Abstract
Background:
Heart attack, or cardiac arrest, became a leading cause of death after the turn of the century. Defibrillation is one of the most important medical advances of the twentieth century. Defibrillation is a critical step in the treatment of cardiac arrest as it can be the only way to restore a normal heart rhythm and save the life of the individual. However, it is important to note that defibrillation is only effective if it is performed quickly and in conjunction with other life-saving measures such as cardiopulmonary resuscitation (CPR). The history of cardiac defibrillation therapy is long and fascinating, spanning several centuries, many countries and continents.
Objective:
The aim of this article was to provide historical information about technical and scientific advances in cardiac devices and the development of today defibrillators.
Methods:
Review of the available literature, historical data, personal contacts, others and personal experience in this field.
Discussion:
In 1947, Beck published the first paper describing open chest defibrillation of the human heart. Ten years later, Kouwenhoven demonstrated that the heart could be defibrillated through a closed chest. The first external defibrillator weighed 120 kg and delivered 500 v of alternating current (AC) potential. The mere size of the defibrillator restricted its use to surgical suites or other areas hospital locations. In many cases, cardiac arrhythmias recurred. This was thought to be related to the amount of energy used to defibrillate the heart which it was believed caused myocardial damage. These factors limited the practical application of defibrillators. By 1956, a unit was built that could be wheeled into the emergency room, plugged into a wall outlet, and deliver 1000 volts. By 1962, Lown realized that AC current resulted in a high frequency of cardiac arrhythmias and cardiac damage. A direct current (DC) defibrillator, consisting of a battery, a capacitor to store energy, and a transformer was developed. The therapy spread from operating rooms to coronary care units and emergency departments and in the late 1960s left the hospital and started appearing on mobile intensive care units. The first portable EMS defibrillators (used by paramedics) emerged in the early 1970s. In 1980 the automatic implantable cardioverter-defibrillator was invented. Automated external defibrillators began appearing in the late 1980s allowing the therapy to be delivered by EMTs and lay people. The ‘father’ of the modern automated external defibrillator (AED), Professor James Francis (1916-2004) was a physician and cardiologist from Northern Ireland who transformed emergency medicine and paramedic services with the invention of the portable defibrillator.
Conclusion:
Defibrillators are critical resuscitation devices. The use of reliable defibrillators has led to more effective treatments and improved patient safety through better control and management of complications during Cardiopulmonary Resuscitation (CPR). The 75th anniversary of the world’s first successful human cardiac defibrillation represents the landmark event that defined the future of cardiovascular medicine and ushered in a new era of advanced cardiac life support.
Keywords: Cardiopulmonary resuscitation (CPR), Sudden cardiac death (SCD), Defibrillation, defibrillator, Automated external defibrillator (AED)
1. BACKGROUND
Heart attack, or cardiac arrest, became a leading cause of death after the turn of the century. Defibrillation is one of the most important medical advances of the twentieth century. Out-of-hospital cardiac arrest is among the leading causes of death in Europe. In the EMS response to a cardiac arrest, ventricular fibrillation is the initial cardiac rhythm in up to 25–50% of patients. Early recognition of cardiac arrest, early initiation of high-quality chest compression, and early defibrillation using an automated external defibrillator (AED) remain the cornerstone to increase patient survival. Defibrillation is a life-saving procedure to restore normal cardiac rhythm in patients suffering from cardiac arrest. It’s an essential aspect of emergency care that can significantly increase the chances of survival and reduce the risk of permanent brain damage. Cardiac defibrillation is the act of administering a transthoracic electrical current to a person experiencing one of the two lethal ventricular dysrhythmias, ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT). Defibrillation is a critical step in the treatment of cardiac arrest as it can be the only way to restore a normal heart rhythm and save the life of the individual. The history of cardiac defibrillation therapy is long and fascinating, spanning several centuries, many countries and continents.
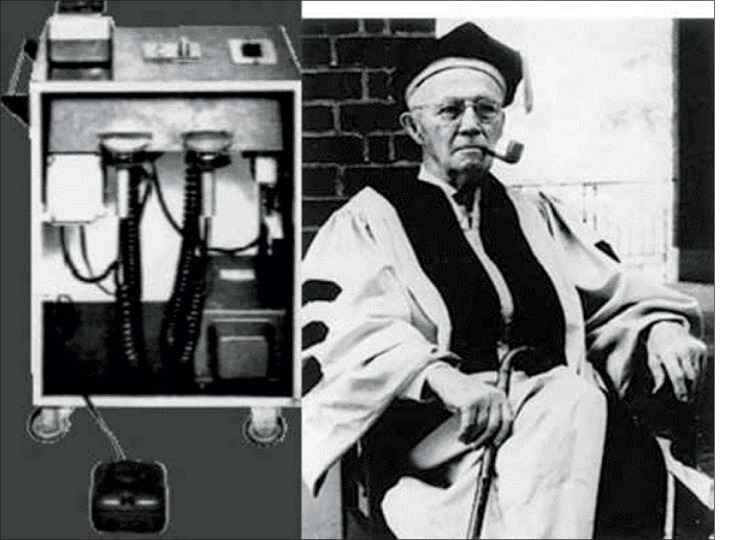
Figure 1. The external defibrillator as known today was invented by Electrical Engineer William Kouwenhoven in 1930.

The History of Cardiac Defibrillation
Electricity first became commercially available in the 1870s when practical generators were developed (1, 2) The increasing use of electricity, both direct current (DC) and alternating current (AC), resulted in many accidental deaths, particularly among power company employees, but the mechanism of death remained elusive. There were many theories - from a loss of magnetic properties in arterial blood to suffocation and heart failure - but insufficient evidence to support any of them (2).
The question was finally answered in 1899, when independent research by Italian physiologists Jean Louis Prevost and Frederic Battelli, and RH Cunningham of Columbia University, demonstrated that strong electric shocks stopped the hearts of experimental animals. Prevost and Battelli discovered that some of the animals with ventricular fibrillation were restored to sinus rhythm by applying further current through electrodes in the mouth and small intestine. According to this, defibrillators were first demonstrated in 1899 by Jean-Louis Prévost and Frédéric Batelli, two physiologists from University of Geneva, Switzerland. They discovered that small electrical shocks could induce ventricular fibrillation in dogs, and that larger charges would reverse the condition. (3-5)
Figure 2. William Kouwenhoven (1886-1975).
At the time, ventricular fibrillation was thought to occur only in animals but John McWilliam, also writing in 1899, suggested that it may also be a cause of death in humans: ‘It is hardly to be expected that such a widespread and probably universal feature of mammalian cardiac action should be unrepresented in the case of man.
Augustus Desiré Waller published the first account of a recorded electro- cardiograph in 1887 (6) paving the way for Willem Einthoven to develop it into a practical clinical tool (7). Bythe 1920s, many arrhythmias had been described and, as the physiology of the heart be- came clearer, various researchers noted that there appeared to be a refractory period in the cardiac cycle where the ventricles were more susceptible to ventricular fibrillation from an electric shock. In 1940, Carl Wiggers and René Wégria demonstrated this conclusively, establishing that a brief electric shock ‘induces fibrillation only when the shocks fall during the vulnerable period of late systole (8).
Louise Robinovitch (sometimes Rabinovitch), a pioneer in the use of medical electricity, noted: ‘It is possible to resuscitate, by means of electric current, subjects in a condition of apparent death caused by chloroform, ether, morphine, electrocution, etc. (4). Robinovich had been championing the cause of electricity as an anaesthetic, as well as a means of resuscitation. By 1911, she had developed several pieces of apparatus, including a portable resus- citation device for use in ambulances. Her preferred equipment produced ‘a direct current, interrupted from 6,000 to 8,000 times per minute, period 1/10’, generating ‘artificial blood pressure and respirations by means of rhythmic electric excitations.
By the 1920s, alternating current had become the standard power and the few remaining DC generators were shut down. Funding provided by power companies led to collaborative projects, such as that between the medical faculty and engineer William Kouwenhoven at Johns Hopkins University. Kouwenhoven and colleagues conducted years of research into the effects of electricity on the heart, publishing several articles in the Journal of Physiology in the early 1930s. In 1933, acknowledging the earlier work of Prevost and Battelli, they definitively established that electrically induced ventricular fibrillation could be reversed with an appropriate counter-shock. (2)
Figure 3. Dr. Beck’s defibrillator built by James H. Rand III in 1947 .

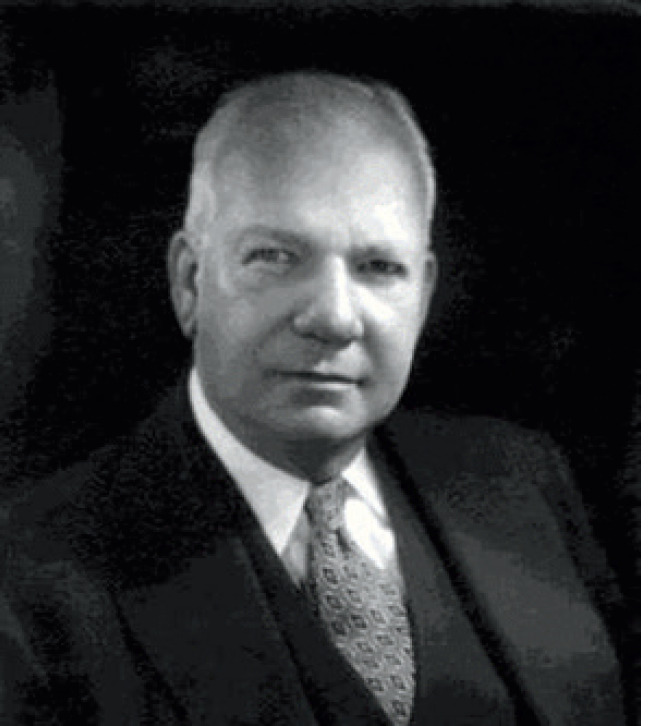
Figure 4. Claude Beck (1894-1971).
In the 1940s, two Soviet doctors, Dr. Naum Lazarevich Gurvich and Dr. G.S. Yuniev, expanded on this knowledge and proposed the first defibrillation waveform. A major breakthrough was the introduction of portable defibrillators used out of hospital in the 1950’s. Pioneered in the old Soviet Union and satellite countries; the Czechoslovakia Gurvich Peleška’s Prema defibrillator was designed to be more portable than original models used elsewhere in the world. In the Soviet Union, a portable version of Gurvich’s defibrillator, model DPA-3, was first reported in 1959. (9, 11)
The First Defibrillation in Humans 1947-1950
Less than a year after Gurvich and Yuniev captured the world’s attention with the first closed-chest defibrillation on a mammal, an American cardiac surgeon named Claude Beck would prove the viability of defibrillating human beings. Claude Beck, Professor of Surgery at Case Western University, Cleveland, having closely followed the work of Kouwenhoven and of Wiggers, developed an alternating current defibrillator for internal defibrillation (5). In 1947, Beck and a group of investigators at the University Hospitals in Cleveland, Ohio, completed the first open-heart defibrillation on a human being. The patient, Richard Heyard, was a 14-year-old boy being treated for a congenital chest defect pectus excavatum. His heart entered ventricular fibrillation near the end of his procedure, and manual massage did nothing to stop the problem. With no other options, Beck connected two electrodes to Heyard’s open heart and shocked it four times at 110 volts. The heart rhythm was restored, and Heyard made a complete recovery. The story made worldwide news headlines. One such headline read, “How Science Brings Americans Back from the Dead.” From that point on, Beck dedicated himself to improving electrical defibrillation for use on human beings. He developed the original prototype defibrillator, which - though monumental for its time - was little more than a large wooden box with two metal electrodes attached. Beck and his colleagues would ultimately go on to develop some of the CPR practices that are still used today. Unknown to Beck and his colleagues in America, investigators in Europe and Russia were far ahead of them in animal research and were beginning to use a single pulse, or dc defibrillation. (6,7,8)
The First Portable External Defibrillator
In 1951, Kouwenhoven started exploring AC power instead, and he was finally on his way to developing a sustainable portable defibrillator. By 1957, he finished work on one of the original closed-chest defibrillators for human use. The device used AC electricity to deliver 480-volt shocks safely to the adult heart. The only problem was that it weighed over 250 pounds (120 kg), which made it completely impractical as a portable device. Still, Kouwenhoven and his team kept innovating, and by 1961, they developed the first truly portable defibrillator. It weighed about 45 pounds and was capable of fitting into a small suitcase. (
Figure 5. Bernard Lown (1921-2021) .
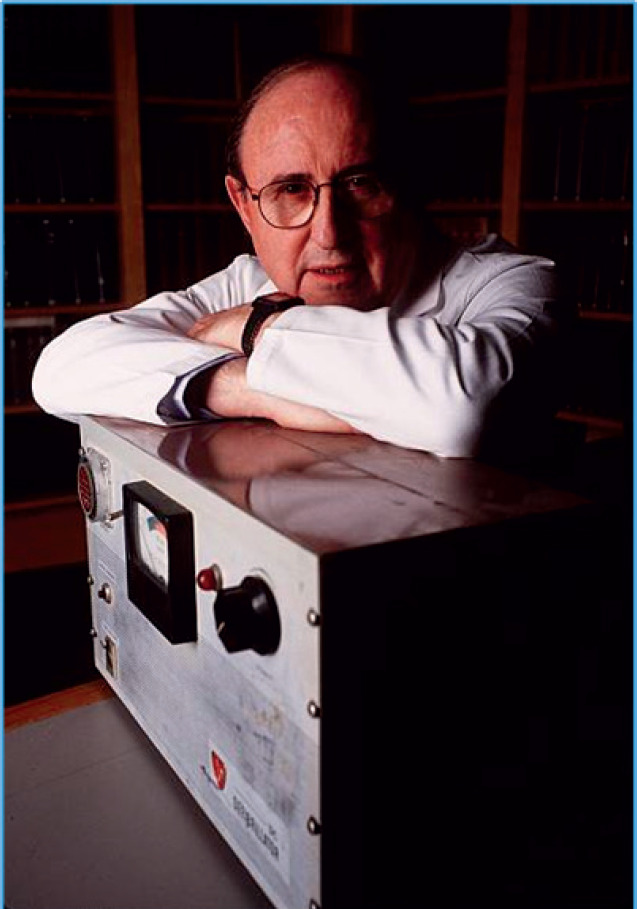
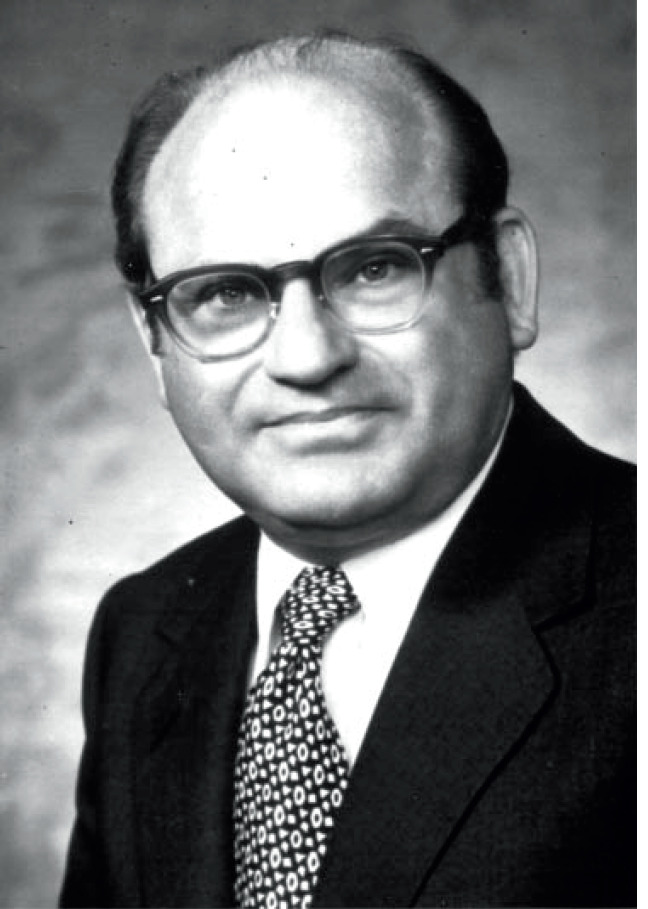
Figure 6. Barouh V. Berkovits. (1926-2012).
Harvard cardiologist Paul Zoll (7), researching external pacing for Stokes Adams attacks, became convinced of the safety of external defibrillation. At his request, Electrodyne constructed a machine with a large transformer to convert 120 V wall outlet power to 720 V. The machine was bulky and heavy but could be moved with difficulty on wheels. In 1956, Zoll reported four patients successfully reversed from ventricular fibrillation to sinus rhythm. Overall, 11 shocks were administered, all of which reversed ventricular fibrillation for a time, but only one of the patients survived to leave hospital. Bernard Lown and colleagues brought all the earlier research together in 1962 when they reported the use of DC current from a synchronised capacitor for the treatment of cardiac arrhythmias. They noted the work of Prevost and Battelli with DC current and Kouwenhoven and Zoll with AC defibrillators, as well as important work by Czech and Russian researchers with DC square wave capacitor discharges (4). The brief pulse wave generated by these capacitors allowed synchronization with any given part of the cardiac cycle. Lown’s work allowed for synchronised shocks and the subsequent development of small portable defibrillators, a standard feature of modern resuscitation. It is now recognized that early defibrillation ‘provides the best chance of survival in victims with VF or pulseless VT. (12, 14)
In early 1961, Bernard Lown of the Peter Bent Brigham Hospital in Boston, Mass, fortunately, and quite accidentally, met a brilliant young electrical engineer, Baruch Berkovits, who was helping Lown’s laboratory with instruments for research projects unrelated to the problem of cardioversion and defibrillation. In April 1961, Lown formally asked Berkovits to study his DC defibrillator in canines and for possible clinical application. A series of intense experiments followed that involved testing the efficacy of multiple waveforms and evaluating the safety of DC shock in a very large number of canines. During these experiments, the Lown-Berkovits investigation group, aware of the importance of avoiding the vulnerable period, introduced for the first time the novel concept of synchronizing delivery of the shock with the QRS complex sensed from the ECG. It was fortunate that Barough Berkovits bridged the gap between East and the West by making the DC transthoracic cardioverter/defibrillator available to Dr Bernard Lown, an interested and dedicated clinician. Bernard Lown is credited in the Western world with initiating the modern era of cardioversion. He was the first in the West to combine defibrillation and cardioversion with portability and safety. In 1959, in a patient with recurrent bouts of ventricular tachycardia (VT), Lown was the first to transthoracically apply AC shock using the Zoll defibrillator to successfully terminate an arrhythmia other than VF. (5, 7, 11, 12)
However, In the west the development of the portable defibrillator is accredited to Prof. Frank Pantridge in Belfast, who in the early 1960s developed the first truly portable device, weighing over 70Kg and needing its own vehicle to transport it! Today, portable defibrillators are among the many very important tools carried by ambulances and also used in public settings by lay-persons. They are the only provable way to resuscitate a person who has suffered a cardiac arrest unwitnessed by Emergency Medical Service (EMS) who are still in persistent ventricular fibrillation or ventricular tachycardia prior to the arrival of an ambulance. By 1968, Pantridge developed an improved portable defibrillator that weighed less than 7 pounds and was powered by a miniature capacitor designed by NASA. This small, lightweight device is often considered the first true portable AED on account of its size and power. Starting as early as the late 1960s, Pentridge’s innovative designs were adopted in hospitals and ambulances throughout the world. Surprisingly, though, the technology caught fire internationally before it became a mainstay of his own homeland. Defibrillators wouldn’t become standard in all UK ambulances until 1990. (13, 16)
The Modern History of AEDs - 1978 to the Present
There were understandable concerns about entrusting untrained laypersons with equipment capable of emitting hundreds of volts of electrical shock to the heart. The solution would come from a group of colleagues in Portland, Oregon, in 1978. Physicians Arch Diack and W. Stanley Welborn collaborated with engineer Robert Rullman with the goal of developing a fool proof portable defibrillator that bystanders could safely use in an emergency, and so they developed the Heart-Aid, the first commercially available AED designed for minimally trained lay-providers. The device contained a specially designed sensor that an operator could insert into the patient’s airway. The sensor could detect if a patient was breathing (and therefore not in cardiac arrest) and would then cease operations. A computer chip could also detect heart rate activity from the electrode and determine if a shockable rhythm was present. And so they developed Heart-Aid, the first commercially available AED designed for minimally trained lay-providers. The device contained a specially designed sensor that an operator could insert into the patient’s airway. The sensor could detect if a patient was breathing (and therefore not in cardiac arrest) and would then cease operations. A computer chip could also detect heart rate activity from the electrode and determine if a shockable rhythm was present. An adhesive electrode pad made the device safe for untrained users, as it allowed the user to take a hands-off approach and avoid the kind of accidental shock that could result from improperly operating a paddle. Finally, the device was equipped with real-time voice coaching, so an untrained user could listen along and deliver emergency treatment. (2, 13)
The ‘father’ of the modern AED, Professor James Francis (1916- 2004) was a physician and cardiologist from Northern Ireland who transformed emergency medicine and paramedic services with the invention of the portable defibrillator. The history of AEDs is still unfolding. Today, most devices weigh around 3 pounds-a far cry from the 250-pound “portable” defibrillator developed by William Kouwenhoven. Many deliver automatic shocks, and most are available for home use. Today’s automated external defibrillators can assess heart rhythms, coaching users in real time, and administering automatic or semi-automatic shocks. (19, 20)
2. CONCLUSION
Defibrillators are critical resuscitation devices. The use of reliable defibrillators has led to more effective treatments and improved patient safety through better control and management of complications during Cardiopulmonary Resuscitation (CPR). We take for granted how intuitive these devices are, but it’s been a long and complicated journey from experiment on animals to defibrillation-on-demand. The complete history of AEDs is complex and compelling. They’re low-maintenance, easy to operate, and constantly improving as new technologies emerge. Different types of defibrillators work in different ways. Automated external defibrillators (AEDs), which are now found in many public spaces, are used to save the lives of people experiencing cardiac arrest. Even untrained bystanders can use these devices in an emergency. The 75th anniversary of the world’s first successful human cardiac defibrillation represents the landmark event that defined the future of cardiovascular medicine and ushered in a new era of advanced cardiac life support.
Author’s contribution:
The author was involved in all steps of the preparation this article, including final proofreading.
Conflict of interest:
None declared.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Battelli F, Prevost JL. La mort par les courants electriques; courant alternatif a bas voltage et a haute tension. J Physiol. 1899;1:399–412. [Google Scholar]
- 2.Ball CM, Featherstone PJ. Early history of defibrillation. Anaesthesia and Intensive Care. 2019;47(2):112–115. doi: 10.1177/0310057X19838914. [DOI] [PubMed] [Google Scholar]
- 3.Cunningham RH. The cause of death from industrial accidents. N Y Med J. 1899;70:581–587. 615-622. [Google Scholar]
- 4.Einthoven W. The different forms of the human electro- cardiogram and their signification. Lancet. 1912;1:853–861. [Google Scholar]
- 5.Robinovitch LG. Electric analgesia, and electric resuscitation after heart failure under chloroform or electrocution. JAMA. 1911;56:478–481. [Google Scholar]
- 6.Beck CS, Pritchard WH, Feil HS. Ventricular fibrillation of long duration abolished by electric shock. JAMA. 1947;135(15):985. doi: 10.1001/jama.1947.62890150005007a. [DOI] [PubMed] [Google Scholar]
- 7.Zoll PM, Linenthal AJ, Gibson W, et al. Termination of ventricular fibrillation in man by externally applied electric countershock. N Engl J Med. 1956;254:727–732. doi: 10.1056/NEJM195604192541601. [DOI] [PubMed] [Google Scholar]
- 8.Lown B, Amarasingham R, Neuman J. New method for terminating cardiac arrhythmias. Use of synchronised capacitor discharge. JAMA. 1962;182:548–555. [PubMed] [Google Scholar]
- 9. [19 March 2019];2016 ANZCOR Guideline 11.4 - Electrical therapy for adult advanced life support, https://resus.org.au/guidelines/ [Google Scholar]
- 10.Efimov IR. Naum Lazarevich Gurvich (1905-1981) and his contribution to the history of defibrillation. Cardiol J. 2009;16(2):190–193. [PMC free article] [PubMed] [Google Scholar]
- 11.Kouwenhoven WHD. Resuscitation by countershock. Electrical Eng. 1933;52:475–477. [Google Scholar]
- 12.Gurvich N, Yuniev G. Restoration of regular rhythm in the mammalian fibrillating heart [in Russian] Byull Eksper Biol Med. 1939;8:55–58. [PubMed] [Google Scholar]
- 13.Cakulev I, Efimov IR, Waldo AL. Cardioversion: past, present, and future. Circulation. 2009;120(16):1623–1632. doi: 10.1161/CIRCULATIONAHA.109.865535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gurvich NL. Restoration of vital functions of the organism following fatal electric shock. [in Russian] Klin Med (Mosk) 1952;30:66–70. [PubMed] [Google Scholar]
- 15.Zoll PM, Linenthal AJ, Gibson W, Paul MH, Norman LR. Termination of ventricular fibrillation in man by externally applied electric countershock. N Engl J Med. 1956;254:727–732. doi: 10.1056/NEJM195604192541601. [DOI] [PubMed] [Google Scholar]
- 16.Peleška B. Cardiac arrhythmias following condenser discharges led through an inductance: comparison with effects of pure condenser discharges. Circ Res. 1965;16:11–18. doi: 10.1161/01.res.16.1.11. [DOI] [PubMed] [Google Scholar]
- 17.Lown , B. The shock that cures: DC and cardioversion. In: Lown B, editor. The Lost Art of Healing. New York, NY: Houghton Mifflin Co; 1996. pp. 188–201. [Google Scholar]
- 18.Schuder JC, McDaniel WC, Stoeckle H. Transthoracic defibrillation of 100 kg calves with bidirectional truncated exponential shocks. Trans Am Soc Artif Intern Organs. 1984;30:520–525. [PubMed] [Google Scholar]
- 19.Rho RW, Page RL. The automated external defibrillator. J Cardiovasc Electrophysiol. 2007;18:896–899. doi: 10.1111/j.1540-8167.2007.00822.x. [DOI] [PubMed] [Google Scholar]
- 20.Ettl F, et al. Effects of an Automated External Defibrilla tor With Additional Video Instructions on the Quality of Cardiopulmonary Resuscitation. Front Med (Lausanne) 2021;8:640721. doi: 10.3389/fmed.2021.640721. [DOI] [PMC free article] [PubMed] [Google Scholar]


