Abstract
Bckground:
The diagnosis of chronic rhinosinusitis (CRS) is confirmed by subjectively assessing a patient’s complaints and objectively by a computed tomography scan (CT scan) and nasoendoscopic examination. The Lund Mackay (LM) score on paranasal sinus CT scans and the Modified Lund Kennedy (MLK) nasoendoscopic score have more advantages than other scores.
Objective:
The aim of this study was to determine the correlation between the LM score on paranasal sinus CT scans and the nasoendoscopic MLK score in patients with CRS at Dr. Hasan Sadikin General Hospital Bandung.
Methods:
This is a cross-sectional analytical observational study conducted on 70 adult CRS patients with nasoendoscopy and paranasal sinus CT scans at Dr. Hasan Sadikin General Hospital Bandung. The Lund Mackay score and nasoendoscopic MLK score were collected, and the data were analyzed using Spearman’s correlation
Results:
In this study, 51.4% were males and 48.6% were females, and most subjects were without polyps (72.9%). This study found a strong positive correlation in subjects with polyps (Spearman’s rank correlation coefficient 0.7) in LM score with nasoendoscopic MLK score and a very small correlation in subjects without polyps
Conclusion:
There is a significant correlation between Lund Mackay score on paranasal sinus CT scan and nasoendoscopic Modified Lund Kennedy score in CRS patients with polyps in Dr. Hasan Sadikin Bandung General Hospital.
Keywords: Chronic rhinosinusitis, Lund-Mackay score, Nasoendoscopic, Modified Lund-Mackay score
1. BACKGROUND
Chronic rhinosinusitis (CRS) in adults was defined by the European Position Paper on Rhinosinusitis and Nasal Polyps in 2012 (EPOS 2012) as inflammation of the nose and the paranasal sinuses characterized by two or more symptoms. One of the symptoms is nasal blockage/obstruction/congestion or nasal discharge (anterior/posterior nasal drip) coupled with the presence or absence of facial pain or pressure in the face, as well as a reduction or loss of smell as long as 12 weeks or more. Chronic rhinosinusitis can be accompanied with or without nasal polyps (1).
Chronic rhinosinusitis is a disease with a high and increasing incidence and prevalence, with multifactorial etiology. It has a very significant impact on the quality of life by resulting in 13 million health consultations, 2 million visits to the emergency department (ED) and 73 million days of lost work productivity in the United States. Chronic rhinosinusitis affects approximately 10.9% of the adult population in Europe and 15% in the United States. The disease also results in large amounts of drug consumption, surgery and hospitalization (2). The Medical Expenditure Panel Survey data in 2007 stated that the estimated health care costs for CRS in the United States are approximately 8.6 billion dollars per year (3). The prevalence of CRS in Indonesia is quite high, and the Ministry of Health of the Republic of Indonesia states that the disease ranked 25th out of 50 major disease patterns in 2003 (4). Data on outpatient visits of the Rhinology Allergy Clinic of the Department of Ear Nose Throat Head and Neck Surgery Dr. Hasan Sadikin General Hospital in 2016 recorded 573 cases (44.5%) of CRS out of a total of 1289 cases in the Rhinology Allergy Clinic, with 37.5% CRS out of the total new patient visits. CT scan of the paranasal sinuses in the Department of Radiology Dr. Hasan Sadikin General Hospital were done on an average of 6-7 patients per month (2-5).
Several scoring systems for rhinosinusitis with CT scan modalities include the Friedman et al. score (1990), Jorgensen score (1991), Kennedy score (1992), Gaskins score (1992), Levine and May score (1993), Lund Mackay score (1993) and Harvard score (1994). Each system has a different score for rhinosinusitis. The Friedman et al. score, Kennedy score, Levine and May score, and Harvard score divide the degree of rhinosinusitis into stages 0-IV based on the pattern obtained, while the Jorgensen score and Lund Mackay score use numerical scores for each sinus. The Lund Mackay score has better popularity because it is easier to use than other scores. The Lund Mackay score is also recommended by the Task Force for Rhinosinusitis from the American Academy of Otolaryngology-Head and Neck Surgery. In a study conducted by Hopkins in 2007, the results showed more severe CRS on CT scans; the more extensive surgery performed is, the higher the level of complexity (6, 7).
Nasoendoscopic examination can provide information about the presence of inflammation in the middle meatus and nasal mucosa and can detect the initial stages of polyps. There are several scoring systems in nasoendoscopic examinations, including the Lund Kennedy score, the Perioperative Sinus Endoscopic (POSE) system score, the discharge, inflammatory, polyp (DIP) score and the modified Lund Kennedy (MLK) score. Research conducted by Alkis J Psaltis et al. in 2014 found that MLK scores had interobserver reliability and correlated well with patient-reported outcome measures (PROMs). The studies of Lu Zhang and Linghao Zhang from 2013 to 2016 showed similar results in that the MLK score had good interobserver reliability and test-retest reliability and could be used in all CRSs without being influenced by their operative status. Nasoendoscopy examination at the Rhinology-Allergy clinic of the Department of Ear Nose Throat Head and Neck Surgery Dr. Hasan Sadikin Bandung General Hospital used MLK scores (8, 9).
A study by Deosthale et al. in 2013 regarding the diagnostic accuracy of nasoendoscopy compared with CT scans in CRS concluded that nasoendoscopy was useful for confirming the diagnosis and assessing the severity of the disease in individuals with symptomatic CRS with a sensitivity of 94% and a specificity of 75%. CT scans are highly recommended in those who have a high clinical suspicion of CRS, negative nasoendoscopy results and persistent symptoms after optimal medical management that require surgery (10).
Lohiya et al., 2013, conducted nasoendoscopic comparative studies using Lund Kennedy scores and paranasal sinus CT scans with Lund Mackay scores in diagnosing CRS and obtained nasoendoscopic results with a sensitivity of 88.04%, specificity of 28.57%, positive predictive value of 94.19%, and negative predictive value of 15.38%, indicating that there is a close correlation between CT scans and nasoendoscopic findings (11). No research has been conducted to confirm the correlations between the use of LM scores on paranasal sinus CT scans and MLK nasoendoscopic scores in CRS patients.
2. OBJECTIVE
The purpose of this study was to determine the correlation of Lund Mackay scores on paranasal sinus CT scans with the modified Lund Kennedy nasoendoscopic score in CRS patients at Dr. Hasan Sadikin General Hospital.
3. MATERIAL AND METHODS
This research was carried out in the Radiology and Ear Nose Throat Surgery Department at Dr. Hasan Sadikin General Hospital from March-July 2019. This research is an analytic observational study with a cross-sectional design. We recruited 70 adult patients over the age of 18 with a diagnosis of CRS who had undergone nasoendoscopic examination and CT scan of the paranasal sinuses.
The study was approved by the Research Ethics Committee of the Faculty of Medicine, Universitas Padjadjaran/Dr. Hasan Sadikin Hospital Bandung, Indonesia No. 1213/UN6.C1.3.2/KEPK/PN/2016. The subjects participating in the assessment were asked to sign a written informed consent on any side effects or discomfort during the nasoendoscopy and CT scan examination.
Patients with malignancy in the sinonasal area, or a history of facial trauma, surgery in the sinonasal area, cleft palate, and cognitive impairment or who were not willing to give consent were excluded from this study. Then, the characteristics of the research subjects were collected based on age, sex and the presence or absence of nasal polyps, and LM scores were collected from the paranasal sinus CT scan and MLK nasoendoscopic score. Data analysis was performed by calculating the Spearman correlation coefficient using the Statistical Product and Service Solution (SPSS) program for Windows version 18.0. All statistical tests were carried out at the 0.05 significance level. The variables used in this study were LM score on paranasal sinus CT scan without contrast and MLK score on nasoendoscopy. These variables are explained in Table 1.
Table 1. Definition of Variable Operations.
| No | Variable | Operational Definition | Measurement | Result | Scale |
|---|---|---|---|---|---|
| 1. | Lund Mackay Score | The sinuses are grouped into: Frontal sinus Anterior ethmoidal cells Posterior ethmoidal cells Maxillary sinus Sphenoid sinus Ostiomeatal complex Each side is graded separately 0 (no abnormality) 1 (partial opacification) 2 (complete opacification) If there is no frontal sinus (aplasia), the score is 0. |
Scores were calculated based on the results of a paranasal sinus CT scan 1-3 mm axial slice thickness with coronal and sagittal reconstruction. | Score 0–24 |
Ordinal |
| 2. | Modified Lund Kennedy Score | Assessment of severity of CRS on nasoendoscopy with the following criteria : Polyps : 0 = No polyps. 1 = Polyps in middle meatus only. 2 = Beyond middle meatus. Edema : 0 = Absent 1 = Mild 2 = Severe Discharge 0 = No discharge 1 = Clear, thin discharge 2 = Thick, purulent discharge |
Scores were calculated based on the results of nasoendoscopic examination. | Score 0–12 |
Ordinal |
4. RESULTS
This study was conducted at the Radiology and Ear Nose Throat Head and Neck Surgery Department Dr. Hasan Sadikin General Hospital. The subjects of this study were 70 adult CRS patients at Dr. Hasan Sadikin General Hospital. Data collection was carried out from March to June 2019. The subjects met the inclusion criteria, did not have the specified exclusion criteria and were willing to fill out an informed consent sheet. During the process of gathering research subjects, 11 CRS patients were excluded because they did not meet the inclusion criteria or there were exclusion criteria such as an age less than 18 years in 3 patients, malignancy in the sinonasal area in 4 patients, and a history of surgery in the sinonasal area in 4 patients.
The research subjects were mostly in the age group of 20-29 years old (22.9%), consisting of 51.4% men and 48.6% women. Based on clinical criteria, 27.1% of subjects had polyps, and 72.9% did not have polyps. This can be seen in Table 2.
Table 2. Subjects’ Characteristics.
| Variable | N=70 | % |
|---|---|---|
| Age (years old) | ||
| >18-19 | 11 | 15,7 |
| 20-29 | 16 | 22,9 |
| 30-39 | 15 | 21,4 |
| 40-49 | 9 | 12,9 |
| 50-59 | 11 | 15,7 |
| >60 | 8 | 11,4 |
| Sex | ||
| Male | 36 | 51,4 |
| Female | 34 | 48,6 |
| Polyps | ||
| Present | 19 | 27,1 |
| Absent | 51 | 72,9 |
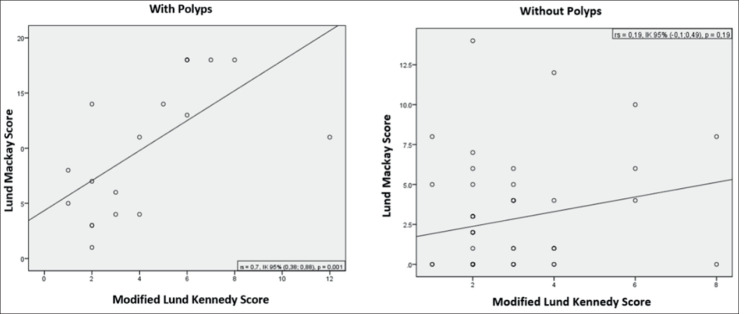
In this study, it was found that the Lund Mackay score on a paranasal sinus CT scan with the MLK nasoendoscopic score had a strong positive correlation in subjects with polyps (Spearman correlation coefficient 0.7 (95% confidence interval (0.38; 0.88)), and the correlation was very small in subjects without polyps (Spearman rank correlation coefficient 0.19 (95% confidence interval (-0.1; 0.49)). This can be seen in diagram 1.
Figure 1. Scatter graph of Lund Mackay score on paranasal sinus CT scan and modified Lund Kennedy nasoendoscopic score in patients with chronic rhinosinusitis at Dr. Hasan Sadikin General Hospital.
5. DISCUSSION
Subject characteristics included age, sex, and presence or absence of nasal polyps. In this study, the total sample included 70 adult CRS patients.
The results of this study show that the prevalence of CRS is higher in men than in women. Karki et al. obtained a ratio of 51.4%:48.6% in men and women. In this research 218 patients were obtained, 110 (50.5%) were males and 108 (49.5%) were females; also according to Shi et al., the CRS prevalence in males was higher than that in females, which was also consistent with other studies in Asia. Some studies in Western countries obtained the opposite data. For example, Fokkens et al. suggested that the prevalence of CRS was higher in women than in men, with a 3:2 women to men ratio. This was likely due to differences between sexes regarding perceptions of CRS-related symptoms and different lifestyles between the east and west (1, 12, 13).
In this study, the highest age group was approximately 20-29 years (22.9%). This is also stated in research conducted by Shi et al., who found that most age groups of CRS patients are approximately 15-34 years and 35-59 years (13).
This study analyzed data by dividing the subjects into two groups: those with and those without nasal polyps. The results of the data analysis found that the Lund Mackay score on a paranasal sinus CT scan with the MLK nasoendoscopic score has a strong positive correlation in subjects with polyps with a Spearman rank of 0.7 (95% confidence interval) and a very small correlation in subjects without polyps with a Spearman rank of 0.19 (95% confidence interval). From these results, it can be concluded that there is a correlation between the results of CT scan mainly using the Lund Mackay score compared with the nasoendoscopic examination with the Modified Lund Kennedy score in CRS patients with polyps. This is in accordance with the research of Hopkins et al., who stated that the increase in the degree of polyps also showed an increase in Lund Mackay scores on paranasal sinus CT scans. The Lund Mackay score also correlates with the extent of the operative action taken (6). This study has some limitations such as a relatively small number of research subjects and a relatively short research time.
6. CONCLUSION
This study found that the majority of CRS patients in Dr. Hasan Sadikin General Hospital are male and in the age group of 20-29 years. The majority of CRS patients at Dr. Hasan Sadikin General Hospital do not have polyps. Lund Mackay scores on a paranasal sinus CT scan with the modified Lund Kennedy nasoendoscopic score had a strong positive correlation in subjects with polyps and a very small correlation in subjects without polyps. Based on the limitations of this study, it is recommended that research be carried out in multiple centers with a longer research time.
Patient Consent Form:
All participants were informed about subject of the study.
Ethics approval and consent:
This study has received ethical approval from the Health Research Ethics Committee of the Faculty of Medicine, Universitas Padjadjaran.
Author’s contribution:
All authors contributed equally to the preparation and final approval of the manuscript.
Conflicts of interest:
There are no conflicts of interest.
Financial support and sponsorship:
None.
REFERENCES
- 1.Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2012. Rhinology. 2012;50(1):1–298. [PubMed] [Google Scholar]
- 2.Data Rekam Medis Rawat Jalan Poliklinik THT-KL RSUP Dr. Hasan Sadikin Bandung. 2016 [Google Scholar]
- 3.Juanda IJ, Madiadipoera T, Ratunanda SS. Adaptasi Budaya, Alih Bahasa Indonesia, dan Validasi Sino-Nasal Outcome Test (SNOT)-22. Majalah Kedokteran Bandung. 2017;49(4):267–273. [Google Scholar]
- 4.Kaplan A. Canadian guidelines for chronic rhinosinusitis: clinical summary. Canadian Family Physician. 2013;59(12):1275–1281. [PMC free article] [PubMed] [Google Scholar]
- 5.Multazar A, Nursiah S, Rambe A, Harahap IS. Ekspresi cyclooxygenase-2 (COX-2) pada penderita rinosinusitis kronis. Oto Rhino Laryngologica Indonesiana. 2012;42(2) [Google Scholar]
- 6.Hopkins C, Browne JP, Slack R, Lund V, Brown P. The Lund-Mackay staging system for chronic rhinosinusitis: how is it used and what does it predict? Otolaryngology - Head and Neck Surgery. 2007;137(4):555–561. doi: 10.1016/j.otohns.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 7.Lund VJ, Kennedy DW. Staging for rhinosinusitis. Otolaryngology-Head and Neck Surgery. 1997;117(3):S35–S40. doi: 10.1016/S0194-59989770005-6. [DOI] [PubMed] [Google Scholar]
- 8.Psaltis AJ, Li G, Vaezeafshar R, Cho KS, Hwang PH. Modification of the Lund‐Kennedy endoscopic scoring system improves its reliability and correlation with patient‐reported outcome measures. The Laryngoscope. 2014;124(10):2216–2223. doi: 10.1002/lary.24654. [DOI] [PubMed] [Google Scholar]
- 9.Zhang L, Zhang L. Comparison of different endoscopic scoring systems in patients with chronic rhinosinusitis: reliability, validity, responsiveness and correlation. Rhinology. 2017;55(4):363–368. doi: 10.4193/Rhin17.109. [DOI] [PubMed] [Google Scholar]
- 10.Deosthale NV, Khadakkar SP, Harkare VV, Dhoke PR, Dhote KS, Soni AJ, et al. Diagnostic accuracy of nasal endoscopy as compared to computed tomography in chronic rhinosinusitis. Indian Journal of Otolaryngology and Head & Neck Surgery. 2017;69(4):494–499. doi: 10.1007/s12070-017-1232-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lohiya SS, Patel SV, Pawde AM, Bokare BD, Sakhare PT. Comparative study of diagnostic nasal endoscopy and CT paranasal sinuses in diagnosing chronic rhinosinusitis. Indian Journal of Otolaryngology and Head & Neck Surgery. 2016;68(2):224–229. doi: 10.1007/s12070-015-0907-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karki S, Pokharel M, Suwal S, Poudel R. Prevalence of Anatomical Variations of the Sinonasal Region and their Relationship with Chronic Rhinosinusitis. Kathmandu University medical journal (KUMJ) 2016;14(56):342–346. [PubMed] [Google Scholar]
- 13.Shi JB, Fu Q, Zhang H, Cheng L, Wang Y, Zhu D, et al. Epidemiology of chronic rhinosinusitis: results from a cross‐sectional survey in seven C hinese cities. Allergy. 2015;70(5):533–539. doi: 10.1111/all.12577. [DOI] [PMC free article] [PubMed] [Google Scholar]