Abstract
Background
During outbreaks of infectious diseases like COVID-19, the healthcare-associated infections (HCAIs) pose a burden on public health system. There are very limited data about infection prevention and control (IPC) implementation in the healthcare facilities of Pakistan. The aim of the study was to conduct assessment with the IPC Assessment Framework (IPCAF) tool in healthcare facilities of the least developed areas.
Methods
A cross-sectional survey was conducted in 12 tertiary level healthcare facilities (HCF) located in the least developed provinces of Pakistan. The facilities were selected through multistage cluster random methods. A well-structured questionnaire, the “IPCAF tool”, was used for data collection. The IPCAF comprises eight sections with a 100 score of each section, thus with a maximum score of 800. The scores from 0 to 800 of the HCFs were divided into four gradual ratings through IPCAF, ie from inadequate to advanced.
Results
The median score of all facilities was 405, with a range from inadequate to advanced. One facility (8.3%) fell into the “inadequate” category with a score of 172.5; 5 (41.6%) facilities achieved “basic” category, another 5 (41.6%) being “intermediate”, and only one (8.3%) hospital achieved “advanced” status. Region-wise median score of facilities of GB was 307.5, facilities in AJK scored 342.5, and a score of 520 was found for health facilities in KPK. The components of Education and Training, HCAIs Surveillance, and Multimodal Strategies achieved the lowest scores.
Conclusion
Most of the facilities have developed an IPC program with key focal persons and IPC committees, but did not have relevant education and training. IPC core capacities are being implemented. Equitable attention is required on all eight components of IPC in all facilities.
Keywords: infection prevention and control, IPCAF, healthcare facilities, healthcare associated infections
Introduction
Healthcare-associated infections (HCAIs) are the infections that pose high risk to the healthcare workers or patients, especially those with low immunity, acquired during the process of admission, treatment, or a procedure within a healthcare facility. This infection is not present or incubating at the time of patients’ admission. HCAI can occur in any healthcare setting regardless of its size. It increases the vulnerability and patient harm. The vulnerabilities to HCAIs increase during the epidemics and can cause a double-burden of disease. The COVID-19 pandemic challenged the IPC system of healthcare facilities across the globe.1 At the same time, it provided the opportunities to work on infection control and improve the IPC structure within the healthcare settings. In Pakistan, IPC activities gained importance after the COVID-19 pandemic.2 Government started to implement some of the activities, including training of healthcare workers, environmental controls, patient education, and control measures for COVID-19, tuberculosis, and other respiratory diseases.3
The World Health Organization (WHO) recommended for healthcare facilities to establish and exercise IPC program with best practices. The safety and effectiveness of any system requires regular monitoring. The WHO suggested evaluating IPC implementation considering standardized guidelines. An IPC program with all its core components is important for patients' and healthcare workers’ safety.4 To determine the level of safety against infections and implementation of IPC activities, the WHO has released the Infection Prevention and Control Assessment Framework (IPCAF) in 2018. It comprises eight WHO IPC core components:1 IPC program;2 IPC guidelines;3 IPC education and training;4 HCAI surveillance;4 multimodal strategies;5 monitoring and audit of IPC practices and feedback;6 workload, staffing, and bed occupancy; and7 the built environment, and materials and equipment for IPC.
WHO core components for IPC are a set of guidelines in each section to be followed by the healthcare management.4,5 This tool helps to assess and evaluate the IPC structure at healthcare facilities and its implementation accordingly. It is designed to support the healthcare system in reducing the burden of HCAIs and improving patient safety as well.5 HCAIs are one of the leading threats to the patient safety in the hospitals.6,7 These infections can occur in any hospital facility at primary, secondary, or tertiary level. The HCAIs have adverse effects for humans, including morbidity, prolonged hospital stays, the economic impact, increased resistance to antimicrobials, and infection-specific mortality.8–10 During the COVID-19 pandemic it was witnessed that poor IPC infrastructure in management facilities increased the burden of infections among patients and healthcare workers as well.5
This study was designed to make a comprehensive assessment of tertiary level healthcare facilities in underdeveloped areas of Pakistan. A tertiary care facility is one that provides full services in pediatrics, general medicine, various branches of surgery, and psychiatry.11 The assessment was made with the aim to highlight the good practices and the gaps in healthcare facilities. The present study tried to evaluate the IPC implementation level of healthcare facilities, identify best practices, and examine the compliance to IPC components of IHR-2005 at subnational level as per the recommendation of WHO.12 For the effective implementation of the IPC core components, frequent assessments in best practices with standardized audit and monitoring are essential.13,14 Prior to this study, only a few health facilities in Pakistan, in relatively developed areas of Islamabad and Punjab, have been assessed by WHO in 2017, and deficiencies were found in the implementation of IPC practices.15 The present study was carried out in 12 healthcare facilities of underdeveloped regions of Pakistan, ie Gilgit Baltistan (GB), Khyber Pakhtunkhwa (KPK), and Azad Jammu and Kashmir (AJK). GB and AJK have greater dependency on federal government in their healthcare interventions. These regions have multiple challenges due to social, geographic, economic, political, and environmental disadvantages and issues to maintain the healthcare system as a whole.16 The findings of the study might facilitate the local and national health departments in improving the IPC system.
Methods
Study Area
The data were collected from the three least developed provinces of Pakistan, namely KPK, AJK, and GB. These provinces are relatively poor, and marginal in terms of public health interventions as compared with Punjab and Sindh. The healthcare facilities in the target provinces have a high influx of outdoor and indoor patients and fewer doctors to provide proper medical services.
Study Subjects
The tertiary level healthcare facilities, with designated COVID-19 sampling, testing, and/or treatment unit at district level, are included in the study for IPCAF assessment. Respondents in the study were the members of hospital IPC committees, heads of facilities, medical doctors, nurses, and staff involved in IPC-related activities. The other staff who had not been working on implementation of IPC were excluded from the study.
Study Design
The study was a cross-sectional survey study. A total of 12 health facilities were evaluated with the IPCAF tool translated into the local language as well. Multistage cluster random sampling technique was used to locate the target population (healthcare facility) in each province. From each province, ie KPK, GB, and AJK, 04 tertiary level healthcare facilities were selected. At first the researchers selected 04 divisions and later 04 districts among selected divisions. From each district one facility was selected as sample for this study.
After getting approval from the designated authorities the researchers developed a plan of assessment of the facilities. The departments and bed capacities of all facilities vary with a range from 30 beds minimum to 480 beds maximum. All facilities were assessed with a combination of teams consisting of a microbiologist, a medical doctor, and a public health system specialist from the National Institutes of Health. IPCAF tool was filled during the interviews of the hospital staff.
Study Instrument and Technique
The assessment was made through IPCAF tool. The tool is structured with defined components and indicators. The tool consists of eight core components of IPC system and 81 measurable indicators considering IPC guidelines. The list of components is as under:
C1- IPC Program
C2- IPC Guidelines
C3- IPC Education
C4- HCAIs Surveillance System
C5- Multimodal Strategies in IPC
C6- Monitoring/Audit/Feedback
C7- Workload, Staffing, and Bed Occupancy within Facility
C8- Environments, Materials, and Equipment in the Facility
Each component (C) in the tool has equal score, ie 100 per component. The maximum cumulative score of all eight components is 800. The tool defines the allocation of individual weightage to the indicator states within all components. A minimum score of 0 and maximum score of 100 was assigned in the tool (Table 1). Data were analyzed by using MS Excel package and descriptive statistics.
Table 1.
IPCAF Tool Scores and Description
| IPCAF Scores | Level | Description |
|---|---|---|
| 0–200 | Inadequate | Insufficient IPC implementation and require significant improvements in almost all components. |
| 201–400 | Basic | These facilities have some functional IPC aspects without proper implementation, and additional improvement is needed. |
| 401–600 | Intermediate | At this level most IPC aspects are properly implemented. |
| 601–800 | Advanced | At this level the IPC are fully implemented according to WHO recommendations. |
Results
All eight core components of IPCAF were assessed in all facilities. Data timeliness and completeness were recorded as 100%. Table 2 lists the region-wise median scores of healthcare facilities through IPCAF. It was found that the median score of KPK was 502, for AJK 342.5, and the facilities of GB have a 307.5 median score.
Table 2.
Province-Wise Percentage and Median Score of Infection Prevention and Control Framework at Facility (IPCAF) Level
| Name of Facility | Score | Percentage | Median Score | |
|---|---|---|---|---|
| KPK | DHQ Haripur | 575 | 71.87 | 520 |
| DHQ Abbottabad | 350 | 43.75 | ||
| ATH Abbottabad | 665 | 83.12 | ||
| Saidu Teaching Hospital Swat | 465 | 58.12 | ||
| AJK | DHQ Mirpur | 497.5 | 62.18 | 342.5 |
| DHQ Kotli | 460 | 57.5 | ||
| DHQ Neelum | 225 | 28.12 | ||
| Muzaffarabad | 225 | 28.12 | ||
| GB | RHQ Skardu | 462.5 | 57.81 | 307.5 |
| PHQ Gilgit | 317.5 | 39.68 | ||
| DHQ Nagar | 172.5 | 21.56 | ||
| DHQ Chilas | 297.5 | 37.18 |
C1: IPC Program
The facilities have an established IPC program with at least an IPC team and some sort of notification of their function (Table 3). Only one facility of GB did not establish an IPC program. Most of the facilities in all three regions scored above 60 in the IPC program.
Table 3.
Component-Wise Detailed Scores Obtained by the Healthcare Facilities of Azad Jammu and Kashmir; Khyber Pakhtunkhwa; and Gilgit Baltistan in IPCAF Assessment
| Name of Facility | C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | Total Score |
|---|---|---|---|---|---|---|---|---|---|
| District Headquarter Hospital, Haripur | 75 | 77.5 | 65 | 55 | 60 | 90 | 70 | 82.5 | 575 |
| District Headquarter Hospital, Abbottabad | 47.5 | 47.5 | 25 | 7.5 | 40 | 55 | 50 | 77.5 | 350 |
| Ayub Teaching Hospital, Abbottabad | 82.5 | 97.5 | 80 | 77.5 | 85 | 92.5 | 65 | 85 | 665 |
| Saidu Teaching Hospital, Swat | 62.5 | 70 | 70 | 47.5 | 55 | 57.5 | 45 | 57.5 | 465 |
| District Headquarter Hospital, Mirpur | 65 | 70 | 60 | 35 | 70 | 75 | 55 | 52.5 | 497.5 |
| District Headquarter Hospital, Kotli | 62.5 | 80 | 50 | 50 | 70 | 92.5 | 40 | 80 | 460 |
| District Headquarter Hospital, Neelum | 72.5 | 90 | 50 | 10 | 65 | 42.5 | 50 | 25 | 225 |
| AIMS Hospital, Muzaffarabad | 70 | 55 | 30 | 15 | 0 | 10 | 20 | 25 | 225 |
| Regional Headquarter Hospital, Skardu | 85 | 75 | 30 | 22.5 | 60 | 90 | 45 | 55 | 462.5 |
| District Headquarter Hospital, Gilgit | 75 | 57.5 | 10 | 27.5 | 25 | 10 | 40 | 72.5 | 317.5 |
| District Headquarter Hospital, Nagar | 0 | 37.5 | 5 | 27.5 | 10 | 15 | 20 | 57.5 | 172.5 |
| District Headquarter Hospital, Chilas | 52.5 | 50 | 10 | 25 | 15 | 25 | 40 | 80 | 297.5 |
C2: IPC Guideline
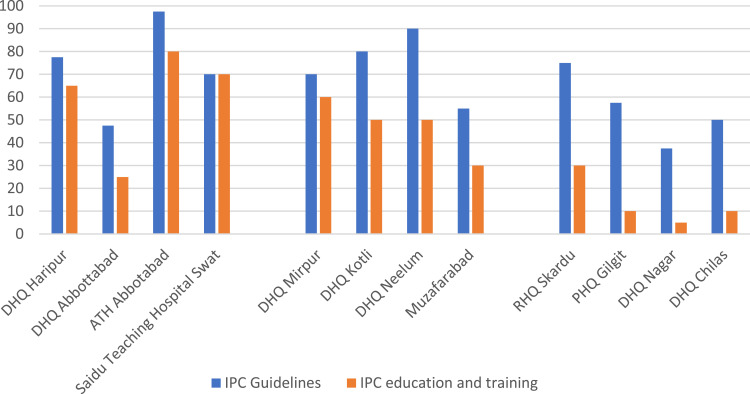
Most of the facilities have developed or adopted IPC guidelines at their facility or in a local context. Two regions, ie KPK and AJK, have improved scores in the development or adaptation of guidelines (Figure 1), whereas the facilities in GB scored less as compared with the other two provinces.
Figure 1.
Region-wise status of development/adaptation of IPC guidelines with IPC Education/Training.
C3: IPC Education
Few internal training records were found regarding IPC. A few of the personnel from all 12 facilities were trained in IPC to regularize the training at their facility. Most of the facilities do not have a system of continuous training and education for IPC implementation and practices (Figure 1).
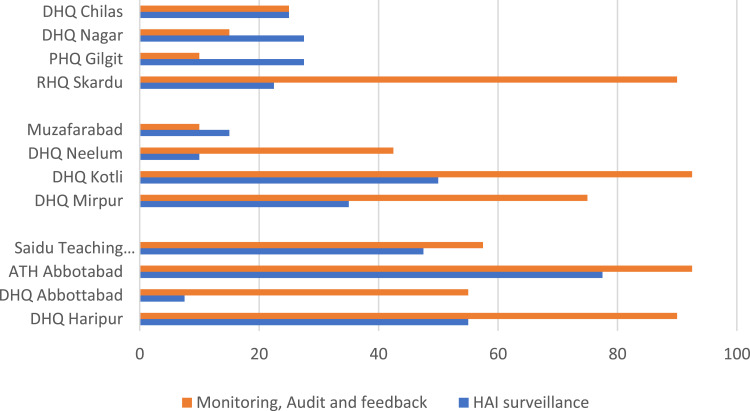
C4: HCAIs Surveillance
Most of the hospitals have no existing HCAI surveillance system in place (Table 3). The facilities in AJK perform HCAIs surveillance on a manual basis, but no dedicated staff are available for the surveillance of HCAIs with supporting logistics (Figure 2).
Figure 2.
Region-wise status of Healthcare Associated Infections Surveillance and Audit/Monitoring System at Facility Level.
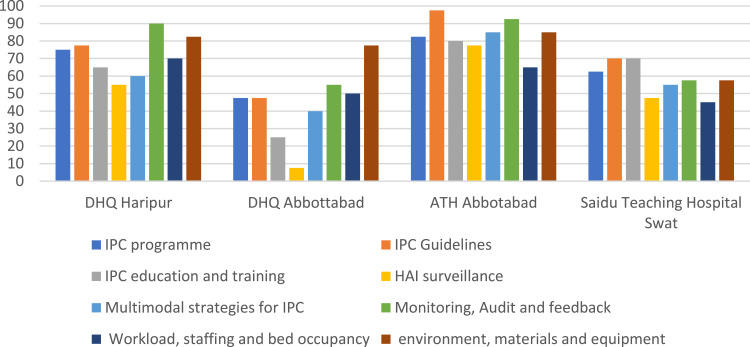
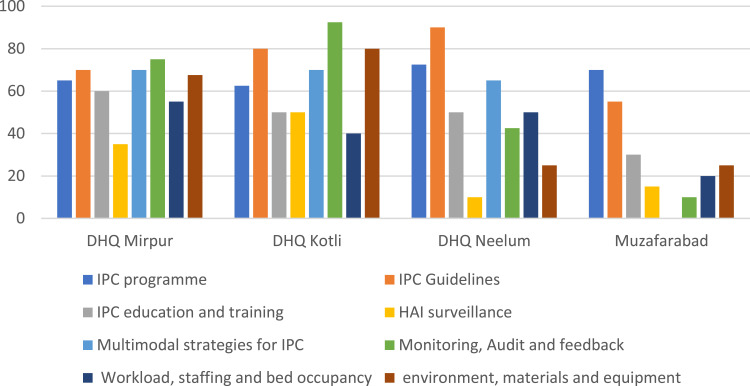
C5: Multimodal Strategies
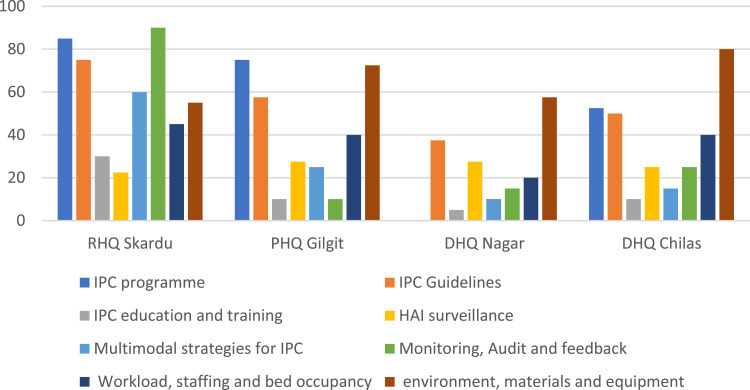
Multimodal strategies are not well established in all facilities. There was inappropriate training and capability-building system (Figures 3 and 4).
Figure 3.
Overall IPC situation in four selected facilities in province Khyber Pakhtunkhwa in March 2022.
Figure 4.
Overall IPC situation in four selected facilities in province Azad Jammu and Kashmir in March 2022.
C6: Monitoring/Audit of IPC Practices and Feedback
Most of the facilities in KPK and AJK have established monitoring and audit systems of IPC at the initial stages. Two facilities in KPK, one in AJK, and one in GB have a good auditing and feedback system (Figure 2).
C7: Workload, Staffing, and Bed Occupancy
The staffing situation was not at the optimal level in all of the facilities as per WHO workload indicators. Most of the facilities were following the WHO recommendation to have a space of >1 meter between patient beds in all departments (Figure 5).
Figure 5.
Overall IPC situation in four selected facilities in province Gilgit Baltistan in March 2022.
C8: Environments, Materials, and Equipment for IPC
Only one region has good stock and supply management of materials and equipment for IPC, (Figure 3), and the least satisfactory of the facilities was Gilgit Baltistan (Figure 5). Water and power services in most of the facilities were readily available at most hospitals for all types of functions.
Discussion
Most of the facilities attained above 200 IPCAF scores except one facility of GB that was scored at inadequate, which was newly established with a 40-bed capacity. A total of 5 out of 12 facilities obtained 200–400 score, with basic capacity in all components of IPC. Four facilities got score between 400–600 as intermediate level of IPCAF, whereas only one facility was in the 600–800 score, with advanced level of implementation. IPC strategies and activities gained more importance due to the stress of COVID-19 response.3 All three regions have different levels in IPC implementation and obtained different scores. The facilities in Gilgit Baltistan attained a relatively low score as compared with other provinces and regions, indicating the inadequate level of IPC implementation and significant improvement is needed. This is not only for the COVID-19 but almost similar to the other respiratory diseases including tuberculosis, influenza-like illness, and severe acute respiratory infections.
Results reveal that most of the facilities have an established IPC Program in hospitals. In this study, there was only one facility that has no formal IPC Program. In 2015, WHO conducted a survey to assess the IPC implementation in 133 countries.17 The results of the survey reveal that 41% (n=54) of total countries have an established national IPC program and 29% (n=39) of the countries have an established IPC program at their tertiary level healthcare facilities. The evidence revealed that effective implementation of IPC core components with trained personnel helped in reducing healthcare-associated infections.18,19 During COVID-19 response, healthcare management paid attention to the IPC implementation across the country. Prior COVID-19, most of the IPC core components were not being exercised in most of the facilities. Tertiary care hospitals in many countries did not exercise proper IPC practices for tuberculosis, influenza-like illness, and other respiratory diseases.20 A similar study conducted in Islamabad, Pakistan indicated inadequate scores for all five hospitals in Islamabad.21
Ongoing COVID-19 response provided the opportunities for the healthcare institutions to initiate the IPC program and development of guidelines at the hospital level.22,23 Enhanced work on COVID-19 prevention and control provided the ways for the hospitals to develop the initial guidelines for different elements included in IPC. Literature reveals that the standardized guidelines for IPC are crucial in improvement of the overall facility scaffold and practices.24 Compliance to the guidelines and IPC standardized procedures help in reducing HCAIs in combination with healthcare workers’ education and training.25
It was found that most of the facilities have access to the IPC training at some level, but it is not regular and standardized for most of the staff. The results suggest that most of the facilities did not have a mechanism to build capacity of their personnel and staff within their healthcare facilities. Regular adult learning and capacity-building sessions on IPC, combined with the other medical skills development programs, are crucial to implement and sustain the IPC activities.14 Most of the hospital staff were dependent on external institutions for IPC training and education.
The HCAI surveillance system supports the estimation and response strategies regarding the AMR and HCAI incidents in the healthcare setting. Literature suggests that a functional surveillance system in the health departments can easily detect outbreaks.26,27 In the present study, according to the IPCAF tool, only 3 hospitals have the initial infrastructure to support the HCAI surveillance system, but without support, the specific IT/computer equipment, tools, and standardized case definitions. Most of the hospitals have a surveillance system for some priority diseases in general, merely dedicated for particular IPC activities and HCAIs within the facilities. Some of the facilities mentioned that they have a monitoring and auditing process but not supported by documentation. Frequent assessments with standardized audit and monitoring is very important in IPC implementation.13
Seven out of 12 hospitals have no system at any hospital to determine staffing needs assessment when staffing levels are low or when bed capacity is exceeded. Overcrowding and understaffing influence infection prevention and control practices significantly.28,29 The previous studies have demonstrated that there is a significant relationship between the low level of staffing and incidence of HCAIs increasing.30,31 In some of the facilities brooms and phenyl were being used to clean floors, which is not recommended.32
All of the facilities have PPE with good quantity, and supplies were at optimal level. Due to COVID-19 pandemic all of the facilities were supplied the PPE in all forms to ensure the safety of the healthcare workers and families. Water, environment, and sanitation conditions are relatively improved as regional government paid proper attention during the COVID-19 response period to improve the basic requirements of the hospitals.
Limitations
The study has some limitations including the relatively small sample size, limited to the IPCAF tool for its measurements and focus on the specific regions instead of all over the country. The limitations were due to time constraints, grant specifications, and implementation in defined geographic areas.
Conclusion
Before COVID-19, tertiary level healthcare facilities in some developed areas were assessed and mostly had inadequate IPC implementation. Most of the tertiary level hospital have some systems of IPC implementations. The unprecedented events of the COVID-19 challenged the public health systems, and also generated numerous opportunities for IPC improvement and future preparedness. The HCFs improved their IPC best practices and capacities gradually. Substantial work in all 8 core capacities is needed for improvement to meet IPC standards. The existing IPC system gained pace during the pandemic response, but there is a need for regular support to sustain the pace of the implementation of IPC. Active IPC programs with dedicated personnel are important to be deployed in all hospitals. Appropriate budget is lacking for operations and continuation of activities including adequate supplies, training, multimodal strategies, hand hygiene stations, and cleanliness. Infection prevention, control policies, and SOPs should be developed and implemented at all hospitals. The HCAIs surveillance system with clear definitions and standardized tools with regular monitoring of IPC practices should be undertaken. There is need to implement multimodal IPC activities which are needed to be sustained in a smooth manner. The assessment with IPCAF should be conducted systematically to improve the IPC system of the healthcare facilities and to comply with WHO guidelines for IPC.
Acknowledgment
The authors acknowledge the WHO-EMRO, WHO Country Office Pakistan, Health Department of AJK, Department of Health Gilgit Baltistan, Department of Health KPK, their tertiary level healthcare facilities, medical doctors, microbiologists, and their teams who display the detailed information, documents, reports and SOPs for IPC to facilitate this study.
Funding Statement
This study was funded by WHO EMR Office TDR grant funding number “AP21-00554” in 2021-22.
Ethics Approval
Prior to study execution, the researchers took ethical approval from Institutional Review Board of NIH, Islamabad. Although the study did not involve humans as subjects of the study, the investigation team got approval for the study. The subjects of the study were the healthcare institutions, tertiary level healthcare care facilities. The data and information belong to the segments of facilities and their IPC implementation during COVID-19 response.
Patient and Public Involvement
There was no direct involvement of the patients and the public in the study design. The public including stakeholders remained involved in the study during data collection, field observation, and group discussion process. The public and patients were involved indirectly in the study during the field visits of the hospitals and indoor facilities. Moreover, the public was also involved in terms of consultation with the hospital managers, subject matter experts (SMEs) during assessment finalization process, study execution, and arrangements.
Disclosure
The authors declare that there are no competing interests for the present study.
References
- 1.World Health Organization EMRO. WHO Pakistan integrating infection, prevention and control measures for COVID-19 response. Pakistan: Pakistan-news; 2020. Available from: https://www.emro.who.int/pak/pakistan-news/who-pakistan-integrating-infection-prevention-and-control-measures-for-covid-19-response.html. Accessed March 27, 2023. [Google Scholar]
- 2.Abbas S, Sultan F. Infection control practices and challenges in Pakistan during the COVID-19 pandemic: a multicentre cross-sectional study. J Infect Prev. 2021;22(5):205–211. doi: 10.1177/17571774211012761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fatima R, Akhtar N, Yaqoob A, Harries AD, Khan MS. Building better tuberculosis control systems in a post-COVID world: learning from Pakistan during the COVID-19 pandemic. Int J Infect Dis. 2021;113:S88–S90. PMID: 33744479. doi: 10.1016/j.ijid.2021.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Infection prevention and control GLOBAL; 2022. Available from: https://www.who.int/health-topics/infection-prevention-and-control#tab=tab_1. Accessed March 27, 2023.
- 5.Tomczyk S, Twyman A, de Kraker MEA, et al. The first WHO global survey on infection prevention and control in health-care facilities. Lancet Infect Dis. 2022;22(6):845–856. doi: 10.1016/S1473-3099(21)00809-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Health care without avoidable infections: the critical role of infection prevention and control; 2023. Available from: https://apps.who.int/iris/handle/10665/246235. Accessed March 27, 2023.
- 7.Haque M, Sartelli M, McKimm J, Bakar MA. Health care-associated infections - an overview. Infect Drug Resist. 2018;11:2321–2333. doi: 10.2147/IDR.S177247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chiang CH, Pan SC, Yang TS, et al. Healthcare-associated infections in intensive care units in Taiwan, South Korea, and Japan: recent trends based on national surveillance reports. Antimicrob Resist Infect Control. 2018;7:1. doi: 10.1186/s13756-018-0422-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jia H, Li L, Li W, et al. Impact of healthcare-associated infections on length of stay: a study in 68 Hospitals in China. Biomed Res Int. 2019;2019:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Metsini A, Vazquez M, Sommerstein R, et al. Point prevalence of healthcare-associated infections and antibiotic use in three large Swiss acute-care hospitals. Swiss Med Wkly. 2018;148:w14617. doi: 10.4414/smw.2018.14617 [DOI] [PubMed] [Google Scholar]
- 11.Government of the Punajb. Tertariy care. specialized healthcare & medical education department; 2022. Available from: https://he0alth.punjab.gov.pk/. Accessed March 27, 2023.
- 12.JEE. Joint external evaluation tool second edition technical framework in support to IHR (2005) monitoring and evaluation international health regulations; 2005.
- 13.Wilson J. Rethinking the use of audit to drive improvement. J Infect Prev. 2018;19(1):3–4. doi: 10.1177/1757177417746732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Storr J, Twyman A, Zingg W, et al. Core components for effective infection prevention and control programmes: new WHO evidence-based recommendations. Antimicrob Resist Infect Control. 2017;6:1. doi: 10.1186/s13756-016-0149-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pakistan Mission. Technical support to establish national and facility level infection prevention and control programs, 18th to 25th April 2018; 2022. Available from: https://phkh.nhsrc.pk/sites/default/files/2019-06/Infection%20Prevention%20and%20Control%20Mission%20Report%202018.pdf. Accessed March 27, 2023.
- 16.Majeed R, Khan MA, Fatima SU, Mahmood N, Sulman N, Shaukat SS. Change- Affected Northern Areas of Pakistan. Inter J Biol Biotechnol. 2020;17(2):307–317. [Google Scholar]
- 17.World Health Organization. Worldwide country situation analysis: worldwide country situation analysis ; 2015. Available from: https://apps.who.int/iris/bitstream/handle/10665/163468/9789241564946_eng.pdf;sequence=1. Accessed April 2, 2023.
- 18.Mermel LA, Jefferson J, Blanchard K, et al. Reducing Clostridium difficile incidence, colectomies, and mortality in the hospital setting: a successful multidisciplinary approach. Jt Comm J Qual patient Saf. 2013;39(7):298–305. [DOI] [PubMed] [Google Scholar]
- 19.Mitchell BG, Gardner A, Stone PW, Hall L, Pogorzelska-Maziarz M. Hospital staffing and health care-associated infections: a systematic review of the literature. Jt Comm J Qual patient Saf. 2018;44(10):613–622. doi: 10.1016/j.jcjq.2018.02.002 [DOI] [PubMed] [Google Scholar]
- 20.Islam MS, Tarannum S, Banu S, et al. Preparedness of tertiary care hospitals to implement the national TB infection prevention and control guidelines in Bangladesh: a qualitative exploration. PLoS One. 2022;17:1–15. doi: 10.1371/journal.pone.0263115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Savul S, Lalani FK, Ikram A, Khan MA, Khan MA, Ansari J. Infection prevention and control situation in public hospitals of Islamabad. J Infect Dev Count. 2020;14(09):1040–1046. doi: 10.3855/jidc.12779 [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. Infection prevention and control health-care facility response for COVID-19. 2020 WHO reference number; 2020. Available from: https://apps.who.int/iris/bitstream/handle/10665/336255/WHO-2019-nCoV-HCF_assessment-IPC-2020.1-eng.pdf. Accessed March 27, 2023.
- 23.World Health Organization. Infection prevention and control during health care when coronavirus disease (COVID-19) is suspected or confirmed: interim guidance; 2020. Available from: https://apps.who.int/iris/bitstream/handle/10665/342620/WHO-2019-nCoV-IPC-2021.1-eng.pdf?sequence=1&isAllowed=y. Accessed March 27, 2023.
- 24.Mehta Y, Gupta A, Todi S, et al. Guidelines for prevention of hospital acquired infections. Indian J Crit Care Med. 2014;18(3):149. doi: 10.4103/0972-5229.128705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Institute of Health Pakistan. National Guidelines Infection Prevention & Control. Minist Natl Heal Serv Regul Coord. 2020;2020:1–204. [Google Scholar]
- 26.Iskandar K, Molinier L, Hallit S, et al. Surveillance of antimicrobial resistance in low- and middle-income countries: a scattered picture. Antimicrob Resist Infect Control. 2021;10(1):1–19. doi: 10.1186/s13756-021-00931-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yao H, Suo J, Xing Y, et al. The minimum data set and quality indicators for national healthcare-associated infection surveillance in mainland china: towards precision management. Biomed Res Int. 2019;2019:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lowe H, Woodd S, Lange IL, Janjanin S, Barnett J, Graham W. Challenges and opportunities for infection prevention and control in hospitals in conflict-affected settings: a qualitative study. Confl Health. 2021;15(1):1–10. doi: 10.1186/s13031-021-00428-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaier K, Mutters NT, Frank U. Bed occupancy rates and hospital-acquired infections--should beds be kept empty? Clin Microbiol Infect. 2012;18(10):941–945. doi: 10.1111/j.1469-0691.2012.03956.x [DOI] [PubMed] [Google Scholar]
- 30.Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012;40(6):486–490. doi: 10.1016/j.ajic.2012.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Manojlovich M, Sidani S, Covell CL, Antonakos CL. Nurse dose: linking staffing variables to adverse patient outcomes. Nurs Res. 2011;60(4):214–220. doi: 10.1097/NNR.0b013e31822228dc [DOI] [PubMed] [Google Scholar]
- 32.Heudorf U, Gasteyer S, Müller M, et al. Manual of infection prevention and control: prevention of catheter-associated urinary tract infections. GMS Hygiene Inf Con. 2019;2016:544. [DOI] [PMC free article] [PubMed] [Google Scholar]