Abstract
Purpose
Reporting sharps injuries is crucial for healthcare worker occupational safety. However, these incidents are often underreported, thus posing potentially dangerous working environments. Previous small and limited studies have quantified this underreporting in specific groups of healthcare workers. This study aims to expand on these studies by further quantifying sharps injury incidences through a national study, thus better understanding healthcare reporting behaviors and the reasons for underreporting.
Patients and Methods
This is a national, multi-center, cross-sectional study conducted via an online anonymous survey distributed through email among United States attending physicians, fellows, residents, medical students, and nurses of all specialties (ie, surgery, medicine, pediatrics). Data analysis used descriptive statistics and regressive modeling with significance defined as p<0.05.
Results
Of over 3000 surveys emailed, 460 (15.3%) healthcare workers responded. The most vulnerable cohort to report sharps injuries were medical students (0.87 injuries per year ±0.69, n=92) and Postgraduate Year (PGY) 1 (0.67±0.81, n=71), PGY2 (0.86±-0.82, n=48), and PGY3 (0.92±0.8, n=45) resident physicians. Healthcare workers in surgical fields reported significantly higher likelihoods (odds ratio=4.61, p<0.001, 95% confidence interval 2.83–7.26) of sharps injuries. Medical students reported sharps injuries the least (40%) and nurses reported sharps injuries the most frequently (71%). The three most common reasons for not reporting sharps injuries included (1) healthcare workers perceiving low infection risk based on patient medical history, (2) fear of peer perception, and (3) belief of lack of reporting utility or that reporting is inconsequential.
Conclusion
Medical students and physicians early in training, especially those in surgical fields, are more vulnerable to sharps injuries, but are less likely to report, while nurses are the most likely to report. Dedicated sharps training, education to reduce stigma around injury, and implementing a simplified reporting process may help encourage reporting as well as consistency in reporting, leading to improved workplace safety.
Keywords: occupational health, compliance, sharps injury, education
Introduction
The United States Center for Disease Control and Prevention (CDC) defines sharps injuries as “a penetrating stab wound from a needle, scalpel, or other sharp object that may result in exposure to blood or other body fluids”. It is estimated that 385,000 sharps injuries occur each year amongst hospital employees.1 A global meta-analysis completed by Bouya et al in 2020 found that 42.8% (95% CI=35.5–50.1; I2=99.7%) of nurses and 46.4% (95% CI=34.1–58.8; I2=98.8%) of physicians reported sharps injuries.2 Amongst medical students, single-institution studies found that between 30% and 58.8% of the students report sharps injuries.3–5 One study by Sharma et al found that 59% of the residents had sharps injuries as medical students with 47% of them not reporting the injuries due to the length of time it takes to report or because the injury was incurred when working with a low-risk patient.6 This study also found that 83% of the residents reported sharps injuries.6
According to the Occupational Safety and Health Administration (OSHA), 5.6 million workers are at risk for developing disease through sharps injuries.7 Occupational disease transmission has a negative impact on health and quality of life as well as an increased risk of employer financial liability.8 Without intervention, the risk of transmission of serious infectious diseases such as the hepatitis B virus (HBV) can be as high as 30%, while the hepatitis C virus (HCV) and human immunodeficiency virus (HIV) transmission is about 1.8% and 0.3%, respectively.1
The CDC has published a set of recommended guidelines to effectively limit postexposure transmission which include (1) minimizing blood-borne pathogens, (2) administering post-exposure prophylaxis, (3) keeping sharps injuries logs, and (4) avoiding injury-prone devices. The CDC emphasizes that the biggest barrier to effectively limiting postexposure transmission is a low rate of compliance due to a lack of understanding the guidelines and the time it takes to report.1 Previous studies have been conducted on small groups of people, for specific training levels, or focus only on one medical field9–15; however, no study has looked at a snapshot of sharps injuries and reporting behavior across all of the medical field and training levels nationally in the United States. The purpose of this study is to quantify the incidence, reporting pattern, and reasons for not reporting sharps-related injuries among attendings, fellows, residents, medical students, attendings, and nurses.
Materials and Methods
An online survey was created using SurveyMonkey and distributed through MailChimp after obtaining approval from the Institutional Review Board at San Joaquin General Hospital in French Camp, California. The study was of national scope with multiple stakeholders, specialties, and institutions.
Consent was obtained by the study participants prior to study commencement and during consent, all participants were informed about the purpose of the study. The survey was anonymous and consisted of 15 multiple-choice questions. Emails were sent to attending physicians, fellows and residents, third- and fourth-year medical students, and nurses across the United States. Email addresses were obtained through the Accreditation Council for Graduate Medical Education (ACGME) website for residency programs. Local hospitals and medical schools in the San Francisco Bay Area were contacted directly. Since some surveys were sent on the behalf of this study, the exact number of surveys distributed is unknown, an estimate of 3000 emails were emailed. The goal was to have at least 15 responses per group. The survey period was open for 3 months. Residency programs were sent a total of five reminders, medical students were sent one reminder, all reminders were sent out by email, local hospitals received no reminders. There was no direct access to medical school or local hospital emailing lists; therefore, the number of reminders was determined by institution.
Raw data from SurveyMonkey were exported to Microsoft Excel (Microsoft Office version 15.40, Seattle, Washington), cleaned, and then subsequently loaded into statistical software (Stata version 14.2) for descriptive statistics and regression modeling. Parameters analyzed using descriptive statistics included (1) absolute number of sharps injuries experienced in the last one year, and the last 10 years, (2) sharps injury incidence which was defined as those who have experienced at least one injury during their career, and (3) sharps injury reporting which showed the percentage of healthcare providers who have reported their injury. Logistic regression was used to look at the relationship between variables associated with (1) sharps injury incidence and (2) reporting behavior from the most recent sharps injuries. Logistic regressions for these two outcomes were run separately, using variables that were hypothesized to potentially affect their respective outcomes. For each outcome (ie, sharps injury or reporting behavior), variables were run individually as a univariate analysis in addition to multivariate analysis. Odds ratio, p-values, and confidence intervals were reported for all regression analyses, with significance defined as p<0.05. All analyses were performed using Stata 14.2 from StataCorp.
Results
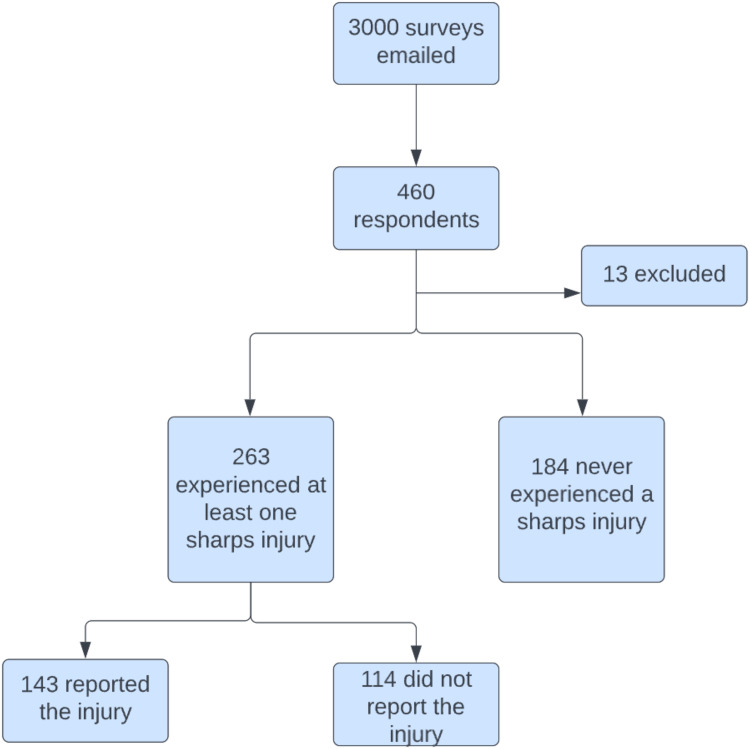
Out of an estimated 3000 surveys distributed, 460 responded (15.3%), of which 13 respondents were excluded due to incomplete responses or containing incompatible data (Figure 1). Data from a total of 447 respondents were included in the final analysis.
Figure 1.
Flow diagram of participants in the surveys.
Analysis showed that 59% (n=263) of the evaluated respondents indicated experiencing at least one sharps injury during their career with 54% reporting the injury (n=143).
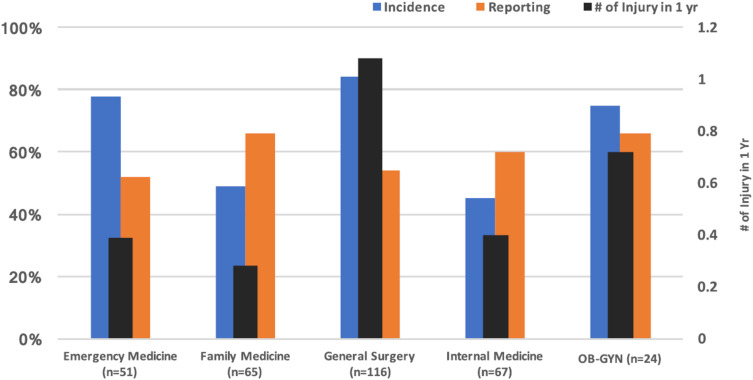
Of emergency medicine respondents (n=51), 78% experienced a sharps injury, with a total of 0.39±0.55 injuries in the past year, 2.34±4.04 injuries in the previous 10 years, and 52% reported their injuries. Of family medicine respondents (n=65), 49% experienced a sharps injury, with a total of 0.28±0.58 injuries in the past year, 1.44±1.87 injuries in the previous 10 years, and 66% reported their injuries. Of general surgery respondents (n=116), 84% experienced a sharps injury, with a total of 1.08±1.41 injuries in the past year, 7.50±14.04 injuries in the previous 10 years, and 54% reported their injuries. Of internal medicine respondents (n=67), 45% experienced a sharps injury, with a total of 0.40±0.56 injuries in the past year, 1.27±0.98 injuries in the previous 10 years, and 60% reported of their injuries. Of OB-GYN respondents (n=24), 75% experienced a sharps injury, with a total of 0.72±0.84 injuries in the past year, 2.83±2.10 injuries in the previous 10 years, and 66% reported their injuries. Of pediatric respondents (n=16), 69% experienced a sharps injury, with a total of 0.00±0.00 injuries in the past year, 0.91±0.83 injuries in the previous 10 years, and 55% reported their injuries (Table 1 and Figure 2).
Table 1.
Sharps Injury Incidence and Reporting by Different Healthcare Providers
| Incidence | Number of Sharps Injuries in Last 1 Year & 10 Years ± Standard Deviation | Reporting | |
|---|---|---|---|
| Emergency Medicine and Critical Care (n=51) | 78% | 0.39 ± 0.55 2.34 ± 4.04 |
52% |
| Family Medicine and Specialties (n=65) | 49% | 0.28 ± 0.58 1.44 ± 1.87 |
66% |
| General Surgery and Specialties (n=116) | 84% | 1.08 ± 1.41 7.50 ± 14.04 |
54% |
| Internal Medicine and Specialties (n=67) | 45% | 0.40 ± 0.56 1.27 ± 0.98 |
60% |
| Obstetrics and Gynecology (n=24) | 75% | 0.72 ± 0.83 2.83 ± 2.10 |
66% |
| Pediatric (n=16) | 69% | 0.00 ± 0.00 0.91 ± 0.83 |
55% |
Figure 2.
Incidence, reporting and number of injuries per year by medical fields.
Notes: To simplify answers choices, medical fields were grouped together as follows: Emergency Medicine=Emergency Medicine, Critical Care, Family Medicine=Family Medicine, Physical Medicine & Rehabilitation, Employee Health, Osteopathic manipulative medicine, General Surgery=General Surgery, Ophthalmology, Vascular Surgery, Oncology Surgery, Orthopedic Surgery, Pediatric Surgery, Thoracic Surgery, Trauma Surgery, Urology, Plastic Surgery, Anesthesiology, Internal Medicine=Internal Medicine, Gastroenterology, Neurology, Infectious Disease, Radiology.
Abbreviation: #, number.
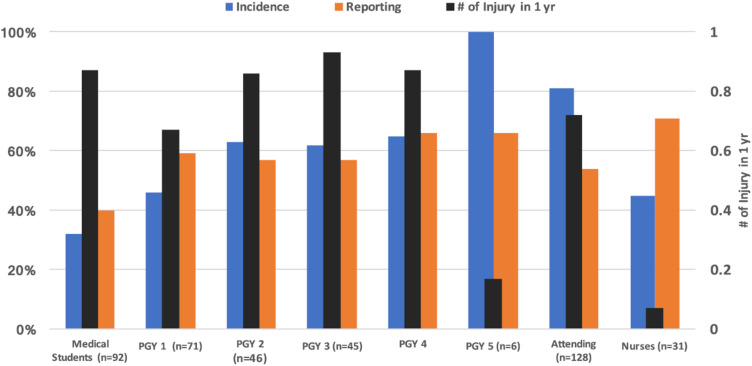
For incidence and absolute number of injuries, there were no significant differences between healthcare worker training level. Of medical student respondents (n=92), 32% experienced a sharps injury, with a total of 0.87±0.69 injuries in the past year, and 40% reported their injuries. Of postgraduate Year (PGY) 1 respondents (n=71), 46% experienced a sharps injury, with a total of 0.67±0.82 injuries in the past year, and 59% reported their injuries. Of PGY2 respondents (n=46), 63% experienced a sharps injury, with a total of 0.86±1.0 injuries in the past year, and 57% reported their injuries. Of PGY3 respondents (n=45), 62% experienced a sharps injury, with a total of 0.93±0.81 injuries in the past year, and 57% reported their injuries. Of PGY4 respondents (n=23), 65% experienced a sharps injury, with a total of 0.87±1.13 injuries in the past year, and 66% reported their injuries. Of PGY5 respondents (n=6), 100% experienced a sharps injury, with a total of 0.17±0.41 injuries in the past year, and 66% reported their injuries. Of attending respondents (n=128), 81% experienced a sharps injury, with a total of 0.72±1.29 injuries in the past year, and 54% reported their injuries. Of nurse respondents (n=31), 45% experienced a sharps injury, with a total of 0.07±0.28 injuries in the past year, and 71% reported their injuries (Table 2 and Figure 3).
Table 2.
Sharps Injury Incidence and Reporting by Healthcare Worker Training Level
| Incidence | Number of Sharps Injuries in Last 1 Year | Reporting | |
|---|---|---|---|
| Medical Students (n=92) | 32% | 0.87 ± 0.69 | 40% |
| PGY1 (n=71) | 46% | 0.67 ± 0.82 | 59% |
| PGY2 (n=46) | 63% | 0.86 ± 1.00 | 57% |
| PGY3 (n=45) | 62% | 0.93 ± 0.81 | 57% |
| PGY4 (n=23) | 65% | 0.87 ± 1.13 | 66% |
| PGY5 (n=6) | 100% | 0.17 ± 0.41 | 66% |
| Attending (n=128) | 81% | 0.72 ± 1.29 | 54% |
| Nurses (n=31) | 45% | 0.07 ± 0.28 | 71% |
Abbreviation: PGY, postgraduate year.
Figure 3.
Incidence, reporting, and number of injuries per year by training year.
Abbreviations: PGY, postgraduate year; #, number.
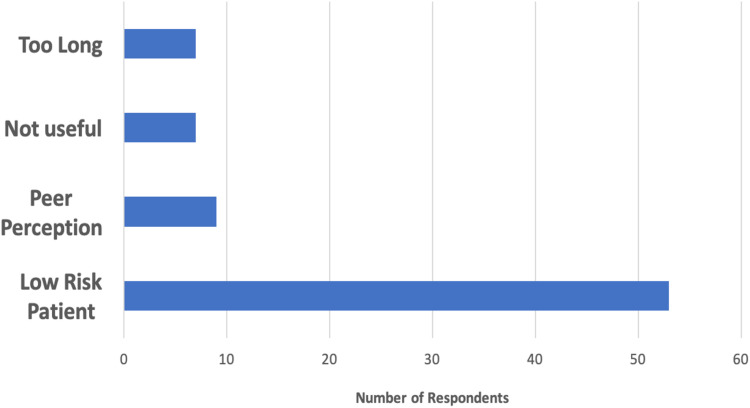
The three most common reasons for not reporting an injury were as follows: (1) healthcare workers perceiving low risk of infection based on the patient’s medical history, (n=46), (2) the healthcare provider worried about looking incompetent to peers, (n=9), and (3) the healthcare provider felt that reporting sharps injuries offered no benefit (n=7) (Figure 4).
Figure 4.
Most common reasons for not reporting sharps injuries by healthcare providers.
Notes: To simplify answers choices, reasons for not reporting sharps injury were grouped together as follows: Low risk=No/low risk, penetration not too deep, device still sterile, did not penetrate skin. Peer Perception=Worried about looking incompetent, did not want to disturb the case.
Regarding reporting behavior (Table 3), results showed that male respondents did not have an increase in odds for reporting sharps injuries compared to female respondents; with odds ratio 0.96, p=0.87, 95% CI=0.60–1.54 for univariate and odds ratio 1.21, p=0.74, 95% CI=0.56–2.23 for multivariate.
Table 3.
Logistic Regression on Reporting Behavior Comparing Gender, Surgical versus Non-Surgical Specialty, Level of Provider Training, Setting of Injury, Device Causing Injury, Sterility of Device Causing Injury, and Patient Risk Factors
| Logistic Regression on Reporting Behavior | ||||||
|---|---|---|---|---|---|---|
| Univariable | Multivariable | |||||
| OR | P | 95% CI | OR | P | 95% CI | |
| Gender | ||||||
| Female | Base | Base | Base | Base | Base | Base |
| Male | 0.96 | 0.87 | 0.60–1.54 | 1.21 | 0.74 | 0.56–2.23 |
| Surgery vs Non-Surgery | ||||||
| Non-Surgery | Base | Base | Base | Base | Base | Base |
| Surgery | 1.02 | 0.93 | 0.62–1.68 | 0.83 | 0.67 | 0.36–1.93 |
| Level of Training | ||||||
| Attending | Base | Base | Base | Base | Base | Base |
| ePGY | 1.17 | 0.59 | 0.65–2.09 | 1.45 | 0.36 | 0.65–3.20 |
| aPGY | 1.15 | 0.37 | 0.62–3.75 | 1.21 | 0.73 | 0.41–3.60 |
| Students | 0.57 | 0.18 | 0.25–1.30 | 0.88 | 0.83 | 0.29–2.73 |
| Setting | ||||||
| Non-OR | Base | Base | Base | Base | Base | Base |
| OR | 1.00 | 0.99 | 0.60–1.66 | 1.06 | 0.88 | 0.43–2.82 |
| Device | ||||||
| Others | Base | Base | Base | Base | Base | Base |
| Syringe | 0.46 | 0.14 | 0.17–1.29 | 0.67 | 0.58 | 0.16–2.82 |
| Suture | 0.25 | 0.04 | 0.94–0.64 | 0.21 | 0.02 | 0.06–0.77 |
| Contaminated Device | ||||||
| Clean | Base | Base | Base | Base | Base | Base |
| Dirty | 1.41 | 0.05 | 1.01–1.99 | 6.85 | 0.01 | 2.77–16.99 |
| Patients with Risk Factors | ||||||
| None | Base | Base | Base | Base | Base | Base |
| Risk Factors | 3.88 | 0.22 | 0.44–33.89 | 1.29 | 0.63 | 0.46–3.65 |
Notes: To simplify answer choices, the following were grouped together as shown follows: ePGY=PGY 1, 2, 3. aPGY=PGY 4, 5, 6, Fellows, Syringes=Syringe, Butterfly Needle. Others=Frozen Section Blade, K-Wire (Pin), Glass from car accident trauma, Bone, Staple, Rake, JP connector tip, Peon, Sternal Wire, Biopsy needle, Jeweler forceps, Irrigation canaliculus for tear duct probing, Skin hook, Fetal scalp electrode. Surgery=General surgery and specialties, Obstetrics and Gynecology. Non-Surgery=Internal Medicine and specialties, Family medicine and specialties, Emergency Medicine, Pediatric, Medical Students.
Respondents from surgical fields did not have an increase in odds for reporting sharps injuries compared to respondents in non-surgical fields; with odds ratio 1.02, p=0.93, 95% CI=0.62–1.68 for univariate and odds ratio 0.83, p=0.67, 95% CI=0.36–1.93 for multivariate.
EPGY respondents did not have an increase in odds for reporting sharps injuries compared to attending respondents; with odds ratio 1.17, p=0.59, 95% CI=0.65–2.09 for univariate and odds ratio 1.45, p=0.36, 95% CI=0.65–3.20 for multivariate. APGY respondents did not have an increase in odds for reporting sharps injuries compared to attending respondents; with odds ratio 1.15, p=0.37, CI=0.62–3.75 for univariate and odds ratio 1.21, p=0.73, 95% CI=0.41–3.60 for multivariate. Student respondents did not have an increase in odds for reporting sharps injuries compared to attending respondents; with odds ratio 0.57, p=0.18, 95% CI=0.25–1.30 for univariate and odds ratio 0.88, p=0.83, 95% CI=0.29–2.73 for multivariate.
There was not an increase in odds for reporting sharps injuries in the operating room setting compared to the non-operating room setting; with odds ratio 1.00, p=0.99, 95% CI=0.60–1.66 for univariate and odds ratio 1.06, p=0.88, 95% CI=0.43–2.82 for multivariate.
There was not an increase in odds for reporting sharps injuries when the device was a syringe compared to another device; with odds ratio 0.46, p=0.14, 95% CI=0.17–1.29 for univariate and odds ratio 0.67, p=0.58, 95% CI=0.16–2.82 for multivariate. There was a statistically significant increase in odds for reporting sharps injuries when the device was a suture compared to another device; with odds ratio 0.25, p=0.04, 95% CI=0.94–0.64 for univariate and odds ratio 0.21, p=0.02, CI=0.06–0.77 for multivariate.
There was an increase in odds for reporting sharps injuries from a contaminated device compared to an uncontaminated device; with odds ratio 1.41, p=0.05, 95% CI=1.01–1.99 for univariate and odds ratio 6.85, p=0.01, 95% CI=2.77–16.99 for multivariate.
There was not an increase in odds for reporting sharps injuries when the patient had risk factors compared to not having risk factors; with odds ratio 3.88, p=0.22, 95% CI=0.44–33.89 for univariate and odds ratio 1.29, p=0.63, 95% CI=0.46–3.65 for multivariate.
Univariate and multivariate analyses for sharps injuries incidence and reporting behavior showed fairly consistent results across the variables assessed, with only a few displaying a statistically significant association. Results showed that male respondents did not have an increase in odds for obtaining sharps injuries compared to female respondents; with odds ratio 0.96, p=0.85, CI=0.67–1.39 for univariate and odds ratio 0.91, p=0.63, 95% CI=0.61–1.34 for multivariate. Respondents in surgical fields had a four-fold increase in odds for obtaining sharps injuries compared to respondents in non-surgical fields; with odds ratio 4.61, p<0.001, 95% CI=2.83–7.26 for univariate and odds ratio 4.63, p<0.0001, 95% CI=2.84–7.55 for multivariate (Table 4).
Table 4.
Logistic Regression on Sharps Injury Incidence Comparing Gender and Surgery versus Non-Surgery Specialties
| Logistic Regression on Sharps Injury Incidence | ||||||
|---|---|---|---|---|---|---|
| Univariable | Multivariable | |||||
| OR | P | 95% CI | OR | P | 95% CI | |
| Gender | ||||||
| Female | Base | Base | Base | Base | Base | Base |
| Male | 0.96 | 0.85 | 0.67–1.39 | 0.91 | 0.63 | 0.61–1.34 |
| Surgery vs Non-Surgery | ||||||
| Non-Surgery | Base | Base | Base | Base | Base | Base |
| Surgery | 4.61 | 0.001 | 2.83–7.26 | 4.63 | 0.001 | 2.84–7.55 |
Notes: To simplify answer choices, the following were grouped together as follows: Surgery=General surgery and specialties, OB-GYN. Non-Surgery=Internal Medicine and specialties, Family Medicine and specialties, Emergency Medicine, Pediatric, Medical Students.
Discussion
In this study, 58.8% of the healthcare providers admitted to receiving at least one injury during their career, while only 54% reported their injury. Among all healthcare providers, medical students reported total sharps injuries the least (32%), which may be due to limited experience in the field, with residents judging that 87% of the injuries were preventable.6 However, this group had one of the highest absolute number of sharps injuries over the last 1 year (0.87±0.69).
Oftentimes, the saying “see one, do one, teach one” is a commonly adopted model by training institutions in an attempt to teach younger trainees. However, this may not be an adequate way of learning, especially for younger trainees who lack experience and do not necessarily know how to safely handle instruments. Without improved teaching techniques, younger trainees will continue to be at an increased risk for sharps injuries.11
Another factor contributing to sharps injuries is the environment. The operating room environment potentially increases the risk for sharps injuries due to the frequent handling and passing of instruments.16 Vergilio et al demonstrated that 68% of the medical students experienced their sharps injury during their surgery rotation.17 It is important to recognize that as students gain more experience over the course of their training, they also become more knowledgeable on sharps injury management, with some studies showing that there was a decreased sharps injury incidence, likely due to the student’s growing awareness.17 Therefore, a targeted and timely training prior to sharps injury prone rotations such as general surgery will likely decrease the incidents of sharps injuries amongst medical students. When comparing sharps injury incidence in the surgical and non-surgical fields, the study found that healthcare providers working in the surgical field had a significantly increase likelihood (odds ratio=4.61, p<0.001, 95% confidence interval=2.83–7.26) of obtaining sharps injuries compared to those not working in the surgical field which is likely due to increased exposure, irrespective of training. According to the American College of Surgeons (ACS), even with many efforts to decrease sharps injuries, these injuries continue to occur more frequently in the surgical field compared to the non-surgical field, where the incidence has been decreasing.16,18 Additionally, the ACS provides many recommendations to minimize exposure to bodily fluids for when a sharps injury does occur. One recommendation is to double glove during procedures. This not only reduces the rate of disease contamination19 but also leads to an early detection of a perforated glove when compared to using a single glove (36.84% vs 86.52%).20,21 There has been some pushback in double gloving due to decreases in their sensitivity and dexterity when performing tasks.22 However, though it is important, especially in a delicate and complicated surgery, to have maximal ease of movement and sensitivity, one must balance against the importance of protecting against blood-borne diseases.
This study also found that sharps injuries are often underreported. In this study, only 54% of healthcare providers reported their injuries. However, a small study looked into the incidence of sharps injuries reported during a survey and compared their results to the injuries report by Occupational Health Services. This study showed that, only 45% of the workers reported their injuries.23 In our study, nurses were the most likely to report their sharps injuries (71%). Reasons for these results include (1) there may exist a culture of silence among physicians and physicians-in-training24 and (2) within our study, nurses were lumped into a single group, therefore not considering their years of experience. More studies should be conducted to further explore variables such as medical student versus nursing student training.
In this study, medical students had a lower reporting rate (40%) compared to all other groups; PGY1 (59%), PGY2 (57%), PGY3 (57%), PGY4 (66%), PGY5 (66%), attendings (54%), and nurses (71%). Although this study did not investigate why medical student reporting rates were low, other studies demonstrated that a common reason was a lack of awareness of the institution’s sharps injury protocol.11 One encouraging result from this study was that senior level medical students did demonstrate on average a higher level of knowledge for sharps injury management than junior students, likely due to having more experience.11 Additionally, students who participated in a skills-training program that emphasized the importance of double gloving were more likely to use double gloves.25 Clinical training starting at the medical school level should include teaching students about sharps injury management so that they are adequately prepared to handle such situations for the remainder of their training and career.
Many variables discouraged healthcare providers from reporting their sharps injuries. One of the most common variables was the use of a suture needle at the time of the incident. This study found that suture needles were by far the most commonly used device at the time of injury, with a suture needle injury significantly decreasing (p<0.004) the likelihood (r=0.25) of reporting the injury. Though hollow-bore needles are most often the instrument associated with high-risk seroconversion, especially with HIV,13 other low-risk devices such as suture needles have the potential to also result in seroconversion, and healthcare providers must be encouraged to report these injuries.26
Another variable resulting in healthcare providers underreporting their sharps injuries is their perception of no, or minimal risk based on the patient’s medical history (n=53) with odds ratio=3.88, p=0.22, and 95% confidence interval=0.44–33.89 in our study. Elmiyeh et al had similar findings, with 70.8% of physicians and 39.3% of nurses reporting the perception of very low risk of transmission.24 Unfortunately, this perceived safety can be dangerous because patients may voluntarily or involuntarily withhold medical information, resulting in an incomplete patient history. The second most common reason for healthcare providers underreporting their sharps injuries was concern about looking incompetent in front of peers (n=9). Sharma et al found that 10% of the participants in their study underreported due to stigma of having a sharps injury.6 Antiretroviral therapy administered within 24 hours of injury can greatly reduce HIV infection.27 Therefore, concerns of peer perception both delay receiving time-sensitive treatments and may prevent someone from receiving lifesaving therapy. The third most common reason for underreporting sharps injuries was that healthcare providers found reporting to not be useful (n=7). While reporting sharps injuries enable healthcare providers to receive appropriate treatment, it can also be used to identify settings or devices that are particularly susceptible to injuries. By having more complete data on sharps injuries, hospitals can improve the sharps-prone settings and make a safer working environment for healthcare providers. Based on these findings, it is important to change these misconceptions of sharps injuries and reporting, and encourage healthcare providers to report their injuries. Similarly, the results from Sharma et al showed that, as medical students, 47% of the residents did not reporting their injuries due to the length of time it takes to report.6 The results from these studies indicate that a simplified reporting system may be beneficial. Further studies need to be conducted to better understand the causes of underreporting so that these barriers can be addressed.
There are several limitations to this study. First, the data represents only a portion of the healthcare workers in the United States since surveys were not administered to every healthcare worker in the country and there was only a 15.3% response rate. Additionally, because many of the surveys were sent to a third party, the exact number of surveys administered is not known, and the reminders to participants to complete the survey was not controlled. Next, the data and results of this study are from self-reporting surveys; thus, there is a risk for misclassification. To address this limitation, an anonymous, and online survey was designed to encourage accurate reporting. This study also lacked the actual reporting data about the occupational health of those who marked in the survey that they reported their injuries. Having this information could strengthen misclassification bias. Lastly, this brings up the limitation of potential recall bias. The survey used in this study contained detailed questions about sharps injuries that may have occurred in the distant past.
Conclusion
Medical students and residents reported the highest incidence of sharps injuries, while medical students were the least likely and nurses were the most likely to report their injuries. Early training targeting less experienced healthcare providers may prevent sharps injuries and encourage reporting behavior. Barriers to reporting need to be further addressed to best encourage reporting behavior including creating a simplified reporting process. The data from this study show that many healthcare providers have misconceptions about reporting their sharps injuries, which results in injury underreporting. Therefore, it is important to address these misconceptions. Finally, the importance of reporting sharps injuries should be communicated and reinforced to all healthcare providers, such as informing them how to prevent blood-borne disease transmission.
Acknowledgments
We would like to thank all the people who participated in the survey and made this study possible. We also want to thank Ms. Hatch for helping us with analysis and the overall structure of the study.
Funding Statement
No funding was associated with this manuscript.
Ethics Approval and Informed Consent
Institutional Review Board approval from San Joaquin General Hospital in French Camp, CA, was obtained. Respondents consented when responding to the online survey.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Dr Jihyun Yun made significant contribution to the conception, study design, execution, acquisition of data, analysis, and interpretation. She drafted and wrote a significant portion of the manuscript. She agrees to submit to the International Journal of General Medicine. She has reviewed and agrees to the current version of the article. She agrees to take responsibility and is accountable for the content of the article.
Kayla Umemoto made significant contribution to the execution, analysis, and interpretation. She drafted and revised a significant portion of the manuscript. She agrees to submit to the International Journal of General Medicine. She has reviewed and agrees to the current version of the article. She agrees to take responsibility and is accountable for the content of the article.
Wenjia Wang made significant contribution to the execution, analysis, and interpretation. She drafted and revised a significant portion of the manuscript. She agrees to submit to the International Journal of General Medicine. She has reviewed and agrees to the current version of the article. She agrees to take responsibility and is accountable for the content of the article.
Dr Dinesh Vyas made significant contribution to the study design execution, analysis, and interpretation. He critically reviewed the article. He agrees to submit to the International Journal of General Medicine. He has reviewed and agrees to the current version of the article. He agrees to take responsibility and is accountable for the content of the article.
Disclosure
Dr Jihyun Yun reports no conflicts of interest in this work. Kayla Umemoto reports no conflicts of interest in this work. Wenjia Wang reports no conflicts of interest in this work. Dr Dinesh Vyas discloses that he is CEO and President of MV Surgical LLC, MV Surgical Medical Technologies Inc., MV Surgical Medical Devices Inc. and Stocks in BlackSwan Inc.
References
- 1.Ken KM, Golda NJ. Contaminated sharps injuries: a survey among dermatology residents. J Am Acad Dermatol. 2019;80(6):1786–1788. doi: 10.1016/j.jaad.2018.12.042 [DOI] [PubMed] [Google Scholar]
- 2.Bouya S, Balouchi A, Rafiemanesh H, et al. Global prevalence and device related causes of needle stick injuries among health care workers: a systematic review and meta-analysis. Ann Glob Health. 2020;86(1):35. PMID: 32346521; PMCID: PMC7181946. doi: 10.5334/aogh.2698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghasemzadeh I, Kazerooni M, Davoodian P, Hamedi Y, Sadeghi P. Sharp injuries among medical students. Glob J Health Sci. 2015;7(5):320–325. PMID: 26156935; PMCID: PMC4803864. doi: 10.5539/gjhs.v7n5p320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patterson JM, Novak CB, Mackinnon SE, Ellis RA. Needlestick injuries among medical students. Am J Infect Control. 2003;31(4):226–230. PMID: 12806360. doi: 10.1067/mic.2003.44 [DOI] [PubMed] [Google Scholar]
- 5.Wicker S, Nürnberger F, Schulze JB, Rabenau HF. Needlestick injuries among German medical students: time to take a different approach? Med Educ. 2008;42(7):742–745. PMID: 18507763. doi: 10.1111/j.1365-2923.2008.03119.x [DOI] [PubMed] [Google Scholar]
- 6.Sharma GK, Gilson MM, Nathan H, Makary MA. Needlestick injuries among medical students: incidence and implications. Acad Med. 2009;84(12):1815–1821. PMID: 19940594. doi: 10.1097/ACM.0b013e3181bf9e5f [DOI] [PubMed] [Google Scholar]
- 7.Occupational safety and health administration healthcare wide hazards needlestick/sharps injuries. Available from: https://www.osha.gov/SLTC/etools/hospital/hazards/sharps/sharps.html. Accessed March 28, 2023.
- 8.Mannocci A, De Carli G, Di bari V, et al. How much do needlestick injuries cost? A systematic review of the economic evaluations of needlestick and sharps injuries among healthcare personnel. Infect Control Hosp Epidemiol. 2016;37:635–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jończyk A, Szczypta A, Talaga-ćwiertnia K. Injures as exposure events in providing medical services by nursing staff. Przegl Epidemiol. 2018;72(3):371–380. doi: 10.32394/pe.72.3.13 [DOI] [PubMed] [Google Scholar]
- 10.Rosenthal E, Pradier C, Keita-Perse O, Altare J, Dellamonica P, Cassuto J. Needlestick injuries among French medical students. JAMA. 1999;281(17):1660. doi: 10.1001/jama.281.17.1660 [DOI] [PubMed] [Google Scholar]
- 11.Varsou O, Lemon JS, Dick FD. Sharps injuries among medical students. Occup Med. 2009;59(7):509–511. doi: 10.1093/occmed/kqp103 [DOI] [PubMed] [Google Scholar]
- 12.Kelly S. Needle-stick reporting among surgeons. Ann R Coll Surg Engl. 2009;91:443–444. doi: 10.1308/003588409X432257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riddell A, Kennedy I, Tong CY. Management of sharps injuries in the healthcare setting. BMJ. 2015;351:h3733. doi: 10.1136/bmj.h3733 [DOI] [PubMed] [Google Scholar]
- 14.U.S. Department of Health & Human Services. Sharps Injuries; 2013. Available from: https://www.cdc.gov/niosh/stopsticks/sharpsinjuries.html. Accessed March 28, 2023.
- 15.Kennedy R, Kelly S, Gonsalves S, McCann PA. Barriers to the reporting and management of needlestick injuries among surgeons. Ir J Med Sci. 2009;178(3):297–299. doi: 10.1007/s11845-009-0359-8 [DOI] [PubMed] [Google Scholar]
- 16.Jagger J, Berguer R, Phillips EK, Parker G, Gomaa AE. Gomaa AE Increase in sharps injuries in surgical settings versus nonsurgical settings after passage of national needlestick legislation. AORN J. 2011;93(3):322–330. doi: 10.1016/j.aorn.2011.01.001 [DOI] [PubMed] [Google Scholar]
- 17.Vergilio JA, Roberts RB, Davis JM. The risk of exposure of third-year medical students to human immunodeficiency virus in the operating room. Arch Surg. 1993;128:36–39. doi: 10.1001/archsurg.1993.01420130040007 [DOI] [PubMed] [Google Scholar]
- 18.American College of Surgeon. Revised state on sharps safety; 2016. Available from: https://www.facs.org/about-acs/statements/94-sharps-safety. Accessed March 28, 2023.
- 19.Naver LP. Incidence of glove perforations in gastrointestinal surgery and the protective effect of double gloves: a prospective, randomised controlled study. Eur J Surg. 2000;166(4):293–295. doi: 10.1080/110241500750009113 [DOI] [PubMed] [Google Scholar]
- 20.Laine T, Aarnio P. How often does glove perforation occur in surgery? Comparison between single gloves and a double-gloving system. Am J Surg. 2001;181(6):564–566. doi: 10.1016/S0002-9610(01)00626-2 [DOI] [PubMed] [Google Scholar]
- 21.Hollaus PH, Lax F, Janakiev D, Wurnig PN, Pridun NS. Glove perforation rate in open lung surgery. Eur J Cardiothorac Surg. 1999;15:461–464. doi: 10.1016/S1010-7940(99)00055-X [DOI] [PubMed] [Google Scholar]
- 22.Matta H, Thompson AM, Rainey JB. Does wearing two pairs of gloves protect operating theatre staff from skin contamination? BMJ. 1988;297(6648):597–598. doi: 10.1136/bmj.297.6648.597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boden LI, Petrofsky YV, Hopcia K, Wagner GR, Hashimoto D. Understanding the hospital sharps injury reporting pathway. Am J Ind Med. 2015;58(3):282–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elmiyeh B, Whitaker IS, James MJ, Chahal CA, Galea A, Alshafi K. Needle-stick injuries in the national health service: a culture of silence. J R Soc Med. 2004;97(7):326–327. PMID: 15229257; PMCID: PMC1079524. doi: 10.1177/014107680409700705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jeffe DB, Mutha S, Kim LE, Evanoff BA, Fraser VJ. Evaluation of a preclinical, educational and skills training program to improve students’ use of blood and body fluid precautions: one-year follow-up. Prev Med. 1999;29:365–373. doi: 10.1006/pmed.1999.0571 [DOI] [PubMed] [Google Scholar]
- 26.Dulon M, Wendeler D, Nienhaus A. Seroconversion after needlestick injuries – analyses of statutory accident insurance claims in Germany. GMS Hyg Infect Control. 2018;13:Doc05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cardo DM, Culver DH, Ciesielski CA, et al. A case-control study of HIV seroconversion in health care workers after percutaneous exposure. Centers for disease control and prevention needlestick surveillance group. N Engl J Med. 1997;337:1485–1490. doi: 10.1056/NEJM199711203372101 [DOI] [PubMed] [Google Scholar]