022;316:114748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Dai Z, Wang H, Xiao W, et al. The association of mindfulness and psychological well-being among individuals who have recovered from COVID-19 in Jianghan District, Wuhan, China: a cross-sectional study. J Affect Disord. 2022;319:437–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Jacobson E. A Physiological and Clinical Investigation of Muscular States and their Significance in Psychology and Medical Practice. Chicago: University of Chicago Press; 1938. [Google Scholar]
- [5].Alhawatmeh H, Albataineh R, Abuhammad S. Differential effects of guided imagery and progressive muscle relaxation on physical and emotional symptoms in nursing students taking initial clinical training: a randomized clinical trial. Heliyon. 2022;8:e11147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Aksu NT, Erdogan A, Ozgur N. Effects of progressive muscle relaxation training on sleep and quality of life in patients with pulmonary resection. Sleep Breath. 2018;22:695–702. [DOI] [PubMed] [Google Scholar]
- [7].Puyat JH, Ahmad H, Avina-Galindo AM, et al. A rapid review of home-based activities that can promote mental wellness during the COVID-19 pandemic. PLoS One. 2020;15:e0243125e0243125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Gupta B, Kumari M, Kaur T. Effectiveness of progressive muscle relaxation technique on physical symptoms among patients receiving chemotherapy. Nurs Midw Res J. 2016;12:33–40. [Google Scholar]
- [9].Pradhan J, Pradhan R, Samantaray K, et al. Progressive muscle relaxation therapy on anxiety among hospitalized cancer patients. Eur J Mol Clin Med. 2020;7:1485–8. [Google Scholar]
- [10].Akgün Şahin Z, Dayapoğlu N. Effect of progressive relaxation exercises on fatigue and sleep quality in patients with chronic obstructive lung disease (COPD). Complement Ther Clin Pract. 2015;21:277–81. [DOI] [PubMed] [Google Scholar]
- [11].Yilmaz CK, Kapucu S. The effect of progressive relaxation exercises on fatigue and sleep quality in individuals with COPD. Holist Nurs Pract. 2017;31:369–77. [DOI] [PubMed] [Google Scholar]
- [12].Saeedi M, Ashktorab T, Saatchi K, et al. The effect of progressive muscle relaxation on sleep quality of patients undergoing hemodialysis. Iran J Crit Care Nurs. 2012;5:23–8. [Google Scholar]
- [13].Huntley A, White AR, Ernst E. Relaxation therapies for asthma: a systematic review. Thorax. 2002;57:127–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Amini E, Goudarzi I, Masoudi R, et al. Effect of progressive muscle relaxation and aerobic exercise on anxiety, sleep quality, and fatigue in patients with chronic renal failure undergoing hemodialysis. Int J Pharm Clin Res. 2016;8:1634–9. [Google Scholar]
- [15].Zendehdel M, Elyasi F, Jahanfar S, et al. Effectiveness of progressive muscle relaxation technique on anxiety caused by Covid-19 in pregnant women: a randomized clinical trial. Neuropsychopharmacol Rep. 2022;42:158–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Yolanda Y, Said I, Suryati T, et al. The effects of progressive muscle relaxation on the level of anxiety in nurses caring for patients with COVID-19. Indonesian Contemp Nurs J. 2022;7:16–24. [Google Scholar]
- [17].Khoirunnisa ML, Putu Putri Ariani GA. Effects of progressive muscle relaxation on anxiety of nurses at covid-19 units. Jurnal Aisyah: Jurnal Ilmu Kesehatan. 2021;6:59–64. [Google Scholar]
- [18].Alawna M, Mohamed A. An integrated intervention combining cognitive-behavioural stress management and progressive muscle relaxation improves immune biomarkers and reduces COVID-19 severity and progression in patients with COVID-19: a randomized control trial. Stress Health. 2022;38:978–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ozlu I, Ozturk Z, Karaman Ozlu Z, et al. The effects of progressive muscle relaxation exercises on the anxiety and sleep quality of patients with COVID-19: a randomized controlled study. Perspect Psychiatr Care. 2021;57:1791–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].GhasemKhanloo A, Sabri V. The effect of progressive muscle relaxation on quality of life and pain intensity in patients with COVID-19 in 2021. Tolooebehdasht J. 2022;21:1–13. [Google Scholar]
- [21].Liu K, Chen Y, Wu D, et al. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement Ther Clin Pract. 2020;39:101132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Herdiman, Fauzi DH, Lindayani L. The effect of progressive muscle relaxation on anxiety in covid-19 patients in bandung. Jurnal Keperawatan Komprehensif. 2022;8:182–7. [Google Scholar]
- [23].Xiao CX, Lin YJ, Lin RQ, et al. Effects of progressive muscle relaxation training on negative emotions and sleep quality in COVID-19 patients: a clinical observational study. Medicine (Baltim). 2020;99:e23185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hegazy ESA, Mahmoud SA, Mohammed E, et al. Effect of mothers’ implementing progressive muscle relaxation technique on anxiety and sleep quality among children with Covid-19. Port Said Sci J Nurs. 2021;8:126–48. [Google Scholar]
- [25].Tufanaru C, Munn Z, Aromataris E, et al. Chapter 3: systematic reviews of effectiveness. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. 2020 edition. JBI: Adelaide, SA; 2020. Available at: https://synthesismanual.jbi.global. [Google Scholar]
- [26].Moola S, Munn Z, Tufanaru C, et al. Chapter 7: systematic reviews of etiology and risk. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. 2020 edition. JBI: Adelaide, SA; 2020. Available at: https://synthesismanual.jbi.global. [Google Scholar]
- [27].Volpato E, Banfi P, Rogers SM, et al. Relaxation techniques for people with chronic obstructive pulmonary disease: a systematic review and a meta-analysis. Evid Based Complement Alternat Med. 2015;2015:628365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Mirzanah S, Yona S, Dahlia D. Effect of progressive muscle relaxation on sleep quality among patients with chronic diseases: a literature review. Belitung Nurs J. 2020;6:30–4. [Google Scholar]
- [29].Moreira WC, Sousa KHJF, Sousa AR, et al. Mental health interventions implemented in the COVID-19 pandemic: what is the evidence? Rev Bras Enferm. 2021;74(suppl 1):e20200635. [DOI] [PubMed] [Google Scholar]
- [30].Demeco A, Marotta N, Barletta M, et al. Rehabilitation of patients post-COVID-19 infection: a literature review. J Int Med Res. 2020;48:300060520948382. [DOI] [PMC free article] [PubMed] [Google Scholar]