Abstract
Objectives
We sought to assess depression among healthcare workers (HCWs) in the context of COVID-19 in Lusaka Province, Zambia.
Design
This cross-sectional study is nested within a larger study, the Person-Centred Public Health for HIV Treatment in Zambia (PCPH), a cluster-randomised trial to assess HIV care and outcomes.
Setting
The research was conducted in 24 government-run health facilities from 11 August to 15 October 2020 during the first wave of the COVID-19 pandemic in Lusaka, Zambia.
Participants
We used convenience sampling to recruit HCW participants who were previously enrolled in the PCPH study, had more than 6 months’ experience working at the facility and were voluntarily willing to participate.
Primary outcome measures
We implemented the well-validated 9-question Patient Health Questionnaire (PHQ-9) to assess HCW depression. We used mixed-effects, adjusted Poisson regression to estimate the marginal probability of HCWs experiencing depression that may warrant intervention (PHQ-9 score ≥5) by healthcare facility.
Results
We collected PHQ-9 survey responses from 713 professional and lay HCWs. Overall, 334 (46.8%, 95% CI 43.1%, 50.6%) HCWs recorded a PHQ-9 score ≥5, indicating the need for further assessment and potential intervention for depression. We identified significant heterogeneity across facilities and observed a greater proportion of HCWs with symptoms of depression in facilities providing COVID-19 testing and treatment services.
Conclusions
Depression may be a concern for a large proportion of HCWs in Zambia. Further work to understand the magnitude and aetiologies of depression among HCWs in the public sector is needed to design effective prevention and treatment interventions to meet the needs for mental health support and to minimise poor health outcomes.
Keywords: COVID-19, epidemiology, HIV & AIDS, mental health
STRENGTHS AND LIMITATIONS OF THIS STUDY.
These data represent important insights regarding the state of mental wellness among a large sample of healthcare workers (HCW) during a public health crisis in a resource-limited setting, where mental wellness, such as depression, is often not measured nor documented.
We include a large number (n=24) of facilities to appreciate the heterogeneity in symptoms of depression among mental health in the sampled facilities in Lusaka Province of Zambia.
An important limitation is lack of data on demographics of HCW respondents due to concern about stigma around mental wellness and potential to identify individuals given inclusion of clinics with small staff.
Without pre-COVID-19 estimates of depression among HCWs in Lusaka, we are not able to show the association between mild-severe depression with the pandemic; however, we show that during the pandemic depression was high and attention to this population is justified to ensure a healthy HCW workforce.
We employed convenience sampling in selecting participants which may limit the representativeness of study results to the wider population of HCWs.
Introduction
COVID-19 has caused a substantial global health hardship and the position of healthcare workers (HCWs) on the frontlines of the public health response places them at great risk for negative effects on health and well-being.1 In addition to excess occupational hazard of contracting COVID-19, their experience as caregivers increases their risk of developing mental health disorders such as anxiety, depression, trauma, insomnia and stress, which may lead to poor physical and psychological well-being.2 A healthy workforce is critical to effectively managing and mitigating COVID-19, as well as providing continuity of high-quality care for other chronic and acute health conditions.3 4 Even prior to COVID-19, countries in sub-Saharan Africa faced limited medical infrastructures, supplies, and an overburdened workforce, which challenged HCW well-being and the provision of quality healthcare.5 6 These challenges, along with pandemic-sensitive barriers such as limited access to personal protective equipment (PPE), further exacerbated HCW stress and vulnerability. While HCWs in resource-limited settings have demonstrated resilience, poor mental health is likely to compromise their ability to make decisions, as well as impact patient interactions.7 Mental health services, like other health resources, are limited, with few trained mental health providers.8 Understanding the mental health and well-being among HCWs can catalyse interventions to provide treatment and improve the healthcare facility environment for the HCWs and patients.8
Several studies have been conducted to assess the mental wellness impact of the pandemic among HCWs; however, the majority of these studies focus on the continent of Asia and very little data are available for HCWs in Africa.9–11 Limited data from Kenya and Ethiopia provide evidence that the prevalence of mental disorders such as depression, insomnia and stress was higher among those HCWs caring for patients with COVID-19, or in areas of higher infection prevalence compared with those working with non-COVID-19 patients or less.2 12–16 The most prevalent reported mental health conditions among HCWs are depression, insomnia and anxiety.17 Characterisation of the state of mental wellness during the COVID-19 pandemic in sub-Saharan African countries among HCWs, specifically in Zambia, remains incomplete.12 18
As part of a larger patient-centred care study, we collected facility-level measures to understand the context of care at 24 study sites. As a part of establishing care context we assessed mental health, specifically depression, using the 9-question Patient Health Questionnaire (PHQ-9) in the context of COVID-19 among HCWs in Lusaka Province, Zambia from 11 August 2020 to 15 October 2020.19
Methods
Setting
This cross-sectional study of HCW depression is nested within a larger study, the Person-Centred Public Health for HIV Treatment in Zambia (PCPH), a cluster-randomised trial to assess HIV care and outcomes running from August 2018 to November 2021 across 24 government-funded health facilities in Lusaka Province (Pan African Clinical Trials Registry number: PACTR202101847907585). All PHQ-9 responses were collected between 11 August 2020 and 15 October 2020 among participating facilities that offered HIV care services and varied in size and location. Facilities were assigned codes to protect the identity of the HCW participants.
Study population
We developed a cohort of HCWs who primarily provide HIV care at one of the 24 health facilities in the PCPH study. This was done by compiling all contact details from the HCWs who had, at the time of the introduction of the depression study, participated in the HCW survey component of the original PCPH study. The PCPH sample comprised both professional HCWs, including nurses, pharmacists, midwives, medical doctors and radiographers, and lay HCWs including treatment supporters and general workers. To augment participation in the PHQ-9 data collection, we expanded the PHQ-9 sample to include any HCW willing to participate and had ≥6 months’ working experience at the study facility. We informed the facility in charge of the PHQ-9 study opportunity who communicated it to staff members.
Measurements
Trained study research assistants visited healthcare facilities and discussed the study opportunity in person with available staff members. Those who expressed interest were screened for eligibility, offered the opportunity to verbally consent and participate immediately in the PHQ-9 study. As a part of the PCPH adaptation to the COVID-19 pandemic, we implemented the 9-question Patient Health Questionnaire (PHQ-9) to screen for presence and severity of depression. The PHQ-9 has been previously used in Zambia to screen for likelihood of depression,19 and has been validated in Tanzania and South Africa which are similar settings as Zambia.19 20 The PHQ-9 instrument was translated from English into Nyanja and Bemba, the most commonly spoken Zambian languages in Lusaka Province, where the survey was conducted.21 Depending on the participant’s preference, the standard PHQ-9 survey was self-administered on paper or surveyor administered by trained study research assistants in the participant’s preferred language. Potentially identifying information such as age, sex and HCW cadre was not collected from respondents to protect privacy. Facility populations were categorised as small (<40 000 clients/year), medium (40 000–99 999 visits/year) and large (≥100 000 visits/year) as recorded in 2019.
Analysis
We followed the standard 27-point scoring system for the PHQ-9 to identify participants with scores consistent with minimal (0–4), mild (5–9), moderate (10–14), moderately severe (15–19) and severe depression (20-27).19–26 Our primary outcome was mild depression or greater (PHQ-9 score ≥5) as this level of depression warrants additional clinical follow-up.19 We developed frequency tables and used a bar graph to illustrate the distribution of PHQ-9 scores by healthcare facility. We developed scatter plots of adjusted marginal probability with 95% CIs to illustrate the probability that an HCW will have a PHQ-9 score ≥5 by healthcare facility. We used mixed-effects Poisson regression to estimate the prevalence ratios for those with mild depression allowing random effects at the facility level and measured fixed effects for month of survey and clinic size category. Facilities were categorised by client population estimates as: small (<40 000 clients), medium (40 000–100 000 clients) and large (>100 000 clients).
Patient and public involvement
The parent study focused primarily on improving the patient experience at routine clinic visits through HCW training, mentorship and audit and feedback. The research approach and content is based on participatory research with HCWs, human-centred design workshops and stakeholder collaborations.22–28 This research guided us to include measures of HCW satisfaction and well-being. In addition to an HCW experience measure throughout PCPH, the advent of COVID-19 led us to include an assessment of HCW depression. Patients were not directly involved in the design nor the recruitment of this substudy assessing the depression levels of HCWs. The findings of this study as well as the parent study will be shared with the Zambian Ministry of Health as well as the study facilities.
Results
A total of 713 HCWs from 24 facilities across Lusaka and Chongwe districts in the Lusaka Province were included in the analysis data set (table 1). The majority (69.6%) of the PHQ-9 survey responses were collected in September 2020 (table 1). The largest proportion of the responses was collected at facilities serving a large client population (41.7%), followed closely by facilities serving a medium-sized client population (37.7%) (table 1). Responses for PHQ-9 questions were largely complete with <1% of responses missing.
Table 1.
Participant characteristics
| Factor | Level | n (%) |
| N | 713 | |
| Facility | 1 | 30 (4.2) |
| 2 | 30 (4.2) | |
| 3 | 30 (4.2) | |
| 4 | 30 (4.2) | |
| 5 | 30 (4.2) | |
| 6 | 30 (4.2) | |
| 7 | 30 (4.2) | |
| 8 | 30 (4.2) | |
| 9 | 30 (4.2) | |
| 10 | 30 (4.2) | |
| 11 | 30 (4.2) | |
| 12 | 27 (3.8) | |
| 13 | 27 (3.8) | |
| 14 | 30 (4.2) | |
| 15 | 30 (4.2) | |
| 16 | 30 (4.2) | |
| 17 | 30 (4.2) | |
| 18 | 30 (4.2) | |
| 19 | 30 (4.2) | |
| 20 | 30 (4.2) | |
| 21 | 30 (4.2) | |
| 22 | 30 (4.2) | |
| 23 | 29 (4.1) | |
| 24 | 30 (4.2) | |
| Clinic population (category) | Small | 147 (20.6) |
| Medium | 269 (37.7) | |
| Large | 297 (41.7) | |
| Month of survey | August 2020 | 205 (28.8) |
| September 2020 | 496 (69.6) | |
| October 2020 | 12 (1.7) |
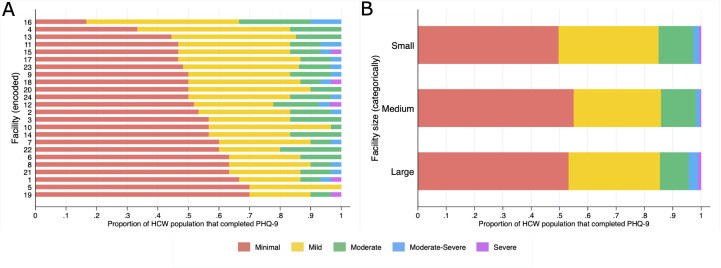
Of the 713 responses, 231 (32.4%, 95% CI 29.0%–36.0%) reported mild depression (PHQ-9 score 5–9), and 81 (11.4%, 95% CI 9.1%–13.9%) reported moderate depression (PHQ-9 score 10–14). A total of 81 (11.4%) respondents had a PHQ-9 score corresponding to moderate depression across all but one facility, 17 (2.4%, 95% CI 1.4%–3.8%) respondents had PHQ-9 scores consistent with moderately severe depression across four facilities and 5 (0.7%, 95% CI 0.2%–1.6%) HCWs had PHQ-9 scores consistent with severe depression across five different facilities (figure 1, online supplemental figure S1, table 2).
Figure 1.
(A) Stacked bar chart of proportion population by 9-question Patient Health Questionnaire (PHQ-9) score category by healthcare facility. (B) Stacked bar chart of proportion population by PHQ-9 score by facility population size category. HCW, healthcare worker.
Table 2.
Proportion of the analysis population by PHQ-9 score category with 95% CIs (N=713)
| Variable | n | Proportion (%) | 95% CI |
| PHQ-9 score ≥5 | 334 | 46.8 | 43.1, 50.6 |
| Mild | 231 | 32.4 | 29.0, 36.0 |
| Moderate | 81 | 11.4 | 9.1, 13.9 |
| Moderate-severe | 17 | 2.4 | 1.4, 3.8 |
| Severe | 5 | 0.7 | 0.2, 1.6 |
CI, confidence interval; PHQ-9, 9-question Patient Health Questionnaire.
bmjopen-2022-069257supp001.pdf (26KB, pdf)
Though we observed facility-level mental health heterogeneity in the proportion of minimal and mild depression scores across clinics, the proportion of scores consistent with moderate depression remains relatively stable across facilities (figure 1).
Mixed-effects adjusted Poisson regression model did not reveal clinic size or month of survey as a significant predictor of PHQ-9 score ≥5 (table 3).
Table 3.
Adjusted Poisson regression results (N=713)
| Covariate | Level | aPR | 95% CI | P value |
| Clinic population (category) | Small | 1.12 | 0.95, 1.33 | 0.170 |
| Medium | 1.00 (ref) | Ref | Ref | |
| Large | 1.04 | 0.81, 1.33 | 0.763 | |
| Month of survey | August | 1.00 (ref) | Ref | Ref |
| September | 1.14 | 0.94, 1.38 | 0.193 | |
| October | 0.98 | 0.54, 1.79 | 0.945 |
Adjusted for survey week and facility.
aPR, adjusted prevalence ratio; CI, confidence interval.
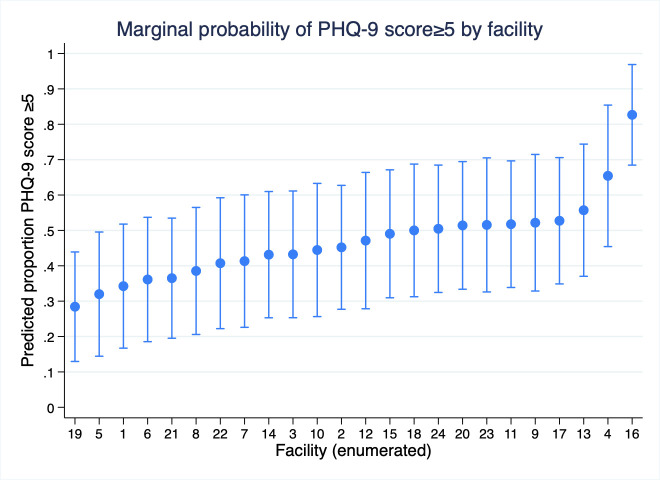
We illustrate significant heterogeneity in the marginal probability of experiencing greater than minimal depression across facilities (figure 2). Notably, the highest marginal probability of HCWs with PHQ-9 score ≥5 was observed in a facility serving as a COVID-19 treatment centre.
Figure 2.
Marginal probability of healthcare worker with greater than minimal depression (score ≥5) per 9-question Patient Health Questionnaire (PHQ-9) score by clinic.
Discussion
We found that a large proportion of the HCW population had a PHQ-9 score ≥5, indicating a need for follow-up to assess and improve mental well-being, 46.8% (95% CI 43.1%, 50.6%). Variation in depression outcomes ranged from 82.7% (95% CI 68.5%, 96.9%) at one of the two large COVID-19 treatment facilities to 28.4% (95% CI 13.0%, 43.9%) at a medium-sized healthcare facility.
Our study shows that HCWs working at the COVID-19 treatment facility had a higher marginal probability of experiencing mild to moderately severe depression. This is consistent with past studies showing that frontline HCWs working in clinics managing diseases considered to be highly infectious, such as COVID-19 treatment centres, were more prone to developing depression and other mental disorders compared to their counterparts in other departments.12 In addition, results of our study demonstrate that HCWs have experienced symptoms of depression during the onset of the COVID-19 pandemic in Zambia, which is aligned with the findings of similar studies using the PHQ-9 in other parts of the world where a pooled prevalence of mild depression was found to be 36.1% (95% CI 31.3%–41.0%).29 Studies conducted in Ethiopia among different cadres of HCWs show that mental disorders which include depression are prevalent among HCWs during the COVID-19 pandemic, with one study from Ethiopia identifying approximately 48% prevalence of greater than minimal depression, consistent with our Zambian estimates.30 31 Similarly, global studies indicate that there is a risk of HCWs experiencing mental health disorders during the pandemic.4 29 30 32 The difficult conditions to which HCWs may be exposed including extended working hours, risk of exposure to the disease, increased workload, concerns about transmitting the infection to their family members, reduced social connectedness and limited resources to care for their patients may amplify poor mental well-being.1 33–35
Further research is needed to understand the heterogeneity in proportions of HCWs with depression. It may be associated variation in HCW access to resources, such as PPE, hand hygiene station/station supplies at clinic entrance and knowledge about the COVID-19 response in Zambia. While the response to the COVID-19 pandemic was standardised, to a certain extent, by guidance from the provincial and zonal levels, the culture and leadership unique to each facility might have played a key role in the HCW experience, contributing to PHQ-9 score distribution differences across facilities.
As we continue to recognise the mental health services gap across many populations in resource-limited settings we give evidence here to support prioritisation of HCWs, especially during public health shocks/emergencies like that presented by COVID-19. Presence of depression among HCWs could lead to poor health outcomes for the HCW workforce and have a sort of ‘knock-on’ effect negatively impacting the quality of care provided to patients.36 37 Interventions like Friendship Bench piloted in neighbouring Zimbabwe designed to encourage positive coping mechanism among HCWs and build a working environment that provides empathy and compassion towards staff may be an efficient option to provide mental wellness support.38 39 Furthermore, system-based interventions should also be encouraged such as change in working culture and reduction in possible system contributors to HCW stress that could lead to depression. Increasing mobile technology availability may further allow for the use of mobile health-based mental wellness services leveraging the framework presented by Osei and Mashamba-Thompson for low and middle-income countries.40 41 Low-cost intervention packages used for patients can be adapted for HCWs and integrated into system-based interventions. They include routine screening for early detection, mental wellness education, problem solving, use of antidepressants, and cognitive–behavioural therapy which can be delivered successfully by trained lay HCWs.42 43
Limitations
This study had some potential limitations. First, we did not collect participant demographics such as age, sex and marital status to protect participant privacy, espeically at small clinics, where staff are few. Data for these potential confounders might help to better understand associations with depression. Second, we employed convenience sampling in selecting participants. This sampling approach may limit the representativeness of the study results to the wider population of HCWs. Finally, without pre-COVID-19 estimates of depression among HCWs in Lusaka, we are not able to show the association between mild-severe depression with the pandemic; however, we show that during the pandemic the depression was high and attention to this population is justified to ensure a healthy HCW workforce. Additionally, though potentially higher than a non-pandemic baseline, these results may be useful as subsequent measures of depression and mental wellness are collected among HCWs.
Conclusions
Depression is a common public health problem; our study demonstrates that HCWs in Zambia may suffer from a high prevalence of depressive symptoms that will require additional clinical follow-up. Routine mental health wellness is important to better understand the role that the COVID-19 pandemic may have had on depression among HCWs in Zambia. Furthermore, support for HCW mental wellness can serve to accelerate destigmatising mental health issues and improve the quality of care provided across healthcare centres in Zambia.
Supplementary Material
Acknowledgments
We thank the Zambian Ministry of Health for their leadership in ensuring that those in care continue to receive life-saving HIV treatment. We also thank the healthcare workers for their participation in the PHQ-9 assessment as well as their faithful delivery of care to patients in the face of the many challenges presented by the COVID-19 pandemic. To the clients seen at our study facilities, we extend our sincere thanks for your cooperation and patience.
Footnotes
Twitter: @aalokemody, @jakepry_epi
LKB and JMP contributed equally.
Contributors: SS: data collection, data framing and manuscript writing. JM, KS and MM: data collection and data curation. LJ and CB: data framing. ITS, CB-M and EG: conceptualisation. AM: manuscript review/editing. AS: conceptualisation and manuscript review/editing. LKB: conceptualisation, data analysis, data framing and manuscript writing. JMP: guarantor, data analysis lead, data framing and manuscript writing.
Funding: Research reported in this publication was supported by the Bill & Melinda Gates Foundation (grant number: OPP1166485), the National Institute of Mental Health of the National Institutes of Health (award number: F31MH109378 (LKB)) and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (award number: K24 AI134413 (EG)).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. De-identified data used for this analysis can be accessed via the Dryad data repository at http://datadryad.org/ with doi https://doi.org/10.25338/B8S646.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved as part of the larger PCPH study by the University of Zambia Biomedical Ethics Committee and the University of Alabama at Birmingham Institutional Review Board, and the National Health Research Authority in Zambia. We obtained waiver of written informed consent and obtained verbal consent from participants prior to administering the survey.
References
- 1.Yıldırım M, Çiçek İ, Şanlı ME. Coronavirus stress and COVID-19 burnout among healthcare staffs: the mediating role of optimism and social connectedness. Curr Psychol 2021;40:5763–71. 10.1007/s12144-021-01781-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robertson LJ, Maposa I, Somaroo H, et al. Mental health of healthcare workers during the COVID-19 outbreak: a rapid scoping review to inform provincial guidelines in South Africa. S Afr Med J 2020;110:1010–9. 10.7196/SAMJ.2020.v110i10.15022 [DOI] [PubMed] [Google Scholar]
- 3.Gupta S, Sahoo S. Pandemic and mental health of the front-line healthcare workers: a review and implications in the indian context amidst COVID-19. Gen Psychiatr 2020;33:e100284. 10.1136/gpsych-2020-100284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saragih ID, Tonapa SI, Saragih IS, et al. Global prevalence of mental health problems among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. International Journal of Nursing Studies 2021;121:104002. 10.1016/j.ijnurstu.2021.104002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ayanore MA, Amuna N, Aviisah M, et al. Towards resilient health systems in sub-Saharan Africa: a systematic review of the english language literature on health workforce, surveillance, and health governance issues for health systems strengthening. Ann Glob Health 2019;85:113. 10.5334/aogh.2514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Semo B-W, Frissa SM. The mental health impact of the COVID-19 pandemic: implications for sub-Saharan Africa. Psychol Res Behav Manag 2020;13:713–20. 10.2147/PRBM.S264286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Med S. Serious health workforce shortage in Zambia: solidar med. 2020. Available: https://www.solidarmed.ch/en/news/shortage-skilled-workers-health-system-zambia
- 8.Munakampe MN. Strengthening mental health systems in Zambia. Int J Ment Health Syst 2020;14:28.:28. 10.1186/s13033-020-00360-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deng D, A Naslund J. Psychological impact of COVID-19 pandemic on frontline health workers in low- and middle-income countries. Harv Public Health Rev 2020;28. 10.54111/0001/Z1 Available: https://hphr.org/edition-26-covid-19/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moitra M, Rahman M, Collins PY, et al. Mental health consequences for healthcare workers during the COVID-19 pandemic: a scoping review to draw lessons for lmics. Front Psychiatry 2021;12:602614. 10.3389/fpsyt.2021.602614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ceri V, Cicek I. Psychological well-being, depression and stress during COVID-19 pandemic in Turkey: a comparative study of healthcare professionals and non-healthcare professionals. Psychol Health Med 2021;26:85–97. 10.1080/13548506.2020.1859566 [DOI] [PubMed] [Google Scholar]
- 12.Shah J, Monroe-Wise A, Talib Z, et al. Mental health disorders among healthcare workers during the COVID-19 pandemic: a cross-sectional survey from three major hospitals in Kenya. BMJ Open 2021;11:e050316. 10.1136/bmjopen-2021-050316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chersich MF, Gray G, Fairlie L, et al. COVID-19 in africa: care and protection for frontline healthcare workers. Global Health 2020;16:46. 10.1186/s12992-020-00574-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yitayih Y, Mekonen S, Zeynudin A, et al. Mental health of healthcare professionals during the early stage of the COVID-19 pandemic in Ethiopia. BJPsych Open 2020;7:e1. 10.1192/bjo.2020.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jemal K, Deriba BS, Geleta TA, et al. Self-reported symptoms of depression, anxiety, and stress among healthcare workers in ethiopia during the COVID-19 pandemic: a cross-sectional study. Neuropsychiatr Dis Treat 2021;17:1363–73. 10.2147/NDT.S306240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asnakew S, Amha H, Kassew T. Mental health adverse effects of COVID-19 pandemic on health care workers in north west Ethiopia: a multicenter cross-sectional study. Neuropsychiatr Dis Treat 2021;17:1375–84. 10.2147/NDT.S306300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sahebi A, Nejati-Zarnaqi B, Moayedi S, et al. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry 2021;107:110247. 10.1016/j.pnpbp.2021.110247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elbay RY, Kurtulmuş A, Arpacıoğlu S, et al. Depression, anxiety, stress levels of physicians and associated factors in COVID-19 pandemics. Psychiatry Res 2020;290:113130.:113130. 10.1016/j.psychres.2020.113130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–13. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JBW, et al. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry 2010;32:345–59. 10.1016/j.genhosppsych.2010.03.006 [DOI] [PubMed] [Google Scholar]
- 21.Sawka KS, Mbewe C, Josephat D, et al. The senga of Zambia: linguistic survey report with recommendations for literature development strategy. SIL International, 2021. [Google Scholar]
- 22.Beres LK, Simbeza S, Holmes CB, et al. Human-centered design lessons for implementation science: improving the implementation of a patient-centered care intervention. J Acquir Immune Defic Syndr 2019;82:S230–43. 10.1097/QAI.0000000000002216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mody A, Tram KH, Glidden DV, et al. Novel longitudinal methods for assessing retention in care: a synthetic review. Curr HIV/AIDS Rep 2021;18:299–308. 10.1007/s11904-021-00561-2 [DOI] [PubMed] [Google Scholar]
- 24.Sikombe K, Mody A, Kadota J, et al. Understanding patient transfers across multiple clinics in Zambia among HIV infected adults. PLoS One 2020;15:e0241477. 10.1371/journal.pone.0241477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holmes CB, Sanne I. Changing models of care to improve progression through the HIV treatment cascade in different populations. Curr Opin HIV AIDS 2015;10:447–50. 10.1097/COH.0000000000000194 [DOI] [PubMed] [Google Scholar]
- 26.Holmes CB, Sikazwe I, Sikombe K, et al. Estimated mortality on HIV treatment among active patients and patients lost to follow-up in 4 provinces of Zambia: findings from a multistage sampling-based survey. PLoS Med 2018;15:e1002489. 10.1371/journal.pmed.1002489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roy M, Czaicki N, Holmes C, et al. Understanding sustained retention in HIV/AIDS care and treatment: a synthetic review. Curr HIV/AIDS Rep 2016;13:177–85. 10.1007/s11904-016-0317-9 [DOI] [PubMed] [Google Scholar]
- 28.Mwamba C, Sharma A, Mukamba N, et al. “They care rudely!”: resourcing and relational health system factors that influence retention in care for people living with HIV in Zambia. BMJ Glob Health 2018;3:e001007. 10.1136/bmjgh-2018-001007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li Y, Scherer N, Felix L, et al. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. PLoS One 2021;16:e0246454. 10.1371/journal.pone.0246454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mulatu HA, Tesfaye M, Woldeyes E, et al. The prevalence of common mental disorders among healthcare professionals during the COVID-19 pandemic at a tertiary hospital in Addis ababa, Ethiopia. J Affect Disord Rep 2021;6:100246. 10.1016/j.jadr.2021.100246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yadeta TA, Dessie Y, Balis B. Magnitude and predictors of health care workers depression during the COVID-19 pandemic: health facility-based study in eastern Ethiopia. Front Psychiatry 2021;12:654430. 10.3389/fpsyt.2021.654430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fond G, Fernandes S, Lucas G, et al. Depression in healthcare workers: results from the nationwide AMADEUS survey. Int J Nurs Stud 2022;135:104328. 10.1016/j.ijnurstu.2022.104328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mokhtari R, Moayedi S, Golitaleb M. COVID-19 pandemic and health anxiety among nurses of intensive care units. Int J Ment Health Nurs 2020;29:1275–7. 10.1111/inm.12800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pfefferbaum B, North CS. Mental health and the covid-19 pandemic. N Engl J Med 2020;383:510–2. 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- 35.Yıldırım M, Çiçek İ. Optimism and pessimism mediate the association between parental coronavirus anxiety and depression among healthcare professionals in the era of COVID-19. Psychol Health Med 2022;27:1898–906. 10.1080/13548506.2021.1966702 [DOI] [PubMed] [Google Scholar]
- 36.Saasa Y. An assessment on the role of human rights and governance in health service delivery. 2019. [Google Scholar]
- 37.Kola L, Kohrt BA, Hanlon C, et al. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry 2021;8:535–50. 10.1016/S2215-0366(21)00025-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abraham A, Chaabna K, Doraiswamy S, et al. Depression among healthcare workers in the eastern mediterranean region: a systematic review and meta-analysis. Hum Resour Health 2021;19:81. 10.1186/s12960-021-00628-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wallén A, Eberhard S, Landgren K. The experiences of counsellors offering problem-solving therapy for common mental health issues at the youth friendship bench in Zimbabwe. Issues Ment Health Nurs 2021;42:808–17. 10.1080/01612840.2021.1879977 [DOI] [PubMed] [Google Scholar]
- 40.Osei E, Mashamba-Thompson TP. Mobile health applications for disease screening and treatment support in low-and middle-income countries: a narrative review. Heliyon 2021;7:e06639. 10.1016/j.heliyon.2021.e06639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mutimushi PM, Mupenda BM, Manda PM, et al. ZICTA 2019 annual report: Zambia information and communications technology authority (ZICTA). 2019. Available: https://www.zicta.zm/storage/posts/attachments/oiBT4oMnpJoN3dgHKpvByoDmNXq5ZDYtp3sxVYM3.pdf
- 42.Chibanda D, Mesu P, Kajawu L, et al. Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health 2011;11:828. 10.1186/1471-2458-11-828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Patel V, Simon G, Chowdhary N, et al. Packages of care for depression in low- and middle-income countries. PLoS Med 2009;6:e1000159. 10.1371/journal.pmed.1000159 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-069257supp001.pdf (26KB, pdf)
Data Availability Statement
Data are available upon reasonable request. De-identified data used for this analysis can be accessed via the Dryad data repository at http://datadryad.org/ with doi https://doi.org/10.25338/B8S646.