Abstract
Introduction
Acculturation‐related characteristics, that is, factors directly connected to culture and familial relationships, are associated with engaged research participation within Latino communities. Despite this, little empirical data exists on whether acculturation changes over time in older Latinos, which has potential implications for Alzheimer's disease and related dementias (ADRD) research study design including longer duration clinical trial implementation.
Methods
Self‐identified Latinos (n = 222; mean age = 71, 76% female) participating in one of three ongoing longitudinal community‐based cohort studies of aging who reported their nativity outside of the United States/District of Columbia (US/DC) contributed, on average, 4.0 ± 1.2 years of annually collected data. This included acculturation‐related characteristics of total, language‐, and social‐based scores from the Short Acculturation Scale for Hispanics (SASH) and total and domain‐specific scores from an abbreviated Sabogal Familism questionnaire. We used ordinal mixed effects models and linear mixed effects models (as appropriate) to assess change in acculturation metrics after adjusting for age, sex, education, income, and duration of time in the US/DC.
Results
Although none of the SASH metrics changed over time (P‐values ≥ 0.25), all Familism metrics declined over time (P‐values ≤ 0.044). Additionally, select participant‐based characteristics including years of education were significantly (and differentially) associated with level of, but not change in, acculturation‐related outcomes.
Discussion
Results suggest that specific acculturation‐related factors (i.e., familism) change over time in older Latinos, and participant‐based characteristics associated with baseline levels of (but not change in) acculturation more generally. Thus, acculturation‐related characteristics are not all static, trait‐like qualities but rather a multi‐faceted, and at times evolving, construct. Considering this dynamic phenotyping is important when contextualizing older Latinos’ lived experience, and when designing, adapting, and conducting ADRD clinical trials and other health‐related interventions.
Keywords: acculturation, Alzheimer's disease and related dementias clinical trials, familism, Hispanics, inclusion science, Latinos, longitudinal change
1. BACKGROUND
Inclusion science focuses on understanding and addressing the under‐inclusion of members from minoritized communities, such as older Latinos, 1 in translational research and clinical interventions. Consisting of essential elements such as equitable study design, engagement, recruitment, and sustainable research participation, 2 inclusion science requires investment in diverse communities, including the recognition of unique/key aspects of the lived experience within them. 3 A key aspect of the lived experience of older Latinos in the United States is acculturation, traditionally defined as adapting to a new environment and potentially adopting its values and practices; however, the exploration of acculturation to inform inclusion science has too often taken place outside of the Alzheimer's disease and related dementias (ADRD) field. For example, within cancer research, adapting and/or adopting US‐based practices including, but not limited to, greater use of the English language has been associated with greater participation in preventative screenings and care use among Latinos. 4 , 5 In contrast, Spanish‐speaking Latinas were six times more likely to participate in actual cancer‐related randomized clinical trials (RCTs) than their Spanish‐/English‐speaking counterparts. 6 Additionally, Latino‐centric ethos including familial obligations and support, and family as a critical referent (i.e., familism) have also been shown to positively predict mid‐ to late‐life Latinos’ preventative screening and care use 7 and participation in RCT‐ 6 , 8 and non–RCT‐based interventions. 9
Despite this knowledge gained, almost all our information about late‐life acculturation in Latinos is from cross‐sectional research, 10 and little has been done to incorporate this information into the design and implementation of ADRD clinical trials. These gaps make it difficult to answer calls to consider acculturation‐related characteristics in ADRD study design and implementation, 11 including those specific for Latino communities that encourage the “family as participant.” 12 Given our limited understanding of whether acculturation changes over time in older Latinos, it remains unclear how best to incorporate their beliefs into a more culturally compatible approach to ADRD research for this historically under‐included community.
We examine longitudinal change in acculturation, specifically overall, language‐, and social‐based acculturation and familism, in older Latinos participating in Rush Alzheimer's Disease Center (RADC) cohort studies. We focused on older Latinos who reported their birth outside of the 50 United States and/or the District of Columbia (US/DC) given differences in acculturation‐related experiences between US‐ and non–US‐born individuals. 13 , 14 Reports in the literature, focused primarily on younger adults, 15 , 16 , 17 suggest that social‐ and family‐based metrics of acculturation do change over time and result in corresponding changes to behavior (e.g., decreasing familism/increasing depression 16 ) leading researchers to advocate for interventions to treat depression that encourage the retention of a familism ethos specific to the Latino culture. Likewise, a lifespan study of caregivers (age range: 18–84 years) 18 found that although feelings of family loyalty, reciprocity, and solidarity (i.e., familism) declined over time, those with higher familism reported more positivity about engaging in caregiving. Thus, we hypothesized that social‐based levels of acculturation and familism would decline over time in older Latinos; however, language‐based acculturation would not change. Additionally, we explored the role of key contributors (e.g., age, education, time in the US/DC) to these longitudinal trajectories. Understanding if and how aspects of acculturation change over time (and what may be associated with such change) could not only shed light on the evolving lived experience of older Latinos, but also set the stage for future studies investigating how these changing perspectives may inform culturally compatible approaches to ADRD research.
2. METHODS
2.1. Consent statement
All participants gave written informed consent in accordance with the Declaration of Helsinki.
2.2. Participants
As previously discussed, 19 , 20 participants were self‐identified Latinos enrolled in one of three ongoing longitudinal community‐based cohort studies of aging: the Rush Memory and Aging Project (MAP; 1997 to present), 21 the RADC Latino Core (2015 to present), 20 or the Religious Orders Study (ROS; 1994 to present). These studies are identical in essential details (e.g., a harmonized protocol that includes the same acculturation measures) and enroll older Latinos free of known dementia at baseline who agree to annual, in‐home, evaluations. Brain donation at the time of death is a condition of MAP and ROS study entry; it is optional for the Latino Core. These cohort studies are conducted by the same bilingual investigators with a single population studies team to ensure data can be efficiently merged and compared. An institutional review board of Rush University Medical Center approved all studies.
At the time of these analyses, 332 Latinos had completed a baseline evaluation including our acculturation metrics (introduced at the RADC in 2016). We excluded eight participants diagnosed with dementia at baseline using a uniform structured clinical evaluation 22 and National Institute of Neurological and Communicative Disorders and Stroke/Alzheimer's Disease and Related Disorders Association criteria. 23 We excluded 57 Latinos who self‐reported their birth within the 50 states and/or the District of Columbia (US/DC). Individuals born in the US territory of Puerto Rico were included given that migration to the US/DC includes experiences that may change levels of acculturation regardless of an individual's point of origin. 19 This left 267 Latinos eligible for inclusion, 83% of whom had ≥2 longitudinal follow‐up evaluations (45 participants had only completed 1 evaluation). Thus, a total of 222 Latinos reporting their nativity outside of US/DC contributed a mean follow‐up of 4.0 ± 1.2 years (range = 2–6 years) of data to our analytic sample.
2.3. Acculturation
The Short Acculturation Scale for Hispanics (SASH) 13 consists of 10 items that ask participants to self‐report their Spanish/Latino and/or English/non‐Latino preferences across a variety of language and socially based situations. Language‐based questions (six in total) focus on what language(s) a participant reads/speaks generally and in specific situations including at home and with friends, used as a child, currently thinks in, and uses to engage in entertainment like movies or television. These questions use a 5‐point Likert scale: 1 = only Spanish to 5 = only English. Social‐based questions (four in total) ask about who a participant's close friends are, and participant preferences at social gatherings and visits as well as when “choosing” family friends using a 5‐point Likert scale: 1 = all Hispanic/Latino to 5 = all non‐Hispanic/non‐Latino. For all questions, 3 = both equally/about half and half. The SASH total score is the mean of all 10 items; the language‐ and social‐based scores are the mean of 6 and 4 items, respectively. For all scores, a higher score (max = 5) indicates levels of acculturation that move away from only Spanish toward only English (median scores represent both equally). Internal consistency of items was adequate: total score (polychoric Cronbach's alpha = 0.95), language‐ (polychoric Cronbach's alpha = 0.97), and social‐based (polychoric Cronbach's alpha = 0.85) subscores.
RESEARCH IN CONTEXT
Systematic Review: The authors reviewed the literature using traditional (e.g., PubMed) sources, which revealed a dearth of information on changes in acculturation in older Latinos.
Interpretation: Our article is, to our knowledge, one of the only studies providing statistical evidence of changes in acculturation over time in older Latinos. It provides evidence that acculturation‐related characteristics are not all static, trait‐like qualities but rather a multi‐faceted, and at times evolving, construct important to consider when contextualizing the aging process in this population.
Future Directions: Given that specific aspects of acculturation appear to facilitate willingness to engage in participatory research, knowledge of how these aspects do or do not change over time may help inform inclusion science approaches to designing and conducting culturally compatible Alzheimer's disease and related dementia clinical trials and health‐related interventions.
The Sabogal Familism measure 24 consists of 14 items assessing aspects of familial identity in Latino communities including family obligation, perceived support, and referents. 25 We administered an abbreviated 6‐item version of this scale, with questions specifically chosen to sample all three aspects of the original 14‐item scale including familial obligation (e.g., “Aging parents should live with relatives”), perceived support (e.g., “When someone has problems he/she can count on help from his/her relatives”), and family as referent (e.g., “One should be embarrassed about the bad things done by his/her brothers and sisters”). Participants rated each item using a 5‐point Likert scale: 1 = disagree a lot to 5 = agree a lot. Responses for all 6 items were summed to create a total score (max = 30; higher score = higher familism). As previously reported, 25 internal consistency of Familism items fell below threshold (≥0.60). 26 In keeping with other studies, 24 , 25 we performed a principal component analysis (PCA) on our six Familism items. Leveraging data from the entire Latino cohort (n = 255 regardless of immigration status), the unrotated PCA resulted in two distinct factor loadings (48.3% of the variance). Factor 1 (28.0% of the variance) consisted of questions pertaining to familial obligation and family as referent; Factor 2 (20.3% of the variance) consisted of familial expectations that were aspirational and/or support related (Table 1). Given the orthogonal nature of the unrotated loadings and that the resulting factor structure was in keeping with previously reported factor structures using identical Familism items, 24 , 25 we did not perform varimax rotation. These factor loadings served as the basis for the creation of two composite scores (i.e., obligation/referent and expectation) that augmented our investigation of the Familism total score.
TABLE 1.
Principal component analysis of Familism items.
| Factor 1 | Factor 2 | |
|---|---|---|
| Much of what a son or daughter does should be done to please the parents. | 0.74029 | −0.14389 |
| Children should live in their parents’ house until they get married | 0.67350 | −0.15059 |
| Aging parents should live with relatives. | 0.53932 | 0.20090 |
| One should be embarrassed about the bad things done by his/her brothers and sisters. | 0.50448 | −0.20053 |
| One should have the hope of living long enough to see his/her grandchildren grow up. | −0.07488 | 0.76192 |
| When someone has problems he/she can count on help from his/her relatives. | 0.36042 | 0.71530 |
| Eigenvalue = 1.68 | Eigenvalue = 1.21 |
Note: Factor loadings are unrotated with bold values representing the primary loading for each item.
2.4. Participant‐based characteristics
In addition to age, sex, and years of education, we considered income and duration of time in the US/DC as additional participant‐based characteristics that may impact longitudinal change in acculturation. Income was measured by asking participants to select 1 of 10 levels of total income (level 1 = $0–$4999 to level 10 = $75,000 and over) outlined on a show‐card that represented their personal income for the past month or year. 27 Participants were queried for the number of years living in the US/DC. All characteristics were evaluated at study baseline. We chose a limited number of participant‐based characteristics given our small and somewhat bespoke analytic sample (i.e., older Latinos who reported their birth outside of the US/DC); more work will be needed in larger samples to explore other possible contributors to longitudinal change in acculturation should it exist.
2.5. Statistical analysis
Descriptive summaries of all variables were conducted. Given that the distributions of individual SASH scores at each evaluation were skewed with a marked floor and ceiling, we rounded each score to the nearest integer (i.e., 1, 2, 3, 4, or 5) combining sparse observations at the end of the ordinal distribution. A similar approach was taken for the expectation composite score derived from the Familism PCA; thus, we grouped total scores on this composite into an ordinal distribution (i.e., scores ≤7 were recoded into a score of 1, scores of 8 into a score of 2, 9 into 3, and 10 into 4). Ordinal mixed effect models were then used to assess longitudinal change in the odds of having higher acculturation‐related characteristics (SASH total, language‐ and social‐based scores, and familial expectations, separately). Linear mixed effects models were used to assess longitudinal change in Familism total and the obligation/reference factor‐based composite score.
Regardless of approach, a crude model included only a term for time since baseline testing (years of study participation); demographics‐adjusted Model 1 added terms for age, sex, education, and interactions of each of these variables with time; and the fully adjusted Model 2 further added income and years in the US/DC along with interactions of each of these variables with time. Model building was conducted to detect potentially different outcomes based on the two groups of participant‐based characteristics. Missing data were not imputed; instead, models allowed for listwise deletion as relevant. Models were carefully examined graphically and analytically. This included analysis of the proportionality of odds score tests or presence of trend in odds 28 and analysis of residual of the linear mixed effects. Model assumptions were found to be adequately met. Analyses were conducted using SAS/STAT software, version 9.4 (SAS Institute); significance was set at P < 0.05.
3. RESULTS
Participants (n = 222) were on average 71 years of age, primarily female, with ≈10 years of education and an average income range of $20,000 to $24,999. Eighty‐five percent of participants were tested in Spanish and reported an average of 42 years in the US/DC. Self‐reported country of origin was predominantly Mexico (n = 123) or Puerto Rico (n = 35). Additional information may be found in Table 2.
TABLE 2.
Participant characteristics at baseline.
| n = 222 | |
|---|---|
| Age (years) | 71.46 (6.52) |
| Sex (male:female ratio) | 53:169 |
| Education (years) | 10.17 (4.92) |
| Income (level) | 5.14 (2.55) |
| Income ($ range for average level) | $20,000–$24,999 |
| Time in the US/DC | 42.16 (14.42) |
| Self‐reported country of origin (n, %) | |
| Mexico | 123, 55.4% |
| Puerto Rico | 35, 15.7% |
| South America | 17, 7.6% Ecuador = 8, Columbia = 6, Peru = 3 |
| Central America | 8, 3.6% Honduras = 4, Guatemala = 3, El Salvador = 1 |
| Cuba | 2, 1% |
| Missing | 37, 16.7% |
| Acculturation‐related outcomes | |
| SASH total score | 1.94 (0.63) |
| SASH language subscore | 1.76 (0.78) |
| SASH social subscore | 2.21 (0.59) |
| Familism | 20.57 (2.94) |
Note: All values are mean (standard deviation) unless otherwise noted.
Abbreviations: SASH, Short Acculturation Scale for Hispanics; US/DC, the 50 United States and/or the District of Columbia.
3.1. Change in acculturation
In crude models, there was no change over time in the SASH total (P = 0.24) or subscores (language P = 0.08; social P = 0.61). Adding age, sex, and education to demographics‐adjusted Model 1 did not change these results (P‐values ≥ 0.31). In fully adjusted Model 2 with additional terms for income, years in the US/DC, and their interactions with time, none of the SASH scores changed over time (P‐values ≥ 0.25).
As seen in Table 3, which displays fully adjusted Model 2 details including terms for all participant‐based characteristics, more educated participants had higher odds of elevated scores on all three SASH measures at baseline (P‐values < 0.001). Additionally, younger participants had higher odds of elevated SASH total (P = 0.026) and language‐based (P = 0.008) scores at baseline. Income at baseline was associated with baseline levels of language‐based acculturation only, and the more years participants’ reported living in the US/DC, the higher their odds of having elevated baseline SASH scores regardless of type (Model 2 details in Table 3). Sensitivity analysis excluding the SASH question regarding what language(s) a participant used as a child (presumably a static response) did not change any previously reported results (data not shown).
TABLE 3.
Changes in acculturation‐related outcomes and key characteristics associated with the fully adjusted ordinal mixed effects models for the Short Acculturation Scale for Hispanics.
| SASH | |||
|---|---|---|---|
| Total score | Language score | Social score | |
| Time in study | −0.07 (0.15), P = 0.63 | −0.05 (0.18), P = 0.76 | −0.15 (0.13), P = 0.25 |
| Age | −0.09 (0.04), P = 0.026 | −0.16 (0.06), P = 0.008 | −0.006 (0.03), P = 0.84 |
| Sex | 0.51 (0.54), P = 0.33 | 0.60 (0.75), P = 0.41 | 0.05 (0.40), P = 0.89 |
| Education | 0.39 (0.05), P < 0.0001 | 0.56 (0.08), P < 0.0001 | 0.23 (0.04), P < 0.0001 |
| Income | 0.09 (0.10), P = 0.38 | 0.33 (0.24), P = 0.02 | −0.02 (0.08), P = 0.75 |
| US/DC years | 0.14 (0.02), P < 0.0001 | 0.22 (0.03), P < 0.0001 | 0.04 (0.01), P = 0.001 |
| Age x time | 0.009 (0.01), P = 0.42 | 0.004 (0.01), P = 0.73 | 0.007 (0.01), P = 0.47 |
| Sex x time | 0.15 (0.15), P = 0.30 | 0.14 (0.16), P = 0.35 | 0.10 (0.13), P = 0.42 |
| Education x time | 0.01 (0.01), P = 0.24 | 0.01 (0.01), P = 0.48 | −0.01 (0.01), P = 0.35 |
| Income x time | 0.02 (0.02), P = 0.43 | −0.02 (0.03), P = 0.46 | 0.03 (0.02), P = 0.17 |
| US/DC years*time | 0.003 (0.005), P = 0.53 | 0.008 (0.006) P = 0.19 | −0.0007 (0.004), P = 0.86 |
Note: Values are estimates (standard errors), P‐value from separate fully adjusted ordinal mixed effect models (i.e., Model 2); bolded values denote significance levels with significance set at P < 0.05 while the bolded term/row denotes the main predictor of interest.
Abbreviations: SASH, Short Acculturation Scale for Hispanics; US/DC, the 50 United States and/or the District of Columbia.
Familism scores declined over time in crude (estimate = −0.28, standard error [SE] = 0.04, P < 0.0001) and demographics‐adjusted (estimate = −0.28, SE = 0.05, P < 0.0001) models. After adding terms for income, years in the US/DC, and their interactions with time, fully adjusted Model 2 continued to provide evidence that familism declined over time (on average, 1.21 points over the average follow‐up period of 4 years; Figure 1). Education was the only participant‐based characteristic associated with baseline familism in Model 2 such that higher levels of education associated with lower levels of familism (Table 4).
FIGURE 1.
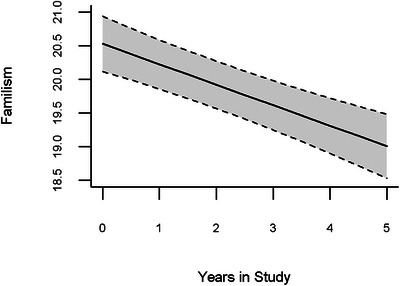
Representation of change in familism over time with 95% confidence intervals also depicted in fully adjusted models (i.e., Model 2) accounting for age, sex, education, income, years living in one of the 50 US states and/or the District of Columbia, and interactions of each of these variables with time. Years in study as reflected on the x‐axis begins at study baseline (i.e., “0”) with each subsequent visit representing the first (“1”) repeat visit, the second (“2”) repeat visit, and so on, with “5” representing the fifth repeat visit. Given visits are annual and started with baseline, the fifth repeat visit equates to the 6th year in the study.
TABLE 4.
Changes in acculturation‐related outcomes and key characteristics associated with the fully adjusted statistical models for Familism.
| Familism | |||
|---|---|---|---|
| Total score | Obligation/referent | Expectation | |
| Time in study | −0.24 (0.12), P = 0.044 | −0.15 (0.04), P = 0.0007 | −0.37 (0.05), P < 0.0001 |
| Age | −0.01 (0.03), P = 0.72 | 0.03 (0.02), P = 0.25 | −0.09 (0.02), P = 0.0002 |
| Sex | 0.65 (0.42), P = 0.12 | 0.45 (0.37) P = 0.22 | 0.54 (0.31) P = 0.090 |
| Education | −0.14 (0.04), P = 0.0005 | −0.16 (0.03), P < 0.0001 | 0.03 (0.03), P = 0.22 |
| Income | −0.10 (0.08), P = 0.22 | −0.06 (0.07), P = 0.36 | −0.06 (0.06) P = 0.33 |
| US/DC years | −0.02 (0.01), P = 0.12 | −0.02 (0.01), P = 0.077 | 0.008 (0.01), P = 0.42 |
| Age x time | −0.001 (0.01), P = 0.92 | −0.007 (0.008), P = 0.36 | 0.01 (0.008) P = 0.17 |
| Sex x time | 0.04 (0.11), P = 0.69 | 0.07 (0.09), P = 0.47 | −0.09 (0.11), P = 0.41 |
| Education x time | 0.008 (0.01), P = 0.47 | 0.01 (0.01) P = 0.18 | −0.008 (0.01) P = 0.43 |
| Income x time | −0.01 (0.02), P = 0.54 | −0.02 (0.01), P = 0.30 | 0.01 (0.02), P = 0.58 |
| US/DC years x time | 0.005 (0.004) P = 0.19 | 0.004 (0.003), P = 0.19 | −0.0007 (0.003) P = 0.84 |
Note: Values are estimates (standard errors), P‐value from separate fully adjusted models (i.e., Model 2) linear mixed effect model for familism total score and obligation/referent composite outcomes, and an ordinal mixed effect model for the Familism expectation composite score outcome; bolded values denote significance levels with significance set at P < 0.05 while the bolded term/row denotes the main predictor of interest.
Abbreviation: US/DC, the 50 United States and/or the District of Columbia.
Both Familism factor‐derived composite scores declined over time in crude (obligation/referent estimate = −0.128, SE = 0.04, P = 0.001; expectation estimate = −0.380, SE = 0.04, P < 0.0001), demographics‐adjusted (obligation/referent estimate = −0.15, SE = 0.04, P = 0.0007; expectation estimate = −0.36, SE = 0.05, P < 0.0001) and fully adjusted (P‐values ≤ 0.007) models. Also in fully adjusted Model 2, education was the only participant‐based characteristic associated with the baseline obligation/referent composite (i.e., higher education, lower obligation/referent), while only age was associated with the baseline expectation composite (i.e., higher age, lower expectation). Table 4 contains all Model 2 details.
4. DISCUSSION
In this study of more than 200 older Latinos, select aspects of older Latinos’ acculturation‐related experiences changed over time. As hypothesized, levels of familism declined over time and language‐based acculturation did not change. In contrast, older Latinos’ social‐based levels of acculturation did not change. Results suggest that while language‐ and social‐based acculturation may represent long‐held beliefs for older Latinos, familism may represent a changing cultural ethos for these same individuals. These results may help inform inclusion science approaches to culturally compatible ADRD research including how and whom to engage for successful recruitment and study sustainability. For example, given that language‐based acculturation did not change over time, researchers taking time to understand language use and proficiency of older Latinos at the inception of their study should have confidence that this acculturation‐related characteristic likely will not change over the course of their research. Thus, initial procedures put in place to accommodate levels of language‐based acculturation (e.g., monolingual Spanish) can and should remain in place in perpetuity. Furthermore, long‐term engagement of older Latinos in clinical trials, regardless of language spoken, may be facilitated by involving family in outreach, education, and the research process more generally. 12 Thus, knowing that familism declines over time, and is a predictor of participatory research for Latinos, 6 , 8 , 9 researchers should regard promoting this Latino‐centric ethos as critical for models of ADRD inclusion science.
Separate from implications for ADRD inclusion science, this study contributes to the broader literature on acculturation in Latinos. First, to our knowledge, this is one of the only studies investigating changes in acculturation over time in older Latinos. Second, it confirms and extends reports of changes in familism previously documented in younger Latinos 15 , 16 , 17 , 18 to an older cohort. Third, our work supports previous qualitative commentary regarding “minimal change” observed in language‐based acculturation for US‐based Puerto Ricans 29 and extends this to include a formal statistical test of acculturation‐related change in a more diverse group of older Latinos born outside of the US/DC. Another contribution is that our work explored the role of participant‐based characteristics on stability and change in acculturation, finding that these characteristics differentially associate with baseline levels of (but not change in) acculturation. Specifically, we confirmed the relationships of education and years in the US/DC 30 with language‐ and social‐based acculturation, as well as the relationships of age 31 and income 32 with language‐based acculturation and extended these results to older Latinos. Our study also found that age and education are differentially related to aspects of familism, extending previous work in adolescent Latinos 33 to an older age cohort. More work in older Latinos is needed to understand the underlying mechanisms for these associations (e.g., Bleakley and Chin 32 ) and determine whether other, not yet investigated, contributors including individual‐level stressors and/or social determinants of health impact acculturation either at baseline or over time.
Longitudinal change in familism was evidenced, even when dividing this construct into PCA‐derived composite scores. These composite scores did allow for the discovery of differential relationships of baseline age and education with levels of familial expectations and obligations/referents, respectively. The fact that older participants showed lower familial expectations supports previous work suggesting that there may be generational 34 , 35 effects to this cultural construct. Furthermore, it may be that older Latinos’ lower familism‐related expectations at baseline, and declines over time more generally, stem from their experiences with younger generations of Latinos, many born in the US/DC, who may not manifest their elders’ desired levels of familism. 36 , 37 Higher levels of education were associated with lower levels of familial obligation/referent perceptions. While an important consideration in its own right, this relationship may be confounded by reasons for immigration and/or individualized experiences and opportunities upon arrival. 36 More work is needed to disentangle these possibilities.
None of our SASH metrics showed evidence of change over time, even after removing the presumably static question related to the language(s) spoken as a child. The lack of change in self‐reported language‐ and social‐based acculturation is likely due, in part, to the fact that our participants, on average, reported considerable time in the US/DC. This rationale, in addition to older age, was also discussed by Vercammen et al. as part of their qualitative commentary on the minimal change in language‐based acculturation seen over 2 and 5 years of follow‐up in their Boston Puerto Rican Health Study. 29 These explanations are bolstered by the fact that both age and duration of time in the US/DC were associated with our participants’ baseline levels of SASH‐measured acculturation. Although many investigators working with Latinos (rightly) state that language and/or social‐based acculturation does not change over time, few studies have empirically tested this assumption. 10 Studies that have discussed this assumption have either deemed the unit change insufficient for formal statistical investigation 29 or only report change within younger generations. 38 Given the needed expansion of studies, especially clinical trials, involving older Latinos, 39 , 40 , 41 empirical documentation of even null results will ensure that statistically tested acculturation‐related phenotyping of this important and growing older adult population is available.
Study limitations should be noted. For example, although we focused our investigation on older Latinos born outside of the US/DC given differences in acculturation‐related experiences between US‐ and non–US‐born individuals, this decision may have limited the generalizability of our results. Likewise, the majority of our analytic sample was from urban Chicagoland areas, making comparisons of urban versus rural areas difficult, further limiting generalizability. While our cohort was relatively diverse, we did not have adequate representation across backgrounds to investigate potential differences in our results by country of origin (e.g., only two Cuban participants). The duration of follow‐up, while a maximum of 6 years for some participants, was, on average, 4 years. While reports of longitudinal change in familism have been noted over shorter 18 and longer 29 periods of time, it will be important to continue our longitudinal study of acculturation. Additional longitudinal follow‐up will also be important given that familism declined, on average, by 1.21 points over 4 years of follow‐up (based on female sex and median values of all other terms in the model) and it is yet to be determined if these small changes will impact behaviors known to be associated with this central ethos of the Latino community. 7 , 42 While we presented information on key factors often investigated in Latinos, that is, language‐ and social‐based acculturation, there are many other facets to acculturation that were omitted from our work, as well as individual and socioenvironmental risk and resilience factors including neighborhood‐level factors related to where our participants live that should also be considered. 19 , 43 , 44 We are actively collecting this additional information so we may consider acculturation within the context of the broader lived experience of our Latino participants.
Strengths should also be noted. Our study adds to the growing research suggesting that acculturation is multi‐dimensional; 19 that it is not a single static, trait‐like quality but a dynamic, at times evolving, construct that should be considered in all its complexities when contextualizing aging in older Latinos. Additionally, the follow‐up participation rate of Latinos with data necessary for our longitudinal analyses was high (83%). Furthermore, data was overall very complete with, on average, 93% of participants (n = 205) included in fully adjusted models. Moreover, by recoding select scores into an ordinal distribution, we were able to model non‐normal data and find robust statistical inference despite a negligible loss of information secondary to the rounding and combining of sparse observations. Last, although we lacked representation across strata from early‐ to late‐life for a formal investigation of age at migration, our participants had a wide range of age at migration (min = .57 years, max = 75), and also a wide range of years lived in the US/DC (min = 6, max = 84). Together, the information provided regarding changes (or the lack thereof) in the currently presented acculturation‐related metrics for older Latinos provides empirical data that may help inform more culturally compatible ADRD clinical trials and spur future research investigating how changes in acculturation may impact changes in cognition, and risk for ADRD.
CONFLICT OF INTEREST STATEMENT
The co‐authors of this manuscript have no conflicts of interest related to the contents of the work presented herein. Author disclosures are available in the supporting information .
Supporting information
Supporting Information
ACKNOWLEDGMENTS
We thank all the participants in the Memory and Aging Project and the Rush Alzheimer's Disease Center's (RADC) Latino Core and the Religious Orders Study as well as the research assistants, outreach and recruitment staff, as well as the Statistics and Data Management Core of the RADC. ROSMAP and Latino Core resources can be requested at https://www.radc.rush.edu. This work was supported by National Institute on Aging (grant numbers P30 AG010161, P30 AG72975, R01 AG15819, R01 AG17917, and R01 AG062711).
Lamar M, Glover CM, Capuano AW, et al. Stability and change in acculturation‐related characteristics in older Latinos: Implications for culturally compatible ADRD research. Alzheimer's Dement. 2023;9:e12380. 10.1002/trc2.12380
REFERENCES
- 1. Shaw AR, Perales‐Puchalt J, Johnson E, et al. Representation of racial and ethnic minority populations in dementia prevention trials: a systematic review. J Prev Alzheimers Dis. 2022;9(1):113‐118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Elliott CL. Together we make the difference: national strategy for recruitment and participation in Alzheimer's and related dementias clinical research. Ethn Dis. 2020;30(suppl 2):705‐708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Babulal GM, Quiroz YT, Albensi BC, et al. Perspectives on ethnic and racial disparities in Alzheimer's disease and related dementias: update and areas of immediate need. Alzheimers Dement. 2019;15(2):292‐312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lara M, Gamboa C, Kahramanian MI, et al. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367‐397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Suarez L, Pulley L. Comparing acculturation scales and their relationship to cancer screening among older Mexican‐American women. J Natl Cancer Inst Monogr. 1995(18):41‐47. [PubMed] [Google Scholar]
- 6. London L, Hurtado‐de‐Mendoza A, Song M, Nagirimadugu A, Luta G, Sheppard VB. Motivators and barriers to Latinas' participation in clinical trials: the role of contextual factors. Contemp Clin Trials. 2015;40:74‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Suarez L, Pap smear and mammogram screening in Mexican‐American women: the effects of acculturation. Am J Public Health. 1994;84(5):742‐746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Burrow‐Sanchez JJ, Hops H, A randomized trial of culturally accommodated versus standard group treatment for Latina/o adolescents with substance use disorders: posttreatment through 12‐month outcomes. Cultur Divers Ethnic Minor Psychol. 2019;25(3):311‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Venner KL, Hernandez‐Vallant A, Hirchak KA, Herron JL. A scoping review of cultural adaptations of substance use disorder treatments across Latinx communities: guidance for future research and practice. J Subst Abuse Treat. 2022;137:108716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kunst JR. Are we facing a “causality crisis” in acculturation research? The need for a methodological evolution. Int J Int Relat. 2021;85:A4‐A8. [Google Scholar]
- 11. Gilmore‐Bykovskyi AL, Jin Y, et al. Recruitment and retention of underrepresented populations in Alzheimer's disease research: a systematic review. Alzheimers Dement. 2019;5:751‐770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Glover CM, Shah RC, Bennett DA, et al. Perceived impediments to completed brain autopsies among diverse older adults who have signed a uniform anatomical gift act for brain donation for clinical research. Ethn Dis. 2020;30(suppl 2):709‐718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Marín G, Sabogal F, Marin BV, Otero‐Sabogal R, Perez‐Stable EJ. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9:183‐205. [Google Scholar]
- 14. Almeida J, Molnar BE, Kawachi I, Subramanian SV. Ethnicity and nativity status as determinants of perceived social support: testing the concept of familism. Soc Sci Med. 2009;68(10):1852‐1858. [DOI] [PubMed] [Google Scholar]
- 15. Ewing BA, Osilla KC, Pedersen ER, Hunter SB, Miles JN, D'Amico EJ. Longitudinal family effects on substance use among an at‐risk adolescent sample. Addict Behav. 2015;41:185‐191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cruz RA, Navarro C, Carrera K, Lara J, Mechammil M, Robins RW. Mexican‐origin youths' trajectories of internalizing symptoms from childhood into adolescence and associations with acculturation processes. J Clin Child Adolesc Psychol. 2021;50(1):118‐130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cruz RA, King KM, Cauce AM, Conger RD, Robins RW. Cultural orientation trajectories and substance use: findings from a longitudinal study of Mexican‐origin youth. Child Dev. 2017;88(2):555‐572. [DOI] [PubMed] [Google Scholar]
- 18. Parveen S, Morrison V. Predicting caregiver gains: a longitudinal study. Br J Health Psychol. 2012;17(4):711‐723. [DOI] [PubMed] [Google Scholar]
- 19. Lamar M, Barnes LL, Leurgans SE. Acculturation in context: the relationship between acculturation and socioenvironmental factors with level of and change in cognition in older Latinos. J Gerontol B Psychol Sci Soc Sci. 2021;76(4):e129‐e139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Marquez DX, Glover CM, Lamar M, et al. Representation of older Latinxs in cohort studies at the rush Alzheimer's disease center. Neuroepidemiology. 2020;54(5):404‐418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bennett DA, Launer LJ, Longitudinal epidemiologic clinical‐pathologic studies of aging and Alzheimer's disease. Curr Alzheimer Res. 2012;9(6):617‐620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bennett DA, Schneider JA, Aggarwal NT, et al. Decision rules guiding the clinical diagnosis of Alzheimer's disease in two community‐based cohort studies compared to standard practice in a clinic‐based cohort study. Neuroepidemiology. 2006;27(3):169‐176. [DOI] [PubMed] [Google Scholar]
- 23. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS‐ADRDA work group under the auspices of department of health and human services task force on Alzheimer's disease. Neurology. 1984;34(7):939‐944. [DOI] [PubMed] [Google Scholar]
- 24. Sabogal F, Marin G, Otero‐Sabogal R. Hispanic familism and acculturation: What changes and what doesn't? Hisp J Behav Sci. 1987;9(4):397‐412. [Google Scholar]
- 25. Campos B, Roesch SC, Gonzalez P, et al. Measurement properties of Sabogal's Familism Scale: findings from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Sociocultural Ancillary Study. J Lat Psychol. 2019;7(4):257‐272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nunnally JC, Bernstein IH. Psychometric Theory. McGraw‐Hill; 1994. [Google Scholar]
- 27. Wilson RS, Scherr PA, Schneider JA, Tang Y, Bennett DA. Relation of cognitive activity to risk of developing Alzheimer disease. Neurology. 2007;69(20):1911‐1920. [DOI] [PubMed] [Google Scholar]
- 28. Capuano AW, Dawson JD, The trend odds model for ordinal data. Stat Med. 2013;32(13):2250‐2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Vercammen KA, McClain AC, Tucker KL, Falcón LM, Mattei J. The association between baseline acculturation level and 5‐year change in adiposity among Puerto Ricans living on the mainland United States. Prev Med Rep. 2019;13:314‐320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wallen GR, Feldman RH, Anliker J. Measuring acculturation among Central American women with the use of a brief language scale. J Immigr Health. 2002;4(2):95‐102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Knight GP, Basilio CD, Cham H, Gonzales NA, Liu Y, Umaña‐Taylor AJ. Trajectories of Mexican American and mainstream cultural values among Mexican American adolescents. J Youth Adolesc. 2014;43(12):2012‐2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bleakley H, Chin A. Language skills and earnings: evidence from childhood immigrants. Rev Econ Stat. 2004;86(2):481‐496. [Google Scholar]
- 33. Killoren SE, Wheeler LA, Updegraff KA, Rodríguez de Jésus SA, McHale SM. Longitudinal associations among parental acceptance, familism values, and sibling intimacy in Mexican‐origin families. Fam Process. 2015;54(2):217‐231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Markides KS, Levin JS, Ray LA. Determinants of physician utilization among Mexican‐Americans. a three‐generations study. Med Care. 1985;23(3):236‐246. [DOI] [PubMed] [Google Scholar]
- 35. Kondo KK, Rossi JS, Schwartz SJ, Zamboanga BL, Scalf CD. Acculturation and cigarette smoking in Hispanic women: a meta‐analysis. J Ethn Subst Abuse. 2016;15(1):46‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Umaña‐Taylor AJ, Yazedjian A. Generational differences and similarities among Puerto Rican and Mexican mothers' experiences with familial ethnic socialization. J Soc Pers Relat. 2006;23(3):445‐464. [Google Scholar]
- 37. Safa MD, Umana‐Taylor AJ. Biculturalism and adjustment among U.S. Latinos: a review of four decades of empirical findings. Adv Child Dev Behav. 2021;61:73‐127. [DOI] [PubMed] [Google Scholar]
- 38. Yan J, Sim L, Schwartz SJ, Shen Y, Parra‐Medina D, Kim SY, Longitudinal profiles of acculturation and developmental outcomes among Mexican‐origin adolescents from immigrant families. New Dir Child Adolesc Dev. 2021;2021(176):205‐225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Marquez DX, Perez A, Johnson JK, et al. Increasing engagement of Hispanics/Latinos in clinical trials on Alzheimer's disease and related dementias. Alzheimers Dement. 2022;8(1):e12331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Manly JJ, Glymour MM. What the aducanumab approval reveals about Alzheimer disease research. JAMA Neurol. 2021;78(11):1305‐1306. [DOI] [PubMed] [Google Scholar]
- 41. National Institutes of Health (NIH), NIH Research, Condition, and Disease Categorization Inclusion Statistics Report National Institutes of Health, Editor. 2022.
- 42. Herrera AP, Lee JW, Nanyonjo RD, Laufman LE, Torres‐Vigil I. Religious coping and caregiver well‐being in Mexican‐American families. Aging Ment Health. 2009;13(1):84‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Abraido‐Lanza AF, Echeverria SE, Florez KR. Latino immigrants, acculturation, and health: promising new directions in research. Annu Rev Public Health. 2016;37:219‐236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hill CV, Pérez‐Stable EJ, Anderson NA, Bernard MA. The national institute on aging health disparities research framework. Ethn Dis. 2015;25(3):245‐254. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


