Abstract
The COVID-19 pandemic is a major health care catastrophe that affects people’s physical and mental well-being worldwide. Medical students are at an increased risk of mental health hazards during the COVID-19 pandemic. Sulaiman Al Rajhi University (SRU), the site of our study, is located in Qassim province in the Kingdom of Saudi Arabia. We conducted this study to assess the prevalence of depression, stress and anxiety symptoms among SRU medical students during the quarantine and while learning online shortly after the announcement of documented COVID-19 cases in Kingdom of Saudi Arabia. In this cross-sectional study, an online questionnaire was sent to all medical students of SRU; 278 students responded (71%). We collected participants’ demographic, socioeconomic, and academic data. The Depression, Anxiety, and Stress scale and the Fear of COVID-19 Scale were used as the validated mental health assessment tools. Depression, anxiety and stress symptoms were found in 23%, 11%, and 6% of students, respectively. Females were more likely to have anxiety (P = .03) than males. Students who had close contact with COVID-19 cases, those whose lives were affected by COVID-19, and those with poor socioeconomic status had significantly higher levels of stress, anxiety, and depression compared to their counterparts (P = .004, .01, .01, respectively). Students from high-viral-load areas, unmarried students, and those who did not live with their families were more stressed (P = .06, .01, .01, respectively). The Fear of COVID-19 Scale was positively correlated with all Depression, Anxiety, and Stress components (depression: r = 0.36, anxiety: r = 0.45, and stress: r = 0.39, P < .001 for all). Medical students, especially female students, are at an increased risk of developing depression, anxiety, and stress symptoms with increased COVID-19 fear during the pandemic. The study highlights the importance of mental health screening for female students, students of low socioeconomic status, and relatives of COVID-19 cases. Our findings could help institutions adjust mental health services in the future amid such pandemics.
Keywords: COVID-19, medical students, mental health, psychological status, public health
1. Introduction
COVID-19 emerged in Wuhan City, China, in December 2019 and has been spreading across the globe.[1] It has been an intense challenge for mankind with devastating consequences. As of July 2022, there were 557,917,904 confirmed cases with 6358,899 deaths, and the numbers are still rising.[2] The Kingdom of Saudi Arabia (KSA), with its previous infection control experience from the 2012 MERS-CoV outbreak, has successfully taken steps to curb the dangers of COVID-19.[3]
It is currently well established that COVID-19 has both short- and long-term effects on the mental and physical health of the population.[4] From a mental health point of view, the COVID-19 pandemic created instability for many individuals worldwide, and consequently, had a negative impact on their general psychological health, especially among vulnerable members of the population. Social isolation, quarantine durations, economic changes, fear of infection, and uncertainty about the future all played a part.[5]
Several studies have investigated the psychological consequences of COVID-19 on the general population worldwide, including KSA.[6,7] In Saudi-based studies, moderate to severe depressive symptoms were reported in 17.1% to 28.3% of the study populations; 10% to 24% of participants reported moderate to severe anxiety symptoms, and 12% to 22.3% reported moderate to severe stress levels.[6,8]
Healthcare workers are more prone to mental health problems than the general population due to their occupational exposure and stressful work conditions in the emergency subspecialties.[9,10] Hence, it is of utmost importance to identify any deviation in the mental health of medical students, our future healthcare workers. Early identification during their undergraduate years will help avoid any future occupational hazards.
The literature has shown that students in general are at an increased risk of mental health issues due to their challenging and competitive study goals.[11] Medical students in particular are at higher risk for depression, anxiety and stress due to the huge study load, multiple assessments, lengthy and costly study programs, and possible contact with COVID-19 cases during hospital training.[12,13]
The literature prior to the COVID-19 pandemic demonstrated increased psychological hazards for medical students; the global anxiety prevalence rate for medical students was 33.8%,[14] and the global depression prevalence rate was 28.0%.[15] However, there is wide variability in the literature regarding fear perceptions, prevalence, and factors affecting depression, anxiety, and stress among medical students amid the COVID-19 pandemic.[13,16]
Accordingly, we aimed to further explore this issue among a sample of medical students in Saudi Arabia amid the COVID-19 pandemic. The study results could shed light on the mental health status of medical students in KSA as a crucial step in their preparation to become future frontline healthcare professionals.
2. Methods
2.1. Study design and participants
This cross-sectional study was approved by the Subcommittee of Health Research Ethics, through the Deanship of Scientific Research at Qassim University (reference number 19-11-13). All participants provided electronic informed consent in the first section of the online survey prior to completing the questionnaire.
We aimed to recruit all medical students in the College of Medicine at Sulaiman Al Rajhi University (SRU) using a population-targeted approach. An online self-administered dual-language (English and Arabic) survey was sent to all SRU medical students via their official email addresses. A total of 278 out of 389 medical students responded (response rate of 71.46%). Data were collected from June 2 to June 23, 2020. This period coincided with the peak of COVID-19 cases in KSA and during the quarantine, restrictions, and total online learning.
2.2. Measurements
The questionnaire (see Supplemental Digital Content, http://links.lww.com/MD/I773) consisted of the following 3 domains:
The sociodemographic variables: age, gender, residence, habitat, study level, marital status, any confirmed case of COVID-19 among relatives or neighborhood, and presence of any healthcare workers in the family. We combined study levels 1 and 2 as pre-clinical, while study levels 3 and above were clinical. The COVID-19 pandemic effect was assessed using a 4-point Likert scale (not affected, slightly affected, moderately affected, and heavily affected); we categorized “life affected by COVID-19” responses into not/slightly affected and moderately/heavily affected groups. Socioeconomic status was assessed using a 4-point Likert scale (quite poor, not well off, quite well off, wealthy); we combined “quite poor” and “not well off” into the poor group, while “quite well off” and “wealthy” were combined as the rich group. The current places of residence were divided into high-viral-load areas (Riyadh, Makkah, and Madinah) and low-viral-load areas (the other ten provinces of Saudi Arabia). High-viral-load areas were provinces that were subjected to strict public health measures (i.e., 24-hour lockdown and curfew).
The validated Depression, Anxiety and Stress Scale (DASS-21); a self-reported questionnaire designed to assess the psychological states of depression, anxiety and stress through 21 items. We used the validated Arabic translation form of the DASS-21 scale.[17] The DASS-21 scale was chosen because of its well-known validity and internal consistency.
The Fear of COVID-19 Scale (FCV-19S) questionnaire, a newly developed scale by Ahorsu et al[18] composed of 7 items rated on a 5-point Likert scale. The minimum and maximum scores were 7 and 35, respectively. A higher reported score on the FCV-19S indicated a higher level of fear of the COVID-19 pandemic. Scores higher or equal to the mean were labeled as “high fear,” and scores less than the mean were labeled as “low fear.” Since its development in March 2020, the FCV-19S scale has been validated for several populations.[19]
2.3. Statistical analysis
Following proper cleaning, the data was analyzed using SPSS 23 (IBM SPSS Statistics, New York, NY). We checked the normality of the data of the entered variables for necessary transformations.
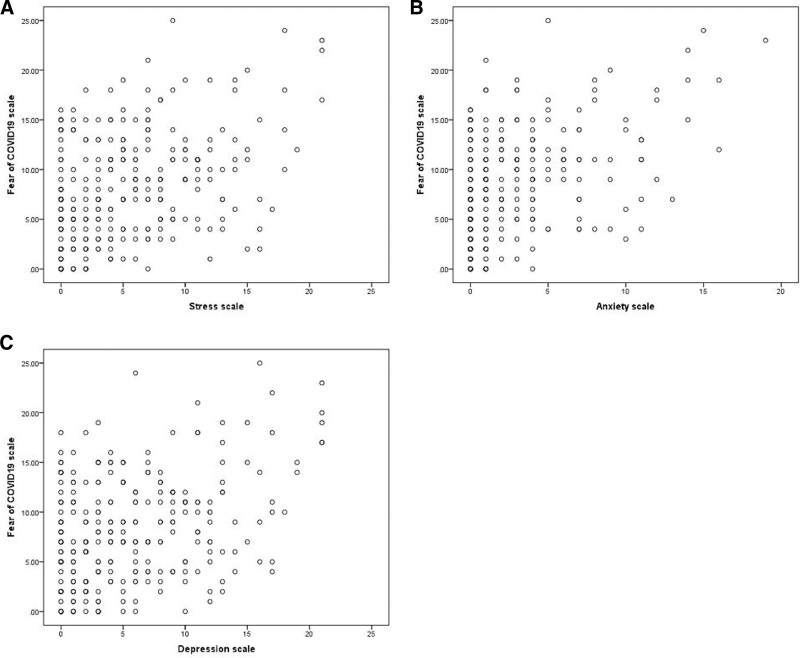
Initially, we assessed the relationship of stress, anxiety, and depression with different variables. We also assessed the relationship of the fear of COVID-19 categories (less and more fear) with the same variables as above. Next, we assessed the correlations of the FCV-19S with the DASS-21 by Pearson’s correlations. Taking all the significant variables from the univariate and bivariate analyses, we constructed 3 separate models on stress, anxiety and depression scales, respectively, to assess the effect of the FCV-19S scale. We also constructed scatter plots between the FCV-19S and each stress, anxiety and depression scale separately in Excel. Qualitative variables were expressed as frequency and percentage, while quantitative variables were shown as mean and standard deviation (M ± SD). We considered a P value of .05 or less to be significant.
3. Results
The mean age of the participants was 21.78 ± 2.11 years; male students constituted more than half of the sample (60.4%). On the depression scale, 77% were normal, 14.4% had mild, 6.8% had moderate, and 1.8% had severe depressive symptoms. On the anxiety scale, 89.2% were normal, 3.2% had mild, 6.1% had moderate, and 1.4% had severe anxiety symptoms. Finally, 93.9% reported no stress, 4.7% had mild, and 1.4% had moderate stress symptoms.
Students who had COVID-19 cases among their neighbors or relatives, those whose lives were affected by COVID-19, and those with poor socioeconomic status had significant stress, anxiety, and depression symptoms compared to others (P < .05). Female students were more anxious than male students (P = .03). Furthermore, students from high-viral-load areas, unmarried students, and students who did not live with their families were more stressed than their counterparts (P < .05) (Table 1).
Table 1.
Demographic variables correlated to the DASS-21 subscale.
| Variables | N (%) | Stress | Anxiety | Depression | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | P | M | SD | P | M | SD | P | ||
| Overall | 278 (100%) | 5.32 | 5.05 | .26 | 2.63 | 3.69 | .20 | 5.60 | 5.29 | .16 |
| Gender | ||||||||||
| Male | 168 (60.4) | 4.91 | 4.84 | .09 | 2.25 | 3.50 | .03 | 5.33 | 5.16 | .29 |
| Female | 110 (39.6) | 5.94 | 5.32 | 3.22 | 3.91 | 6.01 | 5.49 | |||
| Current residence | ||||||||||
| Low viral-load areas | 152 (54.7) | 4.79 | 4.96 | .06 | 2.49 | 3.76 | .47 | 5.13 | 5.04 | .11 |
| High viral-load areas | 126 (45.3) | 5.95 | 5.11 | 2.81 | 3.62 | 6.16 | 5.55 | |||
| Study level | ||||||||||
| Preclinical | 193 (69.4) | 5.43 | 5.26 | .57 | 2.81 | 3.83 | .21 | 5.73 | 5.33 | .54 |
| Clinical | 85 (30.6) | 5.06 | 4.56 | 2.24 | 3.35 | 5.31 | 5.22 | |||
| Marital status | ||||||||||
| Single | 274 (98.6) | 5.36 | 5.07 | .01 | 2.65 | 3.71 | .63 | 5.66 | 5.30 | .003 |
| Married | 4 (1.4) | 2 | 1.41 | 1.75 | 2.06 | 1 | 1.41 | |||
| Confirmed case among relatives or neighbors | ||||||||||
| Yes | 61 (21.9) | 7.28 | 5.05 | .001 | 3.69 | 4.03 | .01 | 7.31 | 5.95 | .004 |
| No | 217 (78.1) | 4.76 | 4.92 | 2.34 | 3.55 | 5.12 | 5.00 | |||
| Currently living with family | ||||||||||
| Yes | 244 (87.8) | 5.30 | 5.06 | .01 | 2.62 | 3.72 | .90 | 5.54 | 5.19 | .64 |
| No | 34 (12.2) | 5.41 | 5.05 | 2.71 | 3.52 | 6.00 | 6.04 | |||
| Family member health worker | ||||||||||
| Yes | 129 (46.4) | 4.97 | 5.03 | .29 | 2.34 | 3.20 | .22 | 5.19 | 5.09 | .24 |
| No | 149 (53.6) | 5.62 | 5.06 | 2.89 | 4.06 | 5.95 | 5.46 | |||
| Life affected by COVID | ||||||||||
| Not/slightly affected | 102 (36.7) | 3.37 | 4.22 | <.001 | 2.00 | 3.62 | .03 | 3.96 | 4.68 | <.001 |
| Moderately/heavily affected | 176 (63.3) | 6.44 | 5.16 | 3.00 | 3.69 | 6.55 | 5.41 | |||
| Socioeconomic status | ||||||||||
| Poor | 90 (32.4) | 6.72 | 5.50 | .001 | 3.77 | 4.29 | .001 | 7.30 | 5.88 | .001 |
| Rich | 188 (67.6) | 4.64 | 4.69 | 2.09 | 3.24 | 4.78 | 4.79 | |||
DASS-21 = Depression, Anxiety, and Stress scale.
Based on the FCV-19S, the overall mean fear score was 8.13 ± 5.34, and the median was 7 (interquartile range = 4–12). Female students, students currently living in high-viral-load areas, unmarried students, and those whose lives were affected by COVID-19 had significantly higher levels of fear (Table 2).
Table 2.
Demographic variables correlated with FCV-19S categories.
| Variables | M ± SD/N (%) | P | |
|---|---|---|---|
| Low fear | High fear | ||
| Age | 21.76 ± 2.17 | 21.81 ± 2.06 | .86 |
| Gender | |||
| Male | 103 (61.3) | 65 (38.7) | .01 |
| Female | 51 (46.4) | 59 (53.6) | |
| Current residence | |||
| Low viral-load areas | 97 (63.8) | 55 (36.2) | .002 |
| High viral-load areas | 57 (45.2) | 69 (54.8) | |
| Study level | |||
| Preclinical | 103 (53.4) | 90 (46.6) | .33 |
| Clinical | 40 (47.1) | 45 (52.9) | |
| Marital status | |||
| Single | 150 (54.7) | 124 (45.3) | .07 |
| Married | 4 (100.0) | 0 (0.0) | |
| Confirmed case among relatives or neighbors | |||
| Yes | 29 (47.5) | 32 (52.5) | .16 |
| No | 125 (57.6) | 92 (42.4) | |
| Currently living with family | |||
| Yes | 137 (56.1) | 107 (43.9) | .50 |
| No | 17 (50.0) | 17 (50.0) | |
| Family member health worker | |||
| Yes | 75 (58.1) | 54 (41.9) | .39 |
| No | 79 (53.0) | 70 (47.0) | |
| Life affected by COVID | |||
| Not/slightly affected | 63 (61.8) | 39 (38.2) | .009 |
| Moderately/heavily affected | 80 (45.5) | 96 (54.5) | |
| Socioeconomic status | |||
| Poor | 42 (46.7) | 48 (53.3) | .27 |
| Rich | 101 (53.7) | 87 (46.3) | |
FCV-19S = Fear of COVID-19 Scale.
We found a statistically significant weak-to-moderate positive correlation between the FCV-19S and DASS-21 subscales (depression, anxiety, and stress [r = 0.36, 0.45, and 0.39, respectively] P < .001 for all) (Table 3 and Fig. 1). In addition, those with a high level of fear of the COVID-19 pandemic had significantly higher scores on all DASS-21 subscales (P < .001).
Table 3.
Correlation between the FCV-19S and DASS-21 subscales.
| FCV-19S categories | Pearson’s correlation of FCV-19S and DASS-21 | ||||||
|---|---|---|---|---|---|---|---|
| Less fear (154) | More fear (124) | P | r | P | |||
| Mean | SD | Mean | SD | ||||
| Depression | 4.30 | 4.328 | 7.21 | 5.917 | <.001 | 0.36 | <.001 |
| Anxiety | 1.42 | 2.574 | 4.14 | 4.281 | <.001 | 0.45 | <.001 |
| Stress | 3.76 | 4.241 | 7.25 | 5.315 | <.001 | 0.39 | <.001 |
DASS-21 = Depression, Anxiety, and Stress scale, FCV-19S = Fear of COVID-19 Scale.
Figure 1.
(A–C) Scatter plots illustrating correlation between the FCV-19S and DASS-21 subscales. (A) FCV-19S versus stress subscale. (B) FCV-19S versus anxiety subscale. (C) FCV-19S versus depression subscale. DASS-21 = Depression, Anxiety, and Stress scale, FCV-19S = Fear of COVID-19 Scale.
Finally, we conducted a multivariate linear regression analysis and found that the FCV-19S scores preserved a statistically significant positive, albeit weak, correlation with all DASS-21 subscales (P < .001 for all) after adjustment for other significant factors mentioned earlier (Table 4).
Table 4.
Multiple linear regressions on DASS-21 subscales.
| Variables in the model | Depression | Anxiety | Stress | |||
|---|---|---|---|---|---|---|
| β | P | β | P | β | P | |
| FCV-19S | 0.29 | <.001 | 0.29 | <.001 | 0.29 | <.001 |
| Life affected by COVID | 1.40 | .03 | −0.07 | .88 | 1.92 | .001 |
| Rich socioeconomic status | −1.99 | .002 | −1.45 | .001 | −1.51 | .01 |
| Female | 0.41 | .50 | 0.76 | .06 | 0.65 | .27 |
| Confirmed case in neighborhood | 1.56 | .03 | 0.83 | .08 | 1.75 | .009 |
| Unmarried | 3.81 | .12 | – | - | 2.34 | .31 |
| Currently living with family | – | – | – | – | −0.32 | .722 |
| ↑ Viral load | – | – | – | – | 0.08 | .90 |
| R 2 | Model: 0.206 Adjusted: 0.188 |
Model: 0.258 Adjusted: 0.244 |
Model: 0.243 Adjusted: 0.220 |
|||
DASS-21 = Depression, Anxiety, and Stress scale, FCV-19S = fear of COVID-19 Scale.
4. Discussion
In this study, we investigated the impact of the COVID-19 pandemic on the mental well-being of medical students. Our results indicated the following psychological burdens: depressive symptoms in 23%, anxiety symptoms in 10.7%, and stress symptoms in 10.8% of participants.
It is clear that the prevalence of depression, anxiety and stress symptoms in our study are far greater than those declared by the World Health Organization in 2019 and even greater than the prevalence for the 5 years prior to the pandemic. This reflects the abrupt implications and consequences of COVID-19 on mental health. Additionally, our study found that almost one-quarter of the participants had depression symptoms, which is higher than the recorded value (18.3%) found in a recent meta-analysis.[7]
Since the start of the pandemic, many studies have evaluated the mental health of medical students amid the pandemic, with great variability in their results. In a recent study conducted in Saudi Arabia, 28.9% of the respondents reported depressive symptoms, 16.4% reported anxiety symptoms, and 17.8% reported stress symptoms.[6]
In a recent Spanish study, 41% of the participants reported depressive symptoms, 25% showed anxiety, and 41% felt stressed.[20] Similar results were reported from Chinese studies; 1 study found that 35% of the participants experienced psychological distress, which was more evident among female respondents, young adults, and migrants.[21] In another Chinese study, 16.5% of the participants reported moderate to severe depressive symptoms, 28.8% had moderate to severe anxiety symptoms, and 8.1% had moderate to severe stress levels; the levels were higher among female students.[22]
A recent cross-sectional study conducted on university students in Saudi Arabia reported higher levels of depression (48.8%), anxiety (86.7%), and stress (40.8%)[23] than what we found. The difference between their finding and ours is likely because 80% of their sample were female students, which matches our findings that female students are more prone to psychological distress.
Higher values were also reported in a study of Egyptian university students. That study revealed a 70.5%, 53.6%, and 47.8% burden of depression, anxiety, and stress, respectively. Female students and medical students were at higher risk of psychological distress.[24]
We attribute the relatively low psychological burden reported by our participants to the following factors: the timing of our study was early in the pandemic when several measures to reduce the risk of contact with COVID-19 cases were in place, including switching to a well stabilized official online learning platform and suspending practical hospital training. Such protective measures might have provided a sense of security, reassured the students regarding their academic studies, and avoided possible contact with suspected COVID-19 cases in training hospitals, at the college campus, and in the students’ accommodation.
Evidence supporting the above potential explanation is provided by a study conducted on 1485 medical and non-medical university students in the United Arab Emirates. The participating students were surveyed at 3 time points: during hospital rotations for medical students, before the beginning of online learning, and after the initiation of online learning. The authors found that medical students displayed more symptoms of anxiety during their hospital placements, which then decreased with the initiation of online learning.[25]
Additionally, most of the students traveled back to their family homes, which could have provided them with more psychological support and stress relief. A safe home environment is a cornerstone of psychological support as it provides students with a healthy lifestyle, including sufficient sleep, a healthy diet, social communication, and recreational opportunities.[26]
SRU students are taught using problem-based methodology with a student-centered approach. This learning system could have a positive effect, enabling the students to gain leadership capabilities, augment their self-esteem, and increase their resilience. These factors have been found to help students cope with different stressors and support their mental health.[27]
An additional factor that could have been a buffer against the increased psychological burden of the pandemic is the religious assistance that was offered to the students and general population in Saudi Arabia during the pandemic. This has been highlighted in the literature as a factor for stress management and spiritual peace.[28]
Cognitive behavioral therapy offered to the students is also a proven way to decrease their anxiety level and modify their emotions and behaviors amid such emergencies.[29] It also could have contributed positively in our case as cognitive behavioral therapy was available at both the local university level through the counseling unit and at the public level through specialized COVID-19 clinics.
Research is still ongoing for a better and more in-depth understanding of the psychological status of medical students. Li et al[30] compared students’ pre- and post-pandemic parameters, with the available data pointing to an increased prevalence of anxiety and depression symptoms after the COVID-19 pandemic.
In the current study, we found the following factors were significantly associated with a higher risk of psychological distress: being female, living in high-viral-load areas, having a poor socioeconomic status, having a relative with a confirmed case of COVID-19, and reporting that one’s life was affected by COVID-19. Our findings match those of previous studies that have consistently revealed a positive correlation between young women and increased psychological burden.[13,31,32]
Additionally, the COVID-19 pandemic brought economic challenges and financial burdens that affected many people across the world, including medical students’ families. This effect was clear in our study; students with a poor socioeconomic status and those who reported being affected by the virus had more psychological distress. Our finding is congruent with those of previous studies that investigated COVID-19 economic burdens.[33,34]
Finally, our finding of a positive correlation between the FCV-19S and DASS-21 scores is supported by previous studies[35,36] and encourages the utilization of the FCV-19S as an emerging rapid and simple mental health assessment tool.
4.1. Limitations
Our study had some limitations, including its cross-sectional design, which precluded us from attributing causality of students’ psychological distress to COVID-19. Also, the online nature of the questionnaire prevented us from directly interacting with the non-responders to determine their psychological status. Furthermore, we were unable to determine the reason for not responding. In addition, we did not follow up with the students to monitor their mental wellbeing over time.
4.2. Strengths
Both male and female medical students with various study levels were represented in the sample, and there was a good response rate to the questionnaire. An important strength was the use of more than one validated scale to measure the students’ mental health. In addition, this study was conducted during the events of quarantine, online learning, and restrictions, so it is likely that our findings are related and specific to the effects of the pandemic.
4.3. Recommendations
Our results could be beneficial to the education and public health authorities as they plan future preventive measures, screenings, and management policies/strategies for the mental wellbeing of undergraduate medical students. For example, early exclusion of students from training in facilities where patients are cared for or pausing the hospital training during peak transmission are two of the measures likely to reduce any negative mental impact on the students.
Moreover, we recommend that all medical teachers to be trained to monitor students’ behavior during such pandemics, to deliver basic cognitive behavioral therapy, and to provide the necessary counseling and social support when needed.
Finally, we recommend further prospective and follow-up studies, supported by direct interviews, to explore the long-term impact of the COVID-19 pandemic on medical students throughout Saudi Arabia and to investigate the best coping strategies for such catastrophes.
5. Conclusion
Medical students, especially female students, are at risk of fear and psychological ill effects, including increased risk of depression, anxiety and stress symptoms amid the COVID-19 pandemic. Our findings shed light on the importance of mental health screening for medical students in Saudi Arabia, especially for those at risk during such pandemics, and the need to curb any psychological hazards they endured during the pandemic.
Acknowledgments
The authors thank Ms. Erin Strotheide for her editorial contributions to this work.
Author contributions
Conceptualization: Mohammed Ewid, Yazan Kalou, Osama A. Zitoun, Adnan Raed Alnaser, Mhd Oubai Nashawi.
Formal analysis: Syed Muhammad Baqui Billah.
Investigation: Yazan Kalou, Osama A. Zitoun, Adnan Raed Alnaser, Mhd Oubai Nashawi.
Methodology: Mohammed Ewid, Yassien Amal.
Project administration: Abdulrahman Almazrou.
Supervision: Mohammed Ewid, Abdulrahman Almazrou.
Writing – original draft: Mohammed Ewid.
Writing – review & editing: Mohammed Ewid, Yassien Amal, Syed Muhammad Baqui Billah, Yazan Kalou, Osama A. Zitoun, Adnan Raed Alnaser, Mhd Oubai Nashawi, Abdulrahman Almazrou.
Supplementary Material
Abbreviations:
- DASS-21
- Depression, Anxiety, and Stress scale
- FCV-19S
- Fear of COVID-19 Scale
- KSA
- Kingdom of Saudi Arabia
- SRU
- Sulaiman Al Rajhi University
This study was funded from the annual budget of the Research Unit of Sulaiman Al Rajhi University. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplemental Digital Content is available for this article.
How to cite this article: Ewid M, Amal Y, Billah SMB, Kalou Y, Zitoun OA, Alnaser AR, Nashawi MO, Almazrou A. Impact of the COVID-19 pandemic on the psychological status of undergraduate medical students in Saudi Arabia: A cross-sectional double-scale study. Medicine 2023;102:14(e33487).
Contributor Information
Yassien Amal, Email: a.haikal@sr.edu.sa.
Syed Muhammad Baqui Billah, Email: sbbillah@gmail.com.
Yazan Kalou, Email: y.kalou@sr.edu.sa.
Osama A. Zitoun, Email: osama.zitoun@outlook.com.
Adnan Raed Alnaser, Email: adnanalnaser96@gmail.com.
Mhd Oubai Nashawi, Email: Oubai.nashawi@gmail.com.
Abdulrahman Almazrou, Email: a.almazrou@sr.edu.sa.
References
- [1].Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Coronavirus disease 2019 (COVID-19): situation report--51. WHO website. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf. [Access date April 20, 2021].
- [3].Barry M, Amri MA, Memish ZA. COVID-19 in the shadows of MERS-CoV in the Kingdom of Saudi Arabia. J Epidemiol Glob Health. 2020;10:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Brennan GK. Multidisciplinary research priorities for the COVID-19 pandemic. Lancet Psychiatry. 2020;7:e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10:227–37. [DOI] [PubMed] [Google Scholar]
- [6].Alamri HS, Algarni A, Shehata SF, et al. Prevalence of depression, anxiety, and stress among the general population in Saudi Arabia during covid-19 pandemic. Int J Environ Res Public Health. 2020;17:91831–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Schafer KM, Lieberman A, Sever AC, et al. Prevalence rates of anxiety, depressive, and eating pathology symptoms between the pre- and peri-COVID-19 eras: a meta-analysis. J Affect Disord. 2022;298:364–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Alkhamees AA, Alrashed SA, Alzunaydi AA, et al. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr Psychiatry. 2020;102:152192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lixia W, Xiaoming X, Lei S, et al. A cross-sectional study of the psychological status of 33,706 hospital workers at the late stage of the COVID-19 outbreak. J Affect Disord. 2022;297:156–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Al-Hanawi MK, Mwale ML, Alshareef N, et al. Psychological distress amongst health workers and the general public during the COVID-19 pandemic in Saudi Arabia. Risk Manag Healthc Policy. 2020;13:733–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sivertsen B, Knapstad M, Petrie K, et al. Changes in mental health problems and suicidal behaviour in students and their associations with COVID-19-related restrictions in Norway: a national repeated cross-sectional analysis. BMJ Open. 2022;12:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Acharya L, Jin L, Collins W. College life is stressful today – emerging stressors and depressive symptoms in college students. J Am Coll Heal. 2018;66:655–64. [DOI] [PubMed] [Google Scholar]
- [13].Lee CM, Juarez M, Rae G, et al. Anxiety, PTSD, and stressors in medical students during the initial peak of the COVID-19 pandemic. PLoS One. 2021;16:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Quek TT, Tam WW, Tran BX, et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Res Public Health. 2019;16:2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Puthran R, Zhang MWB, Tam WW, et al. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50:456–68. [DOI] [PubMed] [Google Scholar]
- [16].AL-Husban N, Alkhayat A, Aljweesri M, et al. Effects of COVID-19 pandemic on medical students in Jordanian universities: a multi-center cross-sectional study: Covid-19 pandemic and medical students. Ann Med Surg. 2021;67:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Moussa MT, Lovibond P, Laube R, et al. Psychometric properties of an Arabic version of the Depression Anxiety Stress Scales (DASS). Res Soc Work Pract. 2017;27:375–86. [Google Scholar]
- [18].Ahorsu DK, Lin CY, Imani V, et al. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2020;20:1537–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Alyami M, Henning M, Krägeloh CU, et al. Psychometric evaluation of the Arabic version of the fear of COVID-19 scale. Int J Ment Health Addict. 2020;19:2219–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Rodríguez-Rey R, Garrido-Hernansaiz H, Collado S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front Psychol. 2020;11:1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Qiu J, Shen B, Zhao M, et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33:100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Heal. 2020;17:1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].AlHadi AN, Alhuwaydi AM. The mental health impact of pandemic COVID-19 crisis on university students in Saudi Arabia and associated factors. J Am Coll Heal. 2021;0:1–9. [DOI] [PubMed] [Google Scholar]
- [24].Ghazawy ER, Ewis AA, Mahfouz EM, et al. Psychological impacts of COVID-19 pandemic on the university students in Egypt. Health Promot Int. 2021;36:1116–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Saddik B, Hussein A, Saheb Sharif-Askari F, et al. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates. Risk Manag Healthc Policy. 2020;13:2395–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hammami A, Harrabi B, Mohr M, et al. Physical activity and coronavirus disease 2019 (COVID-19): specific recommendations for home-based physical training. Manag Sport Leis. 2022;27:26–31. [Google Scholar]
- [27].Konaszewski K, Niesiobędzka M, Surzykiewicz J. Resilience and mental health among juveniles: role of strategies for coping with stress. Health Qual Life Outcomes. 2021;19:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Bryan JL, Lucas S, Quist MC, et al. God, can I tell you something? The effect of religious coping on the relationship between anxiety over emotional expression, anxiety, and depressive symptoms. Psycholog Relig Spiritual. 2019;8:46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Liang L, Feng L, Zheng X, et al. Effect of dialectical behavior group therapy on the anxiety and depression of medical students under the normalization of epidemic prevention and control for the COVID-19 epidemic: a randomized study. Ann Palliat Med. 2021;10:10591–9. [DOI] [PubMed] [Google Scholar]
- [30].Li W, Zhao Z, Chen D, et al. Prevalence and associated factors of depression and anxiety symptoms among college students: a systematic review and meta-analysis. J Child Psychol Psychiatry. 2022;63:1222–30. [DOI] [PubMed] [Google Scholar]
- [31].Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Heal Artic. 2020;17:3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Chinna K, Sundarasen S, Khoshaim HB, et al. Psychological impact of COVID-19 and lock down measures: an online cross-sectional multicounty study on Asian university students. PLoS One. 2021;16:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Arima M, Takamiya Y, Furuta A, et al. Factors associated with the mental health status of medical students during the COVID-19 pandemic: a cross-sectional study in Japan. BMJ Open. 2020;10:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Odriozola-González P, Planchuelo-Gómez A, Irurtia MJ, et al. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020;290:113108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Rahman MA, Hoque N, Alif SM, et al. Factors associated with psychological distress, fear and coping strategies during the COVID-19 pandemic in Australia. Global Health. 2020;16:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Chen IH, Chen CY, Zhao KY, et al. Psychometric evaluation of fear of COVID-19 scale (FCV-19S) among Chinese primary and middle schoolteachers, and their students. Curr Psychol. 2022:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]